Abstract
Objectives
Lack of feeling connected and poor social problem solving has been described in suicide attempters. However, cognitive substrates of this apparent social impairment in suicide attempters remain unknown. One possible deficit, the inability to recognize others' complex emotional states has been observed not only in disorders characterized by prominent social deficits (autism-spectrum disorders and frontotemporal dementia) but also in depression and normal aging. This study assessed the relationship between social emotion recognition, problem solving, social functioning, and attempted suicide in late-life depression.
Design, Participants, Measurements
There were 90 participants: 24 older depressed suicide attempters, 38 non-suicidal depressed elders, and 28 comparison subjects with no psychiatric history. We compared performance on the Reading the Mind in the Eyes test and measures of social networks, social support, social problem solving, and chronic interpersonal difficulties in these three groups.
Results
Suicide attempters committed significantly more errors in social emotion recognition and showed poorer global cognitive performance than elders with no psychiatric history. Attempters had restricted social networks: they were less likely to talk to their children, had fewer close friends, and did not engage in volunteer activities, compared to non-suicidal depressed elders and those with no psychiatric history. They also reported a pattern of struggle against others and hostility in relationships, felt a lack of social support, perceived social problems as impossible to resolve, and displayed a careless/ impulsive approach to problems.
Conclusions
Suicide attempts in depressed elders were associated with poor social problem-solving, constricted social networks, and disruptive interpersonal relationships. Impaired social emotion recognition in the suicide attempter group was related to global cognitive decline, thus it is possible that cognitive decline is one of the risk factors for suicide attempt in late-life, interacting with social deficits and psychosocial factors.
Objectives
Suicide rates are the highest in old age in almost every country in the world. Yet, it is difficult to identify those at risk, since known risk factors, such as depression, pain, disability, or financial problems have limited predictive power (1-3). The role of deficits in cognitive abilities is a poorly understood part of the suicidal diathesis (4, 5), especially in older adults (6). The failure to deal with social stressors may play a particularly important role in suicidal behavior, and indeed suicide attempters report difficulties resolving social problems in questionnaire-based studies (7, 8). However, cognitive substrates of this apparent social incompetence in suicide attempters remain unknown. It is conceivable that a misperception of others' emotions can undermine social problem solving, leading to feelings of hopelessness in the face of losses, conflict, and dependence on caregivers. Deficits in emotion recognition may lead to low levels of social connectedness and belonging, known risk factors for suicide attempt and death by suicide in late life (9-11).
Lesion studies indicate that emotion recognition and other social cognitive abilities depend critically on the orbitofrontal cortex (12-14). Patients with early frontal variant frontotemporal dementia, characterized by orbitofrontal degeneration, are impaired on social cognition tasks when compared to patients with Alzheimer's disease (15, 16). In turn, post-mortem (17) and in vivo imaging (18, 19) studies implicate alterations in the orbitofrontal cortex in completed and attempted suicide. For example, euthymic suicide attempters showed greater BOLD response in the right lateral orbitofrontal cortex during processing of angry faces, compared to non-suicidal affective controls (18). Converging with these results, a study of depressed individuals (20) found that performance on the Reading the Mind in the Eyes test (RME) (21, 22), a widely used measure of complex social emotion recognition, was impaired in individuals with suicidal thoughts, anhedonia, and guilt, or “hopelessness depression”, but unrelated to the overall severity of depression. Given that normal aging is associated with a decline in emotion recognition (23), deficits in social cognition may be particularly pertinent to suicidal behavior in the elderly.
To examine whether impaired emotion recognition and broader social functioning are associated with attempted suicide in old age, we conducted a study in older patients with depression with or without suicide attempts, and in non-depressed elders. We hypothesized that suicide attempters would show impaired social emotion recognition and social problem solving compared both to depressed non-suicidal elders and to the non-psychiatric comparison subjects. Since older suicidal individuals may be socially isolated and may experience conflict in their relationships (10, 11, 24, 25), we also assessed social network diversity, number and frequency of contacts, perceived social support, and chronic interpersonal difficulties. Finally, we explored whether emotion recognition abilities in suicide attempters are associated with self-reported social problem solving, overall cognitive performance, chronic interpersonal difficulties, and medical lethality of the suicide attempt.
Methods
Ninety participants aged 60 and older were recruited between June 2006 and October 2009: 24 depressed suicide attempters and 38 non-suicidal depressed elders were recruited on an inpatient psychogeriatric unit and in a late-life depression clinic; 28 elders with no psychiatric history were recruited from University and community primary care practices. Depressed participants met criteria for major depressive disorder as determined by the Structured Clinical Interview of the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition Axis I Disorders (SCID-IV). Suicide attempts were defined by the O'Carroll criteria (self-injurious act with the intent to die) (26). Non-suicidal depressed participants had no life-time history of suicidal ideation, attempt, or non-suicidal self-injury as ascertained with the SCID and Beck's Scale for Suicidal Ideation (SSI) total score of less than 3 and item 4 (Desire to make an active suicidal attempt) score of 0. We also excluded subjects from the non-suicidal depressed group if they endorsed indirect self-destructive behavior based on a score of 1 or higher on item 5 of the SSI. Depressed participants with co-morbid anxiety disorders or substance use disorders were included to enhance the representativeness of the sample. However, to ensure that there was no acute effect of substance intoxication or withdrawal on cognitive performance, we delayed testing if there was any indication of intoxication or withdrawal within 72 hours. We excluded patients with bipolar disorder, schizophrenia, schizoaffective disorder, sensory disorders that precluded cognitive testing, dementia or severe cognitive impairment as reflected by a score of 23 or lower on the Mini-Mental State Examination (MMSE). Patients who had received electroconvulsive therapy in the previous 6 months and those with neurological disorders, such as stroke, epilepsy, known neurodegenerative disorders, and brain tumors, were also excluded. Non-psychiatric controls could not meet criteria for any SCID-IV diagnosis. All participants provided written informed consent as required by the University of Pittsburgh Institutional Review Board.
