Abstract
Nigeria is highly endemic for infection with Schistosoma haematobium, which most commonly manifests itself with blood in urine. To monitor the impact of annual mass drug administration (MDA) with praziquantel for S. haematobium in Delta State, Nigeria, cross-sectional hematuria surveys of school children were conducted in 8 sentinel villages (SVs) at baseline (n=240) and after two annual doses (n=402). We assessed the comparability of three assessments of hematuria (child’s reported history, nurse visual diagnosis (NVD) and dipstick) to determine the need for mass treatment. Dipstick was considered to be the gold standard. Prior to treatment, history and NVD each identified only the 3 most highly prevalent SVs, and overall this represented just 37.5% of the 8 SVs in need of treatment. Following treatment, after dipstick prevalence decreased by 88.5% (p<0.001), and history and NVD identified only one of two villages still needing treatment. The study suggests that dipsticks should be the recommended method for launching and monitoring mass treatment for S. haematobium.
Keywords: Schistosomiasis, Praziquantel, Mass Treatment, hematuria, monitoring, Nigeria
1. Introduction
Schistosomiasis, also known as Bilharzia, is a significant public health problem, with an estimated 192 million infected people in sub-Saharan Africa, approximately 25% of the total population (Hotez and Kamath, 2009). Urinary schistosomiasis, caused by Schistosoma haematobium (SH), most commonly presents with hematuria, but serious sequelae of persistent infection include bladder fibrosis and calcification, leading to hydronephrosis, hydroureter, and bladder cancer. In addition, schistosomiasis has been associated with growth stunting, undernutrition, and impairment of cognitive development and work capacity (Ezeamama et al., 2005; King, 2010; King and Dangerfield-Cha, 2008; Zhou, 2005). Recently revised estimates incorporating the lifetime burden of disease have yielded disability adjusted life year (DALY) estimates close to that of malaria; between 24–29 million DALYs if a 2% average disability is used, and up to 49–56 million DALYs assuming a 5% estimate of disability (King, 2010).
Nigeria is one of the most endemic countries in Africa (Anosike et al., 2001; Hotez and Kamath, 2009). The distribution of SH in Nigeria was explored in a Federal Ministry of Health survey conducted in 1990–91 that showed that the infection is most prevalent in the north-central and southeastern areas of the country (Hopkins et al., 2002). Intestinal schistosomiasis due to Schistosoma mansoni has also been shown to be a significant problem in Nigeria, although its distribution is less well mapped, as it is more difficult to screen for (Gutman et al., 2008). While detection of microhematuria by reagent dipsticks provides a good proxy for detection of infection (Feldmeier, 1982; Lwambo, 1997; Mott, 1983; Savioli, 1989; Taylor, 1990), screening for intestinal schistosomiasis requires microscopic detection of eggs in the stool (Gutman et al., 2008).
Praziquantel (PZQ) is the best drug available for treatment and control of urinary schistosomiasis. It is effective against both very young and mature worms, but is less effective against juvenile worms. According to current World Health Organization (WHO) recommendations (2006)(World Health Organization, 2006), when mapping studies on a sample of school aged children show the prevalence of hematuria (assessed by history, visual diagnosis of urine, or parasitologic methods) to be ≥10% then all children in the area should receive mass treatment with PZQ every two years (World Health Organization, 2002, 2006). When the prevalence of hematuria is ≥30% by history or visual diagnosis or ≥50% by parasitologic then all children in the area should receive annual mass treatment with PZQ.
Working in central Nigeria, Hopkins noted a ≥90% reduction in prevalence of hematuria (as measured by reagent dipstick) after two rounds of annual PZQ (Hopkins et al., 2002). PZQ administration has been shown to result in short term cure rates as high as 70–98% (Augusto et al., 2009; Barakat and Morshedy, 2011; Tchuente et al., 2004), although if longer periods of follow-up are used, cure rates decrease over time (Sacko et al., 2009). PZQ has been shown to have a beneficial impact on the health status of treated children, resulting in improved growth and cognitive function of treated children (McGarvey et al., 1996; Nokes et al., 1999). In addition to schistosomiasis, PZQ has an impact on other trematodes (intestinal, liver, and lung flukes) as well as cestode infections (van den Enden, 2009).
As part of a larger PZQ mass drug administration (MDA) program in Delta state in southNigeria, we studied eight sentinel villages in Ndokwa East Local Government Area (LGA). Our purpose was to determine the impact of two rounds of PZQ treatment on the prevalence of hematuria and on the health status of children. We also sought to compare the results from heme reagent dipsticks to reported history of hematuria (‘red urine’) and visual assessment of hematuria by trained health professionals (nurses) as alternative methods for determining the need to either initiate or continue PZQ MDA in this part of Nigeria, as 2006 WHO recommendations allow for either parasitologic diagnosis or assessment of visible hematuria in determining risk to a community.
