Abstract
Age-based differences in fall type and neuroanatomy in infants and toddlers may affect clinical presentations and injury patterns.
Objective
Our goal is to understand the influence of fall type and age on injuries to help guide clinical evaluation.
Design/Setting/Participants
Retrospectively, 285 children 0–48 months with accidental head injury from a fall and brain imaging between 2000–2006 were categorized by age (infant=<1 year and toddler=1–4 years) and fall type: low (≤3 ft), intermediate (>3 and <10 ft), high height falls (≥10 ft) and stair falls.
Outcome Measures
Clinical manifestations were noted and head injuries separated into primary (bleeding) and secondary (hypoxia, edema). The influence of age and fall type on head injuries sustained was evaluated.
Results
Injury patterns in children <4 yrs varied with age. Despite similar injury severity scores, infants sustained more skull fractures than toddlers (71% v. 39%). Of children with skull fractures, 11% had no evidence of scalp/facial soft tissue swelling. Of the patients with primary intracranial injury, 30% had no skull fracture and 8% had neither skull fracture nor cranial soft tissue injury. Low height falls resulted in primary intracranial injury without soft tissue or skull injury in infants (6%) and toddlers (16%).
Conclusions
Within a given fall type, age-related differences in injuries exist between infants and toddlers. When interpreting a fall history, clinicians must consider the fall type and influence of age on resulting injury. For young children, intracranial injury is not always accompanied by external manifestations of their injury.
Keywords: falls, brain injury, mechanism, age
Introduction
Pediatric head injury accounts for over 95,000 hospital admissions and 29,000 permanent disabilities annually and is the most common cause of death among US children.1,2 While falls are the most common environmental setting for closed head injuries treated in pediatric observational units, a marked variability in injury mechanism and pattern by age has been noted,3,4,5 particularly between infants and toddlers.1,5–7 Furthermore, the injury mechanism has been shown to influence the resulting injury pattern for a given event.8,9 It is unclear, however, whether injury patterns also vary by age within a given mechanism of injury. Multiple investigators have studied the incidence of accidental trauma and resulting injuries in children.8,10–12 Some have examined differences in head injury patterns by age and mechanism but none have looked at the effect of both age and mechanism on the resulting head injury pattern.
Between birth and four years of age, children undergo significant cranial changes including rapid increase in brain size, development of neural function and suture ossification. These changes may affect the type of head injuries sustained from accidental falls. In addition, changes in child development may influence the fall types leading to head trauma. Examining head injury mechanisms and patterns in more refined age groups may aid in understanding age-dependent contributors to injury and injury mechanisms in unintentional head trauma in infants and toddlers. Further data may help clinicians and researchers better understand the expected range of injury from falls. We hypothesize that both age and fall type influence the injury pattern in young children. The objectives of this study were to 1) describe patterns of head injury in children <4 years of age with accidental trauma from a fall; 2) identify age-dependent variations of injury patterns within fall types; and 3) identify mechanism-dependent variations in injury patterns.
Materials and Methods
A retrospective cohort study of children 0–48 months of age admitted to a tertiary care children’s hospital between 2000 and 2006 with unintentional head injury from a fall was conducted. Patients were identified by reviewing the hospital’s trauma data base for external cause of injury codes (E codes) for accidental falls (E880–888) and a diagnosis of head trauma, and were included if they had head CT and/or MRI performed at the Children’s Hospital of Philadelphia. E codes involving a fall onto an object (i.e. non-flat surface) were excluded. Children with pre-existing neurological or hematological conditions, those cases with E-codes indicative of child abuse (E967), and those where the hospital’s child protection team evaluated the patient and documented concern for possible abuse were excluded. All assigned E codes were verified by a review of the history provided in the medical record. The study was approved by the Institutional Review Board of the Children’s Hospital of Philadelphia.
Demographics, injury mechanism and clinical data related to injury patterns were extracted from medical records. Predictor variables included age and fall type. Children were classified as infants (≤1 year) or toddlers (1–4 years). Falls were divided into low (≤3 ft), intermediate (>3 ft, <10 ft), high height (≥10 ft) falls, and stair falls. The source of the fall was recorded. When fall height was not specified, fall height was estimated by the source of the fall. Falls from a bed or couch were estimated as ≤3 ft, falls from a caretaker’s arms were estimated as >3 ft and <10 ft, and falls from a 2nd story window were estimated as ≥10 ft. These height classifications were chosen to differentiate common household (low height), transitional (intermediate) and multi-story falls (high height).
