Abstract
AIMS
To identify correlates of active syphilis infection among female sex workers (FSWs) in Tijuana and Ciudad Juarez.
DESIGN
Cross-sectional analyses of baseline interview data. Correlates of active syphilis (antibody titers >1:8) were identified by logistic regression.
SETTING
Tijuana and Ciudad Juarez, two Mexican cities on the U.S. border that are situated on major drug trafficking routes and where prostitution is quasi-legal.
PARTICIPANTS
914 FSWs aged ≥18 years without known HIV infection who had recent unprotected sex with clients.
MEASUREMENTS
Baseline interviews and testing for syphilis antibody using Treponema pallidum particle agglutination (TPPA) and rapid plasma reagin (RPR) tests.
FINDINGS
Median age and duration in sex work were 32 and 4 years, respectively. Overall, 18.0% had ever injected drugs, 14.2% often or always used illegal drugs before or during sex in the past month, 37.7% had clients who injected drugs in the last 6 months, and 68.6% reported having clients from the U.S. Prevalence of HIV and active syphilis were 5.9% and 10.3%, respectively. Factors independently associated with active syphilis included injecting drugs (AOR: 2.39; 95% CI: 1.40, 4.80), using illegal drugs before or during sex (AOR: 2.06; 95% CI: 1.16, 3.65), and having any U.S. clients (AOR: 2.85; 95% CI: 1.43, 5.70).
CONCLUSIONS
Among female sex workers in Tijuana and Ciudad Juarez, drug-using behaviors were more closely associated with active syphilis than were sexual behaviors, suggesting the possibility of parenteral transmission of T. pallidum. Syphilis eradication programs should consider distributing sterile syringes to drug injectors and assisting FSWs with safer-sex negotiation in the context of drug use.
Keywords: female sex worker, prostitution, syphilis, injection drug use, needle sharing, Mexico, women
INTRODUCTION
Most large cities in Mexico have developed zonas rojas (red-light districts) where sex work is permitted or regulated. Two such cities situated on Mexico’s northern border are Tijuana, Baja California, abutting San Diego, California and Ciudad Juarez, Chihuahua, abutting El Paso, Texas. In Tijuana, nearly 5,000 female sex workers (FSWs) are registered with the Municipal Health Service, while thousands of others are thought to work without permits. Most of Tijuana’s FSWs work in the Zona Roja which overlaps the Zona Norte, a neighborhood known for heavy drug use. In Ciudad Juarez, there are approximately 4,000 FSWs, but this city does not regulate sex work [1]. In both cities, FSWs work in cantinas, bars, hotels, nightclubs, massage parlors and street corners, and most of their clients are men from the U.S. or Mexico [1].
Drugs are widely available in Tijuana and Ciudad Juarez given that both cities lie on major trafficking routes [2]. The highest rate of illicit drug consumption in Mexico is in Tijuana, where there are an estimated 21,000 drug users, of whom approximately 6,000 are injecting drug users (IDUs) [3]. Ciudad Juarez is home to 3,000–3,500 heavy heroin users and an estimated 6,000 IDUs [3]. Among FSWs in Tijuana and Ciudad Juarez, stimulants such as methamphetamine and cocaine are often used to cope with mood or to stay awake [4, 5].
Literature on HIV and sexually transmitted infections (STIs) in the Mexico-U.S. border region suggests a heavy burden among drug users, especially IDUs. In an early study of hepatitis B among women in Tijuana (N=714), FSWs who used drugs had higher prevalence of syphilis compared to female controls [6]. In Tijuana and Ciudad Juarez, FSWs who injected drugs had consistently higher prevalence of HIV and STIs compared to other FSWs: HIV (16% vs 4%), syphilis (49% vs 22%), gonorrhea (15% vs 4%), and Chlamydia (24% vs 10%) [5].
Syphilis is common among women who use drugs, and thus drug use may be a marker for high-risk sexual behaviors. In a six-year prospective study of 790 IDUs in The Bronx, NY, independent risk factors of early syphilis included younger age, multiple sex partners, incident HIV infection, and being paid for sex [7]. Among incarcerated women in Connecticut who had syphilis, 41% reported cocaine use and 19% reported prostitution [8].
On the other hand, since syphilis can be transmitted through blood transfusion [9–11], it could hypothetically be transmitted through needle sharing. In a cross-sectional study among male and female IDUs in three Russian cities, lifetime syphilis prevalence was associated with daily injection, having an IDU sexual partner, and history of STIs [12]. Among women in the cities of Moscow and Barnaul, sex work was independently associated with testing positive for syphilis antibodies, and in Barnaul, daily injection was also associated with lifetime syphilis prevalence [12]. Although these results were not definitive, the authors suggested a possible causal relationship between injection drug use and syphilis infection.
This study aimed to determine if drug-using behaviors were independently associated with active syphilis infection among FSWs in Tijuana and Ciudad Juarez. Given the intertwined nature of sex work and injection drug use, we hypothesized that FSWs with syphilis titers consistent with active infection would have higher rates of injection drug use and needle sharing, after controlling for high-risk sexual behaviors. If this hypothesis were supported, syphilis eradication programs should include a harm reduction component for drug injectors. Additionally, since high syphilis titers are independently associated with HIV infection among FSWs [13] and IDUs in these cities [14] and elsewhere (e.g., the U.S., Russia, India, Nepal, China) [15–19], interventions to reduce syphilis transmission could also favorably impact HIV prevention efforts [20].
