Abstract
Although neuronal RNA oxidation is a prominent and established feature in age-associated neurodegenerative disorders such as Alzheimer disease (AD), oxidative damage to neuronal RNA in aging and in the transitional stages from normal elderly to the onset of AD has not been fully examined. In this study, we used an in situ approach to identify an oxidized RNA nucleoside 8-hydroxyguanosine (8OHG) in the cerebral cortex of 65 individuals without dementia ranging in age from 0.3 to 86 years. We also examined brain samples from 20 elderly who were evaluated for their premortem clinical dementia rating score and postmortem brain pathological diagnoses to investigate preclinical AD and mild cognitive impairment. Relative density measurements of 8OHG-immunoreactivity revealed a statistically significant increase in neuronal RNA oxidation during aging in the hippocampus and the temporal neocortex. In subjects with mild cognitive impairment but not preclinical AD, neurons of the temporal cortex showed a higher burden of oxidized RNA compared to age-matched controls. These results indicate that although neuronal RNA oxidation fundamentally occurs as an age-associated phenomenon, more prominent RNA damage than in normal aging correlates with the onset of cognitive impairment in the prodromal stage of AD.
Keywords: Aging, 8-hydroxyguanosine, Mild cognitive impairment, Neurodegeneration, Oxidative damage, Preclinical Alzheimer disease, RNA
INTRODUCTION
Cells in the brain encounter a cumulative burden of oxidative and metabolic stress that may be a universal feature of the aging process as well as a major causal factor of age-related dysfunction. Macromolecules, including nucleic acids, proteins, and lipids, are oxidatively modified during aging. Indeed, the brain is particularly vulnerable to free radical damage because of its high oxygen consumption rate, abundant lipid content, and relative paucity of antioxidant enzymes compared with other organs (1, 2). Although oxidative damage to DNA is more frequently investigated than oxidative damage to RNA, cellular RNA molecules may be more susceptible to oxidative insult than DNA because of their single-stranded structure without protective histones. Moreover, ribosomal RNA molecules are located closely to mitochondria, a major source of free radicals (3). We have focused on RNA oxidation and for the first time reported RNA oxidation in vulnerable neurons in Alzheimer disease (AD) (4); this was followed by further in situ and biochemical studies on AD (5–10), as well as studies elucidating neuronal RNA oxidation in other age-associated degenerative disorders such as Parkinson disease (11), dementia with Lewy bodies (12) and amyotrophic lateral sclerosis (13). Although nucleic acids oxidation, predominantly in RNA, was reported in the aged rat brain (14, 15), age-associated changes in the RNA oxidation in human brain have not been investigated.
To understand the process of age-associated neurodegenerative diseases, it is important to investigate not only the underlying mechanisms of brain aging but also the transition from normality to the onset of symptomatic disease. For AD, subjects at the preclinical stage and subsequent prodromal stage of mild cognitive impairment (MCI) have become a research focus. Several previous studies have demonstrated oxidative damage to proteins, lipids and nucleic acids in brains of MCI cases (16–21); some studies have focused on oxidative RNA damage (22, 23). A few recent studies have investigated oxidative protein modification and lipid peroxidation in brains of preclinical AD (24–27), but oxidative RNA damage in preclinical AD has not been studied. Whether or not there are significant changes in levels of oxidative damage in brains of preclinical AD cases is controversial. Using a proteomic approach, Terni et al showed that the mitochondrial ATP-synthase was oxidized in the entorhinal cortex at the early stages of AD-related tau pathology (stages I/II of Braak), which correspond to a clinically silent period (24). Bradley et al reported increased levels of 4-hydroxynonenal and acrolein in the hippocampus and decreased levels of these lipid peroxidation products in the cerebellum in preclinical AD (25). However, that report showed no significant changes in levels of these lipid peroxidation products in the temporal cortex and no significant changes in levels of protein carbonyls in the hippocampus, the temporal cortex or the cerebellum. Aluise et al also observed no significant changes in levels of 4-hydroxynonenal, protein carbonyls and 3-nitrotyrosine in the parietal cortex of preclinical AD cases (26, 27).
In this study, we used an in situ approach to identify an oxidized RNA nucleoside, 8-hydroxyguanosine (8OHG) in the cerebral cortex of subjects from an aging series of non-demented individuals between the first and the ninth decade. We also investigated neuronal RNA oxidation in the cerebral cortex among elderly subjects at transitional stages between normality and dementia, i.e. preclinical AD and MCI.
MATERIALS AND METHODS
Tissue
For experiment 1 (neuronal RNA oxidation in aging brains), brain tissue samples were obtained at autopsy from 2 consecutive series of subjects without dementia or other neurological disorders collected at the Department of Pathology, Case Western Reserve University. Group I consisted of 27 subjects (ages 3–86 years); Group II consisted of 38 subjects (ages 0.3–82 years). Postmortem intervals (PMI) prior to fixation were 4 to 27 hours (mean = 15.6 ± 6.7 [SD] hours) in Group I and 3 to 30 hours (11.1 ± 7.4 hours) in Group II. Slices of the hippocampus and the subiculum from Group I cases were fixed in methacarn (methanol/chloroform/acetic acid, 6:3:1); slices of the temporal cortex including the inferior temporal gyrus or the occipitotemporal gyrus from the Group II cases were fixed in phosphate-buffered formalin. After fixation, all the tissue slices were dehydrated through graded ethanols followed by xylene, and embedded in paraffin. Six-μm-thick sections were cut and mounted on Silane (Sigma, St. Louis, MO)-coated glass slides.
