Abstract
Ever since the first demonstration that transplant tolerance can be induced in neonatal mice by injection of donor bone marrow cells shortly after birth,1 the establishment of tolerance for organ transplants has been a major goal in the field of transplantation immunology. Indeed, an understanding of tolerance has both theoretical and practical implications for transplantation: from a theoretical point of view, an understanding of tolerance is basic to the requirement for self-/nonself-discrimination in the immune system; from a practical point of view, the induction of tolerance could relieve patients from the need for long-term immunosuppressant medications, thereby avoiding the adverse effects and complications that are a major limitation to the success of clinical transplant at present.
Until recently, immunologic tolerance was thought to imply the specific absence of an immune response. However, it has now become clear that, at least in the field of transplantation, tolerance can also be brought about by a positive immunologic response of a regulatory nature.2 Thus, we currently define transplant tolerance operationally as “the specific absence of a destructive immune response to a transplanted tissue in the absence of immunosuppression.” The key elements of this definition are “specific,” meaning that the recipient must remain fully capable of responding to other antigens; “destructive immune response,” allowing downregulatory immune responses to still be included in the definition; and “absence of immunosuppression,” signifying total elimination of the need for immunosuppressive drugs, thus not to be confused with the recent concept of “prope tolerance” or “drug minimization.”3,4
MECHANISMS OF TOLERANCE
Mechanisms responsible for transplant tolerance can be divided into the 2 categories, those leading to “central tolerance” and those leading to “peripheral tolerance.” Intrathymic deletion of T cells as they mature in the thymus is generally thought to be the major mechanism of central tolerance. It involves “negative selection” of those developing T cells that have sufficiently high reactivity to self–major histocompatibility complex (MHC) antigens that they could cause autoimmunity if not deleted. The mechanism for this clonal deletion has been the subject of intense investigation for many years but is still not entirely clear.5 T cells with little or no affinity for self-MHC are also deleted, while the concomitant process of “positive selection” leads to survival of T cells with intermediate affinity for self-MHC-antigens. These latter cells then mature to form the T cells that eventually leave the thymus and serve as functional T cells in the periphery.
The most likely reason for the existence of clonal deletion is the avoidance of autoimmune reactivity, and the same process can also be harnessed for the induction of transplant tolerance. For this to occur, appropriate cells from an allogeneic donor (predominantly dendritic cells), likewise capable of causing clonal deletion, need to be coaxed into taking residence in the host thymus, where they can also delete maturing T cells, in this case, those reactive to the donor. The result is a specific loss of reactivity to self and to donor, while reactivities to all other antigens remain intact, ie, induction of transplant tolerance.
Despite this process of clonal deletion, some T cells that exit the thymus are still capable of reacting against self-antigens and thereby potentially causing autoimmune disease. It is undoubtedly for this reason that mechanisms of “peripheral tolerance” have also evolved. These mechanisms include anergy,6 peripheral deletion,7 and regulation.8 The last of these, regulation, is generally attributed to the presence of regulatory T cells, which can downregulate the activity of autoreactive T cells in the periphery. Again, in the field of transplantation, one can make use of this mechanism to downregulate the immune response to a particular donor, leading to transplant tolerance.
MIXED CHIMERISM
The method for inducing central tolerance to transplant antigens that has been studied most extensively in our laboratory has involved the establishment of mixed hematopoietic chimerism. As illustrated in Figure 1, the initial means by which mixed hematopoietic chimeras were constructed involve lethal irradiation of recipient mice and reconstitution of these mice with a mixture of T-cell–depleted host-plus-donor bone marrow.9 These animals reconstituted as mixed lymphohematopoietic chimeras, in which all lymphoid and hematopoietic elements remained a mixture of host and donor type for the rest of the lives of the animals. T cells had to be depleted from the host (ie, “A‱T”) or else the host T cells would reject the donor bone marrow. Donor T cells also had to be depleted (“B–T”) to eliminate their ability to cause graft-vs-host disease (GVHD) in the recipients. However, when both sets of mature T cells were depleted, the new T cells that subsequently developed from radiation-resistant stem cells were negatively selected for MHC antigens of both A and B, leading to tolerance. The process of negative selection by donor dendritic cells that is thought to lead to this tolerance is illustrated in Figure 2.
Figure 1.
The initial study of tolerance induction through mixed chimerism involved lethal irradiation of recipient mice A leading to recognition of self–major histocompatibility complex plus peptides (eg, A + X), followed by reconstitution with a mixture of T-cell–depleted bone marrow from strain A and the fully mismatched strain B.
