Abstract
Previous studies have provided evidence that, in the early hours of ischemic stroke, a luminal membrane blood-brain barrier (BBB) Na-K-Cl cotransporter (NKCC) participates in ischemia-induced cerebral edema formation. Inhibition of BBB NKCC activity by intravenous bumetanide significantly reduces edema and infarct in the rat permanent middle cerebral artery occlusion model of ischemic stroke. We demonstrated previously that the BBB cotransporter is stimulated by hypoxia, aglycemia, and AVP, factors present during cerebral ischemia. However, the underlying mechanisms have not been known. Ischemic conditions have been shown to activate p38 and JNK MAP kinases (MAPKs) in brain, and the p38 and JNK inhibitors SB-239063 and SP-600125, respectively, have been found to reduce brain damage following middle cerebral artery occlusion and subarachnoid hemorrhage, respectively. The present study was conducted to determine whether one or both of these MAPKs participates in ischemic factor stimulation of BBB NKCC activity. Cultured cerebral microvascular endothelial cell NKCC activity was evaluated as bumetanide-sensitive 86Rb influx. Activities of p38 and JNK were assessed by Western blot and immunofluorescence methods using antibodies that detect total vs. phosphorylated (activated) p38 or JNK. We report that p38 and JNK are present in cultured cerebral microvascular endothelial cells and in BBB endothelial cells in situ and that hypoxia (7% O2 and 2% O2), aglycemia, AVP, and O2-glucose deprivation (5- to 120-min exposures) all rapidly activate p38 and JNK in the cells. We also provide evidence that SB-239063 and SP-600125 reduce or abolish ischemic factor stimulation of BBB NKCC activity. These findings support the hypothesis that ischemic factor stimulation of the BBB NKCC involves activation of p38 and JNK MAPKs.
Keywords: blood-brain barrier, stroke, cerebral edema, bumetanide, SB-239063, SP-600125
although cerebral edema is a major contributor to morbidity and mortality following ischemic stroke (9, 35), mechanisms of edema formation remain incompletely understood. Previous studies have shown that, during the early hours of an ischemic insult, brain edema forms by a process involving increased secretion of Na, Cl, and water across an intact blood-brain barrier (BBB) into the brain (4, 45, 53). This process also involves swelling of perivascular astrocytes as they take up the ions and water transported across the BBB (7, 28, 35). Vasogenic edema, a process involving influx of ions, water, and other plasma constituents from blood into brain due to significant increases in BBB paracellular permeability, generally occurs several hours after the onset of ischemia (21, 25, 35, 44, 53). Others and we hypothesized that ischemia-induced stimulation of one or more luminal BBB Na transporters results in increased secretion of Na from blood into brain, as luminal Na influx is functionally coupled to Na-K-ATPase-mediated abluminal Na efflux from the cells (8, 15, 18, 34, 48, 49, 51, 53). Our previous studies provided evidence that both the luminal BBB Na-K-Cl cotransporter and Na/H exchanger are stimulated by hypoxia, aglycemia, and AVP (8, 18, 33, 37, 48, 49), prominent factors present during cerebral ischemia. In addition, inhibition of BBB Na-K-Cl cotransporter and Na/H exchanger activities by intravenous administration of bumetanide and HOE-642, respectively, significantly reduces edema, brain Na uptake, and infarct in the rat permanent middle cerebral artery occlusion (MCAO) model of stroke (11, 12, 48, 51). Thus, targeting these BBB Na transporters appears to be a promising therapeutic avenue for reduction of edema in ischemic stroke. Nonetheless, the signaling pathways whereby ischemic factors stimulate activities of these BBB Na transporters are poorly understood. A number of studies have investigated signaling mechanisms involved in ischemic stroke; however, the vast majority of those studies focused on astrocytes and/or neurons. It is now well recognized that BBB endothelial cells, together with astrocytes and neurons, are major participants in neurovascular unit function (46, 48) in health and disease. In this regard, understanding how BBB endothelial cells respond to ischemia and, among other things, participate in cerebral edema formation is critically important for identifying potential stroke treatments, including development of prophylactic therapies to prevent ischemia-induced edema formation in patients at risk for stroke.
The p38 and JNK MAP kinases (MAPKs) have been recognized as key mediators of cell responses to a variety of stresses, including ischemia (13, 29, 36). Activation of p38 is achieved by dual phosphorylation (on Thr180 and Tyr182) by upstream kinases (13, 29, 36) in response to hypoxic or ischemic conditions in a variety of cell and tissue types, including perfused rat heart (5), cultured cortical neurons (63), and cerebral microvascular endothelial cells (CMEC) (38, 64). Previous studies have shown that p38 activity is increased in rat cerebral cortex within 15 min of the onset of MCAO-induced ischemia (1, 58) and, furthermore, that the highly selective inhibitor of p38, SB-239063, reduces infarct volume and neurological deficit (1, 2). Similar to p38, JNK is also activated by dual phosphorylation (on Thr183 and Tyr185) via upstream kinases (13, 29, 36) and can be activated in response to hypoxia and ischemia in a variety of cell types (3, 29, 62). Previous studies have also shown that JNK is activated by transient ischemia in rat and mouse cerebral cortex and hippocampus (26, 27, 57) and that inhibition of JNK reduces cerebral infarct in rat and mouse models of transient and permanent ischemia (6, 22, 62). The observations that cerebral p38 and JNK activities are elevated during ischemia and that inhibition of the kinases reduces infarct, together with the finding that the BBB Na-K-Cl cotransporter is also stimulated during cerebral ischemia and appears to contribute to edema formation and infarct, suggest that p38 and/or JNK MAPKs may participate in ischemic factor stimulation of BBB Na-K-Cl cotransporter activity and, thereby, contribute to cerebral edema formation and infarct during ischemic stroke.
Previous studies have shown that AMP-activated protein kinase (AMPK), also known to respond to a variety of stresses (10, 23, 24), is activated in mouse and rat brain by transient ischemia (40, 43) and that the consequent brain infarct is reduced by the AMPK inhibitor compound C (41, 43). Recently, we found that ischemic factors, including hypoxia, aglycemia, and AVP, rapidly activate AMPK and increase Na-K-Cl cotransporter activity in CMEC in a manner inhibited by compound C (60). However, we also found that CMEC AMPK activation, while rapid, is transient and not sustained for the duration of elevated Na-K-Cl cotransporter activity (60). This further suggests that other signaling pathways, in particular p38 and JNK MAPKs, may participate in the BBB endothelial cell response to cerebral ischemia.
The present study was conducted to investigate the involvement of p38 and JNK MAPKs in ischemia-induced stimulation of BBB Na-K-Cl cotransporter activity. We report here that both p38 and JNK activities are rapidly increased in CMEC following exposure to hypoxia, aglycemia, AVP, or O2-glucose deprivation (OGD), although the time courses and magnitudes of activation vary with kinase and ischemic factor. We also report that SB-239063 and SP-600125, highly selective inhibitors of p38 and JNK, respectively, reduce or abolish ischemic factor stimulation of CMEC Na-K-Cl cotransporter activity. Finally, we demonstrate the presence of activated p38 and JNK in BBB endothelial cells in situ.
MATERIALS AND METHODS
CMEC culture.
Cultured bovine CMEC were maintained in DMEM containing 5 mM d-glucose and 1 mM Na pyruvate and supplemented with 2 mM l-glutamine, 50 μg/ml gentamicin, 1 ng/ml basic fibroblast growth factor, 5% calf serum, and 5% horse serum in 95% air-5% CO2 at 37°C, as described previously (18). For Western blot and Na-K-Cl cotransporter activity experiments, CMEC were grown on 6- and 96-well plates, respectively, that were coated with 50 mg/l rat tail collagen, 5 mg/l fibronectin, and 10 mg/l bovine serum albumin for 7–10 days until confluent. Growth medium was replaced every ∼48 h with fresh medium. At 48 h prior to the experiment, the medium was changed to a 50:50 (vol/vol) mixture of fresh DMEM containing 5% calf serum and 5% horse serum and astrocyte-conditioned medium containing 10% FBS. Astrocyte-conditioned medium was prepared using primary cultures of rat neonatal astrocytes, as described previously (49, 50).
Western blot analysis of p38 and JNK MAPK activation.
Abundance of total p38 protein and phosphorylated (activated) p38 (p-p38) protein was assessed by Western blot analysis using antibodies that specifically detect p38 (nonphosphorylated and phosphorylated) or only p-p38. Similarly, abundance of total JNK protein and phosphorylated (activated) JNK (p-JNK) protein was assessed using antibodies that specifically detect JNK (nonphosphorylated and phosphorylated) or only p-JNK. Western blot analysis was performed as described by us previously (37, 60). For these experiments, CMEC monolayers on six-well plates were placed in a hypoxia chamber (COY Laboratory Products, Grass Lake, MI) preset to 37°C with an atmosphere of 5% CO2 and 19%, 7%, or 2% O2 (normoxia, moderate hypoxia, and severe hypoxia, respectively), as described by us previously (18, 60). O2 levels in the chamber and in treatment media were verified by the chamber O2 sensor/regulator and by a dissolved O2 sensor (Corning) with a Checkmate II meter (Corning). Immediately after CMEC were placed in the chamber, growth medium was removed, wells were rinsed once with the appropriate treatment medium preequilibrated to the desired O2 level, and the cells were incubated in that medium for 5, 30, 60, or 120 min. The treatment medium was DMEM with 10 mM HEPES (HEPES-DMEM) containing (in mM) 5.6 d-glucose, 1.0 Na pyruvate, 156 Na+, 119 Cl−, 5.3 K+, 1.8 Ca2+, 44.1 HCO3−, 0.91 H2PO4−, 0.81 Mg2+, and 0.81 SO4−. In experiments testing the effects of aglycemia, glucose and Na pyruvate were omitted from the HEPES-DMEM. For experiments testing the effects of OGD, cells were exposed to hypoxic (2% O2) glucose- and pyruvate-free HEPES-DMEM. In some experiments, normoxic HEPES-DMEM containing AVP (100 nM) was used.
