Abstract
Closures of trauma centers have accelerated since 2001. These closures may be disproportionately affecting disadvantaged communities. We evaluate how driving time between ZIP codes and nearest trauma centers changed nationwide from 2001–2007. During this period, 24% of the population experienced increased driving times to the nearest trauma center. Communities with disproportionately high numbers of African Americans, uninsured, people living in poverty and in rural areas were more likely to experience deteriorating access than other communities. Remaining trauma centers serving these communities should be allocated funding, and efforts to coordinate trauma care at the regional level should account for access disparities.
INTRODUCTION
Timely access to care is critically important for patients with traumatic injuries or emergent conditions. Although health outcomes depend on many factors (e.g., severity of injury), trauma patients who do not receive care in a timely fashion are at increased risk of death.(1–3)
Trauma centers are integral to emergency care because they reduce mortality.(4) While a significant proportion of the public mistakenly believes emergency departments are synonymous with trauma centers,(5) facilities that offer trauma center services are designated or certified by a government or independent entity to provide trauma care in defined areas.
The importance of trauma centers is recognized. Indeed, objective 8 of the Injury and Violence Prevention topic area of the U.S. government's Healthy People 2020 initiative is to increase access to trauma care in the U.S.(6)Unfortunately, trauma centers have been closing at accelerated rates over the past two decades, with 339 of the 1125 existing trauma centers closing from 1990–2005.(7–10) Closures are attributed to the high costs of trauma care, comparatively poorer patient populations, and underfunding.(11–14) Thus, public health experts and patients are concerned that the documented benefits of trauma centers(13, 15, 16) may not be equally available to all populations.
Previous research suggests that hospital closures might affect distance to care, which can lead to negative patient outcomes, especially for time-sensitive conditions.(1–3, 17) This may hold true for trauma center closures as well. Few studies have examined geographic access to trauma care for vulnerable populations measured by time to arrival or distance to care as an outcome variable.
Our study examines whether geographical access to care, defined here as driving time to the nearest trauma center, has improved or deteriorated between 2001 and 2007 for vulnerable population; specifically the socio-economically disadvantaged, racial and ethnic minorities, and rural communities. We consider driving time to nearest trauma center since the majority of field trauma cases are transported on roadways and inter-hospital transfers are beyond the scope of the study.
STUDY DATA AND METHODS
To establish the existence of trauma centers between 2001 and 2007, we extracted data from the American Hospital Association (AHA) Annual Surveys; including all general, acute, short-stay hospitals that offered trauma center services. The survey data also include trauma center characteristics such as size, ownership, and teaching status. We relied on the AHA surveys instead of the Trauma Information Exchange Program database, which identifies trauma centers based on the American College of Surgeons/ Committee on Trauma (ACS) definition, because data was not available for the entirety of our study period. The AHA survey asks hospitals to identify themselves as a: regional resource trauma center, community trauma center, rural trauma hospital, or other (state-specific).
For our analysis, a hospital is considered a trauma care center if it provides any type of trauma care specified in the AHA surveys (all levels included). We obtained the longitude and latitude coordinates of each trauma center's location using physical address or heliport location in order to calculate distance to the nearest trauma center.(18) We linked this dataset with the 2000 Census to obtain demographic characteristics of US communities as defined by ZIP code tabulation area level (created by the U.S. Census Bureau for statistical calculations of U.S. Postal Service ZIP codes, and in most cases identical to ZIP codes; henceforth referred to as “ZIP codes” in this paper) such as percent population under the Federal poverty line, unemployed, uninsured, of racial/ethnic minority groups, elderly, and/or foreign-born, and the longitude and latitude coordinates of each ZIP code. We further supplemented our dataset with county-level percentages of uninsured residents, data obtained from the 2005 Area Resource Files (ARF).(19)
Outcome measures
Distance to trauma care
Although geographic availability of a trauma center is only one component of healthcare access, it is important because of trauma's acute nature. In this study we look at geographic availability of trauma centers as a reasonable, but incomplete, proxy for access to trauma care(2). We measured distance between trauma center location and ZIP code's population center location by calculating the straight-line distance between the two locations. The distance calculation based on longitude and latitude coordinates is highly correlated with actual driving distance, especially for urban areas.(20, 21) To better understand how trauma center closures affected people between 2001–2007, we converted distance between ZIP code and nearest trauma center into driving time. We accomplished this by using a previously validated formula to convert straight-line distance into actual transportation time.(21, 22) We then determined how driving time to the closest trauma center changed between 2001–2007. We classified the communities according to whether the calculated driving time between each community and the nearest trauma center satisfied one of the following conditions between 2001 and 2007: 1. Did not increase (including a handful of communities that experienced a decreased driving time) 2. Increased by less than 30 minutes; or 3. Increased by more than 30 minutes. Because there is no standard measurement for changes in driving time, we looked at the overall mean for the communities with a positive increase in driving time, which was 29 minutes. We chose a 30-minute increase as the cutoff point for trauma access change categories because it represents a meaningful increase in driving time while ensuring adequate sample size.