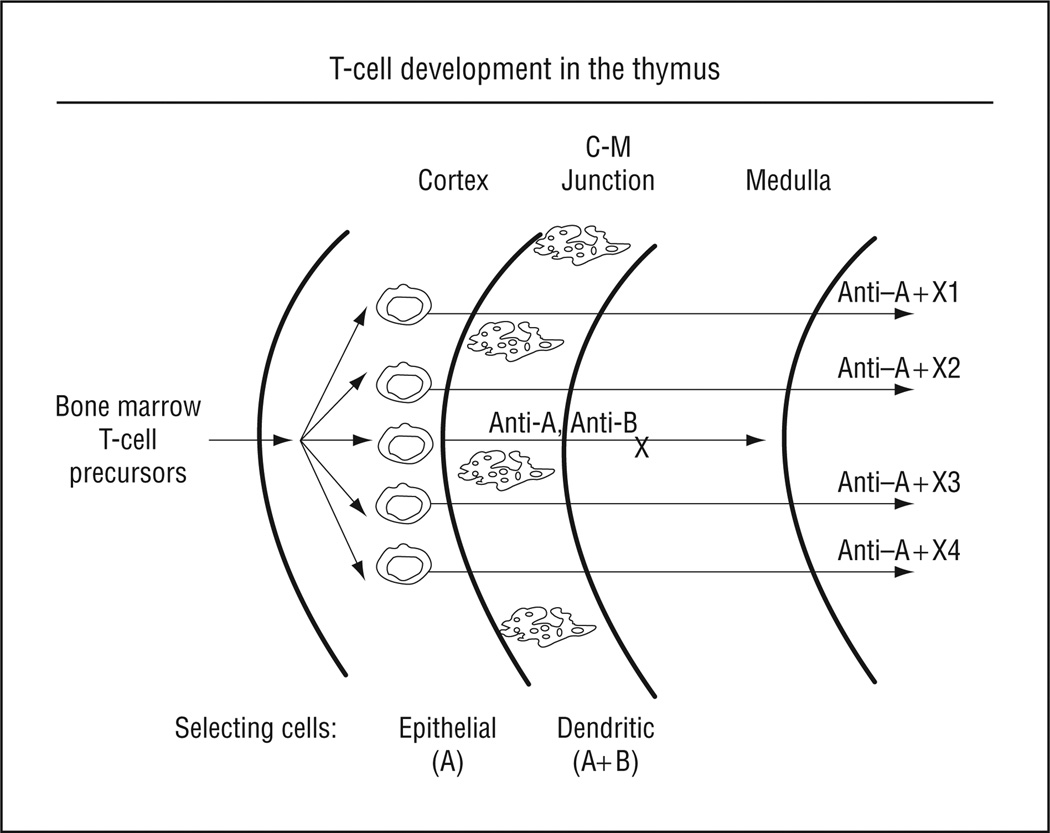
Figure 2.
T cells develop in the thymus from T-cell precursors, derived from the bone marrow, that enter the cortex of the thymus, where they expand and undergo the process of positive selection, induced by their interaction with thymic epithelial cells of host type A. As they then mature, they move toward the medulla, passing through the corticomedullary junction (C–M junction), where the process of negative selection occurs, largely through interaction with dendritic cells, which enter the thymus from the periphery. Since peripheral dendritic cells of mixed chimeras are of both host and donor types, negative selection occurs for cells reactive with both A and B.
Subsequent skin grafts of donor tail skin onto the lateral thorax of these tolerant animals were accepted long-term (Figure 3). However, as seen in Figure 3, these tail skin grafts were actually the most viable skin on these animals, since the rest of the skin showed the effects of the lethal irradiation used as part of the preparative regimen. While lethal irradiation might be acceptable for the induction of tolerance in patients with a malignant disease, for which irradiation might be part of the therapy, it would not be satisfactory for the preparative regimen of patients requiring only an organ transplant. Nevertheless, this initial study proved the principle that mixed chimerism could lead to long-term, donor-specific tolerance. Therefore, subsequent to these initial studies, much effort was devoted to developing nonmyeloablative methods for inducing mixed chimerism.
Figure 3.
Tail skin grafts from strain B placed on the lateral thorax of mixed chimeras many months later were accepted permanently.
