Abstract
We examined healthcare providers’ perceptions of genetic counseling and testing in African American women (AAW) at moderate to high-risk of carrying a BRCA1/2 mutation. We conducted 20 in-depth interviews with genetic counselors (n=5), medical oncologists (n=8), obstetrician/gynecologists (n=2) and surgeons (n=5). Interviews were audiotaped, transcribed and independently coded by two coders using a content analysis approach. Seven themes emerged relevant to providers’ perceptions of AAW’s use of BRCA1/2 genetic services: access factors, cultural beliefs and preferences, effects of testing, patient motivators for genetic counseling and testing, patient-provider communication, reasons for provider referral, and reasons for patient refusal. Providers identified individual- and system-level barriers to AAW’s use of genetic services, including lack of follow-up after referrals to genetic specialists and challenges to obtaining financial coverage for under- and uninsured high-risk women. Results have implications for physician and patient education regarding appropriate referrals to and uptake of genetic services in at-risk AAW.
Keywords: African American women, BRCA1/2, breast cancer genetics, genetic counseling, genetic testing, cancer providers
INTRODUCTION
African American women (AAW) are diagnosed with breast cancer at more advanced stages and have higher rates of breast cancer related mortality than Caucasian women (American Cancer Society, 2009; Newman, 2005). Despite lower overall incidence of breast cancer in AAW compared to Caucasian women, AAW have a higher incidence of early onset breast cancer, defined as diagnosis before age 50 (American Cancer Society, 2009). In the general population, 5%–10% of all breast cancers are due to mutations in the BRCA1 or BRCA2 genes; these genetic mutations are also associated with a high incidence of premenopausal, early onset breast cancer (Chen et al., 2002). BRCA1/2 mutations may explain some of the increased incidence of early onset breast cancer in AAW, especially those from high-risk families (Dangel et al., 1999; Gao, Neuhausen, Cummings, Luce, & Olopade, 1997; Gao et al., 2000; Hall et al., 2009). AAW also experience a high rate of mutations (gene variants) of uncertain significance, which makes risk assessment and genetic test result interpretation quite complex (Nanda et al., 2005; Opatt, Morrow, & Daly, 2006).
Although genetic counseling and testing for BRCA1/2 genes are used to gain information and plan medical management, AAW appear less likely to pursue these services or engage in genetics-related research (Armstrong, Micco, Carney, Stopfer, & Putt, 2005; Moorman et al., 2004; Pal, Permuth-Wey, Holtje, & Sutphen, 2004; Pal et al., 2008; Patterson et al., 2008). In research focused on genetic counseling and testing in AAW, results suggest moderate success in recruiting AAW to participate in the process using direct face-to-face encounters in cancer treatment clinics and physician referrals (Pal et al., 2008; Patterson et al., 2008). In contrast, many strategies to improve the participation of AAW in cancer genetics research, such as self-referral, cancer registries and print advertisements, have not been as successful as anticipated (Halbert et al., 2005; Halbert et al., 2008; Pal et al., 2008; Patterson et al., 2008). When AAW do engage in BRCA1/2 genetic counseling research, investigators report high rates of retention, suggesting on-going involvement once AAW are involved in the process (Halbert et al., 2008).
Evidence associated with AAW’s interest in BRCA1/2 genetic counseling and testing is mixed, with studies reporting both high (Hughes, Fasaye, LaSalle, & Finch, 2003; Hughes et al., 2004; Kinney et al., 2001) and low levels of awareness and interest (Hughes et al. 1997). Barriers to AAW’s interest and participation in genetic counseling and testing include anticipation of experiencing negative emotional reactions to genetic risk information or subsequent stigmatization (Thompson et al., 2002); concerns about racial discrimination (Peters, Rose, & Armstrong, 2004) or confidentiality of genetic test results (Donovan & Tucker, 2000); lower knowledge of cancer genetics (Lipkus, Iden, Terrenoire, & Feaganes, 1999; Simon & Petrucelli, 2009); and having a present temporal orientation, described as a perception of the significance of events and the consequences of one’s behavior in terms of current (vs. past or future) implications (Edwards et al., 2008; Hughes et al., 2003). Earlier research has pointed to AAW’s lower perceived risk of breast cancer even among at-risk patients (Matthews et al., 2000). Finally, disparities in the use of genetic counseling and testing between African Americans and Caucasians may be exacerbated by lower overall access to both basic preventive healthcare and specialized cancer prevention services among African Americans (Hall & Olopade, 2005). Even with culturally-tailored recruitment strategies, participation of AAW in genetic counseling and testing is suboptimal (Halbert, Kessler, Stopfer, Domchek, & Wileyto, 2006; Simon & Petrucelli, 2009). In a study that addressed cultural factors such as communalism and spiritual beliefs, less than half of AAW at increased risk for carrying a BRCA1/2 mutation completed pre-genetic testing education and counseling and only about one-fifth of the overall sample received test results (Halbert et al., 2006). When cost barriers to testing were minimized, African American breast cancer survivors still pursued genetic testing less often than Caucasian survivors (Susswein et al., 2008).
For AAW who do pursue testing, receipt of BRCA1/2 results appears to impact risk management behaviors. African American mutation carriers were more likely than non-carriers to have a mammogram and discuss test results with their primary care physician in the year after receipt of results (Kinney et al., 2006). In terms of specific risk management behavior patterns, African American mutation carriers appear to opt for breast cancer surveillance more often than risk reducing surgery in the year following test result notification (Kinney et al., 2006).
One of the most consistent predictors of who pursues BRCA1/2 genetic counseling and testing is a healthcare provider’s recommendation (Metcalfe et al., 2009; Pal et al., 2008; Schwartz et al., 2005). As with patients, physicians’ knowledge of genetics may be a critical element for appropriate use of or referral to genetic services. For example, barriers to primary care physicians’ use of genetic services (including taking family medical histories and making referrals to specialists) include lack of genetics knowledge and low confidence in delivering genetic services or assessing genetic risk (Suther & Goodson, 2003). Oncologists who had greater knowledge of genetics were more likely to discuss and order BRCA1/2 tests, although the relationship between knowledge and use of genetic services was not found for internists or obstetricians/gynecologists (Doksum, Bernhardt, & Holtzman, 2003). Doksum and colleagues’ results (2003) suggest some physicians may proceed with discussion of BRCA1/2 testing regardless of their knowledge of genetics.
Notably, across providers from a variety of medical specialties, a significant predictor of their patients’ use of genetic services was whether the patient inquired about genetic testing (Wideroff et al., 2003). Rather than directly ordering cancer susceptibility tests, many physicians refer patients to other providers for these tests, with oncologists and genetics professionals (medical geneticists; genetic counselors) each receiving about one-quarter of the referrals for cancer susceptibility testing (Wideroff et al., 2003). Data from a large national physician survey indicate that approximately half of obstetricians/gynecologists and two-thirds of oncologists have ordered tests for or referred patients to genetics services (Wideroff et al., 2003).
BRCA1/2 genetic testing is often ordered by community physicians outside of academic medical settings (Keating et al., 2008). When community providers work closely with genetic counselors or nurse geneticists, they are more likely to discuss the essential elements involved with decision making about BRCA1/2 testing with their patients (Keating et al., 2008). To our knowledge, no studies have yet addressed the practices or perceptions of providers involved with the ordering of and referrals to use of genetic services among at-risk minorities. With physicians of various specialties ordering BRCA1/2 tests (Wideroff et al., 2003; Keating et al., 2008), the essential role of genetic counselors in physicians’ referral patterns and involvement with informed decision-making about BRCA1/2 testing (Keating et al., 2008), and the low rates of BRCA1/2 genetic counseling and testing uptake among AAW, we sought to gain insight into physician and genetic counselors’ perceptions of the genetic counseling and testing process for AAW at high-risk for breast cancer. Expanding what we know about healthcare providers’ perceptions of counseling and testing in this underserved group will allow us to identify targets for education and intervention for both patients and providers. Therefore, we aimed to 1) assess providers’ perceptions of the barriers and facilitators to genetic counseling and testing among moderate to high-risk AAW and 2) identify concepts and potential intervention targets relevant to improving appropriate uptake of genetic counseling and testing among high-risk AAW.