At the end of the exposure period, CMEC monolayers were rinsed three to four times with ice-cold PBS plus protease inhibitors (Complete Protease Inhibitor Cocktail, Roche Diagnostic) and phosphatase inhibitors (100 nM NaF and 100 mM Na pyrophosphate). Cells were then lysed with PBS containing 5 mM EDTA, 20 mM HEPES, 150 mM NaCl, 50 nM Na2HPO4, and 1% SDS plus protease inhibitors and phosphatase inhibitors. Protein contents of the lysates were determined using the bicinchoninic acid method to ensure equal loading of membrane protein into gel lanes. Lysate samples and prestained molecular weight markers (Bio-Rad, Carlsbad, CA) were denatured in SDS reducing buffer containing DTT (Invitrogen NuPage, Carlsbad, CA), heated for 10 min at 70°C, and then loaded onto 12% Tris·HCl gels (PAGE Gold Precast, Lonza, Rockland, ME). Protein was separated by electrophoresis (Mini-Protean II, Bio-Rad, Hercules, CA), and resolved protein was transferred to polyvinylidene fluoride membranes using a Trans-Blot apparatus (Bio-Rad). The blots were rinsed three times in PBS-0.1% Tween, blocked with 7.5% BSA/PBS-0.1% Tween for 1 h at room temperature, and then incubated overnight at 4°C with primary antibodies to p38 (rabbit polyclonal), p-p38 (Thr180/Tyr182, rabbit polyclonal), SAPK/JNK (rabbit polyclonal), or p-SAPK/JNK (Thr183/Tyr185, rabbit polyclonal). All antibodies were purchased from Cell Signaling (Danvers, MA) and diluted 1:1,000 in 7.5% BSA/PBS-0.1% Tween. Blots were again rinsed three times with PBS-0.1% Tween and then incubated in 7.5% nonfat dry milk/PBS-0.1% Tween plus secondary antibody (horseradish peroxidase-conjugated goat anti-rabbit IgG; 1:1,000 dilution; Zymed Laboratories, San Francisco, CA) for 1 h at room temperature. Blots were rinsed three times with PBS-0.1% Tween, and protein was visualized using enhanced chemiluminescence (ECL, GE Healthcare, Buckinghamshire, UK) on a Fuji Film imaging machine (model LAS-4000, Medford, UK). MultiGauge software (Science Lab 2005, Fuji Film) was used to quantitate band density. Densitometry values for kinase abundances observed in hypoxia-, aglycemia-, OGD-, and AVP-treated cells were normalized to their respective normoxic controls, run as an internal standard on each gel. Lane positions for control and experimental lysates were randomized between experiments to avoid lane bias. For these Western blot assays, membranes were also stripped using 10 ml of stripping buffer (2% SDS and 65 mM Tris·HCl, pH 6.8) and 70 μl of β-mercaptoethanol (14.3 M; Sigma) and then reprobed for β-actin using mouse monoclonal antibody (1:5,000 dilution; Abcam, Cambridge, MA).
Na-K-Cl cotransporter activity assay.
Na-K-Cl cotransporter activity was assessed as ouabain-insensitive, bumetanide-sensitive K influx, with 86Rb used as a tracer for K, as described by us previously (49, 50, 60). These studies were conducted in a hypoxia chamber preset to 37°C with an atmosphere of 5% CO2 and 19%, 7%, or 2% O2 (normoxia, moderate hypoxia, or severe hypoxia, respectively), as described for Western blot experiments. CMEC monolayers on 96-well plates were pretreated for 30 min with the p38 inhibitor SB-239063 (20 μM), the JNK inhibitor SP-600125 (40 μM), or vehicle in HEPES-DMEM. Cells were then exposed to normoxia (19% O2) or hypoxia (7% or 2% O2) in HEPES-DMEM or to aglycemia (glucose- and pyruvate-free HEPES-DMEM), OGD (aglycemic HEPES-DMEM at 2% O2), or AVP (100 nM in normoxic HEPES-DMEM) for 5–120 min. SB-239063, SP-600125, or vehicle was also present throughout the treatment period. During the last 5 min of the treatment period, ouabain (100 μM), bumetanide (10 μM), or vehicle was added to the treatment medium. To initiate the assay for Na-K-Cl cotransporter activity, 86Rb (1 μCi/ml) was added to the treatment medium, and the cells were incubated for an additional 5 min. The assay was terminated by aspirating the media and rapidly rinsing wells three times with ice-cold 0.1 M MgCl2. Cell lysates were prepared using 1% SDS for 86Rb quantitation using a liquid scintillation counter (Tri-Carb 2500 TR) and protein determination by bicinchoninic acid assay (Pierce, Rockford, IL).
Immunofluorescence detection of BBB endothelial p38 and JNK MAPK in situ.
This study was conducted in accordance with the animal use and care guidelines issued by the National Institutes of Health, and the protocol was approved by the Animal Use and Care Committee at the University of California, Davis. Normotensive male Sprague-Dawley rats (250–300 g body wt; Charles River Laboratories, Wilmington, MA) were anesthetized by injection of pentobarbital sodium (1 mg/kg ip) and then immediately perfusion-fixed, as described by us previously (60). Briefly, for perfusion fixation, the abdomen of the anesthetized rat was opened, descending aorta and vena cava were clamped, and the chest cavity was opened; then a blunt 15-gauge needle was inserted through an incision in the right atrium, advanced into the ascending aorta, and clamped into place. Ice-cold saline (50 ml) was injected to flush out the blood, then 4% paraformaldehyde (400 ml) was injected (gravity fed, ∼3 ml/min). The brain was removed and further fixed in 4% paraformaldehyde overnight at 4°C and then in 10% paraformaldehyde for 7 days. Brains were embedded in paraffin, and 5-μm sections were mounted on slides. For immunohistochemistry experiments, slides were washed with xylene three times for 5 min, hydrated using an alcohol gradient (100%, 95%, 70%, and 50% ethanol for 5 min each), and then placed in PBS for 5 min. Slides were heated at 70°C in 10 mM Na citrate (pH 6.0, 25 min) for antigen recovery and then allowed to cool for 10 min before immersion in PBS for 5 min. Slides were blocked with 10% goat serum for 2 h at room temperature and then incubated overnight at 4°C with primary antibody (1:50 dilution) in 2% goat serum. The antibodies were as follows: p38 (rabbit polyclonal), p-p38 (Thr180/Tyr182, rabbit polyclonal), SAPK/JNK (rabbit polyclonal), and p-SAPK/JNK (Thr183/Tyr185, rabbit polyclonal). All kinase antibodies were obtained from Cell Signaling (Danvers, MA). We also used antibodies to detect glial fibrillary acidic protein (GFAP, guinea pig polyclonal), an astrocyte-specific marker, and SMI 71, a BBB endothelial cell-specific marker (mouse monoclonal). GFAP and SMI 71 (both used at 1:1,000 dilution) were purchased from Covance (Emeryville, CA). After incubation with primary antibodies, slides were washed in PBS three times for 5 min each and then incubated with secondary antibody (1:400 dilution in 2% goat serum; Alexa 488 anti-rabbit IgG and Alexa 546 anti-guinea pig IgG or Alexa 546 anti-mouse IgG; Molecular Probes, Eugene, OR). Slides were again washed in PBS three times for 5 min each and then dehydrated through an alcohol gradient (50%, 70%, 95%, and 100% ethanol for 5 min each). Finally, slides were washed in xylene three times for 5 min, excess xylene was removed with a KimWipe, and a coverslip was mounted using Permount (Fisher, Pittsburgh, PA). After 24 h, multichannel imaging was performed with a confocal microscope (model LSM 510, Zeiss) using a ×63 or ×40 oil objective. Lasers with excitation wavelengths of 488 and 543 nm were used for Alexa 488 and Alexa 546, respectively. Emission wavelengths were set at 505- to 530-nm band pass for Alexa 488 and at 560-nm long pass for Alexa 546.
Materials.
DMEM and l-glutamine were purchased from GIBCO-BRL (Grand Island, NY), gentamicin from AG Scientific (San Diego, CA), FBS and calf serum from Hyclone (Logan, UT), horse serum and fibronectin from Sigma (St. Louis, MO), bumetanide and ouabain from INC Biomedicals (Costa Mesa, CA), 86Rb from Perkin-Elmer (Welles, MA), and SB-239063 and SP-600125 from Calbiochem (San Diego, CA).
Statistics.
Values are means ± SE; all means represent at least five experiments. Statistical analyses were done using GraphPad Prism 4 software. For kinase protein abundance and Na-K-Cl cotransporter activity, analysis of differences among treatment groups was performed by one-way ANOVA or one-tailed paired t-test P < 0.05 was considered significant.
RESULTS
Ischemic factors activate p38 MAPK in CMEC.
