Abstract
Background
Studies in the 1990s have found that periconceptional dietary folate, supplementation of folic acid or supplemental multivitamins containing folic acid, help prevent neural tube defect (NTDs) if taken at the right time. This literature review assesses the extant folic acid public health campaigns literature and identifies some common variables used in folic acid consumption campaign evaluations.
Methods
This review was part of a larger study that searched PUBMED, PsycINFO and Embase from 1976 to 2010 to identify articles related to the psychosocial and economic impact of NTDs (especially spina bifida) on patients and caregivers.
Results
Awareness of folic acid levels prior to conception improved post-campaign from 6 to 41%. Knowledge about consumption and correct periconceptional use of folic acid also improved. However, in most studies more than 50% of women did not take folic acid as prescribed. Many factors were associated with or without taking folic acid post-campaign, including incomplete outreach, prior awareness and knowledge, closeness to pregnancy, demographics and other personal characteristics.
Conclusions
Sustained campaigning to maintain awareness about and promote periconceptional consumption of folic acid in order to reduce the incidence of NTDs is clearly needed. Additional initiatives could complement existing public health strategies.
Keywords: awareness, campaigns, consumption, folic acid, knowledge
Introduction
After cardiac abnormalities, neural tube defects (NTDs) are the second most common group of serious birth defects. They are burdensome to patients, caregivers, healthcare systems and society.1,2 NTDs are the result of abnormalities in neurulation (closure of the neural folds and neuropores to form the neural tube), a process that is normally completed by 28 days post-conception and usually before a woman knows she is pregnant.3–5 Although NTDs have multiple aetiologies, several studies in the 1990s demonstrated that periconceptional dietary folate, supplementation of folic acid and/or supplemental multivitamins containing folic acid help prevent NTDs.6
Folate is a water-soluble B vitamin that is found naturally in foods such as fruits, dark green vegetables, potatoes, beans and yeast extract. Folic acid is the synthetic form of folate found in dietary supplements and added to enriched flour and grain products such as breads, pasta, rice and cereals.7–9 Compelling evidence about the efficacy of folic acid against NTDs emerged from two randomized controlled trials.10,11 The UK Medical Research Council trial found that 4 mg/day of periconceptional folic acid supplementation in high-risk women (recurrent NTDs) was associated with a 72% reduction in NTD pregnancies. Later, a Hungarian trial showed that 0.8 mg/day of folic acid in a periconceptional multivitamin supplement protected against first occurrences of NTDs (low-risk women). When taken before conception, adequate use of folic acid reduces the incidence of NTDs by 50–70% to a rate of approximately 6 per 10 000 pregnancies.12 However, many women are not aware that folic acid must be taken before conception; in addition, 40–50% of pregnancies are unplanned.13–15 Consequently, national health bodies and clinical practice guidelines (including those in the UK, US, Canada and Australia) recommend an increase of periconceptional folate intake for all women of child-bearing age and specify a folic acid supplement of 4–5 mg per day for women at high risk or 0.4–0.5 mg per day for women at low risk.5,16–20 A US Food and Drug Association (FDA) Advisory Committee for Reproductive Health Drugs recommended that pregnant women (pre-pregnancy and early pregnancy) should increase their intake of folic acid by 400 µg a day.21 Since the 1990s, strategies targeting women of child-bearing age were implemented at local and national levels to help translate national recommendations into action.
One strategy is folate fortification in staple foods such as wheat flour, breads and cereals. Fortification implementation varies widely from country to country. In 1996, the US FDA requested that folic acid be added to all ‘enriched’ grain products to help lower the risk of folic acid preventable birth defects; this became mandatory in 1998.22 However, in Europe there is no regulation for food fortification—although some fortified products are available in some countries.19,20,23 The number of countries with documented national regulations for mandatory wheat-flour fortification increased from 33 in 2004 to 54 in 2007. Worldwide observation of trends indicate an increase in wheat-flour fortification with folic acid and iron from 18% in 2004 to 27% in 2007, with the number of individuals with access to fortified wheat flour increasing by 540 million and the annual number of newborns whose mothers had access during pregnancy increasing by 14 million.24
Another strategy is public health campaigns aimed at informing and influencing behavioral change in all individuals, not just those who seek help.25 Official health education initiatives have promoted folic acid supplementation and a diet rich in folates.26 Campaigns range from media communications and information kits, to free product samples and discount vouchers, to improved labeling and in-store displays promoting dietary sources of folic acid.
Better prenatal detection, as well as increased use of prenatal screening programs to terminate affected pregnancies, has helped prevent live births with NTDs. Improved nutritional awareness has contributed to the decline in incidence of NTDs in many parts of the world.20,27,28 However, despite the education and fortification measures taken to date, research indicates that many women do not take adequate amounts of folic acid pre-conception. More NTDs and induced pregnancy terminations could be prevented if more women took folic acid every day.26,29
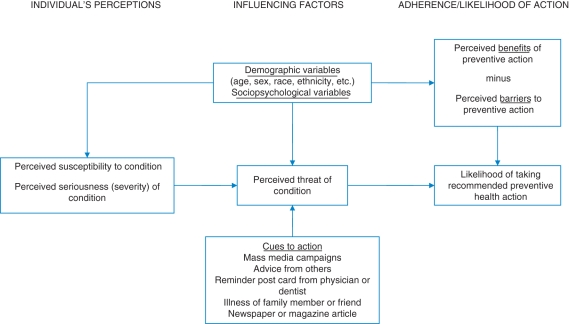
The likelihood of taking recommended preventative health action is dependent on many factors (Fig. 1). The health belief model (HBM) posits that individuals' beliefs about the seriousness of a health condition and how susceptible they are to that condition—as well as cues to action (such as media campaigns and advice from healthcare professionals)—determine the overall perceived threat of a condition.30 HBM states that prior awareness of a condition affects individuals' perceptions of susceptibility to it; individuals who are familiar with a condition may perceive themselves as more susceptible to the condition than those with less knowledge about it.31 Their appraisal of the perceived benefits versus barriers to preventative actions also plays an important role, together with socio-psychological and demographic factors.
