Abstract
Background/Aims
The aim of this study was to evaluate the eradication rate of a triple therapy regimen that included a proton pump inhibitor, amoxicillin, and tetracycline instead of clarithromycin in treatment-Naïve patients and in patients who did not respond to standard triple therapy.
Methods
This study included 110 patients infected with Helicobacter pylori. Patients in groups A and B were treatment-Naïve, and those in group C were not responsive to previous standard triple therapy. Patients in group A (n=40) received lansoprazole 30 mg b.i.d., amoxicillin 1,000 mg b.i.d., and clarithromycin 500 mg b.i.d. for 14 days. Patients in groups B (n=40) and C (n=30) received lansoprazole 30 mg b.i.d., amoxicillin 1,000 mg b.i.d., and tetracycline 500 mg q.i.d. for 14 days.
Results
In group A, eradication was achieved in 18 (45%) of the 40 patients included in the intention-to-treat (ITT) analysis and in 18 (47.4%) of the 38 patients included in the per-protocol (PP) analysis. In group B, eradication was achieved in 15 (37.5%) of the 40 patients included in the ITT analysis and in 15 (39.3%) of the 38 patients included in the PP analysis. In group C, eradication was achieved in 14 (46.6%) of the 30 patients included in the ITT analysis and in 14 (43.8%) of the 29 patients included in the PP analysis. There was no statistically significant difference among the 3 groups with regard to eradication rates (p>0.05).
Conclusions
Despite the low rate of resistance to tetracycline, the combination of lansoprazole, amoxicillin, and tetracycline instead of clarithromycin is not a good option for the eradication of H. pylori.
Keywords: Helicobacter pylori, Tetracycline, Rescue therapy
INTRODUCTION
Helicobacter pylori is associated with chronic active gastritis, peptic ulcer, gastric adenocarcinoma, and mucosa-associated lymphoid tissue lymphoma.1-4 It was accepted as grade 1 carcinogen in 1994 by World Health Organization (WHO).5 While the prevalence of H. pylori frequency is decreasing in developed countries, it is increasing in developing countries.6 Although "test and treat" is an accepted approach in high prevalence locations such as Turkey, resistance to antibiotics is an important problem and eradication rate is decreasing worldwide.7 Clinically adequate regimens should provide H. pylori eradication in at 80% of patients, and should not cause any important adverse effect and clinically significant resistance to antibiotics. The most widely accepted standard triple therapy includes amoxicillin, clarithromycin and a proton pump inhibitor (PPI). However, eradication rates of this regimen are between 40% and 60%.8,9 Resistance to clarithromycin is considered to be the major reason for treatment failure. Tetracycline acts via impairing ribosome functions similar to clarithromycin.10 Since resistance develops to drug itself not to the action mechanism of the drug, we thought that tetracycline could be a good alternative in our country where the rate of resistance to clarithromycin is high. The aim of this study is to evaluate the eradication rate of triple therapy regimen including a PPI, amoxicillin, and tetracycline instead of clarithromycin both in treatment-naïve and those who did not respond to standard triple therapy.
MATERIALS AND METHODS
1. Patients
This prospective, randomized study included 80 treatment-naïve patients who presented to Haydarpaşa Numune Education and Research Hospital Gastroenterology Outpatient Clinic with H. pylori-positive nonulcer dyspepsia and 30 patients with H. pylori-positive nonulcer dyspepsia who previously did not respond to standard triple therapy for 14 days. The presence of H. pylori was assessed via histologic examination and rapid urease test (CLO® test) in treatment naive patients. During upper gastrointestinal endoscopy, two samples were taken from the gastric antrum for histologic assessment and rapid urease test. Patients were eligible for the study if both tests were positive for H. pylori. The presence of H. pylori was also assessed via the same methods in unresponsive patients prior to the previous therapy. Unresponsive patients were included into the study by confirming H. pylori-positivity with C14 urea breath test 4 to 6 weeks after completion of therapy.
Exclusion criteria included a history of treatment for H. pylori, upper gastrointestinal surgery, or gastric malignancy, impaired liver or renal function, pyloric stenosis, pregnancy, and a history of allergy to penicillin or any other antibiotic.
To prevent any interference with H. pylori eradication, patients that had taken bismuths salts, nonsteroidal antiinflammatory drugs, PPIs, H2 receptor blockers, antibiotics, or probiotics within the previous 4 weeks were also excluded. The study protocol was carried out in accordance with the Helsinki Declaration (2004 revision). All subjects were informed about the study protocol and provided written consent. The study protocol was approved by the local ethics committee.
