Abstract
Magnetic resonance imaging (MRI) allows unprecedented access to the anatomy and physiology of the developing brain without the use of ionizing radiation. Over the past two decades, thousands of brain MRI scans from healthy youth and those with neuropsychiatric illness have been acquired and analyzed with respect to diagnosis, sex, genetics, and/or psychological variables such as IQ. Initial reports comparing size differences of various brain components averaged across large age spans have given rise to longitudinal studies examining trajectories of development over time and evaluations of neural circuitry as opposed to structures in isolation. Although MRI is still not of routine diagnostic utility for evaluation of pediatric neuropsychiatric disorders, patterns of typical versus atypical development have emerged that may elucidate pathologic mechanisms and suggest targets for intervention. In this review we summarize general contributions of structural MRI to our understanding of neurodevelopment in health and illness.
MRI of Brain Anatomy in Typical Pediatric Development
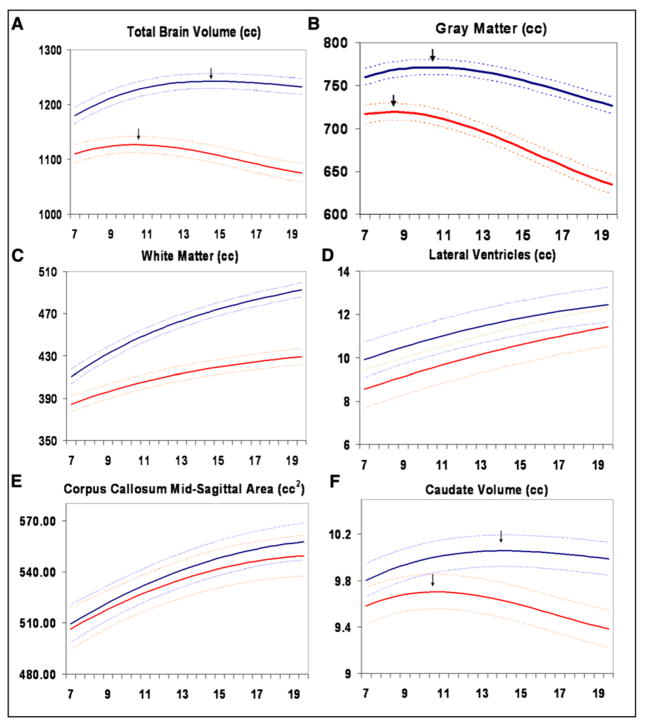
The human brain has a particularly protracted maturation, with different tissue types, brain structures, and neural circuits having distinct developmental trajectories undergoing dynamic changes throughout life. Longitudinal MR scans of typically developing children and adolescents demonstrate increasing white matter (WM) volumes and inverted U shaped trajectories of gray matter (GM) volumes with peak sizes occurring at different times in different regions. Figure 1 shows age by size trajectories from a longitudinal study comprising 829 scans from 387 subjects, ages 3–27 years (see Figure 1 and Supplemental Experimental Procedures).
Figure 1. Developmental Trajectories of Brain Morphometry: Ages 6–20 Years.
Mean volume by age in years for males (n = 475 scans) and females (n = 354 scans). Middle lines in each set of three lines represent mean values, and upper and lower lines represent upper and lower 95% confidence intervals. All curves differed significantly in height and shape with the exception of lateral ventricles, in which only height was different, and midsagittal area of the corpus callosum, in which neither height nor shape was different. (A) Total brain volume, (B) gray matter volume, (C) white matter volume, (D) lateral ventricle volume, (E) midsagittal area of the corpus callosum, and (F) caudate volume. Reprinted from Lenroot et al. 2007).
Total Cerebral Volume
In the Child Psychiatry Branch cohort noted above, total cerebral volume follows an inverted U shaped trajectory peaking at age 10.5 in girls and 14.5 in boys (Lenroot et al., 2007). In both males and females, the brain is already at 95% of its peak size by age 6 (Figure 1A). Across these ages, the group average brain size for males is ~10% larger than for females. This 10% differences is consistent with a vast adult neuroimaging and postmortem study literature but is often explained as being related to the larger body size of males. However, in our pediatric subjects the boys’ bodies are not larger than girls’ until after puberty. Further evidence that brain size is not tightly linked to body size is the fundamental decoupling of brain and body size maturational trajectories, with body size increasing through approximately age 17.
Differences in brain size should not be interpreted as necessarily imparting any sort of functional advantage or disadvantage. In the case of male/female differences, gross structural measures may not reflect sexually dimorphic differences in functionally relevant factors such as neuronal connectivity and receptor density.
Sowell and colleagues measured changes in brain volume in a group of 45 children scanned twice (2 years apart) between ages 5 and 11 (Sowell et al., 2004). Using a very different method, in which the distance was measured between points on the brain surface and the center of the brain, they found increases in brain size during this age span, particularly in the frontal and occipital regions.
Cerebellum
Caviness et al., in a cross-sectional sample of 15 boys and 15 girls aged 7–11, found that the cerebellum was at adult volume in females but not males at this age range, suggesting the presence of late development and sexual dimorphism (Caviness et al., 1996). The function of the cerebellum has traditionally been described as related to motor control, but it is now commonly accepted that the cerebellum is also involved in emotional processing and other higher cognitive functions that mature throughout adolescence (Riva and Giorgi, 2000; Schmahmann, 2004).
In the Child Psychiatry Branch cohort, developmental curves of total cerebellum size were similar to that of the cerebrum following an inverted U shaped developmental trajectory with peak size occurring at 11.3 in girls and 15.6 in boys. In contrast to the evolutionarily more recent cerebellar hemispheric lobes that followed the inverted U shaped developmental trajectory, cerebellar vermis size did not change across this age span (Tiemeier et al., 2010).
