Summary
We describe the case of a 26-year-old man with orthostatic headache. Cerebral angiography revealed thrombosis in the sagittal sinus. Spine MRI showed cerebrospinal fluid collection at the C1-2 level. We performed blood patch and the symptoms disappeared. We report a rare case of intracranial hypotension caused by CSF leak and describe our hypothesis that SIH can change the velocity of cerebral blood flow and cause thrombosis.
Key words: intracranial hypotension, cerebrospinal fluid leakage, thrombosis
Introduction
Spontaneous intracranial hypotension (SIH) has become a well-understood disease during the last a couple of decades1-4. It is generally accepted that SIH is caused by CSF leakage from the dural sac and produce a persistent headache, especially an orthostatic headache. In many cases, subdural fluid collection is common and also combined with meningeal irritation5-8. However, little is known about the relationship between intracranial hypotension and cerebral blood flow. There have been few reports regarding thrombus formation in SIH, to our knowledge9-14. We experienced the case of a young adult with orthostatic headache who showed evidence of CSF leakage at the C1-2 level and thrombosis at the superior sagittal sinus. We suggest that CSF leakage brings about increased intracranial blood volume and causes the stasis of cerebral blood flow, especially at venous drainage, which leads to thrombosis. The aim of this case report is to ascertain the relationship between intracranial hypotension and thrombus formation.
Case Report
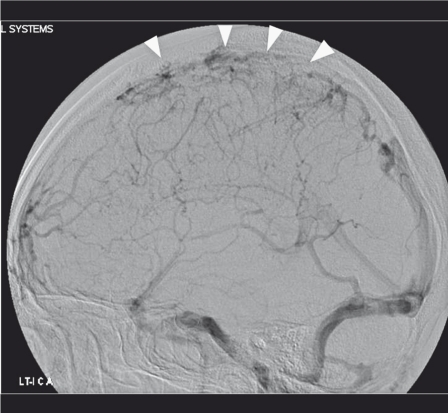
A 26-year-old man who had no remarkable medical or trauma history visited our department. He had neither underlying connective tissue disorders nor risk factors of cerebral venous thrombosis. He had an intractable headache for 1 month, and the headache aggravated when he was in the upright position and completely subsided when he lay flat. The patient underwent brain magnetic resonance (MR) imaging at local clinic, which showed no abnormal findings. He was admitted to a local clinic for three days. After that, his headache became worse and better repeatedly. Finally, his orthostatic headache became intolerable, and he was transferred to our department. He had no neurological deficits except for an orthostatic headache when he initially visited our department. However, brain computed tomography (CT) showed sparse areas of high density along the sylvian cistern on both sides. Thus, we performed diagnostic cerebral angiography to rule out spontaneous subarachnoid hemorrhage and obtained an unusual finding. We also performed a three bottle test of CSF through lumbar puncture. The opening pressure was 50 mmH2O and the color was clear and did not show hemorrhage in CSF which meant no evidence of subarachnoid hemorrhage. Thrombotic occlusion at the superior sagittal sinus and stasis of blood flow were found (Figure 1).
Figure 1.
Diagnostic cerebral angiography (left internal carotid artery lateral view) illustrates thrombus formation in the sagittal sinus (arrowheads).
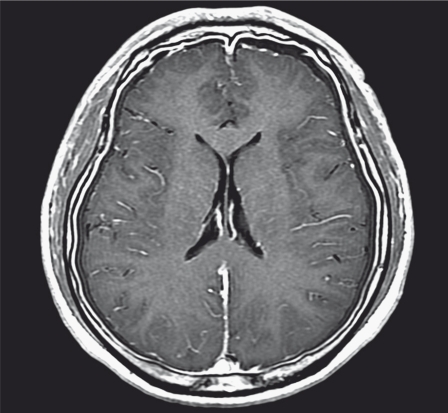
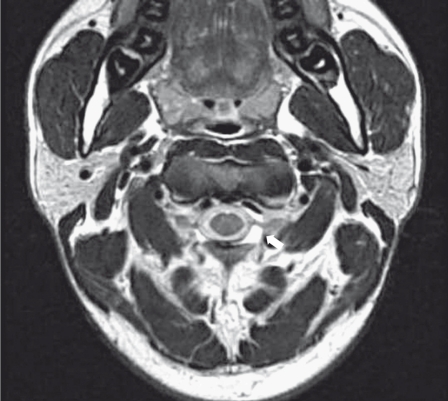
Following brain MR imaging performed again two days after cerebral angiography showed bilateral fluid collection at both frontotemporoparietal areas (Figure 2). A thin subdural hygroma was found unlike brain MR imaging that was performed at the local clinic three days before this presentation. A presumptive diagnosis of SIH was made, and spine MR imaging was performed to confirm spontaneous CSF leakage. Spine MR imaging showed CSF collection at the C1-2 level (Figure 3). The patient was definitively diagnosed with SIH due to CSF leakage. An epidural catheter was inserted at the C6-7 level, and blood patch (7 mL) was injected through the catheter. His symptoms were relieved promptly, and no complications occurred. He was discharged from the hospital seven days after the procedure. At the two-week follow-up, the patient had no further headache.
