Summary
We describe a rare neurointerventional complication, namely a stretched and sheared microcatheter, extending 52 cm from its point of retention within an Onyx cast in an infant patient’s neck mass, to the groin. The tumor was an unusual manifestation of infantile myofibromatosis and prior attempts at resection had proven impossible due to bleeding. Recommendations regarding microcatheter selection, diagnostic workup, and management of the ensuing complication are given.
Key words: infantile myofibromatosis, tumor embolization, onyx, complication, retained microcatheter
Introduction
Preoperative embolization can play a critical role in the treatment of vascular tumors. Simple endovascular proximal vessel ligation is not as effective as deep tumor penetration by the embolic agent in controlling intraoperative bleeding1. Particular technical challenges are posed when the patient is an infant, given limitations on contrast dose and vascular access. Although developed for the embolization of brain AVMs2,3, Onyx (ev3, Irvine, CA, USA) is increasingly used outside the central nervous system because of its attractive physical properties4,5, and its efficacy in dramatically reducing intraoperative blood loss when used for head and neck tumor embolization has been reported6,7. Catheter retention is a well-known potential complication of embolization with liquid embolic agents, associated in particular with n-butyl cyano-acrylate (NBCA)8. Catheter retention in adults is most often asymptomatic, and is typically managed by cutting the catheter at the groin site, allowing it to retract into the common femoral artery and eventually endothelialize along its entire length. However, the smaller caliber of pediatric arteries increases the likelihood that a retained catheter will be occlusive. As illustrated by this case, management of a retained catheter in an infant requires careful imaging workup and multidisciplinary management.
Case Report
The patient presented on day one of life with a cervicofacial skin stain, beneath which a mass rapidly grew. History, physical examination, and imaging (Figure 1) supported a diagnosis of a macrocystic lymphatic malformation. Sclerotherapy at three months was complicated by massive intralesional bleeding, demonstrating the highly vascular nature of the mass. Continued growth led to attempted resection without preceding preoperative embolization at seven months of age; the resection was partial due to copious blood loss, and the procedure had to be aborted. Pathology revealed the diagnosis to be infantile myofibromatosis. The tumor rapidly re-grew, prompting attempted complete excision preceded by preoperative embolization at age 14 months (the patient weighed 9.6 kg).
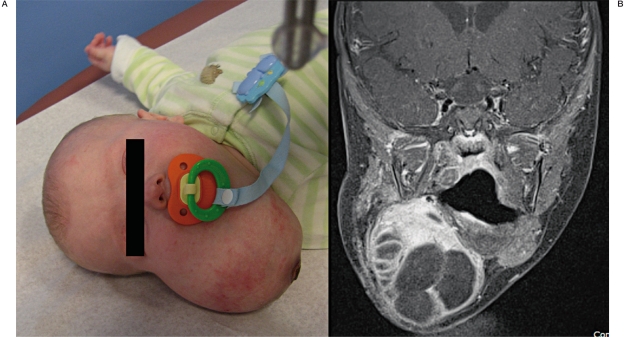
Figure 1.
A) Photograph of the patient at age 3 months, after attempted sclerotherapy. B) Coronal post contrast T1 WI with fat suppression demonstrated a partially cystic, well demarcated mass with avidly enhancing internal septations and solid components.
Preoperative tumor embolization is typically carried out using particulate embolics, such as a slurry of polyvinyl alcohol (PVA) in contrast. However, in an infant, the volume needed to effectively embolize a large, vascular tumor would quickly overtake the maximal weight-based dose limit (up to 7 cc/kg). The decision was therefore made to use Onyx as the embolic agent, given its ability to achieve effective devascularization without a large contrast dose6,7, and our extensive experience with Onyx in other pediatric settings9.
Under general anesthesia, a 5-French Envoy MPD catheter (Cordis, Miami, FL, USA) was used to catheterize the right external carotid artery. Arterial supply to the tumor was primarily via the superior thyroidal and facial arteries (Figure 2); no significant tortuosity of the feeding arteries was present. An Ultraflow microcatheter (Micro Therapeutics, Irvine, CA, USA) was used to superselectively catheterize the right superior thyroidal artery, through which embolization was carried out using Onyx, and the catheter was retrieved uneventfully.
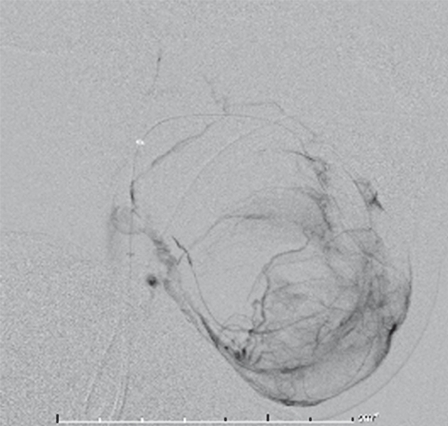
Figure 2.