2. Material and Methods
2.1 The MDA program in Delta State
An initial prevalence survey was conducted in 2003 that followed earlier (1993) WHO guidelines that set a 20% threshold for launching MDA (World Health Organization, 1993). A mobile team visited a total of 240 villages in Ndokwa East LGA. In the village school, a random sample of 30 school aged children (aged 5–15 yrs) was tested for hematuria using heme reagent strips (‘dipsticks’). Where testing of urine showed hematuria prevalence of >20%, single dose PZQ of 40 mg/kg was provided to all school-aged children. Where hematuria prevalence in children was ≥50%, treatment was offered to the entire community. Based on the mapping results, in 2004 and 2005 PZQ MDA was offered to school aged children in 57 communities (23.8% of those villages surveyed in the initial mapping process), and entire community treatments offered those same years in 7 communities (2.9% of communities tested). Overall, 9,766 treatments were provided in Delta state in 2004 and 10,579 in 2005. Children surveyed in villages that were dipstick positive but in which the village did not qualify for MDA were immediately treated with PZQ.
PZQ is relatively expensive compared to other antihelminthics. The average dose costs about US $0.20, meaning medicine costs for Delta state in 2004 and 2005 for 20,345 treatments totaled $4,069 (Savioli et al., 2004). Given these costs, the strategy adopted by the Delta State Ministry of Health, assisted by the Carter Center, was to treat a community for two to three years, and reassess to determine if dipstick hematuria prevalence had been reduced to a level below the 20% MDA treatment threshold. If so, the plan was to rotate the PZQ to other LGAs with endemic communities. As dipstick screening is also expensive, the evaluation process involved additional evaluations using patient history or visual diagnosis of hematuria to determine if cheaper approaches could be used to decide when to treat, when to stop, and when to resume MDA.
2.2 Study sites
Eight sentinel villages (SVs) in Ndokwa East LGA, in Delta State, Nigeria, were identified during the initial prevalence survey in 2003 based on their endemicity levels (>20% prevalence of hematuria) for impact assessment. One primary school in each community was studied. The same schools were visited in both 2003 and 2005, but different samples of children were obtained each year (Fig. 1).
Figure 1.
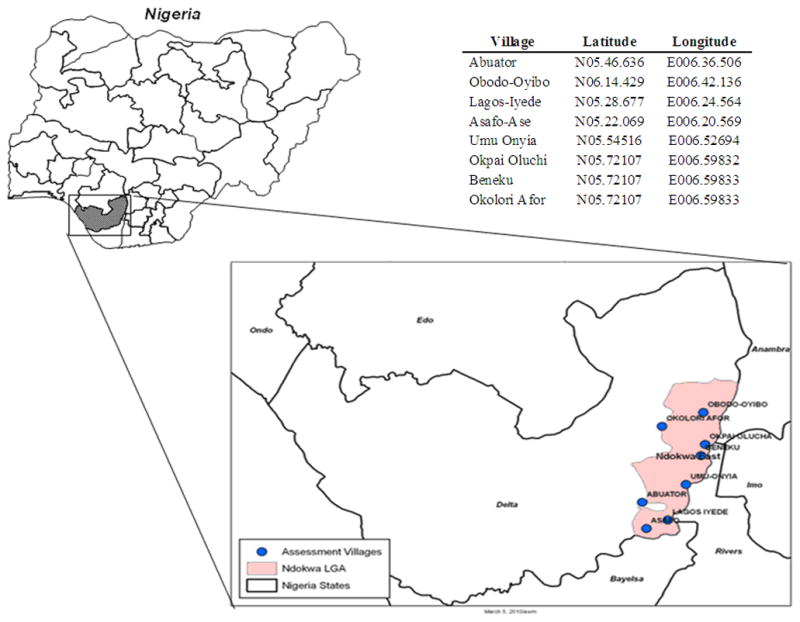
Schistosomiasis Impact Assessment Villages, Ndokwa East, Delta LGA, Nigeria
2.3 PZQ Coverage in sentinel villages
PZQ was provided using height as a surrogate for weight to determine the dose (Chuks and Okeke, 1987; Hopkins et al., 2002; World Health Organization, 2002). Treatment was delivered by trained volunteer community directed distributors (CDDs) who had village registers containing the names of all household members collected from ivermectin MDA (for onchocerciasis) provided for many years in these same communities. For mass treatment villages, coverage was calculated based on the percent of the eligible population (based on these registers) treated, while for villages requiring only school aged treatment, coverage was based on the percent of all school aged children (aged 5– 15 years) treated in that village (Table 1). PZQ MDA was given at a different time of the year than ivermectin MDA.
