Abstract
Objective
Anxiety disorders are prominent in chronic lung disease; lung transplant recipients may therefore also be at high risk for these disorders. We sought to provide the first prospective data on rates and risk factors for anxiety disorders as well as depressive disorders during the first two years after transplantation.
Method
178 lung recipients, and a comparison group (126 heart recipients), received psychosocial and Structured Clinical Interview for DSM-IV assessments at 2-, 7-, 12-, 18-, and 24-months posttransplant. Survival analysis determined onset rates and risk factors.
Results
The panic disorder rate was higher (p<.05) in lung than heart recipients (18% v. 8%). Lung and heart recipients did not differ on rates of transplant-related post-traumatic stress disorder (15% v. 14%), generalized anxiety disorder (4% v. 3%), or major depression (30% v. 26%). Risk factors for disorders included pretransplant psychiatric history, female gender, longer wait for transplant, and early posttransplant health problems and psychosocial characteristics (e.g., poorer caregiver support, use of avoidant coping).
Conclusions
Heightened vigilance for panic disorder in lung recipients and major depression in all cardiothoracic recipients is warranted. Strategies to prevent psychiatric disorder should target recipients based not only on pretransplant characteristics but early posttransplant characteristics as well.
Keywords: lung transplantation, anxiety, depression, risk factors
INTRODUCTION
Lung transplantation has become an accepted therapeutic strategy for a variety of end-stage lung diseases. In comparison to relatively stable rates of kidney, liver, and heart transplantation in the last decade, the rate of lung transplantation has almost doubled in the United States and worldwide.[1,2] Survival time has also improved, with 1-year survival now at 79%–83% and 3-year survival at 63%–66%.[1,2] Nevertheless, survival time remains poorer than for other types of solid organ transplantation where, for example, 3-year survival is 79%–95%.[2] Because the lung is in constant contact with the external environment, lung recipients are at greater risk than other solid organ recipients for posttransplant morbidities including infection, acute allograft rejection, and secondary illnesses.[3,4] Thus, despite improved physical functioning and general quality of life with lung transplantation,[5–11] the prevalence of posttransplant physical symptoms and physical functional impairments remains high even well after the recovery period.[8,12–16]
In the context of these stressors, one might expect that psychiatric morbidity in lung recipients would be prominent. A growing literature has documented elevated global psychiatric symptom and distress levels in these patients.[8,11,16–21] However, beyond small case series,[22–25] there remains no information on rates, clinical characteristics, or risk factors for diagnosable psychiatric disorders in this population. This is an important omission since—as demonstrated in other forms of organ transplantation—clinically significant psychiatric morbidity is prevalent[17,26–29] and can predict negative longer-term health outcomes.[27–30]
Anxiety disorders, and panic disorder in particular, appear to be uniquely associated with chronic lung disease, based on evidence from (nontransplanted) samples.[31–35] Given lung recipients’ own history of lung disease plus their enduring physical symptoms and functional impairments posttransplant, they may be at heightened risk for anxiety disorders posttransplant, relative to risk in other transplant populations. In contrast, depressive disorders are relatively common in many types of chronic disease patients, including transplant recipients.[17,26,36–38] Thus, lung recipients—while at risk for depression due to their exposure to posttransplant stressors—may not have a vulnerability to depression that is greater than that possessed by other organ recipients.
The goal of the present report was to prospectively examine onset rates, clinical characteristics, and risk factors for DSM-IV[39] anxiety and depressive disorders during the first two years after lung transplantation in a relatively large clinical epidemiologic sample. We included a comparison group of heart transplant recipients. We judged that this would constitute the most appropriate comparison group because heart recipients are the only other major group of thoracic transplant patients, both groups generally receive care from the same or overlapping teams posttransplant, and they are seen at similar intervals for follow-up care posttransplant.
Our study, therefore, prospectively examined, first, whether lung recipients differed from the comparison group in rates of psychiatric disorder onset. Second, we examined these groups in terms of the disorders’ clinical characteristics, including episode durations, treatment seeking and medications received, and patterns of comorbidity between the disorders. Third, we examined pretransplant and early posttransplant risk factors for disorder. Potential risk factors were selected for both conceptual and empirical reasons. Conceptual models of the chronic stress process, most notably the vulnerability or diathesis-stress model,[40–43] posit that individuals’ mental health in the face of stressors such as chronic disease and its treatment will be influenced by their background sociodemographic and medical characteristics, their health in the aftermath of treatment, and their psychosocial resources and liabilities (particularly in areas such as social supports and coping). We thus selected factors to represent these domains. Moreover, the factors we selected either are known to increase risk for psychiatric disorder in the general population or were identified in an International Society of Heart and Lung Transplantation (ISHLT) workgroup report[5] as potentially important for mental health outcomes in cardiothoracic transplant populations.
METHODS
Respondents
Respondents were adults (aged ≥18) receiving their first lung or heart transplant between November, 1999 and August, 2004 in the Cardiothoracic Transplantation (CT) Program, University of Pittsburgh Medical Center. The eligibility criterion was survival beyond the posttransplant surgical recovery period (defined as the first 6 weeks after surgery). Of 327 eligible transplant recipients, 23 refused to participate (7.0%). The 304 recipients enrolled (178 lung, 126 heart recipients) did not differ from refusers on type of transplant or demographic characteristics (age, gender, race/ethnicity, education, marital status).
During the study period, 30 patients (9.9%) withdrew consent and 35 patients died (11.5%). As shown in Table 1, lung recipients were no more likely to withdraw than heart recipients, but they were more likely to be lost due to death. This difference is addressed in study analyses. There was no reliable association between reason for loss to follow-up and any variable assessed in the study.
Table 1.
Study participation, background and transplant-related characteristics of lung and heart recipients.
| Group comparison | ||||
|---|---|---|---|---|
| Characteristic | Lung Recipients |
Heart Recipients |
test statistica |
p level |
| Study participation | ||||
| Number enrolled | 178 | 126 | ||
| Lost to follow-up due to withdrawal of consent | 10.7 | 8.7 | 0.32 | .576 |
| Lost to follow-up due to death | 17.9 | 2.4 | 16.12b | <.001 |
| Mode of interview, % at clinic, % at home, % by phone | ||||
| 2-month interview | 70.9, 9.5, 19.6 | 74.8, 7.6, 17.6 | 0.57 | .750 |
| 7-month interview | 53.4, 9.3, 37.3 | 62.1, 6.0, 31.9 | 2.36 | .308 |
| 12-month interview | 50.3, 9.5, 40.1 | 58.6, 7.2, 34.2 | 1.78 | .411 |
| 18-month interview | 43.0, 8.4, 48.6 | 48.3, 5.7, 46.0 | 0.84 | .660 |
| 24-month interview | 28.7, 4.9, 66.4 | 34.3, 10.2, 55.6 | 3.82 | .148 |
| Background | ||||
| Age, M (SD) | 50.7 (11.7) | 52.2 (12.3) | 1.03 | .306 |
| Gender, % male | 52.2 | 68.3 | 7.81 | .005 |
| Race/ethnicity, % European American | 94.9 | 85.7 | 7.77 | .005 |
| Education, % ≤ high school | 48.9 | 48.4 | 0.01 | .936 |
| Occupation, % nonprofessional | 54.8 | 62.7 | 1.89 | .170 |
| Household income below U.S. poverty level,[63] % yes | 13.6 | 25.4 | 6.72 | .010 |
| Marital status, % married | 70.8 | 75.4 | 0.79 | .374 |
| Lifetime psychiatric history | ||||
| Panic disorder, % yes | 18.2 | 12.5 | 1.72 | .189 |
| GAD, % yes | 13.6 | 38.3 | 0.41 | .523 |
| MDD, % yes | 42.0 | 11.7 | 0.25 | .619 |
| Any of these disorders, % yes | 50.0 | 47.1 | 0.24 | .624 |
| Transplant-related | ||||
| Indication for transplant, % lung recipients | ||||
| COPD/emphysema | 35.4 | |||
| Idiopathic pulmonary fibrosis | 21.3 | |||
| Cystic fibrosis | 16.3 | |||
| Other | 27.0 | |||
| Type of lung transplant, % lung recipients | ||||
| Single | 53.4 | |||
| Bilateral | 46.6 | |||
| Indication for transplant, % heart recipients | ||||
| Coronary artery disease | 42.3 | |||
| Myopathy | 41.3 | |||
| Other | 16.6 | |||
| Length of hospitalization post-transplant % | ||||
| ≤ 14 days | 34.8 | 42.5 | 7.73 | .052 |
| 15–21 days | 19.1 | 23.8 | ||
| 22–28 days | 15.2 | 12.7 | ||
| ≥ 29 days | 30.9 | 18.3 | ||
| Functional impairment at 2 mos. posttransplant | ||||
| SF-36 physical functioning (0=low, 100=high), M (SD) | 52.9 (25.6) | 55.7 (25.1) | 0.94 | .349 |
| Chronic dyspnea, (1=extreme, 10=none), M (SD) | 7.0 (2.1) | 7.7 (2.1) | 2.80 | .005 |
χ2 tests (categorical variables) or t tests (continuous variables).
calculated with continuity correction due to small expected values in some cells.