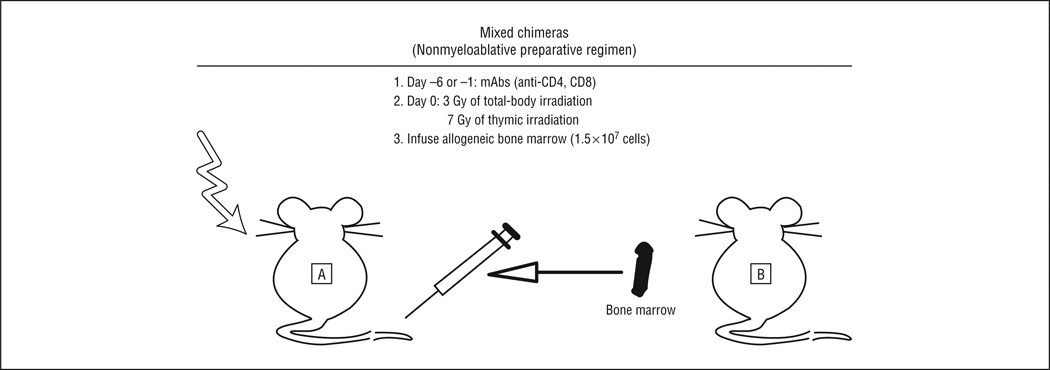
We subsequently demonstrated that similar mixed chimerism could be achieved without lethal irradiation by treating recipients with T-cell–depleting monoclonal antibodies and local thymic irradiation prior to administration of donor bone marrow, as illustrated in Figure4.10 These animals showed none of the adverse effects associated with lethal irradiation and recovered fully from the treatment with or without administration of donor bone marrow (Figure 5). This procedure was therefore thought to be suitable for potential application in patients, and extensive studies in mice,11 miniature swine,12 and monkeys13,14 all supported this hypothesis. There was one major difference between the results in mice and in large animals, however. In mice, mixed chimerism was long lasting, and recipients demonstrated a mixture of host and donor lymphohematopoietic cells for the remainder of their lives.9,10 In monkeys, on the other hand, mixed chimerism was transient, with evidence for donor lymphohematopoietic cells disappearing over the first 1 to 2 months posttransplant.13,14 In pigs, the results were intermediate between these 2 extremes, with some animals remaining mixed chimeras long-term and others losing their chimerism during the first few months post-transplant, depending to some extent on the preparative regimen used.12,15–17
Figure 4.
The nonmyeloablative approach to mixed chimerism used monoclonal antibodies (mAbs) to the mature CD4 and CD8 T-cell subsets rather than lethal irradiation to ablate mature T cells of both recipient and donor, allowing mixed lymphohematopoietic reconstitution with a much less dangerous preparative regimen. To convert grays to rads, multiply by 100.
Figure 5.
A mouse prepared by the nonmyeloablative regimen recovered completely from the treatment, showing premature graying only where it had received a boost of irradiation to the thymus.
Importantly, in these large-animal studies, if the renal transplants were performed while the animals were still mixed chimeras, tolerance of the allografts persisted long-term, despite loss of chimerism.18 Mechanistic studies have suggested that the tolerant state is maintained in this case by peripheral mechanisms, most likely involving regulatory cells, and dependent on the presence of the renal allograft (T. Kawai, MD, A. B. Cosimi, MD, and D.H.S., unpublished data, 2011). In any case, given the long-term tolerance achieved, the relatively mild preparative regimen, and the absence of GVHD, we decided it was appropriate to attempt tolerance induction through mixed chimerism in clinical renal transplant.
INDUCTION OF TOLERANCE IN PATIENTS RECEIVING RENAL ALLOGRAFTS
The Immune Tolerance Network (ITN), sponsored by the National Institute of Allergy and Infectious Diseases, was established in 1999, with the goal of bringing immunologic tolerance to the clinic in the fields of allergy, autoimmunity, and transplantation. Funding has been provided by this organization to carry out 3 trials for induction of tolerance in patients requiring kidney transplants. The first trial involved an attempt to carry out a mixed chimerism procedure in patients with end-stage multiple myeloma, a frequent complication of which is renal failure. These patients were generally unable to receive a kidney transplant because of their refractory malignant disease and unable to be treated further for myeloma because of their renal failure. Since a mixed chimerism protocol for treatment of lymphomas has had promising results,19 it was reasoned that patients with myeloma in renal failure might derive benefit from this procedure, both for treatment of their renal failure and for treatment of their myeloma. The trial was opened to patients with refractory myeloma and end-stage renal disease with HLA antigen–identical siblings who were willing to provide both a kidney and bone marrow. The trial was highly successful, with the first 6 patients all becoming tolerant to their renal transplants, although, as expected, not all were cured of their myeloma.20 The first patient enrolled in the protocol is now more than 10 years past her transplant, has normal renal function, and no clinical evidence of myeloma.