Fig. 1.
HBM for predicting and explaining likelihood of taking recommended preventative health action.
The objective of this paper is to assess the extant folic acid public health campaigns literature and identify some common variables used in folic acid consumption campaign evaluations. Study outcomes and barriers to success for folic acid public health campaigns are compared with other health campaign interventions.
Methods
This literature review was part of a larger study investigating the psychosocial and economic impact of NTDs (especially spina bifida) on patients and caregivers. Examination of the impact of campaigns on folic acid awareness and consumption was not a primary objective of the larger study. However, the search strategy identified many articles that focused on folic acid campaigns, even though ‘campaigns’ was not part of the search strategy. Given the wealth of data uncovered by the search, it was decided to explore the factors influencing the success of campaigns targeting women's folic acid awareness and consumption.
PUBMED, PsycINFO and Embase were searched for relevant articles dating from January 1976 to October 2010. The review used a subject and text word-search strategy with the following terms:
NTDs, SB, anencephaly, meningocele AND
Health-related quality of life, HRQoL, quality of life, QoL symptoms, satisfaction, body image, self-image, emotional, physical, psychological, psychosocial, self-esteem, impact, relationships, caregiver burden, family impact, work, productivity, absenteeism, presenteeism, qualitative, interviews, grounded theory, interpretive phenomenological analysis OR
Cost, cost of illness, cost of disease, economic burden, economic impact, resource use, hospitalization, unmet need OR
Economic evaluation, cost analysis, cost-effectiveness, CEA, cost minimization, CMA, cost consequence, CCA, cost utility, CUA, cost benefit, CBA, cost savings, patient preferences OR
Folic acid, folate, vitamin supplements, food fortifi*, enriched grain OR
Family planning, unplanned pregnancy, pre-natal care, abortion, termination.
Additional internet and manual searches were performed to identify other relevant published material as well as unpublished material not normally found in electronic databases. The review was restricted to English language studies.
To satisfy the initial inclusion criteria, articles had to contain studies that were specific to an appropriate clinical term and a reference to folic acid education and consumption programs. Due to the high number of seemingly relevant articles, conferences, dissertations, books or chapters were excluded and articles were ranked for further review according to three criteria:
Rank 1—Journal article with a patient-reported outcome, cost or folic acid term as the main focus of the article and consequently reported in the title and abstract.
Rank 2—Journal article with patient-reported outcome, cost or folic acid term found in the title and abstract but not main focus of the article. These studies often reported relevant results as secondary outcomes in the abstract.
Rank 3—Journal article with relevant terms in the background or implied in the abstract.
Articles ranked 1 were included in the review; all other articles were excluded. Data extraction tables were developed to accurately summarize relevant features and results of the selected studies. The key components of the data extraction tables were general information about the authors, publication date, country of study and reference. The aims of the studies, strategy/campaign/program, target sample, study design, participants and results were also documented.
Results
Study selection
Of the 166 articles initially identified (4456 abstracts screened and 4288 excluded), 38 articles were relevant to health campaigns. Ten articles focused on pre- and post-campaign awareness, knowledge or consumption data for women of child-bearing age.32–41 The remaining 28 articles focused on data at one time point, trend analysis and/or factors associated with awareness, knowledge or consumption of folic acid.6,12,42–67 Data were collected at time points ranging from 2 days39 to 4 years following pre-assessment.33,40
Public health campaigns: awareness, knowledge and consumption of folic acid
All 38 articles assessed awareness, knowledge and/or consumption of folic acid; our results are summarized below accordingly.
Awareness
The majority of articles defined awareness as whether women had heard of folic acid.32,34,35,37,38,57,58Results showed that awareness of folic acid improved post-campaign, with the percentage improvement between pre- and post-campaigns ranging from 6 34 to 41%.57
Women most often learned about folic acid from public media (particularly TV 66) or learning about a celebrity/famous person who had a child with a disability.58 This was followed by learning from pro-active healthcare professionals, and then friends and relatives, especially those with a child with an NTD.34,42,59,68
Knowledge
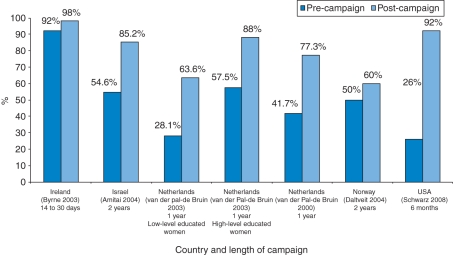
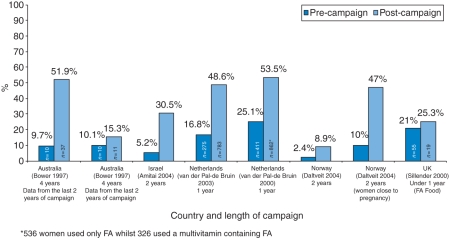
Several studies explored women's knowledge about folic acid, including understanding its role in preventing birth defects (Fig. 2 and Fig. 3)32,34,35,39,40,56,57, food sources and supplementation,34,35,37,40 and timing of consumption.34,35,37,42
Fig. 2.