Abbreviations: GAD, generalized anxiety disorder; MDD, major depressive disorder.
Procedure
The University of Pittsburgh Institutional Review Board approved the study. Respondents provided written informed consent. They participated in individual 90- to 120-minute interviews on three occasions during the first year post-transplant (2, 7, 12 months) and two occasions thereafter (18, 24 months). Interviews were more frequent during the first year in order to better capture a period characterized by marked changes and readjustments related to the transplant.[44] The semi-structured interviews were conducted by trained clinicians with advanced degrees in behavioral medicine fields. Interrater reliability on semi-structured instruments (e.g., the Structured Clinical Interview for DSM-IV, SCID[45]) was maintained at an intraclass correlation of ≥0.90.
When possible, interviews coincided with CT Program outpatient visits. (Per Program protocol, lung and heart recipients returned for follow-up visits every 1–2 months during the first year and every 2–3 months during the second year posttransplant.) Otherwise, interviews were conducted in respondents’ homes or by telephone. There were no significant differences by interview mode for lung vs. heart recipients (see Table 1), neither was interview mode associated with any other study variable. Data on transplant-related characteristics (e.g., indication for transplant) were obtained from medical records.
Instruments
Psychiatric status posttransplant
We examined specific DSM-IV anxiety and depressive disorders, including panic disorder, generalized anxiety disorder (GAD), posttraumatic stress disorder related to the transplant experience (PTSD-T), major depressive disorder (MDD), and adjustment disorder with anxiety and/or depressed mood. Disorders were assessed with the SCID. The 2-month interview assessed disorders from the time of transplant; subsequent interviews covered the period since last assessment.
We adopted a conservative approach to diagnosis, given patients’ medical status. Thus, in individual case review, we assigned diagnoses based primarily on affective/cognitive symptoms; somatic symptoms were used to support the diagnosis only when these symptoms were judged to have been severe, disproportionate to the medical illness or any medications patients were receiving and temporally related to the affective/cognitive symptoms.[46,47]
Potential risk factors for posttransplant psychiatric disorder
Three domains, comprising a total of 17 factors, were assessed at the initial interview. Some factors were single items (e.g., demographic characteristics). Others were assessed by scales with established psychometric properties. For the scales, Table 2 provides details regarding total number of items assessed, time frame, scale scoring, internal consistency reliability for the present sample, and sources for information on psychometric properties.
Table 2.
Patient-report scales used to assess potential risk factors
| Potential risk factor | Instrument | No. of items used; time frame |
Scale endpoints | Cronbach’s α, current sample |
Sources for psychometric properties |
|---|---|---|---|---|---|
| Posttransplant health-related characteristics | |||||
| Physical functional status | RAND Medical Outcomes Study Short Form 36 (SF-36) | 10; Past 4 weeks | 0 = poor, 100 = excellent | .89 | Ware et al.[48] |
| Shortness of breath | Dyspnea Component, Chronic Respiratory Disease Questionnaire | 5; Past 2 weeks | 1 = extreme dyspnea, 10 = no dyspnea | .90 | Guyatt et al.,[49] Schunemann et al. [50] |
| Posttransplant psychosocial characteristics | |||||
| Social support from family caregiver | Patient-Caregiver Support Scale | 20; Current time | 1 = low | .92 | Spanier[51]; Pearlin & Schooler[52] Dew [53] |
| Social support from friends | Friend Support Scale | 12; Current time | 1 = low | .89 | Moos [50] |
| Support from religious faith | Faith items | 4; Current time | 1 = little support from faith, 4 = high support from faith | .80 | King & Hunt[57] |
| Coping with health problems | Brief COPE | 28a; Focus on a recent problem | 1 = did not use, 4 = used strategy a lot | Carver [58] Carver et al. [59] | |
| Active coping | 5 | .75 | |||
| Support seeking/expression of emotions coping | 7 | .69 | |||
| Avoidant coping | 6 | .62 | |||
| Acceptance coping | 8 | .70 | |||
2 items reflecting self-blame coping were not included in Carver et al.’s original work with this scale and were not examined in the present study.
Domain 1: Pretransplant characteristics
In addition to demographic characteristics (gender, age, race/ethnicity, education, income), we determined whether respondents had a pretransplant lifetime history of panic disorder, GAD, or MDD using the SCID at the 2-month interview. Duration of wait for the transplant was extracted from patients’ medical records.
Domain 2: Posttransplant health-related characteristics
We assessed patients’ health status during the first 2 months of recovery with three variables. As shown in Table 2, we assessed physical functional status and level of chronic dyspnea during the patient interviews. In addition, patients’ medical records were reviewed to determine duration of posttransplant hospitalization.
Domain 3: Posttransplant psychosocial characteristics
Two types of characteristics, interpersonal resources and intrapersonal resources, were considered. With respect to interpersonal resources, as shown in Table 2, we assessed the respondent’s perception of support (both emotion and practical) from their primary family caregiver and from their friends. These measures had skewed distributions; scores were dichotomized to identify respondents with the poorest support (lower third of the distribution) relative to remaining respondents.
With respect to intrapersonal resources, five measures were administered. First, we assessed the extent to which respondents’ faith helped them in their daily life (Table 2). This measure was skewed; we dichotomized it to distinguish those with a low degree of this resource (lower third of the distribution) from remaining respondents. In addition, we assessed coping with four scales derived from the Brief COPE.[58] Respondents focused on what they felt was their most serious recent health problem and rated their use of various coping strategies. We created four composite variables from this measure based on results we obtained from a principal components analysis; the variables were consistent with the higher order coping factors identified by Carver et al.[59] Active coping reflected plans or behavior to actively deal with the problem. The support-seeking/expression of emotions factor reflected attempts to turn to others for support and express one’s feelings about the problem. Avoidant coping reflected attempts to shun or deny the problem. Acceptance coping referred to accepting or trying make the best of the situation. These four coping measures were skewed. However, because no single approach to coping is maladaptive for every health problem,[60] we could not use specific cut points on the scales to identify “poor” coping. We thus dichotomized each at its median for use in analyses.
Statistical Analysis
Lung recipients’ background and clinical characteristics were examined relative to the comparison group with χ2 tests (categorical variables) and t tests (continuous variables). Survival analysis, using a life-table approach,[61] was used to determine the cumulative posttransplant onset rates of the assessed psychiatric disorders. We used life-table rather than Kaplan-Meier methods because, by the design of this clinical epidemiologic study, individuals were retrospectively reporting on episodes occurring at any time since either transplant (at the 2-month interview) or since the previous assessment (at all subsequent interviews). The analysis considered whether disorder onsets occurred during each interval between interviews.
We used descriptive approaches (e.g., box plots) to examine disorders’ clinical characteristics (e.g., episode duration, comorbidity). Cox proportional hazards models were fit in order to evaluate the independent predictive effects of potential risk factors on onset of psychiatric disorder. The proportionality assumption was evaluated before fitting the models.[62] We maintained a total respondent-to-total predictor variable ratio exceeding the recommended range of 10:1 to 15:1.[62]
RESULTS
Sample characteristics
Table 1 displays background and transplant-related characteristics of the lung recipients relative to the comparison group. The groups were similar to the respective U.S. populations of lung and heart recipients transplanted during the same time period on distributions of gender, age, ethnicity, and indications for transplantation.[64] The significant between-group differences on several variables are also consistent with national data, and we included these variables in analyses as possible contributors to between-group differences on study outcomes. Lung recipients were hospitalized longer posttransplant and they reported more chronic dyspnea at 2 months posttransplant. However, the groups were similar on overall physical functional status.