Data Analysis
Our unit of analysis was at the community-level, defined by ZIP Codes established by the U.S. Census Bureau. First, we analyzed the change in driving time from 2001–2007 and compared area characteristics between communities that experienced no increase in driving time and those that experienced increased driving time to the nearest trauma centers. We performed a multinomial regression to determine which factors were associated with the community's risk of experiencing an increase in driving time to the nearest trauma center. The change-in-driving time outcome variable was categorical, and defined as: no change in driving time, increased by <30 minutes, and increased by ≥ 30 minutes. The multinomial logit is the appropriate estimation method because our dependent variable is categorical and not continuous. We describe the predicted variables in more detail below. All regression models were weighted by the population of each community in order to obtain population-based estimates of the relative risks. The communities included in the study are nationally representative of >99% of the US population, according to the 2000 Census. All analyses were done using Stata 11.(23)
Predictor Variables
Our main objective was to examine whether vulnerable populations experienced a disproportionate increase in driving times. We divided the communities into urban and rural categories based on whether the ZIP code was in a Metropolitan Statistical Area as defined by the 2000 Census. After differentiating rural and urban areas, we categorized each area according to whether the community had low, medium, or high shares of vulnerable characteristics.
We classified each community using the following steps: first, to characterize vulnerability we looked at the percentage of economically disadvantaged, racial/ethnic minorities, uninsured, foreign born, and the elderly (as detailed below).(19) Second, we categorized each community's level of vulnerable population into low, medium, and high by 3-quartiles of the distribution for each of these vulnerability characteristics in rural and urban areas across the United States. For instance, an urban ZIP code was classified as having a “high” share of elderly if the percentage of its elderly population was in the upper third (67–100%) of the distribution of elderly in all urban areas, and likewise for “medium” (34–66%) and “low” (0–33%) shares. By including the urban/rural indicator and the 3-level categorization of vulnerable population, we determined whether rural communities experienced access deterioration relative to urban communities, and if so, how vulnerable populations fared within them. We categorized vulnerable populations in each ZIP code as follows:
-
-
Economically disadvantaged. We included 2 measures of economically disadvantaged. We divided communities into 3 categories based on distribution of the percent of population below the Federal poverty line for urban and rural areas separately, and similarly for the unemployed. Both measures highlight weak economies that may be more vulnerable to changes in health care access.(24, 25)
-
-
Race/ethnicity. We considered racial and ethnic minorities using standard Census Bureau measures: non-Hispanic African American, Hispanic, and other non-Hispanic, non-black populations. These were compared with the reference group of non-Hispanic Whites.
-
-
Foreign-born. Foreign-born populations have more documented barriers to healthcare.(26) We include this characteristic because specific geographic disparities in access to care for this population have not been studied.
-
-
Uninsured. We categorize communities into low, medium, and high shares of uninsured based on the percent uninsured for the community. Note that percent uninsured is not available at the ZIP code level since the 2000 Census did not collect health insurance information. The smallest geographic unit with reliable uninsured percentage was at the county-level; therefore, ZIP codes that belong to the same county would share the same percent of uninsured.
-
-
Elderly. Elderly patients face higher risks of mortality during trauma; access to trauma is important for this population.(27) We identified elderly populations according to Census Bureau definition as individuals ≥ 65 years of age.
Other Covariates
In addition to population composition, we controlled the supply of hospital care by comparing changes in geographic access to trauma care while holding baseline access constant. We defined the hospital market as a 15-mile radius from the population center of the ZIP code. This fixed-radius market definition is a standard measure of hospital market.(28–31) We include the following indicators for the type of hospital care available within each community's hospital market in the baseline: the presence of at least one trauma center (for some rural communities, there is no trauma center within this radius if the nearest trauma center is more than 15 miles away), the presence of for-profit hospitals, government hospitals, and teaching hospitals.