Folic acid awareness before and after campaign by country.
Fig. 3.
Folic acid consumption before and after campaign by country (around time of conception).
Although knowledge regarding appropriate sources of folic acid (foods or supplements) improved post-campaign, in most studies <50% of women were able to provide details about supplements that contained folic acid.34,35,40 However, one US study found a high proportion of women were knowledgeable about food and supplements. Specifically, among women who reported in the post-campaign survey that they had heard about folic acid, knowledge about the ways to increase consumption increased from 55% in 1997 to 73% in 1999 but correct knowledge about the best time to take folic acid (before or during pregnancy) did not increase.42 A recent Danish study reported that pregnant women who actually use folic acid supplements significantly outnumber those who simply ‘declare their knowledge of folic acid supplementation’.59
Nevertheless, educational campaigns can be effective. One US study found that when women aged 18–45 participated in a 15-min computerized educational session, the percentage of women who understood that folate can prevent birth defects rose from 26% pre-campaign to 92% post-campaign.67 In general, women's knowledge about folic acid's role in preventing birth defects and about food and supplemental sources of folic acid improved after campaigns but women were less likely to understand the importance of taking folic acid before conception.
Consumption
In general, folic acid consumption rose between 12.4 36 and 25.3% after public health campaigns.32 Nevertheless, the percentage of women taking periconceptional folic acid as prescribed ranged from 13 to 57%. This suggests >43% of women were not taking folic acid as prescribed after campaigns ceased.32,33,36,38–41,57
Acknowledged barriers to the success of campaigns
Since results of public health campaigns are mixed in terms of raising appropriate consumption of folic acid, it is essential to identify factors contributing to the success—or failure—of these programs. The following factors were identified.
Incomplete outreach
Campaigns increased awareness and knowledge of folic acid consumption; however it must be recognized that a considerable proportion of the intended population may not have understood or even witnessed the campaign or its key messages for a variety of reasons. For example, women who do not have a television or who do not read magazines may not have been reached by those campaigns’.58,63
Prior awareness and knowledge
Prior knowledge and awareness of folic acid has been linked to whether patients use it.36,40 One study found that participants who had heard of folic acid before (awareness) were more likely to believe in its benefits than those who had not.56 Patient knowledge was also linked to beliefs, which ultimately influenced consumption. For example, in studies exploring women's awareness and consumption of folic acid for the prevention of NTDs, women who saw ‘perceived benefits’ of taking folic acid made statements like the following:56
‘Even if she is not planning a pregnancy every woman capable of becoming pregnant should take folic acid supplements.'
‘It is easy to consume the recommended amount of folic acid through vitamin supplements.’
‘When one is pregnant, one has to take it [folic acid] when the baby's brain is forming. That's an important vitamin.’ 40
‘Perceived barriers’ to taking folic acid included women who did not perceive risk due to medical history or diet and made these following types of statements:56
‘If someone does not have a family history of neural tube defects, she is not at risk of having a baby with a neural tube defect.’
‘I don't need to take folic acid supplements because I get enough in my diet.’
Closeness to pregnancy
Closeness to pregnancy (defined as planning a pregnancy, currently pregnant or giving birth within the last 12 months) was a factor in the use of folic acid supplements post-campaign.35,38 However, in one study only a small proportion (4.7%) of women planning pregnancy took folic acid every day as opposed to no vitamin supplementation.35
Two studies found that women with an unplanned pregnancy were less likely to have used folic acid compared with other women in the study populations.36,46
Demographic and other personal characteristics
Women who took folic acid were usually older,51,52 Caucasian,39 married,38 educated,32,34,35,51,69 non-smokers34,39,51 and of high socio-economic status.51 Research in Puerto Rico using a questionnaire to assess folic acid use found that highly educated women were 8.3 times more likely to consume folic acid.66 In addition to socioeconomic factors, an Israeli study focusing on use of preconceptional folic acid reported that religion was a contributing factor. In particular, the Jewish population exhibited significantly higher rates of folic acid utilization compared with the Arab group (Muslim Arab, Christian Arab and Druze).32 Parous state (having given birth to one or more child) also increased a woman's likelihood of taking folic acid.34,51
Discussion
Main findings of this study
This review found that awareness, knowledge and consumption of folic acid improved following public health campaigns; however, these results were mixed. Knowledge about the benefits and sources of folic acid increased post-campaign, but most women misunderstood the appropriate time to self-administer folic acid. With the exception of one US study, <50% of women could correctly cite the types of food containing folic acid, and generally <50% of women of child-bearing age were actually taking folic acid.33,36,38,57 To summarize, these campaigns usually changed the knowledge and behavior of less than half the target population.
The review also identified factors that impact consumption of folic acid, including incomplete outreach, prior awareness and knowledge, closeness to pregnancy, demographics and other personal characteristics. This information can help identify target groups not currently reached by campaigns and can be used to design health promotion strategies accordingly.