Onset rates and temporal pattern of psychiatric disorders posttransplant
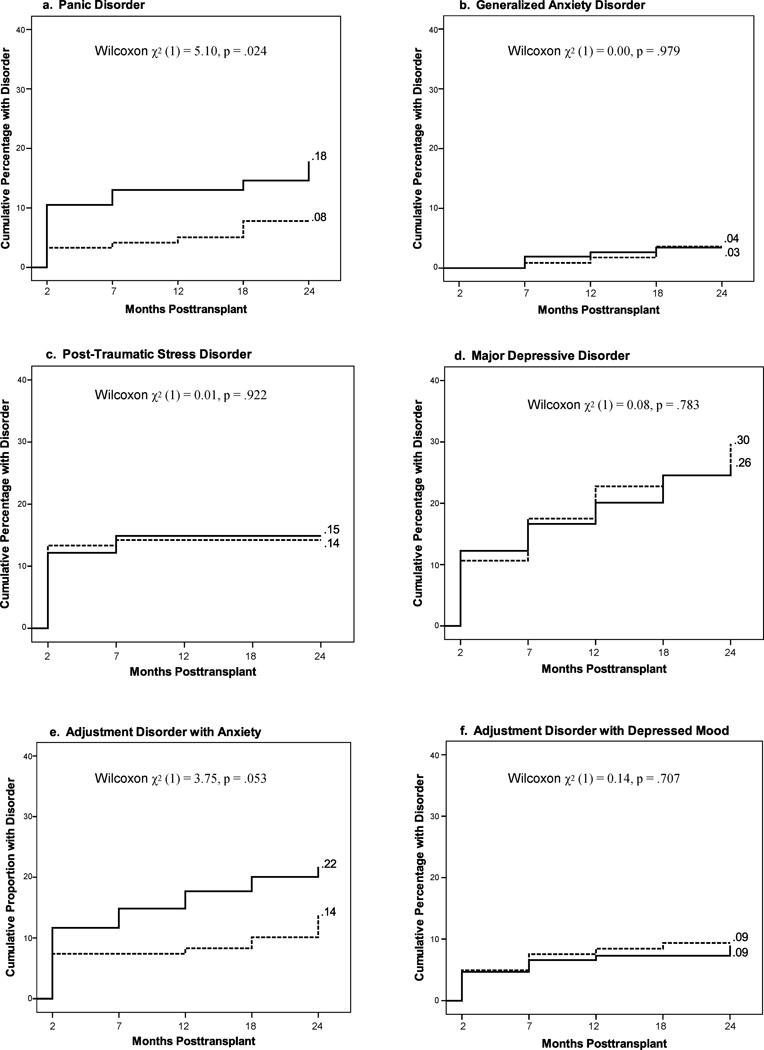
Results of survival analyses of the cumulative rates of posttransplant onset of psychiatric disorders are shown in Figure 1. Lung recipients had a significantly higher rate of panic disorder by two years posttransplant than heart recipients (18% v. 8%; p=.028; Figure 1a). Lung recipients were also more likely to experience adjustment disorder with anxiety (Figure 1e). Other disorders’ cumulative onset rates were similar across groups (Figure 1b–1d; 1f). The group differences on panic disorder and adjustment disorder with anxiety largely accounted for the additional finding that the cumulative rate of any disorder (vs. none) was higher in lung recipients (58%) than heart recipients (47%) by two years posttransplant (Wilcoxon χ2(df=1)=5.12, p=.036; survival plot not shown).
Figure 1.
Cumulative incidence of psychiatric disorder during the first two years posttransplant in lung vs. heart recipients (solid line denotes lung recipients; dotted line denotes heart recipients).
Across both groups, some disorders were more common than others. For example, MDD occurred in 26%–30% of recipients while GAD occurred in 3%–4%. Figure 1 also shows that the various disorders had different temporal patterns of onset. All PTSD-T onsets occurred in the early months posttransplant. Panic disorder, GAD, and adjustment disorder onsets occurred primarily in the first year. In contrast, MDD onsets occurred more gradually across the two-year period.
To address the possibility that the differential death rates between lung and heart recipients influenced the findings in Figure 1, we repeated the survival analyses including only recipients who remained alive throughout the study period. The pattern of results did not change, either for disorder rates, the shape of the incidence curves, or differences between study groups.
The data in Figure 1 indicate onsets posttransplant, but not whether these were first lifetime onsets. Because we also determined pretransplant lifetime history of panic disorder, GAD, and MDD, we examined whether lung and heart recipients with no lifetime history of a given disorder differed in first lifetime onset posttransplant. Survival analyses indicated that 9% of lung recipients with no lifetime history of panic disorder had their first lifetime onset by 2 years posttransplant, compared to 2% of heart recipients (Wilcoxon χ2 (df=1)=5.80, p=.016). Lung and heart recipients did not differ significantly on first lifetime onset rates of GAD posttransplant (1% and 3%, respectively; Wilcoxon χ2 (df=1)=1.78, p=.182) or first lifetime onset of MDD posttransplant (15% and 20%, respectively; Wilcoxon χ2 (df=1)=0.28, p=.593).
Clinical characteristics of psychiatric disorders
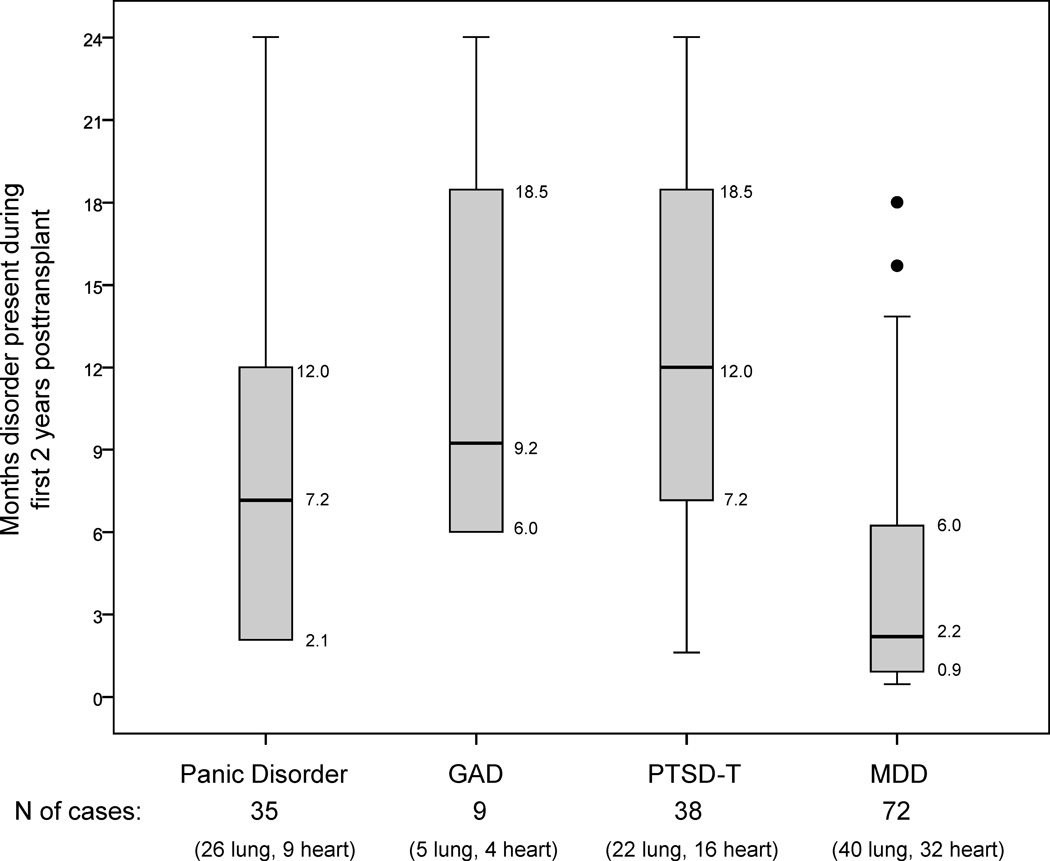
Among individuals meeting criteria for major disorders posttransplant (panic disorder, GAD, PTSD-T, MDD), we examined the total months during the 2-year posttransplant period in which respondents had active disorder. For GAD, PTSD-T, and MDD, this included the index episode plus any recurrence. For panic disorder, we ascertained at each assessment after initial diagnosis whether respondents continued to have panic attacks that met diagnostic criteria. Figure 2 displays box plots of the sample’s distributions of duration of active disorder. For example, PTSD-T had the greatest median duration (12 months), and its interquartile range (IQR) was 7.2 to 18.5 months. The duration of MDD was shortest, with the narrowest IQR. However, the MDD distribution was skewed; some individuals had durations of MDD well above the median. Lung and heart recipients showed no significant differences on total duration of any disorder (all p’s>.05). The box plots’ shapes did not change if analyses were restricted to recipients surviving the entire study period.