STUDY RESULTS
Baseline distance to trauma centers in 2001
Our final sample consists of 31,475 ZIP codes covering 283 million people (about 99% of the US population). To illustrate the baseline distribution, Exhibit 1 shows the 2001 distance to the nearest trauma center in 3 discrete categories of geographic availability: those with trauma centers within 10 miles; between 10–30 miles; and >30 miles. Overall, nearly ¾ of the population resides within 10 miles of a trauma center while 14 percent of the population lives >30 miles away. The distribution is quite different between urban and rural communities: 71 percent of those in urban areas are within 10 miles of the nearest trauma center, and 9 percent are >30 miles away. In rural areas, only 24 percent have trauma centers within 10 miles while nearly a third (29 percent) do not have trauma centers within that radius.
Exhibit 1 (Figure).
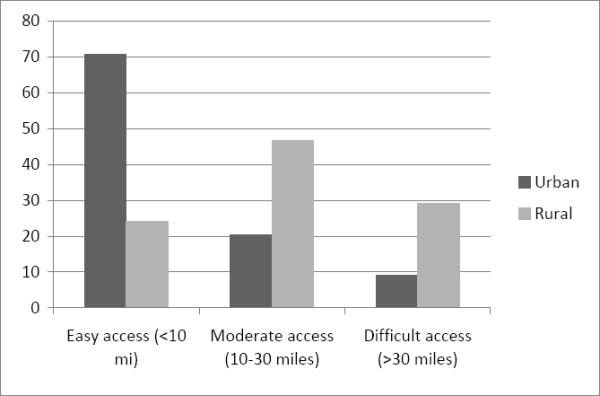
Population Access to Trauma Care Services in 2001
SOURCE: Authors analysis of the American Hospital Association (AHA). Annual Survey.(2001–2007);Washington DC and the U.S. Census Bureau. Census 2000 Summary File 3 Technical Documentation. 2002; Washington DC
Changes in driving time from 2001–2007
Exhibit 2 displays the location of trauma center closures across the United States from 2001–2007. Most closures occurred in urban areas because more trauma centers are located in these areas; yet rural areas have also been affected by closures.
Exhibit 2 (Figure).
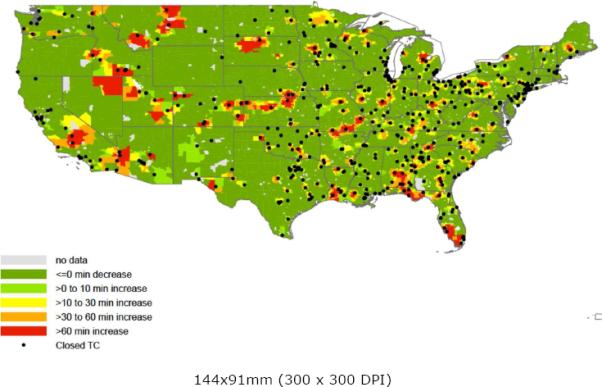
Trauma Center Closures Across the United States During 2001–2007
SOURCE: Authors′ analysis of the American Hospital Association (AHA). Annual Survey.(2001–2007);Washington DC
Exhibit 3 displays the means of the variables used in the statistical model, categorized by the 3 access change categories (no increase in driving time, <30 minute increase, and ≥30 minute increase). Approximately 76% of ZIP codes (214 million U.S. residents) experienced no increase in driving time to the nearest trauma center.
Exhibit 3.
Descriptive Statistics of Population and Health Care Market Characteristics By Trauma Services Access Change Categories
| Change in 2001–2007 |
||||
|---|---|---|---|---|
| Whole Sample | No increase in driving time | Increase driving time <30 min | Increase driving time >=30 min | |
| Baseline vulnerable population characteristics by ZIP code | ||||
| Share of population below Federal | ||||
| poverty line | ||||
| low share (reference group)* | 33% | 33% | 37% | 25% |
| medium share | 33% | 33% | 33% | 39% |
| high share | 33% | 34% | 30% | 36% |
| Share of unemployed population | ||||
| low share (reference group) | 33% | 33% | 36% | 30% |
| medium share | 33% | 33% | 35% | 38% |
| high share | 33% | 34% | 29% | 32% |
| Share of African-American population | ||||
| low share (reference group) | 33% | 34% | 29% | 32% |
| medium share (middle 1/3) | 33% | 33% | 35% | 30% |
| high share (upper 1/3) | 33% | 32% | 37% | 38% |
| Share of Hispanic population | ||||
| low share (reference group) | 34% | 33% | 33% | 39% |
| medium share | 33% | 33% | 35% | 34% |
| high share | 33% | 34% | 32% | 26% |
| Share of other non-White population | ||||
| low share (reference group) | 34% | 32% | 35% | 44% |
| medium share | 33% | 34% | 33% | 31% |
| high share | 33% | 34% | 31% | 25% |
| Share of uninsured population a | ||||
| low share (reference group) | 35% | 36% | 33% | 26% |
| medium share | 35% | 34% | 38% | 44% |
| high share | 30% | 30% | 29% | 30% |
| Share of elderly population | ||||
| low share (reference group) | 33% | 33% | 36% | 32% |
| medium share | 33% | 34% | 31% | 33% |
| high share | 33% | 33% | 33% | 34% |
| Share of foreign-born population | ||||
| low share (reference group) | 33% | 33% | 33% | 43% |
| medium share | 33% | 32% | 37% | 36% |
| high share | 33% | 35% | 31% | 20% |
| Urban communities (reference group) | 81% | 82% | 86% | 57% |
| Rural communities | 19% | 18% | 14% | 43% |
| Average population size | 28273 | 28404 | 29719 | 21646 |
| Baseline hospital market characteristics within 15–mile radius | ||||
| presence of at least 1 trauma center | 71% | 71% | 75% | 60% |