METHODS
Participants and Setting
After obtaining IRB approval from the MedStar Health Research Institute – Georgetown University Joint Oncology Institutional Review Board, participants were purposively selected from medical facilities in the Washington, DC metropolitan area. Through convenience and snowball sampling, we identified a total of 30 healthcare providers who routinely provide or refer women to genetic services. Providers from a variety of specialties were selected so that we could determine how genetic counseling was discussed across a spectrum of medical encounters. We regarded providers as “key informants” because of their medical knowledge and experience working with AAW at moderate to high-risk for breast cancer. Providers were identified through area hospital rosters and recommendations from professional colleagues.
Instrument
Following established qualitative procedures used by our team and others (Patton 2002; Sheppard, Christopher, & Nwabukwu, 2010), we developed a structured open-ended interview guide to elicit providers’ thoughts and referral practices associated with BRCA1/2 counseling and testing in AAW. We developed, reviewed, and refined the interview guide based on feedback from the study team. The final guide included 10 open-ended questions about providers’ perceived advantages and disadvantages of genetic counseling and testing, in general, and for AAW, specifically; preferences for referring patients for genetic counseling and testing; and perceived patient motivators for pursing this technology (see Appendix).
Procedures
A research assistant contacted potential participants by email or telephone and invited providers to participate in the single interview. If the participant agreed to be interviewed, the research assistant scheduled a convenient time and place to meet the provider and conduct the interview. We informed each participant of the nature of the study, seeking permission to audiotape the interview and notifying him/her that we would keep all responses confidential. Two research team members (TMH and JC) trained in qualitative inquiry conducted the interviews between June 2008 and August 2008. Prior to commencing the interview, the interviewer obtained verbal consent per an IRB approved verbal script. We conducted most interviews in-person with the exception of two interviews conducted over the telephone. The trained interviewers meticulously recorded telephone interviews using documented fieldnote techniques (Emerson, Fretz, & Shaw, 1995). All other interviews were audiotaped and transcribed verbatim. On average, interviews lasted about 14 minutes. Providers received $25.00 gift cards for their participation.
Data Analysis
We compared completed transcripts to audiotapes for accuracy and made any necessary revisions to the transcripts prior to coding. We used a whole text content analysis approach to guide data reduction, data display, and data synthesis (conclusion-drawing and verification) (Pope, Ziebland, & Mays, 2000; Strauss & Corbin, 1998). First, we transcribed the recorded interviews, paying particular attention to expressions, tone of voice, and other verbal mannerisms that informed the interview process. Two research team members trained in qualitative data coding and analyses then independently reviewed and coded each transcript; units of text consisted of each complete statement from participants. We used NVIVO qualitative analysis software (QSR International Pty Ltd., 2008) to import the transcribed interviews, label segments of text with codes, categorize quotes, group data and calculate frequencies for identified themes and categories. Coders noted emergent categories and themes during initial coding of transcripts and developed a final list of codes through consensus discussion by the research team. Coders categorized the final list of codes into an initial list of nine themes; after further team discussion, we integrated two of these themes into existing domains to yield the final seven themes: Access Factors, Cultural Beliefs and Preferences, Effects of Testing, Patient Motivators for Genetic Counseling and Testing, Reasons for Provider Referral, Patient-Provider Communication, and Reasons for Patient Refusal. For the few incidents in which text was coded differently by the two reviewers, we resolved these differences through team discussion prior to final analysis. Intercoder reliability was not calculated as data was coded to consensus.
RESULTS
Participants
We contacted 30 providers, 20 of who (66.7%) were available and agreed to participate in this study. The majority of the 10 providers who declined cited lack of time as the reason for non-participation. We did not collect demographic information from decliners. The final sample of 20 providers were from academic medical settings (n = 12) and community practices (n = 8) and represented the following disciplines: genetic counselors (n = 5), medical oncologists (n = 8), obstetrician/gynecologists (n= 2), and breast surgeons (n= 5). Participants had an average of 11.7 years in practice, with a range of 2 to 29 years. More than half (60%) were employed at a university hospital and most (85%) were female. Twenty-five percent (n = 5) of participants were African American, 60% Caucasian (n = 12), and 15% reported another race/ethnicity (n = 3; see Table I). All participants noted that at least 20% of their patient population consisted of African Americans.
Table I.
Characteristics of Providers (N=20)
| Provider Specialty | N | (%) |
|---|---|---|
| Medical Oncologists | 8 | 40 |
| Surgeons | 5 | 25 |
| Genetic Counselors | 5 | 25 |
| OB/GYN | 2 | 10 |
| Years in Practice | Average | Range |
|
| ||
| Total | 11.7 | 2–29 |
| Medical Oncologists | 13.3 | 2–29 |
| Surgeons | 10.8 | 2–22 |
| Genetic Counselors | 10 | 3–15 |
| OB/GYN | 11.5 | 11–12 |
| Work Site | N | (%) |
|
| ||
| Community Facility | 8 | 40 |
| University Hospital | 12 | 60 |
| Gender | % Male | % Female |
|
| ||
| Total | 15 | 85 |
| Medical Oncologists | 25 | 75 |
| Surgeons | 20 | 80 |
| Genetic Counselors | 0 | 100 |
| OB/GYN | 0 | 100 |
| Race | N | (%) |
|
| ||
| African American | 5 | 25 |
| Caucasian | 12 | 60 |
| Other | 3 | 15 |
Provider’s Perceptions and Practices
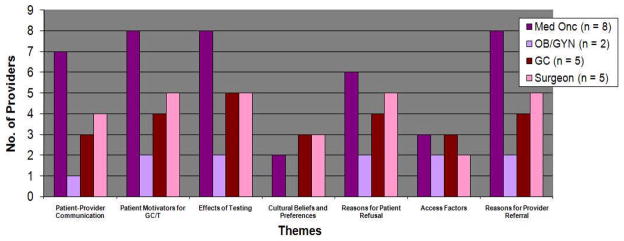
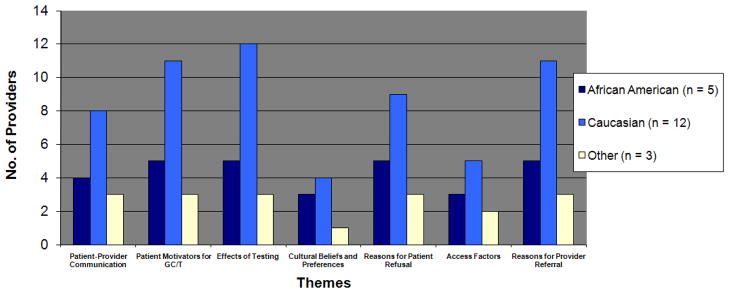
We identified seven major themes as factors relevant to healthcare providers’ perceptions of BRCA1/2 genetic counseling and testing in AAW. In Table II, we summarize the primary themes and sub-domains, indicate how often each theme and sub-domains were reported by providers during their interviews (each mention of an identified theme or sub-domain is called a “reference”) and provide exemplary quotes. Figures I and II provide the frequency of each theme as noted by provider specialty and provider race, respectively. Below we highlight key findings related to each theme with illustrative quotes followed by the provider specialty. We selected quotes that represent either key ideas related to each theme or unique perspectives regarding AAW’s use of BRCA1/2 genetic counseling and testing. Of note, in order to maintain participant confidentiality, we often did not indicate both the provider’s race and specialty at the same time.
Table II.
Identified Themes and Sample Quotes
| Theme | Providers (N = 20) | References to Theme (n = 227 total references) | Sample Quote | ||
|---|---|---|---|---|---|
| # mentioning theme | % mentioning theme | # of references | % of total references | ||
| Access Factors | n = 10 | 50% | n = 21 | 9.3% | “Many African Americans don’t have access to care. Money and cost issues keep them from obtaining the test.” Obstetrician/Gynecologist |
| Cultural Beliefs and Preferences | n = 8 | 40% | n = 15 | 6.6% | “There may be more cultural beliefs and values that [make African American women] less likely to be interested in genetic counseling and undergoing genetic testing. I think the African American community is more historically well-known for atrocities, for instance, Tuskegee…[or] not getting referred for a particular procedure they needed. That may cause people to be a little more distrustful.” Genetic Counselor |
| Effects of Testing | n = 20 | 100% | n = 52 | 22.9% | Beneficial: “It empowers people to find out [their risk of a BRCA1/2 mutation] and alleviate fears. It allows them to play an active role in their health by giving them something to cling to.” Obstetrician/Gynecologist Harmful: “It can certainly raise a person’s anxiety knowing that if they test positive [for a BRCA1/2 mutation] they are at an increased risk for breast cancer. It can make choices at times when they are otherwise healthy difficult, and it could be confounded, for example, if they don’t have good medical care or insurance.” Medical Oncologist |
| Patient Motivators for Genetic Counseling and Testing | n = 19 | 95% | n = 34 | 15% | “I think women are motivated by the fact that there is some degree of clarity on whether or not they should have risk reducing surgery or more intensive screenings, MRI,[or] breast exams.” Medical Oncologist |
| Reasons for Provider Referral | n = 19 | 95% | n = 29 | 12.8% | “Basically if women are [diagnosed with breast cancer] under fifty, you should consider it.” Medical Oncologist |
| Patient Provider Communication | n = 15 | 75% | n = 43 | 18.9% | “[There may be a] disconnect to how information [about genetic counseling and testing] is presented. [Is it done in a] culturally sensitive manner or is it not conveyed adequately to minorities?” Obstetrician/Gynecologist |
| Reasons for Patient Refusal | n = 17 | 85% | n = 33 | 14.5% | “I remember one [patient] who told me I don’t want anybody to peek into my private life. [Another patient] said, I think if I find out I have BRCA1 then…I won’t get health insurance because of discrimination.” Medical Oncologist |
Note: References indicate the number of times providers mentioned each theme/subdomain. Exemplar quotes were selected to highlight key ideas for each theme.