Procedures
Depressed participants were assessed within two weeks of inpatient admission or at the initiation of outpatient treatment. They continued to receive psychotropic medications as indicated clinically. The study assessments were administered by trained study clinicians, all of whom were required to complete regular inter-rater reliability testing. After informed consent was obtained, participants' clinical charts were extensively reviewed to determine past history and severity of any suicide attempts.
Assessments of Clinical Characteristics and Suicidality
Psychiatric diagnoses were made using the SCID-IV and reviewed and verified at research consensus conferences. Depression severity was measured using the 16-item version of the Hamilton Rating Scale for Depression (HRSD-16) that consists of the 17-item version minus the suicide item. The intensity of pharmacotherapy for the current episode of depression was assessed with the cumulative strength score from the Antidepressant Treatment History Form (27). Burden of physical illness was assessed with the Cumulative Illness Rating Scale adapted for Geriatrics (28).
Significant others (family or friends) were asked to sign a separate consent and information on suicide history and clinical course was collected from interviews with significant others. Suicide attempt history was verified by a study psychiatrist, using the interview, medical records, information from the treatment team, and information from family or friends (obtained through separate consent). We excluded participants with significant discrepancies between these sources. All attempters had current suicidal ideation and an active plan as measured by the SSI (29). In attempters, the severity of suicidal intent associated with the attempt was assessed using the Suicidal Intent Scale (30). The medical lethality of the attempt was measured using Beck's Lethality Scale (31). Finally, to control for possible effects of brain injury related to the suicide attempt, study psychiatrists (KS or AYD) assessed participants for any attempts with a score of ≥4 on the Beck's Lethality Scale and any history of systemic hypotension lasting >5 minutes, or asphyxia, or neurotoxic ingestion.
Social Emotion Recognition
The RME (21, 22) was used to measure the capacity for subtle discrimination of others' emotions. This test comprises 36 photographs of facial expressions of complex, social emotions such as suspiciousness, flirtatiousness, irritated. In each photo, only the eye region of the face is visible. Participants were asked to describe the expression from a list of four adjectives. Participants were offered definitions of each adjective if they did not understand the word. This is a challenging test that is capable of detecting subtle impairment, even though there is minimal demand on executive function: healthy middle age adults perform at about 70% accuracy (22).
Social Functioning
The Social Network Index (32) was used to evaluate participants' social relationships, including those with children, friends, parents, parents-in-laws, siblings. We also assessed participants' perceived levels of social support using the Interpersonal Support Evaluation List (ISEL), that includes four sub-scales-- appraisal, belonging, self-esteem, and tangible support-- and also provides an overall measure of support (33). A 15-item version of the Inventory of Interpersonal Problems (IIP) was used to assess chronic interpersonal difficulties (34). Sub-scales on the IIP include measures of interpersonal sensitivity (strong affectivity and reactivity in interpersonal settings), interpersonal ambivalence (struggle against others and an inability to join collaboratively with others), and aggression (hostile interpersonal content). We used the Social Problem Solving Inventory-Revised (SPSI-R) (35) to assess participants' perceptions of their social problem-solving ability.
Cognitive Abilities
The MMSE (36) and the Mattis Dementia Rating Scale (DRS) (37) were used to assess global cognition. In addition, we assessed executive functioning with the Executive Interview (EXIT25) (38).
Statistical Analyses
Continuous measures were compared among the three groups using one way analyses of variance (ANOVA); categorical data were compared with chi-square tests. All tests were two-sided. An analysis of covariance (ANCOVA) was conducted to compare the number of errors on the RME with age, gender, education, substance abuse, and DRS scores as covariates. Tukey Honestly Significant Difference (HSD) post-hoc tests were conducted when significant differences were detected among the groups. Within the attempter group, we also examined Spearman correlations between the RME and Social Problem Solving Inventory subscales, cognitive performance, depression, IIP subscales, and lethality of suicide attempt.
Results
Demographic and Clinical Characteristics (see Table 1)
Table 1.