What is already known about this topic?
Despite folic acid's clear link with NTD prevention, folic acid education campaigns worldwide have had mixed results in terms of knowledge about the benefits and sources of folic acid, and especially in terms of understanding the correct, periconceptional timing of folic acid intake. These mixed results for folic acid campaigns are consistent with the broader context of health campaign research. For example, a systematic UK review in 2010 found little evidence that UK public health campaigns affected health and social outcomes, and acknowledged the difficulties of changing clinical behavior.70,71 Current research on the topic suggests that campaigns and health interventions need to focus upon and understand the ‘drivers’ of health-seeking behavior, i.e. the prevailing socio-political, cultural and economic contexts.72,73
What this study adds
This review synthesizes the published quantitative and qualitative literature regarding public health campaigns and the uptake of folic acid. New qualitative insights emerged from an analytical review and interpretation of data. The researchers categorized information and data meaningful groups and found the following.
Prospects for targeted educational initiatives
This review identified factors that affect the success of folic acid education campaigns, including incomplete outreach, prior awareness and knowledge, closeness to pregnancy, demographics and other personal characteristics. This information can help identify target groups not currently reached by campaigns and can be used to design health promotion strategies accordingly.
For example, one study proposes culturally relevant and specific campaigning (e.g. billboards depicting different ethnicities and age groups) and ‘shock tactic’ campaigns (e.g. depicting children with NTDs and life with an NTD) targeted to populations not yet reached by previous campaigns.21
Other initiatives might target women based on age. For example, several studies found older women planning a pregnancy are more receptive to recommendations, but should be educated about taking folic acid as prescribed. Young women (16–24 years) who are not considering pregnancy were found to be less interested in folic acid recommendations to improve pregnancy outcomes.13–15 Health promotion strategies for this cohort could focus on adopting folic acid supplementation as a ‘healthy lifestyle’ habit rather than as a ‘periconceptional' supplement.
Prospects for targeted supplementation
Because this review confirmed that folic acid campaigns—like most health education campaigns—have mixed results, additional supplementation initiatives should be considered. For example, in 2003, an FDA Advisory Committee discussed the public health issues and clinical benefit of combining folic acid and an oral contraceptive to complement public health efforts to reduce NTDs. In October 2010, the first and only oral contraceptive approved by the FDA to raise folate levels in women (Beyaz) was launched in the USA. This could be extremely beneficial to those who begin trying to conceive immediately after stopping oral contraceptive use. Many women do not inform their healthcare provider when they stop taking oral contraceptives. Consequently, they may not be informed about the importance of folic acid supplementation until their first pre-natal visit, which often occurs after the neural tube should have closed.
If implemented, targeted folic acid supplementation strategies like these, in addition to food/supplementary fortification, could contribute towards achieving the 2010 US Department of Health and Human Services ‘healthy people objectives’ for NTDS; namely, to: (i) reduce the number of NTDs and (ii) ensure that women have appropriate folate levels prior to conception.74
Exploration of the HBM
Results from this review provide some evidence to support the HBM. As suggested by the HBM, women assess the seriousness and severity of having a baby with an NTD, as well as their susceptibility to the condition. Exposure to public health campaigns was found to contribute in part towards women's awareness and their overall perceived threat of the condition. In addition, the perceived benefits minus the various barriers to preventive action (including prior awareness and knowledge, incomplete outreach, closeness to pregnancy and demographic characteristics) also help explain the likelihood that women will take the correct amount of folic acid preconception.
However, it should be noted that the HBM has been criticized for not adequately considering the role of social and economic environments in explaining health behaviors.75 Other social cognition models, such as the theory of planned behavior (TPB) may enhance understanding of the efficacy of folic acid public health campaigns.76–78 For example, the TPB suggests that attitudes, subjective norms and perceived behavioral control predict behavioral intentions, which in turn are associated with health behaviors. Further, health communication research may address other reasons why awareness, knowledge and consumption of folic acid did not increase uniformly among the targeted audiences in the 38 studies considered.79
Limitations of this study
This review was part of a larger study that explored the psychosocial and economic impact of NTDs (especially spina bifida) on patients and caregivers. It was not specifically designed to capture all studies on folic acid campaigns or educational programs. Consequently, there might be other studies not captured in this review.
Because of the study design, the current findings provide an overview of folic acid campaigns worldwide, rather than by country. Closer examination of country-specific issues may reveal important differences to consider in future research. For example, exposure to campaigns can vary according to country-specific beliefs about the benefits and side effects of folic acid. In the US, food fortification is mandatory and all women of child-bearing age are recommended to take folic acid supplements. However, in the Netherlands, women of child-bearing age who are not planning to conceive are not advised to increase their folate intake (taking supplements only when planning to conceive) and folic acid fortification was outlawed. Given the limited success of campaigns to increase the uptake of folic acid, increased understanding of cross-cultural beliefs regarding food fortification is warranted. Better understanding of these beliefs could enhance future food (or other) fortification communication strategies internationally.
‘The long-term effects of public health campaigns have not been studied in the research reported here. Campaign lengths spanned from 2 days 39 to 4 years.34 Though we did not see a difference by campaign length, one could presume that longer campaigns would yield better outcomes. However, as campaigns close new generations of women may miss the messages of these campaigns.’