Table 1.
Treatment with Praziquantel 2004 to 2005
| Village | Tx Type | 2004 | 2005 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Total Pop. | Eligible Pop. | Tx | % Coverage | Total Pop. | Eligible Pop. | Tx | % Coverage | ||
| Abuator | Mass | 1,626 | 1301 | 1280 | 98 | 1,788 | 1431 | 1408 | 98 |
| Obodo-Oyibo | Mass | 682 | 546 | 546 | 100 | 752 | 602 | 586 | 97 |
| Lagos-Iyede | Mass | 702 | 562 | 562 | 100 | 772 | 618 | 600 | 97 |
| Asafo-Ase | School Age | 1,293 | 608 | 590 | 97 | 1,357 | 638 | 609 | 95 |
| Umu Onyia | School Age | 4,725 | 650 | 638 | 98 | 4,553 | 715 | 701 | 98 |
| Okpai Oluchi | School Age | 1,123 | 528 | 458 | 87 | 1,204 | 566 | 503 | 89 |
| Beneku | School Age | 874 | 411 | 408 | 99 | 940 | 442 | 428 | 97 |
| Okolori Afor | School Age | 591 | 278 | 270 | 97 | 638 | 300 | 287 | 96 |
Pop. = Population
Tx = Treatment
2.4 Surveys
Cross-sectional surveys were conducted in the SVs in 2003 and 2005 to determine the point prevalence of children who had blood in the urine. In 2003, sampling followed the overall Delta state mapping protocol, with 30 pupils randomly selected from classes one to six (5 pupils per class, restricted to those aged 5– 15 years) for assessment using the school register. The total number of children in each class was noted, and then this number divided by a number “n” such that selecting every nth child on the list results in 5 children being selected. For the follow-up survey in 2005, in anticipation of reduced hematuria prevalence, up to 60 pupils per school were randomly selected from primary classes one to six (up to 10 pupils per class, restricted to those aged 5– 15 years) for examination, using the same method to ensure a representative sample. In 4 of the eight schools it was not possible to enroll 60 pupils, in which case all eligible children of the proper age range were enrolled.
The surveys also determined the percentage of children tested by dipstick who also reported blood in the urine and the results of a visual examination of the urine by a nurse before dipstick testing (nurse visual diagnosis - NVD). The procedure was as follows: pupils were first asked if they had recently passed blood in their urine (‘red urine’). The child was then given a clean transparent specimen bottle and told to immediately fill it with a mid-terminal urine sample. Upon return, the nurse inspected the urine and recorded the presence of visible hematuria. Once recorded (the entry could not be changed) the heme reagent dipstick test (Medi-Test Combi – 9® Macherey-Nagel) was performed, and read against the key on the dipstick jar as negative, 1+, 2+ or 3+). In the analysis, any positive dipstick result was considered the gold standard for hematuria.
2.5 Data analysis
The results of the 2005 survey were compared with the baseline data obtained in the 2003 using EpiInfo6 (CDC, Atlanta, GA), SPSS (IBM, Somers, NY), and SAS (Version 9.2, Cary, NC) software. We calculated means and standard deviations for numeric variables, prevalence of dipstick positivity, and percent reduction of hematuria. Fisher s exact test was used to determine significance of associations. Test results were considered statistically significant with p- value < 0.05.
Unlike the baseline data, in the follow up evaluation we used current (2006) WHO recommendations for a lower MDA cutoff of 10% as the threshold for deciding if continued treatment to all school- aged children was needed, regardless of the method of assessment (World Health Organization, 2006). The threshold for delivering treatment to the entire community was 30% if a questionnaire or visual method is used, but 50% for parasitologic methods. Heme dipsticks are not mentioned in the 2003 WHO guidelines. However, since heme dipsticks are generally considered to be more sensitive than visual methods, with an ability to detect microscopic hematuria with as few as 1–3 red blood cells per high power field (Shaw et al., 1985), we judged the dipstick results to be equivalent to parasitologic methods, and continued to use a cut-off of 50% prevalence to require community wide therapy.
2.6 Ethical issues
Ministry of health officials gave approval for the study and conveyed this to all the schools through the LGA education authority. Consent was also obtained from each school and community leaders before any pupils were enlisted. Rapid assessment procedures for urinary schistosomiasis were reviewed and deemed as non-research by the Emory University Institutional Review Board.
