Abstract
Tracheobronchopathia osteochondroplastica (TPO) is a rare, benign condition involving the trachea. TPO is characterised by osteocartilaginous nodules developing within the submuscosa of the trachea, sparing the posterior wall. We present the first documented case of TPO in Oman in a 25 year-old Omani male who presented with a recurrent, productive cough from which he had suffered throughout the previous two years. Diagnosis was made by characteristic computed tomography scan, bronchoscopic findings, and a histopathological examination.
Keywords: Tracheobronchopathia; Tracheobronchopathia osteoplastica; Tracheal stenosis; Tracheal disease, Ossification; tracheobronchial; Case report; Oman
Tracheobronchopathia osteochondroplastica (TPO) is a rare, benign condition involving the trachea, and possibly major bronchi. TPO was first described in detail by Wilks in 1857.1 Since then, cases have been reported sporadically throughout the world.
The disease is characterised by diffuse nodularities, or polyps, consisting of cartilaginous and/or osseous metaplastic tissue involving the anterior and lateral walls of the tracheobronchial tree and sparing the pars membranacea. The nodules are 1 to 3 mm in diameter and may cause narrowing and rigidity of the trachea and bronchi if the nodules larger in diameters which rarely hapen.2 The majority of people with TPO remain asymptomatic throughout their lives unless severe airway stenosis develops, in which case patients may experience symptoms such as dyspnoea, hoarseness, persistent and often productive cough, haemoptysis, and recurrent or slowly resolving pneumonia.3,4 Hence, this condition is usually discovered incidentally during bronchoscopy, or at autopsy or during difficult intubation,2,5 It seldom requires any treatment. Here we report possibly the first case of TPO in Oman.
Case Report
A 25 year-old Omani male who presented with a recurrent productive cough of two years duration was examined and further investigated for the underlying cause of unexplained recurrent chest infections. Other than fever during acute episodes of chest infection, he did not have haemoptysis, dyspnoea or weight loss. He was not known to have any chronic illness and had never been admitted to hospital. The patient had no history of smoking, recent travel or usage of illicit drugs. He is a radiographer by profession and his family history was unremarkable.
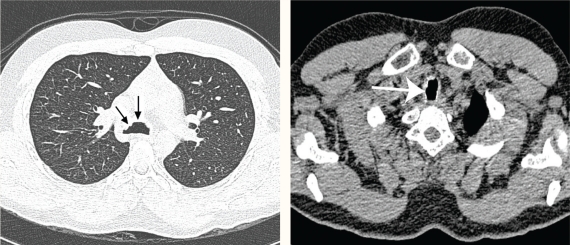
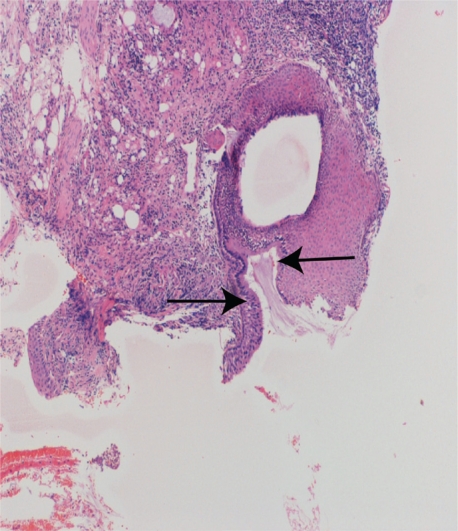
On clinical examination, his general condition was good, with no clubbing or lymphadenopathy, and a systemic examination was unremarkable. All routine blood tests were normal. Sputum microscopy and culture were negative for acid fast bacilli on three consecutive visits and the reaction to a tuberculin test was 10mm. A chest radiograph was normal; however, a plain computed tomography (CT) scan of the chest showed diffuse irregular thickenings of the tracheal wall, with the proximal bronchi, and the infraglottic part of the larynx as indicated by arrows in Figures 1a to 1c. Three subsequent CT scans showed no new changes and the nodularities persisted. Upon simultaneous bronchoscopy multiple whitish nodular lesions were seen in the tracheobronchial tree. A biopsy sample was taken from the right main bronchus and a histopathological examination revealed squamous metaplasia with hyperkeratosis as indicated by the arrows in Figure 2. Hence, after excluding malignancy, interstitial lung disease, and infection as the cause of the lesions, a presumptive diagnosis of endobronchial sarcoidosis was made and the patient was treated with prednisolone. A year later, another bronchoscopy was required due to recurrent chest infection with Klebsiella and Pseudomonas bacterial infections. At this second bronchoscopy, the lesions were still present; however, they had become softer and more fragile compared to the period before the start of systemic steroid treatment. Hence, in addition to prednisolone, gentamicin and ciprofloxacin were added to treat the pneumonia. At a repeat bronchoscopy a few months later, the lesions were still present, with widespread non-uniform thickening of the whole anterolateral tracheal wall along with the proximal bronchi and infraglottic area, sparing the posterior wall. In addition, small calcified papillary projections had also arisen from the lesions, which appeared to be submucosal in origin. A biopsy was taken and a histopathological examination showed cartilaginous tissue, squamous metaplasia, and hyperkeratosis, all features consistent with TPO. Therefore, prednisolone treatment was stopped and no further treatment offered.
