Abstract
The expression and physiology of purine receptors of the human blood–brain barrier endothelial cells were characterised by application of molecular biological, gene-silencing and Ca2+-imaging techniques to hCMEC/D3 cells. Reverse transcription polymerase chain reaction showed the expression of the G-protein-coupled receptors P2Y2-, P2Y6-, P2Y11- as well as the ionotropic P2X4-, P2X5- and P2X7-receptors. Fura-2 ratiometry revealed that adenosine triphosphate (ATP) or uridine triphosphate (UTP) mediated a change in the intracellular Ca2+ concentration ([Ca2+]i) from 150 to 300 nM in single cells. The change in [Ca2+]i corresponded to a fourfold to fivefold increase in the fluorescence intensity of Fluo-4, which was used for high-throughput experiments. Pharmacological dissection using different agonists [UTPγS, ATPγS, uridine diphosphate (UDP), adenosine diphosphate (ADP), BzATP, αβ-meATP] and antagonist (MRS2578 or NF340) as well as inhibitors of intracellular mediators (U73122 and 2-APB) showed a PLC-IP3 cascade-mediated Ca2+ release, indicating that the nucleotide-induced Ca2+ signal was mainly related to P2Y2, 6 and 11 receptors. The gene silencing of the P2Y2 receptor reduced the ATP- or UTP-induced Ca2+ signal and suppressed the Ca2+ signal mediated by P2Y6 and P2Y11 more specific agonists like UDP (P2Y6), BzATP (P2Y11) and ATPγS (P2Y11). This report identifies the P2Y2 receptor subtype as the main purine receptor involved in Ca2+ signalling of the hCMEC/D3 cells.
Keywords: P2 receptors, G-Protein, Neurovascular unit, Gene silencing, siRNA
Introduction
The endothelial cells which line the microvasculature of the central nervous system (CNS) form a dynamic interface between the blood tissue and the brain parenchyma. They are responsible for the maintenance of ionic and metabolic homeostasis in the brain [1, 2]. They differ fundamentally from other endothelia by the presence of tight junctions which allow them to constitute the blood–brain barrier (BBB), a highly selective dam between the blood and the brain parenchyma [3]. To supply the brain with nutrients while maintaining the selective barrier function, the endothelial cells express active transport systems for ions and nutrients, such as glucose and amino acids, and transporters which are responsible for the removal of metabolic wastes from the brain parenchyma into the blood circulation. The transport across the BBB endothelial cells is controlled by inputs from the nervous tissue as well as the blood [4, 5]. These inputs reach the endothelial cells in form of neurotransmitters, hormones and cytokines which bind to specific receptors expressed at the plasma membrane of the endothelial cells [4, 6]. This functional interaction between the neurons, the glial cells, the endothelial cells and the blood tissue has established the concept of the neurovascular unit [2, 7]. This concept refers also to recent observations that pathophysiological processes, such as inflammation in the BBB, are associated with pathologies such as stroke or neurodegenerative diseases [8, 9].
Purinergic signalling was identified as a very important signalling system for the normal function of the neurovascular unit [4], where purine receptors participate in regulation of vasodilatation and are involved in inflammatory reactions [10]. On one side (abluminal), the purine receptors of the endothelial cells could be stimulated by a release of purines or pyrimidines like adenosine triphosphate (ATP) or uridine triphosphate (UTP) from astrocytes in response to stimulation by neurons [11, 12]. On the other (luminal) side, purine receptors of the endothelial cells could be stimulated by the agonists released from blood cells. Moreover, it was shown that pathophysiological conditions, such as inflammatory processes, could affect the ATP release at either side of the endothelial cells. This increase of ATP release could result in a pathological stimulation of the purinergic signalling of the BBB endothelial system [13, 14].
The family of purine receptors are membrane-bound receptors for extracellular nucleosides (P1-receptors) or nucleotides such as ATP or UTP (P2-receptors). The P2-receptors are subdivided into P2X receptors which are ligand-gated ion channels and G-protein-coupled P2Y receptors with seven transmembrane regions [15–17]. The binding of ATP to the ionotropic P2X receptors allows the flux of cations (mainly Na+ and Ca2+) across the membrane. The different P2Y receptors are activated by di- or triphosphates of the nucleosides adenosine and uridine in varying orders of potency. The P2Y1, 11, 12 and 13 receptors respond mainly to adenine nucleotides, the P2Y2 and P2Y4 receptors respond equally to adenine and uracil nucleotides, the P2Y6 receptor subtype is predominantly sensitive to uracil nucleotides, while P2Y14 is stimulated mainly by uridine diphosphate (UDP)-glucose [18]. The P2Y1, 2, 4, 6 and 11 receptor subtypes are coupled to PLC via Gq/11 proteins located at the intracellular side of the membrane, resulting in an IP3-mediated Ca2+ release from internal stores. The P2Y11 also mediates stimulation of adenylyl cyclase (AC) via Gs protein. The P2Y12, 13 and 14 subtypes are linked to AC inhibition via Gi protein [18, 19]. The expression pattern of the purine receptors is species and cell characteristic and seems to be controlled by various physiological states of the tissue [20]. The expression of purine receptors was shown in primary cultivated rat BBB endothelial cells by Ca2+ measurements. The Ca2+ signalling was probably related to the stimulation of the P2Y2 receptor and, to a minor extent, to the activation of the P2Y1 receptor subtype. The P2Y1 receptor-mediated Ca2+ release was not related to the IP3 cascade [21, 22]. Reverse transcription polymerase chain reaction (RT-PCR) experiments could identify mRNA for P2Y1, 2, 4 and 6 [23] in primary rat BBB endothelial cells.
The goal of this report was to characterise the functional expression of the purine receptors in human BBB endothelial cells using hCMEC/D3, a human brain endothelial cell line which recapitulates most of the unique properties of brain endothelium with respect to the transport processes, permeability and pharmacology [24]. At the mRNA level, P2X4, 5 and 7 as well as P2Y2, 6 and 11 were identified. When stimulated, the cells responded with a Ca2+ signal. Pharmacological and gene-silencing experiments showed that this Ca2+ signal was exclusively related to the P2Y2 receptor subtype.
Materials and methods
Chemicals
If not otherwise stated, all chemicals were obtained from Sigma-Aldrich (Taufkirchen, Germany).
Cell culture
The human hCMEC/D3 cells were cultivated as previously described [24]. Briefly, we used EBM-2 medium (Lonza, Basel, Switzerland) supplemented with 5% foetal calf serum, 1.4 μM hydrocortisone, 5 μg/ml ascorbic acid, 10 mM HEPES, 1 ng/ml bFGF and chemically defined lipid concentrate (Invitrogen GmbH, Karlsruhe, Germany) diluted at 1:100. The cells were placed in a cell culture incubator in which a humidified atmosphere composed of 95% air and 5% CO2 at 37°C was maintained. The culture medium was changed every 2–3 days. For experiments, hCMEC/D3 cells up to passage 37 were used.