Demographic and Clinical characteristics
| Attempter (A) N=24 |
Non- suicidal depressed (D) N=38 |
Non- psychiatric control (C) N=28 |
F or X2 | df | p | Post hoc | |
|---|---|---|---|---|---|---|---|
| Age | 68.2 (8.7) | 70.2 (7.7) | 69.6 (6.3) | 0.55 | 2,87 | 0.58 | |
| % Men | 38 | 34 | 61 | 5.07 | 2 | 0.08 | |
| % White | 88 | 87 | 89 | 0.92 | 2 | 0.96 | |
| % Married | 42 | 39 | 57 | 2.23 | 2 | 0.33 | |
| Education, yrs | 13.3 (2.1) | 14.5 (3.0) | 14.9 (2.9) | 2.15 | 2,87 | 0.12 | |
| CIRS-G | 7.9 (3.5) | 9.9 (3.6) | 7.0 (2.8) | 5.62 | 2,79 | 0.005 | D>C |
| HRSD-16 | 19.6 (4.7) | 18.2(3.6) | 2.5 (1.9) | 205.81 | 2,86 | 0.0001 | A,D>C |
| Hopelessness | 10.1 (5.5) | 4.6 (4.9) | 1.6 (1.4) | 24.82 | 2,86 | 0.0001 | A>D>C |
| % ATHF strength ≥3 |
39 (n=18) |
31 (n=32) |
na | 0.30 | 1 | 0.58 | |
| MMSE | 28.0 (2.0) | 28.4 (1.6) | 28.1(1.4) | 0.51 | 2,77 | 0.60 | |
| DRS total | 131.0 (7.1) | 134.7 (4.3) | 137.0 (4.1) | 8.26 | 2,81 | 0.0005 | A<D,C |
| EXIT | 9.1 (4.8) | 7.7 (4.1) | 6.2 (2.7) | 2.85 | 2,71 | 0.065 |
ATHF: Antidepressant Treatment History Form, CIRSG: Cumulative Illness rating Scale Geriatrics, EXIT: Executive interview, DRS: Dementia Rating Scale, EXIT: Executive interview, HRSD: Hamilton Rating Scale, Hopelessness: Beck Hopelessness Scale, MMSE: Mini Mental State Exam.
There were no statistical differences among the three groups in age, gender, race, marital status, level of education, MMSE or EXIT scores. There was no significant difference in gender distribution although we note that 61% of the elders with no psychiatric history were men vs. 38% of attempters and 34% of non-suicidal depressed subjects. Attempters had significantly lower DRS scores than the two other groups. Levels of physical illness burden (CIRS-G scores) and intensity of pharmacotherapy for the current episode of depression (ATHF strength) were similar in the two depressed groups. The lifetime prevalences of comorbid anxiety disorders were similar in the two depressed groups (attempters: 16/24 [67%] vs. non-suicidal depressed: 23/38 [61%]). Attempters were more likely to have a history of current substance use disorder than non-suicidal depressed elders (10/24 [42%] vs. 7/38 [18%] non-suicidal depressed, X2=3.99, df = 1, p=0.05). Twenty-three of the 24 attempters and 5 out of 38 depressed controls were originally treated as inpatients.
Suicide attempters reported serious ideation and suicidal intent as indicated by their mean (SD) current suicidal ideation score (18.6 (9.5)) and intent score (15.5 (5.1)); the mean (SD) medical lethality of their suicide attempts was 3.5 (2.0). Fifteen out of the 24 attempters made their first suicide attempt after age 60, in addition, all attempters had current suicidal ideation and an active plan. Fifteen of the 24 attempters had one suicide attempt, 5 made two attempts and 4 made four attempts.
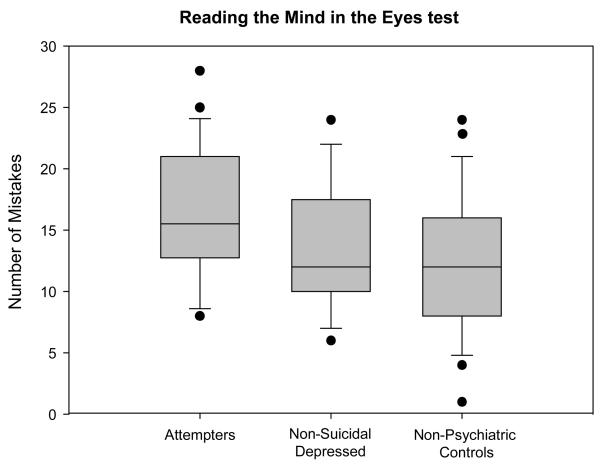
Social Emotion Recognition (see Table 2 and Figure 1)
Table 2.