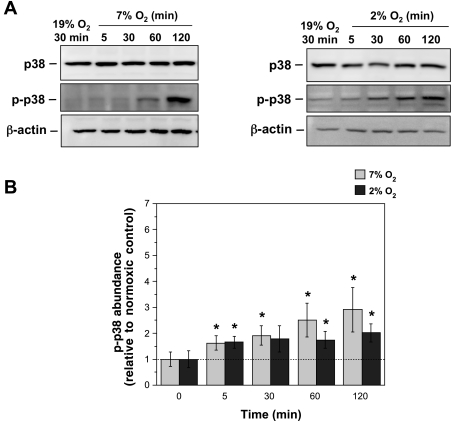
If p38 MAPK is involved in ischemic factor stimulation of BBB Na-K-Cl cotransporter activity and the rapid development of edema that occurs during the early hours of ischemic stroke, we predict that one or more ischemic factors will increase activity of the kinase in these cells with a time course similar to that observed for edema formation, i.e., within 30 min. To test this, we evaluated p38 activity in cultured bovine CMEC following exposure to hypoxia, aglycemia, AVP, or OGD over a time course of 5–120 min. Total p38 protein and p-p38 were assessed by Western blot analysis using antibodies that detect p38 (nonphosphorylated and phosphorylated) and antibodies that detect only p-p38. As shown inFig. 1A, Western blot analysis of lysates prepared from CMEC exposed to 7% O2 or 2% O2 (moderate or severe hypoxia, respectively) revealed prominent bands for p38 and p-p38 at ∼38 kDa. Densitometric analysis of multiple Western blots (Fig. 1B) showed statistically significant increases in p-p38 abundance following 5-, 30-, 60-, and 120-min exposures to 7% O2 (1.63-, 1.92-, 2.52-, and 2.91-fold, respectively) and 5-, 60-, and 120-min exposures to 2% O2 (1.66-, 1.75-, and 2.02-fold, respectively), indicating that p38 is rapidly activated in CMEC by moderate or severe hypoxia. Abundance of p-p38 following 30 min of exposure to 2% O2 also appeared to increase (1.79-fold), but the increase did not reach statistical significance (P = 0.08). Abundance of total p38 protein was not altered by 7% or 2% O2 at any of the exposure times.
Fig. 1.
Hypoxia-induced activation of p38. Cerebral microvascular endothelial cell (CMEC) monolayers were exposed to 19% O2 (normoxic control) or 7% or 2% O2 in HEPES-DMEM for 5, 30, 60, or 120 min. Cell lysates were prepared and subjected to Western blot analysis using antibodies that recognize only phosphorylated (activated) p38 (p-p38) or p-p38 and nonphosphorylated p38 (i.e., total p38 protein). A: representative Western blots. Bands shown for p38 and p-p38 are ∼38 kDa. B: abundance of p-p38. Values at 5–120 min are kinase abundances for 7% and 2% O2 exposures relative to internal normoxic control (0 min) for each experiment and are means ± SE of 8 and 7 separate experiments for 7% and 2% O2, respectively. *Significantly different from normoxic control, P < 0.05 by 1-tailed paired t-test.
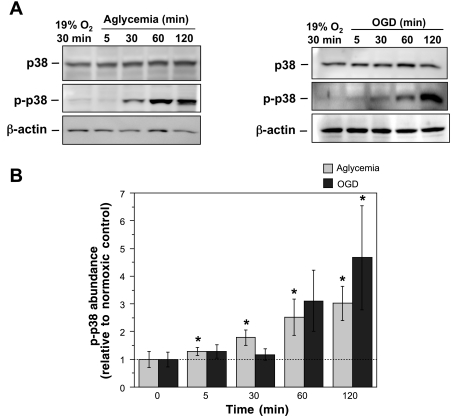
Figure 2 shows that exposure of CMEC to aglycemia or OGD also increased activation of p38. Abundance of p-p38 was significantly increased by 5, 30, 60, and 120 min of exposure to aglycemia (1.28-, 1.79-, 2.52-, and 3.02-fold, respectively), although only the 120-min value reached statistical significance (P = 0.058 for the 60-min value). Exposure of CMEC to OGD for 60 or 120 min also increased p-p38 abundance (3.11- or 4.57-fold, respectively). No significant increases in p-p38 were observed for OGD following 5- or 30-min exposures. As with the hypoxia experiments of Fig. 1, we found that abundance of total p38 protein did not change in response to aglycemia or OGD at any of the exposure times evaluated (data not shown). We further found that AVP (100 nM) also activated p38 in the CMEC (Fig. 3), with exposures of 5, 30, and 120 min significantly increasing p-p38 (1.7-, 1.52-, and 4.14-fold, respectively). The increase in p-p38 abundance following 60 min of AVP exposure (1.56-fold) did not reach statistical significance. Abundance of total p38 protein did not change following exposure to AVP at any of the times evaluated, indicating that, as with hypoxia, aglycemia, and OGD, changes in total p38 protein were not involved in these ischemic factor-induced increases in p-p38.
Fig. 2.
Aglycemia- and O2-glucose deprivation (OGD)-induced activation of p38. CMEC monolayers were exposed to control normoxic HEPES-DMEM, aglycemic normoxic medium (glucose- and pyruvate-free HEPES-DMEM at 19% O2), or hypoxic/aglycemic medium (glucose- and pyruvate-free HEPES-DMEM at 2% O2) for 5, 30, 60, or 120 min. Cell lysates were subjected to Western blot analysis using antibodies that recognize p38 (total kinase) or p-p38 (phosphorylated, active kinase). A: representative Western blots. B: p-p38 abundance. Values are means ± SE of 8 and 7 separate experiments for aglycemia and OGD, respectively. *Significantly different from control, P < 0.05 by 1-tailed paired t-test.
Fig. 3.
AVP-induced activation of p38. CMEC monolayers were exposed to control normoxic medium (glucose-containing HEPES-DMEM) or AVP (100 nM) in normoxic medium for 5, 30, 60, or 120 min. Cell lysates were subjected to Western blot analysis using antibodies that recognize p38 (total kinase) or p-p38 (phosphorylated, active kinase). A: representative Western blots. B: p-p38 abundance. Values are means ± SE of 7 separate experiments. *Significantly different from control, P < 0.05 by 1-tailed paired t-test.
Ischemic factors activate JNK MAPK in CMEC.
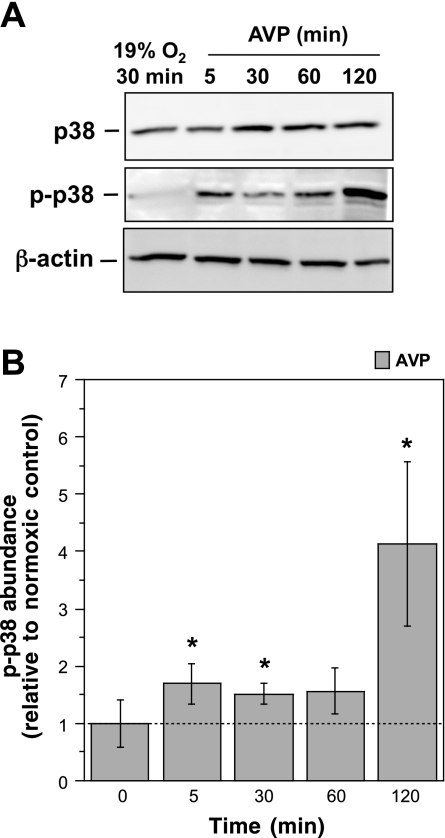
If JNK MAPK participates in ischemic factor-induced stimulation of BBB Na-K-Cl cotransporter activity and formation of edema during ischemic stroke, we predict that one or more ischemic factors will also cause a rapid increase in activity of this MAPK. To test this, we used Western blot methods with antibodies that specifically recognize total (phosphorylated and nonphosphorylated) JNK or p-JNK. As shown in Fig. 4A, Western blot lysates prepared from CMEC exposed to 7% or 2% O2 for 5–120 min revealed prominent bands for p-JNK and JNK at ∼46 and 54 kDa, the predicted molecular sizes for JNK α- and β-subunits, respectively (59). Densitometric analysis (Fig. 4B) showed statistically significant increases in p-JNK abundance following 5 min of exposure to 7% O2 (2.0-fold) and 5 or 30 min of exposure to 2% O2 (1.85- or 1.77-fold, respectively). Apparent increases observed following 30, 60, and 120 min of exposure to 7% O2 (2.21-, 1.57-, and 1.72-fold, respectively) or 60 and 120 min of exposure to 2% O2 (2.10- and 2.45-fold, respectively) did not reach statistical significance. Abundance of total JNK protein was not changed following exposure to 7% or 2% O2 at any of the times evaluated (data not shown).
Fig. 4.
Hypoxia-induced activation of JNK. CMEC monolayers were exposed to control normoxic HEPES-DMEM at 19% O2 or hypoxic medium at 7% O2 or 2% O2 for 5, 30, 60, or 120 min. Cell lysates were subjected to Western blot analysis using antibodies that recognize only phosphorylated (activated) JNK (p-JNK) or p-JNK and nonphosphorylated JNK (i.e., total JNK protein). A: representative Western blots. B: p-JNK abundance. Values are means ± SE of 6 and 5 separate experiments for 7% and 2% O2, respectively. *Significantly different from control, P < 0.05 by 1-tailed paired t-test.
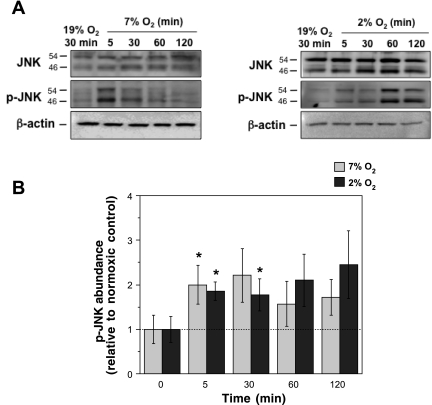
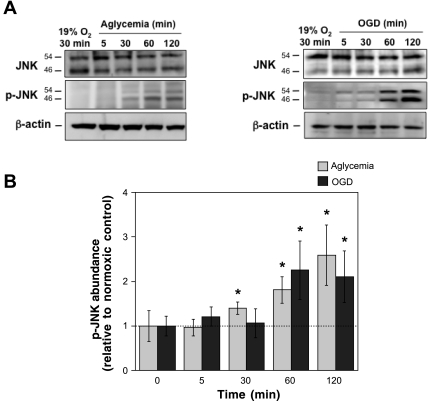
Figure 5 shows that exposure of CMEC to aglycemia or OGD also increased p-JNK abundance, although with a more delayed onset than observed for hypoxia. We found that p-JNK abundance was significantly increased by 30, 60, and 120 min of aglycemia (1.40-, 1.81-, and 2.59-fold, respectively) and 60 and 120 min of OGD (2.25- and 2.10-fold, respectively). As shown in Fig. 6, 30-, 60-, and 120-min exposures to AVP (100 nM) also caused significant increased in CMEC p-JNK abundance (1.49-, 1.67-, and 1.75-fold, respectively). As with hypoxia, we found that total JNK protein levels in the CMEC were not altered by aglycemia, OGD, or AVP at any of the exposure times (data not shown), indicating that ischemic factor-induced activation of JNK did not involve changes in total JNK protein.