Figure 2.
Distribution of total duration of disorder among individuals who met diagnostic criteria during 2-year study period.a
aThe box plots include all individuals, regardless of whether they received treatment for these disorders.
We examined whether total duration of illness reflected one continuous period or a pattern of recurrent episodes. As shown in Table 3, no individuals had recurrent episodes of GAD or PTSD-T during the study period, and all individuals with panic disorder continued to experience panic attacks intermittently after their initial posttransplant episode (and thus had no extended period of remission that would allow for recurrence to be documented). In contrast, one third of patients had recurrent episodes of MDD, with no difference between study groups.
Table 3.
Rates of disorder recurrence, treatment seeking during episodes and receipt of psychotropic medications for disorder during the first two years posttransplant.
| DSM-IV Disorder | Panic disorder (n = 35 cases) |
GAD (n = 9 cases) |
PTSD-T (n = 38 cases) |
MDD (n = 72 cases) |
|---|---|---|---|---|
| Recurrent episodes, % yes (n) | ||||
| Total sample | 0.0a (0) | 0.0 (0) | 0.0 (0) | 30.6 (22) |
| Lung recipients | --- | --- | --- | 32.5 (13) |
| Heart recipients | --- | --- | --- | 28.1 (9) |
| Lung vs. heart, exact p | --- | --- | --- | .799 |
| Sought treatment,b % yes (n) | ||||
| Total sample | 54.3 (19) | 77.8 (7) | 60.5 (23) | 70.8 (51) |
| Lung | 57.7 (15) | 100.0 (5) | 63.6 (14) | 75.0 (30) |
| Heart | 44.4 (4) | 50.0 (2) | 56.3 (9) | 65.6 (21) |
| Lung vs. heart, exact p | .700 | .167 | .742 | .440 |
| Received psychotropic medications,b % yes (n) | ||||
| Total sample | 48.6 (17) | 77.8 (7) | 50.0 (19) | 65.3 (47) |
| Lung | 50.0 (13) | 100.0 (5) | 50.0 (11) | 65.0 (26) |
| Heart | 44.4 (4) | 50.0 (2) | 50.0 (8) | 65.6 (21) |
| Lung vs. heart, exact p | 1.000 | .167 | 1.000 | 1.000 |
As noted in the text, all recipients continuted to experience panic attacks after their initial posttransplant episode, and thus had no period of remission that would allow for recurrent to be documented.
As noted in the text, information on seeking treatment and receiving medications was obtained during the SCID.
Abbreviations: GAD, generalized anxiety disorder; PTSD-T, post-traumatic stress disorder related to the transplant; MDD, major depressive disorder.
Within the SCID, individuals were asked whether they sought treatment and received any psychotropic medications during episodes. MDD and GAD were associated with the highest treatment-seeking rates (Table 3). Recipients were least likely to seek help or receive medications for panic disorder. Lung and heart recipients did not differ in rates of treatment seeking or receipt of medications, although the number of cases is small.
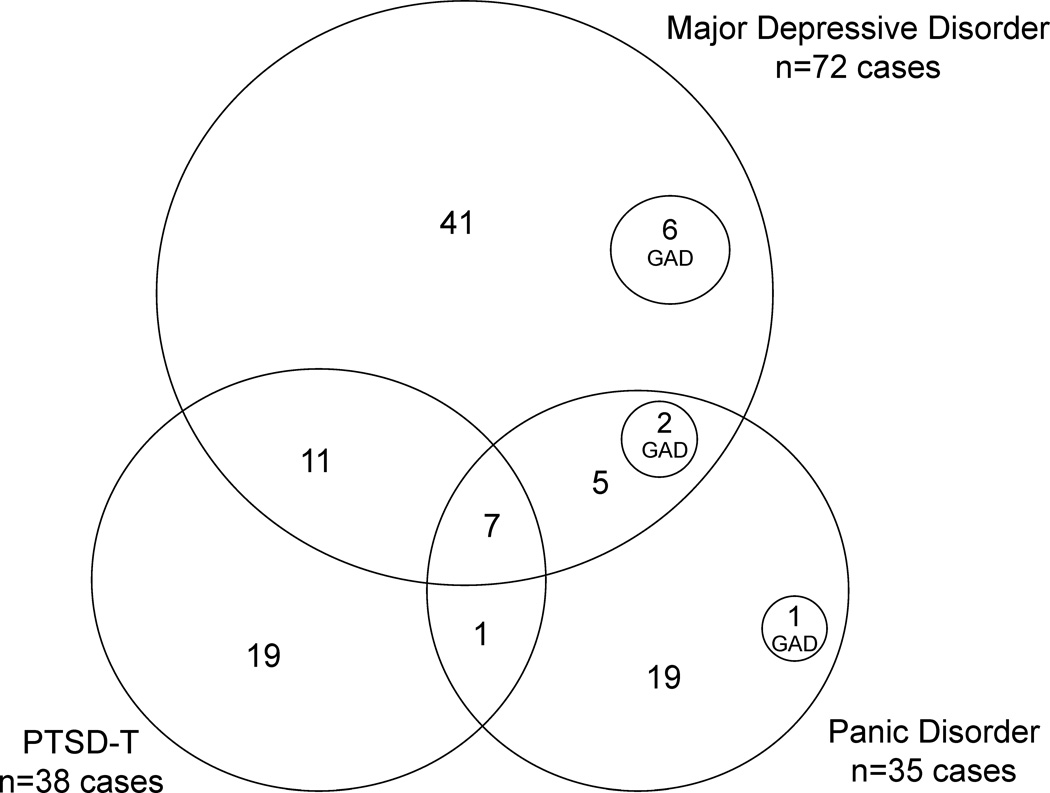
We also considered disorders’ comorbidity patterns. First we examined whether each respondent met criteria for more than one type of major disorder during the two-year study period, regardless of whether the episodes overlapped in time. Figure 3 displays these patterns. For example, 41 persons experienced only MDD, 11 met criteria for both MDD and PTSD-T, and so on. Overall, of the 72 individuals with MDD, 31 (43%) had at least one comorbid disorder. Comorbidity rates were higher for other disorders: 46% of individuals with panic disorder met criteria for another disorder, as did 50% of those with PTSD-T, and 100% of those with GAD. The numbers of cases with specific combinations of disorders were too small to examine by type of transplant. However, the percentage of lung recipients with ≥1 comorbid disorder (27.5%) was similar to that in heart recipients (32.6%; χ2(df=1)=0.32, p=.571).
Figure 3.
Comorbidity of assessed disorders during 2-year study period.
Finally, we examined whether individuals who met criteria for multiple diagnoses had episodes of disorder that overlapped in time. Of the 33 cases in Figure 3 with ≥1 diagnosis, all but 4 (3 lung recipients with MDD and PTSD-T and 1 heart recipient with MDD and panic disorder) had multiple disorders that overlapped at least partially in time.