Social emotion recognition and social functioning
| Attempter (A) N=24 |
Non- suicidal Depressed (D) N=38 |
Non- psychiatric Control (C) N=28 |
F or X2 | df | p | Post hoc | |
|---|---|---|---|---|---|---|---|
| Reading the Mind in the Eyes test errors |
15.7 (5.7) | 13.3 (5.0) | 11.5 (5.1) | 4.25 | 2,87 | 0.017 | A>C |
| SPSI Total | 88.9 (16.2) | 101.8(15.3) | 119.0 (8.7) | 29.74 | 2,81 | 0.0001 | A<D<C |
| SPSI Positive | 91.3 (14.0) | 97.1 (14.6) | 113.4 (11.6) | 18.54 | 2,81 | 0.0001 | A,D<C |
| SPSI Negative | 108.1 (15.1) | 96.9 (11.6) | 88.1 (9.9) | 16.56 | 2,81 | 0.0001 | A>D>C |
| SPSI Rational | 92.9 (15.2) | 98.6 (14.6) | 113.6 (9.5) | 16.76 | 2,81 | 0.0001 | A,D<C |
| SPSI Impulsivity |
106.1 (20.0) | 92.5 (13.3) | 86.0 (9.2) | 12.31 | 2,81 | 0.0001 | A>DC |
| SPSI Avoidance |
108.2 (18.7) | 98.6 (18.2) | 84.1 (7.6) | 14.90 | 2,81 | 0.0001 | A,D>C |
| ISEL Self- esteem |
4.4 (3.1) | 7.5 (2.8) | 9.6 (1.4) | 25.60 | 2,82 | 0.0001 | A<D<C |
| ISEL Appraisal | 8.0 (2.9) | 9.4 (2.3) | 11.2 (1.2) | 13.21 | 2,82 | 0.0001 | A,D<C |
| ISEL Belonging | 6.6 (2.5) | 9.3 (2.6) | 11.0 (1.1) | 24.36 | 2,82 | 0.0001 | A<D<C |
| ISEL Tangible | 7.0 (3.2) | 9.4 (2.4) | 11.5 (0.8) | 22.24 | 2,80 | 0.0001 | A<D<C |
| IIP Sensitive | 6.8 (5.0) | 5.0 (3.3) | 2.4 (2.7) | 9.15 | 2,83 | 0.0001 | A,D>C |
| IIP Ambivalent | 5.6 (4.4) | 2.9 (3.8) | 1.7 (2.4) | 7.57 | 2,82 | 0.001 | A>D,C |
| IIP Aggression | 4.3 (4.0) | 2.9 (2.6) | 1.3 (1.5) | 7.44 | 2,82 | 0.002 | A>C |
| Number of Close Friends+ |
2.5 (2.4) | 3.2 (2.3) | 4.3 (2.2) | 6.26 | 2 | 0.044 | A<C |
| % Participating in Religious Group |
75 | 70 | 64 | 0.47 | 2 | 0.79 | |
| % Doing Volunteer Work |
0 | 30 | 32 | 5.07 | 2 | 0.08 | |
| Proportion of Children with Contact+ |
0.76 (0.28) | 0.96 (0.11) | 0.93 (0.22) | 6.93 | 2 | 0.03 | A<D,C |
| Proportion of Relative with Contact+ |
0.52 (0.44) | 0.64 (0.41) | 0.64 (0.35) | 0.64 | 2 | 0.73 |
Reading the Mind in the Eyes test still significant after controlling for age, gender and education IIP: Inventory of Interpersonal Problems ISEL: Interpersonal Support Evaluation List, SPSI:Social Problem Solving Inventory.
Close friends defined as “people that you feel at ease with, can talk to about private matters, and can call on for help”.
Nonparametric test, Proportion of children or relative with whom the subjects has contact at least once every two weeks (if subject has only 1 child out of 2 with whom she/he has contact at least once every two week, it is 0.5, 1 out of 3 is 0.33, etc.).
Figure 1. Social Emotion Recognition as Measured by the Reading the Mind in the Eyes Test and group status.
Suicide attempters made significantly more mistakes than non-psychiatric controls (F=4.25, df=2,87, p=0.02). The difference remained significant after controlling for age, gender, education, and substance abuse (ANCOVA F=3.68, df=2,83 p=0.03).
One-way ANOVA of error rates on the RME revealed a significant group effect (F= 4.25, df=2,87, p=0.017), with significantly more errors in the suicide attempters compared to non-psychiatric controls (Tukey HSD p=0.05). Non-suicidal depressed participants displayed intermediate performance and did not differ significantly from the other two groups. The difference between attempters and non-psychiatric controls on the RME remained after excluding 2 suicide attempters with possible anoxic/hypoxic brain injury secondary to the suicide attempt (F=5.10, df=2,85, p=0.008). After controlling for age, gender, education, and co-morbid substance use disorders, the group difference remained significant (ANCOVA F=3.68, df=2,83 p=0.03). However, when we also controlled for global cognition measured by the DRS, the group effect became non-significant.
Within the suicide attempters (N=24), we assessed correlations among social emotion recognition and measures of cognitive performance, chronic interpersonal difficulties, depression severity, lethality of suicide attempt, and problem solving abilities. There was a significant correlation between global cognitive performance measured by the DRS and emotion recognition (r=−0.44, p=0.0001), but not with executive performance or with interpersonal difficulties measured by the IIP. There was no correlation between emotion recognition and the severity of depression (measured by the HRSD-16) (r=0.22, p=0.303). Poorer emotion recognition was marginally related to the lethality of the attempt (r=0.39, p=0.05). The association between dysfunctional problem solving (higher levels of negative problem orientation: r=0.42, p=0.059 and impulsive/careless problem solving style: r=0.41, p=0.058) and impaired emotion recognition did not reach statistical significance.