White Matter
The white color of “white matter” is produced by myelin, fatty white sheaths formed by oligodendrocytes that wrap around axons and drastically increase the speed of neuronal signals. The volume of WM generally increases throughout childhood and adolescence (Lenroot et al., 2007), which may underlie greater connectivity and integration of disparate neural circuitry. An important feature that has only recently been appreciated is that myelin does not simply maximize speed of transmission but modulates the timing and synchrony of the neuronal firing patterns that create functional networks in the brain (Fields and Stevens-Graham, 2002). Consistent with this, a study using a measure of white matter density to map regional white matter growth found rapid localized increases between childhood and adolescence. Corticospinal tracts showed increases that were similar in magnitude on both sides, while tracts connecting the frontal and temporal regions showed more increase in the left-sided language-associated regions (Paus et al., 1999).
Gray Matter
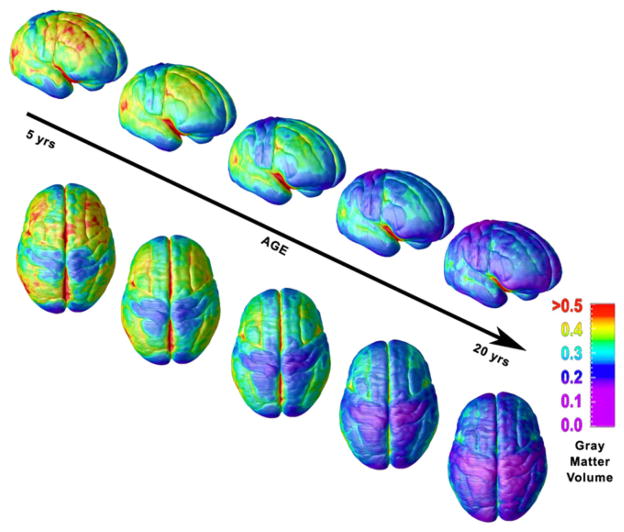
Whereas WM increases during childhood and adolescence, the trajectories of GM volumes follow an inverted U shaped developmental trajectory. The different developmental curves of WM and GM belie the intimate connections among neurons, glial cells, and myelin, which are fellow components in neural circuits and are linked by lifelong reciprocal relationships. Cortical GM changes at the voxel level from ages 4 to 20 years derived from scans of 13 subjects who had each been scanned four times at ~2 year intervals are shown in Figure 2 (animation is available at http://www.nimh.nih.gov/videos/press/prbrainmaturing.mpeg) (Gogtay et al., 2004b). The age of peak GM density is earliest in primary sensorimotor areas and latest in higher-order association areas such as the dorsolateral prefrontal cortex, inferior parietal, and superior temporal gyrus. An unresolved question is the degree to which the cortical GM reductions are driven by synaptic pruning versus myelination along the GM/WM border (Sowell et al., 2001). The volume of the caudate nucleus, a subcortical GM structure, also follows an inverted U shaped developmental trajectory, with peaks similar to the frontal lobes with which they share extensive connections (Lenroot et al., 2007).
Figure 2. Regional Maturation of Cortical Thickness: Ages 4–21 Years.
Right lateral and top views of the dynamic sequence of GM maturation over the cortical surface. The side bar shows a color representation in units of GM volume. Reprinted from Gogtay et al. (2004a).
Developmental Trajectories: The Journey as Well as the Destination
A prominent tenet now established in the neuroimaging literature is that the shape of the age by size trajectories may be related to functional characteristics even more so than the absolute size. For instance, in a longitudinal study comprising 692 scans from 307 typically developing subjects, age by cortical thickness developmental curves were more predictive of IQ than differences in cortical thickness at age 20 years (Shaw et al., 2006a). Age by size trajectories are also more discriminating than static measures for sexual dimorphism where lobar peak GM volumes occur 1–3 years earlier in females (Lenroot et al., 2007). Trajectories are increasingly being employed as a discerning phenotype in studies of psychopathology as well (Giedd et al., 2008).
Many psychiatric disorders (both child and adult) have long been hypothesized to reflect subtle abnormalities in brain development. Anatomic brain developmental studies have revived and extended our understanding of normal and abnormal developmental patterns as well as plastic response to illness. It is beyond the scope of this review to discuss any disorder in great depth, but an overview of a series of studies for attention-deficit/hyperactivity disorder (ADHD), very early (childhood) onset schizophrenia (COS), and autism illustrate some key principles.
Attention-Deficit/Hyperactivity Disorder
ADHD is the most common neurodevelopment disorder of childhood, affecting between 5% and 10% of school-age children and 4.4% of adults (Kessler et al., 2005). There remains controversy over this disorder because of the lack of any biological diagnostic test, the frequency of salient symptoms (inattention, restlessness, and impulsivity) in the general population, the good long-term outcome for about half of childhood cases, and the possible overuse of stimulant drug treatment.
Cross-sectional anatomical imaging studies of ADHD consistently point to involvement of the frontal lobes (Castellanos et al., 2002), parietal lobes (Sowell et al., 2003), basal ganglia (Castellanos and Giedd, 1994), corpus callosum (Giedd et al., 1994), and cerebellum (Berquin et al., 1998). Imaging studies of brain physiology also support involvement of right frontal-basal ganglia circuitry with a powerful modulatory influence from the cerebellum (see Giedd et al., 2001, for review).
