Abstract
Frozen bone-patellar tendon bone allografts are useful in anterior cruciate ligament reconstruction as the freezing procedure kills tissue cells, thereby reducing immunogenicity of the grafts. However, a small portion of cells in human femoral heads treated by standard bone-bank freezing procedures survive, thus limiting the effectiveness of allografts. Here, we characterized the survival rates and mechanisms of cells isolated from rat bones and tendons that were subjected to freeze–thaw treatments, and evaluated the influence of these treatments on the mechanical properties of tendons. After a single freeze–thaw cycle, most cells isolated from frozen bone appeared morphologically as osteocytes and expressed both osteoblast- and osteocyte-related genes. Transmission electron microscopic observation of frozen cells using freeze-substitution revealed that a small number of osteocytes maintained large nuclei with intact double membranes, indicating that these osteocytes in bone matrix were resistant to ice crystal formation. We found that tendon cells were completely killed by a single freeze–thaw cycle, whereas bone cells exhibited a relatively high survival rate, although survival was significantly reduced after three freeze–thaw cycles. In patella tendons, the ultimate stress, Young’s modulus, and strain at failure showed no significant differences between untreated tendons and those subjected to five freeze–thaw cycles. In conclusion, we identified that cells surviving after freeze–thaw treatment of rat bones were predominantly osteocytes. We propose that repeated freeze–thaw cycles could be applied for processing bone-tendon constructs prior to grafting as the treatment did not affect the mechanical property of tendons and drastically reduced surviving osteocytes, thereby potentially decreasing allograft immunogenecity.
Keywords: Allografts, Freeze-thawing, Bone-patellar tendon-bone, Osteocytes
Introduction
Of the knee ligaments, the anterior cruciate ligament (ACL) is most prone to total disruption, which is often followed by repeated episodes of joint instability associated with meniscal injury, increased erosion of joint cartilage, and abnormal osseous metabolic activity (Beynnon et al. 2002). Conservative management of ACL deficiency leads to progressive rotatory instability, meniscal tears, and premature joint degeneration (Barrett 1991). To restore rotatory stability, reconstruction of the ACL is typically performed by a variety of grafting procedures using autografts, allografts, or artificial ligaments. Although autografts are nonimmunogenic and therefore represent a good alternative for the replacement of missing ligaments, allografts have many advantages over autografts, including a lack of donor site morbidity, shorter operation time, and larger grafts are possible (Kleipool et al. 1998). Despite these benefits, viable cells present in allografts are capable of eliciting host immune responses that reduce the effectiveness of ACL reconstruction, and it is unclear what cell types are responsible for the immunoreactivity.
Allografts are transplanted after they are subjected to various processes for reducing antigenicity, sterilization, and preservation. Freezing of tissues at −80°C is generally used for long storage in tissue banks and is also considered to reduce immunogenicity of allografts as tissue cells are killed (Gitelis and Cole 2002; Weyts et al. 2003; Heyligers and Klein-Nulend 2005); however, recent studies have reported that a small portion of bone cells survive in human resected femoral heads after standard bone-bank freezing protocols (Weyts et al. 2003; Heyligers and Klein-Nulend 2005; Simpson et al. 2007). As the detailed characterization of surviving cells in allografts has not been performed, it is important to identify surviving cell types and survival mechanisms during freezing procedures to more effectively target these cells and improve the success of allograft procedures.
During the freezing process, cells undergo injury due to intracellular ice crystal formation and the altered ionic concentrations of solutions (Gage and Baust 1998). Repeated freeze–thaw cycles result in greater tissue destruction than a single freeze–thaw cycle (Gill et al. 1968), due in large part to an increase in cell necrosis (Dilley et al. 1993). We therefore hypothesized that repeated freeze–thaw cycles would reduce the number of surviving cells in allografts, and potentially represents a simple method for reducing immunogenicity. Although we previously reported that a single freeze–thaw cycle did not affect the mechanical properties of tendons (Park et al. 2009), it is unclear how repeated freeze–thaw treatments would affect tendon mechanics and function.
The purpose of this study was to characterize the survival rate and mechanisms of cells from rat bones and tendons that were subjected to repeated freeze–thaw treatments, and evaluate the influence of these treatments on the mechanical properties of tendons.
Materials and methods
Bone preparation
Long bones (femora and tibiae) were harvested from 10-week-old male Wistar rats (Charles River Japan, Yokohama, Japan). Bones from 16 rats were divided into four freeze–thaw (FT) groups: (a) FT0, in which bones were fresh; (b) FT1, in which bones were frozen using an ultra-low temperature freezer (MDF-U581, Sanyo Electric Co., Ltd, Osaka, Japan) and stored at −80°C for 3 weeks; (c) FT2, in which FT1 were thawed at 37°C in for 1 h, and then stored at −80°C for 1 week; and (d) FT3, in which FT2 were subjected to a third thawing and freezing cycle and then stored at −80°C for 1 week.