| presence of for-profit hospitals in the market | 52% | 52% | 55% | 37% |
| presence of government hospitals in the market | 47% | 48% | 49% | 31% |
| presence of teaching hospitals in the market | 47% | 49% | 53% | 6% |
|
| ||||
| Number of observations in the analysis | 31475 | 23914 | 5038 | 2523 |
| Population size | 282,779,035 | 213,860,611 | 53,090,278 | 15,828,146 |
Threshold for urban communities are: 6% and 13% for poverty; 2% and 3% for unemployment; 2% and 9% for African-American; 3% and 12% for Hispanic; 5% and 14% for other non-White; 5% and 7% for elderly; 4% and 13% for foreign-born; 12% and 16% for uninsured.
Threshold for rural communities are: 10% and 16% for poverty; 2% and 3% for unemployment; 0.3% and 4% for African-American; 1% and 3% for Hispanic; 2% and 5% for other non-White; 7% and 9% for elderly; 1% and 3% for foreign-born; 12% and 16% for uninsured.
Share of uninsured is only available at the county level. Therefore ZIP codes that belong to the same county share the same percent of uninsured.
Populations at risk for increased driving time to the nearest trauma center
We present the multivariate results in Exhibit 4. The overall model is statistically significant (p-value <0.01). The first column shows the unadjusted percent of the population that experienced ≥30 minutes increase in driving time, while the second column shows regression-adjusted relative risk ratios. We present the results pertaining to the comparison between the communities that experienced at least a 30-minute increase in driving time and communities that experienced no increase, as this comparison has the greatest policy implications (additional results are presented in the Appendix).
Exhibit 4.
Multinomial Logit Regression Results on the Likelihood that Driving Time to the Nearest Trauma Center Increases By At Least 30 Minutes Between 2001 and 2007
| Reference group: no increase in driving time | % experience ≥ 30min increase | Relative Risk Ratio | CI |
|---|---|---|---|
| Baseline vulnerable population characteristics by ZIP code | |||
| Share of population below Federal poverty line | |||
| low share (reference group) | 7% | 1.00 | |
| medium share | 8% | 1.24* | [1.00,1.54] |
| high share | 10% | 1.32* | [1.03,1.70] |
| Share of unemployed population | |||
| low share (reference group) | 7% | 1.00 | |
| medium share | 8% | 1.07 | [0.88,1.30] |
| high share | 9% | 0.98 | [0.79,1.22] |
| Share of African-American population | |||
| low share (reference group) | 8% | 1.00 | |
| medium share (middle 1/3) | 7% | 1.08 | [0.88,1.33] |
| high share (upper 1/3) | 8% | 1.28* | [1.04,1.59] |
| Share of Hispanic population | |||
| low share (reference group) | 9% | 1.00 | |
| medium share | 8% | 0.94 | [0.76,1.17] |
| high share | 7% | 1.04 | [0.76,1.44] |
| Share of other non-White population | |||
| low share (reference group) | 8% | 1.00 | |
| medium share | 8% | 0.71** | [0.57,0.89] |
| high share | 9% | 0.70* | [0.51,0.94] |
| Share of uninsured population a | |||
| low share (reference group) | 6% | 1.00 | |
| medium share | 9% | 1.69** | [1.37,2.08] |
| high share | 10% | 1.55** | [1.21,1.98] |
| Share of elderly population | |||
| low share (reference group) | 8% | 1.00 | |
| medium share | 7% | 0.90 | [0.74,1.11] |
| high share | 8% | 0.98 | [0.81,1.19] |
| Share of foreign-born population | |||
| low share (reference group) | 9% | 1.00 | |
| medium share | 8% | 0.98 | [0.79,1.22] |
| high share | 6% | 0.55** | [0.39,0.76] |
| Urban communities (reference group) | 5% | 1.00 | |
| Rural communities | 11% | 2.52** | [2.06,3.08] |
| log(zip-code level population) | 1.14** | [1.05,1.24] | |
| Baseline hospital market characteristics within 15-mile radius | |||
| presence of at least 1 trauma center | 1.65** | [1.38,1.97] | |
| presence of for-profit hospitals | 1.06 | [0.88,1.29] | |
| presence of government hospitals | 0.89 | [0.75,1.07] | |
| presence of teaching hospitals | 0.08** | [0.05,0.11] | |
|
| |||
| Number of observations in the analysis | 31475 | ||
statistical significance: + 0.10
0.05
0.01
ZIP codes that belong to the same county share the same percent of uninsured.