The following outcome variables were noted: 1) Clinical manifestations including loss of consciousness (LOC); Glasgow Coma Score (GCS), and Injury Severity Score (ISS) (an anatomically derived survey of injury, ranging 0–75, with higher scores indicating greater injury). 2) Injury patterns including soft tissue injury to the scalp/face, skull fracture, and intracranial injury. Intracranial injury was categorized as primary (epidural (EDH), subdural (SDH), subarachnoid (SAH), intraventricular hemorrhage (IVH), parenchymal hemorrhage or contusion (IPH), and axonal injury (AI)), or secondary (cerebral edema, ischemia, infarct, or loss of gray-white matter differentiation). Information about retinal hemorrhages was recorded if available. The time elapsed to seeking medical care was also recorded. The frequency of clinical manifestations and injury patterns were calculated and compared across age and fall type.
Outcomes are expressed as either mean ± standard deviation or percent within a group. The influence of age and fall type on injuries sustained was evaluated using a Chi-squared with a Tukey-type multiple comparison test for post-hoc analysis and significance was determined by a p value <0.05 (JMP, SAS Institute Inc.).
Results
Patient Characteristics
Of the 360 patients admitted to the hospital with head injury and an E-code for fall, 75 were excluded for pre-existing conditions (n=28), E-code inaccuracy (n=15), suspicion of child abuse (n=24), or inability to locate the medical record (n=8). Of the 285 children included in the study, 157 were infants and 128 were toddlers. Average ages in the infant and toddler groups were 4.2 ± 3.4 and 28.0 ± 10.3 months, respectively. The composition of groups did not differ significantly by gender. The majority (94%) of children were seen within 24 hours of their injury.
Fall Type by Age
Infants were significantly more likely to be admitted for a low height fall compared to toddlers (n=67 infants, n=31 toddlers, p<0.01, Table 1). By comparison, high height falls were more common in toddlers (n=2 infants, n=22 toddlers, p<0.001, Table 1). Both infants and toddlers were hospitalized after stair falls. Because of the small number of children who fell >10 ft, high height falls were excluded from analysis of injuries across age.
Table 1.
Most frequent types of accidental falls in infants and toddlers. P-values note the comparison between the number of infants and number of toddlers in a given fall mechanism category.
| Fall Mechanism | # of children | ||
|---|---|---|---|
| Infants | Toddlers | p value | |
| Accidental Falls ≤ 3 ft | N=67 | N=31 | <0.001 |
| Caretaker’s arms | 9 | 1 | |
| Bed | 18 | 5 | |
| Carrier | 5 | 0 | |
| Chair | 3 | 7 | |
| Table | 4 | 0 | |
| Bouncy chair | 2 | 0 | |
| Couch | 5 | 2 | |
| Stroller | 4 | 2 | |
| Other | 17 | 14 | |
| Accidental Falls ≥ 3 ft, <10 ft | N=51 | N=45 | 0.54 |
| Caretaker’s arms | 34 | 7 | |
| Caretaker’s shoulders | 1 | 4 | |
| Shopping cart | 3 | 9 | |
| Banister | 1 | 3 | |
| Playground equipment | 0 | 3 | |
| Other | 12 | 19 | |
| Accidental Falls ≥ 10 ft | 2 | 22 | <0.002 |
| Accidental Falls, stairs | 37 | 30 | 0.39 |
Injury Patterns by Fall Type and Age
Average ISS and admission GCS (13.9±2.85) did not differ by age or type of fall. For low and intermediate height falls, skull fracture and scalp/facial soft tissue injury were observed more frequently in infants compared to toddlers (p<0.05) (Tables 2A–2B). For infants, there were no significant differences in injury patterns based on fall type (Table 2D). In toddlers, however, only low height falls resulted in primary brain injury without external signs of trauma. Additionally, multiple skull fractures in toddlers only occurred from high height falls (Table 2E) Overall, less than half of the patients who fell sustained a primary intracranial injury and less than 4% sustained a secondary intracranial injury, regardless of age or fall height (Tables 2 & 3). There were 2 reported deaths from falls: a toddler who fell 15 ft from a 2nd story window onto a concrete walkway and presented with a frontal skull fracture, SDH, SAH and IPH; and an infant who fell down 11 steps and presented with frontal and parietal skull fractures, cerebral edema, ischemia, SDH and IPH. Only 2 children required inpatient rehabilitation after their fall.