Isolation and culture of bone cells
For the isolation and culture of bone cells from the FT1 group, frozen bone samples were first thawed at room temperature in a phosphate-buffered saline without Mg2+ and Ca2+ (PBS(−)). Bone samples, including cartilage, were collected by chipping femora and tibiae with scissors. Pieces of bones were then digested twice with collagenase (Wako Pure Chemical Industries, Ltd., Osaka, Japan) in PBS containing Mg2+ and Ca2+ (PBS(+)) at 37°C on a rotary blood mixer for 15 min, as previously described (Mikuni-Takagaki et al. 1995), and a single fraction (Fr) was collected after each digestion to yield Fr 1 and 2. Subsequently, pieces of bones were then consecutively digested three times with collagenase for 20 min, and osteoblastic populations were obtained from each collagenase solution to give Fr 3, 4, and 5. After the collection of Fr 5, osteocyte-rich populations were obtained from the remaining cells by an initial incubation in PBS(−) containing 4 mM EDTA for 15 min to yield Fr 6-1, followed by a 15-min incubation in a collagenase solution for 15 min to give Fr 6-2. This procedure was repeated to yield Fr 7-1 and 7-2. Following the final digestion, cell suspensions were sequentially passed through 100 and 40 μm filters and then cultured in type I collagen-coated culture dishes with alpha-minimum essential medium (α-MEM) supplemented with 5% fetal bovine serum (FBS), 5% calf serum (CS), 0.25 mM ascorbic acid, 100 units/ml penicillin, and 100 μg/ml streptomycin for 1 week at 37°C in a humidified atmosphere containing 5% CO2 (MCO-20AIC, Sanyo Electric Co., Ltd., Osaka, Japan). Adherent bone cells were then observed by phase-contrast microscopy (ECLIPSE TS100, Nikon, Tokyo, Japan) and cell survival frequency (frequency of at least one cell surviving) was then calculated.
Isolation and culture of tendon cells
Patellar tendons (PTs) were collected from both knees of 15 10-week-old male Wistar rats after being freed from surrounding tissues using sharp scissors. The harvested PTs were divided into an FT0 group, which consisted of fresh PTs, and an FT1 group, which consisted of PTs that were frozen using an ultra-low temperature freezer, stored at −80°C for 3 weeks, and then thawed at room temperature in PBS(−). Tendon cells were harvested by collagenase digestion, as previously described (Scutt et al. 2008). Briefly, PTs were rinsed once in PBS(−), diced into small pieces, and then digested in a sterile collagenase solution for either 4, 8, or 18 h at 37°C on a rotary blood mixer at 180 rpm. Following digestion, cell suspensions were sequentially passed through 100 and 40 μm filters, and then cultured in culture dishes with Dulbecco’s Modified Eagle Medium (D-MEM) containing 10% FBS, 50 μg/ml ascorbic acid, 100 units/ml penicillin, and 100 μg/ml streptomycin. After 1 week, PT-derived adherent cells were observed by phase-contrast microscopy and cell survival rate was calculated.
Reverse transcription-polymerase chain reaction (RT–PCR)
To determine the characteristics of surviving cells, cell marker gene expression was analyzed by RT–PCR. Total cellular RNA was first extracted with Trizol Reagent (Invitrogen, Carlsbad, USA) according to the manufacturer’s instructions. To generate cDNA from total RNA, reverse transcription was performed using SuperScriptTM II Reverse Transcriptase (Invitrogen, Carlsbad, USA) (Naruse et al. 2000; Uchida et al. 2007). Expression of the osteoblast-related marker genes alkaline phosphatase (ALP), parathyroid hormone receptor (PTHr), alpha-1 type I collagen (COL1A1), and osteocalcin (OCN) and the osteocyte-related marker genes sclerostin (SOST) and dentin matrix protein-1 (DMP-1) in Fr 5–7 was analyzed by RT–PCR. Newly designed primers were used to amplify OCN, SOST, and DMP-1 (Table 1), and primers designed based on previously published cDNA sequences (Naruse et al. 2004; Uchida et al. 2007) were used for all other target genes. All primers were purchased from Sigma Genosys (Hokkaido, Japan).
Table 1.
Primer pairs used for PCR amplification
| Target gene | Accession no.a | Primer pair sequences (sense/antisense)b | Base pairs | Cycles |
|---|---|---|---|---|
| OCN | X04141 | 5′-TGAGGACCCTCTCTCTGCTC-3′ | 127 | 30 |
| 5′-ACCTTACTGCCCTCCTGCTT-3′ | ||||
| SOST | AF326741 | 5′-CAGCTCTCACTAGCCCCTTG-3′ | 228 | 30 |
| 5′-CTCGGACACGTCTTTGGTGT-3′ | ||||
| DMP-1 | NM_203493 | 5′-AGTTCGATGATGAGGGGATG-3′ | 299 | 30 |
| 5′-AGTCTCGCTCCTGCTTTCCT-3′ |
OCN Osteocalcin, SOST sclerostin, DMP-1 dentin matrix protein-1
aGenbank accession number of the sequences used in designing the primers
bPrimer sequences were designed using BLUEPHIN software (Sigma Genosys, Japan)
RT–PCR was performed under linear conditions, and the following conditions were used for the amplification of all genes: an initial denaturation for 5 min at 94°C, followed by a cycle of denaturation at 94°C for 30 s, a specific annealing temperature (55–60°C) for each pair of primers for 30 s, extension at 72°C for 30 s, followed by a final elongation step of 2 min at 72°C. Amplified PCR products were separated on a 3% agarose gel and stained with ethidium bromide for visualization.
