Abstract
Purpose
A series of 100 children under 2 years of age treated for hydrocephalus is described. All patients received a standard differential low-pressure (SD low) valve as the first cerebrospinal fluid (CSF) shunt treatment. The performance of this group during follow-up is analysed.
Methods
A retrospective cohort study was performed using the intern electronic health record from our hospital. Children younger than 2 years who underwent initial CSF shunt treatment with a SD low valve between 1998 and 2008 were eligible.
Results
Mean follow-up was 7 years. The majority of 81% (81 of 100) of the children did not receive an upgrade of pressure profile throughout follow-up. The first revision was done after a mean of 456 days (median, 64 days; min, 3; and max, 4,183). The 1-year survival rate of the CSF shunt in this cohort was 42%. In the relatively large group of myelomeningocele patients (37 of 100), only one patient developed symptomatic overdrainage. A total of 9% (9 of 100) of the children presented with symptoms of overdrainage. In 3% (3 out of 100) of these children, symptoms of overdrainage persisted, in spite of multiple valve mutations. During the total follow-up, 26% (26 of 100) of the patients had never received shunt revision surgery. Fifteen percent (15 of 100) of the children developed a shunt infection within the first year.
Conclusions
The use of SD low valves in the youngest age group is effective in the majority of children. The aetiology of myelomeningocele appears to protect the patient from symptomatic overdrainage.
Keywords: Hydrocephalus, Paediatric, CSF shunt, Standard differential low-pressure valve, Overdrainage
Introduction
Hydrocephalus can be defined as an active distension of the ventricular system of the brain resulting from inadequate passage of cerebrospinal fluid (CSF) from its point of production within the cerebral ventricles to its point of absorption into the systemic circulation (i.e. triventricular and communicating hydrocephalus respectively) [11]. The former is often related to an obstruction between the third and fourth ventricles while the latter does not show any morphological obstructions. The aetiology of hydrocephalus varies, and a MRI scan is important to define its cause. The overall incidence of infantile hydrocephalus is about 0.66 per 1,000 live births [8].
The most common treatment for the hydrocephalus in infants is the insertion of a CSF shunt. The alternative treatment of endoscopic third ventriculostomy (ETV) in cases of triventricular hydrocephalus is controversial in this youngest age group [3]. Therefore, CSF shunt insertion is considered standard treatment especially in young children. The adverse effects of CSF shunts are well recognized, and a shunt dysfunction is a common problem in neurosurgery. Many different types of shunts have been designed to overcome these problems, but the ideal shunt still does not exist. The shunt trial has shown that different types of valves show comparable outcomes [4, 6]. The number of different valves has been increasing ever since, but basically, these valves can be distinguished according to the differential pressure gradients: low, medium and high. In young children, there is no consensus about the best pressure gradient for valves.
We describe a series of children (n = 100) who all received a standard differential low-pressure (SD low) valve as first shunt treatment. This treatment policy is based on the hypothesis that as long as the sutures of the skull have not closed, the intracranial pressure will be low.
The overall characteristics of this cohort are analysed concerning aetiology and shunt survival rates. A more detailed analysis is presented of a subcategory of patients with serious overdrainage problems. The potential relationship between symptomatic overdrainage and the implantation of SD low valves is analysed and discussed.
Methods
Study design
The present retrospective study was approved by the Medical Ethical Committee of University Hospital Groningen (UMCG), the Netherlands. After informed consent of the parents, we investigated a retrospective cohort of children under the age of 2 years who primary received a CSF shunt with a SD low valve. All patients were treated within the period from 1998 to 2008, at UMCG. A total of 112 patients were treated with a CSF shunt during the period of inclusion. The initial treatment of 12 patients was with a SD medium-pressure valve; these were excluded from this study. Mean follow-up was 7 years.
Children from northern parts of the Netherlands are referred to our clinic. The total population of this area is about 1.7 million. All procedures were performed by a neurosurgeon or resident under supervision of a neurosurgeon.
The standard treatment of hydrocephalus in this young age group has been CSF shunt implantation using a SD low valve (PS Medical Low). This valve has an opening pressure of 5 cm CSF without an anti-siphoning device. Patients are followed by a paediatric neurologist. In the case of a suspected dysfunction, patients are referred to the neurosurgery department. Shunt failure was diagnosed after both clinical and radiological criteria. We identified overdrainage when this was indicated by MRI and explicitly clinically concluded in the medical record of the child.