Social Functioning (see Table 2)
There were significant group differences on each of the three subscales of the IIP. Both depressed groups reported higher levels of interpersonal sensitivity than elders with no psychiatric history (F=9,15, df=2,83, p=0.0001, Tukey HSD p=0.05, A,D>C). Levels of interpersonal aggression were higher in suicide-attempters than non-psychiatric comparators (F=7.44, df=2,82, p=0.002, Tukey HSD p=0.05, A>C). Finally, suicide attempters reported greater interpersonal ambivalence than both non-suicidal depressed and non-psychiatric controls (F=7.57, df=2,82, p=0.001, Tukey HSD p=0.05 revealed that A>C,D). The suicide attempters had significantly lower scores than the depressed and non-depressed comparators on the belonging, tangible support, and self-esteem subscales of the ISEL.
The suicide attempters had fewer close friends than the non-psychiatric comparators as measured by the Social Network Index. While the number of children was similar in the three groups, suicide attempters reported less contact with children than both non-suicidal depressed and non-psychiatric elders. None of the attempters participated in volunteer work; in contrast, one third of non-suicidal depressed or non-depressed participants were involved in volunteer activities. The number of participants that engaged in religious groups was similar (approximately two thirds) in each group.
Conclusions
We identified a deficit in the recognition of complex social facial emotions in older suicide attempters compared to non-psychiatric controls. However, this effect could not be disaggregated from reduced global cognition in suicide attempters. The performance of non-suicidal depressed elders was intermediate between the two groups. There were several indicators of poor social functioning in suicide attempters: they reported a pattern of struggle against others, hostility in relationships, and a perceived lack of social support. Also, their social networks were constricted: they were less likely talk to their children, had fewer close friends, and did not do any volunteer work. Thus, attempted suicide in late life seems to be associated with interpersonal relationships that are disruptive rather than supportive and social isolation.
Social emotion recognition, social problem-solving and suicidal behavior
The emotion recognition performance of non-psychiatric controls (11.5/36 errors) was comparable with that reported in younger adults with a mean age of 46.5 (10/36 errors) (22). The performance of older suicide attempters (16/36 errors) was similar to that of young adults with high-functioning autism (mean age: 30, 14/36 errors), but there was no significant difference between the depressed non-suicidal and the attempter groups. Our results extend the findings of Lee and colleagues (20) of impaired performance on the RME in younger individuals with “hopeless, suicidal depression”. Social cognition is a prerequisite for interpersonal cooperation and empathy, and impaired social cognition may cause miscommunication, disrupt interpersonal relationships, and undermine social support. These data are in agreement with our clinical observations that suicidal elders have difficulties in establishing and maintaining relationships, possibly indicating poor social abilities. Emotion recognition ability in the non-suicidal depressed participants fell intermediate between the suicide attempters and the non-psychiatric comparators, and did not differ significantly from either group. One interpretation of this pattern is that, as Lee and colleagues (20) suggested, emotion recognition difficulties are selectively associated with a cognitive dimension of depression, which includes hopelessness and suicidal behavior. Difficulties in recognition of higher-level emotions from facial expressions increase the likelihood of inappropriate emotional and behavioral responses, experiencing social interactions negatively, and may also contribute to emotion dysregulation. In turn, poor communication skills related to difficulties in recognizing emotions contribute to interpersonal problems and maintenance of psychopathology (23, 39).
Suicide attempters demonstrated a reduced cognitive ability on the DRS, and this effect was correlated significantly with the impairment in recognition of facial emotions. Thus, it is likely that impaired emotion recognition is related to global cognitive decline. However, deficits in emotion recognition were not related to anoxic/hypoxic brain injury secondary to the suicide attempt or to age, gender, education or comorbid substance misuse. In other neuropsychiatric disorders, deficits in social cognition are not systematically related to overall cognitive decline but to specific cognitive decline affecting the frontal and temporal lobes (23). Interestingly, in a previous study, deficits in social cognition (including the RME) were seen in cases with frontal variant fronto-temporal dementia (affecting the orbitofrontal cortex), but not in patients with Alzheimer's disease (40). Our cross-sectional study cannot answer the question whether impaired emotion recognition is a stable long-standing risk factor for suicidal behavior that may interact with age-related environmental and socioemotional factors, or whether declining emotion recognition in old age increases suicide risk in late-life.
Social networks, interpersonal problems, social support, and suicidal behavior
It has been suggested that social support networks have a buffering effect, protecting people from the impact of stressors. Our results confirm previous reports of poor interpersonal functioning in elderly suicide attempters compared to both non-suicidal depressed and non-psychiatric elders. This poor interpersonal functioning was indicated by several measures: perceived social support, social network index, and chronic interpersonal difficulties. Attempters reported lower levels of belonging, self-esteem, tangible support, and lower levels of problem-solving abilities than both non-suicidal depressed and non-psychiatric controls. Although the number of children were similar in the three groups, attempters were less likely to be in regular contact with their children than both non-suicidal depressed participants and the non-psychiatric comparators, implying strained relationships with their offspring. Attempters were less likely to have close friends and they did not participate in any volunteer activities. Small social networks, infrequent participation in social activities, and perceived isolation all have been linked to mental health problems in older adults (41, 42). In an older person who has few meaningful relationships, deficits in social cognition and ensuing social problems may be particularly likely to result in suicidal behavior.
