Abstract
This study compared measures of sleep from an accelerometer worn on the hip to measures obtained from an accelerometer worn on the wrist, the gold standard measure of sleep behavior in community research. The accelerometer worn on the hip provides a measure of TST in 10-11 year old children comparable to the wrist-worn unit. We provide an alternate method to ascertain bedtime and final wake time when diary data are missing. A hip-worn accelerometer may provide a cost-effective means of gathering physical activity and sleep data simultaneously in large samples of children with or without an accompanying sleep diary.
Keywords: obesity, sleep diary, physical activity, adolescent, children
Introduction
Over the past three decades the prevalence of obesity has more than tripled among U.S. children and adolescents (Ogden et al., 2006) and nurse practitioners and pediatricians are struggling to curtail the epidemic (Jacobson & Gance-Cleveland, 2010). While physical activity protects against obesity (Strong et al., 2005), it is well below recommended levels for children and adolescents (Whitt-Glover et al., 2009). Inadequate physical activity is of significant concern as it is strongly predictive of cardiovascular mortality among adults (Mitchell et al., 2010), and cardiovascular risk among youth (Owen et al., 2010), independent of weight status.
Low levels of activity have also been linked to poor sleep quality (Gupta, Mueller, Chan, & Meininger, 2002; Nixon et al., 2008). According to the Third National Health and Nutrition examination Survey (1988-1994) the prevalence of obesity and decreased levels of physical activity parallel the prevalence of sleep deprivation (Vgontzas, 2008). While sleep deprivation is linked to declines in daytime physical activity and to increases in obesity in adolescents (Gupta, Mueller, Chan, & Meininger, 2002; Nixon et al., 2008) the causal direction of this association is still unclear.
One barrier to further exploring the relationship among sleep, physical activity, and obesity is the difficulty inherent in measuring sleep and physical activity simultaneously. Currently, the majority of studies investigating sleep and physical activity use primarily self-report data (Landis, Parker, & Dunbar, 2009; Liou, Liou, & Chang, 2010), which are not reliable in children (Trost, 2007) and do not allow for distinguishing between sedentary, light, and moderate-vigorous physical activity. While accelerometers are an objective means of measuring both sleep and physical activity (Johnson et al., 2007), accelerometer protocols for assessment of sleep and activity are different. Currently, accelerometers are worn at the wrist or ankle to assess sleep among children (Gruber et al., 2007; Pesonen et al., 2009; Sadeh, Gruber, & Raviv, 2002), while accelerometers should be worn at the hip or low back to record physical activity (Trost, McIver, & Pate, 2005). Thus, accurate assessment of both sleep and physical activity requires that a subject wear two accelerometers – an expensive and burdensome endeavor – or switch the accelerometer between hip and wrist, a protocol that would likely be met with low compliance, particularly when a minimum of three consecutive days of accelerometer data are recommended to obtain valid and reliable measures (Littner et al., 2003).
The most complete sleep and physical activity data would be obtained if a single unit worn on the hip could capture both. However, only a handful of studies have assessed sleep with a hip- or trunk-worn accelerometer in children (Butte et al., 2007; Nixon et al., 2008), and no studies have compared wrist to hip placement in children. Therefore, it is unclear if use of a hip-worn accelerometer is a valid approach to measuring sleep. An additional complication when using accelerometers to measure sleep is the need for sleep diaries (to provide the child’s bedtime and final wake time), which are frequently incomplete (Cao & Guilleminault, 2008; Carskadon et al., 1976; Nixon et al., 2008; Treuth et al., 2003).
The primary purpose of this study was to compare estimates of total sleep time (TST) obtained from the Actigraph GT1M (Actigraph, Pensacola, FL) worn at the hip to that obtained from the Mini-MotionLogger (MML) accelerometer (Ambulatory Monitoring Inc., Ardsley, NY) worn on the wrist. Additionally, to maximize valid data when sleep diaries are incomplete or missing, we developed and tested criteria to estimate children’s bedtime and final wake time from accelerometer activity counts. Finally, a hip-worn accelerometer may be less sensitive to small movements during sleep than a wrist-worn accelerometer, which could lead to differences in estimates of sleep time in children with more active sleep patterns. Therefore, we sought to determine if quiet or active sleep patterns (Bullock & Schall, 2005) could account for any difference in TST between the hip- and wrist-worn units.
Methods
Participants
Fifth grade students were recruited to participate in this study from a physical education class in an urban elementary school. Written consent from a parent/guardian and verbal assent from the child were obtained. This study was approved by the University of California San Francisco Committee on Human Research.
