Abstract
Background
Emergency medical services (EMS) personnel commonly encounter sepsis, yet little is known about their understanding of sepsis.
Study Objectives
To determine the awareness, knowledge, current practice, and attitudes about sepsis among EMS personnel.
Methods
We performed an anonymous, multi-agency, online survey of emergency medical technicians (EMTs), firefighter-emergency medical technicians (FF-EMTs), and paramedics in a metropolitan, 2-tier EMS system.
We compared responses according to the level of EMS training, and used multivariable logistic regression to determine the odds of correctly identifying the definition of sepsis, independent of demographic and professional factors.
Results
Overall response rate of study participants was 57% (786/1390), and greatest among EMTs (78%; 276/350). A total of 761 respondents (96%) had heard of the term sepsis. EMTs and FF-EMTs were at significantly reduced odds of correctly defining sepsis compared to paramedics, independent of age, sex, and years of experience (EMTs, OR=0.44, 95%CI:0.3,0.8; FF-EMTs, OR=0.32, 95%CI:0.2,0.6,). Overall, knowledge of the clinical signs and symptoms and recommended treatments for sepsis was typically greater than 75%, though best among paramedics than EMTs or FF-EMTs (p<0.01). The majority of respondents believed sepsis is not recognized by EMS “some” or “a lot” of the time (76%, 596/786).
Conclusions
EMS personnel demonstrated an overall sound awarenessof sepsis. Knowledge of sepsis was less among firefighter-EMTs and EMTs compared to paramedics. These results suggest that paramedics could be integrated into strategies of early identification and treatment of sepsis while EMTs may benefit from focused education and training.
Keywords: emergency medical services, education, sepsis
Introduction
Emergency medical services (EMS) providers are important for the recognition and treatment of patients with critical illness. During out-of-hospital care, both paramedics and emergency medical technicians (EMTs) identify patients with critical cardiovascular diseases such as ST-segment elevation myocardial infarction and stroke, using both subjective and objective criteria. These criteria include historical features, such as dyspnea and chest pain, clinical findings, or triage tools like the 12-lead electrocardiograms and stroke scales.(1-7) Through out-of-hospital recognition, EMS providers initiate a cascade of critical care that improves both system efficiency and clinical outcomes.(8-10)
Out-of-hospital providers also commonly encounter patients with sepsis, a syndrome with a hospital mortality that exceeds myocardial infarction and stroke.(11) Objective, physiologic findings during out-of-hospital care of patients with sepsis are heterogeneous, and not specific to patients with infection and inflammatory response.(12) As such, EMS providers’ knowledge and awareness of sepsis may play a key role in pre-hospital recognition and care. Potential roles for EMS in the care of patients with sepsis may include both diagnostic and therapeutic interventions. Prognostic markers, such as pre-hospital lactate, may be measured among patients at greatest risk for sepsis, and subsequently used for advanced hospital notification or to guide early treatment.(13) Observational data suggests that delivery of fluid resuscitation during out-of-hospital care of patients with sepsis may improve early resuscitation in the emergency department.(14)
Thus, EMS providers’ awareness and knowledge of sepsis could play an essential role in these early care pathways. Yet, little is known about the clinical acumen of EMS providers regarding their understanding of sepsis.(15) We conducted a survey investigation to determine the understanding of sepsis among EMT and paramedic EMS providers. We hypothesized that paramedics would demonstrate greater clinical knowledge of the definition and signs and symptoms of sepsis compared to EMTs or fire-fighter EMTs, independent of demographic and experiential factors.
Materials and methods
Study design
We conducted an anonymous, on-line survey measuring the awareness, knowledge, and attitudes about sepsis among EMS providers. Participating EMS providers, including paramedics, fire-fighter-emergency medical technicians (FF-EMT), and privateemergency medical technicians (EMT), were recruited from the three largest EMS agencies in King County, Washington. Participants were identified through local EMS directors.
Measures
We developed the questionnaire using content from previously published surveys of the general publics’ and physicians’ knowledge and awareness of sepsis.(16, 17) Twelve items were reviewed by a focus group of three EMS directors,one emergency medicine physician, ten intensivists, and two senior paramedics. This group was chosen because they would not otherwise be included in the main study population, but their medical practices and training programs commonly involve emergency care of patients with sepsis. Using feedback from the group, the questionnaire was revised to contain 10 questions (shown in supplemental Appendix). Our final survey included questions which focus on the awareness and recognition of sepsis, the comparative mortality of sepsis with other critical conditions, and how often EMS providers failed to recognize sepsis. We assessed knowledge ofsepsis practice and frequent treatments used by EMS personnel in additional questions. We also assessed respondents’ attitudes about the role of EMS in diagnosis and treatment of patients with sepsis. Response options included Likert-type scales and dichotomized “yes/no” options. We also included questions to assess respondents’ demographic and professional characteristics (e.g. age, gender, years of experience at current EMS position).