Lateral right facial artery angiogram in the late-arterial phase, revealing the mass effect and vascularity of the myofibromatosis lesion.
A new Ultraflow microcatheter was then navigated into the right facial arterial supply to the tumor, and embolization with Onyx 18 undertaken. Onyx reflux along the microcatheter measured 8 mm, and once again, deep intratumoral penetration was seen (Figure 3). After embolization, retrieval of the microcatheter was attempted, but retrieval proved resistant. In order to treat potential vasospasm, ten micrograms of nitroglycerin were injected slowly by hand over two minutes via the guide catheter. Further incremental traction was applied to the microcatheter at the groin, ultimately resulting in retrieval of the catheter, after 23 minutes of intermittent retraction. Post-embolization angiography revealed effective devascularization of the tumor, with no evidence of perforation, extravasation, or non-target embolization. The procedure time was four hours and five minutes (induction to extubation), and the radiation dose was 182 mGy in the A plane and 124 mGy in the lateral plane. 2.2 cc of Onyx were injected for the embolization.
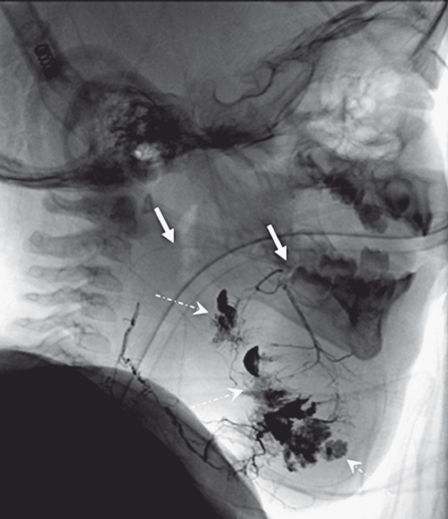
Figure 3.
Post-embolization unsubtracted image in the lateral view showing the Onyx cast. Closer inspection reveals a short segment of the fractured portion of the microcatheter embedded in the Onyx cast (solid arrows), following the course of the facial artery. Note intratumoral penetration of Onyx (dashed arrow).
When the retrieved catheter was examined, it was noted that the distal marker band was absent, and the length of the microcatheter was measured to be 158 cm (130 cm stiff segment and 28 cm floppy segment). Given the baseline 165 cm length of the Ultraflow microcatheter, we concluded that the distal-most 7 cm of the catheter had sheared off into the Onyx cast. Retrospective examination of unsubtracted images from the post-embolization angiogram revealed a short segment of sheared catheter (Figure 3). The presence of a small retained catheter tip within the feeding artery was thought to present no impediment to planned excision of the tumor, which necessarily would involve ligation of the arterial feeder.
The patient was transferred to the ICU for overnight monitoring in anticipation of resection. Several hours later, the ICU team noted that the patient’s right leg was cooler than the left, with femoral and popliteal pulses diminished. An intravenous heparin drip was administered. Sonography was suggestive of a linear foreign body within the right common femoral artery, and plain film radiographs demonstrated a short segment of catheter overlying the right groin; the proximal extent could not be ascertained (Figure 4). Noncontrast CT scan revealed that the sheared catheter remnant had stretched from its initial 7 cm length to extend from the Onyx cast within the right facial artery to the right common femoral artery, a distance of >50 cm (Figure 5). Overnight, the right leg pulses were intermittently identifiable with Doppler, and there were no clinical signs of limb ischemia.
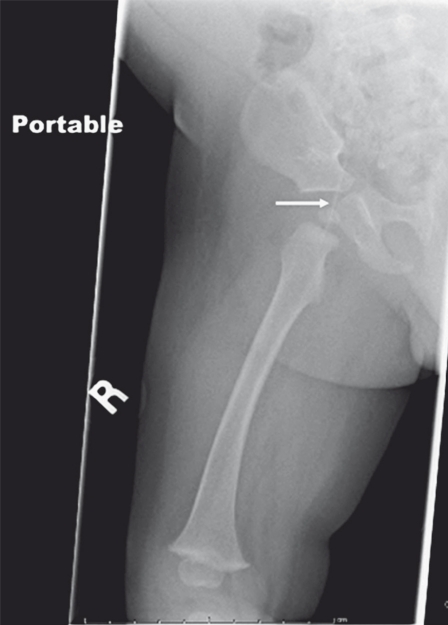
Figure 4.
Frontal radiograph reveals the distal end of the microcatheter overlying the course of the femoral and iliac arteries. The proximal end of the stretched microcatheter could not be delineated.
