Patients with low back pain or radiculopathy were significantly less likely to receive a prescription for narcotics if the patient's MR imaging report included a statement describing the prevalence of common findings in asymptomatic individuals.
Abstract
Purpose:
To retrospectively examine the association between the inclusion of epidemiologic information in lumbar spine magnetic resonance (MR) imaging reports regarding findings in asymptomatic individuals and the rates of subsequent cross-sectional imaging and treatments in patients with low back pain or radiculopathy referred for imaging by primary care providers.
Materials and Methods:
Institutional review board approval was received for a retrospective chart review, with waiver of informed consent and HIPAA authorization. During 3 years, an epidemiologic statement was routinely but arbitrarily included in lumbar spine MR imaging reports. Two hundred thirty-seven reports documenting uncomplicated degenerative changes on initial lumbar spine MR images were identified, 71 (30%) of which included the statement (statement group) and 166 (70%) did not (nonstatement group). The rates of repeat cross-sectional imaging and treatments within 1 year were compared between groups by using logistic regression controlling for severity of MR imaging findings.
Results:
Patients in the statement group were significantly less likely to receive a prescription for narcotics for their symptoms than patients in the nonstatement group (odds ratio = 0.29, P = .01). Repeat cross-sectional imaging and physical therapy referrals were also less common in the statement group than in the nonstatement group (odds ratio = 0.22 and 0.55, respectively), but these differences were not statistically significant (P = .14 and .06, respectively). Rates of steroid injections, surgical consultations, and surgeries were similar between groups.
Conclusion:
Patients were less likely to receive narcotics prescriptions from primary care providers when epidemiologic information was included in their lumbar spine MR imaging reports.
© RSNA, 2012
Introduction
The frequency with which magnetic resonance (MR) imaging of the lumbar spine is used for patients with low back pain (LBP) is increasing (1,2). Treatments for LBP have increased in parallel with increased image utilization, including rates of medication prescriptions, particularly narcotics, epidural steroid injections, and spinal fusion surgeries (2–7). Consequently, expenditures related to LBP have grown substantially, outpacing general health expenditures, and have done so without corresponding improvements in self-assessed health status (8,9).
MR imaging examinations of the lumbar spine frequently reveal numerous findings, including disk desiccation, height loss, or bulging, with questionable relevance to patient symptoms. These findings, which for this analysis are all considered degenerative changes, are common in asymptomatic adults, with prevalences in this group as high as 90% (10–12). Moreover, multiple studies have failed to demonstrate clinical benefit with the use of early MR imaging for LBP compared with radiographs alone or no imaging at all; furthermore, the imaging results may negatively affect patients’ sense of well-being (7,13,14).
Despite this evidence and recommendations against early imaging (15,16), many physicians continue to refer patients with LBP or radiculopathy for early MR imaging of the lumbar spine. Furthermore, these ordering physicians are often primary care providers (15–17) who are less familiar with the nomenclature, clinical importance, and prevalence of many of the frequently encountered MR imaging findings than spine specialists. The purpose of this study was to retrospectively examine the association between the inclusion of epidemiologic information in lumbar spine MR imaging reports regarding findings in asymptomatic individuals and the rates of subsequent cross-sectional imaging and treatments in patients with LBP or radiculopathy referred for imaging by primary care providers.
Materials and Methods
This retrospective study was approved by our institutional review board. As part of a retrospective chart review investigation, the institutional review board waived requirements for informed consent and Health Insurance Portability and Accountability Act authorization.
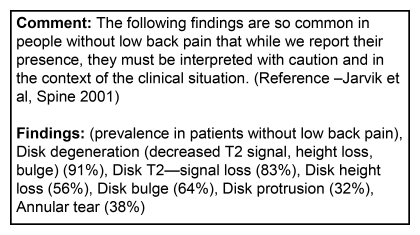
Epidemiologic Statement
Beginning in December 2005, a statement was added to our institution’s dictation software library that lists the reported prevalence rates of common findings at lumbar spine MR imaging in asymptomatic adults (Figure). The prevalence information was obtained from the Longitudinal Assessment of Imaging and Disability of the Back (LAIDback) Study, a prospective imaging study in asymptomatic individuals intended to identify anatomic risk factors for back pain (11). This statement was available to all users and was intended to be included in all lumbar spine MR imaging reports, although it was not part of the default template and was only used by a minority of radiologists.
Figure 1.
Epidemiologic statement included in lumbar spine MR imaging reports.