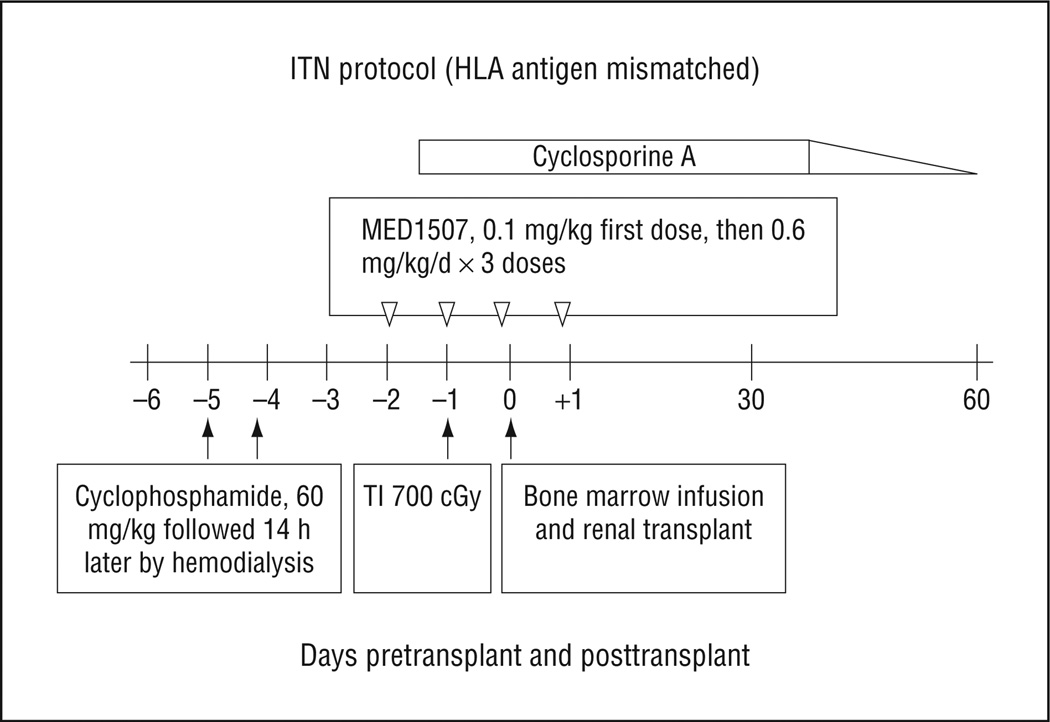
These promising results led to a second ITN-sponsored trial, directed toward induction of tolerance in patients who had neither an HLA antigen–identical sibling nor a malignant disease. The preparative regimen chosen for this study was one of those studied previously for the treatment of lymphoma by mixed bone marrow transplant.19 Although not effective for the treatment of lymphoma because it led only to transient mixed chimerism, this particular regimen had not been associated with the occurrence of GVHD. Graft-vs-host disease had sometimes occurred with other treatment regimens and, as mentioned earlier, would be unacceptable for transplant recipients without a malignancy. However, since transient mixed chimerism had led to tolerance without GVHD in our monkey experiments, this loss of chimerism was not of great concern for a tolerance-induction trial. This second trial was started in 2002 and the results were published in 2008 in the New England Journal of Medicine.21 The article reported that tolerance was induced in 4 of the first 5 patients enrolled in the study, confirming the clinical utility of this approach.
The first patient in the trial had developed renal failure due to Alport syndrome as a child and had already received a previous conventional renal transplant from her father 8 years earlier. Her particular reason for volunteering to be the first patient in the trial was that she had had severe complications related to the immunosuppressive drugs she had taken for that previous transplant and had rejected that transplant in part because of her intolerance of those drugs. She has not taken immunosuppression drugs for more than 8 years now following her transplant and enjoys normal renal function as well as a life free of the adverse effects and complications of immunosuppressive drugs. In her own words, “I now feel like a normal person, and I have never felt normal since I was diagnosed when I was 12 years old.”
