Abstract
Perforation of the ureter is a rare condition that causes a series of problems including retroperitoneal urinoma, urosepsis, abscess formation, infection, and subsequent renal impairment. There are causative factors that induce ureteric rupture, including malignancy, urinary calculi, idiopathic retroperitoneal fibrosis, recent iatrogenic manipulation, external trauma, degenerative kidney conditions, urography with external compression, and spontaneous causes. We report a rare case of ureteric rupture caused by urinary retention. The patient was treated with temporary percutaneous drainage and antibiotics. The present case illustrates that urinary retention can induce not only bladder rupture, but also ureteric rupture. It is thus of paramount importance to effectively manage patients with voiding problems.
Keywords: Neurogenic bladder, neurogenic; Rupture; Ureter; Urinary retention
Ureteric rupture is a potentially dangerous event, the diagnosis of which is often delayed because of its rarity. We report a patient with neurogenic bladder who experienced urinary retention and subsequent ureteric rupture.
CASE REPORT
A 75-year-old woman was admitted to the emergency department with acute right abdominal pain of 2-hour duration. Her medical history included a hysterectomy 30 years ago. From several decades ago, she had almost always voided with abdominal strain. Also, she suffered from tenesmus and weak stream. On examination, she was oriented and cooperative. Her vital signs were as follows: blood pressure, 150/75 mmHg; pulse, 84 beats per minute and regular; respirations, 20 per minute; and body temperature, 36.0℃. Clinical examination revealed diffuse pain in the right abdomen with tenderness. However, costovertebral angle (CVA) tenderness was not prominent. Bowel sounds were increased.
Urinalysis showed 2 to 4 red cells and 0 to 1 white cells per field under high-power magnification. Complete blood cell count results were as follows: 8,500/mm3, with 44.5% neutrophils. Serum chemical analysis showed a urea level of 26 mg/dl, a creatinine level of 1.5 mg/dl, and a C-reactive protein (CRP) level of 0.99 mg/dl. Other values were within the normal limits.
After analgesic injection, her pain subsided. With a presumptive diagnosis of acute gastroenteritis, she was discharged with medication.
The following day, the patient was admitted to the gastrointestinal department with persistent right abdominal pain. An abdominal computed tomographic (CT) scan was performed, which showed a dilated urinary bladder, hydronephroureterosis, and perinephric fluid collection. The patient was referred to our urologists, who recommended insertion of an indwelling Foley catheter. About 2 L of urine was drained shortly after catheter indwelling. Because there was no delayed phase on CT, we performed a non-enhanced CT scan immediately. It showed extravasation of radiocontrast from the right upper ureter at the L3 to 4 transverse process level and improved hydronephroureterosis (Fig. 1).
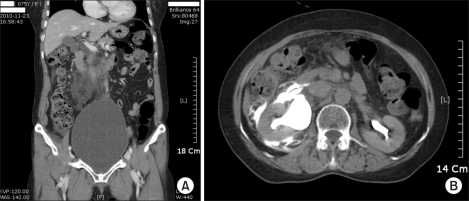
FIG. 1.
(A) CT image showing a dilated bladder, suggestive of urinary retention. (B) CT image showing extravasation of radiocontrast from the ruptured ureter. Contrast medium leakage into the perirenal space is shown. CT, computed tomographic.
A 8.5 F pigtail percutaneous nephrostomy catheter was inserted into the renal pelvis. After 7 days, antegrade pyelography (AGP) performed through the nephrostomy catheter showed no extravasation of radiocontrast from the ureter (Fig. 2). A double-J catheter (6 F, 24 cm) was placed in the right ureter. The percutaneous nephrostomy catheter and Foley catheter were removed. The next day, she was discharged without complications.
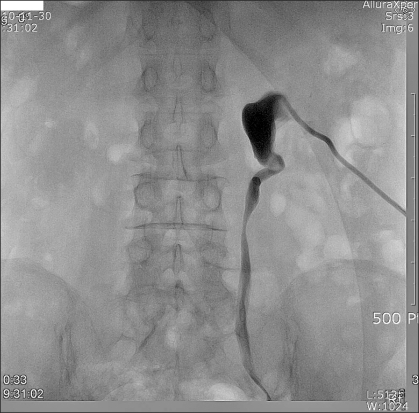
FIG. 2.
Antegrade pyelography showing no leakage of contrast medium after 7 days.
After 2 weeks, the Double-J catheter was removed and we subsequently performed a video-urodynamic study. A total of 500 ml of normal saline was filled in the bladder. The patient then tried to void with abdominal straining, but could not. Maximal detrusor pressure did not exceed 10 cmH2O. In other words, the patient showed detrusor underactivity and no vesicoureteric reflux (VUR). A follow-up CT scan was performed 2 months later. It showed resorption of urinoma in the right peri-renal space and there was neither malignancy nor obstructing lesions. She was managed with alpha-blockers and clean intermittent catheterization.
