Abstract
Aims: It is unclear whether co-morbid anxiety disorders predict worse drinking outcomes during attempts to change drinking behavior. Studies have yielded mixed results, and have rarely examined drinking outcomes based on a specific type of anxiety disorder. Women with alcohol use disorders (AUDs) are of particular interest as they are at risk for co-morbid anxiety [Kessler et al. (1997) Lifetime co-occurrence of DSM-III-R alcohol abuse and dependence with other psychiatric disorders in the national co-morbidity survey. Arch Gen Psychiat 54:313–21]. Methods: Participants were 260 women with AUDs participating in an alcohol-treatment outcome studies. The Timeline Follow-Back was used to assess drinking frequency (percent days drinking) prior, within and 6 months post-treatment. The current study tested the hypothesis that having at least one lifetime anxiety disorder diagnosed at baseline using the Structured Clinical Interview for DSM Disorders would be associated with more drinking at all study time points. Exploratory analyses examined patterns of drinking outcomes by specific anxiety diagnoses. Results: Lifetime anxiety diagnosis was linked to poorer drinking outcomes post-treatment (β = 0.15, P = 0.020), despite less frequent drinking prior to treatment. Analyses by specific anxiety diagnosis indicated that generalized anxiety disorder predicted poorer drinking outcomes within treatment (β = 0.14, P = 0.018) and during follow-up (β = 0.16, P = 0.014). Conclusion: Co-morbid anxiety problems complicate treatment for AUDs among women. Further, specific anxiety disorders should be evaluated as distinct constructs as evidenced by the differential outcomes related to generalized anxiety disorder. Implications for treatment development for women with AUDs are discussed.
INTRODUCTION
Alcohol use disorders (AUDs) are among the most frequently diagnosed disorders, with a 12-month prevalence rate of 8.5%, occurring among 17.6 million adults in the USA (Grant et al., 2004). Although men are more likely than women to be diagnosed with an AUD (Kessler et al., 1997; Kessler et al., 2005b), and are more likely to engage in heavy or hazardous drinking (Caldwell et al., 2002), women with AUDs are likely to experience more negative consequences from drinking, including an increase in alcohol-related medical problems and higher death rates (Smith and Weisner, 2000; Epstein and Menges, 2012). Women with AUDs also differ from men in terms of reasons for drinking and motivations for quitting. Research shows that women drink in response to relationship or affective issues more often than men (Duckert, 1987; McCrady et al., 2003), and cite reasons to quit drinking related to marital, emotional and social criticism (Duckert, 1987; Brady et al., 2007).
Co-occurrence of AUDs and anxiety disorders are of particular interest in relation to women. Women with AUDs are more likely to meet the criteria for a lifetime co-morbid anxiety disorder (60.7%) in comparison to men with AUDs (35.0%; Kessler et al., 1997, 2005a). Among adults seeking treatment for an AUD, 33.3% were diagnosed with at least one current co-morbid anxiety disorder (Grant et al., 2004). Dual diagnoses may complicate treatment response for individuals in treatment for an AUD, especially for women. First, co-morbid disorders may be difficult for clinicians to diagnose during initial assessment (Kushner et al., 2005; Brady et al., 2007). For instance, men are significantly more likely to identify an AUD as their only or primary disorder, whereas women are more likely to identify an AUD as secondary and to have another current psychiatric disorder (Kessler et al., 1997; Epstein and Menges, 2012). Further, women may deny problems related to their alcohol use (Brady et al., 2007). Second, having a co-morbid anxiety diagnosis or elevated sensitivity of anxiety and related sensations has been associated with increased substance use severity (Stewart et al., 2001; Buckner et al., 2008; Schneier et al., 2010; Gillihan et al., 2011). Third, individuals with co-morbid anxiety disorders are less likely to seek treatment (Schneier et al., 2010), drop out of AUD treatment at significantly higher rates (Haver and Gjestad, 2005), and are more likely to relapse (Driessen et al., 2001; Kushner et al., 2005). Finally, some research suggests that individuals with co-morbid anxiety disorders may have difficulty quitting drinking (e.g. Driessen et al., 2001; Back et al., 2005; Haver and Gjestad, 2005; Kushner et al., 2005; Drisessen et al., 2008; Smith and Book, 2010), though other studies have found no differential outcomes (Marquenie et al., 2006). Further research is needed to clarify this predictive role of co-morbid anxiety disorder, especially among women where it is more prevalent.
