Abstract
Purpose
To report the world’s first case of live monozygotic dichorionic diamniotic (DD) twins after a single vitrified-warmed blastocyst transfer in a cycle during which hormone supplements were given.
Methods and results
The patient was a 39-year-old woman with tubal factor infertility. Six oocytes were retrieved and three blastocysts were vitrified after insemination with her husband’s sperm. Two months later, a single warmed blastocyst was transferred on the fifth day after progesterone supplementation during the luteal phase. Two gestational sacs and fetuses with heartbeats showing lambda sign under ultrasonography were recognized at 7 weeks of gestation and the patient gave birth to two female infants at gestational 33 weeks. The pathological examination demonstrated that the DD twin placentas fused in the third trimester.
Conclusions
This report suggests that the splitting of the transferred embryo took place after the blastocyst stage and the popular credo that the timing of embryo division governs the placental configuration of monozygotic twins (MZT) must be re-examined as to its veracity.
Keywords: Blastocyst transfer, Monozygotic DD twins, Placenta, Ultrasonography, Vitrification
Introduction
There is a long-held credo that the timing of embryo division governs the ultimate placental configuration of monozygotic twins (MZT): within 3 days of fertilization, dichorionic diamniotic (DD); between 4 and 8 days, monochorionic diamniotic (MD); and after 8 days, monochorionic monoamniotic (MM) [1]. We report the world’s first case of monozygotic DD twins (two healthy same-sex babies) after a single vitrified-warmed blastocyst transfer on day 5 after IVF during a cycle in which hormone supplements were given and no ovulation or intercourse occurred.
Case
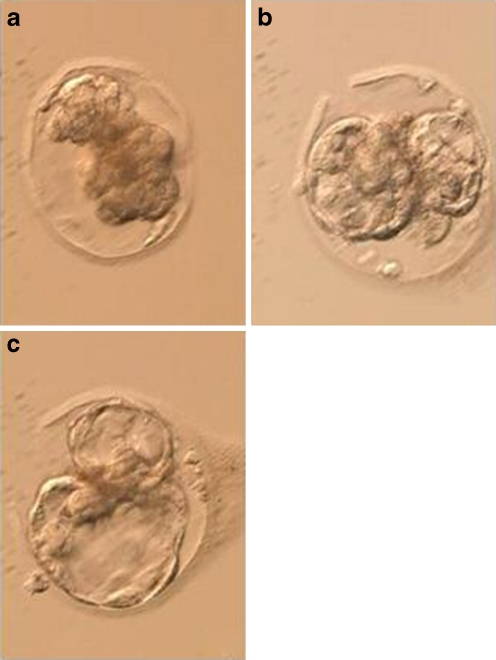
The patient was a 39-year-old woman with tubal factor infertility. We obtained approval from our Institutional Review Board and informed consent from the couple. Oocyte retrieval was performed following GnRH antagonist protocol. Six oocytes were retrieved and inseminated with her husband’s sperm. Five oocytes were fertilized and a 9-cell fresh embryo was transferred, but pregnancy was not achieved. Two blastocysts on day 5 (grade 4BC, 5BA (Fig. 1)) and one blastocyst on day 6 (grade 4BC) [2] were vitrified on a cryotop [3]. Two months later, 6 mg per day of oral estradiol (estradiol tablets, USP; Mylan Pharmaceuticals, Morgantown, USA) was administered from day 1, and 50 mg per day of progesterone (Fuji Pharmaceutical Co., Ltd., Tokyo, Japan) was administered from day 14 (blood E2 level, 415.7 pg/ml; blood progesterone level, 0.2 ng/ml; maximum follicular diameter of both ovaries, less than 10 mm; endometrial thickness, 9.1 mm). A single vitrified-warmed blastocyst was transferred on the fifth day after progesterone administration. 1.5 h after warming, the blastocyst divided into two half-blastocysts, both with trophectoderm and inner cell mass (ICM) components in spontaneously hatching zona pellucida (Fig. 2).
Fig. 1.