Measures
The MML was chosen as the “gold standard” measure of sleep because it has been previously validated against polysomnography in children (Hyde et al., 2007; Sadeh, Sharkey, & Carskadon, 1994; So, Buckley, Adamson, & Horne, 2005; Tonetti, Pasquini, Fabbri, Belluzzi, & Natale, 2008) and is the most widely used measure of sleep in field research (Johnson et al., 2007; Sadeh et al., 1994). The MML is a wrist-watch size, battery-operated microprocessor that senses motion with a piezo-electric linear accelerometer with a sensitivity of ≥ 0.01g, 2-3Hz filter. The GT1M was chosen as the measure of physical activity because its activity counts have been validated against calorimetry in calibration studies (Puyau, Adolph, Vohra, Zakeri, & Butte, 2004; Treuth et al., 2004) and is widely used in research capturing physical activity in youth, including in the National Health and Nutrition Examination Surveys (Mark & Janssen, 2008; Mark & Janssen, 2009). The GT1M is a small (3.8 × 3.7 × 1.8 cm), lightweight (27g) accelerometer designed to detect vertical accelerations ranging in magnitude from 0.05g to 2.00g, with a frequency response of 0.25-2.50 Hz that senses motion using integrated circuitry. Participants were also given sleep diaries and asked to report their bedtime and final wake time.
Procedures
Participants were asked to wear the MML accelerometer on their non-dominant wrist and the GT1M accelerometer at their left hip (on an elastic belt) for three consecutive days and nights (72 hours) and to remove the units only when bathing or swimming. Parents and/or participants were telephoned each night to remind the child to wear the accelerometers appropriately and complete the sleep diary.
Researcher estimate of bedtime and wake time
Bedtime and wake times were available from sleep diaries. In addition, two separate researchers estimated bedtimes and final wake times from each participant’s raw accelerometer data. Bedtime was estimated by identifying the time after which: 1) activity counts dropped by at least 50% of the participant’s average daytime activity level; 2) a period of at least 5 consecutive minutes during which activity counts of 0 occurred; and 3) activity counts did not rise above 50% of daytime activity level for more than 5 consecutive minutes within a 3-hour period. Final wake time was estimated by identifying the time after which activity counts were greater than 0 continuously for at least 10 minutes. The average of the two researchers’ times was used; if these two estimates differed by more than 5 minutes, consensus was achieved with a third researcher (KL), an expert in sleep monitoring.
Sleep scoring routines
Each accelerometer unit has software algorithms based on the Sadeh scoring method (Sadeh et al., 1994) that analyze the raw accelerometer data to calculate sleep time. Action4 software (Ambulatory Monitoring Inc., Ardsley, NY) was used for the MML unit (data collected using zero-crossing mode), and Actilife Lifestyle Monitor version 3.6.0 software (Actigraph, Pensacola, FL) was used for the GT1M unit (data collected using summed magnitude), and each 1-minute epoch was scored in a binary fashion as sleep (1) or wake (0).
The following sleep measures were calculated from raw accelerometer data for each unit: 1) sleep onset time – the 1st minute of the first consecutive 15 min of sleep after bedtime; 2) total sleep period – the number of minutes from sleep onset to final morning awakening; and 3) total sleep time (TST) – the subset of minutes scored as sleep during the total sleep period (excludes any minutes scored as wake). Each sleep measure was calculated separately using bedtime and final wake time from sleep diaries and researcher estimate.
Variations in sleep architecture between active and quiet sleepers (Bullock & Schall, 2005) may affect the validity of the hip-worn accelerometer in estimating TST compared to the more sensitive wrist-worn accelerometer. Participants were categorized as either “quiet” or “active” by reviewing de-identified hypnograms of each child’s sleep patterns from both the GT1M and MML units. Children who primarily manifested inactivity on both hypnograms, were categorized as quiet sleepers. Children with hypnograms showing movement throughout the night were categorized as active sleepers. To control for possible adaptation to wearing the accelerometers during sleep, the second night’s sleep data were used to categorize quiet and active sleepers. For one child, the third night was used because the MML unit was worn incorrectly on the second night.
Primary analyses were limited to those children with complete sleep diary and accelerometer data (n=15). The average TST across nights was used for each child. Pearson correlations determined the strength of the association between the MML and GT1M units in estimating TST for all subjects, and separately for quiet and active sleepers. Paired t-tests compared mean TST between the MML and GT1M units. To determine the reliability of researchers in estimating bedtime and final wake time, we used paired t-tests to compare researcher estimates to diary accounts of bedtime and final wake time within each unit. Statistical analyses were carried out using STATA 10 software (StataCorp LP, College Station, TX).