Subjects
To identify potential subjects, we searched the hospital picture archiving and communication system database for all lumbar spine MR imaging reports for patients 18 years or older generated between December 1, 2005 and December 31, 2008. We chose these dates to correspond with the initial use of the statement and to allow for 1 year of follow-up. This search identified 3902 reports, 379 (approximately 10%) of which included the prevalence statement.
Two authors (B.J.M. and G.R.J., 2nd- and 4th-year radiology residents, respectively) used the MR imaging reports and electronic medical record to screen for additional inclusion and exclusion criteria in an unblinded and independent manner. The available electronic medical record included clinical notes from this hospital, the affiliated university hospital, and a network of outpatient clinics. Our goal was to identify a cohort of patients with uncomplicated LBP or radiculopathy without serious underlying red flag conditions (16) who underwent lumbar spine MR imaging. We included patients with an indication for imaging of LBP (lumbago) or radiculopathy and the availability of clinical notes in the electronic medical record. We excluded patients with substantial trauma, malignancy, or infection; symptoms of cauda equina syndrome; prior lumbar spine MR imaging; a history of lumbar spine surgery; and findings on the current study beyond normal degenerative changes, including fractures, neoplastic processes, or infection. Because spine specialists (including spine surgeons, physiatrists, anesthesiologists, and neurologists) are likely to already be familiar with the nomenclature, importance, and prevalence of the findings described in the statement, we limited our study to examinations ordered by a physician from any other specialty (nonspine providers) who would be acting as primary care provider for the patient. In our sample, these specialties included internal medicine (and subspecialties), family practice, general surgery, emergency medicine, obstetrics and gynecology, and psychiatry. In addition, fewer than 10 subjects were identified who met the above criteria and had findings described as normal without any abnormalities. Because this group would be too small to draw meaningful conclusions, these patients were excluded from analysis.
We have complete information regarding exclusion criteria on the first 324 patients who were likely to be representative of the entire sample. The most common reason for exclusion was prior MR imaging and surgery (n = 124, 38%), which generally went together. Other exclusion criteria included substantial trauma (n = 72, 22%), infection (n = 54, 17%), cauda equina syndrome (n = 25, 8%), and cancer (n = 21, 6%). Patients did not meet inclusion criteria for the following reasons: symptoms were not related to LBP or radiculopathy (n = 14, 4%) and no follow-up clinical notes were available (n = 14, 4%).
We identified 237 subjects who met inclusion and exclusion criteria, of whom 71 (30%) received the epidemiologic statement in their lumbar spine MR imaging report (statement group) and 166 (70%) did not (nonstatement group). Subjects were referred for imaging by 148 different primary care providers (mean MR imaging referrals per provider, 1.6; range, one to nine).
Data Collection
We collected basic demographic data, including age, sex, self-described race or ethnicity, and insurance status at the time of imaging, if available. In many cases, race or ethnicity data were unavailable, and there was a wide array of responses; as such, we simplified this variable to white versus nonwhite.
We categorized the MR imaging findings described in the impression for each report as follows. Mild changes corresponded to the findings listed in the epidemiologic statement as being commonly detected in asymptomatic individuals. These included decreased disk T2 signal (desiccation), disk height loss, disk bulges, disk protrusions, annular fissures, and any other finding described as mild in the MR imaging report, such as central canal or neuroforaminal narrowing. Moderate or severe changes included disk extrusions and any other finding described as moderate or severe in the MR imaging report. As described previously, reports without any documented abnormalities were excluded from analysis.
Outcome Variables
By using the electronic medical record, we searched clinical notes and radiologic reports to identify outcome variables related to further management of the patient’s lumbar spine–related symptoms. These included repeat cross-sectional imaging of the lumbar spine (computed tomography [CT] or MR imaging), a prescription for narcotics, a physical therapy referral, a lumbosacral steroid injection, a surgical consultation, and spine surgery. Because patients may be receiving narcotics for other reasons, this variable was considered positive if the clinical note after receipt of the MR imaging report specifically stated the prescription was for the LBP that prompted the MR imaging. At our institution, lumbosacral steroid injections are performed by certain spine specialists after referral and assessment. All outcome variables were evaluated within 1 year of the initial MR imaging.
Statistical Analysis
We compared baseline patient characteristics between those whose report did and those whose report did not include the epidemiologic statement by using the x2 test. We used multivariate logistic regression analysis to test whether the two groups differed according to each of the outcomes while controlling for severity of MR imaging findings. Because the outcome variables were determined a priori, we did not correct for multiple comparisons. In addition, we repeated these comparisons, also controlling for sex, age, and race or ethnicity. All analyses were performed by using software (Stata, version 10; Stata, College Station, Tex), with a two-sided a level set at .05.