Histological analysis
The cells from fresh and frozen bone were also examined by transmission electron microscopy (TEM). Fresh specimens were pre-fixed with 0.1 M cacodylate buffer containing 4% paraformaldehyde and 2.5% glutaraldehyde, and then post-fixed with 2% osmium tetraoxide in 0.1 M cacodylate buffer and embedded in Quetol 651 resin (Nissin EM Corp., Tokyo, Japan) according to the manufacturer’s instructions. In addition, to evaluate the structure of bone cells in the frozen state, bones were fixed using a freeze-substitution method, as previously described (Park et al. 2009). Briefly, bones were first transferred to acetone containing 2% osmium tetroxide (OsO4) cooled at −80°C, and then stored at −80°C for 1 week. For freeze-substitution, the temperature was elevated stepwise from −20°C for 3 days to 4°C for 3 days. The bones were then added to acetone and washed once with cacodylate buffer at room temperature and embedded in Quetol 651 resin. Cross and longitudinal sections were prepared using an Ultracut UCT ultramicrotome (Leica, Deutsch), stained with 3.5% uranyl acetate and lead citrate, and examined with a transmission electron microscope (Hitachi H-8100; Hitachi, Hitachinaka, Japan).
Mechanical testing of tendons
Bone-patellar tendon-bones (BTBs) from both knees of 24 rats were harvested and divided into three groups: (a) FT0, in which BTBs were fresh; (b) FT1, in which BTBs were frozen using an ultra-low temperature freezer and stored at −80°C for 3 weeks; and (c) FT5, in which BTBs were repeatedly frozen and thawed five times. Immediately prior to testing, all BTBs were allowed to thaw at room temperature in PBS for 3 h. For mechanical testing, we analyzed eight BTB specimens in each group as previously described (Park et al. 2009). Briefly, tendons of BTBs from each group were trimmed to 1 mm in width and their free length was measured using a micrometer caliper. The cross-sectional areas of the tendons were calculated by measuring the width and thickness. The BTB specimens were then mounted using a 27-gauge injection needle in a specially designed device containing resin (OSTRON II; GC Dental Products Corp., Aichi, Japan) to maintain 30° of flexion to the patellar tendon in the sagittal plane and to fix the axis of loading to match that of the patellar tendon. The specimens were tested to failure on a universal testing machine at a strain rate of 9 mm/min, with force detected using a load cell (Showa Measuring Instruments Inc., Tokyo, Japan) with a maximum capacity of 50 N to obtain load deformation curves. Stress–strain curves were then calculated from the load-deformation curves. The mode of failure was noted as a break at the mid-substance of the tendon, because nearly all rat patellar tendons were broken at mid-substance under our experimental conditions, regardless of the number of freeze–thaw cycles, strain rate, and temperature. Ultimate stress, Young’s modulus, and strain at failure were obtained from the stress–strain curves. Ultimate stress was defined as the peak force of the stress–strain curves, while Young’s modulus was calculated using the most linear portion of the failure curve.
Statistical analysis
A multiple comparison test based on Ryan’s method was used to evaluate significant differences among survival rates of the three groups. The significance level was set at 0.008 in this study. To compare the mechanical properties of the tendons between the three groups, statistical assessment was performed using one-way analysis of variance (ANOVA) with Tukey’s multiple test. A P value of <0.05 was considered statistically significant.
Results
Cell morphology of cells isolated from bone
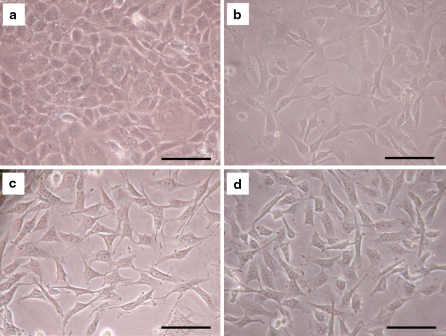
After the isolation of bone cells from femora and tibiae of 10-week-old male Wistar rats, we examined adherent cells to type I collagen-coated culture dishes by phase-contrast microscopy (Fig. 1). The cells in Fr 5, 6, and 7 that were isolated from bone samples without freeze–thaw treatment (FT0) showed two types of morphologies. Approximately half of the cells displayed an osteoblastic morphology and appeared spherical to slightly flattened, which when assembled, appeared cuboidal and displayed a cobble-stone pattern (Fig. 1a). The other type of adherent cells showed osteocytic morphology with a high cytoplasm-to-nucleus ratio, and developed extensive radial cell processes and contacted adjacent cells (Fig. 1b). In Fr 5, 6, and 7, which were obtained from cell suspensions subjected to either one or two freeze–thaw cycles (FT1 and 2, respectively), nearly all cells had a similar morphology to the osteocytic cell type in Fr 5, 6, and 7 isolated from FT0 (Fig. 1c, d).
