Abstract
Background/Aims
Endoscopic papillary large-balloon dilation combined with limited endoscopic sphincterotomy (EPLBD+ES) is promising for the treatment of common bile duct (CBD) stones. The aim of this study was to clarify the recurrence rate and the risk factors for CBD stones after EPLBD+ES.
Methods
In total, 100 patients who underwent EPLBD+ES from 2006 to 2007 were evaluated retrospectively. One hundred and nine patients who were treated with endoscopic sphincterotomy (ES) from 2004 to 2005 were set as the historical control group. Various risk factors for the recurrence of bile duct stones were analyzed.
Results
Of the 209 patients, the duration of follow-up was 32.5±4.5 months in the EPLBD+ES group and 31.8±6.0 months in the ES group. The recurrence rate of CBD stones was 11.0% (11/100) in the EPLBD+ES group and 13.8% (15/109) in the ES group (p=0.546). The cumulative recurrence rate of stones was not significantly different between the EPLBD+ES and ES groups (log rank, p=0.537). Univariate analysis showed that the diameter of the CBD (≥22 mm) was the only predictive variable that could differentiate recurrence from nonrecurrence in the EPLBD+ES group. Multivariate analysis revealed that the diameter of the bile duct was the only risk factor for stone recurrence (p=0.022; odds ratio, 1.175; 95% confidence interval, 1.023 to 1.348).
Conclusions
The recurrence rate of CBD stones after EPLBD+ES is comparable to that of the ES group, and a dilated CBD appears to increase the risk of bile duct stone recurrence.
Keywords: Endoscopic sphincterotomy, Endoscopic papillary large balloon dilation, Common bile duct stone
INTRODUCTION
Since introduction of endoscopic sphincterotomy (ES) by Classen and Demling1 and Kawai et al.2 in 1974, ES has been the standard therapy for treatment of various cholangiopancreatic diseases. Although ES has many advantages, substantial complications associated with ES have been reported. Acute pancreatitis, hemorrhage, duodenal perforation, and acute cholangitis are known to be short-term complications, and recurrence of stones and papillary stenosis are known to be long-term complications of ES.3-5
Endoscopic papillary balloon dilation (EPBD) was first described by Staritz et al.6 and has been advocated as an alternative to ES for facilitation of common bile duct (CBD) stone removal. The potential advantage of EPBD over ES is that it preserves the function of the biliary sphincter and possibly reduces the long-term sequelae of ES. However, due to certain limitations in the clinical setting in that the biliary opening is not enlarged to the same degree as with ES, mechanical lithotripsy is more frequently required for management of large stones.7-9 In addition, there have been a number of reports that EPBD was associated with a higher rate of post-procedure pancreatitis.10
Meanwhile, Ersoz et al.11 have suggested that EPBD with a large balloon following conventional ES might be a very effective method for retrieval of bile duct stones that were difficult to extract by a standard procedure. According to a few recent reports, endoscopic papillary large balloon dilatation (EPLBD) combined with limited ES (EPLBD+ES) has a similar therapeutic effect and is relatively safe in terms of complications for treatment of CBD stones.12,13 Complications, such as hemorrhage and perforation, were less frequent in EPLBD+ES, compared with conventional ES.14-16
Long-term study has shown that the incidence of recurrence of choledocholithiasis after ES is 5.8% to 24%.17-21 There are many descriptions of short-term results of EPLBD+ES; however, little is known about mid-term or long-term complications, such as recurrence of choledocholithiasis after EPLBD+ES.12-14,16 We conducted this study in order to evaluate the recurrence rate of CBD stones between the EPLBD+ES group and the ES group, and to determine the risk factors associated with recurrence of bile duct stones after EPLBD+ES.