For the calcium imaging, glass cover slips were coated with rat collagen-1 and placed in a 24 multiwell plate (150 μg/ml, Trevigen, Gaithersburg, USA). After washing with H2O, cells (6 × 105 cells/well) were added and cultivated in 1 ml culture medium as described above. The Ca2+-imaging experiments were performed 2–3 days after plating when the cells were about 75% confluent.
Measurement of [Ca2+]i
The intracellular Ca2+ concentration was measured using the Fura-2 ratiometric method as previously described [25, 26]. This method allowed us an estimation of [Ca2+]i in single cells but was not efficient for high-throughput experiments. Therefore, [Ca2+]i was measured using the Fluo-4 AM dye (Invitrogen). A dye loading mixture was produced by the addition of 1 μl of a 2 mM Fluo-4 AM (Invitrogen) stock solution dissolved in dimethyl sulfoxide (DMSO), 1 μl of 20% pluronic acid F-127 (Invitrogen) dissolved in DMSO, and 500 μl of a bath solution composed of (in mM) 121 NaCl, 5 KCl, 6 NaHCO3, 5.5 glucose, 0.8 MgCl2, 1.8 CaCl2 and 25 HEPES (pH 7.4). A cover slip covered with adherent cells was transferred into the loading mixture and incubated in a cell culture incubator at 37°C for 60 min. After loading, the cells were washed twice with fresh bath solution to remove external Fluo-4 AM. The dye-loaded cells were transferred into a superfusion chamber mounted on an inverted Nikon Eclipse TE2000-E confocal laser scanning microscope with a 10× objective (Nikon, Düsseldorf, Germany). The intracellular dye was excited with an argon-ion laser at 488 nm, and the emitted fluorescence was registered at 515 nm. For each experiment, 300 images were recorded at 1 Hz. The respective agonists were applied 10 s after the beginning of recording. The images were recorded and conserved using the software EZ-C1 3.50 (Nikon) for later analysis with the software Image J.
For evaluation of single experiments, we defined the measured cells as regions of interest (ROIs). The average intensity of the first ten images was generated using the z-project (http://rsbweb.nih.gov/ij/docs/menus/image.html#stacks). To this average image, an automatic adjustment of the brightness and contrast was applied (http://rsbweb.nih.gov/ij/docs/menus/image.html#adjust) to generate an image where all Fluo-4-loaded cells could be easily recognised. Using the ROI Manager and the elliptical tool (http://rsbweb.nih.gov/ij/docs/menus/analyze.html#manager), up to 100 cells were randomly marked as ROI. To measure the fluorescence intensity of the cells, a multi-measurement was executed for the marked ROI in all 300 images of the respective experiments giving intensity values for each ROI in each image of the experiment. These data were imported in Excel (Microsoft) and Origin (OriginLab) for further calculation, evaluation and graphic representation of the fluorescence intensities. For each cell, the fluorescence intensities measured during the 300 s were normalised to the average of the intensities of the first 10 measured pictures prior the addition of the respective agonists. The results are given as average of at least three independent experiments. For each treatment, 200–300 cells were considered.
P2Y receptor screening
Total RNA from hCMEC/D3 cells (about 2 million cells) was extracted using the Qiagen RNeasy Mini Kit (Qiagen, Hilden, Germany). Genomic DNA was removed by digestion with RNase-free DNase (Fermentas, St. Leon-Rot, Germany) for 60 min at 37°C. First-strand cDNA synthesis of total RNA using the M-MLV RT (Invitrogen) was performed according to manufacturer’s protocols with poly(dT)primer.
cDNA fragments of the various P2Y and P2X receptor subtypes were amplified using a set of self-designed sense and antisense primers (DNA-Star, http://www.dnastar.com) as reported in Table 1. PCR experiments were run on a 96 Universal Gradient PeqStar Thermocycler (PeqLab, Erlangen, Germany) in a final volume of 25 μl containing 50 ng first-strand cDNA as template.
Table 1.
List of the primers used for the RT-PCR
| Target | Primer sequence 5ʹ-3ʹ | Accession no. | Amplicon (bp) | |
|---|---|---|---|---|
| P2RX1 | F | CGTCATCGGGTGGGTGTTTCTCTA | NM_002558 | 400 |
| R | AGGGCGCGGGATGTCGTCA | |||
| P2RX2 | F | GGGCCCCGAGAGCTCCATCATC | NM_012226 | 464 |
| R | GCAGGCAGGTCCAGGTCACAGTCC | |||
| P2RX3 | F | ACTGGCCGCTGCGTGAACTACA | NM_002559 | 522 |
| R | CACGTCGAAGCGGATGCCAAAAG | |||
| P2RX4 | F | CGGCACCCACAGCAACGGAGTCT | NM_002560 | 433 |
| R | TGTATCGAGGCGGCGGAAGGAGTA | |||
| P2RX5 | F | GGCCCCAAGAACCACTACTGC | NM_002561 | 430 |
| R | CCTCGGCCTCCTGGGAACTGTCT | |||
| P2RX6 | F | AGTTGGTGCCCCGTGGAGAGTGG | NM_005446 | 499 |
| R | GTGTGACGGCCGTGGGGATGAG | |||
| P2RX7 | F | CCGGCCACAACTACACCACGAG | NM_002562 | 446 |
| R | GGCCAGACCGAAGTAGGAGAGG | |||
| P2RY1 | F | GGGCCGGCTCAAAAAGAAGAATG | NM_002563 | 505 |
| R | TCCCGCCAAGAAATAGAGAATG | |||
| P2RY2 | F | GCCGTGGCGCTCTACATCTTCTTG | NM_002564 | 546 |
| R | CGAGGTCCCGTAGGCTGGCTTTAG | |||
| P2RY4 | F | TCGGCCTGAAGAGTTTGACCAC | NM_002565 | 412 |
| R | GGGCTTGCCACCACCACAGA | |||
| P2RY6 | F | CCGCCTGGTCCGCTTCCTCT | NM_004154 | 412 |
| R | CTTGCCACGCCGCTCCTG | |||
| P2RY11 | F | GCTGCCGGCTGGGTCCTG | NM_002566 | 427 |
| R | CTGTGGCCTGGGCTATGTCTGC | |||
| P2RY12 | F | CTGGGCATTCATGTTCTTACTCTC | NM_022788 | 509 |
| R | AATTGGGGCACTTCAGCATACT | |||
| P2RY13 | F | TTTGGTGGCCGACTTGATAATGAC | NM_176894 | 415 |
| R | TTTGCCTTCCAGCTTTTTGTTGTT | |||
| P2RY14 | F | AGGGTCTCTGCCGTGCTCTT | NM_014879 | 506 |
| R | GCTTCGGTCTGACTCTTTGTGTAG |
siRNA transfection and quantitative RT-PCR analysis
The human P2Y2 and P2Y6 Silencer Select Validated siRNAs for the gene silencing of the P2Y receptors were obtained from Applied Biosystems (Darmstadt, Germany). siRNA s9966 and s9967 for the human P2Y2 receptor, as well as the siRNA s9972 and s224151 for the human P2Y6 receptor subtype, were tested. The respective target sequences were: s9966 sense 5ʹ-GCUUCAACGAGGACUUCAAtt-3ʹ and s9966 antisense 5ʹ-UUGAAGUCCUCGUUGAAGCgg-3ʹ; s9967 sense 5ʹ-UCUUCUACACCAACCUUUAtt-3ʹ and s9967 antisense 5ʹ-UAAAGGUUGGUGUAGAAGAgg-3ʹ; s9972 sense 5ʹ-CGUGUACACCCUAAACCUUtt-3ʹ and s9972 antisense 5ʹ-AAGGUUUAGGGUGUACACGgc-3ʹ; s224151 sense 5ʹ-GAAGCUCACCAAAAACUAUtt-3ʹ and s224151 antisense 5ʹ-AUAGUUUUUGGUGAGCUUCtg-3ʹ. As control, the Silencer Select Negative Control #2 (neg. siRNA) and the Silencer Select GAPDH siRNA were used.