Figure 2.
Brain MR imaging shows bilateral subdural effusion and diffuse pachymeningeal enhancement, both of which are typical radiographic findings in patients with spontaneous intracranial hypotension.
Figure 3.
Spine MR imaging demonstrates cerebrospinal fluid accumulation at the C1-2 epidural space on the left side (arrow).
Discussion
In 1938, Renowden et al. first described CSF leakage, decrease of CSF production and increase of CSF absorption as the main causes of SIH1. SIH is extremely rare, and there have been only a few reports of SIH during the last a couple of decades. Cerebral venous thrombosis is also a rare disorder affecting only 0.0005% of the general population, and it occurs in about 2% of patients with SIH15. The diagnostic triads of SIH are an orthostatic headache, diffuse pachymeningeal gadolinium enhancement on brain MR imaging and a low CSF opening pressure (below 60 mm of water)16. Over 90% of patients have a CSF pressure of less than 60 mm of water (normal value, 65-195 mm of water)17. Headache in patients with SIH is diffuse or localized (frontal, temporal or occipital), usually bilateral18. It is aggravated gradually and reaches the peak within several hours of onset.
The mechanism of an orthostatic headache is downward displacement of the brain due to loss of CSF buoyancy causes traction on the pain sensitive structure, particularly the dura19. SIH exhibits various symptoms including an orthostatic headache, nausea, vomiting, nuchal pain, blurred vision, tinnitus, dizziness, nystagmus, ear fullness and photophobia21. In our patient, an orthostatic headache and a nuchal pain were prominent. Previous studies have shown that SIH has a preponderance of females with a male to female ratio between 1:1.75 and 1:4. The mean age of patients with SIH is reported to be between 38 and 42 years, regardless of gender. There is no difference in ethnicity22-25. Despite the term ‘spontaneous’, it is sometimes associated with mechanical stress, which plays an important role in the pathogenesis when the dural sac has a focal, weak point20,26. The site of CSF leakage is predominantly at the cervical or thoracic level. SIH is caused by single or multiple spinal CSF leakage, and generalized connective tissue disorder plays a crucial role in the development of spontaneous CSF leakage.
SIH is usually diagnosed by MR imaging27. Diffuse meningeal enhancement is a characteristic MR finding. Bilateral or unilateral subdural fluid collection is frequently associated with SIH. CT myelography is the most useful for determining the exact site of CSF leakage4,28. However, we did not perform CT myelography because fluid collection was definitely found at the C1-2 level on spine MR imaging. Spine MR imaging is a useful tool for detecting a leak site point indirectly.
Our patient had typical symptoms and brain MR imaging findings. Under a diagnosis of SIH, we performed diagnostic cerebral angiography, which showed thrombosis in the sagittal sinus. The reasons why blood flow stasis occurs have been proposed in the literature12,15. Farb et al.29,30 presented a study about venous distension in SIH patients group by using MR image. They analyzed a diameter of transverse sinus on MR image and showed a venous distension of transverse sinus. Based on the suggestions about cerebral venous thrombosis in patients with SIH, we present the following hypothesis. First, intracranial volume is constant by autoregulation. Second, according to the modified Monro-Kellie hypothesis (intracranial blood volume [CBV] + brain + CSF = constant)8,31,32, if CSF volume is decreased by leakage, it increases cerebral blood volume. Third, to maintain increased intracranial blood volume, the diameter of the venous structure, such as the sagittal or transverse sinus, increases12. Fourth, blood flow velocity is decreased in intracranial blood vessels, especially in the venous phase12,15. Finally, repetition of these events contributes to thrombus formation in the venous structure. According to the hydrodynamic theory (continuity equation S1V1=S2V2 where S is cross section and V is flow velocity) implying that flow velocity is inversely proportional to cross section, blood flow velocity in the sagittal sinus is slow compared to other vessels because the sagittal sinus has the biggest diameter among intracranial vessels33. Furthermore, CSF loss reduces the absorption of CSF into the sinus, and it increases blood viscosity15.