Limitations and strengths
The cross-sectional design of our study is a major limitation which precludes causal inferences. Our results suggest that depressed older people who fail to recognize others' emotions experience an accumulation of social problems that, in turn, predispose them to suicidal behavior, although this pathway can only be confirmed in a prospective design. We used a single measure of social cognition (the RME), although previous research has shown this test to correlate with other measures of social cognition (43). Our analyses benefited from comparison groups of both non-suicidal depressed and non-psychiatric elders. Given similar demographic characteristics and medical illness burden in the three groups, observed differences in volunteer activities or in interpersonal contacts cannot be attributed to frailty.
In summary, our findings indicate that impaired social problem solving, constricted social networks, and proneness to conflict (chronic interpersonal difficulties which may lead to lack of perceived social support) are associated with attempted suicide in late-life depression. The deficit in social cognition in the attempters was not statistically significant in comparison to the non-suicidal depressed group, and did not survive controlling for global cognitive decline, thus could be an epiphenomenon of other cognitive deficits related to suicidality. Nevertheless, this constellation of psychological difficulties is likely to hinder interpersonal functioning, leading to conflicts and social isolation. Social cognition deficits may not only heighten suicide risk but may be treatment moderators, and may partly explain why suicidal elders have difficult-to-treat depression (44). This study adds to the growing literature on specific cognitive impairments in younger (5), (45) and older (46) attempters. By identifying cognitive mechanisms that contribute to the accumulation of stressors and to the lack of protective factors in suicidal individuals, we can improve our understanding of the individual diathesis leading to suicidal behavior. In addition, remediating these cognitive deficits by skilled-based interventions could be an important focus of personalized treatment. If social cognition impairments are irreversible, significant others could be made aware of these deficits and family may reduce its impact by compensating for it.
Acknowledgements
Supported by a National Institute of Health K23 grant (MH070471) and an American Foundation for Suicide Prevention Junior Investigator grant to K. Szanto, and the P30 MH71944 and the UPMC Endowment in Geriatric Psychiatry for C. Reynolds.
We are grateful to Professor Baron-Cohen of the Autism Research Centre, University of Cambridge, for providing the Reading the Mind in the Eyes Test.
Clark and Sahakian are affiliated to the Behavioural and Clinical Neuroscience Institute, which is supported by a consortium award from the Medical Research Council (U.K.) and the Wellcome Trust. Clark and Sahakian consult for the Cambridge Cognition. Mulsant currently receives research support from the US National Institute of Mental Health, the Canadian Institutes for Health Research, Bristol-Myers Squibb, and Wyeth. During the past five years, he has also received research support or honoraria from Astra-Zeneca, Eli Lilly, Forest Laboratories, GlaxoSmithKline, Janssen, Lundbeck, and Pfizer. He previously held stocks (all less than $10,000) of Akzo-Nobel, Alkermes, AstraZeneca, Biogen, Celsion, Elan, Eli Lilly, Forest, Orchestra Therapeutics, and Pfizer. Reynolds receives research support in the form of pharmaceutical supplies from Bristol-Myers Squibb, Pfizer, Eli Lilly, and Forest Laboratories.
Footnotes
Conflict of interest:
Szanto, Dombrovski, and Houck do not have any conflict of interest.
References
- 1.Conwell Y, Lyness JM, Duberstein P, et al. Completed suicide among older patients in primary care practices: a controlled study. J Am Geriatr Soc. 2000;48:23–29. doi: 10.1111/j.1532-5415.2000.tb03024.x. [DOI] [PubMed] [Google Scholar]
- 2.Waern M, Rubenowitz E, Runeson B, et al. Burden of illness and suicide in elderly people: case-control study. Bmj. 2002;324:1355. doi: 10.1136/bmj.324.7350.1355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rubenowitz E, Waern M, Wilhelmson K, et al. Life events and psychosocial factors in elderly suicides--a case-control study. Psychological Medicine. 2001;31:1193–1202. doi: 10.1017/s0033291701004457. [DOI] [PubMed] [Google Scholar]
- 4.Keilp JG, Gorlyn M, Oquendo MA, et al. Attention deficit in depressed suicide attempters. Psychiatry Research. 2008;159:7–17. doi: 10.1016/j.psychres.2007.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Keilp JG, Sackeim HA, Brodsky BS, et al. Neuropsychological dysfunction in depressed suicide attempters. American Journal of Psychiatry. 2001;158:735–741. doi: 10.1176/appi.ajp.158.5.735. [DOI] [PubMed] [Google Scholar]