Fig. 1.
Cell morphology of cells isolated from rat femoral and tibial bones. Phase-contrast microscopic images of isolated bone cells from two freeze–thaw (FT) treatment groups. a Osteoblastic cells in FT0, b osteocytic cells in FT0, c osteocytic cells in FT1. d Osteocytic cells in FT3. The scale bars indicate 100 μm
Expression of osteoblast- and osteocyte-related marker genes
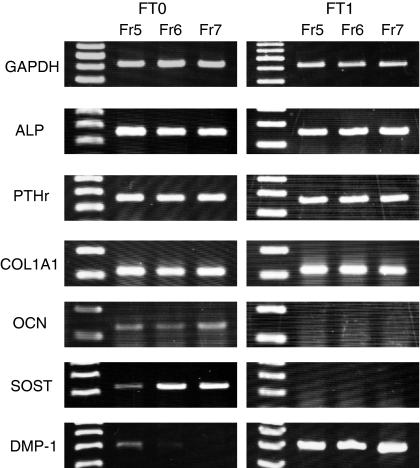
To further characterize the isolated adherent bone cells, the expression of cell-marker genes was analyzed by RT–PCR. The bone cells in Fr 5, 6, and 7 isolated from FT0 expressed several osteoblast-related marker genes, including ALP, PTHr, COL1A1, and OCN (Fig. 2). These cells also expressed the osteocyte-related gene SOST. The expression of DMP-1 was detected in Fr 5 isolated from FT0. The cells in Fr 5, 6, and 7 isolated from FT1 expressed ALP, PTHr, COL1A1, and DMP-1, but the expression of OCN and SOST was not detected. Our preliminary data showed that expression of OCN and SOST increased in a cell density-dependent manner, whereas higher expression levels of DMP-1 were observed at lower cell densities (data not shown).
Fig. 2.
Expression of osteoblast- and osteocyte-related marker genes. RT–PCR was used to analyze the expression of the indicated cell-marker genes in bone cells isolated in fraction (Fr) 5–7 from the freeze–thaw (FT) groups FT0 and FT1. GAPDH, glyceraldehydes-3-phosphate dehydrogenase; ALP alkaline phosphatase, PTHr parathyroid hormone receptor, COL1 alpha-1 type I collagen, OCN osteocalcin, SOST sclerostin, and DMP-1 dentin matrix protein 1
TEM of bone cells
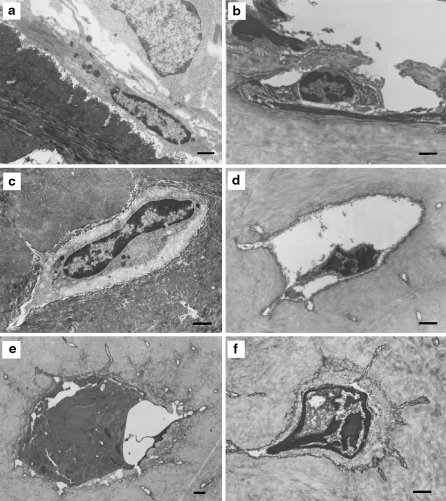
In an attempt to reveal the survival mechanisms of cells in frozen bone tissue, we next observed the cell morphology of isolated osteoblasts and osteocytes in fresh and frozen states using TEM (Fig. 3). In a fresh state, osteoblasts were flattened along bone surfaces and nuclei located at the distal end of cells could be observed (Fig. 3a). In addition, their cytoplasm contained abundant rough endoplasmic reticulum and numerous free ribosomes and mitochondria were also detected. After subjecting osteoblasts to freeze-substitution, nearly all frozen cells were shrunk and contained condensed chromatin granules densely arranged around the inner rim of the nuclear membrane (Fig. 3b). In these cells, the nuclear envelope and cytoplasmic membrane appeared broken down and disrupted.
Fig. 3.
Transmission electron microscopic images of bone cells in fresh and frozen states. a Osteoblastic cell in a fresh state. b Osteoblastic cell in a frozen state. c Osteocytic cell in a fresh state. d–f Osteocytic cells in a frozen state. The scale bars indicates 1 μm
In contrast to osteoblasts, freshly isolated osteocytes appeared more rounded with relatively large nuclei (Fig. 3c). Cell organelles, such as lysosomes and rough endoplasmic reticulum were clearly observed. In the frozen state, numerous shrunken osteocytes contained condensed chromatin granules that were arranged densely at the inner rim of the nuclear membrane, similar to osteoblasts, but the distribution was more sparse and typically located in the center of the nucleus (Fig. 3d). In addition, a number of frozen cells had nuclear envelopes that were disrupted and clearly destroyed. However, several cells maintained relatively large nuclei without cytoplasmic shrinkage, and double layers of nuclear membrane without any interruption were also observed.