Results
Subjects
Patients who received the epidemiologic statement in their MR imaging report (statement group, n = 71) and those who did not (nonstatement group, n = 166) were similar with regard to sex, age group, insurance status, and referring provider specialty (Table 1). The proportion of self-identified whites in the statement group was lower than that in the nonstatement group (40% vs 54%), but this was not statistically significant (P = .06).
Table 1.
Baseline Demographic Characteristics of Statement and Nonstatement Groups
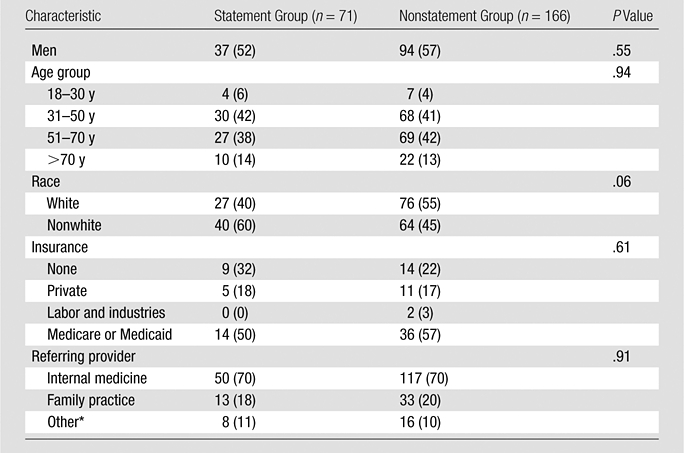
Note.—Data are numbers of patients, with percentages in parentheses.
Other specialties included emergency medicine (n = 4), general surgery (n = 8), obstetrics and gynecology (n = 5), psychiatry (n = 2), and unknown or nonallopathic provider (n = 5).
MR Imaging Findings
Forty (56%) of 71 patients in the statement group had MR imaging findings demonstrating mild changes compared with 74 (45%) of 166 patients in the nonstatement group, but this was not significantly different (P = .10, x2 test). Among patients with moderate or severe changes, central canal stenosis was the most common finding in both groups (18 [58%] of 31 in the statement group and 49 [54%] of 91 in the nonstatement group).
Outcomes
Repeat cross-sectional imaging of the lumbar spine within 1 year of initial MR imaging was uncommon in both groups: one (1%) patient in the statement group was reimaged versus 12 (7%) patients in the nonstatement group (Table 2). Logistic regression controlling for severity of MR imaging findings revealed a nonsignificant odds ratio of 0.22 (95% confidence interval: 0.03, 1.67; P = .14) for repeat cross-sectional imaging with the inclusion of the epidemiologic statement. Two patients were reimaged with CT, both in the nonstatement group, while the rest underwent repeat MR imaging.
Table 2.
Outcomes of Statement and Nonstatement Groups
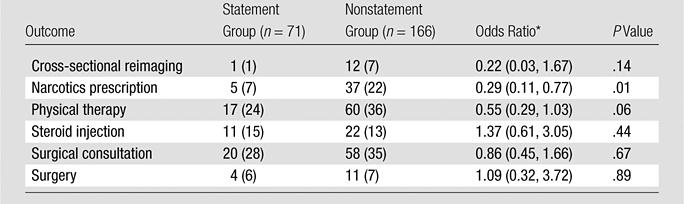
Note.—Unless otherwise indicated, data are numbers of patients, with percentages in parentheses.
Odds ratio represents comparison of statement and nonstatement groups, while controlling for severity of MR imaging findings. Data in parentheses are 95% confidence intervals.
Table 2 lists the numbers and percentages of patients receiving various therapies for their LBP or radiculopathy within 1 year after initial imaging. Logistic regression controlling for severity of MR imaging findings demonstrated that patients in the statement group were significantly less likely to receive a narcotics prescription for their presenting symptom at their follow-up clinic visit than patients in the nonstatement group (odds ratio = 0.29; 95% confidence interval: 0.11, 0.77; P = .01). This difference persisted even after patient sex, age, and race or ethnicity were added as covariates. In addition, there was a trend toward fewer physical therapy referrals in patients receiving the statement compared with the nonstatement group (odds ratio = 0.55; 95% confidence interval: 0.29, 1.03; P = .06). The rates of surgical consultations, lumbosacral steroid injections, and lumbar spine surgeries were similar between groups.