Fig. 5.
Aglycemia- and OGD-induced activation of JNK. CMEC monolayers were exposed to control normoxic HEPES-DMEM, aglycemic normoxic medium (glucose- and pyruvate-free HEPES-DMEM at 19% O2), or hypoxic-aglycemic medium (glucose- and pyruvate-free HEPES-DMEM at 2% O2) for 5, 30, 60, or 120 min. Cell lysates were subjected to Western blot analysis using antibodies that recognize JNK (total kinase) or p-JNK (phosphorylated, active kinase). A: representative Western blots. B: p-JNK abundance. Values are means ± SE for 8 and 9 separate experiments for aglycemia and OGD, respectively. *Significantly different from control, P < 0.05 by 1-tailed paired t-test.
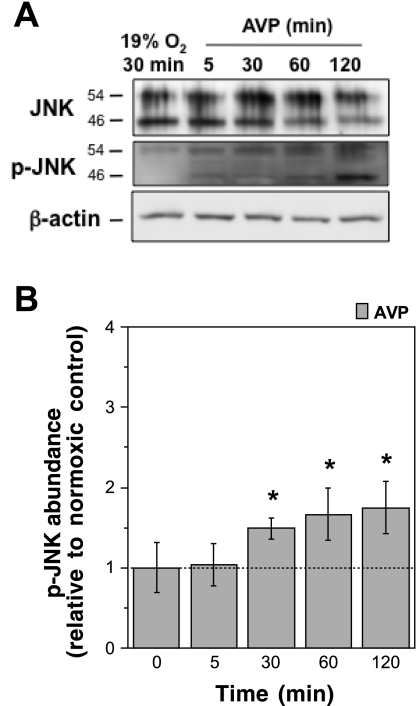
Fig. 6.
AVP-induced activation of JNK. Cells were exposed to control normoxic medium (glucose-containing HEPES-DMEM) or AVP (100 nM) in normoxic medium for 5, 30, 60, or 120 min. Cell lysates were subjected to Western blot analysis using antibodies that recognize JNK (total kinase) or p-JNK (phosphorylated, active kinase). A: representative Western blots. B: p-JNK abundance. Values are means ± SE for 6 separate experiments. *Significantly different from control, P < 0.05 by 1-tailed paired t-test.
Ischemic factor-induced stimulation of CMEC Na-K-Cl cotransporter activity is dependent on p38 MAPK activity.
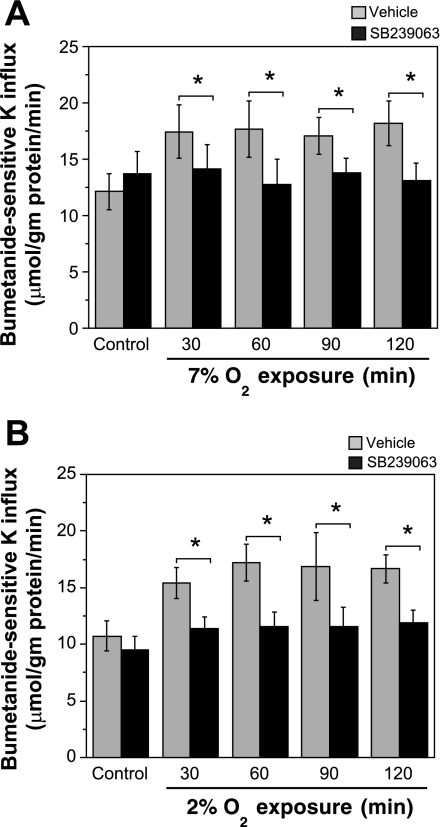
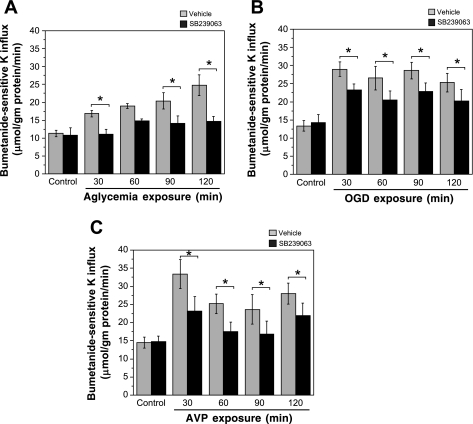
A role for p38 MAPK in stimulation of BBB Na-K-Cl cotransporter activity during ischemic stroke would predict that inhibiting activation of the kinase should reduce or abolish the elevated cotransporter activity observed in the presence of ischemic factors. In previous studies, we demonstrated that hypoxia, aglycemia, OGD, and AVP all stimulate CMEC Na-K-Cl cotransporter activity after exposures of 30–120 min (18, 60). Thus, in the present study, we evaluated Na-K-Cl cotransporter activity of CMEC following exposure to hypoxia, aglycemia, OGD, or AVP (30, 60, 90, and 120 min) in the presence or absence of SB-239063, the highly selective second-generation p38 inhibitor (1, 2). We found that hypoxia-induced stimulation of CMEC cotransporter activity, assessed as bumetanide-sensitive K influx, was abolished by 20 μM SB-239063 (Fig. 7). Whether the cells were exposed to moderate or severe hypoxia (7% or 2% O2, respectively), SB-239063 reduced cotransporter activity in the presence of hypoxia to levels not significantly different from normoxic control cotransporter activity. Similar results were found for CMEC exposed to aglycemia in the presence of SB-239063 (Fig. 8). The p38 inhibitor abolished the aglycemia-induced increase in CMEC cotransporter activity at all exposure times. In experiments evaluating the dose-response effect of SB-239063 (0–60 μM) for inhibition of CMEC cotransporter activity in the presence of 7% O2 or aglycemia, we found maximal inhibition at 20 μM for both ischemic factors (data not shown). Figure 8 also shows that, for cells exposed to OGD or AVP, SB-239063 significantly reduced, but did not abolish, the ischemic factor-induced increase in cotransporter activity at all exposure times. For all experiments shown in Figs. 7 and 8, SB-239063 did not reduce Na-K-Cl cotransporter activity under control, normoxic conditions, indicating that inhibition of p38 activity reduced or abolished ischemic factor stimulation of the cotransporter without altering basal cotransporter activity during normoxia.
Fig. 7.
SB-239063 inhibition of hypoxia-stimulated CMEC Na-K-Cl cotransporter activity. CMEC monolayers were pretreated for 30 min with SB-239063 (20 μM) or vehicle and then exposed for 30–120 min to normoxic control (19% O2) or hypoxia at 7% O2 (A) or 2% O2 (B) in glucose-containing HEPES-DMEM also containing SB-239063 (20 μM) or vehicle. CMEC Na-K-Cl cotransporter activity was assessed as ouabain-insensitive, bumetanide-sensitive K influx. Pretreatment conditions were maintained throughout the assay. Values are means ± SE for 8 separate experiments. *Significantly different (vehicle vs. SB-239063), P < 0.05 by repeated-measures ANOVA with Tukey's post hoc test. Vehicle values are significantly different from control at 30, 60, 90, and 120 min (A) and at 30, 60, 90, and 120 min (B), P < 0.05 by 1-tailed paired t-test. For A and B, SB-23063 values in the presence of hypoxia are not significantly different from SB-239063 values of the normoxic control, by repeated-measures ANOVA.
Fig. 8.
SB-239063 inhibition of aglycemia-, OGD-, and AVP-stimulated CMEC Na-K-Cl cotransporter activity. CMEC monolayers were pretreated for 30 min with SB-239063 (20 μM) or vehicle and then exposed for 30–120 min to normoxic control (19% O2 in HEPES-DMEM), aglycemia (A, glucose- and pyruvate-free HEPES-DMEM), OGD (B, aglycemia at 2% O2), or AVP (C, 100 nM, in normoxic HEPES-DMEM) and SB-239063 or vehicle. CMEC Na-K-Cl cotransporter activity was assessed as ouabain-insensitive, bumetanide-sensitive K influx. Pretreatment conditions were maintained throughout the assay. Values are means ± SE for 6, 8, and 9 separate experiments for aglycemia, OGD, and AVP, respectively. *Significantly different (vehicle vs. SB-239063), P < 0.05 by repeated-measures ANOVA with Tukey's post hoc test. Vehicle values for ischemic factors are significantly different from vehicle control at 30, 60, 90, and 120 min (A and B) and at 30, 60, and 120 min (C), P < 0.05 by 1-tailed paired t-test.
Ischemic factor-induced stimulation of CMEC Na-K-Cl cotransporter activity is dependent on JNK MAPK activity.