3. Results
3.1 Treatment coverage in sentinel villages
In the baseline survey, 3 of the sentinel villages were classified by dipstick estimation of hematuria prevalence as needing total population coverage, while the other 5 required treatment of school aged children (Table 1). In the 3 villages requiring total population coverage, > 90% coverage of the eligible population was attained both years; in the 5 villages requiring treatment of school aged children, coverage rates >90% were obtained both years with the exception of Okpai Oluchi, where coverage was >85% for the two years (Table 1).
Two hundred and forty children were enrolled in the 2003 survey (30 per community), and 403 were enrolled in the 2005 survey (34– 60 children per community). In 2003, 56.6% (95% Confidence Interval 50.3–63.0%) of those enrolled were male, while in 2005, 50.5% (36.9–64.1%) were male (p= 0.36). The mean age of enrolled children was 10.2 years in both 2003 and 2005; there was no significant difference in the age distribution of enrolled children between the 2 surveys.
3.2 Hematuria measured by urinary dipstick
We saw a dramatic decrease in hematuria in all the villages surveyed following two rounds of PZQ treatment, with an 88.5% overall reduction in dipstick positivity from 49.6% to 5.7% (p<0.001) (Table 2). Both the presence of any hematuria and the severity of hematuria decreased; 26.7% of children had 3+ hematuria in 2003, while only 2.5% had grade 3+ hematuria in 2005. By definition, all our SVs exceeded the 20% dipstick threshold for treatment in 2003; in 2005, following 2 rounds of PZQ, only two villages (Abuator and Obodo-Oyibo), exceeded the new WHO threshold of 10%, indicating need for continued school aged treatment (Table 3a).
Table 2.
Impact of PZQ on Schistosomiasis in Delta State by Assessment indicators
| Assessment Indicator | Pre-treatment Survey 2003, n=240 | Post-treatment survey 2005, n=402 | Percent Reduction | P- value | ||
|---|---|---|---|---|---|---|
| Number | % | Number | % | |||
| History | 31 | 12.9 | 14 | 3.5 | 72.9 | <0.001 |
| NVD | 53 | 22.1 | 10 | 2.5 | 88.7 | <0.001 |
| Dipstick | 119 | 49.6 | 23 | 5.7 | 88.5 | <0.001 |
NVD: Nurse Visual Diagnosis of Hematuria
Table 3a.
Prevalence of Schistosomiasis by history, NVD, and urine dipstick in Sentinel communities in Ndokwa East LGA at baseline (2003) and follow-up (2005).
| Baseline data | Follow-up data | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Community | N | History +ve | NVD +ve | Dipstick +ve | N | History +ve | NVD +ve | Dipstick +ve | % Reduction* | p-value |
| Abuator | 30 | 17 (56.7%) | 23 (76.7%) | 28 (93.3%) | 60 | 7 (11.7%) | 7 (11.7%) | 12 (20%) | 78.6 | <0.0001 |
| Obodo-Oyibo | 30 | 4 (13.3%) | 19 (63.3%) | 28 (93.3%) | 35 | 2 (5.7%) | 2 (5.7%) | 5 (14.3%) | 84.7 | <0.0001 |
| Lagos- Iyede | 30 | 5 (16.7%) | 6 (20%) | 20 (66.7%) | 60 | 0 | 0 | 0 | 100 | <0.0001 |
| Asafor Ase | 30 | 1 (3.3%) | 1 (3.3%) | 13 (43.3%) | 42 | 0 | 0 | 0 | 100 | <0.0001 |
| Umu Onyia | 30 | 2 (6.7%) | 0 | 9 (30%) | 52 | 4 (7.7%) | 1 (1.9%) | 4 (7.7%) | 74.3 | 0.0118 |
| Okpai-Oluchi | 30 | 0 | 2 (6.7%) | 8 (26.7%) | 60 | 1 (1.7%) | 1 (1.7%) | 2 (3.3%) | 87.6 | 0.002 |
| Beneku | 30 | 0 | 1 (3.3%) | 7 (23.3%) | 60 | 0 | 0 | 0 | 100 | <0.0001 |
| Okolori-Afor | 30 | 2 (6.7%) | 1 (3.3%) | 6 (20%) | 34 | 0 | 0 | 0 | 100 | 0.0079 |
| Total | 240 | 31 | 53 | 119 (49.6%) | 403 | 14 | 11 | 23 (5.7%) | 88.5 | <0.0001 |
Percent prevalence reduction based on dipstick testing
NVD-Nurse Visual Diagnosis of Hematuria
3.3 Hematuria measured by child’s history and nurse visual diagnosis of hematuria
On the individual level, there was poor correlation between hematuria identified by history and NVD. Only 52% of those children identified as having hematuria by NVD also gave a history of red urine; 73% of those who gave a history of red urine were identified as having hematuria by NVD. The percent of children reporting hematuria decreased significantly, by 72.9% (p<0.001), between baseline and follow-up. Similarly, NVD of hematuria dropped by 88.7% (p<0.001).
