Summary
The venous sinuses commonly found in the margins of the diaphragm and sella are venous interconnections between the bilateral cavernous dural sinuses and are termed intercavernous communications or intercavernous sinuses. They form a venous ring, a single “circular sinus” that extends throughout the skull base. We report the first case to our knowledge of an intercavernous sinus fistula. We emphasize the importance of thorough knowledge of lesion characteristics before considering any interventional procedure.
An 84-year-old woman presented with alarming progressive orbital symptoms for one month affecting her left eye. A cerebral angiogram showed an intercavernous sinus fistula supplied by internal and external carotid arterial branches.
Transvenous embolization through retrograde catheterization of the right inferior petrosal sinus allowed complete coil occlusion of the lesion. Cerebral angiography confirmed the absence of residual blood flow through the fistula.
This report represents the first case of an intercavernous sinus dural arteriovenous fistula successfully treated with transvenous embolization. A detailed awareness of the regional anatomy is essential for treatment approach and favorable outcomes.
Key words: carotid-cavernous fistula, cavernous sinus syndrome, coil embolization, intercavernous sinus, transvenous embolization
Introduction
Cavernous sinus dural arteriovenous fistulas (DAVFs) are often grouped under the same “umbrella” on the basis of the traditional definition of the cavernous sinus as a venous pouch containing the internal carotid artery and cranial nerves. However, this traditional concept has been revised. The modern concept of the cavernous sinus is that of a venous plexus in the lateral intracranial epidural space in continuity with the spinal epidural venous plexus2. Therefore, it is no surprise that cavernous sinus DAVFs can have various morphologic characteristics and angioarchitecture based on the different portions of the cavernous sinus involved. We describe a patient presenting with symptoms typical of a cavernous sinus DAVF but with the DAVF actually located in the intercavernous sinus. This case exemplifies how knowledge and understanding of the exact location of the fistula are critical to proper endovascular treatment.
Case Report
An 84-year-old right-handed woman presented with a history of headache, double vision, pain, and fluid discharge affecting her left eye. Her symptoms had begun spontaneously 1 month before admission and gradually progressed. Physical examination showed left periorbital swelling, exophthalmos, and ptosis. Conjunctival injection and fluid discharge were also noted. She had a partial ophthalmoparesis with partial III and VI nerve palsies restricting lateral and medial gaze. Visual acuity was 20/50 bilaterally.
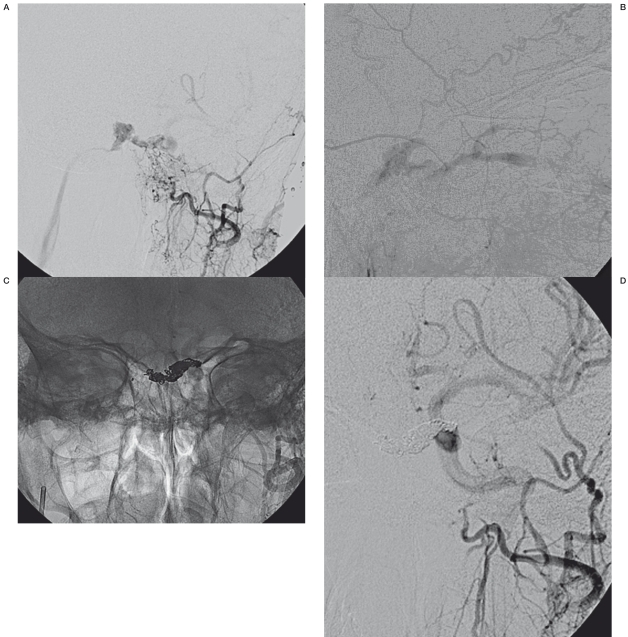
A head computed tomographic scan showed enlargement of the left superior ophthalmic vein and asymmetrical bulging of the lateral wall of the left cavernous sinus. Carotid angiography showed a DAVF of the intercavernous sinus fed by the meningohypophyseal branches of the right internal carotid artery and middle meningeal and distal internal maxillary branches of both external carotid arteries. The fistula drained into the left superior and inferior ophthalmic veins through the left cavernous sinus and into the right inferior petrosal sinus (IPS) through the right cavernous sinus (Figure 1A). The engorged superior and inferior ophthalmic veins from retrograde venous drainage were also identified (Figure 1B).