Data collection and recruitment
Data were collected between March 2009 and February 2010. Study staff contacted EMS directors to request internal distribution of an email invitation to participants. This email included an anonymous link to the secure study website (Catalyst Web Tools©, University of Washington). Because responses were anonymous, we were unable to identify those individuals who had not returned surveys for reminders or who had submitted duplicate responses. Therefore, we contacted all participants after two and four weeks with thank you/reminder emails. Access to the survey website was closed 6 weeks after survey distribution. No incentives were offered. Non-responses were coded as missing data, and respondents were unable to go back and correct questions during the survey procedure.
Statistical analysis
We compared survey responses across three categories of EMS training: 1) paramedic, 2) FF-EMT, and 3) EMT. We present continuous data (age, years of experience) as medians with interquartile range [IQR] due to deviations from normality as assessed from graphical distributions. We compared continuous variables across categories using Kruskal Wallis rank test. We present categorical survey responses as proportions, and analyzed using both omnibus and pairwise χ2 tests. Omnibus tests were used for overall comparisons of awareness and definitional accuracy. A priori, we hypothesized that differences in knowledge of sepsis's signs and symptoms would occur between paramedics and both FFEMTs and EMTs due to extent of training. We used pairwise χ2tests for these comparisons. To determine the independent association between level of training and recognition of the correct definition of sepsis, we developed a multivariable logistic regression using level of training as the independent variable and a correct answer to question #3 (“Which of the following is the correct definition of sepsis?”) as the dependent variable. We included a priori confounders, age, gender, and years of experience, in the model. We used the Huber-White estimator to generate standard errors for regression coefficients. All tests for statistical significance were two tailed (p<0.05), and we conducted all analyses were using STATA version 10.0 (StataCorp, College Station, TX). This study was approved by the University of Washington Institutional Review Board.
Results
Respondents
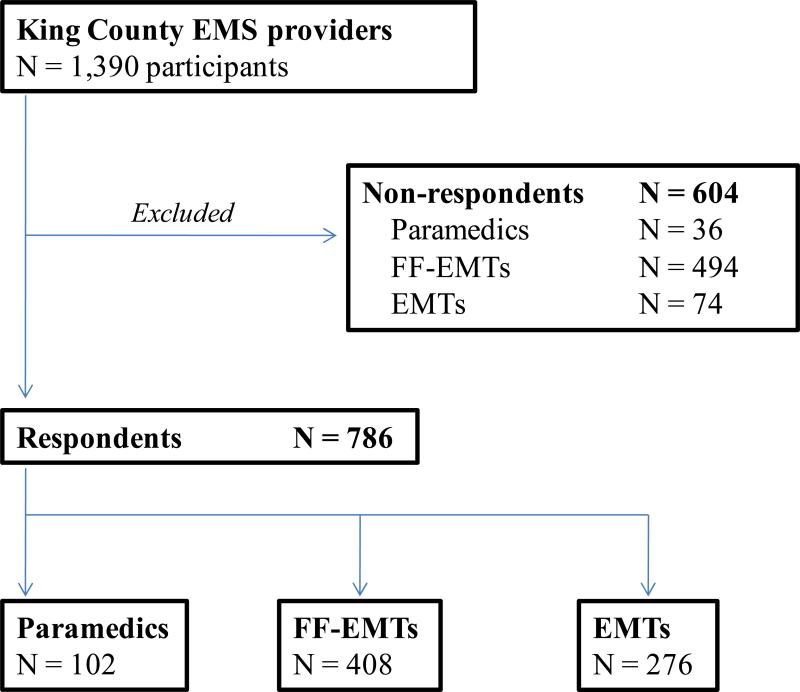
Of the 1,390 individuals contacted (Figure 1), 786 EMS providers responded to the survey (57%). The majority of participants were fire-fighter EMTs (52%), compared to paramedics (13%) or EMTs (21%). Male gender was common among all providers (Table 1), with a greatest proportion among FF-EMTs (89%). Median age was 42 years [IQR: 33 – 49 yrs], and significantly lower among responding EMTs (31 years [IQR: 26 – 41 yrs], p<0.01). We observed that median years of experience at their current EMS position was highest among FF-EMTs (16 yrs [IQR: 10-22 yrs]) and significantly shorter among EMTs (5 yrs [IQR: 2-14 yrs], p<0.01).