As shown in Exhibit 4, communities with a higher share of residents under the federal poverty line were at higher risk of facing at least a 30-minute increase in driving time in both urban and rural areas. High poverty communities were 1.32 times more likely (95% CI 1.03–1.70) to face an increase in driving time of ≥30 minutes compared with low poverty communities.
In addition, communities with high shares of African Americans are also at a higher relative risk (RR 1.28, 95% CI 1.04, 1.59) of experiencing a ≥30-minute increase in driving time to the nearest trauma center compared with areas with low proportions of African Americans. Communities with medium or high shares of uninsured residents are 1.69 (95% CI, 1.37–2.08) and 1.55 (95% CI, 1.21–1.98) times, more likely to experience ≥30 minute increase in driving time, respectively, when compared with communities with low share of uninsured population. We did not find other vulnerable populations to be at higher risk of increased driving time. Indeed, for areas with high proportions of foreign-born, the relative risk of a greater drive time actually decreased (RR 0.55, 95% CI 0.39–0.76).
We also found that rural communities, known to have higher baseline driving times to the nearest trauma center, have an even higher risk (RR 2.52, 95% CI 2.06–3.08) of experiencing a significant increase in driving time compared with urban areas.
LIMITATIONS
We recognize several limitations to our study. First, although the definitions of trauma centers have changed over time, those provided by the American College of Surgeons/Committee on Trauma (ACS) are considered the standard. However, there is no database of ACS-verified trauma centers that reaches back to 2001, so identification of trauma centers is based on self-report according to the definition in the AHA Annual Survey. Despite the slightly different definitions used by the AHA and ACS, we were able to calibrate our data for 1 year between AHA and the Trauma Information Exchange Program, which is based on ACS definitions. We found little difference between the numbers of level I–III trauma centers in our analysis. Using AHA data may have affected the rural data because self-report may not be as accurate as certified data from the Trauma Information Exchange program, especially for Level III and IV trauma centers which exist in greater numbers in rural areas.(13) The second limitation is that ZIP code level Census data are only available every 10 years. Although community characteristics may change within a decade, they should not affect our qualitative results, because these characteristics are highly correlated over the years. Third, while distances were correlated to travel time, 2 people from the same ZIP code might experience different driving time to the same trauma centers, especially in rural communities. For example, some rural communities may have established relationships with aeromedical transport to urban trauma centers; therefore, distance to the nearest trauma center might not be the most relevant proxy for access if patients receive timely airlift. We do know that aeromedical transport accounts for only 3% of all trauma transports and therefore should not invalidate our results.(32) Additionally, we did not account for EMS response and dispatch time, because we assumed that EMS activation time was constant throughout the study.
DISCUSSION
From 2001 to 2007, 69 million people in the US (24% of the population) had to travel farther to the nearest trauma center, with almost 16 million having to travel an additional 30 minutes or more. This deterioration in geographical access has been more acute in communities with high shares of poor, uninsured, and African American populations.
Our findings reveal that rural communities have a higher risk of experiencing declines in geographical access than urban communities. This is concerning because, at baseline, residents in these areas already must travel farther to reach their nearest trauma center. As our results and prior studies demonstrate, rural communities suffer from a lack of generalist and specialist physician presence.(33) These findings are in the context of an even worsening situation for patients needing emergency care in rural areas. In fact, 11.3% of rural hospitals closed from 1990–1999, while the number of emergency visits to rural hospitals rose over 20%.(34)
Despite the emphasis on decreasing disparities in the healthcare system, we show that geographical access to trauma centers, measured by driving times, has not improved. Indeed, geographic access to these services has deteriorated for vulnerable populations. Trauma centers provide expensive care to higher proportions of vulnerable populations and have lower cost recovery when compared with hospitals without trauma centers.(8, 35, 36) Because urban and suburban trauma centers are usually considered unprofitable, they often depend on public financing mechanisms to survive. There are no federal or state mandates for trauma centers or their locations.