For experiment 2 (neuronal RNA oxidation in preclinical AD and MCI), a series of paraffin sections of the temporal cortex and cerebellum were obtained from the Neuropathology Core Laboratory of the Washington University Alzheimer’s Disease Research Center (St. Louis, MO). Cases representing 4 distinct diagnostic categories using the Clinical Dementia Rating (CDR) (28–30) were studied. Control cases were cognitively normal individuals that are generally free of amyloid plaques and neurofibrillary tangles (NFTs) in the brain. Cognitively normal individuals that met current pathological criteria for AD (31) were classified as preclinical AD. The borderline condition between normal and dementia, defined as CDR = 0.5, were classified as MCI. The level of CDR = 0.5 covers not only subjects with the core MCI but also “pre-MCI” and “very mild dementia” (32, 33). Subjects with MCI (CDR = 0.5) and mild dementia (CDR = 1) met pathological criteria for AD (30). There were 5 control cases (ages 80–95 years; PMI 6–13 hours), 4 cases with preclinical AD (ages 83–93 years; PMI 2–17 hours), 6 cases with MCI (ages 90–102 years; PMI 6–23 hours), and 5 cases with mild AD (ages 74–96 years 4–13 hours) (Table). At autopsy, samples of the temporal cortex and cerebellum were fixed in phosphate-buffered formalin and embedded in paraffin. Six-μm-thick sections were cut and mounted on Silane-coated slides.
Table.
Classification of 4 Categories of Subjects According to Clinical Dementia Rating Score and CERAD Pathological Criteria
| Category | CDR | Brain Pathology (CERAD) | (n) | Age, mean (SD) (years) | PMI, mean (SD) (hours) |
|---|---|---|---|---|---|
| Controls | 0 | normal | 5 | 88.4 (5.7) | 10.8 (3.8) |
| Preclinical AD | 0 | definite AD | 4 | 88.8 (4.3) | 10.2 (6.2) |
| MCI | 0.5 | definite AD (n = 5) possible AD (n = 1) |
6 | 93.5 (4.5) | 13.7 (7.0) |
| Mild AD | 1 | definite AD | 5 | 85.4 (8.1) | 9.2 (3.8) |
Immunocytochemistry and Antibodies
Immunostaining was performed in batches of 10 slides at the same time. Samples from subjects of different age decades in Experiment 1 and from subjects in all 4 diagnostic categories in Experiment 2 were included in each batch. All steps of each immunostaining were carefully controlled so that all the slides were processed with the identical solutions and incubated for identical times. Following deparaffinization with xylene (3 times, 10 minutes each), sections were hydrated through a graded ethanol series (100%, 95%, 70% and 50% ethanol, 10 minutes each). Endogenous peroxidase activity was eliminated by 30-minute incubation with 3% H2O2 in methanol and non-specific binding sites were blocked by 30-minute incubation with 10% normal goat serum in Tris-buffered saline (150 mM Tris-HCl, 150 mM NaCl, pH 7.6). A mouse monoclonal antibody against 8OHG (1F7, 1:30; Trevigen, Gaithersburg, MD) was used to detect oxidized nucleosides (34) to detect oxidized nucleosides. Following treatment with 10 μg/ml proteinase K (Boehringer Mannheim, Indianapolis, IN) in phosphate buffered saline (pH = 7.4) for 40 minutes at 37°C, sections were incubated with the 1F7 for 18 hours at 4°C. Sections were then incubated with goat affinity-purified antibody to mouse immunoglobulin (1:50; ICN Pharmaceuticals, Aurora, OH) as secondary antibody for 30 minutes at room temperature (RT). Immunostaining was developed by the peroxidase-antiperoxidase procedure (Mouse ClonoPAP, 1:250; Covance, Gaithersburg, MD) for 60 minutes at RT (35) using 0.75 mg/ml 3,3'-diaminobenzidinesubstrate (Sigma) in 0.015% H2O2, 50 mM Tris-HCl, pH 7.6 for 10 minutes at RT. Subsequently, sections were dehydrated through a graded ethanol series (50%, 70%, 95% and 100% ethanol, 10 minutes each), cleared in xylene (3 times, 10 minutes each), and coverslipped with synthetic mounting medium (Permount, Fisher Scientific, Fair Lawn, NJ). The specificity of 1F7 was confirmed by primary antibody omission or by absorption with purified 8OHG (Cayman Chemical, Ann Arbor, MI) (4). Although 1F7 recognizes RNA-derived 8OHG as well as DNA-derived 8-hydroxydeoxyguanosine with similar binding affinities (34), we confirmed that 1F7 immunolabeling in neurons in AD is predominantly in RNA by the pretreatment with DNase or RNase (4), as well as by immunoelectron microscopy, which showed that most 8OHG is present in the endoplasmic reticulum (5). In this study, additional sections were pretreated with RNase-free DNase I (10 U/μl for 2 hours at 37°C; Roche, Mannheim, Germany) or DNase-free RNase (0.5 μg/μl for 2 hours at 37°C; Boehringer Mannheim) after proteinase-K treatment.