Surgical repair of the leak site is the standard treatment option; however, since it is not available in most cases, the procedure for sealing the hole of the leak site is the second choice of treatment3. It has been demonstrated that autologous epidural patching is the treatment of choice. Fibrin sealant injection is the next choice. Our patient underwent autologous blood patch (7 mL) once, and symptoms disappeared promptly. However, most patients require two or more epidural blood patches. Supportive care, such as hydration, bed rest and caffeine administration, provides only a temporary relief of symptoms18.
Conclusions
Although a few studies on SIH have been published during the last several decades, these studies have reported not on blood stasis but mainly on treatment in patients with SIH. In this study, diagnostic cerebral angiography showed thrombosis in the sagittal sinus. We put forward the hypothesis that CSF leakage results in increasing intracranial blood volume and causes the stasis of cerebral blood flow, which leads to venous thrombosis.
Acknowledgments
This work was supported by the Dankook University Research Fund of 2006.
References
- 1.Renowden SA, Gregory R, Hyman N, et al. Spontaneous intracranial hypotension. J Neurol Neurosurg Psychiatry. 1995;59:511–515. doi: 10.1136/jnnp.59.5.511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mokri B, Piepgras DG, Miller GM. Syndrome of orthostatic headaches and diffuse pachymeningeal gadolinium enhancement. Mayo Clin Proc. 1997;72:400–413. doi: 10.4065/72.5.400. [DOI] [PubMed] [Google Scholar]
- 3.Rai A, Rosen C, Carpenter J, et al. Epidural blood patch at C2, Diagnosis and treatment of spontaneous intracranial hypotension. Am J Neuroradiol. 2005;26:2663–2666. [PMC free article] [PubMed] [Google Scholar]
- 4.Schievink WI. Spontaneous spinal cerebrospinal fluid leaks and intracranial hypotension. J Am Med Asso. 2006;295(19):2286–2296. doi: 10.1001/jama.295.19.2286. [DOI] [PubMed] [Google Scholar]
- 5.Monro A. Observations on the Structure and Functions of the Nervous System. Edinburgh: Creech and Johnson; 1783. pp. 5–6. [Google Scholar]
- 6.Bruera OC, Bonamico L, Giglio JA, et al. Intracranial hypotension: the nonspecific nature of MRI findings. Headache. 2000;40:848–852. doi: 10.1046/j.1526-4610.2000.00154.x. [DOI] [PubMed] [Google Scholar]
- 7.Luijckx GJ, De Jaegere T. Magnetic resonance imaging findings before and after treatment of spontaneous intracranial hypotension. J Neurol Neurosurg Psychiatry. 2001;7:411. doi: 10.1136/jnnp.71.3.411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ferrante E, Wetzl R, Savino A, et al. Spontaneous cerebrospinal fluid leak syndrome: report of 18 cases. Neurol Sci. 2004;25(Suppl. 3):S293–295. doi: 10.1007/s10072-004-0315-3. [DOI] [PubMed] [Google Scholar]
- 9.Berroir S, Grabli D, Héran F, et al. Cerebral sinus venous thrombosis in two patients with spontaneous intracranial hypotension. Cerebrovasc Dis. 2004;17:9–12. doi: 10.1159/000073892. [DOI] [PubMed] [Google Scholar]
- 10.Flemming KD, Link MJ. Spontaneous CSF leak complicated by venous thrombosis and dural arteriovenous fistula. Cephalalgia. 2005;25:751–753. doi: 10.1111/j.1468-2982.2004.00942.x. [DOI] [PubMed] [Google Scholar]
- 11.Katoaka H, Tanizawa E, Ueno S, et al. Spontaneous intracranial hypotension is associated with a risk of venous sinus thrombosis and subdural hematoma. Cerebrovasc Dis. 2007;23:315–317. doi: 10.1159/000098446. [DOI] [PubMed] [Google Scholar]
- 12.Richard S, Kremer S, Lacour J-C, et al. Cerebral venous thrombosis caused by spontaneous intracranial hypotension: two cases. Eur J Neurol. 2007;14:1296–1298. doi: 10.1111/j.1468-1331.2007.01947.x. [DOI] [PubMed] [Google Scholar]
- 13.Savoiardo M, Armenise S, Spagnolo P, et al. Dural sinus thrombosis in spontaneous intracranial hypotension. J Neurol. 2006;253:1197–1202. doi: 10.1007/s00415-006-0194-z. [DOI] [PubMed] [Google Scholar]