- 6.Dombrovski AY, Butters MA, Reynolds CF, 3rd, et al. Cognitive Performance in Suicidal Depressed Elderly: Preliminary Report. Am J Geriatr Psychiatry. 2008;16:109–115. doi: 10.1097/JGP.0b013e3180f6338d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pollock LR, Williams JM. Problem solving and suicidal behavior. Suicide Life Threat Behav. 1998;28:375–387. [PubMed] [Google Scholar]
- 8.Gibbs LM, Dombrovski AY, Morse J, et al. When the solution is part of the problem: problem solving in elderly suicide attempters. Int J Geriatr Psychiatry. 2009 doi: 10.1002/gps.2276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Beautrais AL. A case control study of suicide and attempted suicide in older adults. Suicide Life Threat Behav. 2002;32:1–9. doi: 10.1521/suli.32.1.1.22184. [DOI] [PubMed] [Google Scholar]
- 10.Turvey CL, Conwell Y, Jones MP, et al. Risk factors for late-life suicide: a prospective, community-based study. American Journal of Geriatric Psychiatry. 2002;10:398–406. [PubMed] [Google Scholar]
- 11.Duberstein PR, Conwell Y, Conner KR, et al. Poor social integration and suicide: fact or artifact? A case-control study. Psychol Med. 2004;34:1331–1337. doi: 10.1017/s0033291704002600. [DOI] [PubMed] [Google Scholar]
- 12.Shamay-Tsoory S, T-E Y, Aharon-Peretz J. The ventromedial prefrontal cortex is involved in understanding affective but not cognitive theory of mind stories. Social Neuroscience. 2006;1:149–166. doi: 10.1080/17470910600985589. [DOI] [PubMed] [Google Scholar]
- 13.Stuss DT, Gallup GG, Jr., Alexander MP. The frontal lobes are necessary for 'theory of mind'. Brain. 2001;124:279–286. doi: 10.1093/brain/124.2.279. [DOI] [PubMed] [Google Scholar]
- 14.Heberlein AS, Padon AA, Gillihan SJ, et al. Ventromedial frontal lobe plays a critical role in facial emotion recognition. J Cogn Neurosci. 2008;20:721–733. doi: 10.1162/jocn.2008.20049. [DOI] [PubMed] [Google Scholar]
- 15.Gregory CA, L S, Stone V, Erzinclioglu S, Martin L, Baron-Cohen S, et al. Theory of mind in patients with frontal variant frontotemporal dementia and Alzheimer's disease: theoretical and practical implications. Brain. 2002;125:752–764. doi: 10.1093/brain/awf079. [DOI] [PubMed] [Google Scholar]
- 16.Lough S, Kipps CM, Treise C, et al. Social reasoning, emotion and empathy in frontotemporal dementia. Neuropsychologia. 2006;44:950–958. doi: 10.1016/j.neuropsychologia.2005.08.009. [DOI] [PubMed] [Google Scholar]
- 17.Arango V, Underwood MD, Mann JJ. Postmorten findings in suicide victims: Implications for in vivo imaging studies. Ann NY Acad Sci. 1997;836:269–287. doi: 10.1111/j.1749-6632.1997.tb52365.x. [DOI] [PubMed] [Google Scholar]
- 18.Jollant F, Lawrence NS, Giampietro V, et al. Orbitofrontal Cortex Response to Angry Faces in Men With Histories of Suicide Attempts. Am J Psychiatry. 2008;165:740–748. doi: 10.1176/appi.ajp.2008.07081239. [DOI] [PubMed] [Google Scholar]
- 19.Oquendo MA, Placidi GP, Malone KM, et al. Positron emission tomography of regional brain metabolic responses to a serotonergic challenge and lethality of suicide attempts in major depression. Arch Gen Psychiatry. 2003;60:14–22. doi: 10.1001/archpsyc.60.1.14. [DOI] [PubMed] [Google Scholar]
- 20.Lee L, Harkness KL, Sabbagh MA, Jacobson JA. Mental state decoding abilities in clinical depression. Journal of Affective Disorders. 2005;86:247–258. doi: 10.1016/j.jad.2005.02.007. [DOI] [PubMed] [Google Scholar]
- 21.Baron-Cohen SJ, Mortimore C, Robertson M. Another advances test of theory of mind: evidence frm very high functioning adults with autism or Asperger Syndrome. Journal of Child Psychology and Psychitry. 1997;38:813–822. doi: 10.1111/j.1469-7610.1997.tb01599.x. [DOI] [PubMed] [Google Scholar]
- 22.Baron-Cohen S, Wheelwright S, Hill J, et al. The “Reading the Mind in the Eyes” Test revised version: a study with normal adults, and adults with Asperger syndrome or high-functioning autism. J Child Psychol Psychiatry. 2001;42:241–251. [PubMed] [Google Scholar]
- 23.Ruffman T, Henry JD, Livingstone V, et al. A meta-analytic review of emotion recognition and aging: implications for neuropsychological models of aging. Neurosci Biobehav Rev. 2008;32:863–881. doi: 10.1016/j.neubiorev.2008.01.001. [DOI] [PubMed] [Google Scholar]
- 24.Harrison KE, Dombrovski AY, Morse JQ, et al. Alone? Perceived social support and chronic interpersonal difficulties in suicidal elders. Int Psychogeriatr. 2010;22:445–454. doi: 10.1017/S1041610209991463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wiktorsson S, Runeson B, Skoog I, et al. Attempted suicide in the elderly: characteristics of suicide attempters 70 years and older and a general population comparison group. Am J Geriatr Psychiatry. 18:57–67. doi: 10.1097/JGP.0b013e3181bd1c13. [DOI] [PubMed] [Google Scholar]