Figure I.
Themes Identified by Provider Specialty (N = 20)
Figure II.
Themes Identified by Provider Race
Access Factors
Half of the providers interviewed mentioned access to healthcare as a major factor that could help explain AAW’s underuse of BRCA1/2 genetic counseling and testing. These providers referenced factors such as access to knowledgeable genetics specialists, cost of counseling and testing, and insurance coverage. According to one obstetrician/gynecologist (ob/gyn) provider, “I think the problem is that many African Americans don’t have access to care, money, and the cost [of the test] keeps them from obtaining the test.” Additionally one genetic counselor noted that,
While some African American women may be interested in finding out more about BRCA testing because of a strong family history, the insurance companies may not reimburse for the [BRCA 1/2] test if women are unaffected with cancer or billed incorrectly…it’s all in the billing.
As such, it seemed that some providers perceived that AAW’s underuse was associated with healthcare system level barriers. More African American providers (60%) and providers from other racial backgrounds (66.7%) referenced “Access Factors” (e.g., cost and insurance) as deterrents to BRCA1/2 counseling and testing than did Caucasian providers (41.7%).
The larger problem is access to care, and there are areas where African American women don’t have access to breast specialists that know all about this [BRCA 1/2 counseling and testing]. Some primary care docs may know about it, but [it is] unlikely. - Breast Surgeon
Cost
Providers who referenced access factors described cost as a deterrent to genetic counseling and testing for breast cancer survivors and African American women in particular. This concern was voiced by practitioners from all specialties. One genetic counselor was concerned that the cost of the test would deter many physicians from actually referring their African American patients.
There have been studies…with other medical procedures [where] physicians tend to be less likely to refer [African American patients] for more expensive procedures [and] testing than White patients. - Genetic Counselor
Insurance Coverage
Several practitioners mentioned insurance coverage as a barrier to obtaining genetic counseling and testing in AAW but noted different aspects regarding when insurance might hinder the testing process. For example, genetic counselors, in particular, mentioned insurance coverage concerns as being a factor relevant to genetic counseling and testing utilization. Both medical oncologists (n = 2) and surgeons (n = 2) mentioned insurance coverage, or lack thereof, within the context of follow-up care for mutation carriers. Specifically, medical oncologists and surgeons noted that not having insurance could complicate an African American patient’s ability to afford the costs associated with risk management treatment options if she were a BRCA1/2 mutation carrier.
Something that comes up more often in the African American community is that they tend to be underinsured. So they might test positive and then not be able to get covered for…prophylactic surgeries. - Medical Oncologist
Only two providers (one genetic counselor and one surgeon) mentioned the financial hardship programs offered by genetic testing laboratories. These two providers expressed the difficulty of working with and navigating through financial hardship programs to help offset costs associated with genetic counseling and testing.
Although many African Americans tend to be underinsured, even if [AA] women wanted to get it [BRCA 1/2 counseling/testing] many of the hardship programs at labs aren’t the easiest to wade through. - Breast Surgeon
Despite a general consensus that lack of healthcare insurance often served as a barrier, one surgeon indicated that testing positive for a BRCA1/2 mutation could lead to better access and compensation for follow-up care. Genetic counselors (n = 2) and surgeons (n = 2) also mentioned that the stringent criteria of some insurance companies for covering genetic counseling and testing might prohibit appropriate genetic counseling candidates from obtaining this service.
Cultural Beliefs and Preferences
Sixty percent of African American providers mentioned cultural beliefs and preferences as being related to genetic counseling and testing versus 33% of the non-African American providers. The African American providers referenced “common” beliefs held by some African American women, such as “what’s going to happen will happen…and seeking out information about your future health really doesn’t fall in line with what God has in store for you.” Therefore, they underscored the need for all providers, especially genetic counselors, to recognize the important role cultural beliefs and spiritual practices play in the lives of AAW when discussing information about BRCA 1/2 counseling and testing. As such, these providers saw acknowledging the role of spirituality, for example, as a platform to incorporate teachable moments about BRCA1/2. Conversely, more non-African American providers tended to view faith in God as a possible deterrent to AAW seeking out genetic risk information. According to one medical oncologist, “a lot of the [African American] patients are very spiritual and religious…and they would say, it’s in God’s hands instead of doing something active.” Although non-African American providers did not mention cultural beliefs and practices as often, one genetic counselor suggested that acknowledging cultural beliefs and practices might make it easier for her to “find ways to best help these [AAW] women when they come to a [genetic counseling] session.”
Interestingly, one surgeon commented on the “importance that family plays in the lives of AAW” adding that “I think that… they can easily recruit for social support from other women…. African American women have figured out that the sisterhood thing really works.” This provider’s perception that AAW rely on “sisterhood” and “close family ties” was also voiced by African American providers as an important cultural belief/practice that providers should keep in mind as a platform to talk about BRCA1/2 counseling and testing. Additional cultural beliefs and preferences identified as potential influences on AAW’s genetic counseling and testing uptake included medical mistrust, fear of being labeled, being less open to the technology and being less involved in healthcare, as described below.
Medical Mistrust
Only one provider mentioned medical mistrust as a cultural factor in the underutilization of genetic counseling and testing in AAW. This provider noted historical examples, such as the Tuskegee Syphilis Study, which could account for the origin of mistrust. According to this provider:
I think the African American community is more historically well-known for atrocities, for instance, Tuskegee experiments and some other things that may have happened personally to people like not getting referred for a particular procedure they needed…that may cause people to be a little more distrustful of going from doctor’s visit to doctor’s visit…I think oftentimes [the reasons for distrust] is not understood and these cultural beliefs tend to be dismissed and overlooked, but I think they are very, very important in trying to understand why African Americans that have certain cultural beliefs…won’t participate. - Genetic Counselor
Fear of Being Labeled
Several providers (n = 3) mentioned that AAW might fear being labeled as having a genetic mutation following genetic counseling and testing, although more non-African American providers mentioned this fear compared to African American providers. One African American provider who did mention the idea of being labeled also commented on the uncertainty surrounding some genetic test results: “We’re dealing with a lot as African American women; do we really want something else sticking out there that we’re not even sure about…and the fact that those results are not 100%. Some people don’t find it very helpful to have that.” The non-African American providers noted that fear of being labeled as having a genetic mutation might make African Americans less “open” to genetic counseling and testing.
African American patients oftentimes tend to be more suspicious about [genetic testing]… because they’re so used to being pointed out all the time. And maybe they feel it’s another way of [labeling them]. - Medical Oncologist
Proactivity
Some participants viewed AAW as being less involved in their health compared to other women, while others disagreed. More African American providers made comments about AAW being less proactive in terms of health-related behaviors than non-African American providers. Comments from providers of various racial backgrounds included:
I don’t think African American women are as proactive as White women. - Breast Surgeon
We have some Caucasian patients that clearly don’t need to be tested and are clamoring for it, and it’s…the opposite in the African American community. - Breast Surgeon
Two genetic counselors also referenced perceptions of breast cancer risk as contributing to preventive or risk management behaviors. Specifically, these two providers mentioned that AAW’s lower sense of perceived risk may serve as a potential barrier to utilization of genetic counseling and testing.