Discussion
In this study, patients with LBP or radiculopathy were less likely to receive a prescription for narcotics by primary care providers after lumbar spine MR imaging if the imaging report included a simple statement describing the prevalence of common findings in asymptomatic individuals. Similar trends were observed for repeat cross-sectional imaging and physical therapy referrals, although the differences were not statistically significant. Taken together, these findings suggest primary care providers were more reserved in their treatment of patients whose MR imaging report included the statement.
Because many abnormalities seen on spine radiographs may be incidental and not responsible for the patient’s symptoms, Roland and van Tulder (18) proposed adding statements to reports describing the prevalence of different degenerative findings in patients without back pain. They warned that if the clinician and patient interpreted these structural findings as the cause of the pain, the patient may be more likely to limit physical activity as a protective response, which is contrary to evidence-based recommendations for treating LBP.
Recent evidence has proved that unnecessary imaging may do more harm than good. Multiple randomized controlled trials have shown that the early use of imaging for LBP is not associated with improved outcomes and may even be harmful to the patient (13,14,19–23). The American College of Physicians recently reissued guidelines for imaging patients with LBP, emphasizing not only the inefficiencies of early imaging but also the potential harms (15). Furthermore, as rates of MR imaging of the lumbar spine have increased, so too have treatments, including narcotics prescriptions, lumbosacral injections, and spinal surgery, often without benefit (1,5,6,24–28). Not only do these treatments result in increased expenditures (8,9,28), but, more important, they pose serious risks to the health of the patient. Narcotics are associated with multiple side effects, including respiratory depression, cognitive impairment, constipation, and even death, as well as the development of tolerance and dependency (29,30). Complications from spinal surgeries, especially more invasive fusions, include wound complications, major medical complications, and death (28).
Our study had several limitations. First, our sample size was relatively small, limiting our power to detect statistically significant differences and posing the risk of a type II error. Post hoc power analysis calculation for repeat cross-sectional imaging reveals a power of 0.27. As a consequence, there may well have been a true difference between groups that was not detected with this small study. Despite 3 years of available data, we were only able to identify 237 patients with uncomplicated LBP or radiculopathy referred by primary care providers for initial lumbar spine MR imaging. Second, as a retrospective investigation, we were unable to control for the severity of baseline symptoms and functional impairment. It is possible that patients in the nonstatement group had more severe pain, hence necessitating more treatments and reimaging. However, given the arbitrary nature of including the statement and the lack of clinical differences detected on chart review, this was unlikely. Third, the statement was only included in a minority of reports even though it was intended for all. It is possible that it was preferentially included in reports with mild findings. However, the rates of mild changes were not significantly different between groups, and controlling for this and other baseline variables in our analyses did not affect the results. Fourth, outcome variables were extracted from the electronic medical record in an unblinded manner—the abstractors knew whether patients were in the statement or nonstatement group. We considered trying to blind the medical record reviewers, but this was ultimately not practical because the imaging results were readily available in the electronic medical record. We attempted to mitigate the risk of bias introduced in this manner by having consistent criteria for each outcome (documented clinical notes and procedures) applied as objectively as possible. Finally, the ordering clinicians and the reading radiologists were potential sources of data clustering. The risk of clustering affecting the results was low given the small number of studies ordered per clinician and the fact that the statement was only used by a minority of radiologists but reliably applied.
In conclusion, patients with LBP or radiculopathy were significantly less likely to receive a prescription for narcotics if the patient’s MR imaging report included a statement describing the prevalence of common findings in asymptomatic individuals. We also observed similar nonsignificant trends for repeat cross-sectional imaging and physical therapy referrals. Despite several limitations, these results suggest that the radiology report has a potentially greater influence on patient care than is commonly assumed. Generally expanding the scope of information included in imaging reports may assist the clinician, especially the primary care provider, in interpreting imaging results and optimizing clinical management and resource utilization. Larger-scale prospective studies will be necessary for confirmation of these findings.
Advance in Knowledge.
Patients were significantly less likely to receive a narcotics prescription for low back pain from primary care providers when an epidemiologic statement describing the prevalence of common findings in asymptomatic individuals was included in their lumbar spine MR imaging report.
Implication for Patient Care.
Expanding the scope of information included in imaging reports may better assist the nonspine provider in understanding imaging results and thereby influence subsequent clinical management and resource utilization.