Figure 1:
Sagittal section of trachea with arrows showing thickening and calcified lesions in the anterior wall of the trachea.
Figures 1b & 1c:
Axial sections of the chest with arrows showing thickening and calcified lesions in the anterior wall of the trachea.
Figure 2:
Histopatholgy of tracheal biopsy with arrows showing the squamous metaplasia with hyperkeratosis.
Discussion
TPO is an uncommon abnormality of the cartilaginous tracheal wall.6 Many cases of TPO have been reported since Wilks first identified it in 1857. In a study of 8,760 patients above 6 years of age who underwent bronchoscopy, Jabbardarjani et al. encountered 10 cases of TPO with a median age at diagnosis of 51 years, with a male predominance.7
TPO is characterised by osteocartilaginous nodules developing within the submucosa of the trachea and/or bronchi, sparing the posterior wall, and having a similar presentation to amyloidosis. Its aetiology is unknown, although, theories suggest chronic infection, congenital anomaly, chemical or mechanical irritation, degenerative or metabolic abnormalities, and genetic predisposition as possible factors contributing to a person developing TPO.8
The majority of patients remain asymptomatic unless they develop severe airway obstruction. In a retrospective review of 18 cases, patients had mainly experienced symptoms such as persistent and often productive cough, haemoptysis, dyspnoea and wheezing.9 Chest X-rays are usually normal, or may show signs of chest infections. Pulmonary function tests may also be normal or trace an obstructive type of flow-volume loop.3 Thus, diagnosis is mainly based on a CT scan showing irregular thickening and/or calcified nodularities protruding into the tracheobronchial lumen, and bronchoscopic findings of the same described as having a ‘rock garden’ or ‘cobblestone’ appearance.8 Further confirmation of the diagnosis is done by histopathologic examination of the biopsied tissue of the tracheal or bronchial walls at the site of the nodules. The tissue usually shows an osteocartilageous change, composed of a normal epithelium, but cartilage and bone tissue with intervening bone marrow.8 A magnetic resonance imaging (MRI) examination of the chest may show diffuse thickening of the trachea and bronchi with intermediate signal intensity, and punctiform low signal intensity suggesting calcifications and no enhancement.10
Differential diagnosis of these nodularities includes endobronchial sarcoidosis, amyloidosis, papilomatosis, tuberculosis, bronchial carcinoma, and tracheobronchial calcinosis. It is important to be aware of this condition as a differential diagnosis of neoplasms to avoid unnecessary chemotherapy or surgery.11
Treatment is seldom required except in patients with severe airway obstruction presenting with debilitating symptoms. In this case, bronchoscopic resectioning of the mass is the treatment of choice.12 Other treatment modalities include endobronchial Nd:YAG laser photoevaporation (LPE), coring of the lesions with the tip of a rigid bronchoscope, and endobronchial stent placement.7
Conclusion
TPO is a rare, benign condition characterised by diffuse nodularities consisting of cartilaginous or osseous metaplastic tissue which involves the trachea with or without the major bronchi. The condition is often asymptomatic unless the nodules are large enough to obstruct the airway. Diagnosis is usually based on a CT scan and bronchoscopic biopsy reports. Treatment is usually symptomatic except in the case of severe obstructions, when a surgical approach proves beneficial.