Risk factors for psychiatric disorder
Because there were only 9 cases of GAD, risk factors could not be considered. To limit the number of tests examining risk factor-psychiatric disorder associations, we first examined simple, bivariate associations between each potential risk factor and the occurrence of the remaining three disorders (panic disorder, PTSD-T, MDD). Potential risk factors showing small associations (r or phi <.20) with all three types of disorder were not considered further. Remaining factors were entered simultaneously into Cox proportional hazards analysis, with a separate model fit for each disorder. Table 4 presents hazard ratios (HRs), generated from the regression coefficients, and the 95% confidence interval for each HR. For dichotomous risk factors (e.g., pretransplant history of psychiatric disorder), the HRs indicate the degree of increased risk of a given psychiatric disorder if the risk factor was present. For continuous risk factor variables (e.g., dyspnea), the HRs indicate the degree of increased risk per unit of change on the risk factor.
Table 4.
Cox proportional hazards models examining potential risk factor associations with psychiatric disorder onset during the first two years after cardiothoracic transplantation.a
| Potential Risk Factor | Percentage or Mean (SD) in study sample |
Psychiatric disorder | |||||
|---|---|---|---|---|---|---|---|
| Panic disorder | PTSD-T | MDD | |||||
| HR | CI | HR | CI | HR | CI | ||
| Pretransplant characteristics | |||||||
| Gender, female | 41.1 | 3.62** | 1.52, 8.62 | 1.53 | 0.76, 3.11 | 1.21 | 0.72, 2.04 |
| History of depression or anxiety disorder, yes | 48.8 | 9.01*** | 2.71, 30.30 | 2.61* | 1.21, 5.68 | 2.51** | 1.43, 4.39 |
| Transplant-related health characteristics | |||||||
| Physical functional status at 2 mos posttransplant, 0=low, 100=high | 54.1 (25.4) | 1.00 | 0.98, 1.02 | 0.99 | 0.98, 1.01 | 0.99 | 0.98, 1.00 |
| Chronic dyspnea at 2 mos posttransplant, 1=extreme, 10=none | 7.3 (2.1) | 0.87 | 0.72, 1.05 | 0.82* | 0.69, 0.97 | 0.72 | 0.43, 1.19 |
| Psychosocial characteristics | |||||||
| Interpersonal | |||||||
| Social support from family caregiver, poor | 32.1 | 0.64 | 0.30, 1.36 | 1.12 | 0.57, 2.20 | 1.82* | 1.09, 3.03 |
| Intrapersonal | |||||||
| Support from faith, low | 32.8 | 1.86 | 0.90, 3.84 | 0.69 | 0.32, 1.49 | 0.94 | 0.55, 1.62 |
| Coping: support-seeking/expression of emotions, high | 49.7 | 0.73 | 0.33, 1.61 | 0.89 | 0.43, 1.83 | 1.84* | 1.04, 3.24 |
| Coping: avoidance coping, high | 40.2 | 2.20* | 1.03, 4.67 | 1.61 | 0.80, 3.20 | 1.30 | 0.78, 2.17 |
| Improvement in model fit over null model, χ2 (df=9) | 52.4*** | 27.6** | 44.2*** | ||||
HR, Hazard ratio; CI, confidence interval
p<.05
p<.01
p<.001
All models examining potential risk factors controlled for transplant group (lung vs. heart recipients). Additional pretransplant characteristics (age, education, race/ethnicity, income level, length of wait for transplant) and posttransplant psychosocial characteristics (length of posttransplant hospitalization, support from friends, active coping, acceptance coping) showed small bivariate associations with all psychiatric disorder outcomes variables (r or phi < .20). Thus, they were not included in the multivariate models.
Abbreviations: PTSD-T, post-traumatic stress disorder related to the transplant; MDD, major depressive disorder.
Table 4 shows that risk for each of the disorders was increased from over 2 to 9-fold by a pretransplant history of mood or anxiety disorder. In addition, panic disorder risk was increased by female gender. Panic disorder risk was over twice as great if individuals used avoidance strategies to cope with health problems. Risk for PTSD-T was increased by chronic dyspnea early posttransplant. MDD risk was increased by two psychosocial variables, poor family caregiver support, and use of coping strategies focused on support seeking and expression of emotions.
Beyond these main effects, we added interaction terms between type of transplant and each risk factor variable to the Cox models to determine whether any risk factor effects varied across lung versus heart recipients. There were no differential effects by transplant group.
Lastly, because the number of panic disorder and PTSD-T cases in our sample was relatively small in absolute terms (n=33 and n=38, respectively), a sensitivity analysis was performed. Thus, it has been recommended that when the cases to predictors ratio is small (here, with 9 predictors in a model, the ratio is under 5 for each of these disorders), the Cox models should be re-estimated with weaker predictors excluded in order to determine the stability of any significant results.[65,66] When we excluded weak, nonsignificant predictors listed in Table 4, remaining predictors all retained statistical significance for both panic disorder and PTSD-T.
DISCUSSION
This study provides the first empirical evidence about onset rates and risk factors for psychiatric disorder through two years after lung transplantation. The inclusion of a comparison group of heart recipients from the same transplant program allows us to begin to identify clinical issues that may demand special attention in lung recipients, as well as issues likely to be shared across all cardiothoracic transplant recipients.
Several key findings emerged in this regard. First, lung recipients are at elevated risk for panic disorder. Their cumulative onset rate of panic disorder by two years posttransplant (18%) was over twice that in the comparison group (8%). Both groups’ rates are considerably higher than those for community-based samples, where 12-month and lifetime rates have been found to be 2%–3% and 4%–5% respectively.[67–69] However, our data are consistent with epidemiologic findings that panic disorder is highly comorbid with chronic physical illness,[33,67] and is up to 10 times more prevalent in patients with lung conditions than in the general population.[33]
Our lung recipients’ unique propensity for panic disorder is not explained by a pre-transplant panic disorder history because, even among respondents with no such history, lung recipients’ rate of first lifetime onset of panic disorder during the two years posttransplant (9%) was considerably greater than that in heart recipients (2%). Lung recipients’ elevated panic disorder rate also cannot be explained by the occurrence of episodes of acute dyspnea or average levels of chronic dyspnea. Concerning acute dyspnea, DSM-IV criteria preclude the diagnosis of panic disorder in individuals whose attacks occur solely in response to episodes of dyspnea or situational precipitants of dyspnea.[39] With regard to chronic dyspnea, while lung recipients reported more severe levels than did heart recipients, chronic dyspnea did not emerge in multivariate analyses as an independent risk factor for panic disorder.
It has been suggested that somatic symptom levels per se are less important contributors to panic than is the individual’s neurobiological or cognitive response to those symptoms.[33] Thus, the same biological pathways that underlie conditioned fear in animal models,[70] and/or a pattern of catastrophic thinking in the presence of minor or ambiguous somatic symptoms,[33] may increase an individual’s risk for panic disorder, particularly in the context of chronic respiratory disease.[33,71] Lung recipients in particular, by virtue of their history of respiratory disease and receipt of a major surgical intervention for it, may be exquisitely sensitive and perhaps hypervigilant for symptoms; frightening symptoms may provoke a panic response, followed by increased catastrophic thinking, and a vicious cycle ensues. While our study could not test mechanisms responsible for panic risk in lung recipients, our findings nevertheless suggest that transplant programs should be particularly attentive to this risk in lung recipients, and engage in (a) screening and treatment for panic disorder symptoms and (b) patient education about posttransplant somatic symptoms and ways to self-manage these symptoms.
In contrast, our findings that posttransplant onset rates of other anxiety and mood disorders were similar in lung and heart recipients suggest that transplant programs should pay equal attention to risk for these disorders across both cardiothoracic populations. In particular, MDD risk was substantial, with over one quarter of the sample experiencing it in just the first two years after transplantation. As is typical in cardiothoracic transplant samples,[17,18,72] a large percentage of our patients had pretransplant histories of MDD; MDD is well-known to be a chronic, relapsing disorder. Yet, even in individuals with no pretransplant history, 15%–20% had their first lifetime onset of MDD during the 2-year period posttransplant. This attests to the impact of the transplant experience, as does the occurrence of PTSD-T in 14%–15% of recipients. The rate of PTSD-T, as well as the clustering of onsets almost exclusively in the first year posttransplant, is consistent with past findings in heart recipients.[54] Finally, as in other transplant cohorts,[16,52] GAD occurred infrequently.