For silencing the receptors, the hCMEC/D3 cells were transfected by reverse transfection with Lipofectamine 2000 (Invitrogen) in serum-free Opti-MEM medium (Invitrogen). The respective siRNAs were diluted in Opti-MEM medium to achieve a final concentration of 10 nM. The respective siRNA/Lipofectamine complexes were given in tissue culture dishes (Ø 35 mm; Sarstedt, Nümbrecht, Germany) and 2.5–4.0 × 105 cells in EBM-2 culture medium were plated. For control experiments, cells were cultivated in the presence of the transfection reagents without siRNA.
After 48 h, total RNA was isolated with the Qiagen RNeasy Mini Kit (Qiagen). Genomic DNA was removed by digestion with RNase-free DNase at 37°C and for 60 min according to the manufacturer’s protocols (Fermentas). RNA (70 ng) was used in the quantitative RT-PCR amplification. Gene-specific PCR primer pairs for GAPDH, P2Y2, P2Y6 and the housekeeping gene hACTB (Table 2) designed by Primer3, v 0.4.0 (http://frodo.wi.mit.edu/primer3/) were used.
Table 2.
List of the primers used for the quantitative RT-PCR
| Target | Primer sequence 5ʹ-3ʹ | Accession no. | Amplicon (bp) | |
|---|---|---|---|---|
| P2RY2 | F | GGAATTAAGTTTCAAGAAAGG | NM_002564 | 252 |
| R | AACTCAGCCCTCATTACTTAC | |||
| P2RY6 | F | ACCCCATCCTCTTCTACTT | NM_004154 | 258 |
| R | TGAAGAAATAGTTTTTGGTGA | |||
| GAPDH | F | GCTCATTTCCTGGTATGAC | NM_002046 | 274 |
| R | ACAGGGTACTTTATTGATGGT | |||
| ACTB | F | ATATGAGATGCGTTGTTACAG | NM_001101 | 257 |
| R | CAAAAGCCTTCATACATCTC |
The PCR amplification was performed with the Quantace SensiMix SYBR One-Step Kit (Bioline, Luckenwalde, Germany). The amplification was performed in 44 cycles (15 s at 94°C, 15 s at 53°C and 15 s at 72°C). The PCR products were separated on 2% agarose gels and stained with GelRed (Biotium, Hayward, CA, USA).
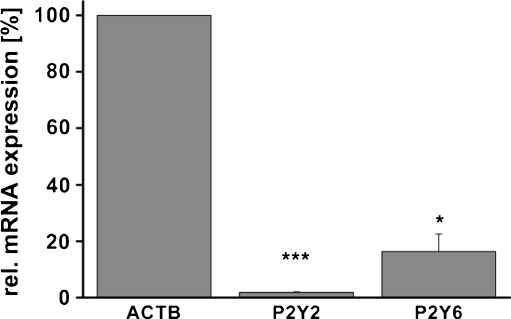
The gene silencing of the P2Y receptors was quantified by the estimation of the 2-ΔΔCT value as described by Schmittgen and Livak [27] and Baier et al. [28]. The amount of the respective mRNA was averaged over three biological and also three technical replicates using the constitutive housekeeping gene hACTB for internal normalisation. Average values were used to calculate relative gene expression levels (2-ΔCT; ΔCT = CTgene-CThACTB). The results presented in Fig. 4 were calculated as means ± SEM. The significance of the change in mRNA content was analysed using the Student’s t-test (*p < 0.05; ***p < 0.001).
Fig. 4.
The gene silencing of P2Y2 and P2Y6 receptor using specific siRNAs was estimated by quantitative RT-PCR experiments. Relative to negative siRNA, the P2Y2 siRNA (s9967) and the P2Y6 siRNA (s224151) reduced the mRNA for the receptors by 98% and 83.7%, respectively. The data were normalised to the housekeeping gene hACTB
Results
Molecular and functional analysis of P2 receptors in hCMEC/D3 cells
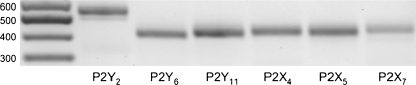
Expression of P2 receptors in the hCMEC/D3 cell line, an in vitro model of BBB endothelial cells was evaluated by RT-PCR. Various pairs of primers against the different P2 receptor subtypes (Table 1) recognised P2Y2, P2Y11 and minimally detectable P2Y6 as well as P2X4, P2X5 and P2X7 receptors in these cells (Fig. 1). As for the P2Y6, original PCR experiments yielded a very weak band. However, the used primer pair was effective in detecting P2Y6 mRNA in human umbilical vein endothelial cells (HUVEC, result not shown). The detected weak band was extracted from the gel and was used for a re-PCR using the same primers to confirm the PCR product by sequencing. This re-PCR product is given in Fig. 1. It is worthy to note that the other purine receptor subtypes detected were also confirmed by sequencing.
Fig. 1.