We’re talking about future cancer risk, not something we know about right now. So, I think sometimes it’s perceived as not absolutely necessary that [they] come in - Genetic Counselor
A lot of African American women felt like they were doing what they could do as far as getting their mammograms every year. They just didn’t see how it would change what they were doing. They’d say, ‘This genetic testing isn’t going to help me to pick it up any earlier.’ If I’m already doing my screenings and everything I’m supposed to do, then how is this going to change my situation? - Genetic Counselor
Interestingly, only one provider noted that healthcare professionals might also view AAW at a lower objective risk for carrying a BRCA1/2 mutation.
With the whole counseling process and testing, I think there is a perception, it might even be among all healthcare workers too, that the gene isn’t as common in African Americans. - Breast Surgeon
Effects of Testing: Beneficial and Harmful
All providers interviewed mentioned both positive and negative effects of testing. Some of the positive effects of testing providers referenced included empowerment from having greater knowledge of risk, the opportunity for education about breast/ovarian cancer risk and alleviation of fear and anxiety. Providers reported psychological impact, false reassurance and guilt as some of the negative effects of testing. In mentioning both positive and negative effects of testing, all providers implicitly or explicitly recognized the personal, value-based nature of decision-making related to BRCA1/2 genetic counseling and testing.
Potential Beneficial Effects of Testing
Compared to non-African American providers, more African American providers commented that AAW might gain a sense of empowerment through the knowledge gained during genetic counseling. One surgeon commented, “It may provide motivation for them getting that needed screening.” Additionally, more African American providers noted that testing could lead to increased access to and use of screening and surveillance services.
Having that information…can be very empowering and may allow them to feel as if they have some control to be able to have access to better screening, more intense screening and surveillance measures or it may just simply motivate them to at least do the basics. - Genetic Counselor
More genetic counselors and medical oncologists made references to the alleviation of fear and anxiety about risk compared to providers from other specialties.
For a woman who has a strong family history she may learn that she doesn’t carry a familial genetic risk factor so she may be relieved from having to make various medical decisions. Sometimes gaining additional information about risk can be reassuring even if people learn that they’re at increased risk because at least they have information. - Genetic Counselor
Potential Harmful Effects of Testing
Negative effects of testing that providers noted included psychological effects of knowing one’s genetic status, false reassurance, guilt and challenges with family communication about genetic risk. Non-African American medical oncologists and genetic counselors were more likely to mention these effects of testing than other providers. Specifically, non-African American medical oncologists and genetic counselors noted that individuals who receive their test results are not able to “go back” after learning about genetic risk. According to one medical oncologist, “Some family members may not have wanted to know their status and it could cause problems…but once you know the information and you share it with your family you can’t go back.”
Some providers mentioned that, at times, women who receive negative genetic testing results may have feelings of false reassurance in which they underestimate their personal and family members’ breast cancer risk. Genetic counselors stressed the importance of post-test counseling to reduce the likelihood of false interpretation of test results. According to one, “…that post-test counseling is key and very important to help patients make sense of the results they get.” In addition to the potential for false reassurance, one surgeon mentioned guilt, describing the tension that can occur in families between those who test positive for the mutation and those who test negative.
If the mother has the gene, she feels like she might have tainted her offspring. If a sister doesn’t have the gene and her sister does, then the sister that doesn’t have it might feel guilty. – Breast Surgeon
Finally, compared to other providers, genetic counselors commented more often about the potential negative impact of test result on family communication, such as “carrier burden.”
In some situations, [it’s] a disadvantage that the first person to be tested in the family gets the job of having to spread the information to everyone and that can be somewhat of a burden for people. - Genetic Counselor
Patient Motivators for Genetic Counseling and Testing
Providers referenced patient motivators for counseling and testing, including concern for family, ability to make more informed medical decisions about risk management, and, for women affected with cancer, helping them more effectively manage their current diagnoses and treatment planning. One ob/gyn commented, “When I do see an interest, usually what emerges from women is that there is an interest because of the desire for knowledge or to figure how to proceed with treatment.” Most providers, regardless of specialty or racial group, mentioned concern for family as a primary motivator for AAW to pursue genetic counseling and testing.
Concern for Family
Providers felt women were strongly motivated to pursue testing out of concern for their children’s cancer risk, noting that this motivation was particularly true for female children. According to one surgeon, “…sometimes there is a desire for knowledge but mostly I see a desire to protect themselves and protect their daughters.” In contrast to the majority of participants, one provider felt that even when AAW women have strong family relationships, concern for family was not necessarily a motivator toward testing.
I would think that one strategy that we could use [to recruit AAW to genetic counseling and testing]…is, knowing that African American women are so very invested in their family, to say this will help you stay around longer for your family. At least in my experience, people were definitely concerned about their family, …[but] that didn’t…motivate them to have genetic testing. - Genetic Counselor
Issues related to medical decision-making and risk management were mentioned equally by the cancer specialists; however, only one of the ob/gyns mentioned this as a motivator.
I think women are motivated by the fact that there is some degree of clarity on whether or not they should have risk reducing surgery or more intensive screenings, MRI,[or] breast exams. - Medical Oncologist
Reasons for Provider Referral
Most participants (n = 19) mentioned at least one characteristic cited by the U.S. Preventive Services Task Force (i.e., multiple cases of breast cancer in the family and early age of diagnosis) as a reason for making a referral for BRCA1/2 genetic counseling and testing (Nelson, Huffman, Fu, Harris, & U.S. Preventive Services Task Force, 2005). None of the participants noted referral of patients based on history of both breast and ovarian cancer. None of the African American providers mentioned bilateral breast cancer or family history of male breast cancer as reasons for referral to genetic counseling. Only medical oncologists (n = 3) listed bilateral breast cancer as a reason for referral. Three medical oncologists and one surgeon mentioned referring patients with a family history of male breast cancer for genetic counseling. Other reasons for referral that providers mentioned that are not listed by the U.S. Preventive Services Task Force included late or delayed childbearing (ob/gyn), increased Gail risk score (surgeon and medical oncologist), per results of the Myriad assessment tool (surgeon), and triple-negative breast cancer (medical oncologists).
Medical oncologists were the only providers to mention a potential association of triple negative disease and likelihood of carrying a BRCA1/2 mutation. Triple negative breast cancer refers to breast cancers that do not involve estrogen, progesterone, or the Her-2 protein hormones. Triple negative breast cancers thus have fewer treatment options and are typically associated with higher rates of morbidity and mortality (Hurvitz & Finn, 2009). This type of breast cancer is more prevalent in AAW than Caucasian women (e.g., 35% vs. 22%; Stark et al. 2010) and other ethnic groups (Bauer, Brown, Cress, Parise, & Caggiano, 2007; Carey et al., 2006; Parise, Bauer, & Caggiano, 2010).
The fact [is] that African American women have more aggressive disease, the triple negative disease…and just being able to figure out potential treatments for these patients [may be helped by testing]. - Medical Oncologist
Patient-Provider Communication
Eighty percent of African American providers referenced patient-provider communication compared to 66.7% of non-African American providers and 100% of providers of other racial backgrounds. A higher percentage of surgeons (80%) and medical oncologists (87.5%) also referenced patient-provider communication compared to providers from the other specialties. According to one surgeon, “…I try to encourage them [AAW] to talk and ask questions…if I see that it [genetic BRCA 1/2 counseling and testing] is appropriate, I give them the information and try help them decide whether or not it is right for them.” In addition to patient-provider communication, African American providers expressed concern that other physicians may not discuss genetic counseling and testing in a culturally appropriate way, thus potentially contributing to lower use among this group. One non-African American provider commented, “[there may be a] disconnect to how information is presented…and I wonder if it is done in a culturally sensitive manner or is it not conveyed adequately to minorities?” Providers also discussed implications for family members, cultural factors, the provider’s role, and the overall counseling and testing process as factors related to patient-provider communication, as noted below.
Implications for Family Members
More non-African American providers, particularly those within the cancer specialties, mentioned discussing the implications of genetic test results for a woman’s family members. These providers noted that talking about the meaning of a woman’s test result in terms of relevance for children, primarily daughters, is quite important to the genetic counseling and testing experience of AAW women.