The most significant difference between the preparative regimen used in this trial and those used previously in cynomolgus monkeys18 and in patients with myeloma20 was the use of an anti-CD2 monoclonal antibody to deplete T cells rather than antithymocyte globulin (Figure 6). The third patient treated developed severe, acute, antibody-mediated rejection of the kidney transplant, despite the absence of evidence for development of T-cell immunity to the donor. Since de novo anti–HLA antigen antibodies are generally only produced as part of a T cell–dependent immune response, while memory B cells do not require T-cell help for further activation, we reasoned that a potential cause for this rejection may have been the presence of sensitized B cells in this patient, despite a negative cross-match at the time of transplant. We therefore added an anti–B cell monoclonal antibody (rituximab, anti-CD20) to the preparative regimen for the remaining 2 patients in this trial, and both proceeded to accept their renal allografts and be successfully weaned from all immunosuppression drugs.
Figure 6.
The nonmyeloablative preparative regimen used clinically was similar to that used for mice and monkeys, except for the use of cytoxan rather than low-dose whole-body irradiation for myelodepletion prior to bone marrow administration. For HLA antigen–mismatched patients, T-cell depletion was effected with an anti-CD2 monoclonal antibody. ITN indicates Immune Tolerance Network; T1, thymic irradiation. To convert centigray to rad, multiply by 100.
A third trial, also sponsored by the ITN, began in 2009, with intent to treat 15 renal allograft recipients by a protocol very similar to that used for the final 2 patients in the second trial, but with 2 additional doses of rituximab posttransplant. The first 5 transplants were to be carried out at Massachusetts General Hospital and followed up by a review of the results by the data and safety monitoring board of the National Institute of Allergy and Infectious Diseases and then the remaining 10 patients would receive transplants carried out at 3 different sites. The first 5 patients have now been entered in this trial and the decision to continue awaits regulatory approval.
FUTURE DIRECTIONS
Until now, all of these clinical renal allograft tolerance trials have required the organs to be derived from living donors, because the preparative regimen of the recipients begins several days prior to the transplant, a condition that cannot be met for deceased donation. Current laboratory efforts are being directed toward protocols that will allow the preparative regimen and the bone marrow administration to be carried out after, rather than before, the kidney transplant.22 If this can be accomplished, the protocol would not only permit use of deceased donors of kidneys but would also potentially open up the procedure to transplant of other organs for which living donation is either precluded (eg, heart transplants) or much more problematic (eg, liver and lung transplants).
Acknowledgments
Funding/Support: This work was supported in part by grant N01 AI15416 from the National Institutes of Health.
Footnotes
Financial Disclosure: None reported.
Previous Presentation: This paper was presented at the 91st Annual Meeting of the New England Surgical Society; October 31, 2010; Saratoga Springs, New York; and is published after peer review and revision.
Additional Contributions: John Hanekamp, MD, PhD, and Christine Huang, PhD, critically reviewed the manuscript and Rebecca Wark provided expert secretarial assistance.
REFERENCES
- 1.Billingham RE, Brent L, Medawar PB. Actively acquired tolerance of foreign cells. Nature. 1953;172(4379):603–606. doi: 10.1038/172603a0. [DOI] [PubMed] [Google Scholar]
- 2.Wood KJ, Sakaguchi S. Regulatory T cells in transplantation tolerance. Nat Rev Immunol. 2003;3(3):199–210. doi: 10.1038/nri1027. [DOI] [PubMed] [Google Scholar]
- 3.Calne R. “Prope” tolerance: induction, lymphocyte depletion with minimal maintenance. Transplantation. 2005;80(1):6–7. doi: 10.1097/01.tp.0000164351.72220.1a. [DOI] [PubMed] [Google Scholar]
- 4.Golshayan D, Pascual M. Tolerance-inducing immunosuppressive strategies in clinical transplantation: an overview. Drugs. 2008;68(15):2113–2130. doi: 10.2165/00003495-200868150-00004. [DOI] [PubMed] [Google Scholar]