MATERIALS AND METHODS
A total of 100 patients with bile duct stones larger than 1 cm in diameter (51 men, 49 women; mean age, 70.9±10.3 years) who underwent EPLBD+ES from May 2006 to December 2007 were studied retrospectively. A total of 109 patients with bile duct stones larger than 1 cm in diameter (48 men, 61 women; mean age, 71.9±12.9 years), who were treated with ES using a sphincterotome in a conventional manner from January 2004 to August 2005, were set as a historical control group. Patients were followed up until December 2009 in the EPLBD+ES group and until May 2007 in the ES group, to match the duration of follow-up between the two groups. Recurrence of CBD stones is defined as recurrence after 6 months of treatment with EPLBD+ES or ES. Exclusion criteria for this study were as follows: 1) patients with hepatolithiasis; and 2) patients with recurrent bile duct stones which were detected less than 6 months after EPLBD+ES or ES.
All endoscopic retrograde cholangiopancreatography (ERCP) procedures were performed using side-viewing endoscopes (TJF-240; Olympus Optical Co., Tokyo, Japan). These ERCPs were carried out by experienced endoscopists. Precutting with a needle knife or guide wire technique was applied in cases of difficult CBD cannulation. In the EPLBD+ES group, EPLBD was performed with a balloon dilator after small or medium ES. Once ES was completed, a guide wire was left in the biliary tree and a balloon dilator (CRE balloon; Boston Scientific Microvasive, Cork, Ireland) was advanced over the guide wire, positioning the middle portion of the balloon across the ampullary orifice. Under endoscopic and fluoroscopic guidance, the balloon was then inflated gradually with diluted contrast media until the notch on the balloon disappeared. Once the notch disappeared, inflation of the balloon was maintained for 30 to 60 seconds. A balloon dilator between 12 to 20 mm in diameter was used and the diameter of the balloon was determined according to the size of the stones. In the ES group, medium or large-sized ES with a pull-type sphincterotome was performed according to the size of CBD stones. The size of sphincterotomy was categorized as large (to the upper margin of the papillary roof), medium (below the upper margin), or small. For stones that were too large for removal in one session, an endoscopic mechanical lithotripsy was attempted in order to fragment the stones. When incomplete stone removal was suspected at the end of the procedure, an endoscopic nasobiliary drainage or plastic stent was inserted in order to prevent cholangitis.
The size and number of stones were documented on the cholangiogram after optimum opacification of the bile duct. Stone size was measured manually with the removed stone or assessed by comparison of the diameter of the stone with the shaft of the endoscope on the cholangiogram. In the same way, other factors including diameter and angulation were measured from the cholangiogram using PACS program (Infinitt, Seoul, Korea). The angulation was measured at the first angle from the ampullary orifice along the CBD. Complete stone removal was confirmed either by final cholangiogram just after ERCP or by follow-up cholangiogram through the nasobiliary drainage catheter. All recurrent CBD stones were confirmed by ERCP. Risk factors for recurrence of bile duct stones and mean intervals between the time of initial treatment and the time of recurrence of CBD stones were analyzed. The protocol was approved by the Institutional Review Board of our hospital.
Statistical analysis was performed using the Student's t-test and the chi-square test using SPSS version 13.0 (SPSS Inc., Chicago, IL, USA). Potential risk factors were assessed by univariate analysis on logistic regression and then a multivariate logistic regression model. Cumulative recurrence rates of bile duct stones during the follow-up intervals were compared using the Kaplan-Meier method. A p-value of less than 0.05 was considered statistically significant.
RESULTS
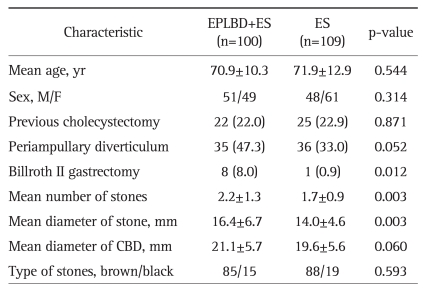
Demographic characteristics of the 209 patients are shown in Table 1. The gender ratio was similar in the two groups. The mean age was 70.9±10.3 years in the EPLBD+ES group and 71.9±12.9 years in the ES group. Billroth II gastrectomy was documented in 8 patients (8.0%) in the EPLBD+ES group and one patient (0.9%) in the ES group (p=0.012). The mean number of stones was 2.2±1.3 in the EPLBD+ES group and 1.7±0.9 in the ES group (p=0.003). The mean diameter of stones was 16.4±6.7 mm in the EPLBD+ES group and 14.0±4.6 mm in the ES group (p=0.003). No significant differences in age, sex, previous cholecystectomy or periampullary diverticulum were observed between the EPLBD+ES and ES groups. The diameter of the CBD was 21.1±5.7 mm in the EPLBD+ES group and 19.6±5.6 mm in the ES group; however, the difference between the two groups was not significant (p=0.060).