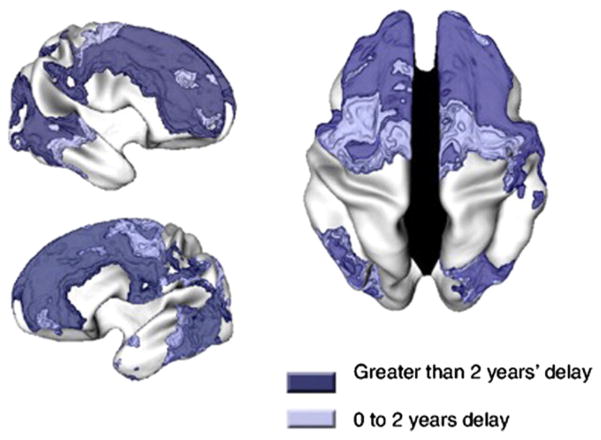
Because of the wide range of clinical outcomes seen in ADHD, longitudinal studies have been of particular interest. Such studies indicate a developmental delay of cortical thickness trajectories most markedly for the frontal lobes (Shaw et al., 2007a) (see Figure 3). The general pattern of primary sensory areas attaining peak cortical thickness before polymodal, high-order association areas occurred in both those with and without ADHD. However, the median age by which 50% of the cortical points attained peak thickness was 10.5 years for ADHD and 7.5 years for controls. The area with the greatest age difference was the middle prefrontal cortex, reaching peak thickness at 10.9 years in those with ADHD and 5.9 years for controls.
Figure 3. Developmental Delay of Cortical Thickness in ADHD.
Regions where the ADHD group had delayed cortical maturation, as indicated by an older age of attaining peak cortical thickness. Reprinted from Shaw et al. (2006b).
A theme of our ADHD studies is that clinical improvement is often mirrored by a convergence of developmental trajectories toward typical development and that persistence of ADHD is accompanied by a progressive divergence away from typical development. We have demonstrated this for the cortex, where right parietal cortical normalization accompanied clinical improvement (Shaw et al., 2006b)—and for the cerebellum, where progressive volume loss of the inferior posterior lobes mirrors persistence of ADHD (Mackie et al., 2007). A similar principle may hold for the hippocampus: children with ADHD who remit show a trajectory that is similar to that of typical development, whereas persistent ADHD is accompanied by a progressive loss of hippocampal volume (Shaw et al., 2007b). These highly significant findings occur independently, and thus one cannot simply see ADHD as “delayed frontal development.” It also should be stressed that, to date, these measures alone or combined are not clinically useful for either diagnosis or clinical outcome.
Stimulants remain the most effective and widely used treatment of ADHD, improving on task behavior and minimizing disruptive symptoms. Earlier studies indicating that stimulants have a normalizing influence on subcortical and white matter development (Castellanos et al., 2002) have been extended to cortical development (Shaw et al., 2009) and to the thalamus (Logvinov et al., 2009). Whether this normalization represents activity-driven or treatment-related plastic changes or a more direct neural effect of medication remains unknown.
There is considerable epidemiological and neuropsychological evidence that ADHD is best considered dimensionally, lying at the extreme of a continuous distribution of symptoms and underlying cognitive impairments. We thus asked if cortical brain development in typically developing children with symptoms of hyperactivity and impulsivity resembles that found in the syndrome. Specifically, we found that a slower rate of cortical thinning during late childhood and adolescence, which we previously found in ADHD, is also linked with severity of symptoms of hyperactivity and impulsivity in typically developing children, providing neurobiological evidence for the dimensionality of the disorder.
Schizophrenia
Schizophrenia is widely considered a neurodevelopmental disorder (Weinberger, 1987; Rapoport et al., 2005). The study of COS provides an excellent opportunity to investigate the specifics of the neurodevelopmental deviations as (1) scans can be obtained during the most dynamic and relevant periods of brain development and (2) childhood-onset counterparts of typical adult-onset illnesses usually show a more severe phenotype less likely to be influenced by environmental factors and more likely to show genetic influences.
A study of COS has been ongoing at the NIMH since 1990. The diagnosis is made using unmodified DSM-III-R/IV criteria and, in most cases, after a drug-free inpatient observation. Although rare, occurring ~1/500th as often as adult-onset schizophrenia (AOS), the COS cases (n = 102 to date) clinically resemble poor-outcome AOS cases, in that all phenomenological, family, and neurobiological studies in COS show similar findings as in AOS, suggesting continuity between these two forms of the illness (Gogtay and Rapoport, 2008).
Neuroimaging findings from the COS cohort are consistent with the AOS literature showing increased lateral ventricular volume, decreased total and regional cortical GM volumes, decreased hippocampal and amygdala volumes, and increased basal ganglia volumes that progressed during adolescence (see Gogtay and Rapoport, 2008, for review). Most strikingly revealed by longitudinal data is progressive cortical GM loss during adolescence (Thompson et al., 2001) and delayed white matter development (Gogtay et al., 2008). The cortical GM reduction becomes more circumscribed with age (as the healthy group trajectory of cortical thinning “catches up” with the accelerated pattern of cortical GM loss seen in COS). The cortical GM loss in schizophrenia has been shown to be due to the loss of “neuropil,” which consists of glia, synaptic and dendritic arbors, and vasculature (Selemon and Goldman-Rakic, 1999). Postmortem studies show no widespread neuronal loss in schizophrenia or a glial response to a potential neuronal injury. Based on these and other converging data, developmental models of abnormal synaptic function or structure have predominated (Weinberger et al., 1992).
