Abstract
Background
Carotid endarterectomy (CEA) reduces the risk of stroke in patients with symptomatic (>50%) and asymptomatic (>60%) carotid artery stenosis. Here we report the midterm results of a microsurgical non-patch technique and compare these findings to those in the literature.
Methods
From 1998 to 2009 we treated 586 consecutive patients with CEA. CEA was performed, under general anesthesia, with a surgical microscope using a non-patch technique. Somatosensory evoked potential and transcranial Doppler were continuously monitored. Cross-clamping was performed under EEG burst suppression and adaptive blood pressure increase. Follow-up was performed by an independent neurologist. Mortality at 30 days and morbidity such as major and minor stroke, peripheral nerve palsy, hematoma and cardiac complications were recorded. The restenosis rate was assessed using duplex sonography 1 year after surgery.
Results
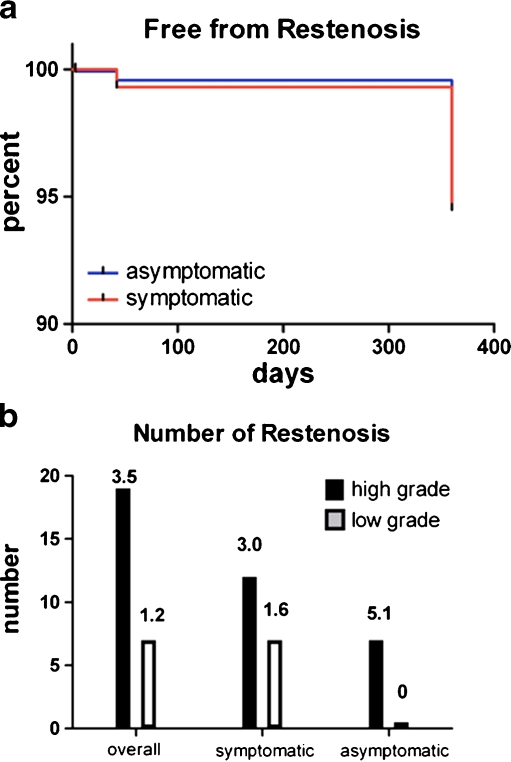
A total of 439 (75%) patients had symptomatic and 147 (25%) asymptomatic stenosis; 49.7% of the stenoses were on the right-side. Major perioperative strokes occurred in five (0.9%) patients [n = 4 (0.9%) symptomatic; n = 1 (0.7%) asymptomatic patients]. Minor stroke was recorded in six (1%) patients [n = 4 (0.9%) symptomatic; n = 2 (1.3%) asymptomatic patients]. Two patients with symptomatic stenoses died within 1 month after surgery. Nine patients (1.5%) had reversible peripheral nerve palsies, and nine patients (1.5%) suffered a perioperative myocardial infarction. High-grade (>70%) restenosis at 1 year was observed in 19 (3.2%) patients [n = 12 (2.7%) symptomatic; n = 7 (4.7%) asymptomatic patients].
Conclusions
The midterm rate of restenosis was low when using a microscope-assisted non-patch endarterectomy technique. The 30-day morbidity and mortality rate was comparable or lower than those in recently published surgical series.
Keywords: Carotid Stenosis, Asymptomatic, Symptomatic, Microsurgical, Non-patch, Restenosis
Introduction
The aim of treating patients with symptomatic or asymptomatic, middle- to high-grade stenoses of the internal carotid artery (ICA) is to reduce the risk of thromboembolic events [19, 28]. Randomized controlled trials (RCT) and meta-analyses of individual patient data have shown that this goal can be reached both by carotid endarterectomy (CEA) and carotid artery stenting (CAS) [5, 11, 18, 26]. However, there are categories of patients that seem to benefit more from either CEA or CAS [11]; current ongoing trials aim to answer these questions [15]. Even though the main aim of treatment is the prevention of thromboembolic events, rates of restenosis are an important surrogate marker for recurrent events [14]. In general, restenosis rates are lower in patients after CEA than CAS [9, 21].
Carotid endarterectomy is one of the most thoroughly investigated surgical and neurosurgical procedures. Techniques and results of CEA have evolved over the last decades, partly as a result of the rapidly progressing and challenging endovascular techniques. The superiority of CEA compared with best medical treatment in symptomatic carotid disease is clearly established as long as surgical procedures can be performed with morbidity and mortality rates of less than 6% [6]. Therefore, it is mandatory to analyze institutional results for safety and quality reasons as well as for comparison with published results of RCTs designed to evaluate CEA and CAS. Recently published series have reported lower rates of perioperative stroke and death both for CEA and CAS. In the face of this evolution, analysis of the rate of restenosis also among surgical series is increasingly important.
We therefore prospectively collected data on restenosis and outcome of all patients who underwent CEA at our neurosurgery department from May 1998 to December 2009.
Materials and methods
Patient selection
All patients scheduled for CEA because of symptomatic (≥50%) or asymptomatic (≥70%) carotid artery stenosis from May 1998 to December 2009 were prospectively assessed at the Department of Neurosurgery, Bern University Hospital, Bern, Switzerland. Admission of patients and preoperative assessment was performed by the Stroke Unit team of the Department of Neurology, Bern University Hospital, Bern, Switzerland. Patients who were considered symptomatic were those with a new ischemic neurological deficit (transient or permanent) corresponding to lesions identified by diffusion-weighted MRI.