Figure 1.
Respondent accrual. Abbreviations: FF-EMTs = firefighter emergency medical technicians, EMTs = emergency medical technicians
Table 1.
Respondent characteristics
| Characteristic | Total | Paramedic | Fire-fighter-EMTs | EMTs | P value* |
|---|---|---|---|---|---|
| Total respondents, N | 786 | 102 | 408 | 276 | |
| Median age, yrs [IQR] | 42 [33-49] | 47 [40-52] | 45 [39-51] | 31 [26-41] | <0.01 |
| Male gender, N (%) | 647 (82) | 86 (84) | 364 (89) | 197 (71) | <0.01 |
| Median years experience at EMS position, [IQR] | 13 [5-20] | 14 [9-21] | 16 [10-22] | 5 [2-14] | <0.01 |
Comparisons across groups using Kruskal-Wallis rank test and χ2 test, as appropriate
Awareness
Most respondents (97%) had heard of sepsis (Table 2), and the majority correctly identified sepsis as having greater hospital mortality than stroke (87%), myocardial infarction (94%), or trauma (76%). Notably, 36% of FF-EMTs incorrectly identified myocardial infarction and 21% of EMTs identified stroke as having a greater mortality than sepsis, respectively. Most respondents correctly identified cardiac arrest with greater comparative mortality than sepsis (76%, 603 of 786).
Table 2.
Out-of-hospital providers’ awareness of sepsis^
| Question | Total (N=786) | Paramedics (N=102) | Fire-fighter-EMTs (N=408) | EMTs (N=276) | P value* |
|---|---|---|---|---|---|
| Q1: Have you heard of the term sepsis? | |||||
| Yes | 761 (97) | 102 (100) | 386 (95) | 273 (99) | 0.016 |
| No | 12 (2) | 0 (0) | 12 (3) | 0 (0) | . |
| Not sure | 12 (2) | 0 (0) | 9 (2) | 3 (1) | . |
| Q2: Does any of these conditions have a greater mortality than sepsis? | |||||
| Traumatic injury | 186 (24) | 20 (20) | 91 (22) | 75 (27) | <0.01 |
| Stroke | 99 (13) | 8 (8) | 35 (9) | 56 (21) | <0.01 |
| **Cardiac arrest | 603 (76) | 88 (86) | 297 (73) | 218 (79) | <0.01 |
| Myocardial infarction | 48 (6) | 17 (17) | 148 (36) | 8 (3) | <0.01 |
| Q3: Which of the following is the definition of sepsis? | |||||
| Allergy | 0 (0) | 0 (0) | 0 (0) | 0 (0) | <0.01 |
| Suspicion or presence of infection | 215 (27) | 13 (13) | 102 (25) | 100 (36) | . |
| **Suspicion or presence of infection with inflammatory response | 501 (64) | 83 (81) | 261 (64) | 157 (57) | . |
| Not sure | 16 (2) | 0 (0) | 9 (2) | 7 (3) | . |
| Other | 41 (5) | 6 (6) | 23 (6) | 12 (4) | . |
| Q4: Is the definition of sepsis commonly accepted within your specialty? | |||||
| Yes | 423 (54) | 51 (50) | 176 (43) | 196 (71) | <0.01 |
| Not sure | 149 (19) | 38 (37) | 72 (18) | 39 (14) | . |
| Not sure | 200 (25) | 13 (13) | 147 (36) | 40 (14) | . |
| Q5: How often is the diagnosis of sepsis missed by EMS providers? | |||||
| A lot of the time | 284 (36) | 33 (33) | 163 (40) | 88 (32) | <0.01 |
| Some of the time | 312 (40) | 51 (50) | 143 (35) | 118 (43) | . |
| A little of the time | 99 (13) | 18 (18) | 41 (10) | 40 (14) | . |
| None of the time | 7 (1) | 0 (0) | 3 (1) | 4 (1) | . |
| Not sure | 15 (2) | 0 (0) | 14 (3) | 1 (<1) | . |
All results presented as N (%), correct answer marked by double asterisk for questions 2 and 3
Chi-square test of significance comparing responses across three groups (P, FF-EMTs, and EMTs)
Knowledge
Respondents knowledge of the correct definition of sepsis (“Suspicion or presence of infection with inflammatory response”) was robust, identified by 83 of 102 paramedics (81%, 95%CI: 72, 88%), 261 of 408 FF-EMTs (64%, 95%CI: 59, 69%), and 157 of 276 EMTs (57%, 95%CI: 51, 63%). In a multivariable logistic regression model, we observed that both EMTs (OR=0.32, 95%CI: 0.18, 0.58) and FF-EMTs (OR=0.44, 95%CI: 0.25, 0.75) were at significantly lower odds of correctly identifying the definition of sepsis compared to paramedics (p<0.01 for both). This association was independent of provider age, gender, and years of experience at current EMS position, none of which were significantly associated with correct definitional awareness (p>0.05 for all). A majority of paramedics (63%), FFEMTs (82%), and EMTs (86%) responded that the 2001 Consensus Conference definition of sepsis was accepted by their specialty.