Relative Scale of 8OHG Immunostaining
All measurements were performed using a Q500IW-EX Image Processing and Analysis System (Leica Microsystems, Wetzlar, Germany) linked to a SONY CCD Camera (XC-75CE) (Sony, Tokyo, Japan) mounted on a Nikon MICROPHOT-FX microscope (Nikon, Tokyo, Japan). Measurements were performed in the pyramidal layer of the hippocampal subiculum, the layer III of the temporal neocortex and the Purkinje cell layer of the cerebellum. Immunoreactivity intensities were evaluated by measuring the average optical density in an area comprising the cytoplasm and nucleus, as previously described (4–7, 12, 36). To prevent possible bias during selection of the fields for analysis, fields were selected according to the following sampling criteria: For the hippocampal subiculum, we selected the pyramidal layer adjacent to the CA1 field, i.e. the prosubiculum. Because an appropriate anatomical landmark was not always identified in the temporal neocortex and cerebellum, a rule for slide scanning was introduced to select the portion of the III layer of the temporal neocortex or the Purkinje cell layer of the cerebellum. The sampling was performed by moving the microscopic field from the upper left field to right along the entire length of the section, then by moving the field vertically down to successive subjacent fields and by moving the field horizontally back to the left. When we encountered each of the target neuronal cell layers, we aligned the microscopic field so that the horizontal line of the field was parallel to each of the neuronal cell layers. Then, 3 adjacent fields (each field = 460 μm × 428 μm) were acquired for image analysis. In each field of the video camera, 5 pyramidal neurons sectioned near their equator (based on a section plane that included the nucleolus) were selected and manually outlined. The selection of the neurons within the field was performed under the same rule as the field selection within the section (upper left first). The nucleus was included for the analysis of optical density because damage to RNA was nuclear as well as cytoplasmic. Because the oxidized RNA was localized predominantly in the cytoplasm rather than nucleus in neurons (4), the area ratio of the nucleus to the cytoplasm might be a factor that influenced the neuronal optical density of 8OHG. Therefore, we selected neurons including the nucleolus so that the nucleus/cytoplasm ratio was expected to be similar among neurons of the same neuron population. The average optical density measurement was obtained for each of the 3 fields and averaged. Finally, the optical density value was corrected for background by subtracting the optical density of the white matter on the same section. All measurements were done under the same optical and light conditions as well as using an electronic shading correction to compensate for any unevenness that might be present in the illumination.
In Experiment 1, the pyramidal layer of the hippocampal subiculum was available in 27 cases of Group I; layer III of the inferior temporal/occipitotemporal gyrus was available in the other 38 cases of Group II. In Experiment 2, layer III of the temporal neocortex and the Purkinje cell layer were analyzed in 20 cases. Statistical analysis was performed with linear regression analysis and analysis of variance (ANOVA), using StatView 5.0 program (Abacus Concepts, Berkeley, CA). Fisher’s Protected Least Significant Difference (PLSD) and Student-Newman-Keuls (SNK) were used for post hoc ANOVA tests. These procedures may be complementary because Fisher’s PLSD is liberal and sensitive to a Type 1 error but SNK test is sensitive to a Type 2 error rather than a Type 1 error (37, 38).
RESULTS
Experiment 1: Neuronal RNA Oxidation in Human Brain Aging
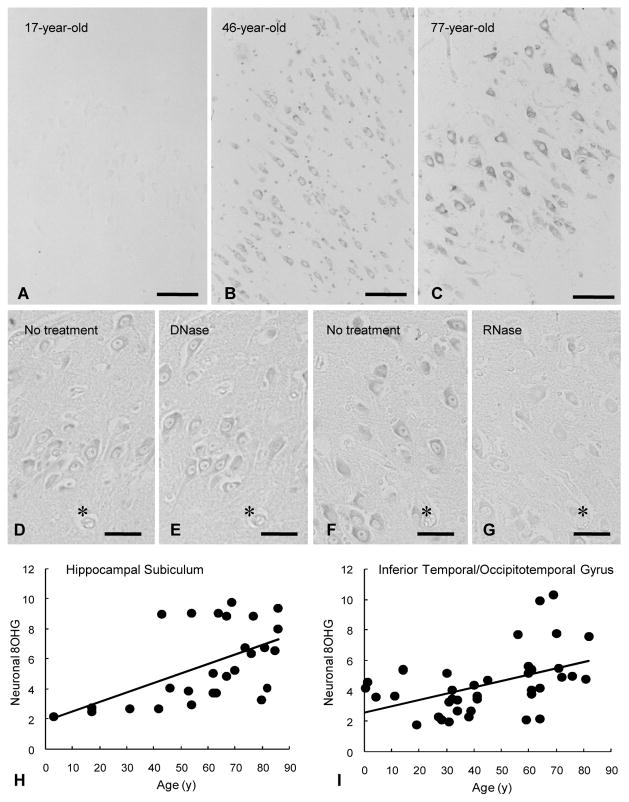
Immunoreactivity for 8OHG was virtually undetectable in cases under 40 years of age (Fig. 1A) but there was faint or moderate immunoreactivity in neuronal cytoplasm in clinically normal, presenile and senile cases (over 40 years of age) (Fig. 1B, C). To investigate whether the 1F7 antibody immunoreactivity was derived from oxidized RNA or oxidized DNA or both, we performed nuclease pre-treatment before the immunostaining. Immunoreactivity in the sections of the presenile and senile cases was diminished greatly by RNase pretreatment (Fig. 1F, G) but not by DNase pretreatment (Fig. 1D, E). We also demonstrated this in sections of AD and dementia with Lewy bodies brains (4, 6, 12). These data indicate that RNA is a major site of nucleic acid oxidation in non-demented presenile and senile individuals as well as in patients with these age-associated neurodegenerative disorders.
Figure 1.
Neuronal RNA oxidation in the aging human brain assessed in situ using 1F7 mouse monoclonal antibody against 8-hydroxyguanosine (8OHG) in hippocampi of individuals without a history of cognitive impairment. (A–C) Immunoreactivity in a young case (17 years old) (A) is virtually undetectable; neurons of a presenile case (46 year old) (B) and a senile case (77 years old) (C) show faint or modest immunoreactivity. Scale bars = 100 μm. (D–G) RNA origin of the immunoreactivity is supported by pre-treatment of sections with from an 81-year-old case with nucleases. 8OHG immunoreactivity in hippocampal sections (D, F) is almost unchanged by treatment with RNase-free DNase (E); in contrast, it is greatly diminished by treatment with DNase-free RNase (G). Panels D, E, F and G, respectively, are adjacent serial sections. Scale bars = 50 μm. Asterisk (*) indicates landmark blood vessel. (H, I) Relative 8OHG immunostaining intensity measurements using a computer-assisted image analysis and linear regression analysis show a significant correlation between age and relative levels of neuronal 8OHG (Y-axis: arbitrary units) in the hippocampal subiculum (r = 0.55, p < 0.01) (H) and in the inferior temporal/occipitotemporal gyrus (r = 0.47, p < 0.01) (I).