The degree of stenosis was measured according to the North American Symptomatic Carotid Endarterectomy (NASCET) criteria by Doppler/duplex sonography, and magnetic resonance angiography (MRA) or computed tomography angiography (CTA). The percentage of stenosis was calculated using the formula: 100 × [1 - (minimal residual lumen/distal lumen)] [36]. Baseline characteristics such as age, sex, neurological and cardiovascular history as well as vascular risk factors (arterial hypertension, smoking, diabetes mellitus, obesity, positive family history and hyperlipidemia) were collected prior to treatment. This prospective study was approved by the ethics committee of the Canton of Bern, Switzerland (KEK 30/02).
Surgery
Surgery was performed by three surgeons (A.B., L.M. and M.R.). Patients were placed under general anesthesia. Neuromonitoring was achieved using intraoperative transcranial Doppler (TCD) and somatosensory evoked potentials (SSEP). Before cross-clamping, a burst-suppression EEG pattern was initiated by propofol (AstraZeneca, London, UK) administration. Intravenous heparin (100 U/kg) (Drosspharm Ltd., Basel, Switzerland) was administered prior to exposing the ICA. Patients were treated with anti-platelet agents such as acetyl salicylic acid (ASA;Bayer, Leverkusen, Germany), clopidogrel (Sanofi-Aventis, Paris, France) or both. Patients treated with warfarin were reverted and also received intravenous heparin. Cross-clamping was initiated on the ICA then the common carotid, external carotid and superior thyroid artery. If the mean TCD flow velocity dropped below 50% of the pre-clamping values and could not be restored by increasing blood pressure, or alternatively if SSEP deteriorated, an intraoperative shunt (Integra Lifesciences, Plainsboro, NJ, USA) was inserted. Before the actual endarterectomy, we inserted the shunt after placing a longitudinal incision below and above the plaque. This procedure was followed by a backflow rinse of the ICA. The initial thromboendarterectomy was performed using surgical loupes; the vessel lumen was inspected, cleaned and the arterectomy vessel’s edges sharpened. The thromboendarterectomy was completed under a neurosurgical microscope (Zeiss, Feldbach, Switzerland), and the arteriotomy was closed with a continuous 6–0 monofilament suture (Tyco Healthcare Switzerland Ltd., Wollerau, Switzerland) (Fig. 1). In patients where the distal plaque in the ICA could not be completely or smoothly removed, tacking sutures (6–0 polypropylene sutures, Covidien plc, Dublin, Ireland) were applied. The arteriotomy was closed after reopening the external carotid artery. Thereafter, the clamp on the common carotid artery was released, followed by removal of the clip on the ICA 30 s later. Flow was controlled with a small microdoppler probe (Mizuho Medical Inc., Tokyo, Japan). Hemostatic foam (Nycomed Pharma AG, Dübendorf, Switzerland) was adapted to the arteriotomy. A wound drainage was routinely placed. Closure of the wound was performed only after stopping any visual bleeding using bipolar coagulation and application of a 40°C saline imbued gauze. If diffuse bleeding could not be stopped, half of the infused heparin was antagonized with protamine (Meda Pharmaceuticals, Wangen-Brüttisellen, Switzerland). Six hours after surgery, 300 mg ASA was administered intravenously, followed by oral administration of 100 to 300 mg ASA daily. In patients who were preoperatively on clopidogrel with or without ASA for cardiac reasons, therapy was resumed 1 day after the operation.
Fig. 1.
Intraoperative situs of endarterectomy. The common carotid artery (CC) is cross-clamped. Vascular incision goes from the CC to the internal carotid artery (IC). External carotid artery (EC) cross-clamped using the vessel loop. Plaque (P) is removed and the vessel cleaned under the microscope. The vessel is closed with a 6–0 suture
Follow-up
Follow-up was performed by an independent neurologist. All neurological and non-neurological complications after CEA were assessed. Vessel patency and rate of restenosis were assessed based on color-coded duplex sonographic findings immediately after the operation and several time points postoperatively: 5 days, 6 weeks and 1 year. Secondary prevention was achieved with administration of ASA or clopidogrel each day. A statin was prescribed in select patients by the treating neurologist until 2006 and to all patients after the publication of the Stroke Prevention by Aggressive Reduction in Cholesterol Levels (SPARCL) study [2]. For classifying the restenosis rate, a postoperative ultrasound 1 year after surgery was performed. In cases of suspected restenosis, either a MRI or CTA was performed.
Death
Patients who died within 30 days after surgery were included in the database and classified as death related to surgery unless another cause was identified. Death from stroke related to a restenosis during the follow-up was recorded as well.
Postoperative stroke definitions
Major stroke was defined as a new neurological deficit lasting more than 3 days or until the clinical follow-up examination performed 30 days after surgery. Minor stroke was defined as a new neurological deficit resolving within 3 days, without causing any transient independency, occurring within 30 days after surgery.
Combined morbidity and mortality
The combined morbidity and mortality rate was defined as all deaths and neurological sequelae, including minor and major strokes, due to the operated carotid artery. Peripheral nerve palsies were assessed separately.
Hematoma
Postoperative hematoma was defined as a swelling due to a local cervical hematoma necessitating a second surgical intervention. Clinically non-relevant postoperative swelling was not recorded.
Peripheral nerve palsy
A peripheral nerve palsy was recorded if a new postoperative palsy for tongue pulling, swallowing or hoarseness was observed (hypoglossal nerve, vagal nerve or ansa cervicalis) and persisted more than 30 days.
Non-neurological complications
Complications other than those mentioned above, such as myocardial infarction (non-ST elevation and ST elevation), were recorded.
Restenosis
Restenosis was assessed 1 year after surgery by color-coded duplex sonography. Restenosis was considered high-grade if peak systolic velocity exceeded 200 cm/s. Moderate stenosis was diagnosed if peak systolic velocity exceeded 120 cm/s. If an increase in the degree of stenosis was detected, additional follow-up visits were required. A second intervention for early redo surgery or stenting was considered only if patients were symptomatic or had stenosis over 70%.