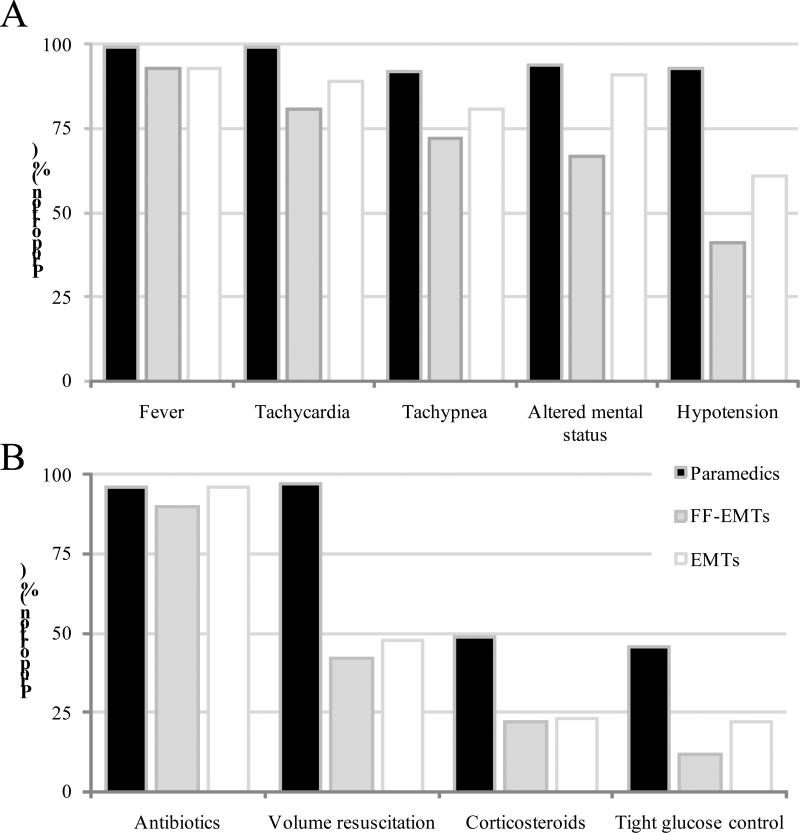
In general, paramedics’, EMTs’, and FF-EMTs’ knowledge of common clinical signs and symptoms was good (Figure 2). Over half of all respondents identified fever, tachycardia, tachypnea, and altered mental status as signs which increase their suspicion for sepsis. A greater proportion of paramedics selected these clinical signs, compared to EMTs and FF-EMTs, except for altered mental status. FFEMTs were less likely, on average, to select hypotension as a sign which increased their suspicion for sepsis (41%, N=160). Even though the majority answered correctly regarding knowledge and clinical sign/symptoms of sepsis, most of respondents suggested that the diagnosis of sepsis was missed some or a lot of the time (76%, N=596 of 786). Respondents less commonly identified, on average, the currently recommended treatments for sepsis, with only antibiotics identified by a majority (Figure 2). Among paramedics, the recommendations for volume resuscitation, corticosteroids, and tight glucose control were identified twice as often than by FF-EMTs or EMTs (p<0.01 for each).
Figure 2.
(A) Proportion of EMS providers identifying clinical signs and symptoms of sepsis, (B) Proportion of EMS providers identifying recommended treatments for sepsis. All tests of significance (PM vs. EMTs; PM vs. FF-EMTs) are p<0.05, except comparing P vs. EMTs for altered mental status (p=0.37) and antibiotics (p=0.85).
