Abstract
Primary signet ring cell carcinoma (SRC) of colon at early stage is quite rare. Only 26 cases were reported until now. We report an early stage of primary SRC which was misdiagnosed as a juvenile polyp and treated with polypectomy followed by surgical resection. A 21-year-old male was administered for hematochezia. Abdominopelvic enhanced computed tomography revealed a polyp with active bleeding at the proximal rectum just below the rectosigmoid junction. Colonoscopy examination revealed a colon polyp with 0.5 cm sized head. Polypectomy was performed with snare and the polyp was completely removed. Biopsy revealed SRC. Surgical resection was also performed and there were no residual tumor or lymph node metastasis in the surgical specimen.
Keywords: Signet ring cell carcinoma, Early colon cancer, Juvenile polyp, Polypectomy
INTRODUCTION
Signet ring cell carcinoma (SRC) in the colon is rare and occurs earlier in life than other types of adenocarcinoma. SRC is usually diagnosed at advanced stages and has a poor prognosis.1,2 The gross morphology of SRC is usually scirrhous or ulcerated.1 We report a case of early stage primary SRC that was initially misdiagnosed as a juvenile polyp and treated with polypectomy followed by surgical resection.
CASE REPORT
A 21-year-old male was admitted to our institution for treatment of hematochezia. The patient had no previous medical history. His vital signs were stable and his hemoglobin level was 13.9 mg/dL. Abdominopelvic enhanced computed tomography (CT) revealed a polyp with active bleeding at the proximal rectum just below the rectosigmoid junction (Fig. 1). Colonoscopy revealed a Yamada type IV colon polyp with a head 0.5 cm in size in the proximal rectum. The head showed erythematous changes and surface erosions, and we therefore assumed that this polyp was the bleeding point. The polyp was initially diagnosed as a juvenile polyp after considering the patient's age, the gross morphology of the polyp and the history of bleeding. After hypertonic saline epinephrine injection, a snare polypectomy was performed and the polyp was completely removed (Fig. 2). The diagnosis was corrected to SRC after biopsy (Fig. 3). The patient's cancer was confined to the muscularis mucosa. Angiolymphatic invasion and tumor budding were not observed in the biopsy specimen. The longitudinal safety margin was 0.9 cm, and the lateral safety margin was 0.4 cm. We observed no dysplasia around the lesion. No additional lesions were found on positron emission tomography CT (PET CT) or esophagogastroduodenoscopy. Surgical resection was performed due to the polyp's poorly differentiated histopathology. There were no residual tumors or lymph node metastasis in the surgical specimen (Fig. 4).
Fig. 1.
Abdominopelvic enhanced computed tomography. A colon polyp with active bleeding is found.
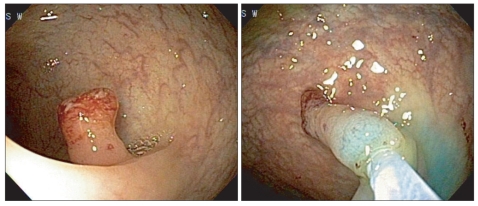
Fig. 2.
A Yamada type IV colon polyp was found at the proximal rectum. After a hypertonic saline epinephrine injection, the polyp was completely removed using a snare.
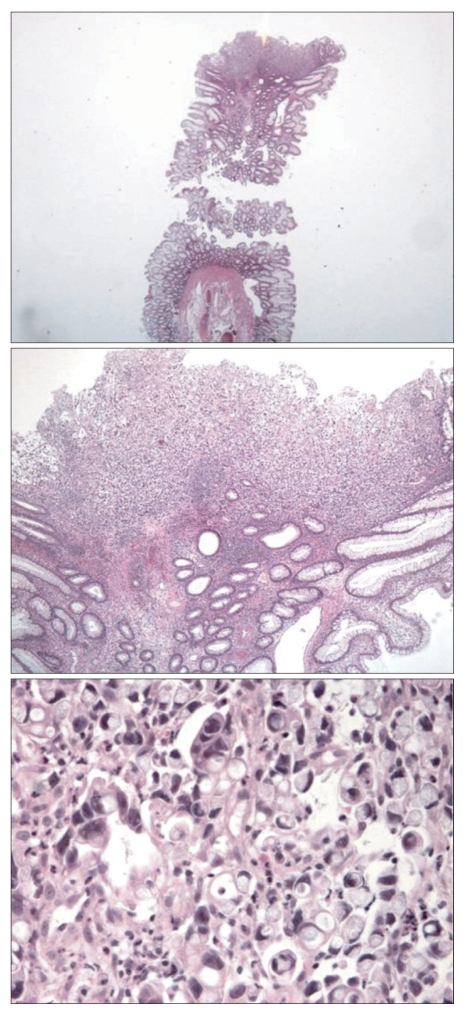
Fig. 3.
The biopsy specimen reveals a signet ring cell carcinoma of the colon. Tumor cells are not found at the resection margin (H&E stain, ×20, ×100, ×200).