2. Study design
This prospective, randomized study included 110 patients infected with H. pylori. Treatment-naïve H. pylori-positive nonulcer dyspepsia patients were randomized into group A and B according to presenting order (1:1). During the study period, patients who admitted to outpatient clinic with H. pylori-positive nonulcer dyspepsia and did not respond to previous standard triple therapy were included in group C.
Patients in group A (n=40) received lansoprazole 30 mg b.i.d. plus amoxicillin 1,000 mg b.i.d. plus clarithromycin 500 mg b.i.d. (LAC) for 14 days. Patients in group B (n=40) and C (n=30) received lansoprazole 30 mg b.i.d. plus amoxicillin 1,000 mg b.i.d. plus and tetracycline 500 mg q.i.d. (LAT) for 14 days.
Patients were asked for any side effects during treatment. Patient compliance was evaluated at the end of treatment by pill count and was considered good if >80% of the medication had been taken. Successful H. pylori eradication was defined as a negative 14C-urea breath test result 4 weeks after discontinuation of therapy.
3. Statistical analysis
All patients were evaluated with intention-to-treat (ITT) analysis, in which patients without a final H. pylori determination or with protocol violations were considered treatment failures. Per-protocol(PP) analysis included all subjects that took at least 80% of the study medication, as prescribed, and completed the final H. pylori status assessment. Statistical calculations were performed using SPSS version 11.0, 2000 software (SPSS Inc., Chicago, IL, USA). Results are presented as mean±standard deviation for quantitative variables, and as number and percentage for qualitative variables. Student's t-test and Mann Whitney U test were used for evaluation of the differences. Probability values less than 0.05 were considered significant.
RESULTS
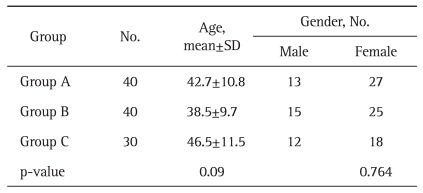
In all, 110 patients (70 females, 40 males) were analyzed with ITT analysis. The patients were randomized into group A (LAC) (n=40), group B (LAT) (n=40) and group C (LAT, not respond to LAC) (n=30). Demographic characteristics of these 3 treatment groups are shown in Table 1. There was no statistically significant difference between groups with regard to age and gender (p>0.05).
Table 1.
Demographic Characteristics of the Patients
SD, standard deviation.
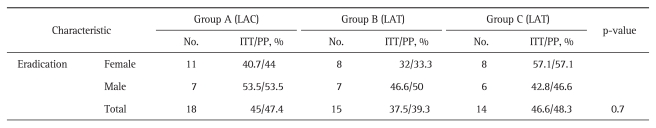
Two patients in group A, 2 patients in group B and 1 patient in group C did not return for the post-treatment follow-up. Accordingly, 38 patients in group A, 38 patients in group B, and 29 patients in group C were enrolled in the PP analysis. Eradication rates of 3 groups are shown in Table 2.
Table 2.
Eradication Rates of the Three Groups
LAC, lansoprazole 30 mg b.i.d. plus amoxicillin 1,000 mg b.i.d. plus clarithromycin 500 mg b.i.d.; LAT, lansoprazole 30 mg b.i.d. plus amoxicillin 1,000 mg b.i.d. plus and tetracycline 500 mg q.i.d.; ITT, intention-to-treat; PP, per-protocol.
One hundred and seven patients completed the study. In group A, H. pylori eradication was achieved in 18 (45%) of the 40 patients included in the ITT analysis and in 18 (47.4%) of the 38 patients included in the PP analysis. In group B, H. pylori eradication was achieved in 15 (37.5%) of the 40 patients included in the ITT analysis and in 15 (39.3%) of the 38 patients included in the PP analysis. In group C, H. pylori eradication was achieved in 14 (46.6%) of the 30 patients included in the ITT analysis, in 14 (43.8%) of the 29 patients included in the PP analysis. There was no statistically significant difference between 3 groups with regard to eradication rates (p>0.05). The relationship between gender and eradication rate was not significant (p>0.05).
The most common side effects were nausea and metallic taste in the mouth. Reported side effects were mild and treatment was well tolerated.