The purpose of the current study was to examine the predictive value of co-morbid anxiety disorders for drinking among women with AUDs (n = 260). We hypothesized that the presence of a lifetime (current or past history) and current co-morbid anxiety diagnosis would be associated with greater alcohol consumption before, during and after treatment for drinking, per findings from Kushner et al. (2005), than women never diagnosed with any anxiety disorder. Further, little research has examined AUD treatment outcomes comparing a range of specific co-morbid anxiety disorders. Rather, studies have typically focused on only one specific anxiety diagnosis [e.g. social anxiety, Haver and Gjestad, 2005; panic disorder, Driessen et al., 2001; post-traumatic stress disorder (PTSD), Back et al., 2005; generalized anxiety disorder (GAD), Smith and Book, 2010] and as a result have been unable to compare results to AUD patients with other types of anxiety disorders. Perhaps specific characteristics of individual anxiety disorders make it harder to cease drinking (Kushner et al., 2005). Therefore, in the current study, a range of specific anxiety disorders were examined in women with AUDs to understand how response to alcohol treatment may vary across different anxiety diagnoses, including GAD, PTSD, panic disorder and social phobia.
MATERIALS AND METHODS
Participants
Participants were 260 women with AUDs participating in two randomized clinical trials comparing manual-based cognitive-behavioral treatments for AUDs.
Women from both samples were actively recruited by community advertisements and local referrals. Eligible participants were female, diagnosed with current alcohol abuse or dependence, had consumed alcohol within the past 60 (Study 1) or 30 (Study 2) days, and were married, cohabiting for at least 6 months, or in a committed heterosexual relationship for at least 1 year. Participants were excluded if either the women or their partners reported current (last 6 months) symptoms of psychosis, gross cognitive impairment or current physiological dependence on drugs (except for nicotine). In Study 1, the spouse/partner had to agree to be involved in assessment and possibly treatment aspects of the program. Spouses/partners of some of the participants in Study 2 had to agree to be involved in the treatment (see below).
Procedure
Potentially eligible women were screened via a brief telephone interview, and then were scheduled for an in-person clinical intake interview with a master's or doctoral level study clinician. After providing informed consent, eligible and interested participants scheduled a subsequent in-person baseline interview with a trained interviewer who collected further drinking and psychopathology data.
All women received weekly outpatient cognitive-behavioral treatment (CBT) for AUDs (Epstein and McCrady, 2009; McCrady and Epstein, 2009), either individual or couples-based. Study 1 (McCrady et al., 2009) compared the efficacy of individual versus couple CBT in a randomized trial of 20 sessions over 6 months. For Study 2, women were allowed to choose between an individual arm and a couple arm of treatment, in each of which two different variations of individual and couples treatments (respectively) were compared over 12 sessions spanning 3–4 months. In the individual arm, women were randomly assigned to gender neutral versus female-specific CBT; in the couple arm, women were randomly assigned to alcohol behavioral couple therapy with spouse involvement for all sessions versus a ‘blended’ individual/couple CBT treatment with spouse attendance at 6 of 12 sessions. In both studies, individual CBT covered both alcohol-focused and general coping skills (e.g. self-monitoring, functional analysis, problem-solving, relapse prevention, etc.) with an overall treatment goal of abstinence. In Study 2, female-specific individual CBT additionally addressed key areas of concern (in one session each) for women drinkers including: managing and improving social networks; coping with anxiety and negative affect; managing anger and assertiveness training, and also incorporated female-specific themes into each session: (a) autonomy/self-confidence, and (b) balancing self-care versus caring for others. In both Studies 1 and 2, couple CBT included the same components as individual treatment (alcohol focused and general coping skills), but with the spouse present for either all or half of the therapy sessions. The couple protocol also focused on increasing spouse support for abstinence, improving communication, promoting joint-problem solving and identifying the partner's role in triggering drinking or urges.