Furthermore, education campaigns usually occur over discrete periods of time.33,40 Thus, campaigns that were widely disseminated in the early to mid-1990s are unlikely to have reached a sub-section of the current target audience of 15–30 year olds in 2008. Clearly, sustained education programs are needed to maintain awareness, knowledge and consumption of folic acid pre-conception.
Finally, while our findings identified a number of factors contributing to consumption of folic acid, it is important to acknowledge that because our study was not designed to be an exhaustive literature search, there may be other factors not identified in this review.
Future research
While this study supports the HBM and deems it appropriate to undergird future public health campaigns promoting folic acid consumption, the HBM alone cannot necessarily explain or justify why behavior leads to action in health behavior. Future research could address models that help predict and explain health behavior change such as the transtheoretical model (TTM).80 The TTM could provide information on how folic acid consumption behavior might change or be maintained.
Conclusion
Many factors contribute to the success of folic acid public health campaigns, including identifying target groups not currently reached by existing campaigns culturally and adapting campaigns to make them relevant to those target groups, would likely increase the effectiveness of campaigns. Inclusion of folic acid benefits within high school and university educational programs would also ensure the message reaches women early in their sexual lives. Furthermore, folic acid fortification in food stuffs and medical products would complement existing public health initiatives. While variables that prove to be barriers to campaigns such as incomplete outreach inevitably need to be overcome, further campaigns are needed to promote and maintain awareness of the correct time to take folic acid to reduce the overall incidence of NTDs.
Funding
This review was supported by Bayer Healthcare. Funding to pay the Open Access publication charges for this article was also provided by Bayer Healthcare.
Acknowledgments
We acknowledge Rebecca Heelis for her initial research support and contribution.
References
- 1.Botto L, Lisi A, Bower C, et al. Trends of selected malformations in relation to folic acid recommendations and fortification: an international assessment. Birth Defects Res A Clin Mol Teratol. 2006;76:693–705. doi: 10.1002/bdra.20307. [DOI] [PubMed] [Google Scholar]
- 2.Tilford J, Grosse S, Robbins J, et al. Health state preference scores of children with spina bifida and their caregivers. Qual Life Res. 2005;14:1087–98. doi: 10.1007/s11136-004-3305-2. [DOI] [PubMed] [Google Scholar]
- 3.Botto LD, Moore CA, Khoury MJ, et al. Neural-tube defects. N Engl J Med. 1999;341:1509–19. doi: 10.1056/NEJM199911113412006. [DOI] [PubMed] [Google Scholar]
- 4.Hobbins JC. Diagnosis and management of neural-tube defects today. N Engl J Med. 1991;324:690–91. doi: 10.1056/NEJM199103073241009. [DOI] [PubMed] [Google Scholar]
- 5.National Health and Medical Research Council. Revised statement on the relationship between dietary folic acid and neural tube defects such as spina bifida. 15th Session of the National Health and Medical Research Council; Australia: 1993. [PubMed] [Google Scholar]
- 6.Bower C, Blum L, Watson C, et al. Folate and the prevention of neural tube defects: evaluation of a health promotion project in Western Australia. Health Promot Int. 1996;11:177–87. [Google Scholar]
- 7.Food and Nutrition Board IoM. Washington, DC: National Academy Press; 1998. Dietary reference intakes for thiamin, riboflavin, niacin, vitamin B6, folate, vitamin B12, pantothenic acid, biotin and choline. (National Academy Press Webpage) http://books.nap.edu/books/0309065542/html/indes.html . [PubMed] [Google Scholar]
- 8.Barrowclough D, Ford F. Folic acid fortification. Proposed UK recommendations. Pract Midwife. 2000;3:32–33. [PubMed] [Google Scholar]
- 9.McDowell MA, Lacher DA, Pfeiffer CM, et al. Blood folate levels: the latest NHANES results. NCHS Data Brief. 2008;6:1–8. [PubMed] [Google Scholar]
- 10.Medical Research Council. Prevention of neural tube defects: results of the Medical Research Council Vitamin Study MRC Vitamin Study Research Group. Lancet. 1991;338:131–37. [PubMed] [Google Scholar]
- 11.Czeizel AE, Dudas I. Prevention of the first occurrence of neural-tube defects by periconceptional vitamin supplementation. N Engl J Med. 1992;327:1832–35. doi: 10.1056/NEJM199212243272602. [DOI] [PubMed] [Google Scholar]
- 12.Berry RJ, Li Z, Erickson JD, et al. Prevention of neural-tube defects with folic acid in China-US Collaborative Project for Neural Tube Defect Prevention. N Engl J Med. 1999;341:1485–90. doi: 10.1056/NEJM199911113412001. [DOI] [PubMed] [Google Scholar]