Table 2.
Frequency (%) of clinical signs and symptoms among low, intermediate, and high height and stair-related falls in infants and toddlers.
| 2A. Low Height Falls (≤ 3 ft) |
0 to 12 mos (n=67) |
12 to 48 mos (n=31) |
|---|---|---|
| Soft Tissue Injury (STI) | 84 | 42 |
| Skull Fracture (Fx) | 73 | 23 |
| Skull fx w/o STI | 5 | 0 |
| Multiple Skull Fx | 8 | 0 |
| No STI and No Skull Fx (no evidence of Impact) | 12 | 58 |
| Primary Intracranial Injury | 55 | 42 |
| Primary Intracranial Injury w/o Skull Fx | 12 | 23 |
| Primary Intracranial Injury with Skull fx | 43 | 19 |
| No STI, No Skull Fx w/Primary Brain Injury | 6 | 16 |
| Secondary Intracranial Injury | 5 | 0 |
| ISS (range, median) |
11.1 ± 0.8 (0–26, 9) |
8.8 ± 1.2 (0–20, 9) |
| GCS (range, median) |
14.2 ± 2.3 (3–15, 15) |
14.3 ± 2.4 (3–15, 15) |
| 2B. Intermediate Height Falls (>3 ft, <10 ft) |
0 to 12 mos (n=51) |
12 to 48 mos (n=45) |
|---|---|---|
| Soft Tissue Injury (STI) | 86 | 64 |
| Skull Fracture (Fx) | 69 | 49 |
| Skull fx w/o STI | 4 | 13 |
| Multiple Skull Fx | 10 | 0 |
| No STI and No Skull Fx (no evidence of Impact) | 8 | 22 |
| Primary Intracranial Injury | 49 | 36 |
| Primary Intracranial Injury w/o Skull Fx | 14 | 9 |
| Primary Intracranial Injury with Skull fx | 35 | 27 |
| No STI, No Skull Fx w/ Primary Intracranial Injury | 2 | 0 |
| Secondary Intracranial Injury | 2 | 2 |
| ISS (range, median) |
10.2 ± 0.9 (0–25, 9) |
9.8 ± 1.0 (0–30, 9) |
| GCS (range, median) |
14.5 ± 2.1 (3–15, 15) |
14.2 ± 2.3 (3–15, 15) |
| 2C. Stairs | 0 to 12 mos (n=37) |
12 to 48 mos (n=30) |
|---|---|---|
| Soft Tissue Injury (STI) | 78 | 57 |
| Skull Fracture (Fx) | 73 | 33 |
| Skull fx w/o STI | 8 | 7 |
| Multiple Skull Fx | 8 | 0 |
| No STI and No Skull Fx (no evidence of Impact) | 14 | 37 |
| Primary Intracranial Injury | 60 | 30 |
| Primary Intracranial Injury w/o Skull Fx | 3 | 7 |
| Primary Intracranial Injury with Skull fx | 57 | 23 |
| No STI, No Skull Fx w/ Primary Intracranial Injury | 0 | 0 |
| Secondary Intracranial Injury | 5 | 0 |
| ISS (range, median) |
10.1 ± 1.1 (0–26, 9) |
8.0 ± 1.3 (0–20, 5) |
| GCS (range, median) |
13.8 ± 2.8 (3–15, 15) |
14.0 ± 2.4 (6–15, 15) |
| 2D. Infant Falls | ≤ 3 ft (n=67) |
> 3 ft, <10 ft (n=51) |
Stairs (n=37) |
|---|---|---|---|
| Soft Tissue Injury (STI) | 84 | 86 | 78 |
| Skull Fracture (Fx) | 73 | 69 | 73 |
| Skull fx w/o STI | 5 | 4 | 8 |
| Multiple Skull Fx | 8 | 10 | 8 |
| No STI and No Skull Fx (no evidence of Impact) | 12 | 8 | 14 |
| Primary Intracranial Injury | 55 | 49 | 60 |
| Primary Intracranial Injury w/o Skull Fx | 12 | 14 | 3 |
| Primary Intracranial Injury with Skull fx | 43 | 35 | 57 |
| No STI, No Skull Fx w/Primary Intracranial Injury | 6 | 2 | 0 |
| Secondary Intracranial Injury | 5 | 2 | 5 |
| ISS (range, median) |
11.1 ± 0.8 (0–26, 9) |
10.2 ± 0.9 (0–25, 9) |
10.1 ± 1.1 (0–26, 9) |
| GCS (range, median) |
14.2 ± 2.3 (3–15, 15) |
14.5 ± 2.1 (3–15, 15) |
13.8 ± 2.8 (3–15, 15) |
| 2E. Toddler Falls | ≤3 ft (n=31) |
> 3 ft, <10 ft (n=45) |
>10 ft (n=22) |
Stairs (n=30) |
|---|---|---|---|---|
| Soft Tissue Injury (STI) | 42 | 64 | 68 | 57 |
| Skull Fracture (Fx) | 23 | 49 | 50 | 33 |
| Skull fx w/o STI | 0 | 13 | 9 | 7 |
| Multiple Skull Fx | 0 | 0 | 18 | 0 |
| No STI and No Skull Fx (no evidence of Impact) | 58 | 22 | 23 | 37* |
| Primary Intracranial Injury | 42 | 36 | 31 | 30 |
| Primary Intracranial Injury w/o Skull Fx | 22.6 | 8.9 | 4.6 | 6.7 |
| Primary Intracranial Injury with Skull fx | 19 | 27 | 27 | 23 |
| No STI, No Skull Fx w/Primary Intracranial Injury | 16 | 0 | 0 | 0 |