Neither history of hematuria nor NVD was a sensitive measure for detecting at risk communities (Table 3b). Prior to treatment, history and NVD each identified only the 3 most highly prevalent SVs, and overall this represented just 37.5% of the 8 SVs in need of treatment. Following MDA, both history and NVD identified only one (Abuator) of two villages (Abuator and Obodo-Oyibo) still in need of school-aged MDA treatment.
Table 3b.
Programmatic Decisions for MDA based on Prevalence of Schistosomiasis by history, NVD, and urine dipstick in Sentinel communities in Ndokwa East LGA at baseline (2003) and follow-up (2005).
| Baseline data | Follow-up data | |||||||
|---|---|---|---|---|---|---|---|---|
| Community | N | MDA History +ve |
MDA NVD +ve |
MDA Dipstick +ve |
N | MDA History +ve |
MDA NVD +ve |
MDA Dipstick +ve |
| Abuator | 30 | C | C | C | 60 | S | S | S |
| Obodo-Oyibo | 30 | S | C | C | 35 | - | - | S |
| Lagos- Iyede | 30 | S | S | C | 60 | - | - | - |
| Asafor Ase | 30 | - | - | S | 42 | - | - | - |
| Umu Onyia | 30 | - | - | S | 52 | - | - | - |
| Okpai-Oluchi | 30 | - | - | S | 60 | - | - | - |
| Beneku | 30 | - | - | S | 60 | - | - | - |
| Okolori-Afor | 30 | - | - | S | 34 | - | - | - |
C=Community wide MDA, S=School aged children MDA
NVD: Nurse Visual Diagnosis of Hematuria
Communities qualified for treatment of all school aged children if the prevalence of hematuria was ≥10% by any method in a sample of school aged children. Communities qualified for community wide treatment if the prevalence of hematuria and visual diagnosis or history was ≥50%
When child’s history and nurse s diagnosis were compared to dipstick reading (the gold standard), overall, history had a sensitivity of 31% and NVD had a sensitivity of 44%, however, the sensitivity of both history and NVD increased with increasing grade of hematuria as assessed by dipstick (Table 4a and b).
Table 4a.
Sensitivity and specificity for history and NVD by year
| 2003 | 2005 | |||
|---|---|---|---|---|
| History | NVD | History | NVD | |
| Sensitivity | 25.2% | 44.5% | 60.9% | 43.5% |
| Specificity | 99.1% | 100% | 100% | 100% |
Table 4b.
Sensitivity of History and NVD as compared to different levels of dipstick positivity
| Positive Dipstick | Positive History | Sensitivity of History | Positive NVD | Sensitivity of NVD | |
|---|---|---|---|---|---|
| 1+ | 42 | 3 | 7.1% | 0 | 0.0% |
| 2+ | 26 | 5 | 19.2% | 3 | 11.5% |
| 3+ | 74 | 36 | 48.7% | 60 | 81.1% |
| Overall | 142 | 44 | 31.0% | 63 | 44.4% |
NVD: Nurse Visual Diagnosis of Hematuria
4. Discussion
Following 2 rounds of PZQ MDA, we observed an 88.5% decrease in prevalence of urinary schistosomiasis, measured by urine dipstick for hematuria, and only 2 of 8 villages had a high enough prevalence of hematuria to warrant further MDA based on 2006 WHO guidelines. Nurse visual diagnosis and child’s history of hematuria did not appear to be sufficiently sensitive methods of assessment for initial mapping when compared to results obtained by urine dipstick analysis, as noted previously (Lwambo, 1997). If only these methods had been used, 5 of the 8 villages where we demonstrated treatment benefit would not have been identified or treated. In addition, in impact assessment both history and NVD identified only 1 of the 2 villages that required continued MDA after two years. Therefore, we believe that dipsticks would be most useful in quickly determining a community for MDA, and later the impact of treatment. Another possibility would be to use a 2 stage screening methodology, whereby visual diagnosis of hematuria precedes use of dipsticks. If a community qualifies for treatment on the basis of prevalence of visible hematuria (≥30%), then there is no need for subsequent assessment with dipsticks. This might provide some cost savings to screening programs. If a PZQ holiday MDA rotation schedule is elected, the dipsticks would also be useful to determine if and when recrudescence was occurring and reinstitution of MDA as needed. Although in this study, the sensitivity and specificity of dipsticks as compared to urine microscopy was not measured, urine dipsticks have been shown in other studies to have high sensitivity and specificity for detection of urinary schistosomiasis (French et al., 2007; Lwambo, 1997). As a tool for large scale screening of villages, urine dipsticks are likely to be more cost effective and logistically much simpler than parasitologic screening. Although in the future, schistosoma specific dipsticks, such as urine CCA dipsticks, may prove to be more useful, currently, the sensitivity and specificity of these tests is inadequate to make them a useful tool for screening of urinary schistosomiasis (Stothard et al., 2009).