- 13.McGovern E, Moss H, Grewal G, et al. Factors affecting the use of folic acid supplements in pregnant women in Glasgow. Br J Gen Pract. 1997;47:635–37. [PMC free article] [PubMed] [Google Scholar]
- 14.Eicholzer M, Tonz O, Zimmermann R. Folic acid: a public-health challenge. Lancet. 2006;367:1352–61. doi: 10.1016/S0140-6736(06)68582-6. [DOI] [PubMed] [Google Scholar]
- 15.Jones EF, Forrest JD. Under-reporting of abortion in surveys of U.S women: 1976 to 1988. Demography. 1992;29:113–26. [PubMed] [Google Scholar]
- 16.McCourt C. Primary prevention of neural tube defects: notice from the HPB (Health Protection Branch) Can Med Assoc J. 1993;148:1451. [PMC free article] [PubMed] [Google Scholar]
- 17.CDC. Recommendations for the use of folic acid to reduce the number of cases of spina bifida and other neural tube defects. MMWR Morb Mort Wkly Rep. 1992;41:1. [PubMed] [Google Scholar]
- 18.Neural Tube Defects. ACOG Practice Bulletin Number 44, July 2003. Obstet Gynecol. 2003;102:203–13. [PubMed] [Google Scholar]
- 19.Czernichow S, Noisette N, Blacher J, et al. Case for folic acid and vitamin B(12) fortification in Europe. Sem Vasc Med. 2005;5:156–62. doi: 10.1055/s-2005-872400. [DOI] [PubMed] [Google Scholar]
- 20.Food Safety Authority of Ireland. Food Safety Authority of Ireland; 2006. Report of the National Committee of Folic Acid Food Fortification. [Google Scholar]
- 21.Advisory Committee Briefing Book. FDA Advisory Committee; 2003. Meeting of the Reproductive and Urologic Drug Products. [Google Scholar]
- 22.US Department of Health and Human Services Food and Drug Administration. Food standards: amendment of the standards of identity for enriched grain products to require addition of folic acid. Fed Reg. 1996;61:8781–809. [Google Scholar]
- 23.Aguilar F, Charrondiere UR, Dusemund B, et al. Inability to assess the safety of folic acid-enriched yeast added for nutritional purposes as a source of folic acid to food supplements and the bioavailability of folic acid from this source, based on the supporting dossier. EFSA Journal. 2009;June:1090. [Google Scholar]
- 24.Maberly G, Grummer-Strawn L, Jefferds ME, et al. Trends in wheat-flour fortification with folic acid and iron - worldwide, 2004 and 2007. MMWR Morb Mort Wkly Rep. 2008;57:8–10. [PubMed] [Google Scholar]
- 25.Ogden J. Health Psychology: A Textbook. 3rd edn. Berkshire, England: Open University Press; 2007. [Google Scholar]
- 26.March of Dimes launches new Ad campaign to alert women about folic acid and birth defects. March Dimes. 2000.
- 27.Roberts HE, Moore CA, Cragan JD, et al. Impact of prenatal diagnosis on the birth prevalence of neural tube defects, Atlanta, 1990–1991. Pediatrics. 1995;96:880–83. [PubMed] [Google Scholar]
- 28.EUROCAT. Central Registry. Prevention of neural tube defects by periconceptional folic acid supplementation in Europe. 2003.
- 29.More women know about folic acid but still don't take it, latest survey finds. March Dimes. 2002.
- 30.Rosenstock IM, Strecher VJ, Becker MH. Social learning theory and the Health Belief Model. Health Educ Questionnaire. 1988;15:175–83. doi: 10.1177/109019818801500203. [DOI] [PubMed] [Google Scholar]
- 31.Smedslund G. A pragmatic basis for judging models and theories in health psychology: the axiomatic method. J Health Psychol. 2000;5:133–49. doi: 10.1177/135910530000500202. [DOI] [PubMed] [Google Scholar]
- 32.Amitai Y, Fisher N, Haringman M, et al. Increased awareness, knowledge and utilization of preconceptional folic acid in Israel following a national campaign. Prev Med. 2004;39:731–37. doi: 10.1016/j.ypmed.2004.02.042. [DOI] [PubMed] [Google Scholar]
- 33.Bower C, Knowles S, Nicol D. Changes in folate supplementation, and in serum and red cell folate levels in antenatal patients over the course of a health promotion project for the prevention of neural tube defects. Aust N Z J Obstet Gynaecol. 1997;37:267–71. doi: 10.1111/j.1479-828x.1997.tb02406.x. [DOI] [PubMed] [Google Scholar]
- 34.Byrne J. Folic acid knowledge and use among relatives in Irish families with neural tube defects: an intervention study. Ir J Med Sci. 2003;172:118–22. doi: 10.1007/BF02914495. [DOI] [PubMed] [Google Scholar]
- 35.Daltveit A, Vollset S, Lande B, et al. Changes in knowledge and attitudes of folate, and use of dietary supplements among women of reproductive age in Norway 1998–2000. Scand J Public Health. 2004;32:264–71. doi: 10.1080/14034940310019515. [DOI] [PubMed] [Google Scholar]
- 36.Sillender M, Pring DW. How effective was the Health Education Authority's folic acid campaign? J Obstet Gynaecol. 2000;20:271–76. doi: 10.1080/01443610050009593. [DOI] [PubMed] [Google Scholar]