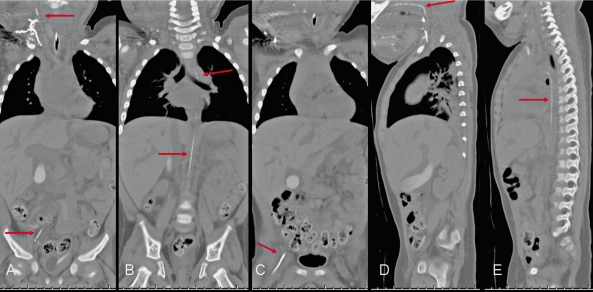
Figure 5.
Coronal (A-C) and sagittal (D,E) CT reformats demonstrating the course of the fractured and stretched microcatheter extending from the right femoral artery to the Onyx cast.
Given the potential need for ongoing anticoagulation to maintain patency of the right femoral artery, the decision was made to attempt removal of the catheter alone without resection of the tumor. Under C-arm fluoroscopy, the onyx cast would be located, then it and the attached microcatheter extracted from above. On intraoperative visual inspection of the cast, the attached microcatheter segment was seen to consist of an inner layer and an outer capsule, partially accordioned upon it. With gentle intermittent traction, it was possible to remove the entire length of the catheter via the cervical incision; the extracted catheter segment measured approximately 52 cm (Figure 6). Both the retrieved distal fragment and the proximal end of the microcatheter were sent to the manufacturer, ev3, for analysis.
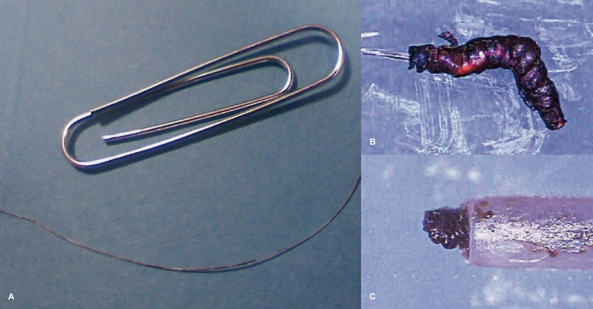
Figure 6.
Photograph of the extracted stretched microcatheter fragment adjacent to a paper clip (A). Magnification views obtained by the manufacturer demonstrate the Onyx cast with catheter extending proximally (B), as well as Onyx within the catheter (C).
Four days later, the patient underwent an uneventful excision of the cervical mass, with minimal blood loss. No intraoperative or postoperative complication was noted. The patient has been complication free since discharge, with a follow-up of 22 months.
Analysis by ev3 engineers revealed that the broken end appeared to be cleanly separated, but, given that the reflux measured along the catheter shaft did not exceed the manufacturer’s recommendation, the cause of the catheter entrapment could not be ascertained.
Discussion
There have been scattered case reports of microcatheter retention and fracture as an adverse outcome of transarterial embolization, but figures on incidence are not available 10-13. The vast majority of these reports concern n-BCA embolization. Femoral artery pseudoaneurysm or thrombosis following microcatheter retention have been reported13. However, in the majority of cases, retained catheters endothelialize and are managed with an initial period of anticoagulation, as the catheter surface is thought to undergo endothelialization. There is paucity of histological follow up in cases where microcatheter was retained early in life, and as such, any comment on long-term pathological consequences from the catheter material itself would be entirely speculative. Given the small arterial lumen of the pediatric population, retained catheter fragments should be investigated and then followed carefully, using either using ultrasound with Doppler or, as illustrated in our case, by CT.
In addition to fastidious attention to contrast and radiation dose in pediatric patients, the total dose of Onyx administered should be limited in order to minimize the potential for DMSO toxicity. When following the manufacturer’s dosing recommendations, we have encountered no DMSO-related toxicity, either systemic nor local, in our fairly large pediatric cohort. We have described these matters, in addition to the relationship between the use of Onyx and radiation dose in pediatric patients, in more detail elsewhere9.
Based on the current case and discussions with colleagues, we hypothesize that Ultraflow microcatheters, which are the only Onyx-compatible catheters designed to be used in truly flow-guided fashion, are prone to stretching and possibly shearing. Since this case, we have thus used this catheter without creating an Onyx plug, more similarly to the technique for nBCA embolization. The other Onyx compatible microcatheters, such as Marathon and Echelon, seem to be more resistant to stretching and shearing, and are better suited to the “plug and push” technique recommended by the manufacturer.
A recent case report describes retrieval of a microcatheter adherent in an Onyx cast using a snare and a “monorail” technique. Evidently, application of the vector of force by the snare at the site of catheter adherence is more efficacious than retracting on the proximal aspect of the catheter itself14. This technique may have been effective in our case as well.