Data collection
We analysed the patient records of all 100 cases concerning basic patient characteristics, aetiology of the hydrocephalus, secondary diagnoses, the dates on which the interventions where made and the type of shunt (including the pressure profile, the type of CSF diversion, cause of shunt dysfunction). Two different groups were identified. The first group contained all children who received an upgrade of the pressure profile (group 1), and the second group did not receive any upgrade (group 2). Group 1 was subdivided into two categories, i.e. category 1A (symptomatic group) that received an upgrade for overdrainage symptoms and group 1B (non-symptomatic group) that received an upgrade for shunt dysfunction without symptoms of overdrainage. The upgrading of the pressure profile in group 1B was performed during shunt revision surgery irrespective of the cause of shunt malfunction but in the absence of symptomatic overdrainage often as an additional act based on personal judgement of the neurosurgeon. No definite guidelines concerning hydrocephalus treatment in general or preference in the type of valve in particular were available at that time. Patients of category 1A were further subdivided between cases with resolved or persistent overdrainage symptoms after upgrading. Analysis took place in September 2010; SPSS 16.0 was used for the processing of data.
Results
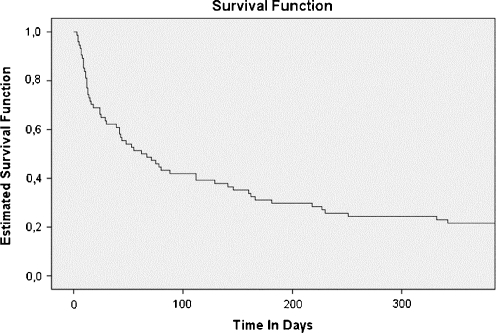
Some of the characteristics of this cohort are shown in Tables 1 and 2. The mean follow-up was 7 years. The first revision was done after a mean of 456 days (median, 64 days; min, 3; and max, 4,183). Most common complications are proximal shunt obstruction and infection. Revision surgery is carried out for shunt obstruction, malposition, overdrainage, or infection. During the first year after the initial placement of the CSF shunt, 58 out of 100 patients needed revision surgery of the CSF shunt. So the 1-year survival rate of the CSF shunt in this cohort was 42% Fig 1. During the total follow-up, 26% (26 of 100) of the patients had never received shunt revision surgery. In the course of the first year, 15% (15 of 100) of the patients developed a shunt infection. A total of 35 patients received other treatments for hydrocephalus prior to the insertion of a CSF shunt, including external ventricular drain, Ommaya reservoir, ETV or a combination of these.
Table 1.
Aetiology of hydrocephalus
| Aetiology | Total (n = 100) | 1A Symptomatic (n = 9) | 1B Non-symptomatic (n = 10) | 2 No upgrade (n = 81) |
|---|---|---|---|---|
| Myelomeningocele | 37 (37%) | 1 (11.1%) | 2 (20%) | 34 (42%) |
| Aqueductal stenosis | 13 (13%) | 2 (22.2%) | 1 (10%) | 10 (12.3%) |
| Post-infectious | 5 (5%) | 0 | 0 | 5 (6.2%) |
| IVH of prematurity | 17 (17%) | 3 (33.3%) | 2 (20%) | 12 (14.8%) |
| Congenital communicating | 3 (3%) | 0 | 1 (10%) | 2 (2.5%) |
| Posterior fossa cyst | 6 (6%) | 1 (11.1%) | 2 (20%) | 3 (3.7%) |
| Tumour (non-midbrain) | 3 (3%) | 0 | 0 | 3 (3.7%) |
| Other | 16 (16%) | 2 (22.2%) | 2 (20%) | 12 (14.8%) |
Table 2.
Characteristics of groups
| Total (n = 100) | Group 1A (n = 9) | Group 1B (n = 10) | Group 2 (n = 81) | |
|---|---|---|---|---|
| Male (%) | 60 | 4 (44.4) | 7 (70) | 49 (60.5) |
| Procedure for hydrocephalus prior to CSF shunt (%) | 35 | 5 (55.6) | 5 (50) | 25 (30.9) |
| Revision within a year (%) | 58 | 2 (22.2) | 8 (80) | 48 (59.3) |
| Total number of revisions; mean (min/max) | 2.36 (0/12) | 6.56 (2/12) | 4.5 (1/8) | 1.69 (0/6) |
| Infection within a year (%) | 15 | 1 (11.1) | 4 (40) | 10 (12.3) |
| Deceased (%) | 11 | 0 (0) | 1 (10) | 10 (12.3) |
Fig. 1.