Results
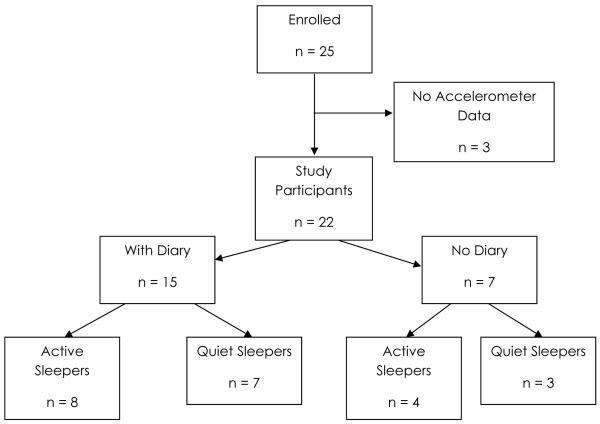
A total of 25 fifth graders were enrolled (age 10 or 11 years), 3 of whom were excluded because of missing accelerometer data (Figure 1). Fifteen participants returned sleep diaries; these children were similar to those who did not return diaries in proportion girls and active vs. quiet sleepers (Figure 1). When possible, analyses were conducted among all 22 study participants, although analyses requiring diary reports of bedtime and final wake time were necessarily limited to the 15 participants with a sleep diary.
Figure 1.
Participants enrolled in study.
Difference between units in TST
On average, children slept less than eight hours per night. Among children with diaries (n=15), the MML and GT1M unit estimates of TST were highly correlated whether bedtime and final wake times were based on diary (r=0.93) or researcher estimate from the raw activity counts (r=0.89). The difference in TST between the hip and wrist was 6.6 min (95% CI −3.6,16.8) when using diary bedtime and final wake time, and 2.2 min (95% CI −10.4, 14.7) when using researchers’ estimate of bedtime and final wake time (Table 1). When looking at all 22 subjects using researchers’ estimate of bedtime and final wake time, the difference between units in TST was 5.8 mins (95% CI −4.7, 16.3 mins).
Table 1.
Total sleep time (TST) from wrist- vs. hip-worn accelerometers (n=15)
| Wrist-worn MML | Hip-worn GT1M | Difference | Effect size | |
|---|---|---|---|---|
| Mean ± SD [Range] |
Mean ± SD [95% CI] |
(Cohen’s d) | ||
| Using Diary Account of Bed/Wake times |
7h 46m ± 50m [5h 34m, 8h 35m] |
7h 53m ± 47m [5h 39m, 8h 50m] |
7m ± 18m [−4m, 17m] |
0.13 |
| Using Researcher Estimate of Bed/Wake times |
7h 51m ± 49m [5h 40m, 8h 46m] |
7h 53m ± 46m [5h 47m, 9h 0m] |
2m ± 23m [−10m, 15m] |
0.05 |
Difference between diary account and researchers’ estimates of bedtime and wake time
Researchers’ estimates of final wake time were within 2 minutes of diary accounts within both the MML and GT1M units (Table 2). Researchers’ estimates of bedtime were approximately 20 minutes later than diary accounts for both units (Table 2). Despite later estimates of bedtime by researchers’ estimate, TST differed by only 0.7 mins (95% CI −11.8, 10.5 mins) within the GT1M unit and by 5.1mins (95% CI −16.4, 6.2 mins) within the MML based on researchers’ estimates vs. diary accounts of bedtime and final wake time.
Table 2.