- 5.Kappler JW, Roehm N, Marrack P. T cell tolerance by clonal elimination in the thymus. Cell. 1987;49(2):273–280. doi: 10.1016/0092-8674(87)90568-x. [DOI] [PubMed] [Google Scholar]
- 6.Rocha B, Grandien A, Freitas AA. Anergy and exhaustion are independent mechanisms of peripheral T cell tolerance. J Exp Med. 1995;181(3):993–1003. doi: 10.1084/jem.181.3.993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wekerle T, Kurtz J, Sayegh M, et al. Peripheral deletion after bone marrow transplantation with costimulatory blockade has features of both activation-induced cell death and passive cell death. J Immunol. 2001;166(4):2311–2316. doi: 10.4049/jimmunol.166.4.2311. [DOI] [PubMed] [Google Scholar]
- 8.Akl A, Luo S, Wood KJ. Induction of transplantation tolerance-the potential of regulatory T cells. Transpl Immunol. 2005;14(3–4):225–230. doi: 10.1016/j.trim.2005.03.011. [DOI] [PubMed] [Google Scholar]
- 9.Ildstad ST, Sachs DH. Reconstitution with syngeneic plus allogeneic or xenogeneic bone marrow leads to specific acceptance of allografts or xenografts. Nature. 1984;307(5947):168–170. doi: 10.1038/307168a0. [DOI] [PubMed] [Google Scholar]
- 10.Sharabi Y, Sachs DH. Mixed chimerism and permanent specific transplantation tolerance induced by a nonlethal preparative regimen. J Exp Med. 1989;169(2):493–502. doi: 10.1084/jem.169.2.493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sykes M. Mechanisms of tolerance induced via mixed chimerism. Front Biosci. 2007;12:2922–2934. doi: 10.2741/2282. [DOI] [PubMed] [Google Scholar]
- 12.Huang CA, Fuchimoto Y, Scheier-Dolberg R, Murphy MC, Neville DMJ, Jr, Sachs DH. Stable mixed chimerism and tolerance using a nonmyeloablative preparative regimen in a large-animal model. J Clin Invest. 2000;105(2):173–181. doi: 10.1172/JCI7913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kawai T, Hoshino T, Fujioka S, et al. Mixed chimerism and immune tolerance induction by low-stress pretreatment before kidney transplantation in monkeys [in Japanese] Nihon Rinsho Meneki Gakkai Kaishi. 1995;18(6):670–674. [PubMed] [Google Scholar]
- 14.Kawai T, Sogawa H, Boskovic S, et al. CD154 blockade for induction of mixed chimerism and prolonged renal allograft survival in nonhuman primates. Am J Transplant. 2004;4(9):1391–1398. doi: 10.1111/j.1600-6143.2004.00523.x. [DOI] [PubMed] [Google Scholar]
- 15.Fuchimoto Y, Yamada K, Shimizu A, et al. Relationship between chimerism and tolerance in a kidney transplantation model. J Immunol. 1999;162(10):5704–5711. [PubMed] [Google Scholar]
- 16.Fuchimoto Y, Huang CA, Yamada K, et al. Mixed chimerism and tolerance without whole body irradiation in a large animal model. J Clin Invest. 2000;105(12):1779–1789. doi: 10.1172/JCI8721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Horner BM, Cina RA, Wikiel KJ, et al. Predictors of organ allograft tolerance following hematopoietic cell transplantation. Am J Transplant. 2006;6(12):2894–2902. doi: 10.1111/j.1600-6143.2006.01563.x. [DOI] [PubMed] [Google Scholar]
- 18.Kawai T, Cosimi AB, Colvin RB, et al. Mixed allogeneic chimerism and renal allograft tolerance in cynomolgus monkeys. Transplantation. 1995;59(2):256–262. [PubMed] [Google Scholar]
- 19.Sykes M, Preffer F, McAfee S, et al. Mixed lymphohaemopoietic chimerism and graft-versus-lymphoma effects after non-myeloablative therapy and HLA-mismatched bone-marrow transplantation. Lancet. 1999;353(9166):1755–1759. doi: 10.1016/S0140-6736(98)11135-2. [DOI] [PubMed] [Google Scholar]
- 20.Fudaba Y, Spitzer TR, Shaffer J, et al. Myeloma responses and tolerance following combined kidney and nonmyeloablative marrow transplantation: in vivo and in vitro analyses. Am J Transplant. 2006;6(9):2121–2133. doi: 10.1111/j.1600-6143.2006.01434.x. [DOI] [PubMed] [Google Scholar]
- 21.Kawai T, Cosimi AB, Spitzer TR, et al. HLA-mismatched renal transplantation without maintenance immunosuppression. N Engl J Med. 2008;358(4):353–361. doi: 10.1056/NEJMoa071074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Koyama I, Nadazdin O, Boskovic S, et al. Depletion of CD8 memory T cells for induction of tolerance of a previously transplanted kidney allograft. Am J Transplant. 2007;7(5):1055–1061. doi: 10.1111/j.1600-6143.2006.01703.x. [DOI] [PMC free article] [PubMed] [Google Scholar]