For both studies, follow-up assessments were conducted immediately post-treatment (to collect within treatment data) and 6 months post-treatment. Participants were compensated for their participation in the research aspects of the program. The majority of the women completed the immediate post-treatment assessment (n = 227, 87.3%) and 211 (81.2%) provided data 6 months post-treatment. Follow-up attrition rates were compared for women with lifetime history of anxiety diagnosis assessed at baseline (n = 81, 31.2%) to women with no pre-treatment history of anxiety. Immediately post-treatment, 81.5% (n = 66) of the women with a lifetime anxiety diagnosis provided follow-up data, in comparison with 89.9% (n = 161) of the women with no anxiety history; χ2 analysis approached but did not meet statistical significance [χ2 (1, n = 260) = 3.6, P = 0.06]. Six months post-treatment, 75.3% (n = 61) of the women with a lifetime anxiety disorder provided follow-up data, in comparison to 83.8% (n = 150) of women with no anxiety history; these attrition rates were not significantly different based on a χ2 analysis.
Measures
The Structured Clinical Interview for DSM Disorders (First et al., 2002) was used to diagnose lifetime anxiety disorders and AUDs. In Study 2, PTSD was diagnosed using the PTSD section of the Psychiatric Research Interview for Substance and Medical Disorders (Hasin et al., 1996). The Timeline Follow-back Interview (Sobell and Sobell, 1996), a calendar-based interview, was used to assess daily alcohol consumption. Frequency of drinking [percent days drinking (PDD)] was calculated from 90 days prior to the last drink before the baseline interview, to 6 months following treatment.
Data management and data analyses
Samples were combined considering the nearly identical inclusion criterion and manual-based treatment protocols for AUDs. Descriptive analyses were completed prior to combining of samples to ensure acceptable compatibility between the groups. There were no significant differences in age, race, years in relationship, number of children, years of education, income or pre-treatment drinking frequency.
All data were checked for missing values, coding errors and logical inconsistencies. Discrepancies were resolved and corrected. Data were also checked for skewness, kurtosis and outliers. Cross tabulations and t-tests were used for descriptive purposes and to calculate attrition rates. A series of hierarchical regressions (Cohen and Cohen, 1983) were used to examine the validity of the predictive variables in predicting PDD within and 6 months post-treatment. Separate regression analyses were run for each independent variable (lifetime anxiety diagnosis, panic disorder, PTSD and GAD). The baseline value of the dependent variable and study number (either 1 or 2) were entered first into the model as a covariate at Step 1. All predictor variables were dummy coded (0, no diagnosis, 1, positive diagnosis).
RESULTS
Descriptive overview
Women were on average 46.3 years of age (SD = 9.1), primarily white (95.4%) and married (83.8%). Women were highly educated (M = 14.9 years of schooling, SD = 2.6) and were of higher socioeconomic status (median household income of $90 000). Women were diagnosed with alcohol dependence (98.5%) or abuse (1.5%), and were on average drinking on 69.0% of the 90 days pre-baseline (SD = 27.68), consuming an average of 7.3 drinks per drinking day (SD = 4.5).
Co-morbid Axis I psychiatric disorders were common. The majority of women had a lifetime co-morbid diagnosis (62.7%) of women, and 28.4% had multiple diagnoses ranging from two to seven. With regard to current co-morbidity, 41.5% presented with at least one additional psychiatric disorder, and 16.5% had more than one diagnosis, ranging from two to three. Specifically, approximately one-third (31.2%) of women had at least one lifetime anxiety diagnosis (current or past) at baseline, while ∼ 8.2% had multiple lifetime anxiety diagnoses. GAD (12.7%) and panic disorder (14.6%) were the most frequently diagnosed anxiety disorders. PTSD (5.8%), social phobia (4.2%) and OCD (2.7%) were less common, although they occurred at higher rates than in the general population. Current rates were as follows: any current anxiety diagnosis (20%), panic disorder (4.6%), social phobia (3.5%), PTSD (2.7%) and OCD (0.4%).Owing to the low prevalence of OCD, this diagnosis was not examined individually in regression analyses.