- 14.Sopelana D, Marcos A, Arroyo R, et al. May intracranial hypotension be a cause of venous sinus thrombosis? Eur Neurol. 2004;51:113–115. doi: 10.1159/000076791. [DOI] [PubMed] [Google Scholar]
- 15.Schievink WI, Maya MM. Cerebral venous thrombosis in spontaneous intracranial hypotension. Headache. 2008;48(10):1511–1519. doi: 10.1111/j.1526-4610.2008.01251.x. [DOI] [PubMed] [Google Scholar]
- 16.Mokri B. Syndrome of cerebral spinal fluid hypovolemia: clinical and imaging features and outcome. Neurology. 2001;56:1607–1608. doi: 10.1212/wnl.56.11.1607-a. [DOI] [PubMed] [Google Scholar]
- 17.Chung SJ, Kim JS, Lee MC, et al. Syndrome of cerebral spinal fluid hypovolemia: clinical and imaging features and outcome. Neurology. 2000;55:1321–1327. doi: 10.1212/wnl.55.9.1321. [DOI] [PubMed] [Google Scholar]
- 18.Nokes SR, Dickins RD, Pierce WB, et al. Spontaneous intracranial hypotension. J Ark Med Soc. 1996;92:595–596. [PubMed] [Google Scholar]
- 19.Schievink WI, Maya MM, Loouy C, et al. Diagnostic criteria for spontaneous spinal CSF leaks and intracranial hypotension. Am J Neuroradiol. 2008;29:853–856. doi: 10.3174/ajnr.A0956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Paldino M, Mogilner AY, Tenner MS, et al. Intracranial hypotension syndrome: a comprehensive review. Neurosurg Focus. 2003;15:ECP2. [PubMed] [Google Scholar]
- 21.Park ES, Kim E. Spontaneous intracranial hypotension: clinical presentation, imaging features and treatment. J Korean Neurosug Soc. 2009;45:1–4. doi: 10.3340/jkns.2009.45.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Berroir S, Loisel B, Ducros A, et al. Early epidural blood patch in spontaneous intracranial hypotension. Neurology. 2004;63:1950–1951. doi: 10.1212/01.wnl.0000144339.34733.e9. [DOI] [PubMed] [Google Scholar]
- 23.Schievink WI, Meyer FB, Atkinson JL, et al. Spontaneous spinal cerebrospinal fluid leaks and intracranial hypotension. J Neurosurg. 1996;84:598–605. doi: 10.3171/jns.1996.84.4.0598. [DOI] [PubMed] [Google Scholar]
- 24.Schievink WI, Morreale VM, Atkinson JL, et al. Surgical treatment of spontaneous spinal cerebrospinal fluid leaks. J Neurosurg. 1998;88:243–246. doi: 10.3171/jns.1998.88.2.0243. [DOI] [PubMed] [Google Scholar]
- 25.Sencakova D, Mokri B, McClelland RL, et al. The efficacy of epidural blood patch in spontaneous CSF leaks. Neurology. 2001;57:1921–1923. doi: 10.1212/wnl.57.10.1921. [DOI] [PubMed] [Google Scholar]
- 26.Miyazawa K, Shiga Y, Hasegawa T, et al. CSF hypovolemia vs intracranial hypotension in ‘‘spontaneous intracranial hypotension syndrome’’. Neurology. 2003;60:941–947. doi: 10.1212/01.wnl.0000049933.51044.81. [DOI] [PubMed] [Google Scholar]
- 27.Mokri B. Spontaneous cerebrospinal fluid leaks: from intracranial hypotension to cerebrospinal fluid hypovolemia - evolution of a concept. Mayo Clin Proc. 1999;74:1113–1123. doi: 10.4065/74.11.1113. [DOI] [PubMed] [Google Scholar]
- 28.Rando TA, Fishman RA. Spontaneous intracranial hypotension: report of two cases and review of the literature. Neurology. 1992;42:481–487. doi: 10.1212/wnl.42.3.481. [DOI] [PubMed] [Google Scholar]
- 29.Farb RI, Forghani R, Lee SK, et al. The venous distension sign: a diagnostic sign of intracranial hypotension at MR of the brain. Am J Neuroradiol. 2007;28:1489–1493. doi: 10.3174/ajnr.A0621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Forghani R, Farb RI. Diagnosis and temporal evolution of signs of intracranial hypotension on MRI of the brain. Neuroradiology. 2008;50:1025–1034. doi: 10.1007/s00234-008-0445-z. [DOI] [PubMed] [Google Scholar]
- 31.Fishman RA, Dillon WP. Dural enhancement and cerebral displacement secondary to intracranial hypotension. Neurology. 1993;43:609–611. doi: 10.1212/wnl.43.3_part_1.609. [DOI] [PubMed] [Google Scholar]
- 32.Mokri B. The Monro-Kellie hypothesis: Applications in CSF volume depletion. Neurology. 2001;56:1746–1748. doi: 10.1212/wnl.56.12.1746. [DOI] [PubMed] [Google Scholar]
- 33.Clancy LJ. Aerodynamics. ed 1. London: Pitman Publishing Ltd; 1975. pp. 345–397. [Google Scholar]