Autism
Autism is defined by abnormal behavior in the spheres of communication, social relatedness, and stereotyped behaviors within the first 3 years of life. In children with autism, there is an early acceleration of brain growth, which overshoots typical dimensions, leading to transient cerebral enlargement (Courchesne et al., 2007). Brain imaging and genetic studies of COS provided unexpected links to autism with respect to a “shift to the right” in early brain development (more rapid brain growth during the first years of life in autism and premature decrease in cortical thickness during adolescence for COS). A possible intermediate phenotype of altered timing of brain developmental events (Rapoport et al., 2009) or alternate “polar” brain pathways have been proposed (Crespi et al., 2010). We predict that future treatment research will focus on agents that have more general “normalizing effects” on brain development. To date, there is limited evidence that stimulant drugs may have such an effect as mentioned above (Sobel et al., 2010).
In summary, clinical studies indicate diagnosis-specific group anatomic brain differences that although not diagnostic are beginning to elucidate the timing and nature of deviations from typical development. Using trajectories (i.e., morphometric measures by age) as an endophenotype may provide discriminating power where static measures do not (Giedd et al., 2008). It is increasingly clear that the same molecular genetic risk can be associated with a range of psychiatric phenotypes, including autism, bipolar disorder, schizophrenia, mental retardation, and epilepsy. Conversely, the same psychiatric phenotype is likely to reflect numerous individually rare genetic abnormalities such as copy number variants (Bassett et al., 2010; McClellan and King, 2010). Exploring the role of genetic variants on timing of brain development may clarify some of these issues of sensitivity and specificity.
High Variability of Brain Measures across Individuals
All of the data presented above must be interpreted in light of the strikingly high variability of brain size measures across individuals (Lange et al., 1997). This high variability extends to measures of brain substructures as well. The high variability and substantial overlap of most measures for most groups being compared has profound implications for the diagnostic utility of psychiatric neuroimaging and the sensitivity/specificity in using neuroimaging to make predictions about behavior or ability in a particular individual. For example, although group average anatomic MRI differences have been reported for all major psychiatric disorders, MRI is not currently indicated for the routine diagnosis of any. Likewise, although on group average there are statistically robust differences between male and female brains, there is nothing on an individual MRI brain scan to confidently discern whether it is of a man or a woman. As an analogy, height for adult men is significantly greater than height for adult women. However, there are so many women taller than so many men that height alone would not be a very useful way to determine someone’s sex. Male/female differences in height are about twice the effect size of most neuroimaging or neuropsychological measures.
Going from group average differences to individual use is one of the preeminent challenges of neuroimaging. As much of the utility of neuroimaging relies on the extent to which this challenge can be met, accounting for the variability is of prime importance. In the following section, we will examine some of the parameters known to influence variation in brain development.
Influences on Developmental Trajectories of Brain Anatomy during Childhood and Adolescence
Genes and Environment
By comparing similarities between monozygotic (MZ) twins, who share ~100% of the same genes, and dizygotic (DZ) twins, who share ~50% of the same genes, we can estimate relative contributions of genetic and nongenetic influences on trajectories of brain development. To pursue this question, we are conducting a longitudinal neuroimaging study of twins and currently have acquired ~600 scans from 90 MZ and 60 DZ twin pairs. Structural equation modeling (SEM) is used to assess age × gene × environment interactions and other epistatic phenomena that challenge conventional interpretation of twin data. SEM describes the interacting effects as (A) additive genetic, (C) shared environmental, or (E) unique environmental factors (Neale and Cardon, 1992). For most brain structures examined, additive genetic effects (i.e., “heritability”) are high and shared environmental effects are low (Wallace et al., 2006). Additive genetic effects for total cerebral and lobar volumes (including GM and WM sub-compartments) ranged from 0.77 to 0.88; for the caudate, 0.80; and for the corpus callosum, 0.85. The cerebellum has a distinctive heritability profile with an additive genetic effect of only 0.49, although wide confidence intervals merit cautious interpretation. Highly heritable brain morphometric measures provide biologic markers for inherited traits and may serve as targets for genetic linkage and association studies (Gottesman and Gould, 2003).
Multivariate analyses allow assessment of the degree to which the same genetic or environmental factors contribute to multiple neuroanatomic structures. Like the univariate variables, these interstructure correlations can be parceled into relationships of either genetic or environmental origin. This knowledge is vitally important for interpretation of most of the twin data, including understanding the impact of genes that may affect distributed neural networks, as well as interventions that may have global brain impacts. Shared effects account for more of the variance than structure-specific effects, with a single genetic factor accounting for 60% of variability in cortical thickness (Schmitt et al., 2007). Six factors account for 58% of the remaining variance, with five groups of structures strongly influenced by the same underlying genetic factors. These findings are consistent with the radial unit hypothesis of neocortical expansion proposed by Rakic (Rakic, 1995) and with hypotheses that global, genetically mediated differences in cell division were the driving force behind interspecies differences in total brain volume (Darlington et al., 1999; Finlay and Darlington, 1995; Fishell, 1997). Expanding the entire brain when only specific functions might be selected for is metabolically costly, but the number of mutations required to affect cell division would be far less than that required to completely change cerebral organization.
Age-related changes in heritability may be linked to the timing of gene expression and related to the age of onset of disorders. In general, heritability increases with age for WM and decreases for GM volumes (Wallace et al., 2006), whereas heritability increases for cortical thickness in regions within the frontal cortex, parietal, and temporal lobes (Lenroot et al., 2009). Knowledge of when certain brain structures are particularly sensitive to genetic or environmental influences during development could have important educational and/or therapeutic implications.