Statistics
Statistical evaluations were performed using a commercially available software package (GraphPad Software, La Jolla, CA, USA). Data are presented as the mean and standard deviation. Groups were compared using Fisher’s exact test. Significance was set at a p value of 0.05.
Results
Demographics
From 1998 to 2009, 586 consecutive patients (70% men; mean age 69.4 ± 8.8 years) were treated with microsurgical CEA at our institution. Mean age in symptomatic patients was 69.6 ± 8.8 years, while the age in asymptomatic patients was 68.8 ± 8.5 years (Table 1). Right- and left-sided stenoses were equally distributed (49.7% right, 50.3% left). Four hundred thirty-nine (75%) patients had symptomatic and 147 (25%) asymptomatic stenosis. We had a proportionally higher number of symptomatic patients in our series compared to other series, especially vascular. This can be explained by the standard referral practice used in our hospital, which refers all symptomatic stenosis patients to the neurology department and thereafter to the neurosurgery department, while asymptomatic patients are rather referred directly to vascular surgeons. As a result of this referral practice, the number of symptomatic patients operated on by neurosurgeons is higher.
Table 1.
Mean age of symptomatic and asymptomatic men and women
| Overall age (mean ± years) | Male age (mean ± years) | Female age (mean ± years) | Total n (%) | |
|---|---|---|---|---|
| Symptomatic and asymptomatic patients | 69.9 ± 8.8 | 69.0 ± 8.8 | 70.4 ± 8.9 | 586 (100%) |
| Symptomatic | 69.7 ± 8.8 | 69.2 ± 8.9 | 70.6 ± 9.5 | 439 (75%) |
| Asymptomatic | 68.8 ± 8.5 | 68.5 ± 8.4 | 69.6 ± 7.1 | 147 (25%) |
Four hundred thirty-seven patients with a symptomatic high-grade stenosis completed the 6-week follow-up examination, 397 were seen after 1 year at our institution, and the remaining 40 patients were followed up with duplex sonography in another facility or lost to follow-up. Two patients died within 30 days after surgery. Patients with duplex sonography performed in another hospital were not included into the 1-year follow-up. All 147 patients with asymptomatic high-grade stenosis completed the 6-week clinical follow-up. One hundred thirty-seven patients were seen after 1 year, and the remaining ten patients were either followed up in another facility or lost to follow-up.
Risk factors and co-morbidities
The following vascular risk factors did not differ among patients with symptomatic or asymptomatic carotid artery stenosis: arterial hypertension, diabetes, hypercholesterolemia, smoking, peripheral arterial vascular disease, obesity and family history of stroke.
Mortality, combined mortality and morbidity
Postoperative death occurred in 2/586 patients (0.34%). Both patients had suffered from a symptomatic carotid stenosis. In one patient there was a fatal intracerebral hemorrhage 72 h (h) after intravenous thrombolysis for middle cerebral artery infarction on the left side and 24 h after CEA. The second fatality was due to a cardiac arrest on postoperative day 2; no autopsy was performed.
The combined mortality and morbidity rate in all patients was 2.2% (13/586), 2.2% (10/439) in symptomatic and 2.0% (3/147) in asymptomatic patients.
Major and minor stroke
Major stroke within 30 days occurred in 5/586 patients (0.85%). Four of these patients (0.9%) were operated on for symptomatic and one patient (0.7%) for asymptomatic high-grade stenosis. Minor stroke within 30 days occurred in six cases (1%); four of these patients had high-grade symptomatic stenosis (Table 2).
Table 2.
Rate of major/minor stroke and restenosis rate in symptomatic and asymptomatic carotid stenosis
| Overall % (n) (N = 586) | Symptomatic % (n) (N = 439) | Asymptomatic % (n) (N = 147) | |
|---|---|---|---|
| Minor stroke | 1.02% (5) | 0.9% (4) | 1.4% (2) |
| Major stroke | 0.85% (5) | 0.9% (4) | 0.7% (1) |
| Restenosis (≥70%) | 3.2% (19) | 2.7% (12) | 4.7% (7) |
| Restenosis (≤69%) | 1.2% (7) | 1.6% (7) | 0% (0) |
Peripheral nerve palsies
Peripheral nerve palsy was observed in 1.53% (9/586) of patients. These deficits resolved rapidly in most of the patients. At 1 year follow-up all patients had normal function of the cranial nerves.
Non-neurological complications
Overall 14 non-neurological complications were observed. Three patients had myocardial infarctions (MI) (n = 2, non-ST elevation MI; n = 1, ST elevation MI), five had angina pectoris, and two had postoperative local infections that were treated with intravenous antibiotics. Additionally, there were two patients with hematomas that required reoperation, one patient with postoperative seizure and one with a newly diagnosed myasthenia gravis
Occlusions
Intraoperative occlusion of the carotid artery during surgery was performed in five (0.8%) patients because of preoperative occlusion and the impossibility of recanalization, and distal extension of the plaques and impossibility of successful recanalization. Three patients were symptomatic and two patients asymptomatic. In addition, one patient had postoperative blood pressure-dependent transient ischemic attacks (TIA), which resolved and did not recur after 30 days.