Our data on duration of posttransplant disorder episodes and comorbidity patterns suggest that the burden of living with these illnesses can be great. Many recipients who met diagnostic criteria spent a substantial proportion of the 2-year study period with active illness, particularly patients with anxiety disorders. Total time living with MDD was shorter, but affected patients were at risk for recurrences. The considerable comorbidity among the disorders further increases their burden. Overall, the price of the illness burden in our sample is likely to be exacted in reduced quality of life. Unfortunately, as is typical in community-based and outpatient samples,[73] many patients did not seek treatment or receive medication. This was particularly so for panic disorder, perhaps because panic episodes occur sporadically and thus this disorder’s symptoms may be even less apparent to treatment providers than symptoms of disorders such as MDD and GAD. The low rates of both treatment-seeking and receipt of treatment for panic disorder, combined with the elevated rate of this disorder in lung recipients, further point to the need for increased vigilance by transplant teams to detect and ensure care for this condition.
The identification of risk factors for anxiety and depressive disorders may also help teams to better target detection efforts. We examined a wide array of potential risk factors, selected for both conceptual and empirical reasons. For example, poor social supports have been conceptualized as key vulnerabilities for psychiatric disorder in the face of chronic stress (such as that experienced in medically ill populations).[40–43] Other characteristics (lifetime psychiatric history; demographic variables such as gender) are well-established in psychiatric epidemiologic studies to affect risk for the disorders we studied.[66,67,74,75]. In the present study, some factors that emerged as important (e.g., gender) will be readily available in a transplant team’s medical records. Other risk factors (e.g., patients’ strategies for coping with health problems, family caregiver support) may require more effort to assess but the effort may be well-spent to the extent that the factors themselves can be modified to reduce risk of significant psychiatric distress. For example, interventions to modify coping strategies in order to improve emotional well-being in transplant populations have shown some success, although studies have been small and have not included lung recipients.[76–78] These interventions have been either telephone-[76,78] or internet-based[77] and hence may show promise in terms of adoption by transplant programs with limited resources for face-to-face clinical strategies, especially given that transplant recipients may reside long distances from their transplant programs and return for care increasingly less often as time elapses posttransplant.
Our study has several limitations. First, it involved patients from a single transplant center. This may affect our findings’ generalizability, although our sample was clinically and demographically similar to national cohorts. Second, we assessed only anxiety and depressive disorders. However, these conditions are prevalent in chronic disease populations, and this led to our focus in the current study. Third, we assessed PTSD only with regard to the transplant experience; we did not examine PTSD either before or after transplantation due to other traumatic events. It is possible that previous PTSD caused by other experiences might potentiate the development and/or complicate the course of PTSD-T. These are important issues to examine in future research.
A fourth study limitation is that, although our total sample size was large, particularly for studies of psychiatric disorder in transplantation, the absolute numbers of cases of disorder remained modest from a statistical standpoint—particularly for panic disorder and PTSD-T. Thus, the Cox models’ findings regarding significant risk factors for these disorders must be interpreted with caution and the effects that we observed require replication. Finally, there are potential risk factors that we did not assess that might influence posttransplant mental health (e.g., psychosocial characteristics such as dispositional optimism, sense of mastery or locus of control). In addition, we focused on factors that could be ascertained close to the time of transplant, given our goal of prospectively examining predictors of initial posttransplant psychiatric disorder onset. However, later-term transplant-related medical complications (e.g., malignancy, chronic graft rejection) are likely to affect patients’ emotional well-being as well. Studies that follow recipients for longer periods will need to incorporate potential risk factors related to the medical issues that they face in the later years posttransplant.
Future work should consider both the development of novel interventions to address psychiatric issues prominent among lung recipients (e.g., panic disorder) and the adaptation of existing mental health interventions designed and initially tested in other organ transplant populations.[76–78] Because psychiatric disorder onset begins early posttransplant, transplant teams should consider whether targeting both screening and intervention efforts to the pretransplant period or early months posttransplant might yield the largest benefits for disorder prevention in cardiothoracic transplant recipients.
Acknowledgments
Preparation of this article was supported in part by Grant R01 MH059229 from the National Institute of Mental Health, Rockville, MD.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Christie JD, Edwards LB, Kucheryavaya AY, et al. The Registry of the International Society for Heart and Lung Transplantation: twenty-seventh official adult lung and heart-lung transplantation report—2010. J Heart Lung Transplant. 2010;29:1104–1118. doi: 10.1016/j.healun.2010.08.004. [DOI] [PubMed] [Google Scholar]
- 2.Organ Procurement and Transplantation Network and the Scientific Registry of Transplant Recipients: 2009 Annual Report, Transplant Data 1999–2008. Rockville, MD: Department of Health and Human Services, Health Resources and Services Administration, Healthcare Systems Bureau, Division of Transplantation; Richmond, VA: United Network for Organ Sharing; Ann Arbor, MI: University Renal Research and Education Association; 2009. [Last accessed, May 4, 2011]. http://optn.transplant.hrsa.gov/data/annualReport.asp. [Google Scholar]
- 3.Korom S, Boehler A, Weder W. Immunosuppressive therapy in lung transplantation: state of the art. European J Cardio-Thorac Surg. 2009;35:1045–1055. doi: 10.1016/j.ejcts.2009.02.035. [DOI] [PubMed] [Google Scholar]
- 4.Knoop C, Estenne M. Acute and chronic rejection after lung transplantation. Semin Respiratory Crit Care Medicine. 2006;27:521–533. doi: 10.1055/s-2006-954609. [DOI] [PubMed] [Google Scholar]
- 5.Cupples SA, Dew MA, Grady KL, et al. The present status of research on psychosocial outcomes in cardiothoracic transplantation: review and recommendations for the field. J Heart Lung Transplant. 2006;25:716–725. doi: 10.1016/j.healun.2006.02.005. [DOI] [PubMed] [Google Scholar]
- 6.Dew MA, Switzer GE, Goycoolea JM, et al. Does transplantation produce quality of life benefits? A quantitative review of the literature. Transplantation. 1997;64:1261–1273. doi: 10.1097/00007890-199711150-00006. [DOI] [PubMed] [Google Scholar]
- 7.Lanuza DM, McCabe M, Norton-Rosko M, Corliss JW, Garrity E. Symptom experiences of lung transplant recipients: comparisons across gender, pretransplantation diagnosis, and type of transplantation. Heart Lung. 1999;28:429–437. doi: 10.1016/s0147-9563(99)70032-4. [DOI] [PubMed] [Google Scholar]