Table 1.
Characteristics of Patients between the EPLBD+ES Group and the ES Group at the Time of the Initial ERCP
Values are presented as mean±SD or number (%).
EPLBD+ES, endoscopic papillary large balloon dilation combined with limited endoscopic sphincterotomy; ES, endoscopic sphincterotomy; ERCP, endoscopic retrograde cholangiopancreatography; CBD, common bile duct.
The duration of follow-up was 32.5±4.5 months (range, 22 to 40 months) in the EPLBD+ES group and 31.8±6.0 months (range, 22 to 41 months) in the ES group. Of the 209 patients who underwent ERCP for choledocholithiasis, recurrent CBD stones appeared in 26 patients, with an overall recurrence rate of 12.4% during the follow-up period. The recurrence rate of CBD stones in the EPLBD+ES group was lower than that of the ES group; however, the difference was not significant (11.0% vs 13.8%, p=0.546) (Table 2). The mean interval between stone removal and stone recurrence in the EPLBD+ES and ES group was 17.2±11.8 months (range, 6 to 34 months) and 18.5±10.2 months (range, 6 to 35 months), respectively (p=0.758). Kaplan-Meier analysis revealed that the cumulative recurrence rate of bile duct stones between the EPLBD+ES group and the ES group was not significantly different (log rank, p=0.537) (Fig. 1).
Table 2.
Comparison of Patients with Recurrent Bile Duct Stones between the EPLBD+ES and the ES Groups at Follow-Up ERCP
Values are presented as the mean±SD (range) or number (%).
EPLBD+ES, e ndoscopic papillary large-balloon dilation combined with limited endoscopic sphincterotomy; ES, endoscopic sphincterotomy; ERCP, endoscopic retrograde cholangiopancreatography; CBD, common bile duct.
Fig. 1.
Kaplan-Meier plot for the cumulative recurrence rate of common bile duct stones in a total of 209 patients between the EPLBD+ES group and the ES group. No statistically significant difference was observed between the two groups (p=0.537, log-rank test). EPLBD+ES, endoscopic papillary large-balloon dilation combined with limited endoscopic sphincterotomy; ES, endoscopic sphincterotomy.
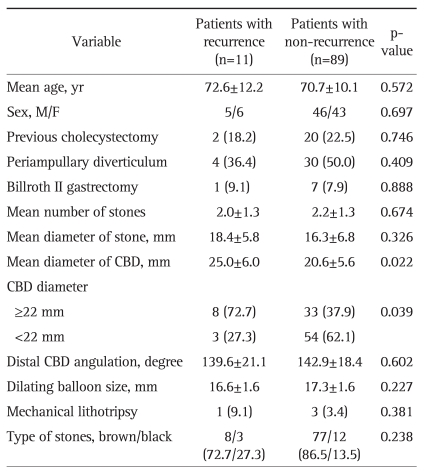
A variety of possible risk factors associated with recurrence of bile duct stones, including age, sex, previous cholecystectomy, periampullary diverticulum, Billroth II gastrectomy, the size of the bile duct, angulation of bile duct, dilating balloon size, the number, size, and type of stones, and mechanical lithotripsy are listed in Table 3. On univariate analysis, the diameter of the CBD was found to be the only predictive variable that could differentiate the recurrence group from the nonrecurrence group: the mean diameter of the CBD in the recurrence group was 25.0±6.0 mm (range, 14.3 to 34 mm), whereas that of the nonrecurrence group was 20.6±5.6 mm (range, 10.9 to 35.5 mm) (p=0.022). The diameter of the CBD ≥22 mm was identified to be the predictive factor for the recurrence of stones. Multivariate analysis determined that the diameter of the CBD was the single risk factor to distinguish the recurrence group from the nonrecurrence group (p=0.022; odds ratio, 1.175; 95% confidence interval, 1.023 to 1.348). None of the variables previously mentioned as not significant were able to provide any improvement to the final model.