DISCUSSION
H. pylori is one of the most important causes in pathophysiology of gastroduodenal diseases. Eradication criteria were defined in the Maastricht III report, published by European H. pylori Study Group in 2005.11 Although "test and treat" is an accepted approach in high prevalence locations such as Turkey, resistance to antibiotics is an important problem and it has been reported that H. pylori eradication rate is decreasing throughout worldwide.7,11 Antibiotics used in H. pylori eradication have various mechanisms of action on the bacteria. Clarithromycin and tetracycline works via impairing ribosome functions, whereas metronidazole and quinolones work via bacterial DNA and RNA. Amoxicillin is destroys the bacterial cell wall. Bismuth salts have direct cytotoxic action on the bacteria.10
While clarithromycin inhibits protein synthesis by binding to 23S rRNA, tetracycline inhibits protein synthesis by binding to 16S rRNA of ribosome of the bacteria.12,13 Clarithromycin has been used more intensively than has tetracycline because of either its lower minimal inhibitor concentration or easy to use and its less frequent adverse effects. Acceptable eradication rates (>80%) were achieved with the use of clarithromycin initially; however, eradication rate has decreased to 40% over the time due to resistance in such locations where unnecessary antibiotic use is common.14,15 In Turkey, the rate of resistance to clarithromycin was 18.7% in 2000,16 while it reached to 41.9% in 2009.17 In an large randomized study performed in our country, eradication rate of standard triple therapy including omeprazole plus clarithromycin plus amoxicillin for 14 days was found to be 43%.18 A meta-analysis by Kadayifçi et al.8 revealed that H. pylori eradication rate of PPI-based triple therapy regimens was 84% in 1997 and decreased to 55.3% in 2004. Similar results were also reported in studies using a PPI plus amoxicillin plus clarithromycin for 1 week. Aydin et al.19 reported that eradication rate of this regimen was 93.3% in 1996 and 47.1% in 2004.
In the present study, we also found eradication rate of standard triple therapy to be very lower than 80%. To date, there is no study combining tetracycline with any agent other than metranidazole in the literature. Similarly, eradication rate was also low in treatment-naïve patients who received lansoprazole plus amoxicillin plus tetracycline. Despite the low rate of resistance to tetracycline, eradication rates are lower than expected probably as a result of that we can not provide sufficient antimicrobial concentrations with amoxycillin combination. Therefore, we can suggest that tetracycline, which is generally preferred in quadruple therapy (a PPI plus metronidazole plus tetracycline plus bismuth), is not suitable for combination in triple therapy.
Eradication rates in the group who did not respond to previous standard triple therapy-similar to naïve patients but far from the acceptable rates-is contraversial. Eradication rates in studies evaluating patients who did not respond to standard triple therapy are various. In a study performed by Matsumoto et al.,20 eradication rates of two different combinations including levofloxacin or metronidazole instead of clarithromycin in patients unresponsive to previous standard triple therapy were 73% and 96%, respectively. In another study performed by Perri et al.,21 three different combinations were used in such patients. Ranitidine bismuth citrate 400 mg b.i.d. plus amoxicillin 1 g b.i.d. plus tinidazole 500 mg b.i.d. (RBCAT) was given to the first group, pantoprazole 40 mg b.i.d. plus amoxycillin 1 g b.i.d. plus levofloxacin 500 mg once a day to the second group and pantoprazole 40 mg b.i.d. plus ranitidine bismuth citrate 240 mg b.i.d. plus tetracycline 500 mg q.i.d. plus metronidazole 500 mg b.i.d. to the third group. Eradication rates were 85%, 63%, and 83%, respectively.
Similar to low eradication rate of LAC due to increased rate of resistance to clarithromycin, we also achieved low eradication rates with the use of triple therapy including tetracycline instead of clarithromycin despite the low rate of resistance to tetracycline. This emphasizes the importance of other factors apart from resistance to antibiotics in H. pylori eradication.
In the light of all these results of the previous and our studies, we can conclude that triple therapy including a PPI plus amoxicillin plus tetracycline is not a good option in H. pylori eradication despite it has the same mechanism of action with clarithromycin and very low resistance rate. However, it should be noted that the number of patients was low in this study. There is need for studies evaluating the efficacy of this regimen including large patient groups.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Marshall BJ. The 1995 Albert Lasker Medical Research Award. Helicobacter pylori. The etiologic agent for peptic ulcer. JAMA. 1995;274:1064–1066. doi: 10.1001/jama.274.13.1064. [DOI] [PubMed] [Google Scholar]