Restenosis after 1 year
High-grade restenosis of more than 70% occurred in 3.6% (19/534) of the patients after CEA: 3.0% (12/439) in symptomatic and 4.7% (7/147) in asymptomatic patients. Moderate-grade stenosis of 50 to 70% was observed in 1.2% (7/534) of patients; these seven patients were all symptomatic patients (Table 2, Fig. 2). Of all high- and moderate-grade restenoses, 1.1% (5/439) had symptomatic restenosis, all occurring in the preoperative symptomatic group. Stenting for high-grade restenosis was performed in 1.36% (8/586) of patients: 0.9% (4/439) in symptomatic and 2.7% (4/147) in asymptomatic patients. In one patient (0.2%) with symptomatic carotid artery stenosis reendarterectomy was performed. Restenosis rates did not differ between the pre- and post-statin era; however, the number of patients with restenosis was low in both asymptomatic (0/7) and symptomatic (2/81) patients.
Fig. 2.
a Kaplan-Meier curve: Free of restenosis (high and low grade restenosis) over time in patients with symptomatic stenosis (in red) and in patients with asymptomatic stenosis (blue). b Bars show the absolute numbers of restenosis overall in symptomatic and asymptomatic patients differentiated for high and low grade stenosis. Numbers show the percent of each group
Intraoperative shunt rate
In 11% of all operations, intraoperative shunting was used. The rate of intraoperative shunt placement in patients suffering postoperative minor or major stroke was 23%; however thromboembolic complications were not significantly more common (p = 0.112) when compared to all operated patients.
Discussion
The NASCET found an absolute risk reduction of ipsilateral stroke of 17% at 2 years in patients with stenosis higher than 70% [28]. Since then, endarterectomy has been recommended for patients with high-grade stenosis. In 1991, the European Carotid Surgery Trial (ECST) demonstrated a significant reduction of the overall stroke risk in operated patients with symptomatic high-grade stenosis (70–99% according to the ECST criteria) compared with best medical treatment [19]. The perioperative risks of stroke and death within 30 days of CEA were 6.8% (95% CI: 5.6–8.0) in the ECST and 6.7% (95% CI: 5.3–8.4%) in the NASCET populations. These risk rates were higher than those reported in many surgical case series as outlined below. The operative risk in the ECST was significantly higher in women (p < 0.0001), although this difference was not seen in the NASCET.
Since these two large multicenter trials demonstrated the benefit of CEA over best medical treatment, two clinically relevant factors have changed, leading to many new RCTs. Firstly CAS has been introduced and equipoise to CEA, defined in specific clinical circumstances. Second, best medical treatment was reinforced with statins [2], thereby rendering the risk of stroke lower than the stroke risk reduction found in NASCET and ECST. Nevertheless, the data of the NASCET and the ECST trial remain the best available for treatment of carotid artery disease. In the Carotid Revascularization Endarterectomy versus Stenting Trial (CREST), the combined rate of stroke and death was reported in 2.1% asymptomatic and 3.2% symptomatic patients with carotid stenosis having undergone CEA [25]. In a US nationwide inpatient study that included 482,394 patients having undergone CEA, the combined stroke and death rate was reported as 0.9% in the asymptomatic and 5.9% in the symptomatic group overall in high-risk and low-risk patients [20]. A meta-analysis of short-term and long-term outcomes of CAS and CEA trials reported a similar range of rates for stroke and death as previously mentioned [17]. Specifically the rates of periprocedural stroke and death were in favor of CEA compared to CAS.
Over the last decades, the CEA procedure has been constantly critically reviewed in many studies, leading to improvement and standardization. CREST has given us new trends toward the choice of indication for CEA or CAS. However, the question of restenosis is often not taken into account in these studies. Overall, various factors such as usage of surgical microscopes, patch techniques, anesthesia, neuromonitoring, intraoperative shunting and most importantly standardized screening procedures have led to a reduction of mortality and morbidity [13, 31, 32, 37].
Preoperative evaluation
Carotid artery stenosis is diagnosed by using color-coded duplex sonography to determine the degree of stenosis. This method also allows accurate assessment of plaque morphology. The exam is completed with TCD sonography of the circle of Willis and the vertebral arteries to assess the flow velocities, the direction of flow and the significance of a collateralization over the anterior and posterior communicating arteries. Intraoperative knowledge about collateral flow lowers the probability of the necessity to place an intraoperative temporary shunt, which is associated with an increased risk of embolism during placement and should thus only be performed when necessary [29, 30, 33].
At our institution, the diagnosis is always confirmed with a second imaging modality, either MRA or CTA. In addition, when determining the anatomical location and extent of the stenosis, MRA allows the visualization of past and present cerebral ischemic areas. This is important in cases of symptomatic carotid artery stenosis with large diffusion-restricted areas since the risk of post-endarterectomy hemorrhagic transformation is increased in these patients [3, 16], especially after intravenous thrombolysis [7]. The previously accepted notion that CEA should be delayed 4 to 6 weeks after stroke is challenged by more recent evidence suggesting that CEA can be safely performed earlier in clinically stable patients who have mild to moderate deficits. This is especially true for patients who have a TIA or minor stroke without or only with minimal imaging evidence of infarction or mass effect, and a stable deficit where there is no reason to empirically delay carotid endarterectomy [4].
Restenosis
As the reported perioperative risks for the treatment of carotid artery stenosis both for CEA and CAS are lower, the rate of restenosis is increasingly more important. Two to 12% of patients with treated carotid stenosis have recurrent cerebrovascular events due to a high-grade restenosis in CAS as well as CEA [14, 21]. Although CEA has overall a lower rate of restenosis rate than CAS [9, 18], the rates of restenosis of surgical series using different operative techniques also have to be reported. The addition of statins to the medical therapy has without doubt reduced the overall recurrence of restenosis [2].