METHODS
Study Population
From 2004 through 2006, FSWs in Tijuana (N=474) and Ciudad Juarez (N=450) were recruited into a behavioral intervention study as described previously [21]. Recruitment was conducted at municipal clinics, at NGOs, or street outreach. Participants were women, at least 18 years old, who self-identified as a FSW (i.e., traded sex for drugs, money, or other material benefit), and reported unprotected vaginal or anal sex with a client at least once during the previous four weeks. To achieve a high-risk FSW population for the intervention study, women were excluded if they practiced consistent use of condoms for vaginal and anal sex with all clients or if they had been employed as a sex worker for less than 4 weeks.
Data Collection
Data were collected by female interviewers during a private, face-to-face interview lasting approximately 40 minutes. Questionnaires were translated into Spanish and back-translated into English. Measures included four domains: i) baseline sociodemographic characteristics, ii) risk behaviors (i.e., condom use and substance use), iii) male client characteristics, and iv) detection of HIV and syphilis antibodies and testing for Chlamydia and gonorrhea.
Baseline Sociodemographic Characteristics
Sociodemographic variables collected included current age, age at initiation into sex work, marital status, having children, study site, migration into the state, and type of sex work (street, dance hostess, barmaid, other).
Condom Use
Condom use was assessed by determining whether participants had condoms with them at the interview; total number of sex acts in the past 6 months; number of protected sex acts in the past 6 months; average amount (USD) paid by clients for protected and unprotected sex; and condom use for vaginal sex with male clients in past the 6 months (never or sometimes versus often or always).
Substance Use
Participants were asked if they used alcohol or illicit drugs before or during sex in the past month; ever injected illicit drugs; injected cocaine, heroin, methamphetamine, or speedball in the past month; number of IDU sex partners in the past month; number of male clients in the last 6 months who ever injected drugs; and if they ever shared needles or injection equipment (including cotton, water or needles) with another person, including a client.
Male Client Characteristics
The questionnaire assessed number, type (regular and non-regular), and origin (U.S. or Mexico) of male clients, as well as the number of times the participant had vaginal sex with clients.
HIV, Syphilis, Chlamydia, and Gonorrhea
Blood samples were obtained by trained phlebotomists to test for HIV and syphilis antibodies. HIV antibody was detected on-site using the “Determine”® rapid HIV antibody test (Abbott Pharmaceuticals, Boston, MA); reactive samples were confirmed by EIA and Western Blot. The rapid plasma reagin (RPR) test was used to detect syphilis antibody (Macro-Vue, Becton Dickenson, Cockeysville, MD, USA); reactive samples were confirmed by Treponema pallidum hemagglutinin assay (TPHA) (Fujirebio, Wilmington, DE, USA). Presence of any syphilis antibodies reflected evidence of lifetime syphilis infection, whereas syphilis titers >1:8 were considered consistent with active infection, as recommended [22]. Cervical swabs were prepared and tested using the Aptima® Combo-2 collection device (Genprobe, San Diego, CA) to detect Neisseria gonorrhea and Chlamydia trachomatis. All STI tests as well as confirmatory HIV tests were conducted at the San Diego County Health Department or the El Paso County Health Department.
Statistical Analysis
Syphilis titers were dichotomized into those consistent with active infection vs. those that were not (i.e., >1:8 vs. ≤1:8). The ratio of protected sex acts in the past 6 months was calculated by dividing the number of protected sex acts by the total number of acts in that period. Bivariate associations by active syphilis status were performed with nonparametric Fisher’s Exact Test and Wilcoxon Two Sample Test, where appropriate.
Logistic regression was performed to identify factors associated with active syphilis. In multivariate regressions, all variables attaining significance (p<0.10) in bivariate analysis were considered for inclusion. Factors with medium-to-high correlation were not included in the same model (r>0.6). Models were reduced using manual stepwise regression (p<0.05). A tolerance test was performed on the final model to assess multicollinearity. No significant differences were observed by city; hence data for both sites were pooled.
Although there is not an exact correlation between RPR titers and duration of syphilis infection [22], higher titers may indicate more recent infection. In order to explore the hypothesis of parental transmission of syphilis through needle sharing with available data, Cochran-Armitage Trend Tests and Exact Permutation Tests were performed to assess trends between higher titers and frequency of drug injection, and frequency of receptive needle sharing in the past month.
RESULTS
Of 924 FSW participants, 10 did not have valid syphilis antibody test results and were excluded. Of the 914 participants remaining, median age was 32 years (IQR: 26, 39) and median duration of sex work was 4 years (IQR: 2, 10). Overall, 246 (26.9%) had evidence of syphilis infection, of whom 94 (38.2%, or 10.3% of the total) had syphilis titers consistent with active infection (titers>1:8).
Bivariate Associations
Comparing FSWs with and without titers consistent with active syphilis infection, there were no significant differences for sociodemographic characteristics, including age, age at initiation into sex work, city of residence, migration, or condom use characteristics (Table 1). However, those having titers consistent with active syphilis infection differed in their substance abuse, client characteristics, and HIV/STI prevalence.
Table 1.