In times of increasing economic hardship, it is possible that some trauma center closures might be due to coordination and consolidation of health care centers in order to improve efficiency and patient outcomes. We therefore cannot assume that closures are uniformly harmful to the community. Optimizing patient outcomes may therefore require better coordination of trauma services at the regional level.(37) The purpose of this analysis is to document how geographic access to trauma centers has changed over time, with the understanding that financial pressures and other documented market factors are predictors of trauma center survival.(10)
Trauma center closures are less often predicated on purposeful evaluation of health outcomes and desire to shut down poor-performers, and more often the result of financial hardships and an inability to offer a wide selection of services (7, 38) especially in communities that need it most. It is important to note that a decreased number of trauma centers does not imply poorer care for these populations, depending on the ability of the system to triage and transport (including aeromedical) patients to the most appropriate facilities.
Our findings provide evidence that poor and African American communities and rural dwellers are disproportionately affected by deteriorating trauma care access. Over the past 2 decades, disparities in health indicators such as mortality from traumatic injuries have worsened for vulnerable populations including black, Hispanic and low-income groups.(39) Deteriorating access to emergency care, such as trauma systems, could create systemic disparities of care for vulnerable patients.(40, 41)
We do not attempt to draw causal relationships but only to substantiate concerns about associations of increased trauma center closures in vulnerable communities and to alert policymakers about them. Potential policy implications could include bolstering financing mechanisms, such as reimbursement for injuries, specifically for hospitals that see a larger proportion of African American, uninsured, or poor populations. For rural areas, it is critical that agreements between existing trauma centers be created to potentially increase access to aeromedical transport.
It is important to build upon this research, which looks at the changes in geographic placement of trauma centers, to study how trauma center closures affect patient outcomes. The overall goal is to progress toward a healthcare system that provides equitable, competent, cost-effective acute care. While this does not equate to establishing a trauma center in every city, it does require careful examination of the effects of closures on individual communities -not simply as dictated by market forces or pressures. The goal of our research is to provide an empirical basis on which policymakers and healthcare providers can rely to establish regionalization schemes designed to provide efficient and equitable access to life-saving care.
Supplementary Material
Acknowledgements
We would like to thank Amy J. Markowitz, JD, for her editorial assistance; Tanja Srebotnjak, PhD, for her technical assistance; and Nicole Gordon, BA, for her administrative assistance.
Funding: RYH was funded by NIH/NCRR UCSF-CTSI Grant Number UL1 RR024131-01 and the Robert Wood Johnson Foundation Physician Faculty Scholars. YS was funded by the Robert Wood Johnson Foundation's Changes in Health Care Financing and Organization Initiative (grant #63974). The authors do not have any financial interests or conflicts in this data. The funders did not have any role in the design and conduct of the study; collection, management, analysis, or interpretation of the data; or preparation, review, or approval of the manuscript. This publication and its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
References
- 1.Clarke JR, Trooskin SZ, Doshi PJ, Greenwald L, Mode CJ. Time to laparotomy for intra-abdominal bleeding from trauma does affect survival for delays up to 90 minutes. The Journal of trauma. 2002 Mar;52(3):420–5. doi: 10.1097/00005373-200203000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Feero S, Hedges JR, Simmons E, Irwin L. Does out-of-hospital EMS time affect trauma survival? The American journal of emergency medicine. 1995 Mar;13(2):133–5. doi: 10.1016/0735-6757(95)90078-0. [DOI] [PubMed] [Google Scholar]
- 3.Fraser JF, Hartl R. Even in trauma, time is brain. Critical care medicine. 2008 Oct;36(10):2951–2. doi: 10.1097/CCM.0b013e31818724f2. [DOI] [PubMed] [Google Scholar]
- 4.Chiara O, Cimbanassi S. Organized trauma care: does volume matter and do trauma centers save lives? Curr Opin Crit Care. 2003 Dec;9(6):510–4. doi: 10.1097/00075198-200312000-00008. [Review] [DOI] [PubMed] [Google Scholar]
- 5.Champion HR, Mabee MS, Meredith JW. The state of US trauma systems: public perceptions versus reality--implications for US response to terrorism and mass casualty events. Journal of the American College of Surgeons. 2006 Dec;203(6):951–61. doi: 10.1016/j.jamcollsurg.2006.08.019. [DOI] [PubMed] [Google Scholar]
- 6.Healthy People 2020: Injury and Violence Prevention Objectives. United States Government: U.S. Department of Health and Human Services. 2011 [updated 6/30/2011; cited 2011 7/14]; Available from: http://healthypeople.gov/2020/topicsobjectives2020/objectiveslist.aspx?topicId=24.