Table 3.
Univariate Analysis of Risk Factors for Recurrent Bile Duct Stones after EPLBD+ES
Values are presented as mean±SD or number (%).
EPLBD+ES, endoscopic papillary large-balloon dilation combined with limited endoscopic sphincterotomy; CBD, common bile duct.
DISCUSSION
Since introduction of endoscopic papillary large balloon dilatation combined with limited ES (EPLBD+ES), many studies of the effectiveness of sequential ES and EPBD have been published.9,11-16 Currently, there are many descriptions of long-term complications after ES, including cholangitis, recurrent bile duct stones, and biliary pancreatitis.3,19,22 Reported incidence of recurrent choledocholithiasis after ES was 6% to 24%, and most recurrences occurred within the first 2 or 3 years after stone removal.17,19-21 Meanwhile, EPBD demonstrated a similar rate of recurrence.7,17,18 However, few studies on long-term follow-up results after EPLBD+ES have been reported.
Causes of recurrence of bile duct stones after ES are multi-factorial: bile stasis, bacterial infection of the bile duct, and duodenocholedochal reflux are known to play crucial roles in pathogenesis of recurrent stone formation.23,24 After ES, bile duct is susceptible to bacterial infection due to loss of sphincter function. Other studies have demonstrated that some bacterial species, e.g., E. coli, produce β-glucuronidase, which is a key enzyme in formation of brown pigment stones after sphicterotomy.25,26 In our study, recurrent bile duct stones in the EPLBD+ES group, as well as the ES group, were mainly brown pigment stones, indicating that secondary bacterial infection of the bile duct via the patulous ampullary opening plays a major role in the process of stone recurrence.
We postulated that, because EPLBD+ES could provide sufficient enlargement for complete removal of bile duct stones compared with ES, recurrence of choledocholithiasis is expected to be reduced. In our study, the recurrence rate of CBD stones in the EPLBD+ES group was lower than that of the ES group, although not statistically significant. In the present study, univariate and multivariate analysis determined that the diameter of the CBD was the only key factor accounting for the increased rate of recurrence of stones in the EPLBD+ES group.
A higher stone recurrence was reported in the gallbladder in situ with stones in the EPBD group (14%) and a very low recurrence rate after cholecystectomy.27 However, in our study, previous cholecystectomy was not associated with risk factors for recurrence. This finding is largely explained by the fact that recurrent stones in our cases were mostly brown stones, which were formed in the bile duct, rather than migrated from the gallbladder; thus, presence or absence of gallbladder appeared not to be associated with the risk of recurrence. Mechanical lithotripsy is frequently required for crushing large stones and is likely to increase the risk of recurrence because even a few missed tiny stone fragments may act as a nidus for stone reaggregation.21 However, lithotripsy was not a significant risk factor for recurrence in the present study. The reasons might be as follows: First, use of mechanical lithotripsy was rarely required in EPLBD+ES, because the papillary orifice can be fully opened. Second, more complete clearance of stone debris might be achieved after stone fragmentation, owing to wider enlargement of the ampullary opening. Periampullary diverticula compress the distal CBD anatomically, leading to bile stasis, and, subsequently, cause bacterial infection of the bile duct via the Oddi orifice.28 However, in our study, periampullary diverticulum was not found to be a risk factor for recurrent stones.