The two techniques used in our series, in comparison to other surgical series, were the use of a neurosurgical microscope, resulting in thorough vessel cleaning, and minimal conserving running suture and the waiver of any additional patch. In the literature there are no data supporting the advantages of the use of a microscope over surgical loupes for CEA. Neurosurgeons tend to use the microscope more often than vascular surgeons. The microscope has one advantage over the loupes in that it enables a higher magnification with perfect coaxial illumination. Therefore, a thorough cleaning of the vessel lumen is possible even with microinstruments. Furthermore, the overlay of the running suture for the vessel closure can be kept at a minimum, resulting in no constriction and practically restoring the original size of the vessel. Guzman et al. demonstrated that intraoperatively assessed dimensions of the carotid artery (common, external and internal) after removal of stenosis corresponded to the postoperative 3D-MRA findings that showed an anatomical normalization of the vessel structure [22]. This might be a reason why our results are comparable to other series using a routine patching technique [12, 38].
Recent literature on patching, however, reports a lower restenosis rate when using polytetrafluoroethylene (PTFE) patches, revealing a superiority over Dacron or saphenous vein grafts [1, 10, 12, 32]. In a prospective randomized trial, 1 year restenosis was favorable for Gore-Tex versus Hemashield patching (2% versus 8%, respectively) [1]. In 2005, Bart et al. reported a worsening restenosis rate 400 days after CEA when comparing venous patch, primary closure and Dacron patch (7%, 11% and 16%, respectively). Byrne et al. reviewed the literature in 2007 comparing primary versus venous patching, and venous versus Dacron patching. Dacron patching performed the worst in all studies, and primary was more often worse than venous patching, leading to the conclusion that venous patching appeared to perform superiorly to primary closure [12]. Regarding this evidence, perhaps a new policy with routine use of a roof PTFE patch angioplasty might further improve the restenosis rate in the future. However, a slight increase in postoperative hemorrhage must be considered as well [35]. Less postoperative hemorrhage has been reported when using a pericard patch; in addition, restenosis with a pericard patch has been reported between 2% to 7% [23, 24, 27]. Based on our midterm analysis of restenosis from this series and the reported literature, we conclude that it is essential to continue with primary closure using a microsurgical technique. In our series, a patch enlargement did not seem necessary. However, this will need to be confirmed by long-term analysis.
Intraoperative shunt
In our series we did not find a significantly higher rate of postoperative neurological deficits related to intraoperative shunting; however, there was an observable increase in neurological deficits in this group of patients. Although the shunt was immediately placed after opening the vessel below and above the plaque and the backflow of the opened ICA rinsed the vessel, it can be hypothesized that a small amount of debris from the remaining plaque embolized and was responsible for the neurological deficits. Given that we had a higher number of symptomatic patients, an adaptation to our surgical routine may require placing the shunt only after cleaning the internal carotid artery under the microscope or only when the SSEP begins to lower.
Local anesthesia/general anesthesia
A recent Cochrane review compared local versus general anesthesia, where patients and surgeons could choose either anesthetic technique depending on the clinical situation and preferences [31]. It is difficult to ascertain the clinical differences of local anesthesia over general anesthesia. Overall, we can assume that general anesthesia remains the most common practice across all specialties performing CEA. A systematic protocol for the different steps in the endarterectomy procedure is important for the success and reduction of morbidity. Furthermore, the type of anesthesia is also dependent on the clinical condition of the patient.
Monitoring
There are a multitude of different intraoperative techniques for evaluating the necessity for an intraoperative shunt, a topic still much debated in the literature. However, in our study, the stroke risk of distal embolization tended to be higher in shunted than in non-shunted patients, although this was not statistically significant. Visual assessment of back bleeding from the ICA is probably the easiest method for subjective assessment of intracranial collateralization, but at the same time probably also the least significant. Measuring the stump pressure may be more objective, but the literature gives values for a cutoff between 25 to 70 mmHg. Despite stump pressures greater than 50 mmHg, up to 9% of patients lost consciousness and required a temporary shunt in two series of CEA performed under local and general anesthesia [8, 34]. Transcranial Doppler ultrasound is gaining increasing importance for a variety of reasons: first, it gives an objective value of flow velocities that leads to the decision to insert a temporary shunt. Second, the increase of arterial blood pressure during cross-clamping can be directly monitored, in addition to monitoring the correct functioning of a temporary shunt. Although SSEP monitoring is slower in response than TCD, it gives additional security and information, especially when TCD is not possible. The combination of TCD and SSEP monitoring in the setup of general anesthesia with routine burst suppression and adaptive blood pressure control after cross-clamping in our series led to good results also in comparison with the literature. We insert a temporary shunt if pre-cross-clamping TCD flow velocities fall to 50% and a sufficient increase in blood pressure cannot be achieved.
In our series we found non-significantly higher rates of postoperative complications in shunted patients. There are two aspects of this issue to be considered: either there is an inherent higher risk of complications using a shunt or the complication rate is higher because it is not routinely used. This can only be answered by a randomized trial with a long-term follow-up (over several years) [33].
Indication for intervention (CEA or CAS)
The recent literature reports that morbidity and mortality need to be lower than 6% in order to perform a CEA, and CAS should also achieve the same rates. It is therefore mandatory to assess results derived from local centers for both CEA and CAS. The recently published results of the CREST study further support a selection of treatment methods according to patient age and presence of symptoms [11]. The findings from our study support the use of CEA both for symptomatic and asymptomatic carotid stenosis using our technical and anesthesiology procedures. The data analysis however does not allow any further specification according to patient age or sex. Furthermore, our study was designed to ascertain the rate of restenosis and the outcome.