The fresh blastocyst on day 5; Grade 5BA before vitrification
Fig. 2.
a The shrunken blastocyst; just after warming. b The blastocyst divided into two half-blastocysts, both with trophectoderm and inner cell mass (ICM) components; 1.5 h after warming. c The blastocyst divided into two half-blastocysts, both with trophectoderm and inner cell mass (ICM) components; 2.5 h after warming
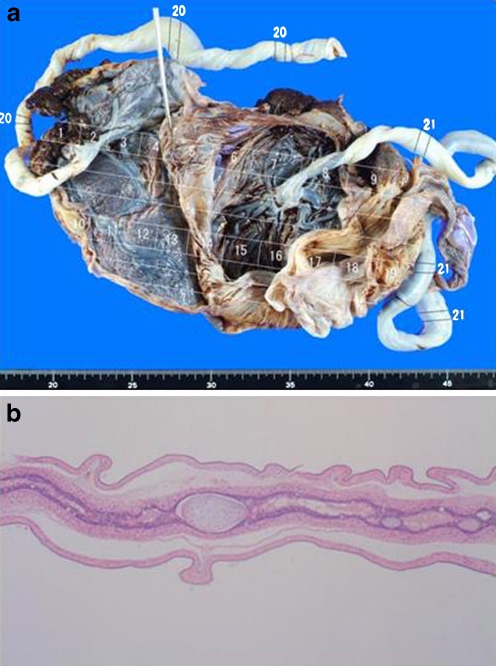
Two gestational sacs and fetuses with heartbeats showing lambda sign were recognized at 7 weeks of gestation (Fig. 3). The patient gave birth to 1,530 g and 1,388 g female infants by cesarean section at gestational 33 weeks. The pathological examination showed that the DD twin placentas fused in the third trimester (Fig. 4). We confirmed no ovulation in this patient and no intercourse between the couple during the treatment.
Fig. 3.
Lambda sign between two gestational sacs and fetuses with fetal heartbeats under ultrasonography at 7 weeks of gestation
Fig. 4.
Pathological finding: Dichorionic Diamniotic fused placentas in the third trimester. a Macroscopic finding. b Microscopic finding
Discussion
There are other reports of atypical hatching leading to twinning in the literature, in particular those of Van Langendonckt et al. [4], Meintjes et al. [5] and Behr and Milki [6], but this case is the first to report a successful birth of same-sex DD twins after a single-blastocyst transfer. Van Langendonckt et al. [4] reported a case of atypical hatching of a human blastocyst leading to monozygotic twinning. They showed a half-blastocyst in the zona pellucida and a half-blastocyst herniated through the zona pellucida in one blastocyst. After a two-blastocyst transfer, they confirmed one gestational sac and fetus with a fetal heartbeat and two gestational sacs and fetuses without fetal heartbeats and concluded that this was a dizygotic trichorial triamniotic triplet pregnancy. Meintjes et al. [5] reported a trichorionic heterozygotic triplet pregnancy with dichorionic monozygotic twins following transfer of two expanded blastocysts, one of which had two distinct ICMs. One of the triplets was ongoing at 33 weeks at the time of the original publication. Behr and Milki [6] reported a case of atypical hatching of a human blastocyst in vitro forming two identical embryos, but they did not transfer the blastocyst, so no pregnancy resulted from this.
We had chosen this embryo because its grade was higher than that of the other embryo. When we found this abnormality in the warmed embryo, we informed the patients, who decided to proceed with the embryo transfer as they did not want to waste the embryo or wait for the other embryo to warm. In our laboratory, we measure the pH of media (7.20–7.40), CO2 levels (5.5–6.5%), O2 levels (4.5–5.5%), and temperature (36.8–37.2°C) every day, and as far as we can ascertain, there were no irregularities. We speculate that this abnormal development was neither laboratory specific nor patient specific. Schieve et al. [7], Schachter et al. [8], and Milki et al. [9] identified assisted hatching, extended culture, and vitrification followed by warming as possible reasons for monozygotic twinning. However, as we followed our standard procedure in this case, the mechanism behind this abnormal development is unknown.
Ultrasonography showed lambda sign between two gestational sacs and fetuses with fetal heartbeats at 7 weeks of gestation. Carroll et al. [10] reported that the most reliable indicator for dichorionicity was a combination using the lambda sign or two separate placentas with a sensitivity and specificity of 97.4% and 100%, respectively.