Other lifetime non-anxiety or substance use disorders (i.e. mood disorders and eating disorders in the current assessment battery) were present among 44.6% of women, which was predominated by depression (81.0%). Co-occurrence of lifetime anxiety and mood disorders was prevalent among 16.9% of women, and anxiety occurring with eating disorders was 7.3%.
Inferential statistics (t-test) revealed that women with at least one co-morbid lifetime anxiety diagnosis assessed at baseline showed a trend toward less frequent drinking (PDD) prior to treatment, in comparison with non-anxious women (M = 64.2, SD = 28.7 versus M = 71.2, SD = 27.0), t(258) = 1.88, P = 0.062. When each specific anxiety disorder was tested, only GAD demonstrated the same pattern of results, that women with the co-occurring anxiety diagnosis had a significantly lower PDD prior to treatment: Pre-treatment PDD for women with GAD was 58.4 (SD = 29.9) versus that without GAD, which was M = 70.5 (SD = 27.1), t(258) = 2.4, P = 0.018. There were no differences in pre-treatment PDD by the number of lifetime or current anxiety diagnoses, or among women with and without other lifetime Axis I disorders (i.e. mood and eating disorders).
Anxiety disorders as predictors of drinking outcomes
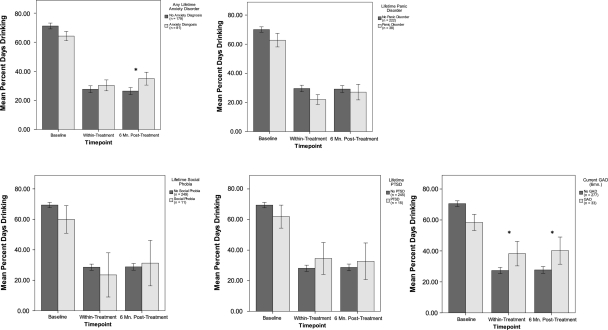
All regression analyses included covariates of baseline value of outcome measure as well as Study (1 or 2). Table 1 summarizes regression results for anxiety disorders. The presence of any lifetime anxiety disorder pre-treatment did not significantly predict within treatment variance in PDD, but did predict higher PDD 6 months post-treatment (β = 0.15, P = 0.020), accounting for 2.2% of added variance in drinking, in addition to the 15.0% of variance already accounted for by covariates. The presence of a lifetime panic disorder, social phobia or PTSD diagnosis did not significantly predict variance in PDD post-treatment or during follow-up. However, GAD diagnosis at baseline predicted higher PDD within treatment (β = 0.14, P = 0.018), accounting for an additional 2.0% (R2 change) of the variance in drinking, over and above the 20.2% of the variance already accounted for. GAD diagnosis also predicted higher PDD 6 months post-treatment (β = 0.16, P = 0.014), accounting for 2.5% (R2 change) of added variance, above 15.0% variance from covariates (see Fig. 1 for a graph of results).
Table 1.
Summary of results for separate regressions of PDDs within and 6-month post-treatment on any anxiety diagnosis and also on each specific diagnosis
| Dependent variable | Predictor | B | Standard error | β |
|---|---|---|---|---|
| PDD within treatment | Any lifetime anxiety | 4.03 | 3.97 | 0.06 |
| Any current anxiety | 11.38 | 4.80 | 0.14** | |
| Lifetime panic disorder | −4.09 | 5.06 | 0.05 | |
| Current panic disorder | 0.46 | 8.77 | 0.01 | |
| Lifetime social phobia | 2.08 | 11.26 | 0.01 | |
| Current social phobia | 3.02 | 12.33 | 0.02 | |
| Lifetime PTSD | 9.09 | 8.37 | 0.07 | |
| Current PTSD | 24.10 | 12.19 | 0.19* | |
| Current GAD | 14.15 | 5.94 | 0.14* | |
| PDD 6 months post-treatment | Any lifetime anxiety | 10.21 | 4.37 | 0.15* |
| Any current anxiety | 17.59 | 5.41 | 0.21** | |
| Lifetime panic disorder | 0.92 | 5.68 | 0.01 | |
| Current panic disorder | 8.33 | 11.20 | 0.05 | |
| Lifetime social phobia | 8.92 | 12.07 | 0.05 | |
| Current social phobia | 16.96 | 13.20 | 0.08 | |
| Lifetime PTSD | 7.20 | 9.42 | 0.05 | |
| Current PTSD | 13.39 | 12.14 | 0.07 | |
| Current GAD | 16.85 | 6.79 | 0.16* |
Baseline PDD and study number (1 or 2) were covariates in all models.