The degree of angulation along the course of CBD may contribute to the bile stasis and thus cause recurrence of stones. A study have reported that an angulation (≤145 degree) of CBD is a risk factor for the recurrence of stones.29 Meanwhile, other investigations demonstrated that distal angulation (≤135 degree) of bile duct was not associated with the recurrence of stones though it was a significant contributing factor to the technical difficulty of stone clearance.30,31 In this study, the angulation of the CBD was not a significant risk factor for recurrence. In fact, the exact measurement of angulation has a technical limitation in patients with anatomical variation of bile duct on a 2-dimensional plane. Balloon dilators, mainly 15 or 18 mm, were used to dilate the ampullary orifice. However, the size of balloons did not show a significant difference between the two groups. Size of the CBD is already known as an important predictor for recurrence of CBD stones. In the present study, the diameter of the CBD (≥22 mm) appears to be a risk factor for recurrent choledocholithiasis in the EPLBD+ES group. Costamagna et al.20 demonstrated that a bile duct diameter ≥22 mm was a prognostic factor for choledocholithasis. Some authors have identified bile duct size >15 mm as a risk factor for recurrent stones.18,21,32 A dilated CBD is likely to lead to bile stasis and bacterial infection, which play central roles in the mechanism of stone formation.20,24,33 There are some possibilities of small fragmented stones missed by cholangiogram in patients with a large bile duct.
In conclusion, although statistical significance was not observed between the EPLBD+ES group and the ES group in terms of the recurrence rate, in our experience, the frequency of recurrent bile duct stones in the EPLBD+ES group was lower than that of the ES group. Large size of the CBD was identified as the only significant predictive factor for increasing the recurrence rate of bile duct stones in the EPLBD+ES group. This study, however, has the limitation of retrospective data; therefore, further study is needed for investigation of the long-term outcome of EPLBD+ES.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Classen M, Demling L. Endoscopic sphincterotomy of the papilla of vater and extraction of stones from the choledochal duct (author's transl) Dtsch Med Wochenschr. 1974;99:496–497. doi: 10.1055/s-0028-1107790. [DOI] [PubMed] [Google Scholar]
- 2.Kawai K, Akasaka Y, Murakami K, Tada M, Koli Y. Endoscopic sphincterotomy of the ampulla of Vater. Gastrointest Endosc. 1974;20:148–151. doi: 10.1016/s0016-5107(74)73914-1. [DOI] [PubMed] [Google Scholar]
- 3.Cotton PB, Lehman G, Vennes J, et al. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc. 1991;37:383–393. doi: 10.1016/s0016-5107(91)70740-2. [DOI] [PubMed] [Google Scholar]
- 4.Freeman ML, Nelson DB, Sherman S, et al. Complications of endoscopic biliary sphincterotomy. N Engl J Med. 1996;335:909–918. doi: 10.1056/NEJM199609263351301. [DOI] [PubMed] [Google Scholar]
- 5.Bergman JJ, van Berkel AM, Groen AK, et al. Biliary manometry, bacterial characteristics, bile composition, and histologic changes fifteen to seventeen years after endoscopic sphincterotomy. Gastrointest Endosc. 1997;45:400–405. doi: 10.1016/s0016-5107(97)70151-2. [DOI] [PubMed] [Google Scholar]
- 6.Staritz M, Ewe K, Meyer zum Büschenfelde KH. Endoscopic papillary dilation (EPD) for the treatment of common bile duct stones and papillary stenosis. Endoscopy. 1983;15(Suppl 1):197–198. doi: 10.1055/s-2007-1021507. [DOI] [PubMed] [Google Scholar]