Researcher Estimate vs. Diary Account of bedtime and final wake time (n=15)
| Researcher Estimate (RE) based on: |
Differences | |||||
|---|---|---|---|---|---|---|
| Diary Account |
MML data |
GT1M data |
Diary vs. RE - MML |
Diary vs. RE - GT1M |
RE - MML vs. GT1M |
|
| Mean ± SD (min) | Mean (min) ± SD [95% CI] | |||||
| Bedtime | 9:36PM ± 48m |
9:57PM ± 48m |
9:57PM ± 46m |
20.9 ± 0.7 [20.6, 21.3] |
21.5 ± 1.6 [18.0, 24.9] |
0.5 ± 2.3 [−0.6, 1.7] |
| Final wake time |
6:04AM ± 24m |
6:05AM ± 17m |
6:03AM ± 17m |
0.9 ± 7.2 [−2.8, 4.5] |
1.5 ± 6.8 [−1.9, 5.0] |
2.4 ± 0.4 [2.2, 2.6] |
Effect of sleep architecture
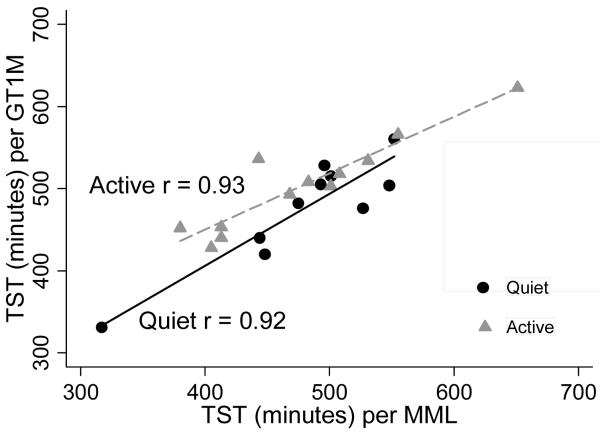
For the 15 subjects with a sleep diary, correlations between the MML and GT1M estimates of TST were the same (r = 0.97) among quiet sleepers and active sleepers based on diary accounts of bedtime and final wake time, and similar for quiet (r=0.94) and active (r=0.96) sleepers based on researchers’ estimates of bedtime and final wake time. The mean difference in TST between units was 9.1 min (95% CI −7.0, 25.3 mins) for quiet sleepers and 10.9 min (95% CI −4.0, 25.8) for active sleepers based on diary accounts on night 2. Using researcher estimate of bedtime and final wake time for all 22 subjects, correlations between units (Figure 2) were similar for quiet (r=0.92) and active sleepers (r=0.93), but the GT1M unit yielded consistently higher estimates of TST than the MML unit for active sleepers (25.3 minutes, 95% CI 4.9, 45.6). For quiet sleepers, TST was similar between units (−4 minutes, 95% CI −23.7, 15.7).
Figure 2. Total Sleep Time (TST) from wrist-worn MML unit vs. hip-worn GT1M unit among active and quiet sleepers on Night 2.
Correlations between GT1M and MML estimates of TST in quiet (n = 10) and active (n = 12) sleepers, with best fit regression lines.
Discussion
This study represents a systematic attempt to validate a hip-worn accelerometer in measuring total sleep time in children against the field gold standard, a wrist-worn accelerometer. The results of this study indicate that the GT1M accelerometer worn on the hip is comparable to the MML wrist-worn accelerometer in estimating TST. With an average difference in TST between units of 6.6 minutes, the hip-worn accelerometer appears to be a useful method for estimating sleep time outside of controlled laboratory conditions when bedtimes and final wake times can be reasonably documented.
This study provides valuable information for practitioners and researchers interested in capturing children’s physical activity and sleep patterns simultaneously while in their natural environment. The present results suggest that a unit worn at the hip can reliably assess sleep in children. To date, we are aware of only one study (Middelkoop, van Dam, Smilde-van den Doel, & Van Dijk, 1997) that compared wrist versus trunk placement of accelerometers in measuring sleep. Middelkoop’s study was done in adults and found weaker correlations (r=0.63-0.79) than the present study. However, Middelkoop used “mean duration of uninterrupted immobility” to calculate sleep time, which codes only continuous epochs with 0 activity counts as sleep (Middelkoop et al., 1997). The present study used the Sadeh scoring method developed for use with children, which allows for some movement during sleep and has been validated against polysomnography (Sadeh et al., 1994). Our findings support the use of a hip-worn accelerometer to capture both sleep and physical activity data.
This study also sought to develop and test criteria for estimating time in bedtime and final wake time from accelerometer data. We found that researcher estimates of bedtime and wake time were closely aligned with sleep diary entries. Despite calling participants or parents in this study nightly to remind them to complete the sleep diary, only 15 of 22 participants returned diaries with usable data. Our findings suggest that researcher estimates based on activity counts from the accelerometer could be used to impute bedtime and final wake time when diary data are missing, thereby maximizing usable data. Although estimating bedtime and final wake time from raw accelerometer data was labor intensive in the present study, further work to develop algorithms to automate estimations might reduce reliance on sleep diaries. The reliability of other technologies currently available to automatically assess bedtime should be considered for future studies. For example, light sensors in combination with an accelerometer unit and event marker to push at the time of lights out and final awakening may be useful in estimating bedtime, although each method is likely to pose its own set of challenges.