- 8.Rodrigue JR, Baz MA, Kanasky WF, Jr, MacNaughton KL. Does lung transplantation improve health-related quality of life? The University of Florida experience. J Heart Lung Transplant. 2005;24:755–763. doi: 10.1016/j.healun.2004.04.012. [DOI] [PubMed] [Google Scholar]
- 9.Santana MJ, Feeny D, Jackson K, Weinkauf J, Lien D. Improvement in health-related quality of life after lung transplantation. Canadian Respiratory J. 2009;16:153–158. doi: 10.1155/2009/843215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.TenVergert EM, Essink-Bot ML, Geertsma A, et al. The effect of lung transplantation on health-related quality of life: a longitudinal study. Chest. 1998;113:358–364. doi: 10.1378/chest.113.2.358. [DOI] [PubMed] [Google Scholar]
- 11.Vermeulen KM, Ouwens JP, van der Bij W, et al. Long-term quality of life in patients surviving at least 55 months after lung transplantation. Gen Hosp Psychiatry. 2003;25:95–102. doi: 10.1016/s0163-8343(03)00007-0. [DOI] [PubMed] [Google Scholar]
- 12.DeVito Dabbs AJ, Dew MA, Stilley CS, et al. Psychosocial vulnerability, physical symptoms and physical impairment after lung and heart-lung transplantation. J Heart Lung Transplant. 2003;22:1268–1275. doi: 10.1016/s1053-2498(02)01227-5. [DOI] [PubMed] [Google Scholar]
- 13.Kugler C, Fischer S, Gottlieb J, et al. Symptom experience after lung transplantation: impact on quality of life and adherence. Clin Transplant. 2007;21:590–596. doi: 10.1111/j.1399-0012.2007.00693.x. [DOI] [PubMed] [Google Scholar]
- 14.Langer D, Gosselink R, Pitta F, et al. Physical activity in daily life 1 year after lung transplantation. J Heart Lung Transplant. 2009;28:572–578. doi: 10.1016/j.healun.2009.03.007. [DOI] [PubMed] [Google Scholar]
- 15.Lanuza DM, Lefaiver C, McCabe M, Farcas GA, Garrity E., Jr Prospective study of functional status and quality of life before and after lung transplantation. Chest. 2000;118:115–122. doi: 10.1378/chest.118.1.115. [DOI] [PubMed] [Google Scholar]
- 16.Myaskovsky L, Dew MA, McNulty ML, et al. Trajectories of change in quality of life in 12-month survivors of lung or heart transplant. Am J Transplant. 2006;6:1939–1947. doi: 10.1111/j.1600-6143.2006.01395.x. [DOI] [PubMed] [Google Scholar]
- 17.Dew MA, DiMartini AF. Psychological disorders and distress after adult cardiothoracic transplantation. J Cardiovasc Nursing. 2005;20(5) Suppl:S51–S66. doi: 10.1097/00005082-200509001-00007. [DOI] [PubMed] [Google Scholar]
- 18.Fusar-Poli P, Lazzaretti M, Ceruti M, et al. Depression after lung transplantation: causes and treatment. Lung. 2007;185:55–65. doi: 10.1007/s00408-006-0093-1. [DOI] [PubMed] [Google Scholar]
- 19.Goetzmann L, Irani S, Schwegler K, et al. Distress and alexithymia in lung recipients - psychosocial strains and associations with chronic allograft dysfunction. Swiss Medical Weekly. 2010;140(25–26):382–387. doi: 10.4414/smw.2010.12770. [DOI] [PubMed] [Google Scholar]
- 20.Limbos MM, Joyce DP, Chan CK, Kesten S. Psychological functioning and quality of life in lung transplant candidates and recipients. Chest. 2000;118:408–416. doi: 10.1378/chest.118.2.408. [DOI] [PubMed] [Google Scholar]
- 21.Stilley CS, Dew MA, Stukas AA, et al. Psychological symptom levels and their correlates in lung and heart-lung transplant recipients. Psychosomatics. 1999;40:503–509. doi: 10.1016/s0033-3182(99)71189-8. [DOI] [PubMed] [Google Scholar]
- 22.Elidemir O, Smith KJ, Schecter MG, et al. Lung transplantation in a patient with thrombophilic disorder. Pediatr Transplant. 2008;12:368–371. doi: 10.1111/j.1399-3046.2007.00815.x. [DOI] [PubMed] [Google Scholar]
- 23.Jayaram G, Casimir A. Major depression and the use of electroconvulsive therapy (ECT) in lung transplant recipients. Psychosomatics. 2005;46:244–249. doi: 10.1176/appi.psy.46.3.244. [DOI] [PubMed] [Google Scholar]
- 24.Jowsey SG, Bruce BK, McGregor CG. Decreased anxiety in lung transplant recipients. Am J Psychiatry. 1994;151:617. doi: 10.1176/ajp.151.4.617a. [DOI] [PubMed] [Google Scholar]
- 25.Köllner V, Schade I, Maulhardt T, et al. Posttraumatic stress disorder and quality of life after heart or lung transplantation. Transplant Proc. 2002;34:2192–2193. doi: 10.1016/s0041-1345(02)03198-6. [DOI] [PubMed] [Google Scholar]
- 26.Dew MA, DiMartini AF. Transplantation. In: HS Friedman HS, editor. Oxford Handbook of Health Psychology. New York: Oxford University Press; 2011. pp. 522–559. [Google Scholar]
- 27.Dew MA, Kormos RL, Roth LH, et al. Early post-transplant medical compliance and mental health predict physical morbidity and mortality one to three years after heart transplantation. J Heart Lung Transplant. 1999;18:549–562. doi: 10.1016/s1053-2498(98)00044-8. [DOI] [PubMed] [Google Scholar]
- 28.DiMartini A, Dew MA, Chaiffetz D, et al. Early trajectories of depressive symptoms after liver transplantation predict long-term survival. Am J Transplant. doi: 10.1111/j.1600-6143.2011.03496.x. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dobbels F, Skeans MA, Snyder JJ, et al. Depressive disorder in renal transplantation: an analysis of Medicare claims. Am J Kidney Dis. 2008;51:819–828. doi: 10.1053/j.ajkd.2008.01.010. [DOI] [PubMed] [Google Scholar]
- 30.Rosenberger E, Dew MA, Crone C, DiMartini AF. Psychiatric disorder as a risk factor for adverse medical outcomes after solid organ transplantation. Curr Opin Transplant. doi: 10.1097/MOT.0b013e3283510928. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chacko RC, Harper RG, Kunik M, Young J. Relationship of psychiatric morbidity and psychosocial factors in organ transplant candidates. Psychosomatics. 1996;37:100–107. doi: 10.1016/S0033-3182(96)71575-X. [DOI] [PubMed] [Google Scholar]
- 32.Karajgi B, Rifkin A, Doddi S, Kolli R. The prevalence of anxiety disorders in patients with chronic obstructive pulmonary disease. Am J Psychiatry. 1990;147:200–201. doi: 10.1176/ajp.147.2.200. [DOI] [PubMed] [Google Scholar]
- 33.Livermore N, Sharpe L, McKenzie D. Panic attacks and panic disorder in chronic obstructive pulmonary disease: a cognitive behavioral perspective. Respiratory Med. 2010;104:1246–1253. doi: 10.1016/j.rmed.2010.04.011. [DOI] [PubMed] [Google Scholar]
- 34.Parekh P, Blumenthal JA, Babyak MA, et al. Psychiatric disorder and quality of life in patients awaiting lung transplantation. Chest. 2003;124:1682–1688. doi: 10.1378/chest.124.5.1682. [DOI] [PubMed] [Google Scholar]
- 35.Yellowlees PM, Ruffin RE. Psychological defenses and coping styles in patients following a life-threatening attack of asthma. Chest. 1989;95:1298–1303. doi: 10.1378/chest.95.6.1298. [DOI] [PubMed] [Google Scholar]
- 36.Dew MA, Cyranowski JM, Pilkonis PA. Medical conditions and depression. In: Ingram RE, editor. International Encyclopedia of Depression. New York: Springer; 2009. pp. 375–380. [Google Scholar]
- 37.DiMartini A, Dew MA, Crone K. Organ transplantation. In: Sadock BJ, Sadock VA, Ruiz P, editors. Kaplan and Sadock’s Comprehensive textbook of psychiatry. 9th ed. Vol. 2. Philadelphia: Lippincott Williams & Wilkins; 2009. pp. 2441–2456. [Google Scholar]
- 38.Katon WJ. Clinical and health services relationships between major depression, depressive symptoms, and general medical illness. Biolog Psychiatry. 2003;54:216–226. doi: 10.1016/s0006-3223(03)00273-7. [DOI] [PubMed] [Google Scholar]
- 39.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: American Psychiatric Association Press; 2000. Text revision. [Google Scholar]
- 40.Dew MA. Psychiatric disorder in the context of physical illness. In: Dohrenwend BP, editor. Adversity, stress and psychopathology. New York: Oxford University Press; 1998. pp. 177–218. [Google Scholar]
- 41.Dohrenwend BP. The role of adversity and stress in psychopathology: some evidence and its implications for theory and research. J Health Soc Behavior. 2000;41:1–19. [PubMed] [Google Scholar]