B denotes unstandardized regression coefficient.
*P < 0.05.
**P < 0.01.
Fig. 1.
PDD at baseline, within treatment, and 6 months post-treatment by lifetime anxiety diagnosis at baseline. Error bars represent +/− 1 Standard Error *p < .05.
Next, we examined whether the pattern of results remained similar when only current baseline anxiety disorders were considered. The results were largely unchanged, with the exception of within treatment drinking. Any current diagnosis predicted significantly higher PDD within treatment (β = 0.14, P = 0.018), accounting for 2.0% (R2 change) of added variance. Similarly, current PTSD at baseline predicted higher PDD within treatment (β = 0.12, P = 0.049), explaining 1.4% (R2 change) unique variance above the 20.2% accounted for by covariates.
Considering the high prevalence of both anxiety and mood disorders at baseline, hierarchical regression analyses were conducted to determine the relative contribution of these disorders of variance to drinking outcomes. Baseline PDD and study number were entered as covariates in Step 1, any mood disorder in Step 2 and any anxiety disorder in Step 3.
Within treatment, lifetime anxiety did not predict significant variance in PDD after controlling for lifetime mood diagnosis, but did account for variance in PDD at 6-month follow-up, over and above covariates in Step 1 and lifetime mood disorder, at a trend level (R2 change = 1.4%, β = 0.13, P = 0.058). With regard to past month disorders, current anxiety diagnosis at baseline accounted for significant variance in within treatment PDD above Step 1 covariates and current mood disorder (R2 change = 1.4%, β = 0.12, P = 0.047). Similarly, current anxiety diagnosis predicted significant variance in PDD at 6-month follow-up (R2 change = 4.5%, β = 0.22, P = 0.001) above Step 1 covariates and current mood disorder.
DISCUSSION
In the current study, we provided a descriptive overview of co-morbid anxiety disorders in a sample of women seeking treatment for AUDs. We also examined anxiety disorders as moderators of alcohol-treatment outcomes. One-third of the sample had at least one lifetime anxiety disorder. Studies of the general population and treatment-seeking adults have found comparable rates of co-morbid anxiety (Grant et al., 2004; Schneier et al., 2010), though some studies have reported higher rates (Kushner et al., 2005; Smith and Book, 2010). We found that GAD was among the most frequent occurring anxiety disorder with AUDs, with PTSD and OCD least common.
Contrary to our hypothesis, women with at least one lifetime anxiety disorder averaged less frequent alcohol use prior to treatment than did women without an anxiety disorder. A similar pattern was observed for GAD. It may be that for women with co-morbid anxiety along with their alcohol use problem, the distress related to anxiety contributed to their motivation to seek treatment rather than distress related to a drinking problem alone.
Interestingly, lifetime and current anxiety diagnosis was linked to drinking outcomes, despite less frequent drinking prior to treatment. Women with at least one lifetime or current anxiety diagnosis demonstrated greater difficulty maintaining treatment gains after starting alcohol treatment and during follow-up. This finding was significant over and above variance predicted by baseline mood diagnosis. These results are comparable with those of Kushner et al. (2005) who found that individuals with any anxiety diagnosis versus those with without an anxiety disorder were less successful in reducing their drinking. In terms of predictive value of specific disorders, a current GAD diagnosis at baseline was predictive of greater drinking frequency within treatment and for at least 6 months following treatment. Current, but not lifetime, PTSD at baseline was predictive of greater alcohol consumption within treatment only. These were the only specific anxiety disorders that were associated with poorer outcomes.