The different purine receptors expressed by the hCMEC-D3 cells as revealed by the RT-PCR. Expression of P2Y2, 6 and 11 as well as P2X4, 5 and 7 subtypes by hCMEC/D3 cells was confirmed by RT-PCR. The original band for P2Y6 was almost undetectable. Another round of PCR was therefore performed following extraction of the original PCR band. The product of this re-PCR is visualised by agarose gel electrophoresis together with the original PCR products for the other purine receptor subtypes. The other P2X and P2Y receptor subtypes were not found
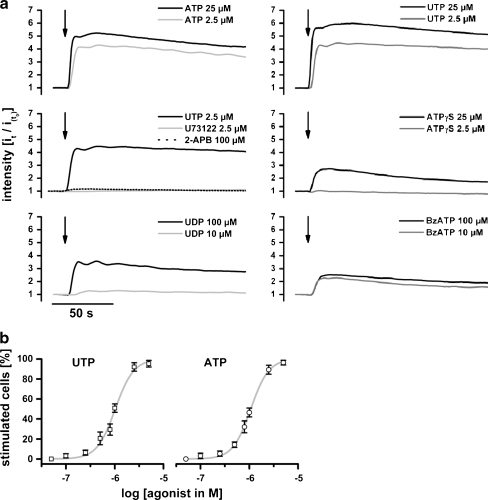
To access the functionality of the receptors, we applied various purinergic agonists to the cells while following changes in the fluorescence intensity of Fluo-4 in the cells to detect changes in the intracellular concentration of free Ca2+ ([Ca2+]i). The results revealed that either ATP or UTP induces an increase in the fluorescence intensity of Fluo-4-loaded cells. Application of 2.5 μM ATP or UTP induces a fourfold increase of the fluorescence intensity within 5 s relative to the initial intensity (Fig. 2a). The rapid increase in the fluorescence intensity was followed by a decrease to the level of nonstimulated cells within 10 min. Fura-2 ratiometric experiments [25, 26] revealed a resting [Ca2+]i in single hCMEC/D3 cells of about 150 nM which was increased to 300 nM by stimulation with ATP or UTP (data not shown). We assume that the fourfold fluorescence increase of Fluo-4-loaded cells correlated with a [Ca2+]i increase by about 150 nM. In the following discussion, the agonist-related increase of the fluorescence intensity of Fluo-4-loaded cells also will be referred to as Ca2+ signal.
Fig. 2.
a Change in fluorescence intensity induced by stimulation of the cells with different agonist concentration. The data show that the cell sensitivity to ATP and UTP was similar. ATPγS, UDP or BzATP could also stimulate the cells. However, the change in fluorescence intensity was reduced (even at high concentrations) in comparison to stimulation with ATP or UTP. The PLC inhibitor U73122 or the IP3 receptor blocker 2-ABP could block the UTP or ATP induced increase in fluorescence intensity. The graphs represent averages of at least 200 cells for each treatment. For the sake of clarity, the error bars are not shown. The maximal SEM was ±0.21. b The concentration dependency of stimulation of the Ca2+ signal in the hCMEC/D3 cells by the putative physiological agonists. The portion of cells stimulated by respective ATP or UTP concentrations is given. The data points were fitted to sigmoid dose–response curves. This allowed to estimate a half stimulation concentration of about 1.25 μM for both agonists
Higher ATP or UTP concentrations (25 μM) enhanced the stimulation of the induced increase in the fluorescence intensity of Fluo-4-loaded cells up to fivefold to sixfold (Fig. 2a). Considering single cells, we defined a cell as stimulated if the fluorescence intensity measured in this particular cell was increased twofold over to the nonstimulated intensity. Interestingly, the total number of single cells which were stimulated by the agonists did not increase with ATP or UTP concentrations. With 2.5 and 25 μM ATP, 88.4% and 88.9% of the cells could be stimulated, respectively (Table 3). A similar result was also obtained for UTP, which stimulated 90.1% and 93.3% of the cells at 2.5 and 25 μM, respectively (Table 3). The reduction of the agonist concentration correlated with a reduction of the portion of stimulated cells (Fig. 2b). We could estimate for each agonist a half stimulation concentration, which correlated to the agonist concentration at which 50% of the cells responded to the agonist. For both UTP and ATP, a half stimulation concentration of about 1.25 μM (Fig. 2b) was found.
Table 3.
The fraction of the cells, which react to stimulation with different agonists
| UTP | ATP | UDP | ATPγS | BzATP | ADP | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Concentration (μM) | 2.5 | 25 | 2.5 | 25 | 10 | 100 | 2.5 | 25 | 10 | 100 | 10 | 100 |
| Untransfected cells (%) | 90.1 | 93.3 | 88.4 | 88.9 | 50.0 | 72.5 | 7.9 | 54.5 | 46.0 | 60.8 | 12.1 | 40.6 |
| Negative siRNA (%) | 86.1 | – | – | – | – | 34.4 | 15.2 | – | – | 58.3 | – | 33.0 |
| P2Y2 siRNA (%) | 25.4 | – | – | – | – | 3.4 | 0 | – | – | 9.8 | – | 3.5 |
The fluorescence images of Fluo-4-loaded cells were taken every second for 300 s. After measuring the fluorescence intensity of the nonstimulated cells during the first 10 s, the respective agonists were added at indicated concentrations while the fluorescence images were continuously monitored. For evaluation, the images were analysed using Image J software (see main text). Each cell was defined as a region of interest and the fluorescence intensity of each individual cell evaluated. The fluorescence intensity registered in each cell for the first 10 s was average, and the fluorescence intensity measured at each second in each cell was normalised to the respective averaged value. A cell was considered as stimulated if the fluorescence intensity of this cell was increased by at least twofold above the average value after addition of the agonist. Three independent experiments were performed, and at least 200 single cells were measured for each treatment. –: Not tested
The finding that UTP, an agonist which does not stimulate P2X receptors, could induce a Ca2+ signal in the hCMEC/D3 cells indicates that the ATP or UTP-related Ca2+ signal was probably related to P2Y receptors. The following observations are also in agreement with this concept. (i) The ATP- or UTP-induced Ca2+ signal was not affected by EGTA in the external bath solution (data not shown). (ii) The ATP- and UTP-related Ca2+ signal was suppressed by the PLC inhibitor U73122 (2.5 μM) or by the IP3-receptor blocker 2-APB (100 μM; Fig. 2a). (iii) The P2X-specific agonist αβ-meATP (500 or 1,000 μM) did not induce a remarkable Ca2+ signal in the hCMEC/D3 cells (data not shown). Taken together, the results indicate that the purinergic stimulation of Ca2+ signalling in the hCMEC/D3 cells acts via the G-protein-coupled P2Y receptor subtypes, which are highly sensitive to ATP and UTP.