Conclusion
Carotid endarterectomy is a safe procedure with an overall low morbidity and mortality in patients with symptomatic and asymptomatic carotid stenosis. Microsurgical techniques using a neurosurgical microscope without patching resulted in a low midterm restenosis rate compared to other surgical series in the literature, especially using patching techniques.
Acknowledgments
The authors would like to thank Susan Wieting, Bern University Hospital, Department of Neurosurgery, Publications Office, Bern Switzerland for editing the final manuscript.
Conflicts of interest
None.
Financial disclosures
There are no financial disclosures for any author in this study
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Footnotes
This work has not been previously published or presented.
Comment
Carotid endarterectomy still represents a valuable technique in the prevention of major neurologic ischemic events in patients with significant carotid stenosis. The different techniques used for carotid artery closure after this procedure aim to guarantee low restenosis rates, both in terms of early and long-term results. Patch closure has been considered an optimal solution in order to reduce the risk of restenosis related to technical inaccuracies during carotid artery closure. The use of a microsurgical non-patch technique for primary closure compared to the standard primary closure has the appeal of eliminating those technical inadequacies in the suture line; the excellent mid-term results obtained in this series confirm this hypothesis. However, it is important to remember that restenosis could be also and maybe primarily related to miointimal hyperplasia or thrombotic apposition in the endarterectomized carotid wall. Both these events have a long time progression, and restenosis could be identified many years after the procedure. It will be really interesting to have a description of the results presented here in the future for the evaluation of long-term restenosis rates after using the micro-surgical non-patch technique. Another important issue is related to the learning curve needed for this procedure. Neurosurgeons are used to microsurgical procedures, and this represents a great advantage when compared to other specialties involved in the treatment of carotid stenosis, as vascular surgeons are. If microsurgical primary closure demonstrates comparable long-term results to patch closure in terms of reduced restenosis rate, microsurgical techniques should be included in vascular surgery training programs.
Domenico d'Avella
Franco Grego
Padova, Italy
The authors here report an institutional series of 586 CEA procedures by three surgeons over 11 years. Follow-up compliance for 1-year ultrasonography was reasonable at about 90%. Surgical skill and technique were excellent, as were the clinical results. The discussion of material issues regarding stent versus CEA and the nuances of the technique is erudite and pertinent.
The main point of this manuscript is to show that microsurgical repair of carotid arteriotomy yields a high-grade restenosis rate of 3.6% at 1 year. This is confounded a bit by the 90% follow-up rate rather than perfect data. However, the conclusion has validity; microsurgical repair with modern techniques yields excellent results.
As I have published many times (1), my preference is for collagen-impregnated Dacron patch repair in every case, no microscope. The high-grade restenosis rate has not yet been published by me, but, simply stated, it is zero at all evaluation time points, many beyond 1 year. So while I accept that these authors are superb technicians—I believe that they have done as well as can possibly be done without patch grafting—yet they still have an honest and valid figure of 3.6% recurrent high-grade stenosis. In my heart, I beleive we can still do better, and in my practice, universal patch grafting is the answer.
I have published many times and completely respect that many techniques can produce good outcomes in CEA. My technique works well for me, and I stand by it. This group shows fine results with a different technique, and I applaud them for their excellent contribution. Christopher M. Loftus
Philadelphia, PA
1. Loftus CM: Carotid Artery Surgery: Principles and Technique. 2nd edition. New York, Informa Publishing 2006.
References
- 1.Aburahma AF, Stone PA, Elmore M, Flaherty SK, Armistead L, AbuRahma Z. Prospective randomized trial of ACUSEAL (Gore-Tex) vs Finesse (Hemashield) patching during carotid endarterectomy: long-term outcome. J Vasc Surg. 2008;48:99–103. doi: 10.1016/j.jvs.2008.01.057. [DOI] [PubMed] [Google Scholar]
- 2.Amarenco P, Bogousslavsky J, Callahan A, 3rd, Goldstein LB, Hennerici M, Rudolph AE, Sillesen H, Simunovic L, Szarek M, Welch KM, Zivin JA. High-dose atorvastatin after stroke or transient ischemic attack. N Engl J Med. 2006;355:549–559. doi: 10.1056/NEJMoa061894. [DOI] [PubMed] [Google Scholar]
- 3.Ballotta E, Da Giau G, Baracchini C, Abbruzzese E, Saladini M, Meneghetti G. Early versus delayed carotid endarterectomy after a nondisabling ischemic stroke: a prospective randomized study. Surgery. 2002;131:287–293. doi: 10.1067/msy.2002.119987. [DOI] [PubMed] [Google Scholar]