Correlations between units in estimating TST were similar for both active and quiet sleepers, although the hip-worn unit yielded consistently higher estimates of sleep time than the wrist unit by an average of 25 minutes among active sleepers. The greater difference in TST seen among active sleepers likely reflects motion of the hands at night among active sleepers (including self-soothing activities such as thumb-sucking) (Wolf & Lozoff, 1989) that goes undetected by the hip-worn unit, but is detected and scored as “wake” time by the wrist-worn unit. This also likely reflects the increased sensitivity of the MML in detecting smaller wrist movements using a zero-crossing mode. Without videography or polysomnography, it is not possible to determine whether the hip unit overestimates sleep, or the wrist unit underestimates sleep. Further work to develop algorithms to determine sleep architecture would be helpful for researchers interested in comparing differences between active and quiet sleepers, and could suggest appropriate corrections to use when assessing TST for active sleepers with a hip-worn accelerometer.
Limitations
While the upper bound of the 95% confidence interval suggests a difference between units in TST of no greater than 16 minutes (based on diary times or researcher estimates), the standard deviations were not trivial. Therefore, hip-worn accelerometers should be used cautiously in assessing sleep for an individual, but the present findings suggest they are reliable for tracking sleep in groups of children. The overall sample size was small, and some differences in TST might have been statistically significant with a larger sample size. However, the 95% CI suggests that even if statistically significant, differences in TST between units would not be clinically important, given the small effect sizes.
We did not use polysomnography as the gold standard measure of true sleep in this study. However, we chose the MML unit because it has been tested in the field and has been validated against polysomnography in multiple studies (Sadeh et al., 1994; So et al., 2005; Tonetti et al., 2008), one specifically in children (Hyde et al., 2007). The GT1M was specifically chosen for this validation study as it is widely used in field studies of physical activity and is the accelerometer being used in the National Health and Nutrition Examination Studies (NHANES) (Matthew, 2005; Troiano, 2005).
The lack of completed diary data by some study participants further limits our study findings. However, even when TST was calculated based on researcher estimated bedtime and wake time for all subjects, the difference between units was less than 6 minutes. It is important to note that using researcher estimates of bedtime precludes any valid calculation of sleep onset latency. “Bedtime” as estimated by researchers in the present study was approximately 20 minutes later than “Time in Bed” per sleep diaries, suggesting that researchers recognize “sleep onset” rather than the time at which children get into bed at night or turn off the light to get to sleep. While diary data or light sensor data would have allowed us to estimate sleep onset latency, that was not a specific aim of the present study.
These findings suggest that a hip-worn accelerometer can accurately assess TST with a sensitivity of about ±15 minutes in groups of young children. The ability to reliably capture both physical activity and sleep data with an accelerometer worn at the hip will facilitate examination of the relationship between physical activity and sleep and their potentially related effects on common childhood health problems such as obesity, attention deficit disorder (ADD), depression, and posttraumatic stress disorder (PTSD) (Davis, Tkacz, Gregoski, Boyle, & Lovrekovic, 2006; Glod, Teicher, Hartman, & Harakal, 1997; Gupta et al., 2002; Hong et al., 2009; Sadeh, Pergamin, & Bar-Haim, 2006). Combined with prior research on the validity of hip-worn accelerometers in assessing physical activity, findings from this research could make studying physical activity and sleep in large populations of children more feasible and cost-effective. Ultimately, greater understanding of the relationship between sleep, physical activity, and obesity may help to develop interventions effective in ameliorating pediatric obesity, and support practitioners as they work to improve child health.