| Secondary Intracranial Injury | 0 | 2 | 5 | 0 |
| ISS (range, median) |
8.8 ± 1.2 (0–20, 9) |
9.8 ± 1.0 (0–30, 9) |
11.6 ± 1.5 (1–30, 8.5) |
8.0 ± 1.3 (0–20, 5) |
| GCS (range, median) |
14.3 ± 2.4 (3–15, 15) |
14.2 ± 2.3 (3–15, 15) |
12.9 4.2 (3–15, 15) |
14.0 ± 2.4 (6–15, 15) |
Shaded boxes indicate values that are significantly (p<0.05) higher than all the other values in the same row except the toddler stair fall indicated with a *, which denotes a value that was not significantly different from the shaded box. ISS presented as mean ± S.E.M.
Similar to other types of falls, infants who fell down stairs were more likely to present with skull fracture compared to toddlers who fell down stairs(p<0.05) (Table 2C). However, unlike non-stair falls, an age-dependence in primary intracranial injury was noted in stair falls (59% of infants vs. 30% of toddlers (p<0.05)). In both infant and toddler stair falls the frequency of clinical signs and injuries were similar to those in low and intermediate falls (Tables 2D–E), with one exception: primary intracranial injury without external head injury was more common in toddler low falls than in toddler stair falls (16% v. 0%, p<0.05). Toddlers who fell from high heights more commonly sustained multiple skull fractures, but were otherwise similar to those who fell down stairs (Table 2E).
Association of Intracranial Injury and External Signs of Trauma
The presence of external signs of trauma did not always correlate with the presence of intracranial injury. Of the 57% of children with a skull fracture from a fall, 11.1% had no soft tissue injury by CT or physical examination. Of the 46% of children with a primary intracranial injury, 30% did not have a skull fracture and 8% had neither a skull fracture nor cranial soft tissue injury.
Extracranial Injuries
Extracranial injuries were uncommon in infants and toddlers who fell from any height. Only 2 children (0.7%) had a long bone fracture, both of whom were toddlers. One child fell out of a 2nd story window and the other fell down a flight of 14 stairs. Solid organ injury was noted in less than 2% of infants and 6% of toddlers, with the exception of toddlers who fell from high heights, in which the frequency of solid organ injury was significantly higher (27%, p<0.02). Of the less than 20% of infants (n=24) and 10% of toddlers (n=8) who received ophthalmic examinations, retinal hemorrhages were seen in 1 (4%) infants and 2 (25%) toddlers. The infant with retinal hemorrhages fell from a caregiver’s lap and was found to have scattered white centered intraretinal hemorrhage in the left eye only, in association with a large ipsilateral epidural hemorrhage that required surgical evacuation. Of the toddlers with retinal hemorrhages, 1 died from a 15-ft fall onto concrete and the other fell 8–10 ft from a deck. The toddler who died was described to have bilateral retinal hemorrhages, although no formal opthalmic exam was performed. The toddler who fell 8–10 ft had bilateral intraretinal hemorrhage in the posterior pole and also had a SDH. The Child Abuse and Neglect team at CHOP was consulted in all cases with retinal hemorrhages, except for the case in which the child died before a consult was performed. In the 2 non-fatal cases, the Child Abuse and Neglect Team performed a full evaluation for non-accidental trauma including a skeletal survey which was negative. The Child Abuse and Neglect Team determined that the injuries were consistent with the history of accidental trauma.