- 4.Baron EM, Baty DE, Loftus CM. The timing of carotid endarterectomy post stroke. Neurol Clin. 2006;24:669–680. doi: 10.1016/j.ncl.2006.06.007. [DOI] [PubMed] [Google Scholar]
- 5.Barrett KM, Brott TG. Carotid artery stenting versus carotid endarterectomy: current status. Neurol Clin. 2006;24:681–695. doi: 10.1016/j.ncl.2006.05.003. [DOI] [PubMed] [Google Scholar]
- 6.Barrett KM, Brott TG. Management of stenosis of the extracranial internal carotid artery: endarterectomy versus angioplasty and stenting. Curr Treat Options Neurol. 2010;12:475–482. doi: 10.1007/s11940-010-0092-7. [DOI] [PubMed] [Google Scholar]
- 7.Bartoli MA, Squarcioni C, Nicoli F, Magnan PE, Malikov S, Berger L, Lerussi GB, Branchereau A. Early carotid endarterectomy after intravenous thrombolysis for acute ischaemic stroke. Eur J Vasc Endovasc Surg. 2009;37:512–518. doi: 10.1016/j.ejvs.2008.12.018. [DOI] [PubMed] [Google Scholar]
- 8.Belardi P, Lucertini G, Ermirio D. Stump pressure and transcranial Doppler for predicting shunting in carotid endarterectomy. Eur J Vasc Endovasc Surg. 2003;25:164–167. doi: 10.1053/ejvs.2002.1823. [DOI] [PubMed] [Google Scholar]
- 9.Bonati LH, Ederle J, McCabe DJ, Dobson J, Featherstone RL, Gaines PA, Beard JD, Venables GS, Markus HS, Clifton A, Sandercock P, Brown MM. Long-term risk of carotid restenosis in patients randomly assigned to endovascular treatment or endarterectomy in the Carotid and Vertebral Artery Transluminal Angioplasty Study (CAVATAS): long-term follow-up of a randomised trial. Lancet Neurol. 2009;8:908–917. doi: 10.1016/S1474-4422(09)70227-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bond R, Rerkasem K, Naylor R, Rothwell PM (2004) Patches of different types for carotid patch angioplasty. Cochrane Database Syst Rev:CD000071 [DOI] [PubMed]
- 11.Brott TG, Hobson RW, 2nd, Howard G, Roubin GS, Clark WM, Brooks W, Mackey A, Hill MD, Leimgruber PP, Sheffet AJ, Howard VJ, Moore WS, Voeks JH, Hopkins LN, Cutlip DE, Cohen DJ, Popma JJ, Ferguson RD, Cohen SN, Blackshear JL, Silver FL, Mohr JP, Lal BK, Meschia JF. Stenting versus endarterectomy for treatment of carotid-artery stenosis. N Engl J Med. 2010;363:11–23. doi: 10.1056/NEJMoa0912321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Byrne J, Feustel P, Darling RC., 3rd Primary closure, routine patching, and eversion endarterectomy: what is the current state of the literature supporting use of these techniques? Semin Vasc Surg. 2007;20:226–235. doi: 10.1053/j.semvascsurg.2007.10.006. [DOI] [PubMed] [Google Scholar]
- 13.Counsell CE, Salinas R, Naylor R, Warlow CP. A systematic review of the randomised trials of carotid patch angioplasty in carotid endarterectomy. Eur J Vasc Endovasc Surg. 1997;13:345–354. doi: 10.1016/S1078-5884(97)80074-3. [DOI] [PubMed] [Google Scholar]
- 14.Crawford RS, Chung TK, Hodgman T, Pedraza JD, Corey M, Cambria RP. Restenosis after eversion vs patch closure carotid endarterectomy. J Vasc Surg. 2007;46:41–48. doi: 10.1016/j.jvs.2007.02.055. [DOI] [PubMed] [Google Scholar]
- 15.Eckstein HH, Ringleb P, Allenberg JR, Berger J, Fraedrich G, Hacke W, Hennerici M, Stingele R, Fiehler J, Zeumer H, Jansen O. Results of the Stent-Protected Angioplasty versus Carotid Endarterectomy (SPACE) study to treat symptomatic stenoses at 2 years: a multinational, prospective, randomised trial. Lancet Neurol. 2008;7:893–902. doi: 10.1016/S1474-4422(08)70196-0. [DOI] [PubMed] [Google Scholar]
- 16.Eckstein HH, Ringleb P, Dorfler A, Klemm K, Muller BT, Zegelman M, Bardenheuer H, Hacke W, Bruckner T, Sandmann W, Allenberg JR. The Carotid Surgery for Ischemic Stroke trial: a prospective observational study on carotid endarterectomy in the early period after ischemic stroke. J Vasc Surg. 2002;36:997–1004. doi: 10.1067/mva.2002.128303. [DOI] [PubMed] [Google Scholar]
- 17.Economopoulos KP, Sergentanis TN, Tsivgoulis G, Mariolis AD, Stefanadis C. Carotid artery stenting versus carotid endarterectomy: a comprehensive meta-analysis of short-term and long-term outcomes. Stroke. 2011;42:687–692. doi: 10.1161/STROKEAHA.110.606079. [DOI] [PubMed] [Google Scholar]
- 18.Ederle J, Dobson J, Featherstone RL, Bonati LH, van der Worp HB, de Borst GJ, Lo TH, Gaines P, Dorman PJ, Macdonald S, Lyrer PA, Hendriks JM, McCollum C, Nederkoorn PJ, Brown MM. Carotid artery stenting compared with endarterectomy in patients with symptomatic carotid stenosis (International Carotid Stenting Study): an interim analysis of a randomised controlled trial. Lancet. 2010;375:985–997. doi: 10.1016/S0140-6736(10)60239-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.European Carotid Surgery Trialists' Collaborative Group Randomised trial of endarterectomy for recently symptomatic carotid stenosis: final results of the MRC European Carotid Surgery Trial (ECST) Lancet. 1998;351:1379–1387. doi: 10.1016/S0140-6736(97)09292-1. [DOI] [PubMed] [Google Scholar]