Bivariate Statistics and Associations by Active Syphilis (titer>1:8) Status for Characteristics of Female Sex Workers (N=914)
| Negative (n=820) | Positive (n=94) | p-value | |
|---|---|---|---|
|
Sociodemographic Characteristics
| |||
| Age | 33.5 (9.2) | 32.5 (8) | 0.44 |
| Age of Initiation into Sex Work, % | 0.72 | ||
| <18 | 80 (10) | 10 (11) | |
| 18+ | 732 (90) | 83 (89) | |
| Marital Status, % | 0.09 | ||
| married/cohabitated | 190 (23) | 30 (32) | |
| single | 402 (49) | 46 (49) | |
| other | 223 (27) | 18 (19) | |
| Has Children, % | 767 (94) | 86 (92) | 0.37 |
| City of Residence, % | 0.28 | ||
| Tijuana | 412 (50) | 53 (56) | |
| Ciudad Juarez | 408 (50) | 41 (44) | |
| Migrated into this State, % | 494 (60) | 57 (61) | 0.99 |
| Sex Worker Type, % | 0.03 | ||
| street worker | 439 (54) | 66 (70) | |
| dance hostess | 181 (22) | 13 (14) | |
| barmaid | 132 (16) | 11 (12) | |
| other | 68 (8) | 4 (4) | |
|
| |||
|
Condom Use
| |||
| Participant brought condoms to the interview, % | 93 (12) | 8 (8) | 0.49 |
| % Unprotected vaginal sex | 43.5 (30.7) | 43.5 (29.5) | 0.86 |
| Average USD earned for sex WITH a condom | 28.9 (26.9) | 26.3 (21.8) | 0.70 |
| Average USD earned for sex WITHOUT a condom | 47.4 (74.9) | 35.7 (28.6) | 0.15 |
| Used condoms for vaginal sex with male clients‡, % | 0.66 | ||
| never/sometimes | 463 (57) | 51 (54) | |
| often/always | 355 (43) | 43 (46) | |
|
| |||
|
Substance Use
| |||
| Used alcohol before/during sex†, % | 0.44 | ||
| never/sometimes | 631 (77) | 76 (81) | |
| often/always | 188 (23) | 18 (19) | |
| Used illegal drug before/during sex†, % | <0.001 | ||
| never/sometimes | 717 (88) | 64 (69) | |
| often/always | 101 (12) | 29 (31) | |
| Ever been an IDU, % | 128 (16) | 34 (36) | <0.001 |
| Ever shared needles/injection equipment, % | 103 (13) | 26 (28) | <0.001 |
| Injected drugs†, % | 144 (18) | 37 (39) | <0.001 |
| Injected cocaine†, % | 52 (7) | 6 (7) | 0.99 |
| Injected heroin†, % | 110 (14) | 31 (33) | <0.001 |
| Injected methamphetamine†, % | 25 (3) | 4 (4) | 0.53 |
| Injected speedball†, % | 52 (6) | 11 (12) | 0.08 |
| Number of IDU sex partners† | 0.8 (4.1) | 0.5 (1.1) | 0.32 |
| Male clients‡ who ever injected drugs, % | 262 (39) | 27 (31) | 0.20 |
| Shared needles with clients†, % | 17 (2) | 3 (3) | 0.45 |
|
| |||
|
Male Client Characteristics
| |||
| Number of male clients‡ | 332 (320.1) | 382.7 (371.5) | 0.24 |
| Number of regular male clients† | 5.8 (9.2) | 7.1 (11) | 0.12 |
| Times you had vaginal sex with regular male clients | 19.2 (23.5) | 21.4 (19.5) | 0.08 |
| Number of non-regular male clients† | 39.9 (48) | 34 (40.5) | 0.37 |
| Times you had vaginal sex with non-regular clients | 43.6 (50.7) | 37.7 (42.6) | 0.38 |
| Had any U.S. clients, % | 547 (67) | 79 (84) | <0.001 |
|
| |||
|
STI Status
| |||
| HIV, % | 37 (4) | 16 (17) | <0.001 |
| Chlamydia, % | 85 (12) | 18 (22) | 0.01 |
| Gonorrhea, % | 32 (4) | 18 (22) | <0.001 |
Univariate Statistics include Mean (SD) and Wilcoxon Test p-value for continuous variables. N (%) and Fisher Exact Test p-value for categorical variables. Categorical variables denoted with %
in the past month
in the past 6 months
FSWs with titers consistent with active syphilis were more likely to report being street workers (70% vs 54%; p=0.03), injecting drugs in the past month (39% vs 18%; p<0.001), often/always using illegal drug before/during sex in the past month (31% vs 12%; p<0.001), ever injecting drugs (36% vs 16%; p<0.001) or sharing needles or injection equipment (28% vs 13%; p<0.001), and to report having any U.S. clients (84% vs 67%; p<0.001). Marginally significant differences were observed between active syphilis infection and injecting speedball in the past month. We did not observe differences by syphilis status for drinking alcohol before/during sex, injecting cocaine or methamphetamine in the past month, mean number of IDU sex partners in the past month, sharing needles with clients, or having male clients in the last 6 months who ever injected drugs (Table 1).
FSWs with titers consistent with active syphilis had more than two and half times the odds of having U.S. clients (Table 2). A marginally significant difference was observed between active syphilis infection and mean number of vaginal sex acts with regular male clients; however, we found no association between active syphilis infection and the mean number of regular or non-regular male clients or frequency of vaginal sex with non-regular clients (Table 1). The odds of having titers consistent with active syphilis was at least two-fold higher for those with concomitant HIV, Chlamydia, and gonorrhea infections (Table 2).
Table 2.