Figure 1.
Dural arteriovenous fistula of intercavernous sinus. A) Anteroposterior external carotid artery angiogram shows arterial supply from the distal internal maxillary artery and the middle meningeal artery to the intercavernous sinus, with drainage into both cavernous sinuses and the right inferior petrosal sinus. B) Retrograde flow into the superior and inferior ophthalmic veins. After embolization with coils (C), the shunting into the intercavernous sinus is eliminated (D).
A transvenous coil embolization was performed without difficulty, using an Echelon 10 (ev3 Inc, Irvine, California) microcatheter directed via the right IPS into the intercavernous sinus. Embolization with coils was then performed in the intercavernous sinus. The patient received heparin anticoagulation therapy during the procedure. After coil placement, angiography showed no residual flow and complete obliteration of the fistula (Figure 1C,1D). The patient recovered uneventfully and without complications.
Discussion
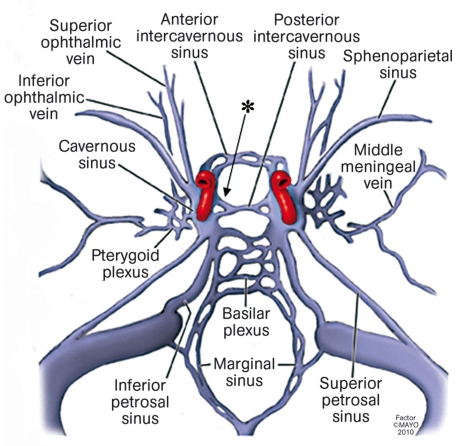
The clinical presentation of this patient did not differ from the presentation of classic, though not pathognomonic, cavernous sinus syndrome observed in patients with cavernous sinus DAVFs3. The symptoms could be explained by the fact that the abnormal hemodynamics created by the fistula altered the venous drainage pattern, resulting in the presenting symptoms. The cavernous sinuses and the intercavernous communications should be regarded as a confluence of venous blood at the center of the skull base, with multiple venous connections with the face, orbits, nasopharynx, middle ear, and mastoid. The intercavernous communications are located in the central area of the skull and are related to important vascular, nerve, and glandular structures4,5 (Figure 2). This anatomical relationship may explain the pathophysiologic features of our patient’s clinical presentation and highlights the importance of identifying the exact anatomical location of the lesion before any interventional procedure is considered.
Figure 2.
Artwork depicting the cavernous sinus and its connective network. The arrow depicts the fistula’s location in the present case.
Cerebral angiography is essential to evaluation of both cavernous and intercavernous DAVFs and is often performed in the same session as treatment. In our patient, the clinical presentation and other imaging studies had given the false impression of a carotid-cavernous sinus fistula. However, definite determination of the exact lesion location was made with cerebral angiography.
The goal of treatment for intercavernous and carotid-cavernous sinus fistulas is to interrupt the fistulous communications and decrease the hemodynamic burden in the cavernous sinus6,7. This goal can be accomplished either by occlusion of arterial feeders and proximal venous drainage through a transarterial approach6 or by retrograde transvenous occlusion of the sinus harboring the fistula8,9. Although transarterial embolization is a reasonable treatment option, selective distal access into numerous feeding vessels can be difficult. The transvenous approach is regarded to be the ideal treatment method for cavernous sinus DAVFs, with the ability to cure a fistula in a single session and with a high success rate.
Various transvenous approaches are available and the choice of the preferential route depends on the type of fistula’s drainage. Access to the cavernous sinus through the ipsilateral IPS is usually the shortest and most favorable route because of the direct connection of the IPS to the internal jugular vein through the petro-occipital fissure. Thrombosis of the IPS can be a major impediment to direct catheterization of the cavernous sinus. However, catheterization of the IPS is possible even when this sinus is not visible angiographically and even in the presence of thrombosis. Based on the complex pattern of drainage of indirect carotid-cavernous fistulas, alternative venous pathways for accessing the cavernous sinus include the contralateral IPS through the intercavernous sinus, the clival venous plexus, the cortical venous drainage, the pterygoid plexus, the inferior ophthalmic vein, and the superior ophthalmic vein through the angular or retromandibular veins. The selection of one of these alternate pathways depends on the individual characteristics of the fistula venous drainage and the anatomical position of the fistula itself in relation to the cavernous sinus. When these routes are not immediately available, percutaneous access though the superior ophthalmic vein with a surgical cutdown is a well-established alternative procedure. Direct percutaneous puncture of the cavernous sinus is also feasible and avoids the need for surgical cutdown. However, intrinsic to direct cavernous sinus punctures is the risk of intraorbital hematoma since no local pressure can be applied upon needle withdrawal.