Discussion
With a large sample of young hospitalized children, our data suggest that in infants and toddlers, head injuries from falls are both age and mechanism dependent. When we evaluated falls across age groups, we found that both fall height and injuries differed significantly between infants and toddlers. Specifically, hospitalized infants were more likely to have fallen ≤3 ft while toddlers were more likely to have fallen >10 ft. Second, for both falls from low (≤3ft) and intermediate (>3ft and <10 ft) heights, we found a higher incidence of head soft tissue injury and skull fracture in infants compared to toddlers. Conversely, toddlers were less likely to have evidence of impact. Interestingly, GCS and ISS were not different in the two age groups, and the overwhelming majority of all patients did well clinically. Finally, we found that the incidence of primary brain injury did not differ significantly between infants and toddlers at low or intermediate fall heights, but were more common for infants who fell down stairs. The higher frequency of primary intracranial injury from infant stair falls may reflect the complexity of these events, including falls from a caregiver’s arms or crush by another individual.13
In our study, most hospitalizations were from falls <10 ft. While some authors have reported that for falls <10 ft, fall height is an important predictor of the frequency and severity of injury patterns,14,15 the data are limited. Interestingly, in our study, for falls <10 ft, fall height did not correlate with any head injury patterns in infants and very few in toddlers. With respect to these falls, our results support a previous prospective study of children <24 months in which the incidence of concussion, epidural hematoma, and linear skull fracture were not dependent on fall height in hospitalized children.8 Our study in infants and toddlers also reflects previous studies in older children and adolescents that found that both low and intermediate height falls can cause intracranial injury.15,16 In our study, toddlers who fell from high heights were more likely to have multiple skull fractures and solid organ injury compared to falls from low and intermediate heights, suggesting that injury patterns may be unique in falls >10 ft. Other researchers have suggested that high height falls are associated with higher morbidity and mortality than lower height falls. For example, Lehman and colleagues report a high incidence of morbidity in falls from 2nd story windows and balconies with a 30% ICU admission rate.17 It is unclear whether these differences are due to intracranial or multisystem injuries. Falls >15 ft are reported to result in a higher mortality rate compared to lower falls18 as well as more orthopedic and thoracic injuries, but similar incidences of intracranial injury.7 Similarly, our results suggest that falls from high heights result in unique and serious injuries, but not necessarily more severe intracranial injuries. We note that the mechanics of falls can be very complex in nature, with several variables acting together (angle of fall, landing surfaces, landing positions, etc.). Although not captured in our study (due to the lack of data in the medical records), we note that the fall angle and landing position likely play a role in the injury patterns from falls, but more detailed information about fall events is needed to evaluate the influence of these variables on injury patterns.
Although ISS did not differ between infants and toddlers for both falls from low and intermediate heights, we found a higher incidence of skull fracture and head soft tissue injury in infants compared to toddlers, which has been reported by other investigators.6,19 This may reflect a more conservative approach to hospitalization of infants after head trauma: despite the lack of severe injury, many infants are hospitalized for observation after falls. In our study, hospitalization for toddlers more commonly occurred after an intermediate to high height fall, likely because toddlers infrequently require evaluation after benign, low height falls.
Historically, falls are considered blunt impact events that result in external signs of trauma with or without intracranial injury. Our findings, however, suggest that a small but notable percentage of children with skull fractures from falls have no scalp bruising or swelling regardless of age or fall height. In addition, one third of our patients with a primary brain injury from a fall had no skull fracture and 8% had no skull fracture or soft tissue swelling. Thus our results suggest that young children can have primary intracranial injury from a fall without external signs of impact. This is important because in evaluating an injured child with a history of a fall, a perceived discrepancy between the type of injury and history provided may raise a concern of child abuse. For example, physicians may look for evidence of external trauma to corroborate a history of a fall with impact. The absence of external soft tissue swelling may be interpreted as evidence that a skull fracture is non-acute and raise the suspicion of abuse. Alternately, the absence of any external sign of impact (i.e. no soft tissue swelling and no skull fracture) in a child with intracranial injury may be deemed inconsistent with injuries resulting from a fall. Our findings suggest that this is not true. We recognize, however, that victims of abusive head trauma may present for medical care with intracranial injury in the absence of external signs of trauma, and that non-contact mechanisms of injury are commonly identified in victims of child abuse.23,24 Because we have not compared abused and unintentionally injured children in this study, we can not comment on the predictive value of identifying intracranial injury in the absence of external signs of trauma. Therefore, it is important not to take this finding out of context, but to recognize simply that contact injuries can sometimes result in intracranial injury in the absence of obvious external cranial injuries. Finally, however, we believe this necessitates consideration when evaluating injury mechanisms in infants and young children, and we caution against assuming an inflicted mechanism simply because evidence of cranial impact is absent. We note that this phenomenon may not just be limited to young children. However our study focused on infants and toddlers, and further data is needed to support this conclusion in a wider age range.