Odd Ratios and 95% Confidence Intervals by Active Syphilis (titer>1:8) Status for Characteristics of Female Sex Workers (N=914)
| OR (95% CI) | |
|---|---|
|
Sociodemographic Characteristics
| |
| Age | 0.94 (0.83, 1.06)* |
| Age of Initiation into Sex Work | |
| <18 | (ref) |
| 18+ | 0.91 (0.45, 1.82) |
| Marital Status | |
| married/cohabitated | (ref) |
| single | 0.72 (0.44, 1.18) |
| other | 0.51 (0.28, 0.95) |
| Has Children | 0.69 (0.31, 1.50) |
| City of Residence | |
| Tijuana | 1.28 (0.83, 1.96) |
| Ciudad Juarez | (ref) |
| Migrated into this State | 1.00 (0.65, 1.55) |
| Sex Worker Type | |
| street worker | (ref) |
| dance hostess | 0.48 (0.26, 0.89) |
| barmaid | 0.55 (0.28, 1.08) |
| other | 0.39 (0.14, 1.11) |
|
| |
|
Condom Use
| |
| Participant brought condoms to the interview | 0.71 (0.33, 1.52) |
| % Unprotected vaginal sex | 1 (0.93, 1.07)** |
| Average USD earned for sex WITH a condom | 0.96 (0.87, 1.05)** |
| Average USD earned for sex WITHOUT a condom | 0.94 (0.88, 1.01)** |
| Used condoms for vaginal sex with male clients‡ | |
| never/sometimes | (ref) |
| often/always | 1.1 (0.72, 1.69) |
|
| |
|
Substance Use
| |
| Used alcohol before/during sex† | |
| never/sometimes | (ref) |
| often/always | 0.79 (0.46, 1.36) |
| Used illegal drug before/during sex† | |
| never/sometimes | (ref) |
| often/always | 3.22 (1.98, 5.23) |
| Ever been an IDU | 3.06 (1.93, 4.86) |
| Ever shared needles/injection equipment | 2.66 (1.62, 4.37) |
| Injected drugs† | 2.99 (1.91, 4.69) |
| Injected cocaine† | 1.01 (0.42, 2.43) |
| Injected heroin† | 3.16 (1.96, 5.08) |
| Injected methamphetamine† | 1.39 (0.47, 4.08) |
| Injected speedball† | 1.98 (0.99, 3.94) |
| Number of IDU sex partners† | 0.59 (0.16, 2.18)** |
| Male clients‡ who ever injected drugs | 0.72 (0.45, 1.17) |
| Shared needles with clients† | 1.56 (0.45, 5.42) |
|
| |
|
Male Client Characteristics
| |
| Number of male clients‡ | 1 (1, 1.01)** |
| Number of regular male clients† | 1.12 (0.94, 1.33)** |
| Times you had vaginal sex with regular male clients | 1.04 (0.96, 1.12)** |
| Number of non-regular male clients† | 0.97 (0.92, 1.02)** |
| Times you had vaginal sex with non-regular clients | 0.97 (0.93, 1.02)** |
| Had any U.S. clients | 2.63 (1.49, 4.65) |
|
| |
|
STI Status
| |
| HIV | 4.32 (2.30, 8.13) |
| Chlamydia | 2.11 (1.19, 3.73) |
| Gonorrhea | 6.07 (3.23, 11.43) |
per 5 years and
per 10 unit increase indicated
in the past month
in the past 6 months
Factors Independently Associated with Active Syphilis
In the multivariate model, having syphilis titers consistent with active infection were independently associated with injecting drugs in the past month (AOR: 2.39; 95% CI: 1.40, 4.80), having used illegal drugs before or during sex within the last month (AOR: 2.06; 95% CI: 1.16, 3.65), and having any U.S. clients (AOR: 2.85; 95% CI: 1.43, 5.70) (Table 3). Model robustness was assessed by forcing age, age at initiation into sex work, or number of years in sex work into the final model. We found only minimal deviations in the significance or odds ratios and no change in significance or direction of the association with active syphilis.
Table 3.