Current practice
Among paramedics, 98% (N=100) reported routine use of intravenous access, and 99% (N=101) reported routine delivery of intravenous fluid prior to hospital arrival in patients with suspected sepsis. Paramedics, on average, self-reported delivering > 1.5 liters (35%) of fluid compared to <0.5 liters (2%), 0.5-1.0 liters (30%), or 1.1-1.5 liters (18%).Fewer paramedics reported routine use of diuretics (2%) or vasopressors (46%) when caring for patients with suspected sepsis.
Attitudes
Most respondents agreed (55%) or strongly agreed (26%) that paramedics can identify patients at great risk for sepsis. EMTs most commonly endorsed these choices (92% with either), compared to FF-EMTs (75%) or paramedics (69%). EMTs also most commonly agreed that out-of-hospital providers may improve outcomes in sepsis (42% agreed, 38% strongly agreed), while paramedics were most likely to be unsure (25%) or disagree (15%).
Discussion
In a multi-agency survey of EMS providers, we observed that most respondents recognized the term “sepsis”, and could correctly identify the definition and its associated signs, symptoms, and treatments. Paramedics had, on average, a better understanding of sepsis than FF-EMTs and EMTs. Yet, we found that most out-of-hospital providers believed the diagnosis of sepsis is missed during out-of-hospital care. Our results suggest that future research is needed to understand how the role of paramedics could be enhanced in sepsis, while additional training and education may be needed for first responders.
Despite an excessive mortality and evidence supporting early, aggressive treatment, sepsis patients are not typically well-integrated into EMS evaluation and care, in comparison to other conditions such as ST-elevation myocardial infarction or stroke.(19-24) There may be multiple barriers preventing greater participation by EMS, including inadequate understanding of sepsis by EMS as well as insufficient appreciation for the optimal EMS role in early triage and care for sepsis patients.(15) The current investigation focused on the EMS understanding of sepsis. Because sepsis will present with significant heterogeneity in the field, without a specific disease-defining symptom or time course, broad knowledge of common signs and symptoms is essential if pre-hospital providers are to effectively identify and treat possible patients at risk for sepsis.(25) While this heterogeneity in presentation challenges accurate recognition, many EMS providers in this survey correctly identified a potential range of presenting signs and symptoms.
The findings may support a more active role by paramedics in the care of sepsis. The acceptable level of understanding and knowledge of sepsis by paramedics provides support for more detailed research into methods to refine case recognition, triage, and treatment. Examples of such research could include efforts to improve triage models for out-of-hospital critical illness based upon objective findings.(26) Implementation studies of these triage tools may involve alternate destinations of care, where greater volume centers may lead to improved outcomes in sepsis.(27) Paramedics’ recognition of patients at greatest risk of sepsis would be essential to facilitate studies which evaluate point-of-care diagnostics during pre-hospital care. Early recognition of sepsis by paramedics will support greater study of field treatments which are adapted from emergency department or hospital-based guidelines.(14, 28) Important early steps to consider include descriptive epidemiology and observational studies of EMS treatment for highest risk sepsis patients.Taken together, paramedics’ robust awareness and knowledge of sepsis provides a foundation for research into many knowledge gaps in early sepsis care.
However, we observed differences in the knowledge of sepsis clinical features and treatments when comparing paramedics to EMTs or FF-EMTs.Although this may be expected given the differences in training and responsibilities, the role of EMTs is essential as their subjective assessments may play a key role in proper triage.(29) For example, EMTs may cancel paramedic (e.g. Advanced Life Support) responses en route, despite the presence of potentially serious chief complaints or abnormal vitals signs, thus limiting the benefits of EMS involvement.(30) Alternatively EMTs can have a beneficial role in early identification as evidenced by successful triage of stroke and traumatic injury by EMTs and FFEMTs.(7, 31)
As such, the current study results suggest an opportunity to improve training and education, particularly among first responders. Greater education could involve empiric, diagnostic protocols, simulation of sepsis scenarios, or system-level toolkits.(15,32,33) Similar education interventions were developed in ST-elevation MI and stroke, leading to greater efficiency of out-of-hospital diagnosis and treatment.(33,34) Because nearly 90% of the general public has never heard the term “sepsis,” EMS providers may also play a key role in communication to patients and families.(16) With further training, EMTs could participate in community outreach programs, similar to stroke and cardiac arrest, while also providing useful information for patients or families during initial care.(35, 36) We also found that EMTs had greater relative confidence in paramedicsin their ability to improve the care of sepsis patients. Ultimately, a broader sense of patient acuity and well-defined responsibilities among EMTs may create a more integrated system of emergency care for sepsis patients.