- 37.van der Pal-de Bruin K, De Walle HEK, de Rover CM, et al. Influence of educational level on determinants of folic acid use. Paediatr Perinat Epidemiol. 2003;17:256–63. doi: 10.1046/j.1365-3016.2003.00497.x. [DOI] [PubMed] [Google Scholar]
- 38.van der Pal-de Bruin K, De Walle HEK, Jeeninga W, et al. The Dutch ‘Folic Acid Campaign’—have the goals been achieved? Paediatr Perinat Epidemiol. 2000;14:111–17. doi: 10.1046/j.1365-3016.2000.00251.x. [DOI] [PubMed] [Google Scholar]
- 39.Watkins M, Brustrom J, Schulman J. Effectiveness of a free folic acid supplement program in family planning clinics. Birth Defects Res A Clin Mol Teratol. 2004;70:403–07. doi: 10.1002/bdra.20035. [DOI] [PubMed] [Google Scholar]
- 40.Watson M, Watson L, Bell R, et al. The increasing knowledge of the role of periconceptional folate in Victorian women of child-bearing age: follow-up of a randomised community intervention trial. Aust N Z J Public Health. 2001;25:389–95. [PubMed] [Google Scholar]
- 41.Watson MJ, Watson LF, Bell RJ, et al. A randomized community intervention trial to increase awareness and knowledge of the role of periconceptional folate in women of child-bearing age. Health Expect. 1999;2:255–65. doi: 10.1046/j.1369-6513.1999.00064.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Centre for Disease Control. Folic acid campaign and evaluation—southwestern Virginia, 1997–1999. MMWR Morb Mort Wkly Rep. 1999;48:914–17. [PubMed] [Google Scholar]
- 43.Botto L, Lisi A, Robert G, et al. International retrospective cohort study of neural tube defects in relation to folic acid recommendations: are the recommendations working? Br Med J (Clinical Research ed.) 2005;330:571. doi: 10.1136/bmj.38336.664352.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Centres for Disease Control. Prevention program for reducing risk for neural tube defects—South Carolina, 1992–1994. MMWR Morb Mort Wkly Rep. 1995;44:141–42. [PubMed] [Google Scholar]
- 45.Cornel MC, de S, de JvdB. Folic acid—the scientific debate as a base for public health policy. Reprod Toxicol. 2005;20:411–15. doi: 10.1016/j.reprotox.2005.03.015. [DOI] [PubMed] [Google Scholar]
- 46.de la Vega A, Salicrup E, Verdiales M. A nationwide program for the use of preconceptional folic acid to prevent the development of open neural tube defects: Who is really using folic acid? Puerto Rico Health Sci J. 2002;21:7–9. [PubMed] [Google Scholar]
- 47.Egen V, Hasford J. Prevention of neural tube defects: effect of an intervention aimed at implementing the official recommendations. Soz Praventivmed. 2003;48:24–32. doi: 10.1007/s000380300003. [DOI] [PubMed] [Google Scholar]
- 48.Hauser K, Lilly C, Frias J. Florida health care providers' knowledge of folic acid for the prevention of neural tube defects. South Med J. 2004;97:437–39. doi: 10.1097/00007611-200405000-00004. [DOI] [PubMed] [Google Scholar]
- 49.Hertrampf E, Cortes F. Folic acid fortification of wheat flour: Chile. Nutr Rev. 2004;62:S44–48. doi: 10.1111/j.1753-4887.2004.tb00074.x. [DOI] [PubMed] [Google Scholar]
- 50.Kannan S, Menotti E, Scherer H, et al. Folic acid and the prevention of neural tube defects: a survey of awareness among Latina women of childbearing age residing in southeast Michigan. Health Promot Pract. 2007;8:60–8. doi: 10.1177/1524839905278934. [DOI] [PubMed] [Google Scholar]
- 51.Knudsen V, Orozova BI, Rasmussen L, et al. Low compliance with recommendations on folic acid use in relation to pregnancy: is there a need for fortification? Public Health Nutr. 2004;7:843–50. doi: 10.1079/phn2004630. [DOI] [PubMed] [Google Scholar]
- 52.Langley E, Langley E. Use of folic acid supplements in the first trimester of pregnancy. J R Soc Health. 2002;122:181–86. doi: 10.1177/146642400212200315. [DOI] [PubMed] [Google Scholar]
- 53.Neill AM, Laing RJ, Perez P, et al. The ‘Folic Acid Campaign’: has the message got through? A questionnaire study. J Obstet Gynaecol. 1999;19:22–5. doi: 10.1080/01443619965895. [DOI] [PubMed] [Google Scholar]
- 54.Oakley G, Bell K, Weber M. Recommendations for accelerating global action to prevent folic acid-preventable birth defects and other folate-deficiency diseases: meeting of experts on preventing folic acid-preventable neural tube defects. Birth Defects Res A Clin Mol Teratol. 2004;70:835–37. doi: 10.1002/bdra.20058. [DOI] [PubMed] [Google Scholar]
- 55.Pereleman V, Singal N, Einarson A, et al. Knowledge and practice by Canadian family physicians regarding periconceptional folic acid supplementation for the prevention of neural tube defects. Can J Clin Pharmacol. 1996;3:145–48. [Google Scholar]
- 56.Quillin JM, Silberg J, Board P, et al. College women's awareness and consumption of folic acid for the prevention of neural tube defects. Genet Med. 2000;2:209–13. doi: 10.1097/00125817-200007000-00002. [DOI] [PubMed] [Google Scholar]