…[S]ometimes I would say, ‘think about how this [understanding the test result] will help you and your children’ and that seems to resonate at times with women…it seems to help with framing the conversation and them [AAW] understand the importance. - Medical Oncologist
The Provider’s Role
Providers saw their role in the genetic counseling and testing process as agents of information. Genetic counselors and medical oncologists were more likely to refer to themselves as having a specific role in the genetic counseling and testing process compared to providers from other specialties. One genetic counselor felt oncologists may be better at referring appropriate genetic counseling and testing candidates than primary care physicians noting, “…since they [oncologists] follow patient’s once they are diagnosed and may have a better idea of the patient’s family history, they may be better equipped to determine which patient is a good candidate, to make referrals to us.” Medical oncologists were more likely to mention their role in communicating the importance of genetic counseling and testing because of its impact on future cancer risk, while genetic counselors saw their role as primarily educating patients about their objective level of risk based on family and personal history and helping them understand the meaning of genetic test results.
Cancer providers mentioned their role as initiating a conversation about genetic counseling and testing “over time.” One oncologist noted an “innate fear of genetic testing” in AAW breast cancer survivors, describing the need to bring up the topic more than once.
I think it’s a conversation over time. There are some women who are ready to go through with it right away, and there are some women who you talk to them for years about it. - Medical Oncologist
I think there’s more of an innate fear of genetic testing, and…oftentimes, I end up talking to them about it multiple times. The only way I can believe I did my job is if I feel I educated them properly…it’s an education process. – Medical Oncologist
The Counseling and Testing Process
Medical oncologists and surgeons noted they did not follow up on recommendations made to their patients to see a genetic counselor.
Truthfully, we don’t ever follow up on that. Sometimes, we follow up sort of informally when I see them back, but I’m not sure if we have a real sense on who [is] getting it or not…. If they met with the counselor and genetic testing wasn’t recommended I don’t know that I would know that. – Breast Surgeon
Usually, I give them the contact information and either they show up or they don’t. - Medical Oncologist
They have to make that step to talk to the counselor first. - Medical Oncologist
Of note, none of the genetic counselors commented about whether physicians follow-up to see if their patients pursue genetic counseling in accord with the physician’s recommendations.
Reasons for Patient Refusal
The majority (85%) of the providers indicated one or more reasons why patients decline recommendations to pursue genetic counseling and testing, including women’s concerns over privacy and insurance discrimination, fear and uncertainty, and a lack of desire for the information.
Privacy and Insurance Discrimination
More non-African American providers mentioned concerns about privacy and potential insurance discrimination as reasons for patient refusal of genetic counseling and testing compared to African American providers. According to one surgeon, “I think they [AAW] are concerned about being discriminated against especially if they test positive.” Surprisingly, only four providers (two African American and two non-African American providers) mentioned the Genetic Information Non-Discrimination Act (GINA). Compared to other specialties, genetic counselors mentioned GINA more often. One genetic counselor mentioned the law’s shortcomings in providing protection against life and long-term care insurance discrimination as reasons why patients may refuse genetic counseling and testing.
“…the ones who don’t get it [BRCA 1/2 counseling and testing], the main reason was because of concerns about discrimination, discrimination by insurance companies mainly. Particularly, there’s no protection, there’s no laws to protect against life insurance discrimination, long-term care insurance discrimination.
So, those individuals that do not get tested, that was the main reason. - Genetic Counselor
Fear and Uncertainty
Genetic counselors described the fear and uncertainty surrounding a variant genetic test result, mentioning that, although more common among AAW, many AAW are not aware of this possible type of genetic test result. These providers emphasized the importance of discussing these types of test results with their African American patients. According to one genetic counselor, “It’s understandable that they [AAW] would be fearful when they get variant results…our job is to try and help women decide appropriate next steps.” Additionally, physicians also reported the difficultly in making management recommendations to patients with a variant result. One breast surgeon commented,
Well, I’ve had several patients, where the test came back as a mutation of unknown significance, and I feel that I’ve seen that more in African American patients than in White patients. They express concern but I don’t know what to make of it. But then, you are in a real quandary about how to treat these patients. Do you treat them as BRCA positive, or do you not? So far, what we try to do is…well, certainly in the young African American patients who come back with these mutations of unknown significance, we actually treat them as if they are BRCA positive. - Breast Surgeon
Lack of Desire for Information
Providers across all specialties mentioned that many patients just “don’t want to know” about genetic risk for cancer. One genetic counselor noted that familial influence may play a role AAW’s disinterest. According to this provider, “Sometimes they [AAW] just don’t want to know or are not ready to know yet…but sometimes it’s really the family that doesn’t want to know so they discourage it [getting tested].” Additionally, it was the perception of some providers that the value of BRCA1/2 genetic counseling and testing seemed less important for AAW in comparison to other issues (e.g., co-morbid conditions, family issues). One ob/gyn noted, “Well, I think sometimes they [AAW] don’t see it as worthwhile because they weren’t going to tell anybody anyway…sometimes they just don’t want to deal with it because they have too much going on.” Another provider added,
…many times they [AAW] are caught up in whatever else is going on, like if they have a new diagnosis of cancer that is obviously their primary concern…if they have to deal with other health conditions or if they have family issues…they will definitely put it on the backburner because there are other things that are going on…sometimes it’s just not the right time. – Genetic Counselor
DISCUSSION
Physician recommendation is an important predictor of who pursues BRCA1/2 genetic counseling and testing (Barnoy, Levy, & Bar-Tal, 2010; Hall & Olopade, 2005; Schwartz et al., 2005; Warner, Curnow, Polglase, & Debinski, 2005) and involvement of genetics professionals like genetic counselors leads to more informed decisions about testing (Keating et al., 2008) and risk management (Samphao et al., 2009). AAW women at high risk for carrying a BRCA1/2 mutation are less likely to pursue counseling and testing and thus we sought to explore health professionals’ opinions related to the genetic counseling and testing process for AAW. Building on prior research that has focused largely on individual-level factors as influential in AAW’s uptake of BRCA1/2 counseling and testing, the present study contributes important system-level information to further explore potential barriers and identify targets for patient- and provider-level education to improve AAW’s appropriate use of genetic counseling and testing clinical services.
Providers viewed genetic counseling and testing as critically important for high-risk AAW and, similar to suggestions within the medical genetics field (Domchek & Weber, 2008), noted that increasing participation among AAW in the testing process will ultimately help improve the interpretation of genetic test results in this population. Providers in the present sample indicated that informing AAW about genetic counseling and testing was often a process that occurred over time; however, several of the referring physicians (medical oncologists and surgeons) specifically remarked that they did not necessarily follow up with their patients to learn whether referrals to genetic counseling and testing resulted in actual counseling appointments.
Similar to results from studies evaluating patient-level barriers to genetic counseling and testing, almost all providers mentioned the impact of cost or insurance coverage as reasons why high-risk AAW may not pursue genetic testing (Hall et al., 2005; Suther & Kiros, 2009). Although genetic counselors in the present sample were familiar with the programs available to help economically disadvantaged women pay for testing, they noted that these programs are often challenging in terms of the process of obtaining approval.
Complex interpretation of the meaning of certain BRCA1/2 genetic test results—particularly variants of uncertain clinical significance which occur with greater frequency in African American women compared to Caucasian women (e.g., 44.2% vs. 27.9% respectively, Nanda et al., 2005)—was cited as a potential deterrent or complicating factor in AAW’s pursuit of genetic counseling and testing. Providers appeared to recognize that as greater numbers of AAW pursue testing, additional information will be available to help provide context for how genetic variants may impact future breast and ovarian cancer risk (Domchek & Weber 2008).
The present results should be interpreted in the context of the study’s limitations. Our sample of providers was selective, as the participants we interviewed routinely provide services to or refer women to genetic counseling and testing. As such, our sample is not representative of healthcare providers who are less familiar with issues related to hereditary breast and ovarian cancer syndromes. Given our qualitative analysis, presenting data from a select sample is a reasonable starting point for exploring system-level factors that may be relevant to AAW’s underuse of genetic counseling and testing services. The average duration of the interviews (14 minutes) was relatively short compared to other qualitative interviews (e.g., 45 minutes; Modin et al., 2010) and thus future work can build upon the present findings. For example, we did not ask providers to specifically compare AAW and Caucasian women, and thus it is important to note that certain barriers mentioned by our participants, such as the impact of genetic test results on family and potential for psychological distress in response to test results, are not unique to AAW women (Graves & Schwartz, 2007).