WHO recommends different treatment strategies depending on the prevalence of infection in the community; however, there are little data on the differing impact of MDA targeting school- aged children only versus targeting the entire community (World Health Organization, 1993, 2002, 2006). In our study, there was a similar percent decrease in hematuria in those communities treated with MDA of the whole community versus school-aged children. However, the force of transmission was likely to have been considerably different between these communities. Baseline and follow-up parasitological examinations of urine with calculations of egg densities might have allowed better distinction of the different force of transmission acting in different communities, and perhaps a differential impact of the two interventions.
School based treatment programs will be less effective in communities where a large proportion of school-aged children do not attend school. This is a particular concern in farming communities in Nigeria where many of the children may be required to help in the fields. To ameliorate this problem, we used community directed distributors who, as a result of their ivermectin MDA work, had community records that allowed them to seek out school aged children both in and out of school for PZQ treatment. It has been suggested that CDDs, as a result of their community level records are better able than teachers to reach school aged children. However, we did not determine in this study if CDDs with their ivermectin records addressed the issues of who misses-out in school-based PZQ treatments (Husein et al., 1996), and ensured high coverage of targeted persons (90% coverage) (Table 1).
Although the prevalence of hematuria (by dipstick) fell below 10% in 6 of the 8 villages, it is unlikely that drug distribution can be permanently withdrawn without recrudescence of infection. Continued monitoring for recrudescence is required in all villages where PZQ holidays are contemplated. In any scenario, intensified health education is needed to get residents (especially school aged boys) to stop urinating in water, but this may extend the time before PZQ must be reinitiated.
5. Conclusion
In independent samples of school children taken from the same schools, we found that two rounds of PZQ treatment reduced hematuria prevalence (as determined by dipstick) by over 88%. Compared to dipstick, both a child’s reported history of hematuria and nurse visual diagnosis had a low sensitivity for detecting villages in need of MDA (31% and 44% of such villages, respectively). History of hematuria and nurse visual diagnosis identified one of the two sentinel village still in need of treatment after two MDA rounds, both of which were the most endemic of all communities at baseline. Dipsticks should be the recommended method for assessing hematuria for deciding on and continuing mass treatment for S. haematobium.
Highlights.
We monitored impact of annual praziquantel for S. haematobium in Delta State, Nigeria
Cross-sectional surveys of school children conducted at baseline and after two years
Compared three assessments of hematuria to determine the need for mass treatment
Following treatment, dipstick prevalence of hematuria decreased by 88.5% (p<0.001)
History and NVD failed to identify all communities in need of treatment
Acknowledgments
We thank the State Ministry of Health Delta for approving this study and providing the logistics, human, and material resources used. We also thank Chevron Nigeria Limited, the John Hussman Foundation, and the Izumi Foundation for funding support to the Delta State schistosomiasis program. Dr. Patricia Graves provided helpful comments to the manuscript. JG was supported in part by PHS Grant UL1 RR025008 and KL2 RR025009 from the Clinical and Translational Science Award program, National Institutes of Health, National Center for Research Resources.
Role of the funding source
The funding sources had no role in the study design, collection, analysis, or interpretation of data, in the writing of the report, or in the decision to submit the paper for publication.
Abbreviations
- SH
Schistosoma haematobium
- DALY
Disability adjusted life year
- PZQ
Praziquantel
- MDA
Mass drug administration
- LGA
Local Government Area
- CDD
Community directed distributor
- NVD
Nurse visual diagnosis
Footnotes
Disclosure Statement
We have no conflicts of interest to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Emmanuel Emukah, Email: emukahe@yahoo.com.
Julie Gutman, Email: gutmanjr@gmail.com.
John Eguagie, Email: eguagiejohn@yahoo.com.
Emmanuel S Miri, Email: emmamiri@yahoo.com.
Paul Yinkore, Email: yinkore11@yahoo.com.
Ndudi Okocha, Email: opokocha@yahoo.com.
Victoria Jibunor, Email: victoriajibunor@yahoo.com.
Nebe Obiageli, Email: nebeoj@yahoo.com.
Nwoye Augustine Ikenna, Email: nwoyeai@yahoo.com.