Finally, we have demonstrated that the pathological finding was the DD twin placentas fused in the third trimester. In conclusion, these previous cases, along with our own report, suggest that the splitting of the transferred embryo took place after the blastocyst stage and the popular credo outlined above must be re-examined as to its veracity.
Acknowledgements
I would like to thank Dr. Masayuki Horiguchi of Ishinomaki Red Cross Hospital for assistance with the pathological examination of the placenta; and Chiharu Onuma, Kanako Narasaki and Steve Beacall for assistance with English.
Conflict of interest The authors declare that they have no conflict of interest.
Footnotes
Capsule
A successful birth of healthy monozygotic dichorionic diamniotic (DD) twins of the same gender following a single vitrified-warmed blastocyst transfer.
References
- 1.Knopman J, Krey LC, Lee J, Fino ME, Novetsky AP, Noyes N. Monozygotic twinning: an eight-year experience at a large IVF center. Fertil Steril. 2010;94:502–510. doi: 10.1016/j.fertnstert.2009.03.064. [DOI] [PubMed] [Google Scholar]
- 2.Gardner DK, Schoolcraft WB. In vitro culture of human blastocysts. In: Jansen R, Mortimer D, editors. Towards reproductive certainty: infertility and genetics beyond. Carnforth: Parthenon; 1999. pp. 378–388. [Google Scholar]
- 3.Kyono K, Fuchinoue K, Yagi A, Nakajo, Kumagai S. Successful pregnancy and delivery after transfer of a single blastocyst derived from a vitrified mature human oocyte. Fertil Steril. 2005;84(1017):e5–6. doi: 10.1016/j.fertnstert.2005.04.051. [DOI] [PubMed] [Google Scholar]
- 4.Langendonckt A, Wyns C, Godin PA, Toussaint-Demylle D, Donnez J. Atypical hatching of a human blastocyst leading to monozygotic twinning: a case report. Fertil Steril. 2000;74:1047–1050. doi: 10.1016/S0015-0282(00)01554-5. [DOI] [PubMed] [Google Scholar]
- 5.Meintjes M, Guerami AR, Rodriguez JA, Crider-Pirkle SS, Madden JD. Prospective identification of an in vitro-assisted monozygotic pregnancy based on a double-inner-cell-mass blastocyst. Fertil Steril. 2001;76(Suppl.1):172–173. doi: 10.1016/S0015-0282(01)02509-2. [DOI] [Google Scholar]
- 6.Behr B, Milki A. Visualization of atypical hatching of a human blastocyst in vitro forming two identical embryos. Fertil Steril. 2003;80:1502–1503. doi: 10.1016/j.fertnstert.2003.07.001. [DOI] [PubMed] [Google Scholar]
- 7.Schieve LA, Meikle SF, Peterson HB, Jeng G, Burnett NM, Wilcox LS. Does assisted hatching pose a risk for monozygotic twinning in pregnancies conceived through in vitro fertilization? Fertil Steril. 2000;74:288–294. doi: 10.1016/S0015-0282(00)00602-6. [DOI] [PubMed] [Google Scholar]
- 8.Schachter M, Raziel A, Friedler S, Strassburger D, Bern O, Ron-El R. Monozygotic twinning after assisted reproductive techniques: a phenomenon independent of micromanipulation. Hum Reprod. 2001;16:1264–1269. doi: 10.1093/humrep/16.6.1264. [DOI] [PubMed] [Google Scholar]
- 9.Milki AA, Jun SH, Hinckley MD, Barry B, Giudice LC, Westphal LM. Incidence of monozygotic twinning with blastocyst transfer compared to cleavage-stage transfer. Fertil Steril. 2003;79:503–506. doi: 10.1016/S0015-0282(02)04754-4. [DOI] [PubMed] [Google Scholar]
- 10.Carroll SGM, Soothill PW, Abdel-Fattah SA, Porter H, Montague I, Kyle PM. Prediction of chorionicity in twin pregnancies at 10–14 weeks of gestation. Br J Obstet Gynecol. 2002;109:182–186. doi: 10.1111/j.1471-0528.2002.01172.x. [DOI] [PubMed] [Google Scholar]