The cavernous sinus is a plexus of veins with connections to various afferent and efferent veins. The carotid-cavernous fistulas involve different anatomical compartments of this space and have different drainage based on anatomical location and hemodynamic factors. In this respect, a detailed knowledge of the anatomy of this region is the mainstay to planning the most effective and targeted therapeutic approach to the lesion while preventing complications1. In the case presented, identification of the correct fistula point prevented unnecessary embolization and occlusion of the surrounding normal vasculature. Such unnecessary occlusion may have resulted in hemodynamic shifts and drainage overload of portion of the cavernous sinus only secondarily involved by the fistula such as the superior ophthalmic vein.
Although there occasionally are complications after transvenous embolization for dural carotid-cavernous fistulas9, our patient recovered without any adverse effect after treatment.
Conclusions
To our knowledge, this is the only case in the medical literature that describes a patient with an intercavernous sinus fistula.
As in all cases with dural arteriovenous malformations, we strongly consider thorough evaluation of the patient with cerebral angiography to be of utmost importance for exact localization of the lesion and treatment plan organization.
Treatment with transvenous coil embolization had excellent results in both imaging and neurologic outcome.
References
- 1.Agid R, Willinsky RA, Haw C, et al. Targeted compartmental embolization of cavernous sinus dural arteriovenous fistulae using transfemoral medial and lateral facial veins approaches. Neuroradiology. 2004;46(2):156–160. doi: 10.1007/s00234-003-1131-9. [DOI] [PubMed] [Google Scholar]
- 2.Parkinson D. Lateral sellar compartment O.T. (cavernous sinus): History, anatomy, terminology. Anat Rec. 1998;251:486–490. doi: 10.1002/(SICI)1097-0185(199808)251:4<486::AID-AR7>3.0.CO;2-Q. [DOI] [PubMed] [Google Scholar]
- 3.Stiebel-Kalish H, Setton A, Nimii Y, et al. Cavernous sinus dural arteriovenous malformations: Patterns of venous drainage are related to clinical signs and symptoms. Ophthalmology. 2002;109:1685–1691. doi: 10.1016/s0161-6420(02)01166-1. [DOI] [PubMed] [Google Scholar]
- 4.Aquini MG, Marrone AC, Schneider FL. Intercavernous venous communications in the human skull base. Skull Base Surg. 1994;4:145–150. doi: 10.1055/s-2008-1058966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kaplan HA, Browder J, Krieger AJ. Intercavernous connections of the cavernous sinuses. The superior and inferior circular sinuses. J Neurosurg. 1976;45:166–168. doi: 10.3171/jns.1976.45.2.0166. [DOI] [PubMed] [Google Scholar]
- 6.Gemmete JJ, Ansari SA, Gandhi DM. Endovascular techniques for treatment of carotid-cavernous fistula. J Neuroophthalmol. 2009;29:62–71. doi: 10.1097/WNO.0b013e3181989fc0. [DOI] [PubMed] [Google Scholar]
- 7.Miller NR. Diagnosis and management of dural carotid-cavernous sinus fistulas. Neurosurg Focus. 2007;23:E13. doi: 10.3171/FOC-07/11/E13. [DOI] [PubMed] [Google Scholar]
- 8.Cheng KM, Chan CM, Cheung YL. Transvenous embolisation of dural carotid-cavernous fistulas by multiple venous routes: A series of 27 cases. Acta Neurochir (Wien) 2003;145:17–29. doi: 10.1007/s00701-002-1013-7. [DOI] [PubMed] [Google Scholar]
- 9.Kim DJ, Kim DI, Suh SH, et al. Results of transvenous embolization of cavernous dural arteriovenous fistula: A single-center experience with emphasis on complications and management. Am J Neuroradiol. 2006;27:2078–2082. [PMC free article] [PubMed] [Google Scholar]