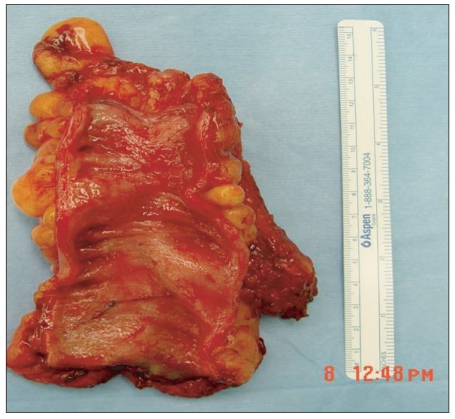
Fig. 4.
Surgical specimen. There is no residual tumor or metastasis to the lymph nodes.
DISCUSSION
More than 96% of cases of SRC arise in the stomach, and the rest occur in the colon, rectum, gallbladder, pancreas, urinary bladder, and breast.3 In the present case, the primary lesion was believed to be the rectum because no other organ involvement was detected by esophagogastroduodenoscopy, abdominal CT or PET CT. An additional surgical resection was performed due to a report indicating that lymph node metastasis often occurs in association with very small SRCs.4 The surgical specimen was free of lesions. In a previous study of 26 cases of early stage primary colon SRC2 with a mean age of 57.1 years (range, 6 to 69 years), six cases with mucosal cancer were documented, 16 with flat depressed lesions and 10 with polypoid lesions.2 SRC of the colon (including the advanced form) comprises about only 1% of all cases of colon cancer.2 When compared with other types of adenocarcinoma, patients with SRC in the colon are younger, more likely to experience lymph node metastasis and have a poorer prognosis.5 Colon cancer is rare in children and adolescents, with only 159 cases (ages, 4 to 20 years) reported between January 1974 and December 2005 worldwide. Young colon cancer patients experienced poorer prognoses than adults, and 18% of juvenile colorectal cancer cases were SRC.6 Common endoscopic characteristics of juvenile polyps are erythematous changes and erosion of the head. Bleeding is also quite common in juvenile polyps, making them even more difficult to diagnose. The practice of routine colonoscopy for health screening is increasing in South Korea, but in the absence of pain or bleeding, most physicians do not perform colonoscopies in younger patients, which results in late discovery of SRC, usually in the advanced form.
There are two proposed pathways for the origin of SRC: a de novo pathway and origination from adenoma.7,8 In the present case, few elongated glands were found in the head of the polyp, which laid under the signet ring cells. However, it is difficult to determine whether the lesion originated from a juvenile polyp due to the small number of elongated glands observed. We were unable to eliminate the possibility of malignant transformation from a juvenile polyp. We hypothesized that, in our case, SRC originated by the de novo pathway because we observed no dysplasia around the lesion. Due to the scarcity of reports regarding colon SRC, it is difficult to interpret the prognosis or natural history of this lesion. More case reports, accompanied by additional pathological and molecular biological studies, are required in order to establish an effective treatment strategy for primary SRC of the colon.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Makino T, Tsujinaka T, Mishima H, et al. Primary signet-ring cell carcinoma of the colon and rectum: report of eight cases and review of 154 Japanese cases. Hepatogastroenterology. 2006;53:845–849. [PubMed] [Google Scholar]
- 2.Fu KI, Sano Y, Kato S, et al. Primary signet-ring cell carcinoma of the colon at early stage: a case report and a review of the literature. World J Gastroenterol. 2006;12:3446–3449. doi: 10.3748/wjg.v12.i21.3446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tung SY, Wu CS, Chen PC. Primary signet ring cell carcinoma of colorectum: an age- and sex-matched controlled study. Am J Gastroenterol. 1996;91:2195–2199. [PubMed] [Google Scholar]
- 4.Urabe T, Kuroda Y, Urushihara T, Amano H, Yonehara S, Arihiro K. Two-mm diameter signet ring cell carcinoma of the rectum with lymph node metastasis: a report of case. Stomach Intest. 1998;33:1179–1183. [Google Scholar]
- 5.Nissan A, Guillem JG, Paty PB, Wong WD, Cohen AM. Signetring cell carcinoma of the colon and rectum: a matched control study. Dis Colon Rectum. 1999;42:1176–1180. doi: 10.1007/BF02238570. [DOI] [PubMed] [Google Scholar]
- 6.Sultan I, Rodriguez-Galindo C, El-Taani H, et al. Distinct features of colorectal cancer in children and adolescents: a populationbased study of 159 cases. Cancer. 2010;116:758–765. doi: 10.1002/cncr.24777. [DOI] [PubMed] [Google Scholar]
- 7.Tsujinaka Y, Tsuchiya S, Ooki S, et al. IIc type early carcinoma of the rectum originating "de novo", report of a case. Stomach Intest. 1983;18:211–217. [Google Scholar]
- 8.Nakamura T, Nakano G, Sakamoto K. Adenoma of the rectum with multiple foci of signet-ring cell carcinoma. Report of a case. Dis Colon Rectum. 1983;26:529–532. doi: 10.1007/BF02563747. [DOI] [PubMed] [Google Scholar]