- 42.Hammen C. Stress and depression. Ann Rev Clin Psychol. 2005;1:293–319. doi: 10.1146/annurev.clinpsy.1.102803.143938. [DOI] [PubMed] [Google Scholar]
- 43.Zuckerman M. Vulnerability to psychopathology: A biosocial model. Washington, DC: American Psychological Association; 1999. [Google Scholar]
- 44.Dew MA, DiMartini AF, Kormos RL. Organ transplantation, Stress of. In: Fink G, editor. Encyclopedia of Stress. 2nd ed. Vol. 3. Oxford, UK: Academic Press (Elsevier); 2007. pp. 35–44. [Google Scholar]
- 45.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders, Clinician Version (SCID-CV) Washington, D.C: American Psychiatric Press, Inc.; 1996. revised 2002. [Google Scholar]
- 46.Cavanaugh S. Diagnosing depression in the hospitalized patient with chronic medical illness. J Clin Psychiatry. 1994;45:13–16. [PubMed] [Google Scholar]
- 47.DiMartini AF, Crone C, Fireman M, Dew MA. Psychiatric aspects of organ transplantation in critical care. Crit Care Clinics N America. 2008;24:949–981. doi: 10.1016/j.ccc.2008.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ware JE, Snow KK, Kosinski M, Gandek B. SF-36 health survey: Manual and interpretation guide. Boston: The Health Insititute, New England Medical Center; 1993. [Google Scholar]
- 49.Guyatt GH, Berman LB, Townsend M, Pugsley SO, Chambers LW. A measure of quality of life for clinical trials in chronic lung disease. Thorax. 1987;42:773–778. doi: 10.1136/thx.42.10.773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Schünemann HJ, Puhan M, Goldstein R, Jaeschke R, Guyatt GH. Measurement properties and interpretability of the Chronic Respiratory Disease Questionnaire (CRQ) J Chronic Obstructive Pulm Dis. 2005;2:81–89. doi: 10.1081/copd-200050651. [DOI] [PubMed] [Google Scholar]
- 51.Spanier GB. Measuring dyadic adjustment: New scales for assessing the quality of marriage and similar dyads. J Marriage Family. 1976;38:15–30. [Google Scholar]
- 52.Pearlin LI, Schooler C. The structure of coping. J Health Social Behavior. 1978;19:2–21. [PubMed] [Google Scholar]
- 53.Dew MA, Simmons RG, Roth LH, Schulberg HC, Thompson ME, Armitage JM, Griffith BP. Psychosocial predictors of vulnerability to distress in the year following heart transplantation. Psycholog Medicine. 1994;24:929–945. doi: 10.1017/s0033291700029020. [DOI] [PubMed] [Google Scholar]
- 54.Dew MA, Kormos RL, DiMartini AF, et al. Prevalence and risk of depression and anxiety-related disorders during the first three years after heart transplantation. Psychosomatics. 2001;42:300–313. doi: 10.1176/appi.psy.42.4.300. [DOI] [PubMed] [Google Scholar]
- 55.Dew MA, Myaskovsky L, DiMartini AF, et al. Onset, timing and risk for depression and anxiety in family caregivers to heart transplant recipients. Psychological Med. 2004;34:1065–1082. doi: 10.1017/s0033291703001387. [DOI] [PubMed] [Google Scholar]
- 56.Moos RH. Evaluating correctional and community settings. NY: Wiley; 1975. [Google Scholar]
- 57.King M, Hunt R. Measuring the religious variable: national replication. J Sci Study Religion. 1975;14:13–22. [Google Scholar]
- 58.Carver CS. You want to measure coping but your protocol’s too long: Consider the Brief COPE. Internat J Behavioral Med. 1997;4:92–100. doi: 10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- 59.Carver CS, Scheier MF, Weintraub JK. Assessing coping strategies: A theoretically based approach. J Personality Social Psychol. 1989;56:267–283. doi: 10.1037//0022-3514.56.2.267. [DOI] [PubMed] [Google Scholar]
- 60.Folkman S, Moskowitz JT. Coping: pitfalls and promise. Ann Rev Psychol. 2004;55:745–774. doi: 10.1146/annurev.psych.55.090902.141456. [DOI] [PubMed] [Google Scholar]
- 61.Cox DR, Oakes D. Analysis of survival data. 2nd edition. London: Chapman & Hall; 1984. [Google Scholar]
- 62.Tabachnick BG, Fidell LS. Using multivariate statistics. 5th edition. Needham Heights, MA: Pearson/Allyn & Bacon; 2007. [Google Scholar]
- 63.Department of Health and Human Services, United States Government. Annual Update of the HHS Poverty Guidelines. Fed Register. 2002 February 14;67:6931–6933.
- 64.U.S. Organ Procurement and Transplantation Network and the Scientific Registry of Transplant Recipients. 2006 Annual Report, Transplant Data 1996–2005. Rockville, MD: Dept. of Health and Human Services, Health Resources and Services Administration, Healthcare Systems Bureau, Division of Transplantation; Richmond, VA: United Network for Organ Sharing; Ann Arbor, MI: University Renal Research and Education Association; 2006. [Last accessed June 24, 2011]. http://optn.transplant.hrsa.gov/data/annualReport.asp. [Google Scholar]
- 65.Peduzzi P, Concato J, Feinstein AR, Holford TR. Importance of events per independent variable in proportional hazards regression analysis. II. Accuracy and precision of regression estimates. J Clin Epidemiol. 1995;48:1503–1510. doi: 10.1016/0895-4356(95)00048-8. [DOI] [PubMed] [Google Scholar]
- 66.Vittinghoff E, McCulloch CE. Relaxing the rule of ten events per variable in logistic and Cox regression. Am J Epdemiol. 2007;165:710–718. doi: 10.1093/aje/kwk052. [DOI] [PubMed] [Google Scholar]
- 67.Goodwin RD, Faravelli C, Rosi S, et al. The epidemiology of panic disorder and agoraphobia in Europe. European Neuropsychopharmacology. 2005;15:435–443. doi: 10.1016/j.euroneuro.2005.04.006. [DOI] [PubMed] [Google Scholar]
- 68.Grant BF, Hasin DS, Stinson FS, et al. The epidemiology of DSM-IV panic disorder and agoraphobia in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2006;67:363–374. doi: 10.4088/jcp.v67n0305. [DOI] [PubMed] [Google Scholar]
- 69.Kessler RC, Chiu WT, Jin R, et al. The epidemiology of panic attacks, panic disorder, and agoraphobia in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2006;63(4):415–424. doi: 10.1001/archpsyc.63.4.415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Gorman JM, Kent JM, Sullivan G, Coplan JD. Neuroanatomical hypothesis of panic disorder, revised. Am J Psychiatry. 2000;157:493–505. doi: 10.1176/appi.ajp.157.4.493. [DOI] [PubMed] [Google Scholar]
- 71.Katon WJ. Panic disorder. New England J Medicine. 2006;354:2360–2367. doi: 10.1056/NEJMcp052466. [DOI] [PubMed] [Google Scholar]
- 72.Dobbels F, De Geest S, Cleemput I, et al. Psychosocial and behavioral selection criteria for solid organ transplantation. Prog Transplant. 2001;11:121–130. doi: 10.1177/152692480101100208. [DOI] [PubMed] [Google Scholar]
- 73.Wang PS, Lane M, Olfson M, et al. Twelve-month use of mental health services in the United States: results from the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:629–640. doi: 10.1001/archpsyc.62.6.629. [DOI] [PubMed] [Google Scholar]
- 74.Addington AM, Gallo JJ, Ford DE, Eaton WW. Epidemiology of unexplained fatigue and major depression in the community: The Baltimore ECA follow-up, 1981–1994. Psycholog Medicine. 2001;31:1037–1044. doi: 10.1017/s0033291701004214. [DOI] [PubMed] [Google Scholar]
- 75.Kessler RC, Chiu WT, Demler O, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey replication. Arch Gen Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Blumenthal JA, Babyak MA, Keefe FJ, et al. Telephone-based coping skills training for patients awaiting lung transplantation. J Consulting Clin Psychology. 2006;74:535–544. doi: 10.1037/0022-006X.74.3.535. [DOI] [PubMed] [Google Scholar]
- 77.Dew MA, Goycoolea JM, Harris RC, et al. An internet-based intervention to improve psychosocial outcomes in heart transplant recipients and family caregivers: development and evaluation. J Heart Lung Transplant. 2004;3:745–758. doi: 10.1016/j.healun.2003.07.002. [DOI] [PubMed] [Google Scholar]
- 78.Rodrigue JR, Baz MA, Widows MR, Ehlers SL. A randomized evaluation of quality-of-life therapy with patients awaiting lung transplantation. Am J Transplant. 2005;5:2425–2432. doi: 10.1111/j.1600-6143.2005.01038.x. [DOI] [PubMed] [Google Scholar]