The risk of catheter entrapment can be dramatically lowered through the use of a detachable tip microcatheter, such as the Sonic (Balt Extrusion, Montmorency, France). Unfortunately, this catheter is not approved for use in the US.
Conclusion
Onyx remains a valuable part of the armamentarium for embolizing vascular lesions. However, in cases of difficult catheter retrieval and a sheared catheter segment, microcatheter stretching may result in severe underestimation of the retained length. Unlike the case in adults, where retained microcatheters are largely asymptomatic, in infants, luminal compromise of large-caliber vessels is a likely possibility. The threshold for obtaining a CT scan to visualize the full extent of the retained segment should be low, to allow for informed treatment planning.
References
- 1.Bendszus M, Klein R, Burger R, et al. Efficacy of trisacryl gelatin microspheres versus polyvinyl alcohol particles in the preoperative embolization of meningiomas. Am J Neuroradiol. 2000;21(2):255–261. [PMC free article] [PubMed] [Google Scholar]
- 2.van Rooij WJ, Sluzewski M, Beute GN. Brain AVM embolization with Onyx. Am J Neuroradiol. 2007;28(1):172–177. discussion 177. [PMC free article] [PubMed] [Google Scholar]
- 3.Weber W, Kis B, Siekmann R, et al. Endovascular treatment of intracranial arteriovenous malformations with onyx: technical aspects. Am J Neuroradiol. 2007;28(2):371–377. [PMC free article] [PubMed] [Google Scholar]
- 4.Arat A, Cil BE, Vargel I, et al. Embolization of high-flow craniofacial vascular malformations with onyx. Am J Neuroradiol. 2007;28(7):1409–1414. doi: 10.3174/ajnr.A0547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rezende MT, Piotin M, Mounayer C, et al. Dural arteriovenous fistula of the lesser sphenoid wing region treated with Onyx: technical note. Neuroradiology. 2006;48(2):130–134. doi: 10.1007/s00234-005-0020-9. [DOI] [PubMed] [Google Scholar]
- 6.Gore P, Theodore N, Brasiliense L, et al. The utility of onyx for preoperative embolization of cranial and spinal tumors. Neurosurgery. 2008;62(6):1204–1211. doi: 10.1227/01.neu.0000333292.74986.ac. discussion 11-2. [DOI] [PubMed] [Google Scholar]
- 7.Elhammady MS, Wolfe SQ, Ashour R, et al. Safety and efficacy of vascular tumor embolization using Onyx: is angiographic devascularization sufficient? J Neurosurg. 2009;112(5):1039–1045. doi: 10.3171/2009.7.JNS09351. [DOI] [PubMed] [Google Scholar]
- 8.Bingol H, Sirin G, Akay HT, et al. Management of a retained catheter in an arteriovenous malformation. Case report. J Neurosurg. 2007;106(3):481–483. doi: 10.3171/jns.2007.106.3.481. [DOI] [PubMed] [Google Scholar]
- 9.Thiex R, Williams A, Smith E, et al. The use of Onyx for embolization of central nervous system arteriovenous lesions in pediatric patients. Am J Neuroradiol. 2009;31(1):112–120. doi: 10.3174/ajnr.A1786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Frizzel RT, Fisher WS., 3rd Cure, morbidity, and mortality associated with embolization of brain arteriovenous malformations: a review of 1246 patients in 32 series over a 35-year period. Neurosurgery. 1995;37(6):1031–1039. doi: 10.1227/00006123-199512000-00001. discussion 1039-1040. [DOI] [PubMed] [Google Scholar]
- 11.Pelz DM, Fox AJ, Vinuela F, et al. Preoperative embolization of brain AVMs with isobutyl-2 cyanoacrylate. Am J Neuroradiol. 1988;9(4):757–764. [PMC free article] [PubMed] [Google Scholar]
- 12.Whittle IR, Johnston IH, Besser M, et al. Experience with bucrylate (isobutyl-2-cyanoacrylate) embolization of cerebral arteriovenous malformations during surgery. Surg Neurol. 1983;19(5):442–449. doi: 10.1016/0090-3019(83)90143-x. [DOI] [PubMed] [Google Scholar]
- 13.Zoarski GH, Lilly MP, Sperling JS, et al. Surgically confirmed incorporation of a chronically retained neurointerventional microcatheter in the carotid artery. Am J Neuroradiol. 1999;20(1):177–178. [PubMed] [Google Scholar]
- 14.Kelly ME, Turner Rt, Gonugunta V, et al. Monorail snare technique for the retrieval of an adherent microcatheter from an onyx cast: technical case report. Neurosurgery. 2008;63(1) Suppl 1:ONSE89. doi: 10.1227/01.neu.0000335018.68369.e8. discussion ONSE. [DOI] [PubMed] [Google Scholar]