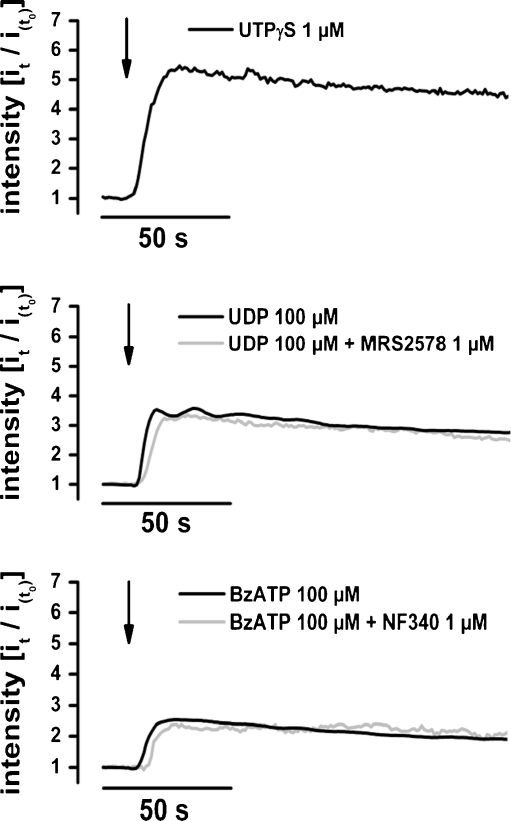
Since we observed a possible expression of the Gq-protein-coupled receptors P2Y2 and P2Y6 as well as P2Y11, we tested whether more specific agonists for P2Y6 (UDP) or P2Y11 (ATPγS or BzATP) could induce Ca2+ signals. UDP (100 μM), ATPγS (25 μM) as well as BzATP (10 or 100 μM) were able to induce a limited increase in the fluorescence intensity of Fluo-4-loaded cells. Compared to nonstimulated cells, a maximal increase of the fluorescence intensity up to threefold, 2.7-fold and 2.5-fold was induced, respectively, by UDP (100 μM), ATPγS (25 μM) as well as by BzATP (100 μM; Fig. 2a). At single-cell level, UDP, ATPγS and BzATP stimulated a smaller population of cells compared to ATP or UTP (Table 3). Considering single cells as stimulated if the agonist induces an increase of the fluorescence of Fluo-4-loaded cells by at least twofold, we observed that 10 μM or 100 μM of UDP stimulated 50% and 72.5% of the cells. At 2.5 and 25 μM, ATPγS stimulated 7.9% and 54.5%, respectively, of the cells. BzATP stimulated 46% of the cells at 10 μM or 60.8% at 100 μM (Table 3). Further pharmacological experiments showed that UTPγS (Biozol, Eching, Germany), a specific agonist for P2Y2 and P2Y4 receptor [29–32] efficiently induced Ca2+ signal in the cells (Fig. 3). At single-cell level, UTPγS stimulated 95% of the cells at 1 μM. Since the cells did not express P2Y4, the result shows the importance of the P2Y2 receptor in these cells. Additionally, we analysed whether MRS2578 or NF340 (Biozol), the respective specific inhibitor of P2Y6 and P2Y11 [30–34], could affect Ca2+ signals induced by UDP or BzATP. We observed that neither MRS2578 (1 μM) nor NF340 (1 μM) reduced the Ca2+ signals induced by UDP or BzATP (Fig. 3). Taken together, these findings indicate that the P2Y2 receptor is the main purine receptor related to the Ca2+ signalling in hMEC/D3 cells.
Fig. 3.
The specific agonist of P2Y2 and P2Y4 receptor UTPγS induced Ca2+ signals in the hCMEC/D3 cells. Since the cells did not express P2Y4 receptor (Fig. 1) the signal is related to P2Y2 receptors. Additionally, MRS2578 or NF340 the specific inhibitors of P2Y6 and P2Y11 respectively did not affect the UDP or the BzATP induced Ca2+ signal in hCMEC/D3 cells
P2Y2 receptor siRNA suppresses the purinergic signalling in the hCMEC/D3 cell line
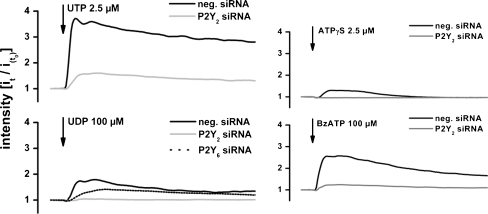
Based on the RT-PCR and our physiological results, we assumed that the P2Y2 receptor subtype is the most important subtype of the G-protein-coupled purine receptor family in these cells. In further studies, we induced gene silencing of the P2Y2 receptor using specific siRNA. The amount of the P2Y2 receptor mRNA was reduced by about 98% at 48 h after transfection of the cells with P2Y2 receptor siRNA (s9967) as revealed by quantitative RT-PCR (Fig. 4). At the functional level, the reduction of the P2Y2 receptor mRNA correlated with a reduction of the cell sensitivity toward UTP (2.5 μM). UTP (2.5 μM) induced an increase in the fluorescence intensity in cells transfected with siRNA against the P2Y2 mRNA by only 1.5-fold compared to a fourfold increase in fluorescence of cells transfected with nonspecific siRNA (Fig. 5). At single-cell level and again considering single cells as stimulated if the agonist induced an increase in the fluorescence of Fluo-4-loaded cells by at least twofold, we found that only 25.4% of cells transfected with P2Y2 siRNA were stimulated by UTP (2.5 μM). In comparison, 86.1% of the cells, which were transfected with nonspecific siRNA, were stimulated by UTP application (Table 3). Interestingly, the sensitivity of the cells to the agonists UDP (100 μM) or ATPγS (2.5 μM) and BzATP (100 μM) of the P2Y6 or P2Y11 receptor subtypes was completely abolished in cells transfected with P2Y2 siRNA (Fig. 5; Table 3). Furthermore, we observed that, after silencing the P2Y6 receptor subtype using P2Y6 siRNA, the cells could still react to stimulation with UDP (Fig. 5) despite an 83.7% reduction of the P2Y6 mRNA (Fig. 4). The results indicate that the P2Y6 receptor is not involved in the nucleotide-mediated Ca2+ signal.
Fig. 5.
Silencing the P2Y2 receptor reduced the sensitivity of the cells to UTP and suppressed the sensitivity to UDP, ATPγS, BzATP. Cells in which the P2Y6 was silenced by specific siRNA still react to UDP stimulation. It is noteworthy that the negative siRNA reduced the sensitivity of the cells to the agonists. This is probable due to a nonspecific effect related to the Lipofectamine 2000 used during the transfection
Discussion
Endothelial cells express different purine receptors that are involved in the regulation of various pathological processes such as inflammation [13]. In the BBB, recent results demonstrate the importance of purine receptors in the regulation of vasodilatation, inflammatory processes in stroke-related injury and other CNS inflammatory diseases [8–10, 13]. In the present report, we used the hCMEC/D3 cell line, an in vitro model of human cerebral microvascular endothelial cells [24], to determine the expression and the physiology of purine receptors involved in the BBB. The hCMEC/D3 cell line is characterised by the presence of the nuclear SV40-T antigen and a high expression level of nuclear and perinuclear hTERT protein [24]. It is known that the immortalised cells expressing hTERT protein maintain a stable genotype and retain critical phenotypic markers [35, 36]. Accordingly, the hCMEC/D3 cells have a stable diploid karyotype [24]. We cannot completely exclude that the immortalisation process affects the cells; however, the hCMEC/D3 cells have phenotypical and physiological similarities with microvascular endothelial cells that allow an analysis of the BBB endothelial cell physiology [37].