GAD is characterized by pathological, uncontrollable, chronic worry and anxiety about potential negative outcomes of day-to-day events, such as safety of family members not present, inability to pay bills, poor performance at school, etc. (Barlow et al., 2007). PTSD is a common reaction to a traumatic event, and is characterized by persistent re-experiencing of the trauma memory (e.g. nightmares, flashbacks), increased arousal (e.g. insomnia, exaggerated startle response, irritability) and maintained by behavioral and emotional avoidance (Kessler, 2000). Sustained increased arousal levels present in GAD and PTSD have been linked to repeated worry and maladaptive coping methods that may function to avoid more negative affect. This pervasive nature of these disorders may contribute to difficulties decreasing drinking. Additionally, women who drink also may be particularly lacking in skills allowing them to tolerate discomfort and uncertainty.
In contrast, Kushner et al. (2005) examined rates of relapse across type of co-morbid anxiety disorder and found that social phobia was the strongest predictor of drinking after treatment, and that panic disorder was predictive of a return to alcohol dependence post-treatment. There are a few notable differences between the samples that may account for the variance in results on specific anxiety diagnoses. The current study examined the role of anxiety in drinking outcomes in an all-female AUD sample, whereas Kushner et al.'s sample was predominately male (64.2%). It is possible that the predictive value of specific anxiety disorders is dependent on gender. Further, the studies varied in treatment setting and protocol (i.e. weekly outpatient CBT versus 21-day residential treatment). It is possible that certain types of AUD interventions may be better suited for some anxiety disorders over others. These results also may support the use of dual-treatment methods, which would address both anxiety and drinking. There are a few study limitations that should be noted. While we consider this a treatment-seeking sample (i.e. women responded to advertisements to participate in a treatment study and presented with a relatively severe psychopathology, these results may differ from others samples of women who are recruited directly from treatment clinics. Next, the homogeneity of the current sample may have limited the variance in and possible generalizability of outcomes. The study recruited only women, all of whom were required to be married or in a committed relationship. Women were also generally well educated and of a relatively high mean socioeconomic status. Additionally, women with co-morbid anxiety disorders were not specifically recruited for the study, so while this gives a more generalizable estimate of the prevalence of anxiety in an AUD treatment-seeking women, it may have resulted in a smaller percentage of women in the ‘anxious’ group relative to previous studies. This reduced the statistical power of the analyses, particularly to detect differences as a function of specific anxiety disorders, relative to a study in which anxious women were specifically recruited.
Nonetheless, a strength of the current study is that it is one of few to examine the baseline, within and post-treatment drinking as a function of several different anxiety disorders within a large sample. Future studies should consider including a dimensional measure of anxiety, as the current results do not evaluate the severity of anxiety diagnoses, therefore, it is unclear whether or not these co-morbid women had more severe anxiety disorders. Further, it is unknown how the co-morbid anxiety diagnoses changed over the course of treatment.
There are several noteworthy implications. When clinicians are initially assessing women with AUDs, particular focus should be paid to diagnosing anxiety disorders in general, and GAD and PTSD in particular, to determine the need for adjunct interventions or treatments targeted to alleviate the anxiety problem. Assessing previous anxiety pathology or level of anxiety sensitivity is important even if a current anxiety diagnosis is not present. With regard to treatment protocols, CBT is highly recommended for co-morbid anxiety and AUDs (Brady et al., 2007); however, serotonin reuptake inhibitors have shown to be efficacious as well (e.g. Brady et al., 2005; Book et al., 2008). Researchers should consider examining additional treatment modules to address anxiety symptoms, including interoceptive exposures (Zvolensky et al., 2008; Gillihan et al., 2011) and practice tolerating uncertainty, which may aid in habituation to unpleasant or uncomfortable worries and bodily sensations. The current study used different types of CBT treatments for AUDs, including individual CBT (gender neutral and female-specific) and couple CBT (standard and ‘blended’ individual/couple). Our team previously found that women with AUDs who were randomized to couple CBT, versus gender neutral individual CBT, had superior drinking outcomes (McCrady et al., 2009). The female-specific CBT treatment may be particularly helpful for women with a co-morbid anxiety diagnosis, as it uniquely addresses anxiety and depression, each in a single session. This, and other specific treatment condition effects, will be examined by subsequent studies from the current data in the future.