Male/Female Differences
Given that nearly all neuropsychiatric disorders have different prevalence, age of onset, and symptomatology between males and females, sex differences in typical developmental brain trajectories are highly relevant for studies of pathology. Robust sex differences in developmental trajectories are noted for nearly all structures, with GM volume peaks generally occurring 1–3 years earlier in females (Lenroot et al., 2007). To assess the relative contributions of sex chromosomes and hormones, our group is studying subjects with anomalous sex chromosome variations (e.g., XXY, XXX, XXXY, XYY) (Giedd et al., 2007), as well as subjects with anomalous hormone levels (e.g., congenital adrenal hyperplasia, familial male precocious puberty, Cushing syndrome) (Merke et al., 2003, 2005).
Specific Genes
As with any quantifiable behavioral or physical parameter, individuals can be categorized into groups based on genotype. Brain images of individuals in the different genotype groups can then be averaged and compared statistically. In adult populations, one of the most frequently studied genes has been apolipoprotein E (apoE), which modulates risk for Alzheimer’s disease. Carriers of the 4 allele of apoE have increased risk, whereas carriers of the 2 allele are possibly at decreased risk. To explore whether apoE alleles have distinct neuroanatomic signatures identifiable in childhood and adolescence, we examined 529 scans from 239 healthy subjects aged 4–20 years (Shaw et al., 2007c). Although there were no significant IQ-genotype interactions, there was a stepwise effect on cortical thickness in the entorhinal and right hippocampal regions, with the 4 group exhibiting the thinnest, the 3 homozygotes in the middle range, and the 2 group the thickest. These data suggest that pediatric assessments might one day be informative for adult-onset disorders.
Summary/Discussion
Maturational themes relevant to both health and illness include the importance of considering developmental trajectories and the high variability of measures across individuals. Despite high individual variation, several statistically robust patterns of average maturational changes are evident. Specifically, WM volumes increase and GM volumes follow an inverted U developmental trajectory with peaks latest in high association areas such as dorsolateral prefrontal cortex. These anatomic changes are consistent with electroencephalographic, functional MRI, postmortem, and neuropsychological studies indicating an increasing “connectivity” in the developing brain. “Connectivity” characterizes several neuroscience concepts. In anatomic studies, connectivity can mean a physical link between areas of the brain that share common developmental trajectories. In studies of brain function, connectivity describes the relationship between different parts of the brain that activate together during a task. In genetic studies, it refers to different regions that are influenced by the same genetic or environmental factors. All of these types of connectivity increase during adolescence. Characterizing developing neural circuitry and the changing relationships among disparate brain components is one of the most active areas of neuroimaging research as detailed by Power et al. (2010) (this issue of Neuron).
Although other higher association areas also mature relatively late, the developmental course of the dorsolateral prefrontal cortex has most prominently entered discourse affecting the social, legislative, judicial, parenting, and educational realms because of its involvement in judgment, decision making, and impulse control. It is also consistent with a growing body of literature indicating a changing balance between earlier-maturing limbic system networks (which are the seat of emotion, and later-maturing frontal lobe networks) and later-maturing frontal systems (Casey et al., 2010a [this issue of Neuron]). The frontal/limbic relationship is highly dynamic. Appreciating the interplay between limbic and cognitive systems is imperative for understanding decision making during adolescence.
Psychological tests are usually conducted under conditions of “cold cognition”—hypothetical, low-emotion situations. However, real-world decision making often occurs under conditions of “hot cognition”—high arousal, with peer pressure and real consequences. Neuroimaging investigations continue to discern the different biological circuitry involved in hot and cold cognition and are beginning to map how the parts of the brain involved in decision making mature. For instance, adolescents show exaggerated nucleus accumbens activation to reward compared to children but not a difference in orbital frontal activation (Galvan et al., 2006). Prolonged maturation of the PFC has also been shown to be related to age-related improvement in memory for details of experiences (in contrast to earlier maturing medial temporal lobe structures subserving nonexperiential memories) (Ofen et al., 2007).
The “journey as well as the destination” tenet highlights the fundamentally dynamic nature of brain and cognitive development in children. Adolescence is a particularly critical stage of neural development, and the relationship between typical maturational changes and the onset of psychopathology in this age group is an area of active investigation. The onset of several classes of psychiatric illness in the teen years (e.g., anxiety and mood disorders, psychosis, eating disorders, and substance abuse) (Kessler et al., 2005) may be related to the many brain changes occurring during this time (Paus et al., 2008). More broadly, understanding the mechanisms and influences on structural and functional brain development across childhood may help us to harness the brain’s developmental plasticity to help guide interventions for clinical disorders and for elucidating the path to promote optimal healthy development.
Supplementary Material
Footnotes
Supplemental Information includes methodologic considerations and can be found with this article online at doi:10.1016/j.neuron.2010.08.040.