First year shunt survival
Group 1A consisted of patients with overdrainage symptoms, which resulted in an upgrade of the pressure profile of the valve from SD low to SD medium. Nine percent (9 of 100) of the patients presented with overdrainage symptoms. In 6% (6 of 100) of the patients, the upgrade from a SD low-pressure valve to a SD medium-pressure valve resulted in adequate drainage. In the remaining 3% (3 of 100) of the patients, symptoms of overdrainage persisted.
Group 1B involved patients without symptoms of overdrainage, who received an upgrade from a SD low valve to a SD medium valve during surgery for shunt dysfunction. There was no clear indication for upgrading in these patients, but the decision was made for various reasons often not specified and based on personal judgement of the neurosurgeon.
One patient became shunt independent during the follow-up period. Eleven patients died during follow-up. The mean age at death was 614 days (median, 399 days; min, 19; max, 1,646). One patient died of shunt dysfunction. Due to a delayed referral, the patient developed increased intracranial pressure with subsequent irreversible brain damage. Another patient died of haemolytic–uremic syndrome after meningitis. The remaining nine patients died of causes not related to shunt dysfunction.
Discussion
After a mean follow-up period of 7 years, 81% (81 of 100) of the patients were adequately treated with SD low shunts. No symptoms of overdrainage were recorded in these patients. Ten patients without symptoms of overdrainage received upgrading of the SD valves from low to medium pressure during shunt dysfunction surgery irrespective of the cause of shunt malfunction as an additional act based on personal judgement of the neurosurgeon. It remains uncertain whether this intervention contributed to the prevention of symptomatic overdrainage or not.
The other nine patients received an upgrading of the SD valves because of symptoms of overdrainage. In six patients, these symptoms resolved after upgrading. However, a group of three patients was identified with persisting symptoms of overdrainage in spite of the upgrading of the valves. Replacement with various types of valves could not solve these symptoms.
An alternative treatment option is an ETV with subsequent removal of the shunt regardless of the cause of the hydrocephaly [1]. Two of our patients with persistent symptoms had the aetiology of intraventricular haemorrhage (IVH) of prematurity with patent aqueducts. An ETV has not been tried in these two patients. The third patient started with an ETV for his triventricular hydrocephalus with aqueductal stenosis at the age of 4 months. The hydrocephalus did not resolve, and a shunt was given. At the age of 3 years, a second ETV was tried in order to treat the overdrainage symptoms. Again, the ETV did not work sufficiently, and another shunt was required.
We produced ‘head circumference for age’ curves for the nine patients with symptoms of overdrainage. Four of the nine patients presented with a normal head circumference at the end of follow-up. Three of these four patients presented with persistent symptoms of overdrainage despite the upgrading of the valves. It is remarkable that the patients with persistent symptoms presented with normal head circumference. The other five presented with head circumferences with a variation of more than 1 standard deviation from the expected value at the end of follow-up: four with a small head circumference and one with a large head circumference. Unexpectedly, none of these patients presented with persistent symptoms of overdrainage. All together, these results do not show a clear association between a small head circumference and persistent symptoms of overdrainage.
In literature, an early insertion of CSF shunt is suggested to be a risk factor for developing slit ventricle syndrome with subsequent symptoms of overdrainage [5]. Only 3% (3 of 100) of the present cohort showed signs of a persistent overdrainage syndrome. As is shown in Table 3, these three patients with persistent overdrainage received initial CSF shunt treatment at a mean of 88 postnatal days. For the whole cohort, the mean time between birth and first insertion of the CSF shunt was 54 days. It remains uncertain whether there is a relation between the age of insertion between these groups and the development of symptomatic overdrainage.
Table 3.