Disclosures of Potential Conflicts of Interest: B.J.M. Financial activities related to the present article: none to disclose. Financial activities not related to the present article: RSNA resident research grant. Other relationships: none to disclose. G.R.J. No potential conflicts of interest to disclose. B.I.M. Financial activities related to the present article: none to disclose. Financial activities not related to the present article: author receives salary support as a research associate on a limited term project related to back pain from the National Bureau of Economic Research; author receives salary from the University of Washington through a subcontract on NIH grant R01AR054912 to examine complications of surgery for spinal stenosis; author receives salary support from Dartmouth College for work on two grants 1RC1A036268 (NIAMS) and HS018405 (AHRQ) to examine the epidemiology and safety of spinal surgery; author receives support from the University of Missouri-Kansas City as a research consultant on grant R01AT005061 (NCCAM) to examine costs related to complementary and alternative medicine in back pain; author received fees from Ohio State University for developing online modules for a comparative training effectiveness program. Other relationships: none to disclose. J.G.J. Financial activities related to the present article: none to disclose. Financial activities not related to the present article: author is consultant for GE Healthcare (CER Advisory Board) and HealthHelp; author has patents for, receives royalties from, has stock options for, and is cofounder of PhysioSonics. Other relationships: none to disclose.
Acknowledgments
The authors acknowledge the contribution of Annemarie Relyea-Chew, JD, MS, for her organization and administrative support for this project.
Received March 24, 2011; revision requested May 12; revision received September 14; accepted September 29; final version accepted October 17.
Funding:This research was supported by the National Institutes of Health (grant RO1 HS019222-01).
Abbreviations:
- LBP
- low back pain
References
- 1.Deyo RA, Mirza SK, Turner JA, Martin BI. Overtreating chronic back pain: time to back off? J Am Board Fam Med 2009;22(1):62–68 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Weiner DK, Kim YS, Bonino P, Wang T. Low back pain in older adults: are we utilizing healthcare resources wisely? Pain Med 2006;7(2):143–150 [DOI] [PubMed] [Google Scholar]
- 3.Gray DT, Deyo RA, Kreuter W, et al. Population-based trends in volumes and rates of ambulatory lumbar spine surgery. Spine (Phila Pa 1976) 2006;31(17):1957–1963; discussion 1964 [DOI] [PubMed] [Google Scholar]
- 4.Carrino JA, Morrison WB, Parker L, Schweitzer ME, Levin DC, Sunshine JH. Spinal injection procedures: volume, provider distribution, and reimbursement in the U.S. medicare population from 1993 to 1999. Radiology 2002;225(3):723–729 [DOI] [PubMed] [Google Scholar]
- 5.Friedly J, Chan L, Deyo R. Increases in lumbosacral injections in the Medicare population: 1994 to 2001. Spine (Phila Pa 1976) 2007;32(16):1754–1760 [DOI] [PubMed] [Google Scholar]
- 6.Luo X, Pietrobon R, Hey L. Patterns and trends in opioid use among individuals with back pain in the United States. Spine (Phila Pa 1976) 2004;29(8):884–890; discussion 891 [DOI] [PubMed] [Google Scholar]
- 7.Jarvik JG. Imaging of adults with low back pain in the primary care setting. Neuroimaging Clin N Am 2003;13(2):293–305 [DOI] [PubMed] [Google Scholar]
- 8.Martin BI, Deyo RA, Mirza SK, et al. Expenditures and health status among adults with back and neck problems. JAMA 2008;299(6):656–664 [DOI] [PubMed] [Google Scholar]
- 9.Martin BI, Turner JA, Mirza SK, Lee MJ, Comstock BA, Deyo RA. Trends in health care expenditures, utilization, and health status among US adults with spine problems, 1997-2006. Spine (Phila Pa 1976) 2009;34(19):2077–2084 [DOI] [PubMed] [Google Scholar]
- 10.Boden SD, Davis DO, Dina TS, Patronas NJ, Wiesel SW. Abnormal magnetic-resonance scans of the lumbar spine in asymptomatic subjects: a prospective investigation. J Bone Joint Surg Am 1990;72(3):403–408 [PubMed] [Google Scholar]