Characteristics Independently Associated with Active Syphilis (titer>1:8) (N=769)
| Characteristic | AOR (95% CI) |
|---|---|
| Injected drugs in the past month | 2.39 (1.40, 4.08) |
| Often/Always used illegal drug before/during sex in past month | 2.06 (1.16, 3.65) |
| Had any U.S. clients | 2.85 (1.43, 5.70) |
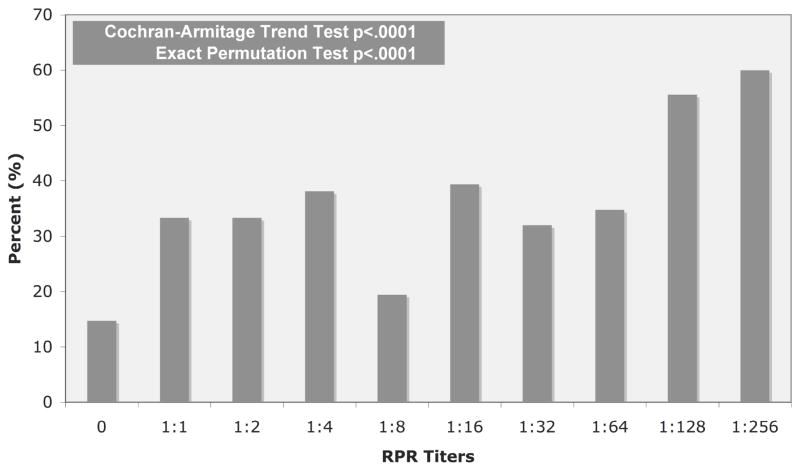
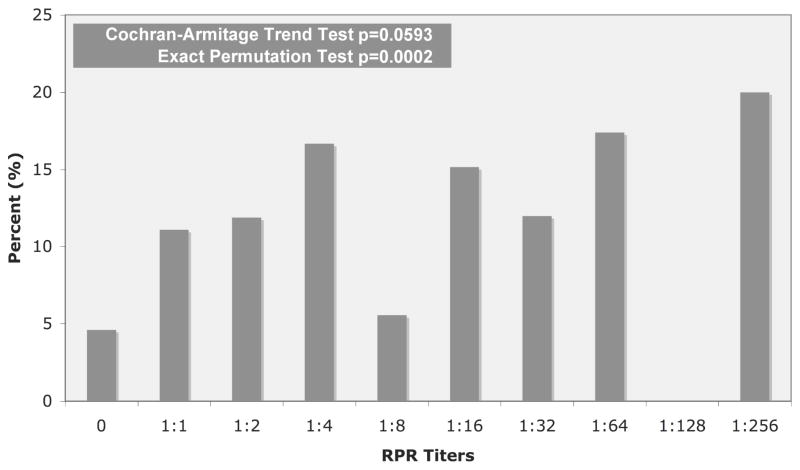
Trend Tests
A significant association was indicated between higher syphilis titers and increasing frequency of drug injection in the past month as well as higher frequency of receptive needle sharing in the past month (Figures 1 and 2).
Figure 1.
Drug Injection in the Past Month by Syphilis Titers
Figure 2.
Receptive Needle Sharing in the Past Month by Syphilis Titers
DISCUSSION
In Mexico overall, syphilis incidence is 1.2 per 100,000 [23], but among Mexico’s 32 states, syphilis incidence is highest in Baja California (7.4 per 100,000), and fourth highest in Chihuahua (3.8 per 100,000) [23]. Our findings suggest that in addition to sexual risks, drug use may play both a direct and an indirect role in syphilis transmission in these two Mexico-U.S. border states. In particular, after taking into account the use of illicit drugs during sex, injection drug use was independently associated with nearly three-fold higher odds of active syphilis infection.
Our findings extend those from a recent study suggesting that parental exposure may be an important risk factor for syphilis among some IDU populations. A cross-sectional study conducted among male and female IDUs in Barnaul, Russia found that syphilis was significantly associated with daily drug injection, duration of injection, and having IDU sexual partners [12]. However, that study did not differentiate between prevalent and incident syphilis infections, which compromised its ability to draw causal inferences. Our study examined syphilis titers >1:8, which are consistent with active infections that are more likely to have been acquired recently [22]. Our trend analysis also lends support to the hypothesis that syphilis may be parenterally transmitted through needle sharing in these cities. While we cannot rule out the possibility that our findings are a result of residual confounding, our data suggest that this contention is highly plausible. Further prospective studies that assess IgM versus IgG titers among IDU populations may help to further elucidate causal inferences.
Our findings suggest the need for syphilis eradication programs to consider including a safer injection component, and conversely, for harm reduction programs to incorporate STI testing and treatment. Despite widespread heroin use in these cities, few methadone maintenance programs exist, only one of which is publicly funded [24]. In recent years, mobile clinics (condonetas) offering condom provision and HIV testing operate in most Mexican states, and sometimes offer sterile syringe exchange. However, the availability of rapid testing for syphilis and other STIs and on-site treatment is sporadic.
Providing IDUs access to sterile syringes through over-the-counter sales or through needle exchange programs (NEPs) has also been a challenge in Mexico. Although in Mexico, syringes can be legally purchased without a prescription at pharmacies and there are no paraphernalia laws that prevent IDUs from carrying syringes, IDUs attempting syringe purchases in Tijuana report being charged higher prices or being refused purchase [25]. IDUs in both Tijuana and Ciudad Juarez have consistently reported being arrested for carrying sterile or used syringes [25, 26], and history of arrest for this supposed offense was independently associated with receptive needle sharing in both cities [26]. Indeed, fear of arrest was cited by many IDUs in both cities as a main reason why they sought to inject in shooting galleries, where used syringes are borrowed or rented [25, 27]. Despite concerns from community stakeholders about harm reduction interventions in Tijuana [24], NEPs are operating in both Tijuana and Ciudad Juarez and four other Mexican states: Coahuila, Nuevo Leon, Oaxaca, Sinaloa, and Zacatecas [28, 29]. However, the demand for syringes appears consistently to outstrip their availability.
We also observed that having recently used illegal drugs before or during sex was independently associated with active syphilis. This may reflect FSWs’ compromised ability to negotiate condom use while impaired, as reported elsewhere [30, 31]. FSWs on the Mexico-Guatemala border reported difficulties negotiating condom use when their male partner was under the influence of alcohol or drugs [30]. STI prevalence among African-American adolescent females was significantly associated with their male partners’ alcohol or drug use [32]. These studies suggest that risk reduction interventions among FSWs should also focus on their intimate partners and clients. When available, women can be encouraged to use female condoms when a male condom cannot be negotiated [30, 33, 34].