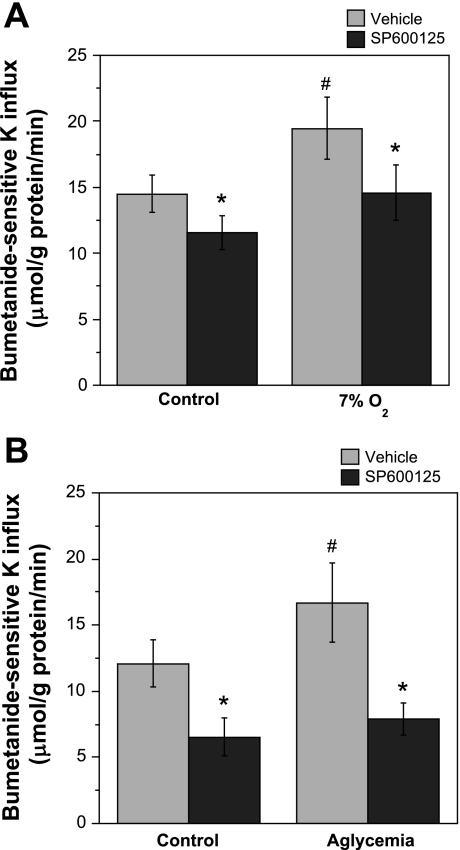
If JNK MAPK is involved in stimulation of BBB Na-K-Cl cotransporter activity during ischemia, then we should see not only that ischemic conditions activate JNK but also that inhibition of the kinase reduces or abolishes ischemic factor stimulation of the cotransporter. Thus we also evaluated the effects of the JNK inhibitor SP-600125 on CMEC Na-K-Cl cotransporter activity following exposure of the cells to hypoxia (7% O2) or aglycemia. As shown in Fig. 9, we found that SP-600126 (40 μM) abolished the increase in CMEC Na-K-Cl cotransporter activity with hypoxia or aglycemia (30 min exposure). We also found that SP-600125 inhibition of JNK significantly reduced Na-K-Cl cotransporter activity of CMEC exposed to control (normoxic, normoglycemic) conditions, suggesting that JNK participates in maintenance of CMEC cotransporter activity, even in the absence of ischemic conditions. In additional experiments evaluating the effects of SP-600125 (0–60 μM) on inhibition of CMEC Na-K-Cl cotransporter activity following exposure of the cells to normoxia or aglycemia, we found maximal inhibition at 40 μM under both conditions (data not shown).
Fig. 9.
SP-600125 inhibition of hypoxia- and aglycemia-stimulated CMEC Na-K-Cl cotransporter activity. CMEC monolayers were pretreated for 30 min with SP-600125 (40 μM) or vehicle and then exposed for 30 min to normoxic control (19% O2 in HEPES-DMEM), hypoxia (A, 7% O2 in HEPES-DMEM), or aglycemia (B, glucose- and pyruvate-free normoxic HEPES-DMEM) and SP-600125 (40 μM) or vehicle. CMEC Na-K-Cl cotransporter activity was assessed as ouabain-insensitive, bumetanide-sensitive K influx. Pretreatment conditions were maintained throughout the assay. Values are means ± SE for 6 and 5 separate experiments for 7% O2 and aglycemia, respectively. *Significantly different from vehicle, P < 0.05 by 1-tailed paired t-test. #Significantly different from normoxic control, P < 0.05 by 1-tailed paired t-test.
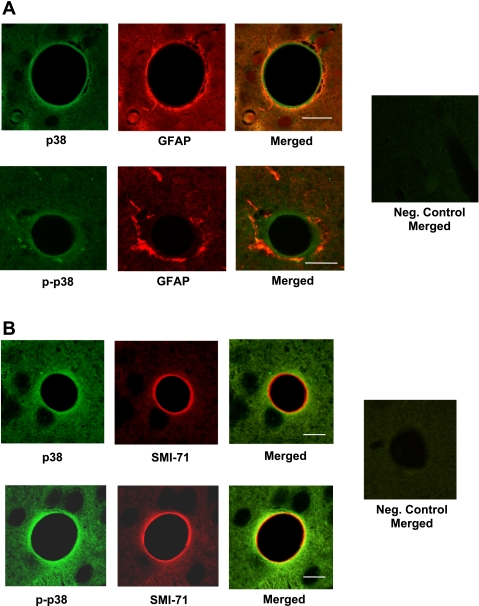
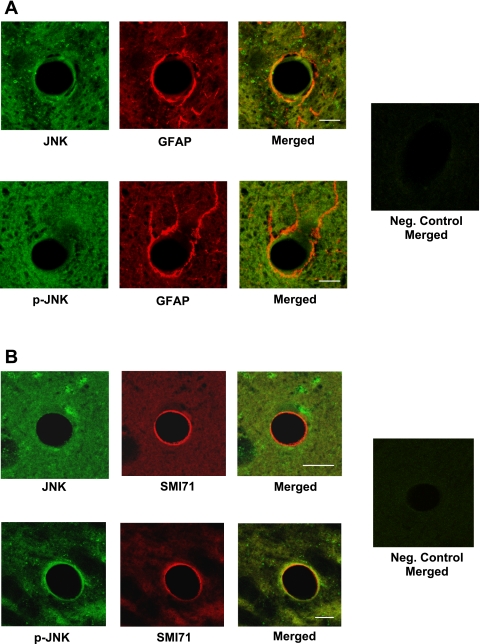
Detection of p38 and JNK MAPKs in BBB endothelial cells in situ.
To determine whether our findings regarding p38 and JNK involvement in ischemic factor stimulation of CMEC Na-K-Cl cotransporter activity are relevant to BBB endothelial cells in vivo, we conducted an initial investigation of p38 and JNK in cerebral microvessels of perfusion-fixed rat brain. We used confocal immunofluorescence microscopy and antibodies to detect total and phosphorylated p38 and JNK in the brain slices, along with antibodies to specifically identify BBB endothelial cells and perivascular astrocytic endfeet. Figure 10 shows representative confocal images of perfusion-fixed rat brain generated using antibodies specific for p38 and p-p38, together with antibodies that detect the astrocyte marker GFAP or the BBB endothelial cell-specific marker SMI 71. Figure 10A shows images obtained using antibodies for p38 or p-p38 and GFAP. p38 can be observed in the BBB endothelial cells. Merged p38 and GFAP images reveal that p38 is also present in perivascular astrocytes. p-p38 is also detected in the BBB endothelial cells and the perivascular astrocytes (Fig. 10A, bottom). Figure 10B shows images obtained with antibodies for p38 or p-p38 and SMI 71. Here again, p38 and p-p38 are observed in the endothelial cells, as well as in surrounding brain parenchymal cells. Negative control images (for Fig. 10, A and B), generated using only secondary antibodies reveal little to no fluorescence in the absence of primary antibodies. Figure 11 shows representative confocal images of perfusion-fixed rat brain generated using antibodies specific for JNK and p-JNK, along with antibodies for GFAP or SMI 71. In Fig. 11A, JNK and p-JNK can be observed in BBB endothelial cells, as well as perivascular astrocytes. In Fig. 11B, JNK and p-JNK are also observed in the BBB endothelial cells, as well as in surrounding brain parenchymal cells. Here again, in the negative control images (using secondary antibodies only), little to no fluorescence is observed. These initial investigations reveal that p38 and JNK are present in BBB endothelial cells in situ.
Fig. 10.
Immunofluorescence detection of p38 and p-p38 in blood-brain barrier (BBB) endothelial cell in situ. Perfusion-fixed normoxic rat brains were embedded in paraffin, sectioned (5 μm), and mounted on glass slides. Paraffin was removed, sections were lightly rehydrated, and immunohistochemistry was performed with antibodies for p38, p-p38, and the astrocyte marker glial fibrillary acidic protein (GFAP, A) or the BBB endothelial cell marker SMI 71 (B). Multichannel imaging of brain sections was performed with a Zeiss LSM 510 confocal microscope using a ×63 (A) or a ×40 (B) oil objective. p38 and p-p38 (green) are detected in BBB endothelial cells adjacent to the vessel lumen (black) and surrounding cells outside the endothelium. GFAP (red) can be seen in astrocytes surrounding the BBB endothelial cells (A), and SMI 71 (red) can be seen in BBB endothelial cells adjacent to the vessel lumen (B). Merged images show p38 and p-p38 in endothelial cells (green in A, orange-yellow in B), as well as in astrocytes (orange-yellow in A). For A and B, negative control images were generated using secondary antibodies only. Scale bars, 20 and 10 μm for top and bottom, respectively, in A and 10 μm for top and bottom in B.
Fig. 11.
Immunofluorescence detection of JNK and p-JNK in BBB endothelial cells in situ. Perfusion-fixed normoxic rat brains were embedded in paraffin, sectioned (5 μm), and mounted on glass slides. Paraffin was removed, sections were lightly rehydrated, and immunohistochemistry was performed with antibodies for JNK, p-JNK, and the astrocyte marker GFAP or the BBB endothelial cell marker SMI 71. Imaging was performed as described in Fig. 10 legend. JNK and p-JNK (green) are detected in BBB endothelial cells and perivascular astrocytes. GFAP (red) appears in the perivascular astrocytic endfeet surrounding the BBB endothelial cells, and SMI 71 (red) appears in BBB endothelial cells. Merged images show JNK and p-JNK in BBB endothelial cells (green in A, yellow in B), as well as in astrocytes (yellow in A). For A and B, negative control images were generated using secondary antibodies only. Scale bars, 10 μm.