- 7.Bazzoli GJ, Meersman PJ, Chan C. Factors that enhance continued trauma center participation in trauma systems. The Journal of trauma. 1996 Nov;41(5):876–85. doi: 10.1097/00005373-199611000-00021. [DOI] [PubMed] [Google Scholar]
- 8.Dailey JT, Teter H, Cowley RA. Trauma center closures: a national assessment. The Journal of trauma. 1992 Oct;33(4):539–46. discussion 46–7. [PubMed] [Google Scholar]
- 9.Eastman AB, Bishop GS, Walsh JC, Richardson JD, Rice CL. The economic status of trauma centers on the eve of health care reform. The Journal of trauma. 1994 Jun;36(6):835–44. discussion 44–6. [PubMed] [Google Scholar]
- 10.Shen Y-C, Hsia RY, Kuzma K. Understanding the Risk Factors of Trauma Center Closures: Do Financial Pressure and Community Characteristics Matter? Medical care. 2009;47(9):968–78. doi: 10.1097/MLR.0b013e31819c9415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bazzoli GJ, Kang R, Hasnain-Wynia R, Lindrooth RC. An update on safety-net hospitals: Coping with the late 1990's and early 2000's. Health Affairs. 2005 July/August;24(4):1047–56. doi: 10.1377/hlthaff.24.4.1047. 2005. [DOI] [PubMed] [Google Scholar]
- 12.Zuckerman S, Bazzoli G, Daviodoff A, LoSasso A. How did safety-net hospitals cope in the 1990's. Health Affairs. 2001 July/August;20(4):159–68. doi: 10.1377/hlthaff.20.4.159. 2001. [DOI] [PubMed] [Google Scholar]
- 13.Branas CC, MacKenzie EJ, Williams JC, Schwab CW, Teter HM, Flanigan MC, et al. Access to trauma centers in the United States. Jama. 2005 Jun 1;293(21):2626–33. doi: 10.1001/jama.293.21.2626. [DOI] [PubMed] [Google Scholar]
- 14.MacKenzie EJ, Hoyt DB, Sacra JC, Jurkovich GJ, Carlini AR, Teitelbaum SD, et al. National inventory of hospital trauma centers. Jama. 2003 Mar 26;289(12):1515–22. doi: 10.1001/jama.289.12.1515. [DOI] [PubMed] [Google Scholar]
- 15.MacKenzie EJ, Rivara FP, Jurkovich GJ, Nathens AB, Frey KP, Egleston BL, et al. A national evaluation of the effect of trauma-center care on mortality. The New England journal of medicine. 2006 Jan 26;354(4):366–78. doi: 10.1056/NEJMsa052049. [DOI] [PubMed] [Google Scholar]
- 16.Hulka F, Mullins RJ, Mann NC, Hedges JR, Rowland D, Worrall WH, et al. Influence of a statewide trauma system on pediatric hospitalization and outcome. The Journal of trauma. 1997 Mar;42(3):514–9. doi: 10.1097/00005373-199703000-00020. [DOI] [PubMed] [Google Scholar]
- 17.Buchmueller TC, Jacobson M, Wold C. How far to the hospital? The effect of hospital closures on access to care. J Health Econ. 2006 Jul;25(4):740–61. doi: 10.1016/j.jhealeco.2005.10.006. [DOI] [PubMed] [Google Scholar]
- 18.Horwitz JR, Nichols A. Hospital ownership and medical services: market mix, spillover effects, and nonprofit objectives. Journal of health economics. 2009 Sep;28(5):924–37. doi: 10.1016/j.jhealeco.2009.06.008. [Research Support, Non-U.S. Gov't] [DOI] [PubMed] [Google Scholar]
- 19.U.S. Census Bureau . Census 2000 Summary File 3 Technical Documentation. 2002. [Google Scholar]
- 20.Love RF, Morris JG. Mathematical models of road travel distances. Management Science. 1979;25:130–9. [Google Scholar]
- 21.Phibbs C, Luft H. Correlation of travel time on roads versus straight line distance. Med Care Res Rev. 1995;52(4):532–42. doi: 10.1177/107755879505200406. [DOI] [PubMed] [Google Scholar]
- 22.Lane P, Sorondo B, Baez A. Factors influencing the access of severely injured children and elderly patients involved in motor vehicle collisions to trauma center care. Annual proceedings / Association for the Advancement of Automotive Medicine. 2001;45:251–67. [PubMed] [Google Scholar]
- 23.StataCorp . Stata Statistical Software: Release 11. College Station, TX; StataCorp LP: 2009. [Google Scholar]
- 24.Brenner MH, Mooney A. Unemployment and Health in the Context of Economic Change. Social Science & Medicine. 1983;17(16):1125–39. doi: 10.1016/0277-9536(83)90005-9. [DOI] [PubMed] [Google Scholar]