Relative scale measurements of the 8OHG immunoreactivity demonstrated an age-associated increase in intensity of neuronal 8OHG immunoreactivity. The relative density of neuronal 8OHG immunoreactivity increased significantly in the hippocampal subiculum and in the inferior temporal/occipitotemporal gyrus with age (Fig. 1H, I). These results cannot be explained by neuronal shrinkage because the average neuronal cell profile area was not significantly changed during aging (p = 0.76 in the hippocampal subiculum and p = 0.40 in the inferior temporal/occipitotemporal gyrus by linear regression analysis between age and neuronal cell size). Levels of relative 8OHG immunoreactivity were not related to PMI (p = 0.13 in the hippocampal subiculum and p = 0.65 in the inferior temporal/occipitotemporal gyrus by linear regression analysis). Furthermore, we found similar average values of relative 8OHG immunoreactivity in subjects who died from accident (5.1), heart failure (6.3), internal malignancy (7.2), rupture of aneurysm (3.9), and others (5.2) in the hippocampal subiculum (p = 0.45 by ANOVA); and heart failure (5.3), internal malignancy (5.0), leukemia (5.3), and others (4.6) in the inferior temporal/occipitotemporal gyrus (p = 0.95 by ANOVA).
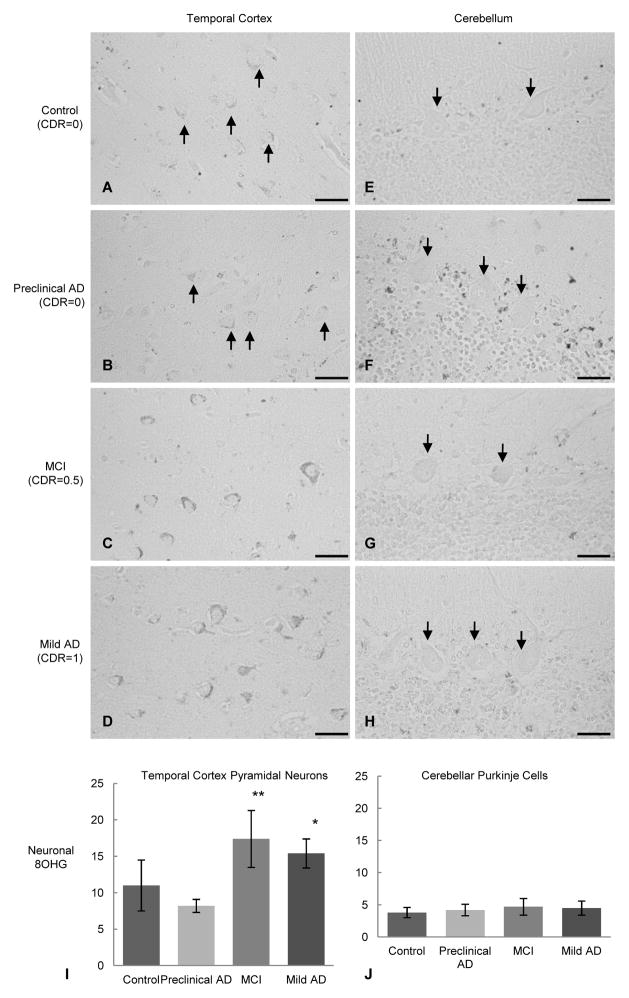
Experiment 2: Neuronal RNA Oxidation in Preclinical AD and MCI
There were no significant differences in age (p = 0.19) or PMI (p = 0.56) among the 4 categories of subjects by ANOVA (Table). In all 10 cases classified as mild AD and MCI, as well as one 95-year-old control case, neurons with marked cytoplasmic 8OHG immunoreactivity were widely distributed in the temporal cortex whereas neurons in the same region in the 4 preclinical AD and the remaining 4 control cases showed significantly lower levels of 8OHG immunoreactivity (Fig. 2A–D). In all cases, Purkinje cells of the cerebellum contained insignificant 8OHG levels (Fig. 2E–H). Relative 8OHG immunostaining intensities of temporal cortex pyramidal neurons in the mild AD and MCI groups were significantly higher than the preclinical AD and control groups (Fig. 2I). Interestingly, levels of 8OHG immunostaining intensities were higher in the MCI group than in the mild AD group, although not significantly (Fig. 2I). No significant differences among the 4 groups were detected in relative 8OHG immunostaining intensities of cerebellar Purkinje cells (Fig. 2J).
Figure 2.