DISCUSSION
Previous studies have shown that BBB Na-K-Cl cotransporter activity is stimulated by factors present during cerebral ischemia, including hypoxia, aglycemia, and AVP (8, 18, 33, 49), and we previously showed that bumetanide inhibition of BBB cotransporter activity reduces edema and infarct in the rat MCAO model of cerebral ischemia (11, 51). These findings suggest that the BBB Na-K-Cl cotransporter is a promising therapeutic target for reducing edema formation in ischemic stroke. The signaling pathways responsible for ischemic factor stimulation of the BBB Na-K-Cl cotransporter are not well understood; yet identification of these pathways could lead to therapies that would reduce or prevent ischemia stimulation of the cotransporter in patients at risk for stroke. Several kinases, including AMPK and the p38 and JNK MAPKs, are known to be activated in the brain by ischemia (17, 29, 30, 47, 56, 57, 61). In addition, pharmacological inhibition of these kinases decreases injury in stroke (2, 3, 38, 39, 55, 62). However, whether any or all of these kinases participates in ischemic factor stimulation of BBB Na-K-Cl cotransporter activity and ischemia-induced edema formation has not been known. We recently demonstrated that AMPK is rapidly activated in BBB endothelial cells by ischemic conditions and that inhibition of AMPK activity abolishes ischemic factor stimulation of the BBB Na-K-Cl cotransporter (60). In the present study, we demonstrate that p38 and JNK MAPKs are also rapidly activated by ischemic factors in BBB endothelial cells and that pharmacological inhibition of these kinases reduces or abolishes ischemic factor stimulation of the BBB Na-K-Cl cotransporter. We also provide evidence that p38 and JNK are present and active in BBB endothelial cells in situ. Together, these findings suggest that the signaling pathways by which ischemic factors stimulate BBB Na-K-Cl cotransporter activity involve activation of p38 and JNK MAPKs in addition to AMPK.
Our present studies reveal that p38 and JNK are activated in CMEC by hypoxia, aglycemia, AVP, and OGD. However, the time courses of activation vary depending on the kinase and ischemic factor. With respect to p38, moderate and severe hypoxia, as well as aglycemia and AVP, activate the kinase in CMEC within 5 min in a manner that is sustained through at least 120 min. JNK is also activated by hypoxia within 5 min, but the activation is not sustained beyond 30 min. In contrast, aglycemia and AVP activate JNK by 30 min, with activation sustained through 120 min. For p38 and JNK, severe hypoxia plus aglycemia (OGD) produces a delayed activation, occurring after 60 or more minutes. In none of these cases does the total amount of p38 or JNK change, indicating that activation of these kinases does not involve changes in the expression of the kinase proteins. It is noteworthy that the pattern for ischemic factor activation of p38 MAPK in the BBB endothelial cells is clearly one of rapid onset (by 5 min) for hypoxia, aglycemia, and AVP, with elevated activity throughout the 120-min experiment. The JNK MAPK pattern of activation, while more variable, is similar in trend to that of p38 MAPK, in that it is a sustained response. This is in contrast to our previous finding that ischemic factor activation of AMPK is also rapid (occurring by 5 min) but short-lived, falling back to control levels within 30 min (60). Determining whether and how ischemic factors affect the activation and/or expression levels of p38 and JNK following exposures beyond 120 min will require further investigation. In any case, our observed time courses of p38 and JNK activation in CMEC following exposure to hypoxia, aglycemia, or AVP are consistent with a role for the kinases in ischemia stimulation of the BBB Na-K-Cl cotransporter, given that when CMEC are exposed to these factors, elevated cotransporter activity is observed within 5–15 min and is sustained through 120 min or beyond (18, 49). Our findings are also consistent with previous studies from other laboratories that have demonstrated activation of p38 and JNK in rodent brain following induction of cerebral ischemia. In a study of rats subjected to permanent MCAO, p38 activation was observed at 1, 3, and 6 h following onset of ischemia (earlier times were not evaluated) (1). Permanent MCAO in mice increased activation of p38 and JNK after 10 min of ischemia, with activation sustained through 30 and 360 min for p38 and JNK, respectively (61). In studies of ischemia-reperfusion, p38 and JNK were increased in mouse brain as early as 5 min of reperfusion following ischemia (57) and by 5–15 min after transient forebrain ischemia in gerbils (16, 56). With respect to BBB endothelial cells, p38, but not JNK, activation was found to increase in human CMEC at 2–24 h following anoxia-reoxygenation (38), while in bEnd.3 cells (immortalized human CMEC), p38 and JNK activation was observed after 16–20 h of exposure to anoxia, but not after 8 h (the earliest time examined) (64).
The present study also demonstrates that SB-239063 inhibition of p38 abolishes the ability of hypoxia and aglycemia to stimulate CMEC Na-K-Cl cotransporter activity and markedly reduces stimulation by AVP and OGD, an effect sustained throughout the 120-min observation period. While SB-239063 effectively interferes with ischemic factor stimulation of Na-K-Cl cotransporter activity, we also found that it does not alter cotransporter activity under control, normoxic conditions. This suggests that administration of the p38 inhibitor prior to ischemic stroke may be a valuable approach to prevent ischemia stimulation of BBB cotransporter activity and edema formation without affecting cotransporter activity in the healthy, normoxic patient. We also show here that SP-600125 inhibition of JNK abolishes the ability of hypoxia and aglycemia to stimulate CMEC Na-K-Cl cotransporter activity. Unlike SB-239063, however, SP-600125 does reduce Na-K-Cl cotransporter activity under control, normoxic conditions. This suggests that JNK plays a role in maintaining baseline activity of the BBB cotransporter in healthy, nonischemic cells. These initial studies of SP-600125 were carried out following only 30 min of exposure to hypoxia or aglycemia. Additional studies are needed to address the effects of the inhibitor at prolonged exposure times. The observation that SP-600125 reduces cotransporter activity under control conditions suggests that it is less ideal for use as a preventative therapy in patients at risk for stroke, although additional studies are certainly needed to more fully evaluate the effects of the inhibitor for use in this capacity. In addition, future experiments are needed to evaluate the effects of SB-239063 and SP-600125 on ischemia-induced cerebral edema formation. The findings of our present experiments investigating kinase inhibitor effects of BBB Na-K-Cl cotransporter activity further support the hypothesis that p38 and JNK MAPKs are involved in ischemic factor stimulation of BBB cotransporter activity, thereby participating in edema formation during the early hours of ischemic stroke.
Our studies further demonstrate that p38 and JNK proteins are present in BBB endothelial cells in situ. Staining of perfusion-fixed rat brain slices with antibodies specific to these kinases along with antibodies to identify BBB endothelial cells and astrocytes revealed that p38 and JNK are present in BBB endothelial cells, as well as in astrocytes. In these experiments, we found p-p38 and p-JNK in control, nonischemic brain. This is consistent with our Western blot studies showing a low level of p-p38 and p-JNK, even in control, normoxic CMEC. In preliminary studies, we also found detectable p-p38 and p-JNK in brains of rats subjected to 30 min of MCAO. Additional studies are needed to evaluate BBB p-p38 MAPK and p-JNK abundances at different times following induction of ischemia to determine whether and over what time course these kinases are activated in the BBB endothelial cells in situ during cerebral ischemia. Previous studies investigating p38 and JNK in brain reported the presence of the kinases in the brain without concern as to the cell type or used markers to identify the kinases in neurons and/or astrocytes (1, 16, 56, 57, 61) without examining distribution in brain vasculature. In addition, previous studies examining these kinases in BBB endothelial cells were limited to in vitro cultured CMEC experiments. To our knowledge, the present study provides the first demonstration that p38 and JNK are indeed present and active in BBB endothelial cells in situ.
Determining the downstream events by which p38 and/or JNK MAPKs increase activity of the BBB Na-K-Cl cotransporter will require further investigation. Our previous studies showed increased phosphorylation of CMEC Na-K-Cl cotransporter (NKCC) protein following exposure of the cells to hypoxia or AVP (18). In those studies, we found significant increases in p-NKCC following 30, 90, and 180 min of exposure to 7% O2 and following a 10-min exposure to AVP (the only time evaluated for AVP). While our investigations support the hypothesis that ischemia activates p38 and JNK MAPKs, which in turn phosphorylate NKCC and increase cotransporter activity in BBB endothelial cells, our findings do not preclude the involvement of other kinases. Previous studies of Na-K-Cl cotransporter stimulation by reduced intracellular Cl concentration and cell shrinkage showed that STE20/SPS1-related proline/alanine-rich kinase (SPAK) and odd-skipped related 1 (OSR1) directly bind to, phosphorylate, and increase activity of NKCC1 (14, 31). SPAK and OSR1 are activated by upstream kinases that include the with no lysine (WNK) kinases WNK1, WNK3, and WNK4 (14, 20, 31, 32). Other upstream kinases, e.g., PKCδ and PKCθ, have been found to activate SPAK/OSR1 in airway epithelial cells (54) and lymphocytes (42). There is also evidence that WNK can cause trafficking of NKCC1 to the plasma membrane, thereby increasing activity of the cotransporter in a SPAK/OSR1-independent manner (19). Whether WNK and/or SPAK/OSR1 participate in p38 and JNK MAPK stimulation of BBB Na-K-Cl cotransporter activity remains to be determined in future studies. In the context of how p38 MAPK may link to stimulation of Na-K-Cl cotransporter activity, it is noteworthy that a previous study showed coimmunoprecipitation of p38 MAPK with the Na-K-Cl cotransporter in mouse brain lysates, suggesting an interaction of these two proteins (52).
In summary, the present study provides evidence that p38 and JNK MAPKs are activated during cerebral ischemia and contribute to ischemia-induced stimulation of BBB Na-K-Cl cotransporter activity. Together with our previous finding that intravenous bumetanide inhibition of BBB Na-K-Cl cotransporter activity reduces edema and infarct in the rat permanent MCAO model of stroke, this suggests that activation of p38 and JNK promotes edema formation during ischemic stroke. Our recent finding that compound C inhibition of AMPK activity greatly reduces ischemic factor stimulation of CMEC Na-K-Cl cotransporter activity, but that AMPK activation is relatively brief (5–30 min only) (60), suggests that other signaling pathways likely contribute to the increased Na-K-Cl cotransporter activity that is sustained through at least 120 min in the presence of ischemia. The present observation that p38 activation by all ischemic factors evaluated is sustained through at least 120 min, as is JNK activation by aglycemia, AVP, and OGD, suggests that these MAPKs may work in concert with AMPK to bring about sustained stimulation of the BBB cotransporter. Elucidating whether and how these signaling pathways interact to stimulate BBB events during cerebral ischemia will require further investigation. Additional studies are also needed to determine whether inhibitors of AMPK, and the p38 and JNK MAPKs, alone and in combination, effectively reduce edema formation in ischemic stroke. Future investigations will also need to clarify signaling components downstream from p38 and JNK MAPKs and the pathways that link the cotransporter with these kinases.