References
- Bassett AS, Costain G, Alan Fung WL, Russell KJ, Pierce L, Kapadia R, Carter RF, Chow EW, Forsythe PJ. Clinically detectable copy number variations in a Canadian catchment population of schizophrenia. J Psychiatr Res. 2010 doi: 10.1016/j.jpsychires.2010.06.013. in press. Published online July 18, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berquin PC, Giedd JN, Jacobsen LK, Hamburger SD, Krain AL, Rapoport JL, Castellanos FX. Cerebellum in attention-deficit hyperactivity disorder: a morphometric MRI study. Neurology. 1998;50:1087–1093. doi: 10.1212/wnl.50.4.1087. [DOI] [PubMed] [Google Scholar]
- Casey BJ, Duhoux S, Cohen MM. Adolescence: What do transmission, transition, and translation have to do with it? Neuron. 2010a;67:749–760. doi: 10.1016/j.neuron.2010.08.033. this issue. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castellanos FX, Giedd JN. Quantitative morphology of the caudate nucleus in ADHD. Biol Psychiatry. 1994;35:725. doi: 10.1176/ajp.151.12.1791. [DOI] [PubMed] [Google Scholar]
- Castellanos FX, Lee PP, Sharp W, Jeffries NO, Greenstein DK, Clasen LS, Blumenthal JD, James RS, Ebens CL, Walter JM, et al. Developmental trajectories of brain volume abnormalities in children and adolescents with attention-deficit/hyperactivity disorder. JAMA. 2002;288:1740–1748. doi: 10.1001/jama.288.14.1740. [DOI] [PubMed] [Google Scholar]
- Caviness VSJ, Jr, Kennedy DN, Richelme C, Rademacher J, Filipek PA. The human brain age 7–11 years: a volumetric analysis based on magnetic resonance images. Cereb Cortex. 1996;6:726–736. doi: 10.1093/cercor/6.5.726. [DOI] [PubMed] [Google Scholar]
- Courchesne E, Pierce K, Schumann CM, Redcay E, Buckwalter JA, Kennedy DP, Morgan J. Mapping early brain development in autism. Neuron. 2007;56:399–413. doi: 10.1016/j.neuron.2007.10.016. [DOI] [PubMed] [Google Scholar]
- Crespi B, Stead P, Elliot M. Evolution in health and medicine Sackler colloquium: Comparative genomics of autism and schizophrenia. Proc Natl Acad Sci USA. 2010;107(Suppl 1):1736–1741. doi: 10.1073/pnas.0906080106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darlington RB, Dunlop SA, Finlay BL. Neural development in metatherian and eutherian mammals: variation and constraint. J Comp Neurol. 1999;411:359–368. [PubMed] [Google Scholar]
- Fields RD, Stevens-Graham B. New insights into neuron-glia communication. Science. 2002;298:556–562. doi: 10.1126/science.298.5593.556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finlay BL, Darlington RB. Linked regularities in the development and evolution of mammalian brains. Science. 1995;268:1578–1584. doi: 10.1126/science.7777856. [DOI] [PubMed] [Google Scholar]
- Fishell G. Regionalization in the mammalian telencephalon. Curr Opin Neurobiol. 1997;7:62–69. doi: 10.1016/s0959-4388(97)80121-3. [DOI] [PubMed] [Google Scholar]
- Galvan A, Hare TA, Parra CE, Penn J, Voss H, Glover G, Casey BJ. Earlier development of the accumbens relative to orbitofrontal cortex might underlie risk-taking behavior in adolescents. J Neurosci. 2006;26:6885–6892. doi: 10.1523/JNEUROSCI.1062-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giedd JN, Castellanos FX, Casey BJ, Kozuch P, King AC, Hamburger SD, Rapoport JL. Quantitative morphology of the corpus callosum in attention deficit hyperactivity disorder. Am J Psychiatry. 1994;151:665–669. doi: 10.1176/ajp.151.5.665. [DOI] [PubMed] [Google Scholar]
- Giedd JN, Blumenthal J, Molloy E, Castellanos FX. Brain imaging of attention deficit/hyperactivity disorder. Ann N Y Acad Sci. 2001;931:33–49. doi: 10.1111/j.1749-6632.2001.tb05772.x. [DOI] [PubMed] [Google Scholar]
- Giedd JN, Clasen LS, Wallace GL, Lenroot RK, Lerch JP, Wells EM, Blumenthal JD, Nelson JE, Tossell JW, Stayer C, et al. XXY (Klinefelter syndrome): a pediatric quantitative brain magnetic resonance imaging case-control study. Pediatrics. 2007;119:e232–e240. doi: 10.1542/peds.2005-2969. [DOI] [PubMed] [Google Scholar]
- Giedd JN, Lenroot RK, Shaw P, Lalonde F, Celano M, White S, Tossell J, Addington A, Gogtay N. Trajectories of anatomic brain development as a phenotype. Novartis Found Symp. 2008;289:101–112. doi: 10.1002/9780470751251.ch9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gogtay N, Rapoport JL. Childhood-onset schizophrenia: insights from neuroimaging studies. J Am Acad Child Adolesc Psychiatry. 2008;47:1120–1124. doi: 10.1097/CHI.0b013e31817eed7a. [DOI] [PubMed] [Google Scholar]
- Gogtay N, Giedd JN, Lusk L, Hayashi KM, Greenstein D, Vaituzis AC, Nugent TF, 3rd, Herman DH, Clasen LS, Toga AW, et al. Dynamic mapping of human cortical development during childhood through early adulthood. Proc Natl Acad Sci USA. 2004a;101:8174–8179. doi: 10.1073/pnas.0402680101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gogtay N, Herman D, Ordonez A, Giedd J, Hayashi K, Greenstein D, Vaitiuzis C, Nugent TF, Classen L, Thompson P, Rapoport J. Dynamic mapping of cortical brain development in pediatric bipolar illness. Neuropsychopharmacology. 2004b;29:S82–S82. [Google Scholar]