Our study has limitations associated with the patient population and reliability of details reported in the history. By including only patients who had an MRI or CT scan and were admitted to a tertiary care children’s hospital, our study is likely biased towards a younger or more severely injured patient population. As such, the results may not be generalizable to all accidental falls in young children and should be interpreted in the context of hospitalized children for whom imaging was performed. Second, because of the retrospective nature of our study, we relied on the data reported in medical records. Not all variables were well documented and the variables that were documented rely on an accurate report of the details of the event. Finally, our study excludes cases suspected of non-accidental trauma. It is possible that cases of child abuse were misclassified and included as unintentional in this study. Alternately, cases are sometimes determined to be suspicious for abuse because the observed injuries are more severe than what might be expected in an accidental scenario, causing patients with severe accidental injuries to be excluded. However, in this study less than 7% of patients with an accidental fall E-code were excluded because of suspected abuse so contributions from this limitation are likely minimal, but should still be noted.
Despite our limitations, the results of this study show that head injury patterns vary by age and mechanism in a cohort of infants and toddlers with accidental head trauma from falls. Although fall types differ between infants and toddlers, even within a given fall type, some age-related differences in resulting injury exist. When interpreting a fall history, clinicians must consider not only the mechanism of injury, but the influence of age on resulting injury. For these young children, intracranial injury is not always accompanied by external manifestations of their injury.
Therefore, when evaluating infants and toddlers for possible abuse, caution should be taken when assessing the veracity of a caregiver’s history, based on injury pattern alone.
HIGHLIGHTS REVISED.
Head injury patterns vary by age and mechanism in infants and toddlers with accidental head trauma from falls.
The presence of intracranial injury cannot be predicted from altered mental status or external signs of trauma.
Intracranial injury is not always accompanied by external manifestations of their injury.
For similar ISS and admission GCS, toddlers more commonly had altered mental status than infants.
In contrast, infants more commonly had skull fracture and scalp/facial soft tissue injury than toddlers.
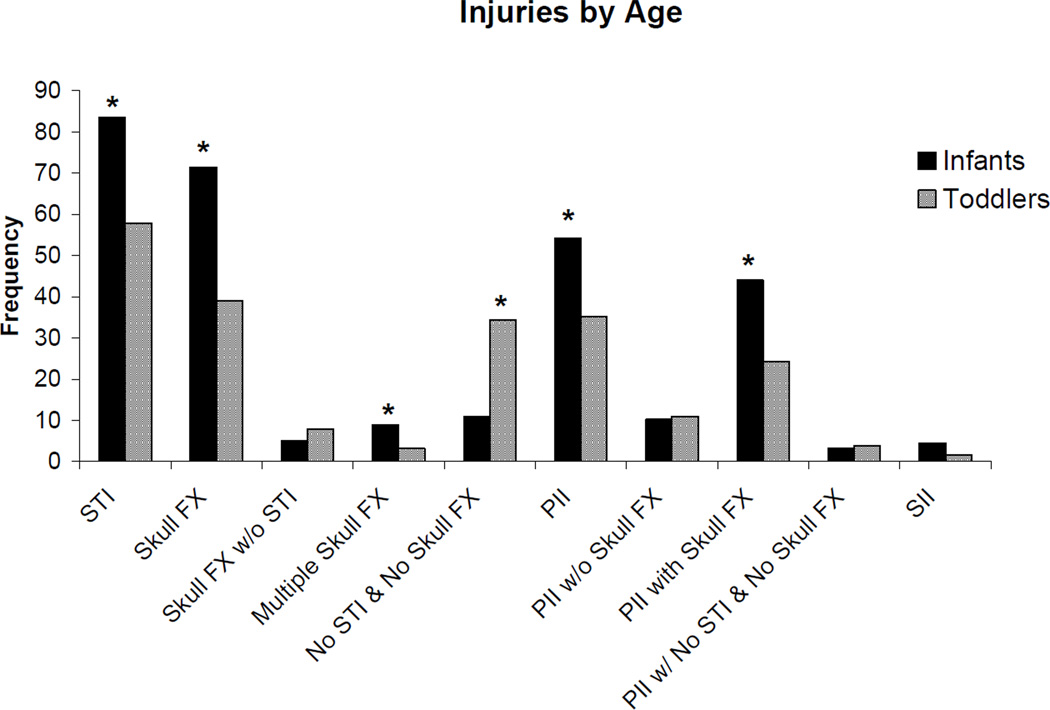
Figure 1.