Acknowledgments
This research was supported by the following grants: NIH/NICHD K23HD054470; American Heart Association 0865005F; Robert Wood Johnson Active Living Research 65715; NIH/NCRR/OD UCSF-CTSI TL1 RR024129. The authors wish to thank the school and the families who participated in this study and the PACCTR program at UCSF.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Bullock GL, Schall U. Dyssomnia in children diagnosed with attention deficit hyperactivity disorder: A critical review. The Australian and New Zealand Journal of Psychiatry. 2005;39(5):373–377. doi: 10.1080/j.1440-1614.2005.01584.x. doi:10.1111/j.1440-1614.2005.01584.x. [DOI] [PubMed] [Google Scholar]
- Butte NF, Puyau MR, Adolph AL, Vohra FA, Zakeri I. Physical activity in nonoverweight and overweight hispan ic children and adolescents. Medicine and Science in Sports and Exercise. 2007;39(8):1257–1266. doi: 10.1249/mss.0b013e3180621fb6. doi:10.1249/mss.0b013e3180621fb6. [DOI] [PubMed] [Google Scholar]
- Cao M, Guilleminault C. Sleep difficulties and behavioral outcomes in children. Archives of Pediatrics & Adolescent Medicine. 2008;162(4):385–389. doi: 10.1001/archpedi.162.4.385. doi:10.1001/archpedi.162.4.385. [DOI] [PubMed] [Google Scholar]
- Carskadon MA, Dement WC, Mitler MM, Guilleminault C, Zarcone VP, Spiegel R. Self-reports versus sleep laboratory findings in 122 drug-free subjects with complaints of chronic insomnia. The American Journal of Psychiatry. 1976;133(12):1382–1388. doi: 10.1176/ajp.133.12.1382. [DOI] [PubMed] [Google Scholar]
- Davis CL, Tkacz J, Gregoski M, Boyle CA, Lovrekovic G. Aerobic exercise and snoring in overweight childre n: A randomized controlled trial. Obesity (Silver Spring, Md.) 2006;14(11):1985–1991. doi: 10.1038/oby.2006.232. doi:10.1038/oby.2006.232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glod CA, Teicher MH, Hartman CR, Harakal T. Increased nocturnal activity and impaired sleep maintenance in abused children. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36(9):1236–1243. doi: 10.1097/00004583-199709000-00016. [DOI] [PubMed] [Google Scholar]
- Gruber R, Grizenko N, Schwartz G, Bellingham J, Guzman R, Joober R. Performance on the continuous performance test in children with ADHD is associated with sleep efficiency. Sleep. 2007;30(8):1003–1009. doi: 10.1093/sleep/30.8.1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta NK, Mueller WH, Chan W, Meininger JC. Is obesity associated with poor sleep quality in adolescents? American Journal of Human Biology: The Official Journal of the Human Biology Council. 2002;14(6):762–768. doi: 10.1002/ajhb.10093. doi:10.1002/ajhb.10093. [DOI] [PubMed] [Google Scholar]
- Hong X, Li J, Xu F, Tse LA, Liang Y, Wang Z, Yu IT, Griffiths S. Physical activity inversely associated with the presence of depression among urban adolescents in regional china. BMC Public Health. 2009;9(1):148. doi: 10.1186/1471-2458-9-148. doi:10.1186/1471-2458-9-148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hyde M, O’Driscoll DM, Binette S, Galang C, Tan SK, Verginis N, Davey MJ, Horne RS. Validation of actigraphy for determining sleep and wake in children with sleep disordered breathing. Journal of Sleep Research. 2007;16(2):213–216. doi: 10.1111/j.1365-2869.2007.00588.x. doi:10.1111/j.1365-2869.2007.00588.x. [DOI] [PubMed] [Google Scholar]
- Jacobson D, Gance-Cleveland B. A systematic review of primary healthcare provider education and training using the chronic care model for childhood obesity. Obesity Reviews: An Official Journal of the International Association for the Study of Obesity. 2010 doi: 10.1111/j.1467-789X.2010.00789.x. doi:10.1111/j.1467-789X.2010.00789.x. [DOI] [PubMed] [Google Scholar]
- Johnson NL, Kirchner HL, Rosen CL, Storfer-Isser A, Cartar LN, Ancoli-Israel S, Emancipator JL, Kibler AM, Redline S. Sleep estimation using wrist actigraphy in adolescents with and without sleep disordered breathing: A comparison of three data modes. Sleep. 2007;30(7):899–905. doi: 10.1093/sleep/30.7.899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landis AM, Parker KP, Dunbar SB. Sleep, hunger, satiety, food cravings, and caloric intake in adolescents. Journal of Nursing Scholarship: An Official Publication of Sigma Theta Tau International Honor Society of Nursing / Sigma Theta Tau. 2009;41(2):115–123. doi: 10.1111/j.1547-5069.2009.01262.x. doi:10.1111/j.1547-5069.2009.01262.x. [DOI] [PubMed] [Google Scholar]