- Gogtay N, Lu A, Leow AD, Klunder AD, Lee AD, Chavez A, Greenstein D, Giedd JN, Toga AW, Rapoport JL, Thompson PM. Three-dimensional brain growth abnormalities in childhood-onset schizophrenia visualized by using tensor-based morphometry. Proc Natl Acad Sci USA. 2008;105:15979–15984. doi: 10.1073/pnas.0806485105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gottesman II, Gould TD. The endophenotype concept in psychiatry: etymology and strategic intentions. Am J Psychiatry. 2003;160:636–645. doi: 10.1176/appi.ajp.160.4.636. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Lange N, Giedd JN, Castellanos FX, Vaituzis AC, Rapoport JL. Variability of human brain structure size: ages 4–20 years. Psychiatry Res. 1997;74:1–12. doi: 10.1016/s0925-4927(96)03054-5. [DOI] [PubMed] [Google Scholar]
- Lenroot RK, Gogtay N, Greenstein DK, Wells EM, Wallace GL, Clasen LS, Blumenthal JD, Lerch J, Zijdenbos AP, Evans AC, et al. Sexual dimorphism of brain developmental trajectories during childhood and adolescence. Neuroimage. 2007;36:1065–1073. doi: 10.1016/j.neuroimage.2007.03.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lenroot RK, Schmitt JE, Ordaz SJ, Wallace GL, Neale MC, Lerch JP, Kendler KS, Evans AC, Giedd JN. Differences in genetic and environmental influences on the human cerebral cortex associated with development during childhood and adolescence. Hum Brain Mapp. 2009;30:163–174. doi: 10.1002/hbm.20494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Logvinov SV, Plotnikov MB, Zhdankina AA, Smol’iakova VI, Ivanov IS, Kuchin AV, Chukicheva IV, Varakuta EIu. Morphological changes in retinal neurons in rats with streptozotocin diabetes and their correction by O-isobornylphenol derivative. Morfologiia. 2009;136:42–45. [PubMed] [Google Scholar]
- Mackie S, Shaw P, Lenroot R, Pierson R, Greenstein DK, Nugent TF, 3rd, Sharp WS, Giedd JN, Rapoport JL. Cerebellar development and clinical outcome in attention deficit hyperactivity disorder. Am J Psychiatry. 2007;164:647–655. doi: 10.1176/ajp.2007.164.4.647. [DOI] [PubMed] [Google Scholar]
- McClellan J, King MC. Genetic heterogeneity in human disease. Cell. 2010;141:210–217. doi: 10.1016/j.cell.2010.03.032. [DOI] [PubMed] [Google Scholar]
- Merke DP, Fields JD, Keil MF, Vaituzis AC, Chrousos GP, Giedd JN. Children with classic congenital adrenal hyperplasia have decreased amygdala volume: potential prenatal and postnatal hormonal effects. J Clin Endocrinol Metab. 2003;88:1760–1765. doi: 10.1210/jc.2002-021730. [DOI] [PubMed] [Google Scholar]
- Merke DP, Giedd JN, Keil MF, Mehlinger SL, Wiggs EA, Holzer S, Rawson E, Vaituzis AC, Stratakis CA, Chrousos GP. Children experience cognitive decline despite reversal of brain atrophy one year after resolution of Cushing syndrome. J Clin Endocrinol Metab. 2005;90:2531–2536. doi: 10.1210/jc.2004-2488. [DOI] [PubMed] [Google Scholar]
- Neale MC, Cardon LR North Atlantic Treaty Organization, Scientific Affairs Division. Methodology for Genetic Studies of Twins and Families. Dordrecht; Boston: Kluwer Academic Publishers; 1992. [Google Scholar]
- Ofen N, Kao YC, Sokol-Hessner P, Kim H, Whitfield-Gabrieli S, Gabrieli JD. Development of the declarative memory system in the human brain. Nat Neurosci. 2007;10:1198–1205. doi: 10.1038/nn1950. [DOI] [PubMed] [Google Scholar]
- Paus T, Zijdenbos A, Worsley K, Collins DL, Blumenthal J, Giedd JN, Rapoport JL, Evans AC. Structural maturation of neural pathways in children and adolescents: in vivo study. Science. 1999;283:1908–1911. doi: 10.1126/science.283.5409.1908. [DOI] [PubMed] [Google Scholar]
- Paus T, Keshavan M, Giedd JN. Why do many psychiatric disorders emerge during adolescence? Nat Rev Neurosci. 2008;9:947–957. doi: 10.1038/nrn2513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Power JD, Fair DA, Schlaggar BL, Petersen SE. The development of human functional brain networks. Neuron. 2010;67:735–748. doi: 10.1016/j.neuron.2010.08.017. this issue. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rakic P. A small step for the cell, a giant leap for mankind: a hypothesis of neocortical expansion during evolution. Trends Neurosci. 1995;18:383–388. doi: 10.1016/0166-2236(95)93934-p. [DOI] [PubMed] [Google Scholar]
- Rapoport JL, Addington AM, Frangou S, Psych MR. The neurodevelopmental model of schizophrenia: update 2005. Mol Psychiatry. 2005;10:434–449. doi: 10.1038/sj.mp.4001642. [DOI] [PubMed] [Google Scholar]
- Rapoport J, Chavez A, Greenstein D, Addington A, Gogtay N. Autism spectrum disorders and childhood-onset schizophrenia: clinical and biological contributions to a relation revisited. J Am Acad Child Adolesc Psychiatry. 2009;48:10–18. doi: 10.1097/CHI.0b013e31818b1c63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riva D, Giorgi C. The cerebellum contributes to higher functions during development: evidence from a series of children surgically treated for posterior fossa tumours. Brain. 2000;123:1051–1061. doi: 10.1093/brain/123.5.1051. [DOI] [PubMed] [Google Scholar]
- Schmahmann JD. Disorders of the cerebellum: ataxia, dysmetria of thought, and the cerebellar cognitive affective syndrome. J Neuropsychiatry Clin Neurosci. 2004;16:367–378. doi: 10.1176/jnp.16.3.367. [DOI] [PubMed] [Google Scholar]