Neuronal RNA oxidation in subjects with preclinical Alzheimer disease (AD), mild cognitive impairment (MCI) and mild AD (Experiment 2) assessed using the 1F7 antibody against 8-hydroxyguanosine (8OHG) in the temporal cortex and cerebellum. (A–D) Neurons in the temporal cortex of a control case (90 years old; CDR = 0) (A) and a case of preclinical AD (91 years old; CDR = 0) (B) show only faint or moderate 8OHG immunoreactivity (upward pointing arrows); neurons in the temporal cortex of a case of MCI (92 years old; CDR = 0.5) (C) and a case of mild AD (88 years old; CDR = 1) (D) show prominent immunoreactivity that is predominantly in the cytoplasm. (E–H) 8OHG immunoreactivity in the cerebellum from the same case as shown in panels A, B, C and D, respectively. In all cases, 8OHG immunoreactivity is virtually undetectable in cerebellar Purkinje cells (downward pointing arrows). Scale bars = 50 μm. (I, J) Relative 8OHG immunoreactivity measurements and ANOVA with post-hoc Fisher’s Protected Least Significant Difference (PLSD) demonstrate that there are significant increases in relative levels of 8OHG (Y-axis: arbitrary units) in pyramidal neurons of the temporal cortex (I), but not in the cerebellar Purkinje cells (J), in the MCI cases vs. controls (**p < 0.01) or preclinical AD cases (**p < 0.01), as well as in the mild AD cases vs. the controls (*p < 0.05) or the preclinical AD cases (*p < 0.05). These differences in the multiple comparisons were significant also with post-hoc Student-Newman-Keuls (SNK) test (p < 0.05 in all comparisons). MCI cases show higher levels of 8OHG than mild AD, although the differences are not significant. Data are mean ± SD. CDR= Clinical Dementia Rating.
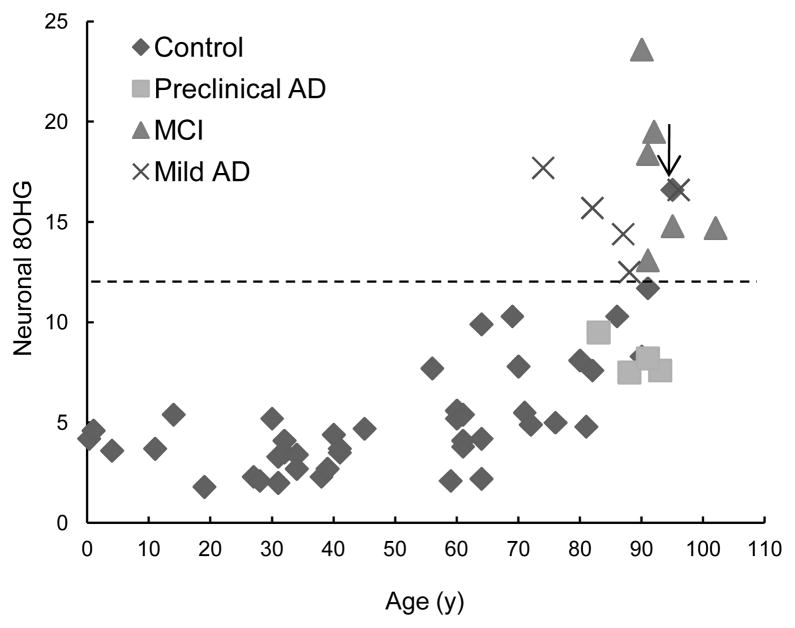
Figure 3 is a plot of relative neuronal 8OHG immunostaining intensities in the temporal cortex as a function of age in 58 cases (38 cases of the Experiment 1 [Group II] and 20 cases of the Experiment 2). This shows a distinct range of the relative neuronal 8OHG of the MCI and mild AD from the cognitively intact controls and preclinical AD. There was an exceptional control case (marked by an arrow) with a relative 8OHG level comparable to that of MCI and mild AD cases; this patient died from renal failure at the age of 95.
Figure 3.
Overview of changes in relative levels of neuronal 8-hydroxyguanosine (8OHG) immunoreactivity (Y-axis: arbitrary units) as a function of age in the temporal cortex of all subjects from Experiments 1 and 2. Subjects with mild cognitive impairment (MCI) and mild Alzheimer disease (AD) show a distinct range of relative 8OHG levels (the range above the dotted line) from that of cognitively intact subjects, including controls and preclinical AD (the range below the dotted line). Exceptionally, only a 95-year-old control case (↓) who was cognitively intact and pathologically had only diffuse plaques of amyloid β showed a relative 8OHG level within the upper range occupied by cases of MCI and mild AD.
DISCUSSION
This study demonstrates for the first time that there is an age-associated increase in oxidative damage to RNA in neuronal cells of human brain that may be an important background of neurodegeneration in the process of aging. Several recent experimental studies with aging rodents showed significant levels of RNA oxidation in liver (39), skeletal muscle (40) and brain (14, 15) in aged animals. One of them showed neuronal RNA oxidation in the hippocampus of old animals that paralleled spatial memory deficit (14), which is consistent with our present data. Although we found no significant relationship between causes of death and levels of neuronal RNA oxidation, a recent study reported significantly elevated levels of RNA oxidation in the cerebral cortex of patients with hepatic encephalopathy (41). Such an association of metabolic insufficiency with RNA oxidation in brain and a small capacity of metabolic compensation due to advanced age might explain the “exceptional” elevation in neuronal RNA oxidation observed in the 95-year-old control case who died from renal failure. One important remaining question is whether the neuronal RNA oxidation is a crucial background of age-associated neurodegeneration or is merely a phenomenon that occurs during the process of aging.
To elucidate a possible relationship of oxidized RNA with neurodegeneration at the initial phase of functional decline, we investigated subjects representing clinical and pathological stages from normality to mild dementia. As in our previous study of subjects with MCI in the hippocampus (23), there was a significant level of neuronal RNA oxidation in the temporal cortex. Selective vulnerability was evident by comparison of 8OHG immunoreactivity in the temporal cortex pyramidal neurons with that in cerebellar Purkinje cells. The neuronal vulnerability in RNA damage is consistent with the selective iron accumulation in the cerebral cortex neurons but not in the cerebellar Purkinje cells in MCI brains, while some glial cells contain considerable level of iron in the cerebellum (42). Because abnormalities in mitochondria and iron homeostasis likely contribute to damage cellular RNA as a source and an amplifier of reactive oxygen species (3), further investigations on mitochondrial dysfunction in MCI may provide a particular key in elucidating the pathogenesis of the onset of cognitive decline.