Frank O. Richards, Email: frich01@emory.edu.
References
- Anosike JC, Nwoke BE, Njoku AJ. The validity of haematuria in the community diagnosis of urinary schistosomiasis infections. Journal of Helminthology. 2001;75:223–225. [PubMed] [Google Scholar]
- Augusto G, Magnussen P, Kristensen TK, Appleton CC, Vennervald BJ. The influence of transmission season on parasitological cure rates and intensity of infection after praziquantel treatment of Schistosoma haematobium-infected schoolchildren in Mozambique. Parasitology. 2009;136:1771–1779. doi: 10.1017/S0031182009006210. [DOI] [PubMed] [Google Scholar]
- Barakat R, Morshedy HE. Efficacy of two praziquantel treatments among primary school children in an area of high Schistosoma mansoni endemicity, Nile Delta, Egypt. Parasitology. 2011;138:440–446. doi: 10.1017/S003118201000154X. [DOI] [PubMed] [Google Scholar]
- Chuks EG, Okeke GC. Chemotherapy of Urinary Schistosomiasis in Nigeria. Journal of Tropical Medicine and Hygeine. 1987;90:149–151. [PubMed] [Google Scholar]
- Ezeamama AE, Friedman JF, Acosta LP, Bellinger DC, Langdon GC, Manalo DL, Olveda RM, Kurtis JD, McGarvey ST. Helminth infection and cognitive impairment among Filipino children. American Journal of Tropical Medicine and Hygeine. 2005;72:540–548. [PMC free article] [PubMed] [Google Scholar]
- Feldmeier H, Doehring E, Daffalla AA. Simultaneous use of a sensitive filtration technique and reagent strips in urinary schistosomiasis. Trans R Soc Trop Med Hyg. 1982;76:416–421. doi: 10.1016/0035-9203(82)90204-8. [DOI] [PubMed] [Google Scholar]
- French MD, Rollinson D, Basanez MG, Mgeni AF, Khamis IS, Stothard JR. School-based control of urinary schistosomiasis on Zanzibar, Tanzania: Monitoring micro-haematuria with reagent strips as a rapid urological assessment. Journal of pediatric urology. 2007;3:364–368. doi: 10.1016/j.jpurol.2007.01.198. [DOI] [PubMed] [Google Scholar]
- Gutman J, Fagbemi A, Alphonsus K, Eigege A, Miri ES, Richards FOJ. Missed treatment opportunities for schistosomiasis mansoni, in an active programme for the treatment of urinary schistosomiasis in Plateau and Nasarawa states, Nigeria. Annals of Tropical Medicine and Parasitology. 2008;102:335–346. doi: 10.1179/136485908X278810. [DOI] [PubMed] [Google Scholar]
- Hopkins DR, Eigege S, Miri ES, Gontor I, Ogah G, Umaru J, Gwomkudu CD, Matha W, Jinadu MY, Amadiegwu S, Oyeneka OK, Korve K, Richards FOJ. Lymphatic filariasis elimination and schistosomiasis control in combination with onchocerciasis control in Nigeria. American Journal of Tropical Medicine and Hygeine. 2002;67:266–272. doi: 10.4269/ajtmh.2002.67.266. [DOI] [PubMed] [Google Scholar]
- Hotez PJ, Kamath A. Neglected Tropical Diseases in Sub-Saharan Africa: Review of Their Prevalence, Distribution, and Disease Burden. PLoS Neglected Tropical Diseases. 2009;3:e412. doi: 10.1371/journal.pntd.0000412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Husein MH, Talaat M, El-Sayed MK, El-Badawi A, Evans DB. Who misses out with school-based health programmes? A study of schistosomiasis control in Egypt. Trans R Soc Trop Med Hyg. 1996;90:362–365. doi: 10.1016/s0035-9203(96)90506-4. [DOI] [PubMed] [Google Scholar]
- King CH. Parasites and poverty: The case of schistosomiasis. Acta Tropica. 2010;113:95–104. doi: 10.1016/j.actatropica.2009.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King CH, Dangerfield-Cha M. The unacknowledged impact of chronic schistosomiasis. Chronic Illness. 2008;4:65–79. doi: 10.1177/1742395307084407. [DOI] [PubMed] [Google Scholar]
- Lwambo N, Savioli L, Kisumku UM, Alawi KS, Bundy DA. Control of Schistosoma haematobium morbidity on Pemba Island: validity and efficiency of indirect screening tests. Bull World Health Organ. 1997;75:247–252. [PMC free article] [PubMed] [Google Scholar]