Age at first CSF shunt insertion in days
| Age at first CSF shunt implantation in days, mean (min/max) | |
|---|---|
| Total | 54 (1/318) |
| Group 1A | |
| Whole (n = 9) | 66 (19/187) |
| Problematic (n = 3) | 88 (28/187) |
| Group 1B | 54 (2/230) |
| Group 2 | 53 (1/318) |
Analysis according to hydrocephalus aetiology revealed symptomatic overdrainage in only 1 of 37 myelomeningocele patients. Neither the patients with communicating nor those with post-infectious hydrocephalus showed any signs of overdrainage. We observed overdrainage most frequently in the etiologic subgroup of children with IVH of prematurity, 3 out of 17 patients. In our series, 2 out of 13 patients with aqueductal stenosis developed overdrainage. In one patient with persisting symptoms of overdrainage, an ETV was performed prior to the CSF shunt insertion. One may speculate whether the failed ETV had an impact on the development of symptomatic overdrainage during subsequent shunting with SD low-pressure valves. The ETV that was performed prior to the CSF shunt could have led to a situation where not only the ventricles are being drained by the shunt but also the subarachnoid space. This may have resulted in reduced volume of the subarachnoid space, which may have caused a further disruption of CSF homeostasis.
Only two out of nine from group 1A (symptomatic) needed a revision within a year after primary CSF shunt surgery versus eight out of ten from group 1B (non-symptomatic). The total number of revisions in group 1A and 1B were, respectively, 6.6 and 4.5. This implies that the patients in the symptomatic group (1A) started to develop shunt dysfunction at a later age, but continued to require more revisions after the first shunt dysfunction.
In our study, we found a 1-year shunt complication rate of 58%. In literature, rates of about 40% are found [7, 17]. This might be explained by selection and size of our series. The patients in our study were very young at first insertion of the CSF shunt. All patients were younger than 1 year of age, which is reported as a risk factor for developing shunt failure [14]. Many other studies with a lower complication rate concern ‘children’ with ages up till the age of 18 years old [12, 13, 16].
An increased risk for a second shunt dysfunction was present for patients with an early shunt dysfunction within 6 months after implantation. The risk of repeated revision in this category was 76%. Shunts that were revised after 6 months after initial implantation had a 33% risk of repeated revision. For the next revision, we found similar numbers (72% versus 50%). Similar results were found in literature. The HR for the second and third episodes of shunt failure that occurred within 6 months was approximately 1.5 times that for failures that occurred after 6 months [8].
The infection rate in our study is 15% within the first year. In literature, rates vary from 11.7% to 13.6% of the patients with a range of 3–20% in a review [10, 13, 16]. Young age at first implantation of a CSF shunt is a well-known risk factor for CSF shunt infection [10]. Nevertheless, the infection rate in our analysis of 100 patients is relatively high. Multiple studies showed radical drops in infection rates after implication of shunt protocols [2, 9]. To improve outcomes in a training hospital like ours, both infection surveillance and implementation of protocols are requiring continuous attention. The mortality rate in our series is 11%. Comparable figures can be found in the literature [15].
In spite of some limitations in this study, involving a retrospective design and relatively small number of patients, some interesting conclusions can be derived. First, the use of SD low-pressure valves in the youngest age group appears to be effective in the majority of patients. The aetiology of myelomeningocele appears to protect the patient from symptomatic overdrainage. The patients with persistent symptoms despite the upgrading of the valves presented with normal head circumference at the end of follow-up.
The findings of this study show a safe and effective use of SD low valves in young children. Future studies comparing implantation of alternative valves may indicate whether SD low valves are superior or not.