- 20.Giles KA, Hamdan AD, Pomposelli FB, Wyers MC, Schermerhorn ML. Stroke and death after carotid endarterectomy and carotid artery stenting with and without high risk criteria. J Vasc Surg. 2010;52:1497–1504. doi: 10.1016/j.jvs.2010.06.174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Goodney PP, Nolan BW, Eldrup-Jorgensen J, Likosky DS, Cronenwett JL. Restenosis after carotid endarterectomy in a multicenter regional registry. J Vasc Surg. 2010;52:897–904. doi: 10.1016/j.jvs.2010.05.005. [DOI] [PubMed] [Google Scholar]
- 22.Guzman R, Lovblad KO, Altrichter S, Remonda L, de Koning P, Andres RH, El-Koussy M, Kelly ME, Reiber JH, Schroth G, Oswald H, Barth A. Clinical validation of an automated vessel-segmentation software of the extracranial-carotid arteries based on 3D-MRA: a prospective study. J Neuroradiol. 2008;35:278–285. doi: 10.1016/j.neurad.2008.07.001. [DOI] [PubMed] [Google Scholar]
- 23.Hines GL, Feuerman M, Cappello D, Cruz V. Results of carotid endarterectomy with pericardial patch angioplasty: rate and predictors of restenosis. Ann Vasc Surg. 2007;21:767–771. doi: 10.1016/j.avsg.2007.07.005. [DOI] [PubMed] [Google Scholar]
- 24.Ladowski JM, Ladowski JS. Retrospective analysis of bovine pericardium (Vascu-Guard) for patch closure in carotid endarterectomies. Ann Vasc Surg. 2011;25:646–650. doi: 10.1016/j.avsg.2010.11.008. [DOI] [PubMed] [Google Scholar]
- 25.Mantese VA, Timaran CH, Chiu D, Begg RJ, Brott TG. The Carotid Revascularization Endarterectomy versus Stenting Trial (CREST): stenting versus carotid endarterectomy for carotid disease. Stroke. 2010;41:S31–S34. doi: 10.1161/STROKEAHA.110.595330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mas JL, Trinquart L, Leys D, Albucher JF, Rousseau H, Viguier A, Bossavy JP, Denis B, Piquet P, Garnier P, Viader F, Touze E, Julia P, Giroud M, Krause D, Hosseini H, Becquemin JP, Hinzelin G, Houdart E, Henon H, Neau JP, Bracard S, Onnient Y, Padovani R, Chatellier G. Endarterectomy Versus Angioplasty in Patients with Symptomatic Severe Carotid Stenosis (EVA-3S) trial: results up to 4 years from a randomised, multicentre trial. Lancet Neurol. 2008;7:885–892. doi: 10.1016/S1474-4422(08)70195-9. [DOI] [PubMed] [Google Scholar]
- 27.Matsagas MI, Bali C, Arnaoutoglou E, Papakostas JC, Nassis C, Papadopoulos G, Kappas AM. Carotid endarterectomy with bovine pericardium patch angioplasty: mid-term results. Ann Vasc Surg. 2006;20:614–619. doi: 10.1007/S10016-006-9102-3. [DOI] [PubMed] [Google Scholar]
- 28.North American Symptomatic Carotid Endarterectomy Trial Collaborators Beneficial effect of carotid endarterectomy in symptomatic patients with high-grade carotid stenosis. N Engl J Med. 1991;325:445–453. doi: 10.1056/NEJM199108153250701. [DOI] [PubMed] [Google Scholar]
- 29.Prioleau WH, Jr, Alken AF, Hairston P. Carotid endarterectomy: neurologic complications as related to surgical techniques. Ann Surg. 1977;185:678–683. doi: 10.1097/00000658-197706000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Reddy K, West M, Anderson B. Carotid endarterectomy without indwelling shunts and intraoperative electrophysiologic monitoring. Can J Neurol Sci. 1987;14:131–135. doi: 10.1017/s031716710002624x. [DOI] [PubMed] [Google Scholar]
- 31.Rerkasem K, Rothwell PM (2008) Local versus general anaesthesia for carotid endarterectomy. Cochrane Database Syst Rev:CD000126 [DOI] [PubMed]
- 32.Rerkasem K, Rothwell PM (2009) Patch angioplasty versus primary closure for carotid endarterectomy. Cochrane Database Syst Rev:CD000160 [DOI] [PMC free article] [PubMed]
- 33.Rerkasem K, Rothwell PM (2009) Routine or selective carotid artery shunting for carotid endarterectomy (and different methods of monitoring in selective shunting). Cochrane Database Syst Rev:CD000190 [DOI] [PubMed]
- 34.Ricotta JJ, Charlton MH, DeWeese JA. Determining criteria for shunt placement during carotid endarterectomy. EEG versus back pressure. Ann Surg. 1983;198:642–645. doi: 10.1097/00000658-198311000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rosenbaum A, Rizvi AZ, Alden PB, Tretinyak AS, Graber JN, Goldman JA, Sullivan TM. Outcomes related to antiplatelet or anticoagulation use in patients undergoing carotid endarterectomy. Ann Vasc Surg. 2011;25:25–31. doi: 10.1016/j.avsg.2010.06.007. [DOI] [PubMed] [Google Scholar]
- 36.Staikov IN, Nedeltchev K, Arnold M, Remonda L, Schroth G, Sturzenegger M, Herrmann C, Rivoir A, Mattle HP. Duplex sonographic criteria for measuring carotid stenoses. J Clin Ultrasound. 2002;30:275–281. doi: 10.1002/jcu.10078. [DOI] [PubMed] [Google Scholar]
- 37.Touze E, Trinquart L, Chatellier G, Mas JL. Systematic review of the perioperative risks of stroke or death after carotid angioplasty and stenting. Stroke. 2009;40:e683–e693. doi: 10.1161/STROKEAHA.109.562041. [DOI] [PubMed] [Google Scholar]
- 38.Verhoeven BA, Pasterkamp G, de Vries JP, Ackerstaff RG, de Kleijn D, Eikelboom BC, Moll FL. Closure of the arteriotomy after carotid endarterectomy: patch type is related to intraoperative microemboli and restenosis rate. J Vasc Surg. 2005;42:1082–1088. doi: 10.1016/j.jvs.2005.08.011. [DOI] [PubMed] [Google Scholar]