- 25.O'Toole TP, Gibbon JL, Seltzer D, Hanusa BH, Fine MJ. Urban homelessness and poverty during economic prosperity and welfare reform: changes in self-reported comorbidities, insurance, and sources for usual care, 1995–1997. J Urban Health. 2002 Jun;79(2):200–10. doi: 10.1093/jurban/79.2.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lucas JW, Barr-Anderson DJ, Kington RS. Health status of non-Hispanic U.S.-born and foreign-born black and white persons: United States, 1992–95. Vital Health Stat 10. 2005 Jul;(226):1–20. [PubMed] [Google Scholar]
- 27.Champion HR, Copes WS, Buyer D, Flanagan ME, Bain L, Sacco WJ. Major trauma in geriatric patients. American journal of public health. 1989 Sep;79(9):1278–82. doi: 10.2105/ajph.79.9.1278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Garnick DW, Luft HS, Robinson JC, Tetreault J. Appropriate measures of hospital market areas. Health Serv Res. 1987 Apr;22(1):69–89. [PMC free article] [PubMed] [Google Scholar]
- 29.Robinson JC, Luft HS. Competition, regulation, and hospital costs, 1982 to 1986. Jama. 1988 Nov 11;260(18):2676–81. [PubMed] [Google Scholar]
- 30.Gresenz CR, Rogowski J, Escarce JJ. Updated variable-radius measures of hospital competition. Health Serv Res. 2004 Apr;39(2):417–30. doi: 10.1111/j.1475-6773.2004.00235.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chang DC, Shiozawa A, Nguyen LL, Chrouser KL, Perler BA, Freischlag JA, et al. Cost of inpatient care and its association with hospital competition. Journal of the American College of Surgeons. 2011 Jan;212(1):12–9. doi: 10.1016/j.jamcollsurg.2010.09.014. [DOI] [PubMed] [Google Scholar]
- 32.McGinnis KK, Judge T, Nemitz B, O'Connor R, Bass R, Bishop B, et al. Air Medical Services: future development as an integrated component of the Emergency Medical Services (EMS) System: a guidance document by the Air Medical Task Force of the National Association of State EMS Officials, National Association of EMS Physicians, Association of Air Medical Services. Prehosp Emerg Care. 2007 Oct–Dec;11(4):353–68. doi: 10.1080/10903120701536578. [DOI] [PubMed] [Google Scholar]
- 33.Rosenthal MB, Zaslavsky A, Newhouse JP. The geographic distribution of physicians revisited. Health Serv Res. 2005 Dec;40(6 Pt 1):1931–52. doi: 10.1111/j.1475-6773.2005.00440.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Emergency Departments - An Essential Access Point to Care2001 March Contract No.: 1. [Google Scholar]
- 35.Baker L. The effect of HMOs on fee-for-service health care expenditures: evidence from Medicare. Journal of Health Economics. 1997;16:453–81. doi: 10.1016/s0167-6296(96)00535-8. [DOI] [PubMed] [Google Scholar]
- 36.Eastman AB, Rice CL, Bishop G, Richardson JD. An analysis of the critical problem of trauma center reimbursement. The Journal of trauma. 1991 Jul;31(7):920–5. doi: 10.1097/00005373-199107000-00007. discussion 5–6. [DOI] [PubMed] [Google Scholar]
- 37.Trunkey DD. Regionalization of trauma care. Top Emerg Med. 1981 Jul;3(2):91–6. [PubMed] [Google Scholar]
- 38.Lindrooth RC, Lo Sasso AT, Bazzoli GJ. The effect of urban hospital closure on markets. J Health Econ. 2003 Sep;22(5):691–712. doi: 10.1016/S0167-6296(03)00060-2. [DOI] [PubMed] [Google Scholar]
- 39.Aday LA. At Risk in America: the health and health care needs of vulnerable populations. Jossey-Bass; San Francisco: 2001. [Google Scholar]
- 40.Institute of Medicine, editor. Hospital-Based Emergency Care: At the Breaking Point. Institute of Medicine; 2007; National Academy Press; Washington, DC: [Google Scholar]
- 41.Institute of Medicine . America's Health Care Safety Net: Intact but Endangered. National Academy Press; Washington, DC: 2000. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