Based on study results, several potential clinical and policy implications can be considered. First, although providers appear to be sensitive to the potential barriers that might impede high-risk AAW women from seeking genetic counseling, few seem to follow up with patients regarding adherence to seeking out recommended referrals for counseling. Perhaps providers do not want to be overly directive or forceful in their approach to follow-up, or tracking adherence to referrals may be logistically complicated. Possible solutions to this issue can be taken into account by healthcare professionals and policy-makers. For example, some clinics implement standard family history collection forms and patients consent to be contacted if their personal or family histories meet a certain risk threshold. These types of risk assessment procedures may help reduce the burden on providers to ensure that patients receive information about genetic counseling programs. Providers might also want to discuss the benefits of genetic counseling more fully with patients, and emphasize that testing does not have to be pursued immediately or at all if not desired by the patient.
Second, awareness of and easy access to funds to pay for or waive the steep cost of genetic testing may be quite low. Genetic counselors appear to be familiar with the process of helping women through these procedures, but the process is often arduous and not always fruitful. Even for women who meet certain criteria related to the likelihood of carrying a BRCA1/2 mutation, the extent to which genetic counseling and testing services are covered by Medicaid varies across the country based on state policies. Moreover, high-risk women may encounter subsequent financial barriers should they choose to have intensive cancer surveillance (e.g., a breast MRI) or pursue prophylactic surgery for breast and ovarian cancer risk reduction. In addition, depending on the billing structures set up within different medical facilities, genetic counseling fees might not be reimbursed by insurance companies.
Third, even among our highly select sample of professional who were very familiar with genetic counseling and testing, only a small subset mentioned GINA. Healthcare providers outside of specialized areas may not be fully aware of the protections afforded through GINA. Eliciting patients’ concerns regarding the potential for insurance and/or employment discrimination may provide a “teachable moment” for providers to inform them about existing protections. Several informative websites and/or printed materials exist that providers can give to patients regarding GINA protection (e.g., Genetics and Public Policy Center at Johns Hopkins University 2010; National Coalition for Health Professional Education in Genetics 2010; U.S. Department of Health and Human Services 2009). Finally, providers raised very valid questions and concerns related to not knowing how to advise patients regarding the best practices for management of future risk following receipt of a test result involving a variant of uncertain clinical significance. As the evidence accumulates related to the meaning of these variants, both patients and professionals alike may have a clearer understanding of how to proceed. Providers can encourage patients to participate in research studies, which may help clarify the significance of these variants, and also encourage patients to keep current contact information on file so that they can be informed if additional information becomes available.
Our results also provide initial information on potential steps that genetic counselors might be able to take to help reduce barriers to BRCA1/2 genetic counseling and testing among AAW women. First, genetic counselors can align their services within hospitals and clinics that treat a large number of AAW. Setting up the infrastructure to provide specialized genetic counseling and testing services within diverse clinical settings might be challenging, but has certainly been done. For example, the clinical genetics service at Georgetown University Hospital – Lombardi Comprehensive Cancer Center has implemented care at an affiliated hospital one day a week to provide genetic counseling and testing to a largely minority and underserved population. Second, genetic counselors can work closely with the medical staff and physicians within oncology clinics and obstetrician-gynecology offices to establish direct communication and referral systems, such as through use of family history forms as mentioned above. In this way, either the medical staff or the genetic counselor can follow up with women appropriate for or referred to genetics services by their physician. Finally, genetic counselors or other medical personnel may be able to set up systems of referral for AAW women diagnosed with cancer at a young age through existing patient support or navigation programs at hospital- and community-based cancer centers.
Healthcare practitioners may not have expertise in cancer risk assessment; professionals in relevant specialty areas will have greater knowledge of and feel more comfortable identifying AAW women who are appropriate candidates for BRCA1/2 genetic counseling. Future research can examine the best ways to educate non-specialist physicians on how to take a family history so that high risk women can be referred to genetic counselors for more in-depth education about the benefits and limitations of BRCA1/2 genetic testing. With accumulating evidence suggesting the utility of patient navigation services for underserved cancer survivor populations (Davis, Darby, Likes, & Bell, 2009; Ell et al., 2009; Giese-Davis et al., 2006; Sheppard et al., 2010), incorporating genetics services into the array of patient education and supportive service options available may be one way to address the apparent gap in referrals to services and uptake of counseling and testing. In the interest of upholding the ethical principles of justice, it is important for all individuals to have access to genetic testing and follow-up services in both clinical and research contexts.
CONCLUSIONS
Healthcare professionals who treat AAW at high risk for breast cancer are cognizant of several patient-level factors that might influence appropriate uptake of BRCA1/2 genetic counseling and testing. System-level barriers to AAW’s use of counseling and testing appear to relate to lack of follow-up after a recommendation for counseling is made, the complicated processes for obtaining financial coverage of genetic counseling and testing services for under- or uninsured at-risk women, and the challenges inherent in interpreting variants of uncertain clinical significance. Recent additions to the objectives of Healthy People 2020 to increase the number of high risk women who receive BRCA1/2 genetic counseling and testing highlight the importance of these services for all women (U.S. Department of Health and Human Services, 2009). Improving high-risk AAW’s participation in genetics services and research has begun through exploration of both individual- and system-level barriers; these efforts should continue not only among individual AAW women and their providers, but also through renewed attention toward health policy and public awareness of genetic risk for cancer.
Acknowledgments
This study was funded by grants from the Jess and Mildred Fisher Center for Familial Cancer Research (2007-01: Sheppard) and the American Cancer Society (MRSGT–06-132-01 CPPB: Sheppard). The authors would like to thank the healthcare providers interviewed for this project for their time and comments. We also appreciate the contributions of Susan Marx, Yvonne Jennings and Yasmin Salehizadeh for their assistance with manuscript preparation.
Appendix: Interview Guide
What would you say are the advantages of genetic testing for breast and ovarian cancer risk.
What would you say are the advantages of genetic testing for breast and ovarian cancer risk to African American women specifically?
What are the disadvantages of genetic testing for breast and ovarian cancer risk?
What would you say are the disadvantages of genetic testing for breast and ovarian cancer risk to African American women specifically?
What causes you to refer a woman for genetic testing for breast and ovarian cancer risk?
What would prompt you to motivate an African American woman, in particular, for genetic testing for breast and ovarian cancer risk?
Where do you refer women for genetic testing for breast and ovarian cancer risk?
What has motivated women you see professionally to participate in genetic testing for breast and ovarian cancer risk?
Was there something unique or special you said to persuade them to participate? If so, please explain.
Out of the women you have referred for genetic testing for breast and ovarian cancer risk who refused or rejected your recommendation, what were the reasons?