Effect of freeze–thaw cycle number on cell survival rate in bone and tendons
Following the isolation and culture of cells from rat femora and tibiae, it was confirmed that surviving cells were present in all fractions from each of the eight bone samples in the FT0 group (8/8) (Table 2). Upon a single freeze–thaw treatment, however, the cell survival rate in Fr 1 from FT1 (2/8) was significantly lower compared with Fr 1 from FT0 (8/8) (P < 0.008). An additional cycle of freeze–thawing further reduced the cell survival rate, with no viable cells observed in Fr 1 (0/8) and only limited survival in Fr 2 (2/8) from FT2 (P < 0.008). The cell survival rate in Fr 3 to 7 from FT2 also decreased, however, the differences were not statistically significant from Fr 3 to 7 of the FT0 group. Subjecting the isolated bone cells to a third round of freeze–thawing drastically reduced the cell survival rate, as all fractions from FT3 showed significantly decreased survival compared with FT0 (P < 0.008) and no detectable surviving cells in the first three fractions (Fr 1–3; 0/0).
Table 2.
Effect of freeze-thaw cycle number on cell survival rate in bone
| Fr 1 | Fr 2 | Fr 3 | Fr 4 | Fr 5 | Fr 6 | Fr 7 | |
|---|---|---|---|---|---|---|---|
| FT0 | 8/8 | 8/8 | 8/8 | 8/8 | 8/8 | 8/8 | 8/8 |
| FT1 | 2/8* | 8/8 | 8/8 | 8/8 | 8/8 | 8/8 | 8/8 |
| FT2 | 0/8* | 2/8* | 3/8 | 3/8 | 3/8 | 4/8 | 3/8 |
| FT3 | 0/8* | 0/8* | 0/8* | 1/8* | 1/8* | 2/8* | 2/8* |
FT Freeze–thaw, Fr fraction
*Nominal significance level for FT0 (P < 0.008)
Finally, the survival of cells harvested from tendons in the FT0 and FT1 were compared after variable incubation times after freeze–thaw treatment (Table 3). Similar to the isolated bone cells, while tendon-derived adherent cells were observed in all samples of the FT0 group, no adherent cells in the FT1 group were detected after 4-, 8-, or 18-h incubation periods (Table 3).
Table 3.
Effect of a single freeze–thaw cycle on cell survival rate in tendons
| Group | Incubation time (h) | ||
|---|---|---|---|
| 4 | 8 | 18 | |
| FT0 | 5/5 | 5/5 | 5/5 |
| FT1 | 0 | 0 | 0 |
FT Freeze–thaw
Mechanical properties of tendons
To compare the effects of freeze–thawing on the mechanical properties of tendons, BTB samples from the three freeze–thaw treatment groups were assayed by the tensile failure test (Table 4). Tendon failure in all BTB samples occurred at the mid-substance under our experimental conditions. The ultimate stress, Young’s modulus profiles, and strain at failure showed no significant differences among the FT0, FT1, and FT5 groups.
Table 4.
Mechanical properties of tendons subjected to freeze–thaw treatment
| Group | Number of samples | Ultimate stress (MPa) | Young’s modulus (MPa) | Strain at failure (%) |
|---|---|---|---|---|
| FT0 | 8 | 42.6 ± 16.3 | 206.8 ± 99.2 | 22.0 ± 4.8 |
| FT1 | 8 | 30.7 ± 17.8 | 185.0 ± 119.4 | 17.4 ± 4.1 |
| FT5 | 8 | 46.1 ± 17.9 | 211.4 ± 108.3 | 23.8 ± 4.9 |
FT freeze thaw
All values are presented as the mean ± SD
Discussion
We examined the survival rate of cells isolated from rat bones and tendons that were subjected to freeze–thaw treatment. Results showed that tendon cells were completely killed by a single freeze–thaw cycle, whereas bone cells exhibited a relatively high survival rate, although the cell survival rate was significantly reduced after three freeze–thaw cycles. Nearly all cells isolated from femora and tibiae after a single freeze–thaw cycle appeared morphologically as osteocytes and expressed both osteoblast- and osteocyte-related genes. TEM images of freeze-substituted bone revealed that a number of osteocytes maintained large intact nuclei and cytoplasm, indicating that a portion of osteocytes in bone matrix were resistant to ice crystal formation. In addition, although tendon cells were completely killed after freezing, five consecutive freeze–thaw cycles did not affect the mechanical properties of tendons.