- Liou YM, Liou TH, Chang LC. Obesity among adolescents: Sedentary leisure time and sleeping as determinants. Journal of Advanced Nursing. 2010;66(6):1246–1256. doi: 10.1111/j.1365-2648.2010.05293.x. doi:10.1111/j.1365-2648.2010.05293.x. [DOI] [PubMed] [Google Scholar]
- Littner M, Kushida CA, Anderson WM, Bailey D, Berry RB, Davila DG, Hirshkowitz M, Kapen S, Kramer M, Loube D, Wise M, Johnson SF, Standards of Practice Committee of the American Academy of Sleep Medicine Practice parameters for the role of actigraphy in the study of sleep and circadian rhythms: An update for 2002. Sleep. 2003;26(3):337–341. doi: 10.1093/sleep/26.3.337. [DOI] [PubMed] [Google Scholar]
- Mark AE, Janssen I. Dose-response relation between physical activity and blood pressure in youth. Medicine and Science in Sports and Exercise. 2008;40(6):1007–1012. doi: 10.1249/MSS.0b013e318169032d. doi:10.1249/MSS.0b013e318169032d. [DOI] [PubMed] [Google Scholar]
- Mark AE, Janssen I. Influence of bouts of physical activity on overweight in youth. American Journal of Preventive Medicine. 2009;36(5):416–421. doi: 10.1016/j.amepre.2009.01.027. doi:10.1016/j.amepre.2009.01.027. [DOI] [PubMed] [Google Scholar]
- Matthew CE. Calibration of accelerometer output for adults. Medicine and Science in Sports and Exercise. 2005;37(11 Suppl):S512–22. doi: 10.1249/01.mss.0000185659.11982.3d. [DOI] [PubMed] [Google Scholar]
- McAdams CB. The environment and pediatric overweight: A review for nurse practitioners. Journal of the American Academy of Nurse Practitioners. 2010;22(9):460–467. doi: 10.1111/j.1745-7599.2010.00537.x. doi:10.1111/j.1745-7599.2010.00537.x. [DOI] [PubMed] [Google Scholar]
- Middelkoop HA, van Dam EM, Smilde-van den Doel DA, Van Dijk G. 45-hour continuous quintuple-site actimetry: Relations between trunk and limb movements and effects of circadian sleep-wake rhythmicity. Psychophysiology. 1997;34(2):199–203. doi: 10.1111/j.1469-8986.1997.tb02132.x. [DOI] [PubMed] [Google Scholar]
- Mitchell JA, Bornstein DB, Sui X, Hooker SP, Church TS, Lee CD, Lee DC, Blair SN. The impact of combined health factors on cardiovascular disease mortality. American Heart Journal. 2010;160(1):102–108. doi: 10.1016/j.ahj.2010.05.001. doi:10.1016/j.ahj.2010.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Sleep Foundation 2006 sleep america poll. 2006 Retrieved 01/15, 2006, from http://www.sleepfoundation.org/sites/default/files/2006_summary_of_findings.pdf.
- Nixon GM, Thompson JM, Han DY, Becroft DM, Clark PM, Robinson E, Waldie KE, Wild CJ, Black PN, Mitchell EA. Short sleep duration in middle childhood: Risk factors and consequences. Sleep. 2008;31(1):71–78. doi: 10.1093/sleep/31.1.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the united states, 1999-2004. JAMA: The Journal of the American Medical Association. 2006;295(13):1549–1555. doi: 10.1001/jama.295.13.1549. doi:10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- Owen CG, Nightingale CM, Rudnicka AR, Sattar N, Cook DG, Ekelund U, Whincup PH. Physical activity, obesity and cardiometabolic risk factors in 9- to 10-year-old UK children of white european, south asian and black african-caribbean origin: The child heart and health study in england (CHASE) Diabetologia. 2010;53(8):1620–1630. doi: 10.1007/s00125-010-1781-1. doi:10.1007/s00125-010-1781-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pesonen AK, Raikkonen K, Matthews K, Heinonen K, Paavonen JE, Lahti J, Komsi N, Lemola S, Jarvenpaa AL, Kajantie E, Strandberg T. Prenatal origins of poor sleep in children. Sleep. 2009;32(8):1086–1092. doi: 10.1093/sleep/32.8.1086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pratt KJ, Lamson AL, Collier DN, Harris N, Ballard S, Saporito M, Sarvey S, Gross K, Crawford YS. Camp golden treasures: A multidisciplinary weight-loss and a healthy lifestyle camp for adolescent girls. Families, Systems & Health: The Journal of Collaborative Family Healthcare. 2009;27(1):116–124. doi: 10.1037/a0014912. doi:10.1037/a0014912. [DOI] [PubMed] [Google Scholar]