References
- American Cancer Society. Breast Cancer Facts & Figures 2009–2010. Atlanta, GA: American Cancer Society, Inc; 2009. [Accessed July 10, 2010]. from http://www.cancer.org/acs/groups/content/@nho/documents/document/f861009final90809pdf.pdf. [Google Scholar]
- Armstrong K, Micco E, Carney A, Stopfer J, Putt M. Racial differences in the use of BRCA1/2 testing among women with a family history of breast or ovarian cancer. JAMA. 2005;293(14):1729–1736. doi: 10.1001/jama.293.14.1729. [DOI] [PubMed] [Google Scholar]
- Barnoy S, Levy O, Bar-Tal Y. Nurse or physician: whose recommendation influences the decision to take genetic tests more? Journal of Advanced Nursing. 2010;66(4):806–813. doi: 10.1111/j.1365-2648.2009.05239.x. [DOI] [PubMed] [Google Scholar]
- Bauer KR, Brown M, Cress RD, Parise CA, Caggiano V. Descriptive analysis of estrogen receptor (ER)-negative, progesterone receptor (PR)-negative, and HER2-negative invasive breast cancer, the so-called triple-negative phenotype: a population-based study from the California cancer Registry. Cancer. 2007;109(9):1721–1728. doi: 10.1002/cncr.22618. [DOI] [PubMed] [Google Scholar]
- Carey LA, Perou CM, Livasy CA, Dressler LG, Cowan D, Conway K, et al. Race, breast cancer subtypes, and survival in the Carolina Breast Cancer Study. JAMA. 2006;295(21):2492–2502. doi: 10.1001/jama.295.21.2492. [DOI] [PubMed] [Google Scholar]
- Chen WY, Garber JE, Higham S, Schneider KA, Davis KB, Deffenbaugh AM, et al. BRCA1/2 genetic testing in the community setting. Journal of Clinical Oncology. 2002;20(22):4485–4492. doi: 10.1200/JCO.2002.08.147. [DOI] [PubMed] [Google Scholar]
- Dangel J, Wagner-Costalas J, Bove B, Vanderveer L, Itzen M, Daly M, et al. Novel germline BRCA1 mutation (155del4) in an African American with early-onset breast cancer. Human Mutation. 1999;14(6):545. doi: 10.1002/(SICI)1098-1004(199912)14:6<545::AID-HUMU19>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- Davis C, Darby K, Likes W, Bell J. Social workers as patient navigators for breast cancer survivors: what do African American medically underserved women think of this idea? Social Work and Healthcare. 2009;48(6):561–578. doi: 10.1080/00981380902765212. [DOI] [PubMed] [Google Scholar]
- Doksum T, Bernhardt BA, Holtzman NA. Does knowledge about the genetics of breast cancer differ between nongeneticist physicians who do or do not discuss or order BRCA testing? Genetics in Medicine. 2003;5(2):99–105. doi: 10.1097/01.GIM.0000055198.63593.32. [DOI] [PubMed] [Google Scholar]
- Domchek S, Weber BL. Genetic variants of uncertain significance: flies in the ointment. Journal of Clinical Oncology. 2008;26(1):16–17. doi: 10.1200/JCO.2007.14.4154. [DOI] [PubMed] [Google Scholar]
- Donovan KA, Tucker DC. Knowledge about genetic risk for breast cancer and perceptions of genetic testing in a sociodemographically diverse sample. Journal of Behavioral Medicine. 2000;23(1):15–36. doi: 10.1023/a:1005416203239. [DOI] [PubMed] [Google Scholar]
- Edwards TA, Thompson HS, Kwate NO, Brown K, McGovern MM, Forman A, et al. Association between temporal orientation and attitudes about BRCA1/2 testing among women of African descent with family histories of breast cancer. Patient Education and Counseling. 2008;72(2):276–282. doi: 10.1016/j.pec.2008.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ell K, Vourlekis B, Xie B, Nedjat-Haiem FR, Lee PJ, Muderspach L, et al. Cancer treatment adherence among low-income women with breast or gynecologic cancer: a randomized controlled trial of patient navigation. Cancer. 2009;115(19):4606–4615. doi: 10.1002/cncr.24500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emerson RM, Fretz RI, Shaw LL. Writing ethnographic fieldnotes. Chicago, IL: University of Chicago Press; 1995. [Google Scholar]
- Gao Q, Neuhausen S, Cummings S, Luce M, Olopade OI. Recurrent germ-line BRCA1 mutations in extended African American families with early-onset breast cancer. American Journal of Human Genetics. 1997;60(5):1233–1236. [PMC free article] [PubMed] [Google Scholar]
- Gao Q, Tomlinson G, Das S, Cummings S, Sveen L, Fackenthal J, et al. Prevalence of BRCA1 and BRCA2 mutations among clinic-based African American families with breast cancer. Human Genetics. 2000;107(2):186–191. doi: 10.1007/s004390000290. [DOI] [PubMed] [Google Scholar]
- Genetics and Public Policy Center at Johns Hopkins University. [Accessed July 10, 2010];New educational resources on law against genetic discrimination now available. 2010 from http://www.dnapolicy.org/news.release.php?action+detail&pressrelease_id=139.
- Giese-Davis J, Bliss-Isberg C, Carson K, Star P, Donaghy J, Cordova MJ, et al. The effect of peer counseling on quality of life following diagnosis of breast cancer: an observational study. Psycho-oncology. 2006;15(11):1014–1022. doi: 10.1002/pon.1037. [DOI] [PubMed] [Google Scholar]
- Graves KD, Schwartz MD. Psychological and behavioral impact of genetic testing. In: Isaacs C, Rebbeck TR, editors. Hereditary breast cancer. 1. New York: Informa Healthcare; 2007. pp. 255–276. [Google Scholar]
- Halbert CH, Brewster K, Collier A, Smith C, Kessler L, Weathers B, et al. Recruiting African American women to participate in hereditary breast cancer research. Journal of Clinical Oncology. 2005;23(31):7967–7973. doi: 10.1200/JCO.2004.00.4952. [DOI] [PubMed] [Google Scholar]
- Halbert CH, Kessler L, Stopfer JE, Domchek S, Wileyto EP. Low rates of acceptance of BRCA1 and BRCA2 test results among African American women at increased risk for hereditary breast-ovarian cancer. Genetics in Medicine. 2006;8(9):576–582. doi: 10.1097/01.gim.0000237719.37908.54. [DOI] [PubMed] [Google Scholar]
- Halbert CH, Love D, Mayes T, Collier A, Weathers B, Kessler L, et al. Retention of African American women in cancer genetics research. American Journal of Medical Genetics Part A. 2008;146A(2):166–173. doi: 10.1002/ajmg.a.32067. [DOI] [PubMed] [Google Scholar]
- Hall M, Olopade OI. Confronting genetic testing disparities: knowledge is power. JAMA. 2005;293(14):1783–1785. doi: 10.1001/jama.293.14.1783. [DOI] [PubMed] [Google Scholar]
- Hall MA, McEwen JE, Barton JC, Walker AP, Howe EG, Reiss JA, et al. Concerns in a primary care population about genetic discrimination by insurers. Genetics in Medicine. 2005;7(5):311–316. doi: 10.1097/01.gim.0000162874.58370.c0. [DOI] [PubMed] [Google Scholar]
- Hall MJ, Reid JE, Burbidge LA, Pruss D, Deffenbaugh AM, Frye C, et al. BRCA1 and BRCA2 mutations in women of different ethnicities undergoing testing for hereditary breast-ovarian cancer. Cancer. 2009;115(10):2222–2233. doi: 10.1002/cncr.24200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes C, Fasaye GA, LaSalle VH, Finch C. Sociocultural influences on participation in genetic risk assessment and testing among African American women. Patient Education and Counseling. 2003;51(2):107–114. doi: 10.1016/s0738-3991(02)00179-9. [DOI] [PubMed] [Google Scholar]
- Hughes C, Gomez-Caminero A, Benkendorf J, Kerner J, Isaacs C, Barter J, et al. Ethnic differences in knowledge and attitudes about BRCA1 testing in women at increased risk. Patient Education and Counseling. 1997;32(1–2):51–62. doi: 10.1016/s0738-3991(97)00064-5. [DOI] [PubMed] [Google Scholar]
- Hughes C, Peterson SK, Ramirez A, Gallion KJ, McDonald PG, Skinner CS, et al. Minority recruitment in hereditary breast cancer research. Cancer Epidemiology, Biomarkers & Prevention. 2004;13(7):1146–1155. [PubMed] [Google Scholar]
- Hurvitz SA, Finn RS. What’s positive about ‘triple-negative’ breast cancer? Future Oncology. 2009;5(7):1015–1025. doi: 10.2217/fon.09.68. [DOI] [PubMed] [Google Scholar]
- Kinney AY, Croyle RT, Dudley WN, Bailey CA, Pelias MK, Neuhausen SL. Knowledge, attitudes, and interest in breast-ovarian cancer gene testing: a survey of a large African American kindred with a BRCA1 mutation. Preventive Medicine. 2001;33(6):543–551. doi: 10.1006/pmed.2001.0920. [DOI] [PubMed] [Google Scholar]
- Kinney AY, Simonsen SE, Baty BJ, Mandal D, Neuhausen SL, Seggar K, et al. Risk reduction behaviors and provider communication following genetic counseling and BRCA1 mutation testing in an African American kindred. Journal of Genetic Counseling. 2006;15(4):293–305. doi: 10.1007/s10897-006-9026-7. [DOI] [PubMed] [Google Scholar]
- Lipkus IM, Iden D, Terrenoire J, Feaganes JR. Relationships among breast cancer concern, risk perceptions, and interest in genetic testing for breast cancer susceptibility among African American women with and without a family history of breast cancer. Cancer Epidemiology, Biomarkers & Prevention. 1999;8(6):533–539. [PubMed] [Google Scholar]
- Matthews AK, Cummings S, Thompson S, Wohl V, List M, Olopade OI. Genetic testing of African Americans for susceptibility to inherited cancers. Use of focus groups to determine factors contributing to participation. Journal of Psychosocial Oncology. 2000;18(2):1–19. [Google Scholar]
- Metcalfe KA, Fan I, McLaughlin J, Risch HA, Rosen B, Murphy J, et al. Uptake of clinical genetic testing for ovarian cancer in Ontario: a population-based study. Gynecologic Oncology. 2009;112(1):68–72. doi: 10.1016/j.ygyno.2008.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Modin S. Family physicians’ experiences when collaborating with district nurses in home care-based medical treatment. A grounded theory study. BMC Family Practice. 2010;11:82. doi: 10.1186/1471-2296-11-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moorman PG, Skinner CS, Evans JP, Newman B, Sorenson JR, Calingaert B, et al. Racial differences in enrolment in a cancer genetics registry. Cancer Epidemiology, Biomarkers & Prevention. 2004;13(8):1349–1354. [PubMed] [Google Scholar]
- Nanda R, Schumm LP, Cummings S, Fackenthal JD, Sveen L, Ademuyiwa F, et al. Genetic testing in an ethnically diverse cohort of high-risk women: a comparative analysis of BRCA1 and BRCA2 mutations in American families of European and African ancestry. JAMA. 2005;294(15):1925–1933. doi: 10.1001/jama.294.15.1925. [DOI] [PubMed] [Google Scholar]
- National Coalition for Health Professional Education in Genetics. [Accessed July 9, 2010];The Genetic Information and Nondiscrimination Act (GINA): A discussion guide for clinicians. 2010 from http://www.nchpeg.org/index.php?option=com_content&view=article&id=97&Itemid=120.