GRANTS
This work was supported by National Institute of Neurological Disorders and Stroke Grant NS-039953 (M. E. O'Donnell) and American Heart Association Western States Affiliate Predoctoral Fellowship 10PRE3330016, a Howard Hughes Integrating Medicine Into Basic Science Fellowship, and an Achievement Rewards for College Scientists Foundation award (B. K. Wallace). The investigation was conducted in part in a facility constructed with support from National Center for Research Resources Research Facilities Improvement Program Grant C06 RR-17348-01.
DISCLOSURES
No conflicts of interest, financial or otherwise, are declared by the authors.
AUTHOR CONTRIBUTIONS
B.K.W. and K.A.J. performed the experiments; B.K.W., K.A.J., and M.E.O. analyzed the data; B.K.W. and M.E.O. interpreted the results of the experiments; B.K.W., K.A.J., and M.E.O. prepared the figures; B.K.W. drafted the manuscript; B.K.W., K.A.J., and M.E.O. edited and revised the manuscript; M.E.O. was responsible for conception and design of the research; M.E.O. approved the final version of the manuscript.
REFERENCES
- 1.Barone FC, Irving EA, Ray AM, Lee JC, Kassis S, Kumar S, Badger AM, Legos JJ, Erhardt JA, Ohlstein EH, Hunter AJ, Harrison DC, Philpott K, Smith BR, Adams JL, Parsons AA. Inhibition of p38 mitogen-activated protein kinase provides neuroprotection in cerebral focal ischemia. Med Res Rev 21: 129–145, 2001 [DOI] [PubMed] [Google Scholar]
- 2.Barone FC, Irving EA, Ray AM, Lee JC, Kassis S, Kumar S, Badger AM, White RF, McVey MJ, Legos JJ, Erhardt JA, Nelson AH, Ohlstein EH, Hunter AJ, Ward K, Smith BR, Adams JL, Parsons AA. SB 239063, a second-generation p38 mitogen-activated protein kinase inhibitor, reduces brain injury and neurological deficits in cerebral focal ischemia. J Pharmacol Exp Ther 296: 312–321, 2001 [PubMed] [Google Scholar]
- 3.Bennett BL, Sasaki DT, Murray BW, O'Leary EC, Sakata ST, Xu W, Leisten JC, Motiwala A, Pierce S, Satoh Y, Bhagwat SS, Manning AM, Anderson DW. SP600125, an anthrapyrazolone inhibitor of Jun N-terminal kinase. Proc Natl Acad Sci USA 98: 13681–13686, 2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Betz AL. Alterations in cerebral endothelial cell function in ischemia. Adv Neurol 71: 301–313, 1996 [PubMed] [Google Scholar]
- 5.Bogoyevitch MA, Gillespie-Brown J, Ketterman AJ, Fuller SJ, Ben-Levy R, Ashworth A, Marshall CJ, Sugden PH. Stimulation of the stress-activated mitogen-activated protein kinase subfamilies in perfused heart—p38/RK mitogen-activated protein kinases and c-Jun N-terminal kinases are activated by ischemia/reperfusion. Circ Res 79: 162–173, 1996 [DOI] [PubMed] [Google Scholar]
- 6.Borsello T, Clarke PGH, Hirt L, Vercelli A, Repici M, Schorderet DF, Bogousslavsky J, Bonny C. A peptide inhibitor of c-Jun N-terminal kinase protects against excitotoxicity and cerebral ischemia. Nat Med 9: 1180–1186, 2003 [DOI] [PubMed] [Google Scholar]
- 7.Bourke RS, Kimelberg HK, Nelson LR, Barron KD, Auen EL, Popp AJ, Waldman JB. Biology of glial swelling in experimental brain edema. Adv Neurol 28: 99–109, 1980 [PubMed] [Google Scholar]
- 8.Brillault J, Lam TI, Rutkowsky JM, Foroutan S, O'Donnell ME. Hypoxia effects on cell volume and ion uptake of cerebral microvascular endothelial cells. Am J Physiol Cell Physiol 294: C88–C96, 2008 [DOI] [PubMed] [Google Scholar]
- 9.Bronner LL, Kanter DS, Manson JE. Primary prevention of stroke. N Engl J Med 333: 1392–1400, 1995 [DOI] [PubMed] [Google Scholar]
- 10.Carling D. The AMP-activated protein kinase cascade—a unifying system for energy control. Trends Biochem Sci 29: 18–24, 2004 [DOI] [PubMed] [Google Scholar]
- 11.Chen YJ, Anderson SE, O'Donnell ME. Bumetanide and HOE642 administered after initiation of middle cerebral artery occlusion effectively reduce rat brain Na uptake and infarct (Abstract). FASEB J 23: A614.613, 2009 [Google Scholar]
- 12.Chen YJ, Lam TI, Anderson SE, Walton JH, O'Donnell ME. Blood-brain barrier Na-K-Cl cotransporter and Na/H exchanger: therapeutic targets for ischemia-induced Na uptake and edema formation (Abstract). J Cereb Blood Flow Metab 29: S489, 2008 [Google Scholar]
- 13.Cowan KJ, Storey KB. Mitogen-activated protein kinases: new signaling pathways functioning in cellular responses to environmental stress. J Exp Biol 206: 1107–1115, 2003 [DOI] [PubMed] [Google Scholar]
- 14.Delpire E, Austin TM. Kinase regulation of Na+-K+-2Cl− cotransport in primary afferent neurons. J Physiol 588: 3365–3373, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ennis SR, Ren XD, Betz AL. Mechanisms of sodium transport at the blood-brain barrier studied with in situ perfusion of rat brain. J Neurochem 66: 756–763, 1996 [DOI] [PubMed] [Google Scholar]
- 16.Ferrer I, Ballabriga J, Pozas E. Transient forebrain ischemia in the adult gerbil is associated with a complex c-Jun response. Neuroreport 8: 2483–2487, 1997 [DOI] [PubMed] [Google Scholar]
- 17.Ferrer I, Friguls B, Dalfo E, Planas AM. Early modifications in the expression of mitogen-activated protein kinase (MAPK/ERK), stress-activated kinases SAPK/JNK and p38, and their phosphorylated substrates following focal cerebral ischemia. Acta Neuropathol (Berl) 105: 425–437, 2003 [DOI] [PubMed] [Google Scholar]
- 18.Foroutan S, Brillault J, Forbush B, O'Donnell ME. Moderate-to-severe ischemic conditions increase activity and phosphorylation of the cerebral microvascular endothelial cell Na+-K+-Cl− cotransporter. Am J Physiol Cell Physiol 289: C1492–C1501, 2005 [DOI] [PubMed] [Google Scholar]
- 19.Gamba G, Garbarini NJ, Delpire E. Regulation of cation-chloride cotransproters. In: Physiology and Pathology of Chloride Transporters and Channels in the Nervous System: From Molecular to Diseases, edited by Alvarez-Leefmans FJ, Delpire E. London: Academic, 2009, p. 357–381 [Google Scholar]
- 20.Giménez K. Molecular mechanism and regulation of furosemide-sensitive Na-K-Cl cotransporters. Curr Opin Nephrol Hypertens 15: 517–523, 2006 [DOI] [PubMed] [Google Scholar]
- 21.Gotoh O, Asano T, Koide T, Takakura K. Ischemic brain edema following occlusion of the middle cerebral artery in the rat. I. The time courses of the brain water, sodium and potassium contents and blood-brain barrier permeability to 125I-albumin. Stroke 16: 101–109, 1985 [DOI] [PubMed] [Google Scholar]
- 22.Guo Y, Signore AP, Yin W, Cao G, Yin XM, Sun F, Luo Y, Graham SH, Chen J. Neuroprotection against focal ischemic brain injury by inhibition of c-Jun N-terminal kinase and attenuation of the mitochondrial apoptosis-signaling pathway. J Cereb Blood Flow Metab 25: 694–712, 2005 [DOI] [PubMed] [Google Scholar]
- 23.Hardie DG. The AMP-activated protein kinase pathway—new players upstream and downstream. J Cell Sci 117: 5479–5487, 2004 [DOI] [PubMed] [Google Scholar]
- 24.Hardie DG. The AMP-activated protein kinase cascade: the key sensor of cellular energy status. Endocrinology 144: 5179–5183, 2003 [DOI] [PubMed] [Google Scholar]
- 25.Hatashita S, Hoff JT. Brain edema and cerebrovascular permeability during cerebral ischemia in rats. Stroke 21: 582–588, 1990 [DOI] [PubMed] [Google Scholar]
- 26.Herdegen T, Claret FX, K T, Martin-Villalba A, Winter C, Hunter T, Karin M. Lasting N-terminal phosphorylation of c-Jun and activation of c-Jun N-terminal kinases after neuronal injury. J Neurosci 18: 5124–5135, 1998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hu BR, Liu CL, Park DJ. Alteration of MAP kinase pathways after transient forebrain ischemia. J Cereb Blood Flow Metab 20: 1089–1095, 2000 [DOI] [PubMed] [Google Scholar]
- 28.Iadecola C. Mechanisms of cerebral ischemic damage. In: Cerebral Ischemia: Molecular and Cellular Pathophysiology, edited by Walz W. Totowa, NJ: Humana, 1999, p. 3–34 [Google Scholar]
- 29.Irving EA, Bamford M. Role of mitogen- and stress-activated kinases in ischemic injury. J Cereb Blood Flow Metab 22: 631–647, 2002 [DOI] [PubMed] [Google Scholar]
- 30.Irving EA, Barone FC, Reith AD, Hadingham SJ, Parsons AA. Differential activation of MAPK/ERK and p38/SAPK in neurones and glia following focal cerebral ischaemia in the rat. Brain Res Mol Brain Res 77: 65–75, 2000 [DOI] [PubMed] [Google Scholar]