A diagnosis of TPO should be considered in patients who have an irregular thickening and/or calcified nodularities protruding into the tracheobronchial lumen, or who have similar bronchoscopic findings. A histopathological examination should always be carried out in order to distinguish TPO from other diseases that present similar types of radiological or bronchoscopic examination results.
Acknowledgments
We acknowledge with gratitude the help of Dr. Atheel Kamona, Senior Consultant Radiologist, and Dr. Sosama Thomas, Senior Consultant Histologist, of the Royal Hospital, for their contribution in the CT report and histology report, respectively.
References
- 1.Wilks S. Ossific deposit on the larynx, trachea and bronchi. Trans Pathol Soc Lond. 1857;8:88. [Google Scholar]
- 2.Williams SM, Jones ET. General case of the day. Radiographics. 1997;17:797–9. doi: 10.1148/radiographics.17.3.9153715. [DOI] [PubMed] [Google Scholar]
- 3.Bergeron D, Cormier Y, Desmeules M. Tracheobronchopathia osteochondroplastica. J Am Rev Respir Dis. 1976;114:803–6. doi: 10.1164/arrd.1976.114.4.803. [DOI] [PubMed] [Google Scholar]
- 4.Zack JR. Tracheobronchopathia osteochondroplastica: report of three cases. J Comput Assist Tomogr. 2002;26:33–6. doi: 10.1097/00004728-200201000-00006. [DOI] [PubMed] [Google Scholar]
- 5.Tadjeddein A, Khorgami Z, Akhlaghi H. Tracheobronchopathia osteoplastica: cause of difficult tracheal intubation. J Ann Thorac Surg. 2006;81:1480–2. doi: 10.1016/j.athoracsur.2005.04.013. [DOI] [PubMed] [Google Scholar]
- 6.Restrepo S, Pandit M, Villamil MA, Rojas IC, Perez JM, Gascue A. Tracheobronchopathia osteochondroplastica: helical CT findings in 4 cases. J Thoracic Imaging. 2004;19:112. doi: 10.1097/00005382-200404000-00010. [DOI] [PubMed] [Google Scholar]
- 7.Jabbardarjani HR, Radpey B, Kharabian S, Masjedi MR. Tracheobronchopathia osteochondroplastica: presentation of ten cases and review of the literature. Lung. 2008;186:293–7. doi: 10.1007/s00408-008-9088-4. [DOI] [PubMed] [Google Scholar]
- 8.Doshi H, Thankachen R, Philip MA, Kurien S, Shukla V, Korula RJ. Tracheobronchopathia osteochondroplastica presenting as an isolated nodule in the right upper lobe bronchus with upper lobe collapse. J Thorac Cardiovasc Surg. 2005;130:901–2. doi: 10.1016/j.jtcvs.2005.01.020. [DOI] [PubMed] [Google Scholar]
- 9.Vilkman S, Keistinen T. Tracheobronchopathia osteochondroplastica. Report of a young man with severe disease and retrospective review of 18 cases. J Respiration. 1995;62:151–4. doi: 10.1159/000196411. [DOI] [PubMed] [Google Scholar]
- 10.Hantous-Zannad S, Sebaï L, Zidi A, Ben Khelil J, Mestiri I, Besbes M, et al. Tracheobronchopathia osteochondroplastica presenting as a respiratory insufficiency: Diagnosis by bronchoscopy and MRI. Eur J Radiol. 2003;45:113–6. doi: 10.1016/s0720-048x(02)00028-1. [DOI] [PubMed] [Google Scholar]
- 11.Meyer CN. Tracheobronchopathia osteochondroplastica. J Respir Med. 1997;91:499–502. doi: 10.1016/s0954-6111(97)90117-7. [DOI] [PubMed] [Google Scholar]
- 12.Van Nierop MA, Wagenaar SS, van den Bosch JM, Westermann CJ. Tracheobronchopathia osteochondroplastica. Report of four cases. Eur J Respir Dis. 1983;64:129–33. [PubMed] [Google Scholar]