- 57.Ward M, Hutton J, Mc D, et al. Folic acid supplements to prevent neural tube defects: trends in East of Ireland 1996–2002. Ir Med J. 2004;97:274–76. [PubMed] [Google Scholar]
- 58.Prue CE, Flores AL, Panissidi P, et al. But I've already had a healthy baby: folic acid formative research with Latina mothers. J Women Health. 2008;17:1257–69. doi: 10.1089/jwh.2008.0980. [DOI] [PubMed] [Google Scholar]
- 59.Rasmussen MM, Clemmensen D. Folic acid supplementation in pregnant women. Dan Med Bull. 2010;57:A4134. [PubMed] [Google Scholar]
- 60.Bell KN, Oakley J. Update on prevention of folic acid-preventable spina bifida and anencephaly. Birth Defects Res A Clin Mol Teratol. 2009;85:102–07. doi: 10.1002/bdra.20504. [DOI] [PubMed] [Google Scholar]
- 61.Flynn MAT, Anderson WA, Burke SJ, et al. Session 1: Public health nutrition folic acid food fortification: the Irish experience. Proc Nutr Soc. 2008;67:381–89. doi: 10.1017/S0029665108008720. [DOI] [PubMed] [Google Scholar]
- 62.Lindsey LLM, Silk KJ, Friederichs-Fitzwater MM, et al. Developing effective campaign messages to prevent neural tube defects: a qualitative assessment of women's reactions to advertising concepts. J Health Commun. 2009;2:131–59. doi: 10.1080/10810730802659137. [DOI] [PubMed] [Google Scholar]
- 63.Tedstone A, Browne M, Harrop L, et al. Fortification of selected foodstuffs with folic acid in the UK: consumer research carried out to inform policy recommendations. J Public Health. 2008;30:23–29. doi: 10.1093/pubmed/fdm073. [DOI] [PubMed] [Google Scholar]
- 64.Nichols JAA, Curtis EPP, Rayman MP. Survey of total folate intake at conception and assessment of impact of fortification. J Nutr Environ Med. 2008;17:44–55. [Google Scholar]
- 65.Sharp GF, Naylor LA, Cai J, et al. Assessing awareness, knowledge and use of folic acid in Kansas women between the ages of 18 and 44 years. Matern Child Health J. 2009;13:814–21. doi: 10.1007/s10995-008-0414-5. [DOI] [PubMed] [Google Scholar]
- 66.Garcia-Fragoso L, Garcia-Garcia I, Rivera CE. The use of folic acid for the prevention of birth defects in Puerto Rico. Ethn Dis. 2008;18:S2–71. [PMC free article] [PubMed] [Google Scholar]
- 67.Schwarz EB, Sobota M, Gonzales R, et al. Computerized counseling for folate knowledge and use. A randomized controlled trial. Am J Prev Med. 2008;35:568–71. doi: 10.1016/j.amepre.2008.06.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Zipitis C, Paschalides C. Caring for a child with spina bifida: understanding the child and carer. J Child Health Care. 2003;7:101–12. doi: 10.1177/1367493503007002004. [DOI] [PubMed] [Google Scholar]
- 69.van dPdBK, van d, Buitendijk S, den O. Periconceptional folic acid use and the prevalence of neural tube defects in The Netherlands. Eur J Obstet Gynecology Reprod Biol. 2003;108:33–39. doi: 10.1016/s0301-2115(02)00362-7. [DOI] [PubMed] [Google Scholar]
- 70.Evans D, Pilkington P, McEachran M. Rhetoric or reality? A systematic review of the impact of participatory approaches by UK public health units on health and social outcomes. J Public Health. 2010;32:418–26. doi: 10.1093/pubmed/fdq014. [DOI] [PubMed] [Google Scholar]
- 71.McColl A, Gabbay J, Roderick P. Improving health outcomes—a review of case studies from English health authorities. J Public Health Med. 1998;20:302–11. doi: 10.1093/oxfordjournals.pubmed.a024773. [DOI] [PubMed] [Google Scholar]
- 72.Shaikh BT, Hatcher J. Health seeking behaviour and health service utilization in Pakistan: challenging the policy makers. J Public Health. 2005;27:49–54. doi: 10.1093/pubmed/fdh207. [DOI] [PubMed] [Google Scholar]
- 73.Knai C, McKee M. Tackling childhood obesity: the importance of understanding the context. J Public Health. 2010;32:506–11. doi: 10.1093/pubmed/fdq019. [DOI] [PubMed] [Google Scholar]
- 74.Yu SM. Health People 2010. Matern Child Health J. 1998;2:63–66. doi: 10.1023/a:1021801927353. [DOI] [PubMed] [Google Scholar]
- 75.Ogden J. Health Psychology. A Textbook. 2nd edn. Berkshire, UK: Open University Press; 2000. [Google Scholar]
- 76.Ajzen I. From intentions to actions: a theory of planned behaviour. In: Kuhl J, Beckman J, editors. Action Control: From Cognition to Behavior. Heidelberg: Springer; 1985. pp. 11–39. [Google Scholar]
- 77.Ajzen I, Madden TJ. Prediction of goal-directed behavior: attitudes, intentions and perceived behavioral control. J Exp Soc Psychol. 1986;22:453–74. [Google Scholar]
- 78.Ajzen I. Attitudes, Personality and Behavoir. Chicago: Dorsey Press; 1988. [Google Scholar]
- 79.Willliams D. Communication Skills in Practice: A Practical Guide for Health Professionals. London: Jessica Kingsley; 1999. [Google Scholar]
- 80.Prochaska JO, DiClemente CC. The Transtheoretical Approach: Crossing Traditional Boundaries of Therapy. Malabar, FL: Krieger; 1984. [Google Scholar]