This study extends the categories of subjects to preclinical cases who exhibit full features of AD brain pathology but no or few signs of cognitive decline. We found no significant difference in levels of neuronal RNA oxidation in preclinical cases compared to age-matched controls; this result is consistent with previous results of no significant changes in levels of lipid peroxidation and oxidative protein modification in the cerebral neocortex of preclinical AD (25–27). However, these observations are inconsistent with several previous findings, such as elevation of iron content in brains of preclinical AD (42), elevation of a lipid peroxidation product, F2-isoprostane, in the cerebrospinal fluid of preclinical familial AD (43), and temporal primacy of neuronal RNA oxidation to amyloid β (Aβ) deposition in brains in an aging series of cases with Down syndrome (36). Nevertheless, the present data support early involvement of oxidative stress in the transition of normal to cognitive impairment. The National Institute on Aging and the Alzheimer’s Association workgroup now accept that, for defined purposes, preclinical AD consisting of approximately 40% of non-demented elderly at the mean age of 84 years (44) is a stage of AD progression (45). Indeed, preclinical AD might represent a compensatory period in which the brain is capable of maintaining cellular vitality and minimizing oxidative stress and consequently preserving cognitive function. It is speculated that certain coping mechanisms against formation and/or propagation of free radicals are still intact at the preclinical phase in the cognitively normal elderly; such compensatory mechanism might be compromised even in young adulthood in cases of preclinical familial AD and Down syndrome due to their genetic basis (6, 36).
We previously reported the relationship between levels of extra- and intra-neuronal Aβ burden and neuronal oxidative damage to RNA. The results were contrary to the common notion that levels of Aβ burden should parallel each stage of neurodegeneration. Indeed, there was an inverse relationship between levels of extra-neuronal Aβ deposition and neuronal oxidative damage to RNA in subjects with sporadic AD (5), familial AD (6), and Down syndrome (36), but no significant relationship in controls (5). Recently, we showed that there was also an inverse relationship between the levels of intra-neuronal Aβ42 immunostaining intensity and neuronal oxidative damage to RNA in AD (7). Moreover, we found more prominent oxidative RNA damage in neurons without NFTs or granulovacuolar degeneration vs. neurons with NFTs or granulovacuolar degeneration in AD (5, 46). These unexpected observations enabled us to hypothesize that the development of AD-related pathology might represent a compensatory response to neuronal oxidative insults (7, 46, 47). In this context it would be very interesting to learn whether there is a specific relationship between Aβ, NFTs, or granulovacuolar degeneration burden and neuronal oxidative damage in the transitional stages from normal aging to the onset of AD.
Recent studies have indicated that RNA oxidation has detrimental effects on cellular function whether the damaged RNA species are coding for proteins (messenger RNA) or performing translation (ribosomal RNA and transfer RNA) (8, 10, 22, 48, 49). Indeed, levels of neuronal RNA oxidation parallel spatial memory deficits in aging animals, and age-associated oxidative RNA damage and memory deficits can be reduced by antioxidants or mitochondrial metabolites (14). Therefore, oxidative RNA damage in vulnerable neurons is a promising candidate of targets for prevention and treatment of AD from prodromal to early stages of the disease.
In summary, the present results indicate that 1) a modest level of oxidative RNA damage in cerebral neurons occurs during the process of aging, and 2) a prominent level of oxidative RNA damage in vulnerable neurons corresponds with the earliest stage of cognitive decline in the transition from cognitively normal aging to AD. Further investigations aimed at the cellular consequences of oxidative RNA damage and compensatory mechanisms might provide insights into the process of aging and the pathogenesis of age-associated neurodegeneration. Such approaches may provide novel strategies for prevention and treatment of AD.
Acknowledgments
Sources of Support: Work in the authors’ laboratories is supported by funding from the Japan Society for the Promotion of Science (Grant-in-Aid for Scientific Research (C) 20591387 to AN). The authors thank John C. Morris, MD, and the Washington University Alzheimer Disease Research Center, funded by National Institute on Aging grants P50 AG05681 and P01 AG03991, for the clinical characterization of cases contributed to this study.