DISCUSSION
Ureteric rupture is rare and can be traumatic or, less commonly, nontraumatic in nature [1]. The most common cause of traumatic ureteric rupture is iatrogenic trauma, followed by penetrating trauma, and occasionally, blunt abdominal trauma. Nontraumatic ureteric rupture includes transmitted back pressure from a downstream obstruction caused by ureteric stones, surgical ligature, or an abdominal or pelvic mass [2].
The most common symptoms are sudden, severe, persistent lower abdominal pain with severe peritoneal irritation [3]. Another report described massive urinary leakage into the peritoneal cavity, resulting in abdominal compartment syndrome, respiratory distress, and anuria [4].
Excretory urography has been described as the most sensitive means of diagnosing ureteric rupture [3]. Recently, CT scanning is considered the optimal evaluation for diagnosing ureteric rupture, because of the expected poor resolution of intravenous urography in an unprepared patient. Also, one can obtain more accurate information about the location and the size of the urinoma on a CT scan, and the progression of its characteristics can be readily assessed [5]. In this case, we diagnosed ureteric rupture easily by use of a CT scan. In delayed-phase images, extravasation of radiocontrast from the perforated ureter was seen.
Many authors have resorted to open surgery earlier for complete management of spontaneous rupture and urinoma [3,6,7]. The incidence of late complications, such as ureteric stricture, ureteropelvic stenosis, or peri-ureteric fibrosis remains unknown. Davies et al. [8] believe that in urinary extravasation, treatment should be supportive initially (i.e., careful observation and analgesics). Persistent obstruction and severe pain, infection, and failing renal function necessitate more active treatment [9].
Although nontraumatic perforation of the ureter is relatively benign, it may predispose the patient to perinephric abscess. Stravodimos et al. [5] reported successful treatment of ureteric rupture by the insertion of a Double-J ureteric stent under fluoroscopy. They achieved unobstructed urinary outflow, healing of the perforation, and stabilization and gradual absorption of the urinoma. In the modern era, open surgical intervention is rarely indicated, because minimally invasive techniques such as percutaneous drainage can be used to manage complications [5].
In our case, there was no evidence of factors that cause ureteric rupture other than urinary retention. Urine cytology was negative for malignancy. Video-urodynamic study showed detrusor underactivity without VUR. The follow-up CT scan showed neither malignancy nor an obstructing lesion. Urinary retention may inhibit urinary flow to the bladder and result in high intraureteric pressure. As intraureteric pressure rises, the ureteric wall fails to withstand the pressure and becomes ruptured.
Severe urinary retention may cause ureteric rupture in rare cases. Urologists should be aware of the possibility of ureteric rupture in the differential diagnosis of an acute abdomen, particularly in patients with urinary retention. Management of these patients should include minimally invasive techniques accompanied by active management of urinary retention.
Footnotes
The authors have nothing to disclose.
References
- 1.Kaplan LM, Farrer JH, Lupu AN. Spontaneous rupture of ureter. Urology. 1987;29:313–316. doi: 10.1016/0090-4295(87)90078-1. [DOI] [PubMed] [Google Scholar]
- 2.Titton RL, Gervais DA, Hahn PF, Harisinghani MG, Arellano RS, Mueller PR. Urine leaks and urinomas: diagnosis and imaging-guided intervention. Radiographics. 2003;23:1133–1147. doi: 10.1148/rg.235035029. [DOI] [PubMed] [Google Scholar]
- 3.Diamond DA, Marshall FF. The diagnosis and management of spontaneous rupture of the ureter. J Urol. 1982;128:808–810. doi: 10.1016/s0022-5347(17)53198-5. [DOI] [PubMed] [Google Scholar]
- 4.Katz R, Meretyk S, Gimmon Z. Abdominal compartment syndrome due to delayed identification of a ureteric perforation following abdomino-perineal resection for rectal carcinoma. Int J Urol. 1997;4:615–617. doi: 10.1111/j.1442-2042.1997.tb00320.x. [DOI] [PubMed] [Google Scholar]
- 5.Stravodimos K, Adamakis I, Koutalellis G, Koritsiadis G, Grigoriou I, Screpetis K, et al. Spontaneous perforation of the ureter: clinical presentation and endourologic management. J Endourol. 2008;22:479–484. doi: 10.1089/end.2007.0196. [DOI] [PubMed] [Google Scholar]
- 6.Chapman JP, Gonzales J, Diokno AC. Significance of urinary extravasation during renal colic. Urology. 1987;30:541–545. doi: 10.1016/0090-4295(87)90432-8. [DOI] [PubMed] [Google Scholar]
- 7.El-Boghdadly SA. Spontaneous rupture of the ureter proximal to ureteric stone. J R Soc Med. 1985;78:255–257. doi: 10.1177/014107688507800316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Davies P, Bates CP, Price HM. Chronic peripelvic extravasation treated conservatively. Br J Urol. 1981;53:412–415. doi: 10.1111/j.1464-410x.1981.tb03219.x. [DOI] [PubMed] [Google Scholar]
- 9.Kettlewell M, Walker M, Dudley N, De Souza B. Spontaneous extravasation of urine secondary to ureteric obstruction. Br J Urol. 1973;45:8–14. [PubMed] [Google Scholar]