Previous studies have shown that freshly frozen human femoral head allografts contain viable cells upon thawing that are morphologically indistinguishable from those cultured from freshly harvested trabecular bone, and display similar mRNA profiles with respect to osteoblast-related gene expression (Simpson et al. 2007). In our present investigation involving femoral and tibial bones from Wistar rats, surviving cells could be cultured from freshly frozen bone. Nearly all of the isolated cells were morphologically characterized as osteocytes and were indistinguishable from fresh bone-derived osteocytic cells. Although the cells isolated from frozen bone expressed both osteoblast- and osteocyte-related genes, the expression of OCN, DMP-1, and SOST was only observed in cells isolated from untreated bone samples. Expression profiles of OCN, DMP-1 and SOST may be affected by cell density rather than cell phenotype, because cell survival rates decrease with freeze–thawing treatment. Our results suggest that not only osteoblasts, but also osteocytes, survive in freeze–thawed bone.
Moreover, we also examined cell morphology in the frozen state to reveal the survival mechanisms of cells in frozen bone tissue. TEM images of bone cells subjected to a freeze-substitution method revealed that subcellular organelles in many cells were destroyed by ice crystals (Fig. 3). Surprisingly, a small percentage of osteocytes maintained relatively large nuclei with double-layered membranes and intact cell membranes and cytoplasm. Suspended and adherent cells were nearly completely killed by freeze–thawing in the absence of cryoprotectant (Shimada 1977). We speculate that the bone microenvironment, particularly the bone matrix which surrounds osteocytes provides protection from cryoinjury, such as the damage caused by ice crystal formation and salt injury. The importance of the bone matrix for protection is also supported by the fact that no cells survived in tendons after freezing, and indicates the matrix plays a role in the survival mechanism of osteocytes, which were the predominant cells isolated after the freeze–thaw treatment of bone.
Several studies have reported that surviving cells in allograft tissue are potentially immunogenic (Enneking 1957; Chalmers 1959; Langer et al. 1975). For example, Rodeo et al. (2000) reported that class-I and -II major histocompatibility complex antigens persist on cells of a meniscus prepared for transplantation even after two freeze–thaw cycles. It is therefore considered that the complete killing of cells is important for successful allogenic transplantations. Compared to a single freeze–thaw treatment, the repeated freeze–thaw of tissues, including the palate, liver, and skin, is known to produce more extensive and thorough tissue destruction and increase necrosis (Gage and Baust 1998). Here, we found that tendon cells were completely killed by a single freeze–thaw cycle, while bone cells were significantly reduced after three freeze–thaw cycles. Cryobiological research has demonstrated that all parts of the freeze–thaw cycle, particularly the cooling and warming rates, are associated with tissue destruction and cell injury (Gage and Baust 1998). For example, intracellular ice crystal formation is more likely to occur with rapid cooling rates (Gage and Baust 1998). As we have demonstrated that osteocytes survive even after three consecutive freeze–thaw cycles, further investigation is needed to reveal the conditions required for complete disappearance of allograft immunogenicity using freeze–thaw cycles.
The initial strength of tendons used for transplantation is important for successful ACL reconstruction. Several studies have reported that the various procedures used for tendon allograft preparation, such as freezing and irradiation, adversely affect the mechanical properties of tendons (Clavert et al. 2001; Fideler et al. 1995; Noyes and Grood 1976). Conflicting results regarding the effects of cryopreservation on the mechanical properties of tendons have been reported, with several studies stating that mechanical properties are not affected (Nikolaou et al. 1986; Noyes and Grood 1976; Woo et al. 1986), while others have indicated that biomechanical changes did occur (Clavert et al. 2001; Smith et al. 1996). Although we previously found that the mechanical properties of rat tendons subjected to a single freeze–thaw cycle were not significantly different than those of fresh tendons (Park et al. 2009). In the present study, even an additional four freeze–thaw cycles did not significantly decrease the mechanical properties of rat tendons. Our previous study showed that many spaces were present in the interfibrillar substance of tendons, and collagen fibrils were divided and squeezed by these spaces in the frozen state. However, such spaces and ice crystal formation were not observed in freeze–thawed tendons (Park et al. 2009). In addition, we did not observe significant differences in the fibril occupation ratio and cycle length of intraperiodic bands of collagen fibrils between the control and freeze–thawed tendons. Taken together, these results suggest that repeated freeze-thaw cycles may not significantly affect the mechanical properties of tendons.
A number of studies using animal models, including dogs, monkeys, and rats, have shown that mechanical of tendons failure mostly occurs at tibial insertion sites during tensile testing (Clavert et al. 2001; Noyes and Grood 1976; Shino et al. 1984; Su et al. 2008). Our preliminary experiments also revealed that nearly all BTBs failed at tibial insertion sites when the tibial tuberosity was maintained at 0° of flexion to the patellar tendon in the sagittal plane (data not shown). We previously attempted to optimize experimental conditions to evaluate the mechanical properties of tendon substances and found that failure of tendons reproducibly occurred at mid-substance with when the tibial tuberosity was held at 30° of flexion to the patellar tendon in the sagittal plane. Here, we therefore evaluated the effects of repeated freeze-thaw cycles on tendon substances under these previous experimental conditions. In clinical situations, cruciate ligament ruptures occur not only in mid-substance, but also at insertion sites. Thus, further investigation under other experimental conditions may be needed to confirm the applicability of our current findings to clinical situations.