- Puyau MR, Adolph AL, Vohra FA, Zakeri I, Butte NF. Prediction of activity energy expenditure using accelerometers in children. Medicine and Science in Sports and Exercise. 2004;36(9):1625–1631. [PubMed] [Google Scholar]
- Sadeh A, Gruber R, Raviv A. Sleep, neurobehavioral functioning, and behavior problems in school-age children. Child Development. 2002;73(2):405–417. doi: 10.1111/1467-8624.00414. [DOI] [PubMed] [Google Scholar]
- Sadeh A, Pergamin L, Bar-Haim Y. Sleep in children with attention-deficit hyperactivity disorder: A meta-analysis of polysomnographic studies. Sleep Medicine Reviews. 2006;10(6):381–398. doi: 10.1016/j.smrv.2006.03.004. doi:10.1016/j.smrv.2006.03.004. [DOI] [PubMed] [Google Scholar]
- Sadeh A, Sharkey KM, Carskadon MA. Activity-based sleep-wake identification: An empirical test of methodological issues. Sleep. 1994;17(3):201–207. doi: 10.1093/sleep/17.3.201. [DOI] [PubMed] [Google Scholar]
- So K, Buckley P, Adamson TM, Horne RS. Actigraphy correctly predicts sleep behavior in infants who are younger than six months, when compared with polysomnography. Pediatric Research. 2005;58(4):761–765. doi: 10.1203/01.PDR.0000180568.97221.56. doi:10.1203/01.PDR.0000180568.97221.56. [DOI] [PubMed] [Google Scholar]
- Strong WB, Malina RM, Blimkie CJR, Daniels SR, Dishman RK, Gutin B, Hergenroeder AC, Must A, Nixon PA, Pivarnik JM, Rowland T, Trost S, Trudeau F. Evidence based physical activity for school-age youth. The Journal of Pediatrics. 2005;146(6):732–737. doi: 10.1016/j.jpeds.2005.01.055. doi:DOI: 10.1016/j.jpeds.2005.01.055. [DOI] [PubMed] [Google Scholar]
- Tonetti L, Pasquini F, Fabbri M, Belluzzi M, Natale V. Comparison of two different actigraphs with polysomnography in healthy young subjects. Chronobiology International. 2008;25(1):145–153. doi: 10.1080/07420520801897228. doi:10.1080/07420520801897228. [DOI] [PubMed] [Google Scholar]
- Treuth MS, Schmitz K, Catellier DJ, McMurray RG, Murray DM, Almeida MJ, Going S, Norman JE, Pate R. Defining accelerometer thresholds for activity intensities in adolescent girls. Medicine and Science in Sports and Exercise. 2004;36(7):1259–1266. [PMC free article] [PubMed] [Google Scholar]
- Treuth MS, Sherwood NE, Butte NF, McClanahan B, Obarzanek E, Zhou A, Ayers C, Adolph A, Jordan J, Jacobs DR, Rochon J. Validity and reliability of activity measures in african-american girls for GEMS. Medicine and Science in Sports and Exercise. 2003;35(3):532–539. doi: 10.1249/01.MSS.0000053702.03884.3F. doi:10.1249/01.MSS.0000053702.03884.3F. [DOI] [PubMed] [Google Scholar]
- Troiano RP. A timely meeting: Objective measurement of physical activity. Medicine and Science in Sports and Exercise. 2005;37(11 Suppl):S487–9. doi: 10.1249/01.mss.0000185473.32846.c3. [DOI] [PubMed] [Google Scholar]
- Trost SG, McIver KL, Pate RR. Conducting accelerometer-based activity assessments in field-based research. Medicine and Science in Sports and Exercise. 2005;37(11 Suppl):S531–43. doi: 10.1249/01.mss.0000185657.86065.98. [DOI] [PubMed] [Google Scholar]
- Trost SG. State of the art reviews: Measurement of physical activity in children and adolescents. American Journal of Lifestyle Medicine. 2007 July/August;1:299–314. [Google Scholar]
- Vgontzas AN. Does obesity play a major role in the pathogenesis of sleep apnoea and its associated manifestations via inflammation, visceral adiposity, and insulin resistance? Archives of Physiology and Biochemistry. 2008;114(4):211–223. doi: 10.1080/13813450802364627. doi:10.1080/13813450802364627. [DOI] [PubMed] [Google Scholar]
- Whitt-Glover MC, Taylor WC, Floyd MF, Yore MM, Yancey AK, Matthews CE. Disparities in physical activity and sedentary behaviors among US children and adolescents: Prevalence, correlates, and intervention implications. Journal of Public Health Policy. 2009;30(Suppl 1):S309–34. doi: 10.1057/jphp.2008.46. doi:10.1057/jphp.2008.46. [DOI] [PubMed] [Google Scholar]
- Wolf AW, Lozoff B. Object attachment, thumbsucking, and the passage to sleep. Journal of the American Academy of Child and Adolescent Psychiatry. 1989;28(2):287–292. doi: 10.1097/00004583-198903000-00024. [DOI] [PubMed] [Google Scholar]