- 7.Mathuna PM, White P, Clarke E, Merriman R, Lennon JR, Crowe J. Endoscopic balloon sphincteroplasty (papillary dilation) for bile duct stones: efficacy, safety, and follow-up in 100 patients. Gastrointest Endosc. 1995;42:468–474. doi: 10.1016/s0016-5107(95)70052-8. [DOI] [PubMed] [Google Scholar]
- 8.Mac Mathuna P, White P, Clarke E, Lennon J, Crowe J. Endoscopic sphincteroplasty: a novel and safe alternative to papillotomy in the management of bile duct stones. Gut. 1994;35:127–129. doi: 10.1136/gut.35.1.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Maydeo A, Bhandari S. Balloon sphincteroplasty for removing difficult bile duct stones. Endoscopy. 2007;39:958–961. doi: 10.1055/s-2007-966784. [DOI] [PubMed] [Google Scholar]
- 10.Baron TH, Harewood GC. Endoscopic balloon dilation of the biliary sphincter compared to endoscopic biliary sphincterotomy for removal of common bile duct stones during ERCP: a metaanalysis of randomized, controlled trials. Am J Gastroenterol. 2004;99:1455–1460. doi: 10.1111/j.1572-0241.2004.30151.x. [DOI] [PubMed] [Google Scholar]
- 11.Ersoz G, Tekesin O, Ozutemiz AO, Gunsar F. Biliary sphincterotomy plus dilation with a large balloon for bile duct stones that are difficult to extract. Gastrointest Endosc. 2003;57:156–159. doi: 10.1067/mge.2003.52. [DOI] [PubMed] [Google Scholar]
- 12.Heo JH, Kang DH, Jung HJ, et al. Endoscopic sphincterotomy plus large-balloon dilation versus endoscopic sphincterotomy for removal of bile-duct stones. Gastrointest Endosc. 2007;66:720–726. doi: 10.1016/j.gie.2007.02.033. [DOI] [PubMed] [Google Scholar]
- 13.Kim HG, Cheon YK, Cho YD, et al. Small sphincterotomy combined with endoscopic papillary large balloon dilation versus sphincterotomy. World J Gastroenterol. 2009;15:4298–4304. doi: 10.3748/wjg.15.4298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Minami A, Hirose S, Nomoto T, Hayakawa S. Small sphincterotomy combined with papillary dilation with large balloon permits retrieval of large stones without mechanical lithotripsy. World J Gastroenterol. 2007;13:2179–2182. doi: 10.3748/wjg.v13.i15.2179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kochhar R, Dutta U, Shukla R, Nagi B, Singh K, Wig JD. Sequential endoscopic papillary balloon dilatation following limited sphincterotomy for common bile duct stones. Dig Dis Sci. 2009;54:1578–1581. doi: 10.1007/s10620-008-0534-1. [DOI] [PubMed] [Google Scholar]
- 16.Bang S, Kim MH, Park JY, Park SW, Song SY, Chung JB. Endoscopic papillary balloon dilation with large balloon after limited sphincterotomy for retrieval of choledocholithiasis. Yonsei Med J. 2006;47:805–810. doi: 10.3349/ymj.2006.47.6.805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ikeda S, Tanaka M, Matsumoto S, Yoshimoto H, Itoh H. Endoscopic sphincterotomy: long-term results in 408 patients with complete follow-up. Endoscopy. 1988;20:13–17. doi: 10.1055/s-2007-1018117. [DOI] [PubMed] [Google Scholar]
- 18.Ohashi A, Tamada K, Wada S, et al. Risk factors for recurrent bile duct stones after endoscopic papillary balloon dilation: long-term follow-up study. Dig Endosc. 2009;21:73–77. doi: 10.1111/j.1443-1661.2009.00835.x. [DOI] [PubMed] [Google Scholar]
- 19.Bergman JJ, van der Mey S, Rauws EA, et al. Long-term follow-up after endoscopic sphincterotomy for bile duct stones in patients younger than 60 years of age. Gastrointest Endosc. 1996;44:643–649. doi: 10.1016/s0016-5107(96)70045-7. [DOI] [PubMed] [Google Scholar]