- Schmitt JE, Wallace GL, Rosenthal MA, Molloy EA, Ordaz S, Lenroot R, Clasen LS, Blumenthal JD, Kendler KS, Neale MC, Giedd JN. A multivariate analysis of neuroanatomic relationships in a genetically informative pediatric sample. Neuroimage. 2007;35:70–82. doi: 10.1016/j.neuroimage.2006.04.232. [DOI] [PubMed] [Google Scholar]
- Selemon LD, Goldman-Rakic PS. The reduced neuropil hypothesis: A circuit based model of schizophrenia. Biol Psychiatry. 1999;45:17–25. doi: 10.1016/s0006-3223(98)00281-9. [DOI] [PubMed] [Google Scholar]
- Shaw P, Greenstein D, Lerch J, Clasen L, Lenroot R, Gogtay N, Evans A, Rapoport J, Giedd J. Intellectual ability and cortical development in children and adolescents. Nature. 2006a;440:676–679. doi: 10.1038/nature04513. [DOI] [PubMed] [Google Scholar]
- Shaw P, Lerch J, Greenstein D, Sharp W, Clasen L, Evans A, Giedd J, Castellanos FX, Rapoport J. Longitudinal mapping of cortical thickness and clinical outcome in children and adolescents with attention-deficit/hyperactivity disorder. Arch Gen Psychiatry. 2006b;63:540–549. doi: 10.1001/archpsyc.63.5.540. [DOI] [PubMed] [Google Scholar]
- Shaw P, Eckstrand K, Sharp W, Blumenthal J, Lerch JP, Greenstein D, Clasen L, Evans A, Giedd J, Rapoport JL. Attention-deficit/hyperactivity disorder is characterized by a delay in cortical maturation. Proc Natl Acad Sci USA. 2007a;104:19649–19654. doi: 10.1073/pnas.0707741104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw P, Gornick M, Lerch J, Addington A, Seal J, Greenstein D, Sharp W, Evans A, Giedd JN, Castellanos FX, Rapoport JL. Polymorphisms of the dopamine D4 receptor, clinical outcome, and cortical structure in attention-deficit/hyperactivity disorder. Arch Gen Psychiatry. 2007b;64:921–931. doi: 10.1001/archpsyc.64.8.921. [DOI] [PubMed] [Google Scholar]
- Shaw P, Lerch JP, Pruessner JC, Taylor KN, Rose AB, Greenstein D, Clasen L, Evans A, Rapoport JL, Giedd JN. Cortical morphology in children and adolescents with different apolipoprotein E gene polymorphisms: an observational study. Lancet Neurol. 2007c;6:494–500. doi: 10.1016/S1474-4422(07)70106-0. [DOI] [PubMed] [Google Scholar]
- Shaw P, Sharp WS, Morrison M, Eckstrand K, Greenstein DK, Clasen LS, Evans AC, Rapoport JL. Psychostimulant treatment and the developing cortex in attention deficit hyperactivity disorder. Am J Psychiatry. 2009;166:58–63. doi: 10.1176/appi.ajp.2008.08050781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobel LJ, Bansal R, Maia TV, Sanchez J, Mazzone L, Durkin K, Liu J, Hao X, Ivanov I, Miller A, et al. Basal ganglia surface morphology and the effects of stimulant medications in youth with attention deficit hyperactivity disorder. Am J Psychiatry. 2010;167:977–986. doi: 10.1176/appi.ajp.2010.09091259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sowell ER, Thompson PM, Tessner KD, Toga AW. Mapping continued brain growth and gray matter density reduction in dorsal frontal cortex: Inverse relationships during postadolescent brain maturation. J Neurosci. 2001;21:8819–8829. doi: 10.1523/JNEUROSCI.21-22-08819.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sowell ER, Thompson PM, Welcome SE, Henkenius AL, Toga AW, Peterson BS. Cortical abnormalities in children and adolescents with attention-deficit hyperactivity disorder. Lancet. 2003;362:1699–1707. doi: 10.1016/S0140-6736(03)14842-8. [DOI] [PubMed] [Google Scholar]
- Sowell ER, Thompson PM, Toga AW. Mapping changes in the human cortex throughout the span of life. Neuroscientist. 2004;10:372–392. doi: 10.1177/1073858404263960. [DOI] [PubMed] [Google Scholar]
- Thompson PM, Vidal C, Giedd JN, Gochman P, Blumenthal J, Nicolson R, Toga AW, Rapoport JL. Mapping adolescent brain change reveals dynamic wave of accelerated gray matter loss in very early-onset schizophrenia. Proc Natl Acad Sci USA. 2001;98:11650–11655. doi: 10.1073/pnas.201243998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tiemeier H, Lenroot RK, Greenstein DK, Tran L, Pierson R, Giedd JN. Cerebellum development during childhood and adolescence: a longitudinal morphometric MRI study. Neuroimage. 2010;49:63–70. doi: 10.1016/j.neuroimage.2009.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallace GL, Eric Schmitt J, Lenroot R, Viding E, Ordaz S, Rosenthal MA, Molloy EA, Clasen LS, Kendler KS, Neale MC, Giedd JN. A pediatric twin study of brain morphometry. J Child Psychol Psychiatry. 2006;47:987–993. doi: 10.1111/j.1469-7610.2006.01676.x. [DOI] [PubMed] [Google Scholar]
- Weinberger DR. Implications of normal brain development for the pathogenesis of schizophrenia. Arch Gen Psychiatry. 1987;44:660–669. doi: 10.1001/archpsyc.1987.01800190080012. [DOI] [PubMed] [Google Scholar]
- Weinberger DR, Berman KF, Suddath R, Torrey EF. Evidence of dysfunction of a prefrontal-limbic network in schizophrenia: a magnetic resonance imaging and regional cerebral blood flow study of discordant monozygotic twins. Am J Psychiatry. 1992;149:890–897. doi: 10.1176/ajp.149.7.890. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.