- Nelson HD, Huffman LH, Fu R, Harris EL U.S. Preventive Services Task Force. Genetic risk assessment and BRCA mutation testing for breast and ovarian cancer susceptibility: systematic evidence review for the U.S. Preventive Services Task Force. Annals of Internal Medicine. 2005;143(5):362–379. doi: 10.7326/0003-4819-143-5-200509060-00012. [DOI] [PubMed] [Google Scholar]
- Newman LA. Breast cancer in African American women. Oncologist. 2005;10(1):1–14. doi: 10.1634/theoncologist.10-1-1. [DOI] [PubMed] [Google Scholar]
- Opatt DM, Morrow M, Daly M. The incidence of BRCA1 and BRCA2 variants of unknown significance caries in different ethnic populations. Journal of Clinical Oncology; 2006 ASCO Annual Meeting Proceedings Part I; 2006. Jun 20, p. 10002. Supplement. [Google Scholar]
- Pal T, Permuth-Wey J, Holtje T, Sutphen R. BRCA1 and BRCA2 mutations in a study of African American breast cancer patients. Cancer Epidemiology, Biomarkers & Prevention. 2004;13(11 Pt 1):1794–1799. [PubMed] [Google Scholar]
- Pal T, Vadaparampil S, Betts J, Miree C, Li S, Narod SA. BRCA1/2 in high-risk African American women with breast cancer: providing genetic testing through various recruitment strategies. Genetic Testing. 2008;12(3):401–407. doi: 10.1089/gte.2007.0108. [DOI] [PubMed] [Google Scholar]
- Parise CA, Bauer KR, Caggiano V. Variation in breast cancer subtypes with age and race/ethnicity. Critical Reviews in Oncology/Hematology. 2010;76(1):44–52. doi: 10.1016/j.critrevonc.2009.09.002. [DOI] [PubMed] [Google Scholar]
- Patterson AR, Davis H, Shelby K, McCoy J, Robinson LD, Rao SK, et al. Successful strategies for increasing African American participation in cancer genetic studies: hopeful signs for equalizing the benefits of genetic medicine. Community Genetics. 2008;11(4):208–214. doi: 10.1159/000116881. [DOI] [PubMed] [Google Scholar]
- Patton MQ. Qualitative research and evaluation methods. 3. Thousand Oaks, CA: Sage; 2002. [Google Scholar]
- Peters N, Rose A, Armstrong K. The association between race and attitudes about predictive genetic testing. Cancer Epidemiology, Biomarkers & Prevention. 2004;13(3):361–365. [PubMed] [Google Scholar]
- Pope C, Ziebland S, Mays N. Qualitative research in healthcare. Analysing qualitative data. BMJ. 2000;320(7227):114–116. doi: 10.1136/bmj.320.7227.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- QSR International Pty Ltd. NVIVO qualitative data analysis software (Version 8) [Computer software] 2008 Available from www.qsrinternational.com.
- Samphao S, Wheeler A, Rafferty E, et al. Diagnosis of breast cancer in women age 40 and younger: delays in diagnosis result from underuse of genetic testing and breast imaging. Am J Surg. 2009;198:538–543. doi: 10.1016/j.amjsurg.2009.06.010. [DOI] [PubMed] [Google Scholar]
- Schwartz MD, Lerman C, Brogan B, Peshkin BN, Isaacs C, DeMarco T, et al. Utilization of BRCA1/BRCA2 mutation testing in newly diagnosed breast cancer patients. Cancer Epidemiology, Biomarkers & Prevention. 2005;14(4):1003–1007. doi: 10.1158/1055-9965.EPI-03-0545. [DOI] [PubMed] [Google Scholar]
- Sheppard VB, Christopher J, Nwabukwu I. Breaking the silence barrier: opportunities to address breast cancer in African-born women. Journal of the National Medical Association. 2010;102(6):461–468. doi: 10.1016/s0027-9684(15)30553-8. [DOI] [PubMed] [Google Scholar]
- Sheppard VB, Williams KP, Harrison TM, Jennings Y, Lucas W, Stephen J, et al. Development of decision-support intervention for Black women with breast cancer. Psycho-oncology. 2010;19(1):62–70. doi: 10.1002/pon.1530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simon MS, Petrucelli N. Hereditary breast and ovarian cancer syndrome: the impact of race on uptake of genetic counseling and testing. Methods in Molecular Biology. 2009;471:487–500. doi: 10.1007/978-1-59745-416-2_25. [DOI] [PubMed] [Google Scholar]
- Stark A, Kleer CG, Martin I, Awuah B, Nsiah-Asare A, Takyi V, Braman M, Quayson SE, Zarbo R, Wicha M, Newman L. African ancestry and higher prevalence of triple-negative breast cancer: findings from an international study. Cancer. 2010;116(21):4926–32. doi: 10.1002/cncr.25276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strauss AL, Corbin J. Basics of qualitative research: Techniques and procedures for developing grounded theory. 2. Newbury Park, CA: Sage; 1998. [Google Scholar]
- Susswein LR, Skrzynia C, Lange LA, Booker JK, Graham ML, III, Evans JP. Increased uptake of BRCA1/2 genetic testing among African American women with a recent diagnosis of breast cancer. Journal of Clinical Oncology. 2008;26(1):32–36. doi: 10.1200/JCO.2007.10.6377. [DOI] [PubMed] [Google Scholar]
- Suther S, Goodson P. Barriers to the provision of genetic services by primary care physicians: a systematic review of the literature. Genetics in Medicine. 2003;5(2):70–76. doi: 10.1097/01.GIM.0000055201.16487.61. [DOI] [PubMed] [Google Scholar]
- Suther S, Kiros GE. Barriers to the use of genetic testing: a study of racial and ethnic disparities. Genetics in Medicine. 2009;11(9):655–662. doi: 10.1097/GIM.0b013e3181ab22aa. [DOI] [PubMed] [Google Scholar]
- Thompson HS, Valdimarsdottir HB, Duteau-Buck C, Guevarra J, Bovbjerg DH, Richmond-Avellaneda C, et al. Psychosocial predictors of BRCA counseling and testing decisions among urban African American women. Cancer Epidemiology, Biomarkers & Prevention. 2002;11(12):1579–1585. [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. [Accessed July 9, 2010];“GINA” The Genetic Information Nondiscrimination Act of 20008: Information for Researchers and Healthcare Professionals. 2009 from http://www.genome.gov/Pages/PolicyEthics/GeneticDiscrimination/GINAInfoDoc.pdf.
- U.S. Department of Health and Human Services. [Accessed July 9, 2010];Healthy People 2020 Public Meetings: 2009 Draft Objectives. 2009 from http://www.healthypeople.gov/hp2020/Objectives/files/Draft2009Objectives.pdf.
- Warner BJ, Curnow LJ, Polglase AL, Debinski HS. Factors influencing uptake of genetic testing for colorectal cancer risk in an Australian Jewish population. Journal of Genetic Counseling. 2005;14(5):387–394. doi: 10.1007/s10897-005-1623-3. [DOI] [PubMed] [Google Scholar]
- Wideroff L, Freedman AN, Olson L, Klabunde CN, Davis W, Srinath KP, et al. Physician use of genetic testing for cancer susceptibility: results of a national survey. Cancer Epidemiology, Biomarkers & Prevention. 2003;12(4):295–303. [PubMed] [Google Scholar]