- 26.O'Carroll PW, Berman AL, Maris RW, et al. Beyond the Tower of Babel: a nomenclature for suicidology. Suicide Life Threat Behav. 1996;26:237–252. [PubMed] [Google Scholar]
- 27.Sackeim HA, Haskett RF, Mulsant BH, et al. Continuation pharmacotherapy in the prevention of relapse following electroconvulsive therapy: a randomized controlled trial. JAMA. 2001;285:1299–1307. doi: 10.1001/jama.285.10.1299. [DOI] [PubMed] [Google Scholar]
- 28.Miller MD, Paradis CF, Houck PR, et al. Rating chronic medical illness burden in geropsychiatric practice and research: application of the Cumulative Illness Rating Scale. Psychiatry Res. 1992;41:237–248. doi: 10.1016/0165-1781(92)90005-n. [DOI] [PubMed] [Google Scholar]
- 29.Beck AT, Kovacs M, Weissman A. Assessment of suicidal intention: the Scale for Suicide Ideation. J Consult Clin Psychol. 1979;47:343–352. doi: 10.1037//0022-006x.47.2.343. [DOI] [PubMed] [Google Scholar]
- 30.Beck AT, Shuyler D, Herman I. Development of suicidal intent scales. In: Beck AT, Resnik HLP, Lettieri DJ, editors. The prediction of suicide. Charles Press; Bowie, MD: 1974. pp. 45–56. [Google Scholar]
- 31.Beck AT, Beck R, Kovacs M. Classification of suicidal behaviors: I. Quantifying intent and medical lethality. Am J Psychiatry. 1975;132:285–287. doi: 10.1176/ajp.132.3.285. [DOI] [PubMed] [Google Scholar]
- 32.Cohen S, Doyle WJ, Skoner DP, et al. Social ties and susceptibility to the common cold. Jama. 1997;277:1940–1944. [PubMed] [Google Scholar]
- 33.Cohen S, Mermelstein R, Kamarck T, et al. Measuring the functional components of social support. In: Sarason IG, Sarason B, editors. Social support: Theory, research and applications. The Hague; Martinus Nijhoff: 1985. pp. 73–94. [Google Scholar]
- 34.Morse JQ, Pilkonis PA. Screening for personality disorders. J Personal Disord. 2007;21:179–198. doi: 10.1521/pedi.2007.21.2.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.D'Zurilla TJ, Chang EC, Nottingham EJt, et al. Social problem-solving deficits and hopelessness, depression, and suicidal risk in college students and psychiatric inpatients. J Clin Psychol. 1998;54:1091–1107. doi: 10.1002/(sici)1097-4679(199812)54:8<1091::aid-jclp9>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- 36.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 37.Mattis S. Psychological Assessment Resources. Odessa, FL: 1988. Dementia Rating Scale (DRS) [Google Scholar]
- 38.Royall DR, Mahurin RK, Gray KF. Bedside assessment of executive cognitive impairment: the executive interview. J Am Geriatr Soc. 1992;40:1221–1226. doi: 10.1111/j.1532-5415.1992.tb03646.x. [DOI] [PubMed] [Google Scholar]
- 39.Kornreich C, Philippot P, Foisy ML, et al. Impaired emotional facial expression recognition is associated with interpersonal problems in alcoholism. Alcohol Alcohol. 2002;37:394–400. doi: 10.1093/alcalc/37.4.394. [DOI] [PubMed] [Google Scholar]
- 40.Gregory C, Lough S, Stone V, et al. Theory of mind in patients with frontal variant frontotemporal dementia and Alzheimer's disease: theoretical and practical implications. Brain. 2002;125:752–764. doi: 10.1093/brain/awf079. [DOI] [PubMed] [Google Scholar]
- 41.Cornwell EY, Waite LJ. Social disconnectedness, perceived isolation, and health among older adults. J Health Soc Behav. 2009;50:31–48. doi: 10.1177/002214650905000103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rowe JL, Conwell Y, Schulberg HC, et al. Social support and suicidal ideation in older adults using home healthcare services. Am J Geriatr Psychiatry. 2006;14:758–766. doi: 10.1097/01.JGP.0000218324.78202.25. [DOI] [PubMed] [Google Scholar]
- 43.Torralva T, Kipps CM, Hodges JR, et al. The relationship between affective decision-making and theory of mind in the frontal variant of fronto-temporal dementia. Neuropsychologia. 2007;45:342–349. doi: 10.1016/j.neuropsychologia.2006.05.031. [DOI] [PubMed] [Google Scholar]
- 44.Szanto K, Mulsant BH, Houck P, et al. Occurrence and course of suicidality during short-term treatment of late-life depression. Archives of General Psychiatry. 2003;60:610–617. doi: 10.1001/archpsyc.60.6.610. [DOI] [PubMed] [Google Scholar]
- 45.Jollant F, Bellivier F, Leboyer M, et al. Impaired decision making in suicide attempters. American Journal of Psychiatry. 2005;162:304–310. doi: 10.1176/appi.ajp.162.2.304. [DOI] [PubMed] [Google Scholar]
- 46.Dombrovski AY, C L, Siegle GJ, Butters M, Ichikawa N, Sahakian B, Szanto K. Reward/punishment reversal learning in older suicide attempters. American Journal of Psychiatry. 2010 doi: 10.1176/appi.ajp.2009.09030407. [DOI] [PMC free article] [PubMed] [Google Scholar]