Funding
This work was supported by the National Institute on Alcohol Abuse and Alcoholism (R37 AA07070 and T32 AA07569 to B.S.M. and E.E.E.).
Conflict of interest statement. None declared.
REFERENCES
- Back SE, Jackson JL, Sonne S, et al. Alcohol dependence and posttraumatic stress disorder: differences in clinical presentation and response to cognitive-behavioral therapy by order of onset. J Subst Abuse Treat. 2005;29:29–37. doi: 10.1016/j.jsat.2005.03.002. [DOI] [PubMed] [Google Scholar]
- Barlow DH, Allen LB, Basden SL. Psychological treatments for panic disorders, phobias, and generalized anxiety disorder. In: Nathan PE, Gorman JM, editors. A Guide to Treatments that Work. New York: Oxford University Press; 2007. pp. 351–95. [Google Scholar]
- Book SW, Thomas SE, Randall PK, et al. Paroxetine reduces social anxiety in individuals with a co-occurring alcohol use disorder. J Anxiety Disord. 2008;22:310–8. doi: 10.1016/j.janxdis.2007.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brady KT, Sonne S, Anton RF, et al. Sertraline in the treatment of co-occurring alcohol dependence and posttraumatic stress disorder. Alcohol Clin Exp Res. 2005;29:395–401. doi: 10.1097/01.alc.0000156129.98265.57. [DOI] [PubMed] [Google Scholar]
- Brady KT, Tolliver BK, Verduin ML. Alcohol use and anxiety: diagnostic and management issues. Am J Psychiat. 2007;164:217–21. doi: 10.1176/ajp.2007.164.2.217. [DOI] [PubMed] [Google Scholar]
- Buckner JD, Timpano KR, Zvolensky MJ, et al. Implications of co-morbid alcohol dependence among individuals with social anxiety disorder. Depress Anxiety. 2008;25:1028–37. doi: 10.1002/da.20442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caldwell TM, Rodgers B, Jorm AF, et al. Patterns of association between alcohol consumption and symptoms of depression and anxiety in young adults. Addiction. 2002;97:583–95. doi: 10.1046/j.1360-0443.2002.00092.x. [DOI] [PubMed] [Google Scholar]
- Cohen J, Cohen P. Applied Multiple Regression/Correlation Analysis for the Behavioral Sciences. Hillsdale, NJ: Erlbaum; 1983. 2nd edn. [Google Scholar]
- Driessen M, Meier S, Hill A, et al. The course of anxiety, depression and drinking behaviours after completed detoxification in alcoholics with and without co-morbid anxiety and depressive disorders. Alcohol Alcohol. 2001;36:249–55. doi: 10.1093/alcalc/36.3.249. [DOI] [PubMed] [Google Scholar]
- Drisessen M, Schulte S, Luedecke C, et al. Trauma and PTSD in patients with alcohol, drug, or dual dependence: a multi-center study. Alcohol Clin Exp Res. 2008;32:481–8. doi: 10.1111/j.1530-0277.2007.00591.x. [DOI] [PubMed] [Google Scholar]
- Duckert F. Recruitment into treatment and effects of treatment for female problem drinkers. Addict Behav. 1987;12:137–50. doi: 10.1016/0306-4603(87)90020-7. [DOI] [PubMed] [Google Scholar]
- Epstein EE, McCrady BS. Overcoming Alcohol Problems: a Cognitive-Behavioral Treatment Program: Therapist Guide. New York, NY: Oxford University Press; 2009. [Google Scholar]
- Epstein EE, Menges D. Women and addiction. In: McCrady BS, Epstein EE, editors. Addictions: A Comprehensive Guidebook. 2nd edn. New York: Oxford University Press; 2012. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, et al. Structured Clinical Interview for the DSM-IV-TR Axis I Disorders, Research Version, Patient Edition (SCID-I/P) New York: Biometrics Research, New York State Psychiatric Institute; 2002. [Google Scholar]
- Gillihan SJ, Farris SG, Foa EB. The effect of anxiety sensitivity on alcohol consumption among individuals with comorbid alcohol dependence and posttraumatic stress disorder. Psychol Addict Behav. 2011;25:721–6. doi: 10.1037/a0023799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the national epidemiologic survey on alcohol and related conditions. Alcohol Res Health. 2004;29:107–20. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- Hasin DS, Trautman KD, Miele GM, et al. Psychiatric Research Interview for Substance and Mental Disorders (PRISM): reliability for substance abusers. Am J Psychiat. 1996;153:1195–201. doi: 10.1176/ajp.153.9.1195. [DOI] [PubMed] [Google Scholar]