- 31.Kahle KT, Rinehart J, Lifton RP. Phosphoregulation of the Na-K-2Cl and K-Cl cotransporters by the WNK kinases. Biochim Biophys Acta 1802: 1150–1158, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kahle KT, Rinehart J, Ring A, Gimenez I, Gamba G, Hebert SC, Lifton RP. WNK protein kinases modulate cellular Cl− flux by altering the phosphorylation state of the Na-K-Cl and K-Cl cotransporters. Physiology (Bethesda) 21: 326–335, 2006 [DOI] [PubMed] [Google Scholar]
- 33.Kawai N, McCarron RM, Spatz M. Effect of hypoxia on Na+-K+-Cl− cotransport in cultured brain capillary endothelial cells of the rat. J Neurochem 66: 2572–2579, 1996 [DOI] [PubMed] [Google Scholar]
- 34.Keep RF. Potassium transport at the blood-brain and blood-CSF barriers. In: Frontiers in Cerebral Vascular Biology: Transport and Its Regulation, edited by Drewes LR, Betz AL. New York: Plenum, 1993, p. 43–54 [DOI] [PubMed] [Google Scholar]
- 35.Kimelberg HK. Current concepts of brain edema. Rev Lab Invest J Neurosurg 83: 1051–1059, 1995 [DOI] [PubMed] [Google Scholar]
- 36.Kyriakis JM, Avruch J. Mammalian mitogen-activated protein kinase signal transduction pathways activated by stress and inflammation. Physiol Rev 81: 807–869, 2001 [DOI] [PubMed] [Google Scholar]
- 37.Lam TI, Wise PM, O'Donnell ME. Cerebral microvascular endothelial cell Na/H exchange: evidence for the presence of NHE1 and NHE2 isoforms and regulation by arginine vasopressin. Am J Physiol Cell Physiol 297: C278–C289, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lee SR, Lo EH. Interactions between p38 mitogen-activated protein kinase and caspase-3 in cerebral endothelial cell death after hypoxia-reoxygenation. Stroke 34: 2704–2709, 2003 [DOI] [PubMed] [Google Scholar]
- 39.Legos JL, McLaughlin B, Skaper SD, Strijbos PJLM, Parsons AA, Aizenman E, Herin GA, Barone FC, Erhardt JA. The selective p38 inhibitor SB-239063 protects primary neurons from mild to moderate excitotoxic injury. Eur J Pharmacol 447: 37–42, 2002 [DOI] [PubMed] [Google Scholar]
- 40.Li J, McCullough LD. Effects of AMP-activated protein kinase in cerebral ischemia. J Cereb Blood Flow Metab 30: 480–492, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Li J, Zeng Z, Viollet B, Ronnett GV, McCullough LD. Neuroprotective effects of adenosine monophosphate-activated protein kinase inhibition and gene deletion in stroke. Stroke 38: 2992–2999, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Li Y, Hu J, Vita R, Sun B, Tabata H, Altman A. SPAK kinase is a substrate and target of PKCθ in T-cell receptor-induced AP-1 activation pathway. EMBO J 23: 1112–1122, 2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.McCullough LD, Zeng Z, Li H, Landree LE, McFadden J, Ronnett GV. Pharmacological inhibition of AMP-activated protein kinase provides neuroprotection in stroke. J Biol Chem 280: 20493–204502, 2005 [DOI] [PubMed] [Google Scholar]
- 44.Menzies SA, Betz AL, Hoff JT. Contributions of ions and albumin to the formation and resolution of ischemic brain edema. J Neurosurg 78: 257–266, 1993 [DOI] [PubMed] [Google Scholar]
- 45.Menzies SA, Hoff JT, Betz AL. Extravasation of albumin in ischaemic brain oedema. Acta Neurochir (Wien) 51: 220–222, 1990 [DOI] [PubMed] [Google Scholar]
- 46.Neuwelt EA, Bauer B, Fahlke C, Fricker G, Iadecola C, Janigro D, Leybaert L, Molnár Z, O'Donnell ME, Povlishock JT, Saunders NR, Sharp F, Stanimirovic D, Watts RJ, Drewed LR. Engaging neuroscience to advance translational research in brain barrier biology. Nat Rev Neurosci 12: 169–182, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Nito C, Kamada H, Endo H, Niizuma K, Myer DJ, Chan PH. Role of the p38 mitogen-activated protein kinase/cytosolic phospholipase A2 signaling pathway in blood-brain barrier disruption after focal cerebral ischemia and reperfusion. J Cereb Blood Flow Metab 28: 1686–1696, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.O'Donnell ME. Ion and water transport across the blood-brain barrier. In: Physiology and Pathology of Chloride Transporters and Channels in the Nervous System, edited by Alvarez-Leefmans FJ, Delpire E. London: Academic, 2009, p. 585–606 [Google Scholar]
- 49.O'Donnell ME, Duong V, Suvatne J, Foroutan S, Johnson DM. Arginine vasopressin stimulation of cerebral microvascular endothelial cell Na-K-Cl cotransporter activity is V1 receptor and [Ca] dependent. Am J Physiol Cell Physiol 289: C283–C292, 2005 [DOI] [PubMed] [Google Scholar]
- 50.O'Donnell ME, Martinez A, Sun D. Cerebral microvascular endothelial cell Na-K-Cl cotransport: regulation by astrocyte-conditioned medium. Am J Physiol Cell Physiol 268: C747–C754, 1995 [DOI] [PubMed] [Google Scholar]
- 51.O'Donnell ME, Tran L, Lam TI, Liu XB, Anderson SE. Bumetanide inhibition of the blood-brain barrier Na-K-Cl cotransporter reduces edema formation in the rat middle cerebral artery occlusion model of stroke. J Cereb Blood Flow Metab 24: 1046–1056, 2004 [DOI] [PubMed] [Google Scholar]
- 52.Piechotta K, Garbarini N, England R, Delpire E. Characterization of the interaction of the stress kinase SPAK with the Na+-K+-2Cl− cotransporter in the nervous system. Evidence for a scaffolding role of the kinase. J Biol Chem 278: 52848–52856, 2003 [DOI] [PubMed] [Google Scholar]
- 53.Schielke GP, Moises HC, Betz AL. Blood to brain sodium transport and interstitial fluid potassium concentration during focal ischemia in the rat. J Cereb Blood Flow Metab 11: 466–471, 1991 [DOI] [PubMed] [Google Scholar]
- 54.Smith L, Smallwood N, Altman A, Liedtke CM. PKCδ acts upstream of SPAK in the activation of NKCC1 by hyperosmotic stress in human airway epithelial cells. J Biol Chem 283: 22147–22156, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Strassburger M, Braun H, Reymann KG. Anti-inflammatory treatment with the p38 mitogen-activated protein kinase inhibitor SB239063 is neuroprotective, decreases the number of activated microglia and facilitates neurogenesis in oxygen-glucose-deprived hippocampal slice cultures. Eur J Pharmacol 592: 55–61, 2008 [DOI] [PubMed] [Google Scholar]
- 56.Sugino T, Nozaki K, Takagi Y, Hattori I, Hashimoto N, Moriguchi T, Nishida E. Activation of mitogen-activated protein kinases after transient forebrain ischemia in gerbil hippocampus. J Neurosci 20: 4506–4514, 2000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Takagi Y, Nozaki K, Sugino T, Hattori I, Hashimoto N. Phosphorylation of c-Jun NH2-terminal kinase and p38 mitogen-activated protein kinase after transient forebrain ischemia in mice. Neurosci Lett 294: 117–120, 2000 [DOI] [PubMed] [Google Scholar]
- 58.Tian D, Litvak V, Lev S. Cerebral ischemia and seizures induce tyrosine phosphorylation of PYK2 in neurons and microglial cells. J Neurosci 20: 6478–6487, 2000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Waetzig V, Herdegen T. Context-specific inhibition of JNKx: overcoming the dilemma or protection and damage. Trends Pharmacol Sci 26: 454–461, 2005 [DOI] [PubMed] [Google Scholar]
- 60.Wallace BK, Foroutan S, O'Donnell ME. Ischemia-induced stimulation of Na-K-Cl cotransport in cerebral microvascular endothelial cells involves AMP kinase. Am J Physiol Cell Physiol 301: C316–C326, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wu DC, Ye W, Che XM, Yang GY. Activation of mitogen-activated protein kinases after permanent cerebral artery occlusion in mouse brain. J Cereb Blood Flow Metab 20: 1320–1330, 2000 [DOI] [PubMed] [Google Scholar]
- 62.Yatsushige H, Ostrowski RP, Tsubokawa T, Colohan A, Zhang JH. Role of c-Jun N-terminal kinase in early brain injury after subarachnoid hemorrhage. J Neurosci Res 85: 1436–1448, 2007 [DOI] [PubMed] [Google Scholar]
- 63.Zhu Y, Mao XO, Sun Y, Xia Z, Greenberg DA. p38 Mitogen-activated protein kinase mediates hypoxic regulation of Mdm2 and p53 in neurons. J Biol Chem 277: 22909–22914, 2002 [DOI] [PubMed] [Google Scholar]
- 64.Zhu Y, Sun Y, Xie L, Jin K, Sheibani N, Greenberg DA. Hypoxic induction of endoglin via mitogen-activated protein kinases in mouse brain microvascular endothelial cells. Stroke 34: 2483–2488, 2003 [DOI] [PubMed] [Google Scholar]