Consistent with an earlier report from our group [35], having U.S. clients was independently associated with having active syphilis among FSWs in Tijuana and Ciudad Juarez. In the same study, FSWs with U.S. clients had higher rates of drug-using behavior, including injecting drugs in the last month. They were also more likely to use drugs before/during sex, and to have clients who use and inject drugs [35]. Since more than two-thirds of FSWs in these cities report clients from the U.S. [35], these data suggest that U.S. men seeking paid sex across the border in Mexico are at considerable risk of acquiring and transmitting syphilis and other STIs. Rates for primary and secondary syphilis in San Diego County increased from 3.8 to 11.8 per 100,000 between 2003 and 2007 [36], and between 2006 to 2007, reported a 47% increased incidence in acquired syphilis [37].
Results of our study should be interpreted bearing in mind its limitations. In the absence of information on whether participants had recently been treated for syphilis, antibody titers alone are not sufficient to determine whether syphilis titers>1:8 accurately reflect infectious status. However, since 98% of FSWs in this study were unaware that they had an STI [1], it is unlikely that many infections were being treated. In these settings, lacking aggressive case-finding and partner notification, it is possible that some syphilis infections may not have been recently acquired, which would have attenuated associations towards the null. Despite our detailed analysis of syphilis antibody titers, our study was cross-sectional, precluding the confirmation of causal inferences that require prospective studies. Although convenience sampling may limit the external validity of our findings, it should not influence the direction or the magnitude of the associations we observed.
Socially desirable responding of measures may introduce potential reporting bias. Given the stigma associated with drug use, the validity of self-reported measures, such as current or past drug use may have been underreported. However, strategies to improve validity included assuring participants of the confidentiality and selecting empathic and skillful trained female interviewers, many of whom were ex-FSWs who could establish rapport [38]. Although there are no studies that focus on validity of self-reports among FSWs, self-reported risk behaviors among IDUs are reliable and valid [39].
Given the sizable overlap between FSW and IDU populations in these cities [5] and the consistent associations we observed between syphilis infection and injection behaviors, our findings suggest that harm reduction should be integrated into STI prevention programs. This could include access to sterile syringes in health clinics where STI testing is offered, offering rapid STI testing and on-site treatment at NEPs and drug treatment programs, and encouraging dis-infection of injection equipment in cases where sterile syringes are unavailable (e.g. prisons). Like most countries, STI prevention and harm reduction programs are not well integrated in Mexico. Our data suggest that failure to integrate these programs could exacerbate the course of both HIV and syphilis epidemics.
Acknowledgments
This research was made possible with support from NIMH Grant R01MH065849, NIDA Grant R01DA023877 and NIDA Diversity Supplement Grant DA019829-02S1. The authors gratefully acknowledge the study staff and participants of Proyecto Mujer Segura and the following organizations for their cooperation: the Municipal and State Health Departments of Tijuana, Baja California and Ciudad Juárez, Chihuahua; Salud y Desarollo Comunitario de Ciudad Juárez A.C. (SADEC), Patronato Pro-COMUSIDA and Federación Mexicana de Asociaciones Privadas (FEMAP); and the Universidad Autónoma de Baja California (UABC) and Universidad Autónoma de Ciudad Juárez (UACJ). In addition we would like to thank the County Health Departments of San Diego and El Paso for their assistance with STI and HIV testing. O. Loza also gratefully acknowledges her dissertation committee: V.D. Ojeda from the University of California at San Diego and Sue Lindsay and Ming Ji from San Diego State University.
Footnotes
Clinical Trial Registration: The intervention study that provided the data analyzed in this paper is registered with the U.S. National Institutes of Health on ClinicalTrials.gov as Protocol #NCT00338845.
Conflict of Interest Declaration:
Funding for this study was provided by the U.S. National Institutes of Health under Grants R01MH065849, R01DA023877, and Diversity Supplement DA019829-02S1. The authors declare that they have no connection with any companies in the tobacco, alcohol, pharmaceutical, or gaming industries.