- Haver B, Gjestad R. Phobic anxiety and depression as predictor variables for treatment outcome. A LISREL analysis on treated female alcoholics. Nord J Psychiat. 2005;59:25–30. doi: 10.1080/08039480510018797. [DOI] [PubMed] [Google Scholar]
- Kessler RC. Posttraumatic stress disorder: the burden to the individual and to society. J Clin Psychiat. 2000;61:4–14. [PubMed] [Google Scholar]
- Kessler RC, Crum RM, Warner LA, et al. Lifetime co-occurrence of DSM-III-R alcohol abuse and dependence with other psychiatric disorders in the national co-morbidity survey. Arch Gen Psychiat. 1997;54:313–21. doi: 10.1001/archpsyc.1997.01830160031005. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national co-morbidity survey replication. Arch Gen Psychiat. 2005a;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, et al. Prevalence, severity, and co-morbidity of 12-month DSM-IV disorders in the national co-morbidity survey replication. Arch Gen Psychiat. 2005b;62:617–27. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kushner MG, Abrams K, Thuras P, et al. Follow-up study of anxiety disorder and alcohol dependence in co-morbid alcoholism treatment patients. Alcohol Clin Exp Res. 2005;29:1432–43. doi: 10.1097/01.alc.0000175072.17623.f8. [DOI] [PubMed] [Google Scholar]
- Marquenie LA, Schade A, Van Balkom AJLM, et al. Origin of the comorbidity of anxiety disorders and alcohol dependence: Findings of a general population study. Eur Addict Res. 2006;13:39–49. doi: 10.1159/000095814. [DOI] [PubMed] [Google Scholar]
- McCrady BS, Epstein EE. Overcoming Alcohol Problems: A Couples-Focused Program Therapist Guide. New York: Oxford University Press; 2009. [Google Scholar]
- McCrady BS, Epstein EE, Sell RD. Theoretical bases of family approaches to substance abuse treatment. In: Rotgers F, Keller DS, Morgenstens J, editors. Treatment of Substance Abusers: Theory and Technique. 2nd edn. New York: Guilford Press; 2003. pp. 112–39. [Google Scholar]
- McCrady BS, Epstein EE, Cook S, et al. A randomized trial of individual and couple behavioral alcohol treatment for women. J Consult Clin Psych. 2009;77:243–56. doi: 10.1037/a0014686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneier FR, Foosel TE, Hasin DS, et al. Social anxiety disorder and alcohol use disorder co-morbidity in the National Epidemiologic Survey on Alcohol and Related Conditions. Psychol Med. 2010;40:977–88. doi: 10.1017/S0033291709991231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Timeline Followback: a Calendar Method for Assessing Alcohol and Drug Use (Users Guide) Toronto: Addiction Research Foundation; 1996. [Google Scholar]
- Smith WB, Weisner C. Women and alcohol problems: a critical analysis of the literature and unanswered questions. Alcohol Clin Exp Res. 2000;24:1320–1. [PubMed] [Google Scholar]
- Smith JP, Book SW. Co-morbidity of generalized anxiety disorder and alcohol use disorders among individuals seeking outpatient substance abuse treatment. Addict Behav. 2010;35:42–5. doi: 10.1016/j.addbeh.2009.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart SH, Zvolensky MJ, Eifert GH. Negative-reinforcement drinking motives mediate the relation between anxiety sensitivity and increased drinking behavior. Pers Indiv Differ. 2001;31:157–71. [Google Scholar]
- Zvolensky M, Yartz A, Gregor K, et al. Interoceptive exposure-based cessation intervention for smokers high in anxiety sensitivity: a case series. J Cogn Psych. 2008;22:346–65. [Google Scholar]