- 2.Parsonnet J, Hansen S, Rodriguez L, et al. Helicobacter pylori infection and gastric lymphoma. N Engl J Med. 1994;330:1267–1271. doi: 10.1056/NEJM199405053301803. [DOI] [PubMed] [Google Scholar]
- 3.Blaser MJ, Berg DE. Helicobacter pylori genetic diversity and risk of human disease. J Clin Invest. 2001;107:767–773. doi: 10.1172/JCI12672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wilkinson M. Helicobacter pylori: an overview. Br J Biomed Sci. 2001;58:59–60. [PubMed] [Google Scholar]
- 5.Eslick GD, Lim LL, Byles JE, Xia HH, Talley NJ. Association of Helicobacter pylori infection with gastric carcinoma: a meta-analysis. Am J Gastroenterol. 1999;94:2373–2379. doi: 10.1111/j.1572-0241.1999.01360.x. [DOI] [PubMed] [Google Scholar]
- 6.Suerbaum S, Michetti P. Helicobacter pylori infection. N Engl J Med. 2002;347:1175–1186. doi: 10.1056/NEJMra020542. [DOI] [PubMed] [Google Scholar]
- 7.Kearney DJ. Retreatment of Helicobacter pylori infection after initial treatment failure. Am J Gastroenterol. 2001;96:1335–1339. doi: 10.1111/j.1572-0241.2001.03788.x. [DOI] [PubMed] [Google Scholar]
- 8.Kadayifçi A, Büyükhatipoğlu H, Koruk M, et al. Efficacy of a proton pump inhibitor plus amoxicillin plus clarithromycin in the eradication of H. pylori in Turkey: a meta-analysis. Turk J Gastroenterol. 2004;15(Suppl 1):5. [Google Scholar]
- 9.Güliter S, Keleş H, Ozkurt ZN, Cengiz DU, Kolukisa E. Can lansoprazole, amoxicillin, and clarithromycin combination still be used as a first-line therapy for eradication of Helicobacter pylori? Turk J Gastroenterol. 2005;16:29–33. [PubMed] [Google Scholar]
- 10.Katzung BG. Basic & clinical pharmacology. New York: McGraw Hill; 2006. pp. 726–771. [Google Scholar]
- 1.Malfertheiner P, Megraud F, O'Morain C. Guidelines for the management of Helicobacter pylori infection: summary of the Maastricht-3 2005 Consensus Report. European Gastroenterology Review 2005. London: Touch Briefings; 2005. [Google Scholar]
- 12.Moder KA, Layer F, König W, König B. Rapid screening of clarithromycin resistance in Helicobacter pylori by pyrosequencing. J Med Microbiol. 2007;56(Pt 10):1370–1376. doi: 10.1099/jmm.0.47371-0. [DOI] [PubMed] [Google Scholar]
- 13.Wu JY, Kim JJ, Reddy R, Wang WM, Graham DY, Kwon DH. Tetracycline-resistant clinical Helicobacter pylori isolates with and without mutations in 16S rRNA-encoding genes. Antimicrob Agents Chemother. 2005;49:578–583. doi: 10.1128/AAC.49.2.578-583.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Baglan PH, Bozdayi G, Ozkan M, Ahmed K, Bozdayi AM, Ozden A. Clarithromycin resistance prevalence and Icea gene status in Helicobacter pylori clinical isolates in Turkish patients with duodenal ulcer and functional dyspepsia. J Microbiol. 2006;44:409–416. [PubMed] [Google Scholar]
- 15.Toracchio S, Marzio L. Primary and secondary antibiotic resistance of Helicobacter pylori strains isolated in central Italy during the years 1998-2002. Dig Liver Dis. 2003;35:541–545. doi: 10.1016/s1590-8658(03)00265-2. [DOI] [PubMed] [Google Scholar]
- 16.Göral V, Zeyrek FY, Gül K. Antibiotic resistance in Helicobacter pylori infection. T Klin Gastroenterohepatol. 2000;11:87–92. [Google Scholar]
- 17.Bakir Ozbey S, Ozakin C, Keskin M. Antibiotic resistance rates of Helicobacter pylori isolates and the comparison of E-test and fluorescent in situ hybridization methods for the detection of clarithromycin resistant strains. Mikrobiyol Bul. 2009;43:227–234. [PubMed] [Google Scholar]
- 18.Gumurdulu Y, Serin E, Ozer B, et al. Low eradication rate of Helicobacter pylori with triple 7-14 days and quadriple therapy in Turkey. World J Gastroenterol. 2004;10:668–671. doi: 10.3748/wjg.v10.i5.668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Aydin A, Önder GF, Akarca US, et al. Efficacy of pantoprazole plus amoxicillin plus clarithromycin for 1 week and 2 weeks in the eradication of clarithromycin-sensitive and clarithromycinresistant H. pylori. Turk J Gastroenterol. 2004;15(Suppl 1):151. [Google Scholar]
- 20.Matsumoto Y, Miki I, Aoyama N, et al. Levofloxacin-versus metronidazole-based rescue therapy for H. pylori infection in Japan. Dig Liver Dis. 2005;37:821–825. doi: 10.1016/j.dld.2005.06.002. [DOI] [PubMed] [Google Scholar]
- 21.Perri F, Festa V, Merla A, Barberani F, Pilotto A, Andriulli A. Randomized study of different 'second-line' therapies for Helicobacter pylori infection after failure of the standard 'Maastricht triple therapy'. Aliment Pharmacol Ther. 2003;18:815–820. doi: 10.1046/j.1365-2036.2003.01755.x. [DOI] [PubMed] [Google Scholar]