- 11.Jarvik JJ, Hollingworth W, Heagerty P, Haynor DR, Deyo RA. The Longitudinal Assessment of Imaging and Disability of the Back (LAIDBack) Study: baseline data. Spine (Phila Pa 1976) 2001;26(10):1158–1166 [DOI] [PubMed] [Google Scholar]
- 12.Jensen MC, Brant-Zawadzki MN, Obuchowski N, Modic MT, Malkasian D, Ross JS. Magnetic resonance imaging of the lumbar spine in people without back pain. N Engl J Med 1994;331(2):69–73 [DOI] [PubMed] [Google Scholar]
- 13.Modic MT, Obuchowski NA, Ross JS, et al. Acute low back pain and radiculopathy: MR imaging findings and their prognostic role and effect on outcome. Radiology 2005;237(2):597–604 [DOI] [PubMed] [Google Scholar]
- 14.Ash LM, Modic MT, Obuchowski NA, Ross JS, Brant-Zawadzki MN, Grooff PN. Effects of diagnostic information, per se, on patient outcomes in acute radiculopathy and low back pain. AJNR Am J Neuroradiol 2008;29(6):1098–1103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chou R, Qaseem A, Owens DK, Shekelle P; Clinical Guidelines Committee of the American College of Physicians. Diagnostic imaging for low back pain: advice for high-value health care from the American College of Physicians. Ann Intern Med 2011;154(3):181–189 [DOI] [PubMed] [Google Scholar]
- 16.Chou R, Qaseem A, Snow V, et al. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med 2007;147(7):478–491 [DOI] [PubMed] [Google Scholar]
- 17.Shreibati JB, Baker LC. The relationship between low back magnetic resonance imaging, surgery, and spending: impact of physician self-referral status. Health Serv Res 2011;46(5):1362–1381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Roland M, van Tulder M. Should radiologists change the way they report plain radiography of the spine? Lancet 1998;352(9123):229–230 [DOI] [PubMed] [Google Scholar]
- 19.Kendrick D, Fielding K, Bentley E, Kerslake R, Miller P, Pringle M. Radiography of the lumbar spine in primary care patients with low back pain: randomised controlled trial. BMJ 2001;322(7283):400–405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kerry S, Hilton S, Dundas D, Rink E, Oakeshott P. Radiography for low back pain: a randomised controlled trial and observational study in primary care. Br J Gen Pract 2002;52(479):469–474 [PMC free article] [PubMed] [Google Scholar]
- 21.Deyo RA, Diehl AK, Rosenthal M. Reducing roentgenography use: can patient expectations be altered? Arch Intern Med 1987;147(1):141–145 [DOI] [PubMed] [Google Scholar]
- 22.Gilbert FJ, Grant AM, Gillan MG, et al. Low back pain: influence of early MR imaging or CT on treatment and outcome—multicenter randomized trial. Radiology 2004;231(2):343–351 [DOI] [PubMed] [Google Scholar]
- 23.Jarvik JG, Hollingworth W, Martin B, et al. Rapid magnetic resonance imaging vs radiographs for patients with low back pain: a randomized controlled trial. JAMA 2003;289(21):2810–2818 [DOI] [PubMed] [Google Scholar]
- 24.Deshpande A, Furlan A, Mailis-Gagnon A, Atlas S, Turk D. Opioids for chronic low-back pain. Cochrane Database Syst Rev 2007;(3):CD004959. [DOI] [PubMed] [Google Scholar]
- 25.Airaksinen O, Brox JI, Cedraschi C, et al. Chapter 4: European guidelines for the management of chronic nonspecific low back pain. Eur Spine J 2006;15(suppl 2):S192–S300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Deyo RA, Gray DT, Kreuter W, Mirza S, Martin BI. United States trends in lumbar fusion surgery for degenerative conditions. Spine (Phila Pa 1976) 2005;30(12):1441–1445; discussion 1446–1447 [DOI] [PubMed] [Google Scholar]
- 27.Mirza SK, Deyo RA. Systematic review of randomized trials comparing lumbar fusion surgery to nonoperative care for treatment of chronic back pain. Spine (Phila Pa 1976) 2007;32(7):816–823 [DOI] [PubMed] [Google Scholar]
- 28.Deyo RA, Mirza SK, Martin BI, Kreuter W, Goodman DC, Jarvik JG. Trends, major medical complications, and charges associated with surgery for lumbar spinal stenosis in older adults. JAMA 2010;303(13):1259–1265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bartleson JD. Evidence for and against the use of opioid analgesics for chronic nonmalignant low back pain: a review. Pain Med 2002;3(3):260–271 [DOI] [PubMed] [Google Scholar]
- 30.Paulozzi LJ, Ryan GW. Opioid analgesics and rates of fatal drug poisoning in the United States. Am J Prev Med 2006;31(6):506–511 [DOI] [PubMed] [Google Scholar]