Acknowledgments
Conflict of interest
The authors declare that they have no conflict of interest.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
References
- 1.Baskin JJ, Manwaring KH, Rekate HL. Ventricular shunt removal: the ultimate treatment of the slit ventricle syndrome. J Neurosurg. 1998;88:478–484. doi: 10.3171/jns.1998.88.3.0478. [DOI] [PubMed] [Google Scholar]
- 2.Choksey MS, Malik IA. Zero tolerance to shunt infections: can it be achieved? J Neurol Neurosurg Psychiatry. 2004;75:87–91. [PMC free article] [PubMed] [Google Scholar]
- 3.Drake JM. The surgical management of pediatric hydrocephalus. Neurosurgery. 2008;62(SHC Suppl 2):SHC633–SHC642. doi: 10.1227/01.neu.0000316268.05338.5b. [DOI] [PubMed] [Google Scholar]
- 4.Drake JM, Kestle JR, Milner R, Cinalli G, Boop F, Piatt J, Jr, Haines S, Schiff SJ, Cochrane DD, Steinbok P, MacNeil N. Randomized trial of cerebrospinal fluid shunt valve design in pediatric hydrocephalus. Neurosurgery. 1998;43:294–303. doi: 10.1097/00006123-199808000-00068. [DOI] [PubMed] [Google Scholar]
- 5.Kan P, Walker ML, Drake JM, Kestle JR. Predicting slitlike ventricles in children on the basis of baseline characteristics at the time of shunt insertion. J Neurosurg. 2007;106:347–349. doi: 10.3171/ped.2007.106.5.347. [DOI] [PubMed] [Google Scholar]
- 6.Kestle J, Drake J, Milner R, Sainte-Rose C, Cinalli G, Boop F, Piatt J, Haines S, Schiff S, Cochrane D, Steinbok P, MacNeil N. Long-term follow-up data from the Shunt Design Trial. Pediatr Neurosurg. 2000;33:230–236. doi: 10.1159/000055960. [DOI] [PubMed] [Google Scholar]
- 7.Kestle JR, Walker ML. A multicenter prospective cohort study of the Strata valve for the management of hydrocephalus in pediatric patients. J Neurosurg. 2005;102:141–145. doi: 10.3171/jns.2005.102.2.0141. [DOI] [PubMed] [Google Scholar]
- 8.Persson EK, Anderson S, Wiklund LM, Uvebrant P. Hydrocephalus in children born in 1999–2002: epidemiology, outcome and ophthalmological findings. Childs Nerv Syst. 2007;23:1111–1118. doi: 10.1007/s00381-007-0324-7. [DOI] [PubMed] [Google Scholar]
- 9.Pirotte BJ, Lubansu A, Bruneau M, Loqa C, Van Cutsem N, Brotchi J. Sterile surgical technique for shunt placement reduces the shunt infection rate in children: preliminary analysis of a prospective protocol in 115 consecutive procedures. Childs Nerv Syst. 2007;23:1251–1261. doi: 10.1007/s00381-007-0415-5. [DOI] [PubMed] [Google Scholar]
- 10.Prusseit J, Simon M, von der Brelie C, Heep A, Molitor E, Volz S, Simon A. Epidemiology, prevention and management of ventriculoperitoneal shunt infections in children. Pediatr Neurosurg. 2009;45:325–336. doi: 10.1159/000257520. [DOI] [PubMed] [Google Scholar]
- 11.Rekate HL. A contemporary definition and classification of hydrocephalus. Semin Pediatr Neurol. 2009;16:9–15. doi: 10.1016/j.spen.2009.01.002. [DOI] [PubMed] [Google Scholar]
- 12.Shah SS, Hall M, Slonim AD, Hornig GW, Berry JG, Sharma V. A multicenter study of factors influencing cerebrospinal fluid shunt survival in infants and children. Neurosurgery. 2008;62:1095–1102. doi: 10.1227/01.neu.0000325871.60129.23. [DOI] [PubMed] [Google Scholar]
- 13.Simon TD, Hall M, Riva-Cambrin J, Albert JE, Jeffries HE, Lafleur B, Dean JM, Kestle JR, Network Hydrocephalus Clinical Research. Infection rates following initial cerebrospinal fluid shunt placement across pediatric hospitals in the United States. J Neurosurg Pediatr. 2009;4:156–165. doi: 10.3171/2009.3.PEDS08215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tuli S, Drake J, Lawless J, Wigg M, Lamberti-Pasculli M. Risk factors for repeated cerebrospinal shunt failures in pediatric patients with hydrocephalus. J Neurosurg. 2000;92:31–38. doi: 10.3171/jns.2000.92.1.0031. [DOI] [PubMed] [Google Scholar]
- 15.Tuli S, Tuli J, Drake J, Spears J. Predictors of death in pediatric patients requiring cerebrospinal fluid shunts. J Neurosurg. 2004;100:442–446. doi: 10.3171/ped.2004.100.5.0442. [DOI] [PubMed] [Google Scholar]
- 16.Vinchon M, Dhellemmes P. Cerebrospinal fluid shunt infection: risk factors and long-term follow-up. Childs Nerv Syst. 2006;22:692–697. doi: 10.1007/s00381-005-0037-8. [DOI] [PubMed] [Google Scholar]
- 17.Wu Y, Green NL, Wrensch MR, Zhao S, Gupta N. Ventriculoperitoneal shunt complications in California: 1990 to 2000. Neurosurgery. 2007;61:557–562. doi: 10.1227/01.NEU.0000290903.07943.AF. [DOI] [PubMed] [Google Scholar]