In conclusion, we found that surviving cells in rat femoral and tibial bones subjected to freeze-thawing consisted of not only osteoblasts, but also significant numbers of osteocytes. We demonstrated that tendon cells were completely killed by a single freeze-thaw cycle, while bone cells displayed relatively high survival rates, although survival was significantly reduced after three freeze-thaw cycles. Significantly, five consecutive freeze-thaw cycles did not affect the mechanical properties of rat tendons in this experiment.
Acknowledgments
This investigation was supported in part by grants-in-aid from the Ministry of Education, Sports, Culture, Science, and Technology of Japan and by grants-in-aid from the Ministry of Health, Labour, and Welfare, Japan for Research on Human Genome, Tissue Engineering, and Food Biotechnology to M. I.. This research was also supported by grants-in-aid from the Ministry of Education, Sports, Culture, Science, and Technology of Japan to K. N. and K. U., and by research grants from the Parents’ Association of Kitasato University School of Medicine, the Nakatomi Foundation, and SDS Inc. to K. N.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
References
- Barrett DS. Proprioception and function after anterior cruciate reconstruction. J Bone Joint Surg Br. 1991;73:833–837. doi: 10.1302/0301-620X.73B5.1894677. [DOI] [PubMed] [Google Scholar]
- Beynnon BD, Johnson RJ, Fleming BC, Kannus P, Kaplan M, Samani J, Renstrom P. Anterior cruciate ligament replacement comparisn of bone-patellar tendon-bone grafts with two-strand hamstring grafts. A prospective, randomized study. J Bone Joint Surg Am. 2002;84A:1503–1513. doi: 10.2106/00004623-200209000-00001. [DOI] [PubMed] [Google Scholar]
- Chalmers J. Transplantation immunity in bone homografting. J Bone Joint Surg Br. 1959;41-B:160–179. doi: 10.1302/0301-620X.41B1.160. [DOI] [PubMed] [Google Scholar]
- Clavert P, Kempf JF, Bonnomet F, Boutemy P, Marcelin L, Kahn JL. Effects of freezing/thawing on the biomechanical properties of human tendons. Surg Radiol Anat. 2001;23:259–262. doi: 10.1007/s00276-001-0259-8. [DOI] [PubMed] [Google Scholar]
- Dilley AV, Dy DY, Warlters A, Copeland S, Gillies AE, Morris RW, Gibb DB, Cook TA, Morris DL. Laboratory and animal model evaluation of the Cryotech LCS 2000 in hepatic cryotherapy. Cryobiology. 1993;30:74–85. doi: 10.1006/cryo.1993.1007. [DOI] [PubMed] [Google Scholar]
- Enneking WF. Histological investigation of bone transplants in immunologically prepared animals. J Bone Joint Surg Am. 1957;39-A:597–615. [PubMed] [Google Scholar]
- Fideler BM, Vangsness CT, Jr, Lu B, Orlando C, Moore T. Gamma irradiation: effects on biomechanical properties of human bone-patellar tendon-bone allografts. Am J Sports Med. 1995;23:643–646. doi: 10.1177/036354659502300521. [DOI] [PubMed] [Google Scholar]
- Gage AA, Baust J. Mechanisms of tissue injury in cryosurgery. Cryobiology. 1998;37:171–186. doi: 10.1006/cryo.1998.2115. [DOI] [PubMed] [Google Scholar]
- Gill W, Fraser J, Carter DC. Repeated freeze-thaw cycles in cryosurgery. Nature. 1968;219:410–413. doi: 10.1038/219410a0. [DOI] [PubMed] [Google Scholar]
- Gitelis S, Cole BJ. The use of allografts in orthopaedic surgery. Instr Course Lect. 2002;51:507–520. [PubMed] [Google Scholar]
- Heyligers IC, Klein-Nulend J. Detection of living cells in non-processed but deep-frozen bone allografts. Cell Tissue Bank. 2005;6:25–31. doi: 10.1007/s10561-005-1089-4. [DOI] [PubMed] [Google Scholar]
- Kleipool AE, Zijl JA, Willems WJ. Arthroscopic anterior cruciate ligament reconstruction with bone-patellar tendon-bone allograft or autograft. A prospective study with an average follow up of 4 years. Knee Surg Sports Traumatol Arthrosc. 1998;6:224–230. doi: 10.1007/s001670050104. [DOI] [PubMed] [Google Scholar]
- Langer F, Czitrom A, Pritzker KP, Gross AE. The immunogenicity of fresh and frozen allogeneic bone. J Bone Joint Surg Am. 1975;57:216–220. [PubMed] [Google Scholar]