Incidences of injury types by age group in young children. STI=Scalp/facial Soft Tissue Injury, PII=Primary Intracranial Injury, SII=Secondary Intracranial Injury. * indicate significantly different groups (p<0.05)
Table 3.
Classification of primary and secondary intracranial injuries in infants and toddlers.
| Analysis Categories | Signs and Symptoms | Infants (%) | Toddlers (%) |
|---|---|---|---|
| Primary Intracranial Injuries | Epidural Hematoma | 16 | 21 |
| (10) | (16) | ||
| Sudural Hematoma | 47 | 19 | |
| (30) | (15) | ||
| Subarachnoid | 24 | 4 | |
| Hemorrhage | (15) | (3) | |
| Intraventricular | 0 | 0 | |
| Hemorrhage | (0) | (0) | |
| Parenchymal | 5 | 12 | |
| Contusion/laceration | (3) | (9) | |
| Intraparenchymal | 6 | 5 | |
| Hemorrhage | (4) | (4) | |
| Diffuse Axonal Injury | 2 | 0 | |
| (1) | (0) | ||
| Secondary Intracranial Injuries |
Loss of Grey/White | 3 | 0 |
| Matter Diff | (2) | (0) | |
| Ischemia/Infarct | 4 | 0 | |
| (3) | (0) | ||
| Cerebral Edema | 2 | 2 | |
| (1) | (2) | ||
Acknowledgements
We acknowledge Dr. Michael Nance for the use of the Trauma Registry Database at CHOP. This work was funded by NSF through the Center for Child Injury Prevention Studies (CChIPS) and NINDS (NIH RO1NS 39679).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Nicole G. Ibrahim, Department of Bioengineering, University of Pennsylvania, Philadelphia, PA USA, 19104,Present address: US Food and Drug Administration, Silver Spring MD USA 20993 (nicole.ibrahim@fda.hhs.gov)
Joanne Wood, Department of Pediatrics, Children’s Hospital of Philadelphia, Philadelphia, PA USA, 19104 (woodjo@email.chop.edu).
Susan S. Margulies, Department of Bioengineering, University of Pennsylvania, Philadelphia, PA USA, 19104, (Margulies@seas.upenn.edu)
Cindy W. Christian, Department of Pediatrics, Children’s Hospital of Philadelphia, Philadelphia, PA USA, 19104 (Christian@email.chop.edu)
References
- 1.CDC National Vital Statistics Report. 2004 Report No.: Vol 52, Num 21. [Google Scholar]
- 2.Schutzman SA, Greenes DS. Pediatric minor head trauma. Ann Emerg Med. 2001;37(1):65–74. doi: 10.1067/mem.2001.109440. [DOI] [PubMed] [Google Scholar]
- 3.Agran PF, et al. Rates of pediatric injuries by 3-month intervals for children 0 to 3 years of age. Pediatrics. 2003;111(6 Pt 1):e683–e692. doi: 10.1542/peds.111.6.e683. [DOI] [PubMed] [Google Scholar]
- 4.Spady DW, et al. Patterns of injury in children: a population-based approach. Pediatrics. 2004;113(3 Pt 1):522–529. doi: 10.1542/peds.113.3.522. [DOI] [PubMed] [Google Scholar]
- 5.Holsti M, et al. Pediatric closed head injuries treated in an observation unit. Pediatr Emerg Care. 2005;21(10):639–644. doi: 10.1097/01.pec.0000181426.25342.a9. [DOI] [PubMed] [Google Scholar]
- 6.Lallier M, et al. Falls from heights among children: a retrospective review. J Pediatr Surg. 1999;34(7):1060–1063. doi: 10.1016/s0022-3468(99)90564-x. [DOI] [PubMed] [Google Scholar]
- 7.Wang MY, et al. Injuries from falls in the pediatric population: an analysis of 729 cases. J Pediatr Surg. 2001;36(10):1528–1534. doi: 10.1053/jpsu.2001.27037. [DOI] [PubMed] [Google Scholar]
- 8.Duhaime A, et al. Head injury in very young children: Mechanisms, injury types, and ophthalmologic findings in 100 hospitalized patients under two years of age. Pediatrics. 1992;90(2):179–185. [PubMed] [Google Scholar]