References
- 1.Patterson TL, Semple SJ, Fraga M, Bucardo J, de la Torre A, Salazar J, et al. Comparison of sexual and drug use behaviors between female sex workers in Tijuana and Ciudad Juarez, Mexico. Subst Use Misuse. 2006;41:1535–49. doi: 10.1080/10826080600847852. [DOI] [PubMed] [Google Scholar]
- 2.Brouwer KC, Case P, Ramos R, Magis-Rodriguez C, Bucardo J, Patterson TL, et al. Trends in production, trafficking, and consumption of methamphetamine and cocaine in Mexico. Subst Use Misuse. 2006;41:707–27. doi: 10.1080/10826080500411478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bucardo J, Brouwer KC, Magis-Rodriguez C, Ramos R, Fraga M, Perez SG, et al. Historical trends in the production and consumption of illicit drugs in Mexico: implications for the prevention of blood borne infections. Drug Alcohol Depend. 2005;79:281–93. doi: 10.1016/j.drugalcdep.2005.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bucardo J, Semple SJ, Fraga-Vallejo M, Davila W, Patterson TL. A qualitative exploration of female sex work in Tijuana, Mexico. Arch Sex Behav. 2004;33:343–51. doi: 10.1023/B:ASEB.0000028887.96873.f3. [DOI] [PubMed] [Google Scholar]
- 5.Strathdee SA, Philbin MM, Semple SJ, Pu M, Orozovich P, Martinez G, et al. Correlates of injection drug use among female sex workers in two Mexico-US. border cities. Drug Alcohol Depend. 2008;92:132–40. doi: 10.1016/j.drugalcdep.2007.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hyams KC, Escamilla J, Lozada Romero R, Macareno Alvarado E, Bonilla Giraldo N, Papadimos TJ, et al. Hepatitis B infection in a non-drug abusing prostitute population in Mexico. Scand J Infect Dis. 1990;22:527–31. doi: 10.3109/00365549009027091. [DOI] [PubMed] [Google Scholar]
- 7.Gourevitch MN, Hartel D, Schoenbaum EE, Selwyn PA, Davenny K, Friedland GH, et al. A prospective study of syphilis and HIV infection among injection drug users receiving methadone in the Bronx, NY. Am J Public Health. 1996;86:1112–5. doi: 10.2105/ajph.86.8_pt_1.1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Farley TA, Hadler JL, Gunn RA. The syphilis epidemic in Connecticut: relationship to drug use and prostitution. Sex Transm Dis. 1990;17:163–8. doi: 10.1097/00007435-199010000-00003. [DOI] [PubMed] [Google Scholar]
- 9.Infectious disease testing for blood transfusions. NIH Consens Statement. 1995;13:1–27. [PubMed] [Google Scholar]
- 10.Greenwalt TJ, Rios JA. To test or not to test for syphilis: a global problem. Transfusion. 2001;41:976. doi: 10.1046/j.1537-2995.2001.41080976.x. [DOI] [PubMed] [Google Scholar]
- 11.Moore EA, Moore LM. Encyclopedia of sexually transmitted diseases. Jefferson, N.C: McFarland; 2005. [Google Scholar]
- 12.Platt L, Rhodes T, Judd A, Koshkina E, Maksimova S, Latishevskaya N, et al. Effects of sex work on the prevalence of syphilis among injection drug users in 3 Russian cities. Am J Public Health. 2007;97:478–85. doi: 10.2105/AJPH.2005.069732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Patterson TL, Semple SJ, Staines H, Lozada R, Orozovich P, Bucardo J, et al. Prevalence and correlates of HIV infection among female sex workers in 2 Mexico-US border cities. J Infect Dis. 2008;197:728–32. doi: 10.1086/527379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Strathdee SA, Lozada R, Ojeda VD, Pollini RA, Brouwer KC, Vera A, et al. Differential effects of migration and deportation on HIV infection among male and female injection drug users in Tijuana, Mexico. PLoS ONE. 2008;3:e2690. doi: 10.1371/journal.pone.0002690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lowndes CM, Alary M, Platt L. Injection drug use, commercial sex work, and the HIV/STI epidemic in the Russian Federation. Sex Transm Dis. 2003;30:46–8. doi: 10.1097/00007435-200301000-00010. [DOI] [PubMed] [Google Scholar]
- 16.Reynolds SJ, Risbud AR, Shepherd ME, Rompalo AM, Ghate MV, Godbole SV, et al. High rates of syphilis among STI patients are contributing to the spread of HIV-1 in India. Sex Transm Infect. 2006;82:121–6. doi: 10.1136/sti.2005.015040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rompalo AM, Joesoef MR, O’Donnell JA, Augenbraun M, Brady W, Radolf JD, et al. Clinical manifestations of early syphilis by HIV status and gender: results of the syphilis and HIV study. Sex Transm Dis. 2001;28:158–65. doi: 10.1097/00007435-200103000-00007. [DOI] [PubMed] [Google Scholar]
- 18.Silverman JG, Decke MR, Gupta J, Dharmadhikari A, Seage GR, 3rd, Raj A. Syphilis and hepatitis B Co-infection among HIV-infected, sex-trafficked women and girls, Nepal. Emerg Infect Dis. 2008;14:932–4. doi: 10.3201/eid1406.080090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ruan Y, Cao X, Qian HZ, Zhang L, Qin G, Jiang Z, et al. Syphilis among female sex workers in southwestern China: potential for HIV transmission. Sex Transm Dis. 2006;33:719–23. doi: 10.1097/01.olq.0000218881.01437.99. [DOI] [PubMed] [Google Scholar]
- 20.Reza-Paul S, Beattie T, Syed HU, Venukumar KT, Venugopal MS, Fathima MP, et al. Declines in risk behaviour and sexually transmitted infection prevalence following a community-led HIV preventive intervention among female sex workers in Mysore, India. AIDS. 2008;22(Suppl 5):S91–100. doi: 10.1097/01.aids.0000343767.08197.18. [DOI] [PubMed] [Google Scholar]
- 21.Patterson TL, Semple SJ, Fraga M, Bucardo J, de la Torre A, Salazar J, et al. A sexual risk reduction intervention for female sex workers in Mexico: Design and baseline characteristics. Journal of HIV/AIDS & Social Services. 2006;5:115–37. [Google Scholar]
- 22.Golden MR, Marra CM, Holmes KK. Update on syphilis: resurgence of an old problem. JAMA. 2003;290:1510–4. doi: 10.1001/jama.290.11.1510. [DOI] [PubMed] [Google Scholar]
- 23.Consejo Nacional para la Prevención y el Control del VIH-SIDA (CONASIDA) Panorama epidemiológico del VIH/SIDA e ITS en México (30 de junio del 2007) Epidemiological panorama of HIV/AIDS and STIs in Mexico. 2007 June 30; [cited 2009 March 11]; Available from: http://www.censida.salud.gob.mx/interior/panorama.html.