References
- 1.Coyle JT, Puttfarcken P. Oxidative stress, glutamate, and neurodegenerative disorders. Science. 1993;262:689–95. doi: 10.1126/science.7901908. [DOI] [PubMed] [Google Scholar]
- 2.Mattson MP, Chan SL, Duan W. Modification of brain aging and neurodegenerative disorders by genes, diet, and behavior. Physiol Rev. 2002;82:637–72. doi: 10.1152/physrev.00004.2002. [DOI] [PubMed] [Google Scholar]
- 3.Nunomura A, Hofer T, Moreira PI, et al. RNA oxidation in Alzheimer disease and related neurodegenerative disorders. Acta Neuropathol. 2009;118:151–66. doi: 10.1007/s00401-009-0508-1. [DOI] [PubMed] [Google Scholar]
- 4.Nunomura A, Perry G, Pappolla MA, et al. RNA oxidation is a prominent feature of vulnerable neurons in Alzheimer's disease. J Neurosci. 1999;19:1959–64. doi: 10.1523/JNEUROSCI.19-06-01959.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nunomura A, Perry G, Aliev G, et al. Oxidative damage is the earliest event in Alzheimer disease. J Neuropathol Exp Neurol. 2001;60:759–67. doi: 10.1093/jnen/60.8.759. [DOI] [PubMed] [Google Scholar]
- 6.Nunomura A, Chiba S, Lippa CF, et al. Neuronal RNA oxidation is a prominent feature of familial Alzheimer's disease. Neurobiol Dis. 2004;17:108–13. doi: 10.1016/j.nbd.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 7.Nunomura A, Tamaoki T, Tanaka K, et al. Intraneuronal amyloid β accumulation and oxidative damage to nucleic acids in Alzheimer disease. Neurobiol Dis. 2010;37:731–7. doi: 10.1016/j.nbd.2009.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shan X, Tashiro H, Lin CL. The identification and characterization of oxidized RNAs in Alzheimer's disease. J Neurosci. 2003;23:4913–21. doi: 10.1523/JNEUROSCI.23-12-04913.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shan X, Lin CL. Quantification of oxidized RNAs in Alzheimer's disease. Neurobiol Aging. 2006;27:657–62. doi: 10.1016/j.neurobiolaging.2005.03.022. [DOI] [PubMed] [Google Scholar]
- 10.Honda K, Smith MA, Zhu X, et al. Ribosomal RNA in Alzheimer disease is oxidized by bound redox-active iron. J Biol Chem. 2005;280:20978–86. doi: 10.1074/jbc.M500526200. [DOI] [PubMed] [Google Scholar]
- 11.Zhang J, Perry G, Smith MA, et al. Parkinson's disease is associated with oxidative damage to cytoplasmic DNA and RNA in substantia nigra neurons. Am J Pathol. 1999;154:1423–9. doi: 10.1016/S0002-9440(10)65396-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nunomura A, Chiba S, Kosaka K, et al. Neuronal RNA oxidation is a prominent feature of dementia with Lewy bodies. Neuroreport. 2002;13:2035–9. doi: 10.1097/00001756-200211150-00009. [DOI] [PubMed] [Google Scholar]
- 13.Chang Y, Kong Q, Shan X, et al. Messenger RNA oxidation occurs early in disease pathogenesis and promotes motor neuron degeneration in ALS. PLoS ONE. 2008;3:e2849. doi: 10.1371/journal.pone.0002849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liu J, Head E, Gharib AM, et al. Memory loss in old rats is associated with brain mitochondrial decay and RNA/DNA oxidation; partial reversal by feeding acetyl-L-carnitine and/or R-α-lipoic acid. Proc Natl Acad Sci U S A. 2002;99:2356–61. doi: 10.1073/pnas.261709299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cui L, Hofer T, Rani A, et al. Comparison of lifelong and late life exercise on oxidative stress in the cerebellum. Neurobiol Aging. 2009;30:903–9. doi: 10.1016/j.neurobiolaging.2007.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mecocci P. Oxidative stress in mild cognitive impairment and Alzheimer disease; a continuum. J Alzheimers Dis. 2004;6:159–63. doi: 10.3233/jad-2004-6207. [DOI] [PubMed] [Google Scholar]
- 17.Keller JN, Schmitt FA, Scheff SW, et al. Evidence of increased oxidative damage in subjects with mild cognitive impairment. Neurology. 2005;64:1152–6. doi: 10.1212/01.WNL.0000156156.13641.BA. [DOI] [PubMed] [Google Scholar]
- 18.Markesbery WR, Kryscio RJ, Lovell MA, et al. Lipid peroxidation is an early event in the brain in amnestic mild cognitive impairment. Ann Neurol. 2005;58:730–5. doi: 10.1002/ana.20629. [DOI] [PubMed] [Google Scholar]
- 19.Butterfield DA, Poon HF, St Clair D, et al. Redox proteomics identification of oxidatively modified hippocampal proteins in mild cognitive impairment; insights into the development of Alzheimer's disease. Neurobiol Dis. 2006;22:223–32. doi: 10.1016/j.nbd.2005.11.002. [DOI] [PubMed] [Google Scholar]
- 20.Butterfield DA, Reed TT, Perluigi M, et al. Elevated levels of 3-nitrotyrosine in brain from subjects with amnestic mild cognitive impairment; implications for the role of nitration in the progression of Alzheimer's disease. Brain Res. 2007;1148:243–8. doi: 10.1016/j.brainres.2007.02.084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang J, Markesbery WR, Lovell MA. Increased oxidative damage in nuclear and mitochondrial DNA in mild cognitive impairment. J Neurochem. 2006;96:825–32. doi: 10.1111/j.1471-4159.2005.03615.x. [DOI] [PubMed] [Google Scholar]
- 22.Ding Q, Markesbery WR, Chen Q, et al. Ribosome dysfunction is an early event in Alzheimer's disease. J Neurosci. 2005;25:9171–5. doi: 10.1523/JNEUROSCI.3040-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lovell MA, Markesbery WR. Oxidatively modified RNA in mild cognitive impairment. Neurobiol Dis. 2008;29:169–75. doi: 10.1016/j.nbd.2007.07.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Terni B, Boada J, Portero-Otin M, et al. Mitochondrial ATP-synthase in the entorhinal cortex is a target of oxidative stress at stages I/II of Alzheimer's disease pathology. Brain Pathol. 2010;20:222–33. doi: 10.1111/j.1750-3639.2009.00266.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bradley MA, Markesbery WR, Lovell MA. Increased levels of 4-hydroxynonenal and acrolein in the brain in preclinical Alzheimer disease. Free Radic Biol Med. 2010;48:1570–6. doi: 10.1016/j.freeradbiomed.2010.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Aluise CD, Robinson RA, Beckett TL, et al. Preclinical Alzheimer disease; brain oxidative stress, Aβ peptide and proteomics. Neurobiol Dis. 2010;39:221–8. doi: 10.1016/j.nbd.2010.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Aluise CD, Robinson RA, Cai J, et al. Redox proteomics analysis of brains from subjects with amnestic mild cognitive impairment compared to brains from subjects with preclinical Alzheimer's disease; insights into memory loss in MCI. J Alzheimers Dis. 2011;23:257–69. doi: 10.3233/JAD-2010-101083. [DOI] [PubMed] [Google Scholar]