- McGarvey ST, Aligui G, Graham KK, Peters P, Olds GR, Olveda R. Schistosomiasis japonica and Childhood Nutritional Status in Northeastern Leyte, the Philippines: A Randomized Trial of Praziquantel Versus Placebo. American Journal of Tropical Medicine and Hygeine. 1996;54:498–502. doi: 10.4269/ajtmh.1996.54.498. [DOI] [PubMed] [Google Scholar]
- Mott K, Dixon H, Osei-Tut E, England EC. Relation between intensity of Schistosoma haematobium infection and clinical haematuria and proteinuria. Lancet. 1983;1:1005–1008. doi: 10.1016/s0140-6736(83)92641-7. [DOI] [PubMed] [Google Scholar]
- Nokes C, McGarvey ST, Shiue L, Wu G, Wu H, Bundy DA, Olds GR. Evidence for an improvement in cognitive function following treatment of Schistosoma japonicum infection in Chinese primary schoolchildren. American Journal of Tropical Medicine and Hygeine. 1999;60:556–565. doi: 10.4269/ajtmh.1999.60.556. [DOI] [PubMed] [Google Scholar]
- Sacko M, Magnussen P, Traore M, Landoure A, Doucoure A, Reimert CM, Vennervald BJ. The effect of single dose versus two doses of praziquantel on Schistosoma haematobium infection and pathology among school-aged children in Mali. Parasitology. 2009;136:1851–1857. doi: 10.1017/S0031182008000486. [DOI] [PubMed] [Google Scholar]
- Savioli L, MA, Engles D, Montresor A. Progress in the prevention and control of schistosomiasis and soil-transmitted helminthiasis. Parasitology International. 2004;53:103–113. doi: 10.1016/j.parint.2004.01.001. [DOI] [PubMed] [Google Scholar]
- Savioli L, Mott KE. Urinary schistosomiasis on Pemba Island: low-cost diagnosis for control in a primary health care setting. Parasitol Today. 1989;5:333–337. doi: 10.1016/0169-4758(89)90129-4. [DOI] [PubMed] [Google Scholar]
- Shaw ST, Poon SY, Wong ET. ‘Routine Urinalysis’ Is the Dipstick Enough? JAMA: The Journal of the American Medical Association. 1985;253:1596–1600. doi: 10.1001/jama.253.11.1596. [DOI] [PubMed] [Google Scholar]
- Stothard JR, Sousa-Figueiredo JC, Standley C, Van Dam GJ, Knopp S, Utzinger J, Ameri H, Khamis AN, Khamis IS, Deelder AM, Mohammed KA, Rollinson D. An evaluation of urine-CCA strip test and fingerprick blood SEA-ELISA for detection of urinary schistosomiasis in schoolchildren in Zanzibar. Acta Tropica. 2009;111:64–70. doi: 10.1016/j.actatropica.2009.02.009. [DOI] [PubMed] [Google Scholar]
- Taylor P, Chandiwana SK, Matanhire D. Evaluation of the reagent strip test for haematuria in the control of Schistosoma haematobium infection in schoolchildren. Acta Trop. 1990;47:91–100. doi: 10.1016/0001-706x(90)90071-7. [DOI] [PubMed] [Google Scholar]
- Tchuente LAT, Shaw DJ, Polla L, Cioli D, Vercruysse J. Efficacy of Praziquantel against Schistosoma hematobium infection in Children. American Journal of Tropical Medicine and Hygeine. 2004;71:778–782. [PubMed] [Google Scholar]
- van den Enden E. Pharmacotherapy of helminth infection. Expert Opinion on Pharmacotherapy. 2009;10:435–451. doi: 10.1517/14656560902722463. [DOI] [PubMed] [Google Scholar]
- World Health Organization. World Health Organization Technical Report Series. 1993. WHO Expert Committee on the Control of Schistosomiasis. The control of schistosomiasis: second report of the WHO Expert Committee; p. 830. [PubMed] [Google Scholar]
- World Health Organization. World Health Organization Technical Report Series. 2002. Prevention and Control of Schistosomiasis and Soil Transmitted Helminths: report of a WHO expert committee; p. 912. [Google Scholar]
- World Health Organization. Preventive chemotherapy in human helminthiasis : coordinated use of anthelminthic drugs in control interventions : a manual for health professionals and programme managers. Geneva, Switzerland: WHO; 2006. [Google Scholar]
- Zhou H, Ohtsuka R, Yankang HE, Yuan L, Yamauchi T, Sleigh A. Impact of Parasitic Infections and Dietary Intake on Child Growth in the Schistosomiasis-Endemic Dongting Lake Region, China. Am J Trop Med Hyg. 2005;72:534–539. [PubMed] [Google Scholar]