- 9.Ewing-Cobbs L, et al. Neuroimaging, physical, and developmental findings after inflicted and noninflicted traumatic brain injury in young children. Pediatrics. 1998;102(2 Pt 1):300–307. doi: 10.1542/peds.102.2.300. [DOI] [PubMed] [Google Scholar]
- 10.Chadwick DL, et al. Deaths from falls in children: how far is fatal? J Trauma. 1991;31(10):1353–1355. doi: 10.1097/00005373-199110000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Hennrikus WL, et al. Injuries when children reportedly fall from a bed or couch. Clin Orthop. 2003;407:148–151. doi: 10.1097/00003086-200302000-00022. [DOI] [PubMed] [Google Scholar]
- 12.Pickett W, et al. Injuries experienced by infant children: a population-based epidemiological analysis. Pediatrics. 2003;111(4 Pt 1):e365–e370. doi: 10.1542/peds.111.4.e365. [DOI] [PubMed] [Google Scholar]
- 13.Chiaviello CT, et al. Stairway-related injuries in children. Pediatrics. 1994;94(5):679–681. [PubMed] [Google Scholar]
- 14.Johnson K, et al. Accidental head injuries in children under 5 years of age. Clin Radiol. 2005;60(4):464–468. doi: 10.1016/j.crad.2004.09.013. [DOI] [PubMed] [Google Scholar]
- 15.Park SH, et al. Head injuries from falls in preschool children. Yonsei Med J. 2004;45(2):229–232. doi: 10.3349/ymj.2004.45.2.229. [DOI] [PubMed] [Google Scholar]
- 16.Murray JA, et al. Pediatric falls: is height a predictor of injury and outcome? Am Surg. 2000;66(9):863–865. [PubMed] [Google Scholar]
- 17.Lehman D, Schonfeld N. Falls from heights: a problem not just in the northeast. Pediatrics. 1993;92(1):121–124. [PubMed] [Google Scholar]
- 18.Kim KA, et al. Analysis of pediatric head injury from falls. Neurosurgical Focus. 2000;8(1):e3. doi: 10.3171/foc.2000.8.1.154. [DOI] [PubMed] [Google Scholar]
- 19.Chang LT, Tsai MC. Craniofacial injuries from slip, trip, and fall accidents of children. J Trauma. 2007;63(1):70–74. doi: 10.1097/01.ta.0000219142.15584.b8. [DOI] [PubMed] [Google Scholar]
- 20.Arbogast KB, et al. Initial neurologic presentation in young children sustaining inflicted and unintentional fatal head injuries. Pediatrics. 2005;116(1):180–184. doi: 10.1542/peds.2004-2671. [DOI] [PubMed] [Google Scholar]
- 21.Durham SR, et al. CHOP Infant Coma Scale ("Infant Face Scale"): a novel coma scale for children less than two years of age. J Neurotrauma. 2000;17(9):729–737. doi: 10.1089/neu.2000.17.729. [DOI] [PubMed] [Google Scholar]
- 22.Reilly PL, et al. Children's Hospital A. Assessing the conscious level in infants and young children: a paediatric version of the Glasgow Coma Scale. Childs Nerv Syst. 1988;4(1):30–33. doi: 10.1007/BF00274080. [DOI] [PubMed] [Google Scholar]
- 23.Hymel KP, et al. Mechanisms, clinical presentations, injuries, and outcomes from inflicted versus noninflicted head trauma during infancy: results of a prospective, multicentered, comparative study. Pediatrics. 2007;119(5):922–929. doi: 10.1542/peds.2006-3111. [DOI] [PubMed] [Google Scholar]
- 24.Starling SP, et al. Analysis of perpetrator admissions to inflicted traumatic brain injury in children. Arch Pediatr Adolesc Med. 2004;158(5):454–458. doi: 10.1001/archpedi.158.5.454. [DOI] [PubMed] [Google Scholar]