At the mRNA level, RT-PCR revealed that the hCMEC/D3 cells express the G-protein-coupled P2Y-receptor subtypes P2Y2, P2Y11 and minimally detectable P2Y6 as well as the ionotropic P2X4, P2X5 and P2X7 receptors (Fig. 1). Other purine receptor subtypes could not be found although the used primers were able to detect the other receptor subtypes in other human cell lines. For G-protein-coupled receptors, the P2Y1 and P2Y6 used primers were able to detect the corresponding receptor mRNAs in HUVEC (data not shown). As for the P2Y4 receptor, a primer pair was also used that had been shown to recognise this receptor [38] but failed to detect the P2Y4 receptor in hCMEC/D3 cells. The results suggest that the purine receptor subtypes that were not detected were not expressed in the hCMEC/D3 cells. Data from a variety of studies have shown that the expression pattern of purine receptors may be cell-type-specific [39]. The expression of P2Y2, 6 and 11 as well as P2X4, 5 and 7 seems to be a BBB endothelial cell-specific profile since a slightly different expression pattern of purine receptors was observed in HUVEC [40].
We performed physiological experiments to address the contribution of each receptor subtype to the physiology of the endothelial BBB cells. We found that the stimulation of hCMEC/D3 cells with ATP (2.5 or 25 μM) induces an increase in [Ca2+]i (Fig. 2a). Analysing other purinergic agonists, we found that UTP could also elicit the Ca2+ signal in the cells. The portion of stimulated cells was related to the applied agonist concentration. At 0.1 μM, ATP or UTP stimulated about 3% of the cells. The amount of stimulated cells increased with increasing agonist concentration to achieve a maximum of about 95% of the cells at about 10 μM. A half maximal stimulation concentration of 1.25 μM was found for both ATP and UTP (Fig. 2b). Considering whether a single cell react or not, it can be assumed that ATP and UTP stimulate the cells with a similar efficiency. However, we observed that UTP induced a Ca2+ signal more robust than that induced by ATP (Fig. 2a). The reason of the increased efficiency of UTP compared to ATP is probably related to the nucleotide binding site of the receptors. It is known that the P2Y2 receptor subtype suited better UTP than ATP [41].
The UTP-mediated Ca2+ signal could be suppressed by the PLC inhibitor U73122 or the IP3 receptor blocker 2-APB (Fig. 2a). The results indicate that the purinergic stimulation of the Ca2+ signalling was related to stimulation of the Gq-protein-coupled receptor subtypes P2Y2 and P2Y6,which activate the IP3 signalling cascade [17, 42], as well as to stimulation of the P2Y11 receptor, which activates Gq as well as Gs protein [18, 19, 42]. The ionotropic P2X receptor subtypes also allow an increase in [Ca2+]i when stimulated by ATP. However, this P2X receptor-mediated [Ca2+]i is related to Ca2+ influx from the extracellular space. In our case, the absence of external Ca2+ did not suppress the ATP induced Ca2+ signal (data not shown), suggesting that the observed P2X receptors are not involved in the induced Ca2+ signalling. This assumption is further emphasised by the finding that a high concentration of the P2X-specific agonist αβ-meATP (500–1,000 μM) did not affect the [Ca2+]i (results not shown). Taken together, the RT-PCR and the physiological results indicate that the purine receptor system of hCMEC/D3 cells is mainly linked to Ca2+ signalling induced by P2Y2 and probable P2Y6 as well as P2Y11 receptor subtypes. After those findings, we then turned to the question whether the three P2Y receptor subtypes participate equally in the induced Ca2+ response or not. For this, we used UDP which stimulates specifically P2Y6 receptors and the agonists BzATP or ATPγS which bind more to P2Y11 than to the other P2Y receptor subtypes. UDP or BzATP (10 μM) were not able to elicit a significant Ca2+ signal. ATPγS (2.5 μM) stimulated a very limited Ca2+ signal (Fig. 2a). Higher concentrations of the agonists were able to elicit a Ca2+ signal in a subpopulation of hCMEC/D3 cells. ATPγS at 25 μM could stimulate 54.5% of the cells, whereas UDP or BzATP at 100 μM stimulated 72.5% or 60.8% of the cells, respectively (Table 3). The results could be interpreted as a minor involvement of P2Y6 and P2Y11 in Ca2+ signalling in BBB endothelial cells. A second possibility is that neither P2Y6 nor P2Y11 is involved in the Ca2+ signalling of the endothelial cells of the BBB. The observed Ca2+ signals induced by high concentrations of UDP, ATPγS, or BzATP (Fig. 2a) might be related to nonspecific binding of these molecules to the P2Y2 receptor. Two pharmacological experiments could support the second possibility. (i) The specific agonist of P2Y2 and P2Y4 receptor UTPγS [29–32] stimulated the cells like UTP or ATP (Fig. 3). Since the cells did not express P2Y4 (Fig. 1), the UTPγS induced Ca2+ can only be related to P2Y2 receptors. (ii) MRS2578 and NF340, the specific antagonists for P2Y6 and P2Y11, respectively, [30–34] did not affect the UDP- or BzATP-induced Ca2+ signals (Fig. 3). To gain more evidences for this possibility, we applied siRNA technology to silence P2Y2 receptors achieving a reduction in P2Y2 mRNA within 48 h by 98% (Fig. 4). This mRNA silencing correlated with a reduction in the percentage of cells which could be stimulated by 2.5 μM UTP from ~86.1% to 25.4% (Table 3). Furthermore, gene silencing of the P2Y2 mRNA completely suppressed induction of a Ca2+ signal in the hCMEC/D3 cells by UDP, ATPγS or BzATP (Fig. 5). We propose therefore that the Ca2+ signal observed after purinergic stimulation is exclusively related to stimulation of the P2Y2 receptor subtype and not due to other receptors such as P2Y6. This proposition is consistent with the observation that silencing of the P2Y6 receptor with specific P2Y6 siRNA did not suppress the UDP-mediated Ca2+signal in the cells (Fig. 5).