- 28.Morris JC. The Clinical Dementia Rating (CDR); current version and scoring rules. Neurology. 1993;43:2412–4. doi: 10.1212/wnl.43.11.2412-a. [DOI] [PubMed] [Google Scholar]
- 29.Price JL, Morris JC. Tangles and plaques in nondemented aging and "preclinical" Alzheimer's disease. Ann Neurol. 1999;45:358–68. doi: 10.1002/1531-8249(199903)45:3<358::aid-ana12>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- 30.Goldman WP, Price JL, Storandt M, et al. Absence of cognitive impairment or decline in preclinical Alzheimer's disease. Neurology. 2001;56:361–7. doi: 10.1212/wnl.56.3.361. [DOI] [PubMed] [Google Scholar]
- 31.Mirra SS, Heyman A, McKeel D, et al. The Consortium to Establish a Registry for Alzheimer's Disease (CERAD). Part II. Standardization of the neuropathologic assessment of Alzheimer's disease. Neurology. 1991;41:479–86. doi: 10.1212/wnl.41.4.479. [DOI] [PubMed] [Google Scholar]
- 32.Morris JC, Roe CM, Grant EA, et al. Pittsburgh compound B imaging and prediction of progression from cognitive normality to symptomatic Alzheimer disease. Arch Neurol. 2009;66:1469–75. doi: 10.1001/archneurol.2009.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chao LL, Mueller SG, Buckley ST, et al. Evidence of neurodegeneration in brains of older adults who do not yet fulfill MCI criteria. Neurobiol Aging. 2010;31:368–77. doi: 10.1016/j.neurobiolaging.2008.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yin B, Whyatt RM, Perera FP, et al. Determination of 8-hydroxydeoxyguanosine by an immunoaffinity chromatography-monoclonal antibody-based ELISA. Free Radic Biol Med. 1995;18:1023–32. doi: 10.1016/0891-5849(95)00003-g. [DOI] [PubMed] [Google Scholar]
- 35.Sternberger LA. Immunocytochemistry. New York: Wiley; 1986. [Google Scholar]
- 36.Nunomura A, Perry G, Pappolla MA, et al. Neuronal oxidative stress precedes amyloid-β deposition in Down syndrome. J Neuropathol Exp Neurol. 2000;59:1011–7. doi: 10.1093/jnen/59.11.1011. [DOI] [PubMed] [Google Scholar]
- 37.Armstrong RA, Slade SV, Eperjesi F. An introduction to analysis of variance (ANOVA) with special reference to data from clinical experiments in optometry. Ophthalmic Physiol Opt. 2000;20:235–41. [PubMed] [Google Scholar]
- 38.Hilton A, Armstrong RA. Stat Note 6: post hoc ANOVA tests. Microbiologist. 2006;7:34–36. [Google Scholar]
- 39.Seo AY, Hofer T, Sung B, et al. Hepatic oxidative stress during aging; effects of 8% long-term calorie restriction and lifelong exercise. Antioxid Redox Signal. 2006;8:529–38. doi: 10.1089/ars.2006.8.529. [DOI] [PubMed] [Google Scholar]
- 40.Hofer T, Marzetti E, Xu J, et al. Increased iron content and RNA oxidative damage in skeletal muscle with aging and disuse atrophy. Exp Gerontol. 2008;43:563–70. doi: 10.1016/j.exger.2008.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gorg B, Qvartskhava N, Bidmon HJ, et al. Oxidative stress markers in the brain of patients with cirrhosis and hepatic encephalopathy. Hepatology. 2010;52:256–65. doi: 10.1002/hep.23656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Smith MA, Zhu X, Tabaton M, et al. Increased iron and free radical generation in preclinical Alzheimer disease and mild cognitive impairment. J Alzheimers Dis. 2010;19:363–72. doi: 10.3233/JAD-2010-1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ringman JM, Younkin SG, Pratico D, et al. Biochemical markers in persons with preclinical familial Alzheimer disease. Neurology. 2008;71:85–92. doi: 10.1212/01.wnl.0000303973.71803.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Price JL, McKeel DW, Jr, Buckles VD, et al. Neuropathology of nondemented aging; presumptive evidence for preclinical Alzheimer disease. Neurobiol Aging. 2009;30:1026–36. doi: 10.1016/j.neurobiolaging.2009.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sperling RA, Aisen PS, Beckett LA, et al. Toward defining the preclinical stages of Alzheimer's disease; recommendations from the National Institute on Aging-Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimers Dement. 2011;7:280–92. doi: 10.1016/j.jalz.2011.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Castellani RJ, Gupta Y, Sheng B, et al. A novel origin for granulovacuolar degeneration in aging and Alzheimer's disease: parallels to stress granules. Lab Invest. 2011;91:1777–86. doi: 10.1038/labinvest.2011.149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Nunomura A, Castellani RJ, Zhu X, et al. Involvement of oxidative stress in Alzheimer disease. J Neuropathol Exp Neurol. 2006;65:631–41. doi: 10.1097/01.jnen.0000228136.58062.bf. [DOI] [PubMed] [Google Scholar]
- 48.Shan X, Chang Y, Lin CL. Messenger RNA oxidation is an early event preceding cell death and causes reduced protein expression. FASEB J. 2007;21:2753–64. doi: 10.1096/fj.07-8200com. [DOI] [PubMed] [Google Scholar]
- 49.Tanaka M, Chock PB, Stadtman ER. Oxidized messenger RNA induces translation errors. Proc Natl Acad Sci U S A. 2007;104:66–71. doi: 10.1073/pnas.0609737104. [DOI] [PMC free article] [PubMed] [Google Scholar]