- Mikuni-Takagaki Y, Kakai Y, Satoyoshi M, Kawano E, Suzuki Y, Kawase T, Saito S. Matrix mineralization and the differentiation of osteocyte-like cells in culture. J Bone Miner Res. 1995;10:231–242. doi: 10.1002/jbmr.5650100209. [DOI] [PubMed] [Google Scholar]
- Naruse K, Mikuni-Takagaki Y, Azuma Y, Ito M, Oota T, Kameyama K, Itoman M. Anabolic response of mouse bone-marrow-derived stromal cell clone ST2 cells to low-intensity pulsed ultrasound. Biochem Biophys Res Commun. 2000;268:216–220. doi: 10.1006/bbrc.2000.2094. [DOI] [PubMed] [Google Scholar]
- Naruse K, Urabe K, Mukaida T, Ueno T, Migishima F, Oikawa A, Mikuni-Takagaki Y, Itoman M. Spontaneous differentiation of mesenchymal stem cells obtained from fetal rat circulation. Bone. 2004;35:850–858. doi: 10.1016/j.bone.2004.05.006. [DOI] [PubMed] [Google Scholar]
- Nikolaou PK, Seaber AV, Glisson RR, Ribbeck BM, Bassett FH., III Anterior cruciate ligament allograft transplantation. Long-term function, histology, revascularization, and operative technique. Am J Sports Med. 1986;14:348–360. doi: 10.1177/036354658601400502. [DOI] [PubMed] [Google Scholar]
- Noyes FR, Grood ES. The strength of the anterior cruciate ligament in humans and Rhesus monkeys. J Bone Joint Surg Am. 1976;58:1074–1082. [PubMed] [Google Scholar]
- Park HJ, Urabe K, Naruse K, Onuma K, Nemoto N, Itoman M. The effect of cryopreservation or heating on the mechanical properties and histomorphology of rat bone-patellar tendon-bone. Cell Tissue Bank. 2009;10:11–18. doi: 10.1007/s10561-008-9109-9. [DOI] [PubMed] [Google Scholar]
- Rodeo SA, Seneviratne A, Suzuki K, Felker K, Wickiewicz TL, Warren RF. Histological analysis of human meniscal allografts. A preliminary report. J Bone Joint Surg Am. 2000;82-A:1071–1082. doi: 10.2106/00004623-200008000-00002. [DOI] [PubMed] [Google Scholar]
- Scutt N, Rolf CG, Scutt A. Tissue specific characteristics of cells isolated from human and rat tendons and ligaments. J Orthop Surg Res. 2008;3:32. doi: 10.1186/1749-799X-3-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shimada K (1977) Effect of cryoprotective addictives on intracellular ice formation and survival in very rapidly cooled Hela cells. Contrib Inst Low Temp Sci 19:49–70
- Shino K, Kawasaki T, Hirose H, Gotoh I, Inoue M, Ono K. Replacement of the anterior cruciate ligament by an allogeneic tendon graft. An experimental study in the dog. J Bone Joint Surg Br. 1984;66:672–681. doi: 10.1302/0301-620X.66B5.6501359. [DOI] [PubMed] [Google Scholar]
- Simpson D, Kakarala G, Hampson K, Steele N, Ashton B. Viable cells survive in fresh frozen human bone allografts. Acta Orthop. 2007;78:26–30. doi: 10.1080/17453670610013385. [DOI] [PubMed] [Google Scholar]
- Smith CW, Young IS, Kearney JN. Mechanical properties of tendons: changes with sterilization and preservation. J Biomech Eng. 1996;118:56–61. doi: 10.1115/1.2795946. [DOI] [PubMed] [Google Scholar]
- Su WR, Chen HH, Luo ZP. Effect of cyclic stretching on the tensile properties of patellar tendon and medial collateral ligament in rat. Clin Biomech (Bristol., Avon.) 2008;23:911–917. doi: 10.1016/j.clinbiomech.2008.04.002. [DOI] [PubMed] [Google Scholar]
- Uchida K, Urabe K, Naruse K, Ujihira M, Mabuchi K, Itoman M. Comparison of the cytokine-induced migratory response between primary and subcultured populations of rat mesenchymal bone marrow cells. J Orthop Sci. 2007;12:484–492. doi: 10.1007/s00776-007-1159-5. [DOI] [PubMed] [Google Scholar]
- Weyts FA, Bos PK, Dinjens WN, van Doorn WJ, van Biezen FC, Weinans H, Verhaar JA. Living cells in 1 of 2 frozen femoral heads. Acta Orthop Scand. 2003;74:661–664. doi: 10.1080/00016470310018162. [DOI] [PubMed] [Google Scholar]
- Woo SL, Orlando CA, Camp JF, Akeson WH. Effects of postmortem storage by freezing on ligament tensile behavior. J Biomech. 1986;19:399–404. doi: 10.1016/0021-9290(86)90016-3. [DOI] [PubMed] [Google Scholar]