Ca2+-imaging experiments have shown that primary cultures of BBB endothelial cells from rats express mainly P2Y2 receptors [21, 22]. From our molecular biological and physiological experiments, we can postulate that the human system is similar to the rat system where the purinergic stimulation of the Ca2+ signalling is only related to P2Y2 receptor subtype [21, 22]. The PCR experiments showed expression of P2Y11 receptor in hCMEC/D3 (Fig. 1). However, both physiological and gene-silencing experiments showed that P2Y11 was not involved in nucleotide-mediated Ca2+ signalling. It was shown that ATP could induce cAMP synthesis in rat BBB endothelial cells by a nonidentified mechanism [21, 23]. Since P2Y11 is coupled to Gs protein, it is tempting to speculate that the P2Y11 receptor could be a regulator of cAMP production in endothelial cells of the BBB. The role of the P2X receptor subtypes in the physiology of the endothelial cells of the BBB is also not clear. So far, we have shown that these receptors are not involved in Ca2+ signalling. As ionotropic receptors, the detected P2X4, 5 and 7 may be involved in regulation of the membrane potential of the cells. Further combined electrophysiological and molecular biological experiments should clarify this issue in the future.
Conclusion
In this report, we analysed the expression of the purine receptors in the human BBB endothelial cell line hCMEC/D3. The receptor subtypes P2Y2, P2Y6 and P2Y11 as well as P2X4, P2X5 and P2X7 are expressed at the mRNA level. At functional levels, we found that purinergic stimulation of the hCMEC/D3 cells induced Ca2+ signalling only by the P2Y2receptor which activated Ca2+ release from intracellular stores. This exclusively P2Y2-dependent signalling was also identified in primary cultivated rat BBB endothelial cells. Our results show that at a physiological level human BBB endothelial cells express a purine receptor system similar to that of the rat. Furthermore, it is shown that the hCMEC/D3 cell line is a suitable model for in vitro analysis of further purinergic signalling cascades in the human BBB and for nucleotide-mediated interactions in the neurovascular unit.
Acknowledgments
The authors thank Prof. Dr. Helge Küster and his team for discussion on the manuscript. The work was supported by the NANOTOME project (Biophotonik III) and by Boehringer Ingelheim International.
References
- 1.Drewes LR. Molecular architecture of the brain microvasculature: perspective on blood–brain transport. J Mol Neurosci. 2001;16:93–98. doi: 10.1385/JMN:16:2-3:93. [DOI] [PubMed] [Google Scholar]
- 2.Abbott NJ, Rönnbäck L, Hansson E. Astrocyte–endothelial interactions at the blood–brain barrier. Nat Rev Neurosci. 2006;7:41–53. doi: 10.1038/nrn1824. [DOI] [PubMed] [Google Scholar]
- 3.Banks WA. Physiology and pathology of the blood–brain barrier: implications for microbial pathogenesis, drug delivery and neurodegenerative disorders. J Neurovirol. 1999;6:538–555. doi: 10.3109/13550289909021284. [DOI] [PubMed] [Google Scholar]
- 4.Iadecola C, Nedergaard M. Glial regulation of the cerebral microvasculature. Nat Neurosci. 2007;10:1369–1376. doi: 10.1038/nn2003. [DOI] [PubMed] [Google Scholar]
- 5.Zoppo GJ. Virchow’s triad: the vascular basis of cerebral injury. Rev Neurol Dis. 2008;5:S12–S21. [PMC free article] [PubMed] [Google Scholar]
- 6.Paemeleire K. Calcium signaling in and between brain astrocytes and endothelial cells. Acta Neurol Belg. 2002;102:137–140. [PubMed] [Google Scholar]
- 7.Zoppo GJ. The neurovascular unit in the setting of stroke. J Intern Med. 2010;67:156–171. doi: 10.1111/j.1365-2796.2009.02199.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zoppo GJ. Inflammation and the neurovascular unit in the setting of focal cerebral ischemia. Neuroscience. 2009;158:972–982. doi: 10.1016/j.neuroscience.2008.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stolp HB, Dziegielewska KM. Role of developmental inflammation and blood–brain barrier dysfunction in neurodevelopmental and neurodegenerative diseases. Neuropathol Appl Neurobiol. 2009;35:132–146. doi: 10.1111/j.1365-2990.2008.01005.x. [DOI] [PubMed] [Google Scholar]
- 10.Peterson TS, Camden JM, Wang Y, Seye CI, Wood WG, Sun GY, Erb L, Petris MJ, Weisman GA. P2Y2 nucleotide receptor-mediated responses in brain cells. Mol Neurobiol. 2010;41:356–366. doi: 10.1007/s12035-010-8115-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lazarowski ER, Harden TK. Quantification of extracellular UTP using a sensitive enzymatic assay. Br J Pharmacol. 1999;127:1272–1278. doi: 10.1038/sj.bjp.0702654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Xu HL, Pelligrino DA. ATP release and hydrolysis contribute to rat pial arteriolar dilatation elicited by neuronal activation. Exp Physiol. 2007;92:647–651. doi: 10.1113/expphysiol.2006.036863. [DOI] [PubMed] [Google Scholar]
- 13.Virgilio F, Ceruti S, Bramanti P, Abbracchio MP. Purinergic signalling in inflammation of the central nervous system. Trends Neurosci. 2009;32:79–87. doi: 10.1016/j.tins.2008.11.003. [DOI] [PubMed] [Google Scholar]
- 14.Pineau I, Lacroix S. Endogenous signals initiating inflammation in the injured nervous system. Glia. 2009;57:351–361. doi: 10.1002/glia.20763. [DOI] [PubMed] [Google Scholar]
- 15.King BF, Townsend-Nicholson A. Nucleotide and nucleoside receptors. Tocris Rev. 2003;23:1–12. [Google Scholar]
- 16.Kügelgen I. Pharmacological profiles of cloned mammalian P2Y-receptor subtypes. Pharmacol Ther. 2006;110:415–432. doi: 10.1016/j.pharmthera.2005.08.014. [DOI] [PubMed] [Google Scholar]
- 17.Abbracchio MP, Burnstock G, Boeynaems JM, Barnard EA, Boyer JL, Kennedy C, Knight GE, Fumagalli M, Gachet C, Jacobson KA, Weisman GA. International Union of Pharmacology LVIII: update on the P2Y G protein-coupled nucleotide receptors: from molecular mechanisms and pathophysiology to therapy. Pharmacol Rev. 2006;58:281–341. doi: 10.1124/pr.58.3.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fischer W, Krügel U. P2Y receptors: focus on structural, pharmacological and functional aspects in the brain. Curr Med Chem. 2007;14:2429–2455. doi: 10.2174/092986707782023695. [DOI] [PubMed] [Google Scholar]