- 24.Philbin MM, Mantsios A, Lozada R, Case P, Pollini RA, Alvelais J, et al. Exploring stakeholder perceptions of acceptability and feasibility of needle exchange programmes, syringe vending machines and safer injection facilities in Tijuana, Mexico. Int J Drug Policy. 2009;20:329–35. doi: 10.1016/j.drugpo.2008.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Strathdee SA, Fraga WD, Case P, Firestone M, Brouwer KC, Perez SG, et al. “Vivo para consumirla y la consumo para vivir” [“I live to inject and inject to live”]: high-risk injection behaviors in Tijuana, Mexico. J Urban Health. 2005;82:iv58–73. doi: 10.1093/jurban/jti108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pollini RA, Brouwer KC, Lozada RM, Ramos R, Cruz MF, Magis-Rodriguez C, et al. Syringe possession arrests are associated with receptive syringe sharing in two Mexico-US border cities. Addiction. 2008;103:101–8. doi: 10.1111/j.1360-0443.2007.02051.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Philbin M, Pollini RA, Ramos R, Lozada R, Brouwer KC, Ramos ME, et al. Shooting gallery attendance among IDUs in Tijuana and Ciudad Juarez, Mexico: correlates, prevention opportunities, and the role of the environment. AIDS Behav. 2008;12:552–60. doi: 10.1007/s10461-008-9372-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Consejo Nacional Contra Las Adicciones (CONADIC) El consumo de drogas inyectadas y la epidemia del VIH/SIDA en Mexico. Un problema de salud pública: Documento de posicion. Injection drug use and the HIV/AIDS epidemic in Mexico. A public health problem. Position paper. Mexico City. 2003 [cited 2009 April 4]; Available from: http://www.salud.gob.mx/unidades/cdi/documentos/Drogas_EpidemiaVIH.pdf.
- 29.Magis-Rodriguez CORL, Ortiz Mondragon R. Drug Use Harm Reduction Activities: Interna Report 2006. Mexico City: 2006. Actividades de Reducción del Daño en Usuarios de Drogas: Informe Interno 2006. Available from: http://www.censida.gob.mx. [Google Scholar]
- 30.De Caso LE, Egremy-Mendívil G, Uribe-Zúñiga P, Chin-Quee C, Robledo C, Valin-Hebrard J. El uso del condón femenino como una posible alternativa con clientes bajo efectos de alcohol y/o drogas que rechazan el condón masculino [The use of female condom as a possible alternative with clients who reject male condom use and are under the effects of alcohol and/or use of drugs]. VIII Congreso Nacional Sobre SIDA e Infecciones de Trasmisión Sexual; 2002; Veracruz, Mexico. [Google Scholar]
- 31.Rodríguez García de Cortázar A, Hernán García M, Cabrera León A, García Caleja JM, Romo Avilés N. ¿Qué opinan adolescentes y jóvenes sobre el consumo de drogas recreativas y las conductas sexuales de riesgo? [What do adolecents think about recreational drug use and sexual risk behavior?] Adicciones. 2007;19:153–68. [PubMed] [Google Scholar]
- 32.Crosby RA, Diclemente RJ, Wingood GM, Salazar LF, Lang D, Rose E, et al. Co-occurrence of intoxication during sex and sexually transmissible infections among young African American women: does partner intoxication matter? Sex Health. 2008;5:285–9. doi: 10.1071/sh07098. [DOI] [PubMed] [Google Scholar]
- 33.Telles Dias PR, Souto K, Page-Shafer K. Long-term female condom use among vulnerable populations in Brazil. AIDS Behav. 2006;10:S67–75. doi: 10.1007/s10461-006-9139-x. [DOI] [PubMed] [Google Scholar]
- 34.Witte SS, Wada T, El-Bassel N, Gilbert L, Wallace J. Predictors of female condom use among women exchanging street sex in New York City. Sex Transm Dis. 2000;27:93–100. doi: 10.1097/00007435-200002000-00007. [DOI] [PubMed] [Google Scholar]
- 35.Strathdee SA, Lozada R, Semple SJ, Orozovich P, Pu M, Staines-Orozco H, et al. Characteristics of female sex workers with US clients in two Mexico-US border cities. Sex Transm Dis. 2008;35:263–8. doi: 10.1097/OLQ.0b013e31815b0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Centers for Disease Control and Prevention (CDC) Sexually Transmitted Disease Surveillance. 2007 [cited 2009 April 4]; Available from: http://www.cdc.gov/std/stats07/syphilis.htm.
- 37.County of San Diego. Sexually Transmitted Diseases Quarterly Report. (1) 2007 January–December; [cited 2009 April 4]; Available from: http://www.sdcounty.ca.gov/hhsa/programs/phs/documents/STDQuarterlyReport-IssueNo1.pdf.
- 38.Rouse BA, Kozel NJ, Richards LG, editors. Self-Report Methods of Estimating Drug Use: Meeting Current Challenges to Validity. NIDA Research Monograph. 1985;57 [cited 2009 September 24]; Available from: www.drugabuse.gov/pdf/monographs/57.pdf. [PubMed]
- 39.Darke S, Hall W, Heather N, Ward J, Wodak A. The reliability and validity of a scale to measure HIV risk-taking behaviour among intravenous drug users. AIDS. 1991;5:181–5. doi: 10.1097/00002030-199102000-00008. [DOI] [PubMed] [Google Scholar]