- 20.Costamagna G, Tringali A, Shah SK, Mutignani M, Zuccalà G, Perri V. Long-term follow-up of patients after endoscopic sphincterotomy for choledocholithiasis, and risk factors for recurrence. Endoscopy. 2002;34:273–279. doi: 10.1055/s-2002-23632. [DOI] [PubMed] [Google Scholar]
- 21.Sugiyama M, Atomi Y. Risk factors predictive of late complications after endoscopic sphincterotomy for bile duct stones: long-term (more than 10 years) follow-up study. Am J Gastroenterol. 2002;97:2763–2767. doi: 10.1111/j.1572-0241.2002.07019.x. [DOI] [PubMed] [Google Scholar]
- 22.Fujita N, Maguchi H, Komatsu Y, et al. Endoscopic sphincterotomy and endoscopic papillary balloon dilatation for bile duct stones: a prospective randomized controlled multicenter trial. Gastrointest Endosc. 2003;57:151–155. doi: 10.1067/mge.2003.56. [DOI] [PubMed] [Google Scholar]
- 23.Bergman JJ, Rauws EA, Fockens P, et al. Randomised trial of endoscopic balloon dilation versus endoscopic sphincterotomy for removal of bileduct stones. Lancet. 1997;349:1124–1129. doi: 10.1016/S0140-6736(96)11026-6. [DOI] [PubMed] [Google Scholar]
- 24.Geenen DJ, Geenen JE, Jafri FM, et al. The role of surveillance endoscopic retrograde cholangiopancreatography in preventing episodic cholangitis in patients with recurrent common bile duct stones. Endoscopy. 1998;30:18–20. doi: 10.1055/s-2007-993722. [DOI] [PubMed] [Google Scholar]
- 25.Tanaka M, Takahata S, Konomi H, et al. Long-term consequence of endoscopic sphincterotomy for bile duct stones. Gastrointest Endosc. 1998;48:465–469. doi: 10.1016/s0016-5107(98)70086-0. [DOI] [PubMed] [Google Scholar]
- 26.Cetta F. Do surgical and endoscopic sphincterotomy prevent or facilitate recurrent common duct stone formation? Arch Surg. 1993;128:329–336. doi: 10.1001/archsurg.1993.01420150085016. [DOI] [PubMed] [Google Scholar]
- 27.Tsujino T, Kawabe T, Isayama H, et al. Management of late biliary complications in patients with gallbladder stones in situ after endoscopic papillary balloon dilation. Eur J Gastroenterol Hepatol. 2009;21:376–380. doi: 10.1097/MEG.0b013e328317f4a0. [DOI] [PubMed] [Google Scholar]
- 28.Lobo DN, Balfour TW, Iftikhar SY, Rowlands BJ. Periampullary diverticula and pancreaticobiliary disease. Br J Surg. 1999;86:588–597. doi: 10.1046/j.1365-2168.1999.01121.x. [DOI] [PubMed] [Google Scholar]
- 29.Keizman D, Shalom MI, Konikoff FM. An angulated common bile duct predisposes to recurrent symptomatic bile duct stones after endoscopic stone extraction. Surg Endosc. 2006;20:1594–1599. doi: 10.1007/s00464-005-0656-x. [DOI] [PubMed] [Google Scholar]
- 30.Baek YH, Kim HJ, Park JH, et al. Risk factors for recurrent bile duct stones after endoscopic clearance of common bile duct stones. Korean J Gastroenterol. 2009;54:36–41. doi: 10.4166/kjg.2009.54.1.36. [DOI] [PubMed] [Google Scholar]
- 31.Kim HJ, Choi HS, Park JH, et al. Factors influencing the technical difficulty of endoscopic clearance of bile duct stones. Gastrointest Endosc. 2007;66:1154–1160. doi: 10.1016/j.gie.2007.04.033. [DOI] [PubMed] [Google Scholar]
- 32.Pereira-Lima JC, Jakobs R, Winter UH, et al. Long-term results (7 to 10 years) of endoscopic papillotomy for choledocholithiasis. Multivariate analysis of prognostic factors for the recurrence of biliary symptoms. Gastrointest Endosc. 1998;48:457–464. doi: 10.1016/s0016-5107(98)70085-9. [DOI] [PubMed] [Google Scholar]
- 33.Fujimoto T, Tsuyuguchi T, Sakai Y, et al. Long-term outcome of endoscopic papillotomy for choledocholithiasis with cholecystolithiasis. Dig Endosc. 2010;22:95–100. doi: 10.1111/j.1443-1661.2010.00936.x. [DOI] [PubMed] [Google Scholar]