- 19.Erb L, Liao Z, Seye CI, Weisman GA. P2 receptors: intracellular signaling. Pflugers Arch. 2006;452:552–562. doi: 10.1007/s00424-006-0069-2. [DOI] [PubMed] [Google Scholar]
- 20.Ralevic V, Burnstock G. Receptors for purines and pyrimidines. Pharmacol Rev. 1998;50:413–492. [PubMed] [Google Scholar]
- 21.Albert JL, Boyle JP, Roberts JA, Challiss RA, Gubby SE, Boarder MR. Regulation of brain capillary endothelial cells by P2Y receptors coupled to Ca2+, phospholipase C and mitogen-activated protein kinase. Br J Pharmacol. 1997;122:935–941. doi: 10.1038/sj.bjp.0701453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sipos I, Dömötör E, Abbott NJ, Adam-Vizi V. The pharmacology of nucleotide receptors on primary rat brain endothelial cells grown on a biological extracellular matrix: effects on intracellular calcium concentration. Br J Pharmacol. 2000;131:1195–1203. doi: 10.1038/sj.bjp.0703675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Anwar Z, Albert JL, Gubby SE, Boyle JP, Roberts JA, Webb TE, Boarder MR. Regulation of cyclic AMP by extracellular ATP in cultured brain capillary endothelial cells. Br J Pharmacol. 1999;128:465–471. doi: 10.1038/sj.bjp.0702792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Weksler BB, Subileau EA, Perrière N, Charneau P, Holloway K, Leveque M, Tricoire-Leignel H, Nicotra A, Bourdoulous S, Turowski P, Male DK, Roux F, Greenwood J, Romero IA, Couraud PO. Blood–brain barrier-specific properties of a human adult brain endothelial cell line. FASEB J. 2005;19:1872–1884. doi: 10.1096/fj.04-3458fje. [DOI] [PubMed] [Google Scholar]
- 25.Grynkiewicz G, Poenie M, Tsien RY. A new generation of Ca2+ indicators with greatly improved fluorescence properties. J Biol Chem. 1985;260:3440–3450. [PubMed] [Google Scholar]
- 26.Bintig W, Baumgart J, Walter JW, Heisterkamp A, Lubatschowski H, Ngezahayo A. Purinergic signalling in rat GFSHR-17 granulosa cells: an in vitro model of granulosa cells in maturing follicles. J Bioenerg Biomembr. 2009;41:85–94. doi: 10.1007/s10863-009-9199-5. [DOI] [PubMed] [Google Scholar]
- 27.Schmittgen TD, Livak KJ. Analyzing real-time PCR data by the comparative C(T) method. Nat Protoc. 2008;3:1101–1108. doi: 10.1038/nprot.2008.73. [DOI] [PubMed] [Google Scholar]
- 28.Baier MC, Keck M, Gödde V, Niehaus K, Küster H, Hohnjec N. Knockdown of the symbiotic sucrose synthase MtSucS1 affects arbuscule maturation and maintenance in mycorrhizal roots of Medicago truncatula. Plant Physiol. 2010;152:1000–1014. doi: 10.1104/pp.109.149898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lazarowski ER, Watt WC, Stutts MJ, Brown HA, Boucher RC, Harden TK. Enzymatic synthesis of UTPγS, a potent hydrolysis resistant agonist of P2U-purinoceptors. Br J Pharmacol. 1996;117:203–209. doi: 10.1111/j.1476-5381.1996.tb15175.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Brunschweiger A, Müller CE. P2 receptors activated by uracil nucleotides—an update. Curr Med Chem. 2006;12:763–771. doi: 10.2174/092986706775476052. [DOI] [PubMed] [Google Scholar]
- 31.Jacobson KA, Ivanov AA, Castro S, Harden TK, Ko H. Development of selective agonists and antagonists of P2Y receptors. Purinergic Signal. 2009;5:75–89. doi: 10.1007/s11302-008-9106-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jacobson KA, Boeynaems JM. P2Y nucleotide receptors: promise of therapeutic applications. Drug Discov Today. 2010;15:570–578. doi: 10.1016/j.drudis.2010.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mamedova LK, Joshi BV, Gao ZG, Kügelgen I, Jacobson KA. Diisothiocyanate derivatives as potent, insurmountable antagonists of P2Y6 nucleotide receptors. Biochem Pharmacol. 2004;67:1763–1770. doi: 10.1016/j.bcp.2004.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ullmann H, Meis S, Hongwiset D, Marzian C, Wiese M, Nickel P, Communi D, Boeynaems JM, Wolf C, Hausmann R, Schmalzing G, Kassack MU. Synthesis and structure activity relationships of suramin-derived P2Y11 receptor antagonists with nanomolar potency. J Med Chem. 2005;48:7040–7048. doi: 10.1021/jm050301p. [DOI] [PubMed] [Google Scholar]
- 35.Morales CP, Holt SE, Ouellette M, Kaur KJ, Yan Y, Wilson KS, White MA, Wright WE, Shay JW. Absence of cancer-associated changes in human fibroblasts immortalized with telomerase. Nature Genet. 1999;21:115–118. doi: 10.1038/5063. [DOI] [PubMed] [Google Scholar]
- 36.Ouellette M, McDaniel LD, Wright WE, Shay JW, Schultz RA. The establishment of telomerase -immortalized cell line representing human chromosome instability syndromes. Hum Mol Genet. 2000;9:403–411. doi: 10.1093/hmg/9.3.403. [DOI] [PubMed] [Google Scholar]
- 37.Poller B, Gutmann H, Krähenbühl S, Weksler B, Romero I, Couraud PO, Tuffin G, Drewe J, Huwyler J. The human brain endothelial cell line hCMEC/D3 as a human blood–brain barrier model for drug transport studies. J Neurochem. 2008;107:1358–1368. doi: 10.1111/j.1471-4159.2008.05730.x. [DOI] [PubMed] [Google Scholar]
- 38.Hansen MR, Krabbe S, Novak I. Purinergic receptors and calcium signalling in human pancreatic duct cell lines. Cell Physiol Biochem. 2008;22:157–168. doi: 10.1159/000149793. [DOI] [PubMed] [Google Scholar]
- 39.Burnstock G. Purinergic signalling—an overview. Novartis Found Symp. 2006;276:46–48. [PubMed] [Google Scholar]
- 40.Wang L, Karlsson L, Moses S, Hultgårdh-Nilsson A, Andersson M, Borna C, Gudbartsson T, Jern S, Erlinge D. P2 receptor expression profiles in human vascular smooth muscle cells and endothelial cells. J Cardiovasc Pharmacol. 2002;40:841–853. doi: 10.1097/00005344-200212000-00005. [DOI] [PubMed] [Google Scholar]
- 41.Hillmann P, Ko GY, Spinrath A, Raulf A, Kügelgen I, Wolff SC, Nicholas RA, Kostenis E, Höltje HD, Müller CE. Key determinants of nucleotide-activated G protein-coupled P2Y2 receptor function revealed by chemical and pharmacological experiments, mutagenesis and homology modeling. J Med Chem. 2009;52:2762–2775. doi: 10.1021/jm801442p. [DOI] [PubMed] [Google Scholar]
- 42.Kügelgen I, Wetter A. Molecular pharmacology of P2Y-receptors. Naunyn SchmiedebergsArch Pharmacol. 2000;362:310–323. doi: 10.1007/s002100000310. [DOI] [PubMed] [Google Scholar]