Limitations
We recognize several limitations to our study. Our response rate was modest, and data may not reflect the knowledge and awareness of non-respondents. The response rate was typical of physician surveys, and is much greater than other web or paper-based EMS surveys.(37,38) Although our anonymous design limits the objective assessment of response bias, we observed a broad range in demographic and professional characteristics among respondents. Another limitation in our design was the absence of case-based scenarios. Clinical scenarios may test how EMS providers operationalize their knowledge, or provide context to knowledge questions; however, we emphasized brief survey length to improve participation. Our findings may not be generalizable to all EMS systems, particularly those with different organizational characteristics (e.g. 1-tier), rural geography, or different training curricula. Yet, we queried three types of EMS providers from multiple agencies with distinct EMS leadership, continuing medical education, and catchment areas in King County. We also cannot identify if cheating behavior modified the performance of respondents, including submission of duplicate responses. Because cheating is most common among unproctored internet tests with high extrinsic motivation or situational pressures, we do notbelieve this issue contributed importantly to our results.(39) The current study did not assess challenges related to how EMS identification and care should be effectively integrated into a regional system of hospital care. Future studies which evaluate the impact of EMS provider knowledge and treatment of sepsis will require outcome assessment over the entire critical care delivery system, from out-of-hospital encounters through hospital-based intensive care.
Conclusions
In a multi-agency survey, we observed a sound understanding of sepsis among EMS personnel. Knowledge of clinical characteristics and treatment of sepsis was greatest among paramedics, compared to firefighter-EMTs and EMTs. Taken together, these results suggest that paramedics could be integrated into strategies of early identification and treatment of sepsis while EMTs may benefit from focused education and training.
Acknowledgements
We would like to acknowledge the contribution of the paramedics, emergency medical technicians, and firefighter-emergency medical technicians who gratefully participated in this survey.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Meisel ZF, Pollack CV, Mechem CC, et al. Derivation and internal validation of a rule to predict hospital admission in prehospital patients. Prehosp Emerg Care. 2008;12(3):314–319. doi: 10.1080/10903120802096647. [DOI] [PubMed] [Google Scholar]
- 2.Weaver WD, Eisenberg MS, Martin JS, et al. Myocardial Infarction Triage and Intervention Project--phase I: patient characteristics and feasibility of prehospital initiation of thrombolytic therapy. J Am Coll Cardiol. 1990;15(5):925–931. doi: 10.1016/0735-1097(90)90218-e. [DOI] [PubMed] [Google Scholar]
- 3.Aufderheide TP, Hendley GE, Thakur RK, et al. The diagnostic impact of prehospital 12-lead electrocardiography. Ann Emerg Med. 1990;19(11):1280–1287. doi: 10.1016/s0196-0644(05)82288-7. [DOI] [PubMed] [Google Scholar]
- 4.Kudenchuk PJ, Maynard C, Cobb LA, et al. Utility of the prehospital electrocardiogram in diagnosing acute coronary syndromes: the Myocardial Infarction Triage and Intervention (MITI) Project. J Am Coll Cardiol. 1998;32(1):17–27. doi: 10.1016/s0735-1097(98)00175-2. [DOI] [PubMed] [Google Scholar]
- 5.Chenkin J, Gladstone DJ, Verbeek PR, et al. Predictive value of the Ontario prehospital stroke screening tool for the identification of patients with acute stroke. Prehosp Emerg Care. 2009;13(2):153–159. doi: 10.1080/10903120802706146. [DOI] [PubMed] [Google Scholar]
- 6.Kidwell CS, Starkman S, Eckstein M, et al. Identifying stroke in the field. Prospective validation of the Los Angeles prehospital stroke screen (LAPSS). Stroke. 2000;31(1):71–76. doi: 10.1161/01.str.31.1.71. [DOI] [PubMed] [Google Scholar]
- 7.Kothari R, Barsan W, Brott T, et al. Frequency and accuracy of prehospital diagnosis of acute stroke. Stroke. 1995;26(6):937–941. doi: 10.1161/01.str.26.6.937. [DOI] [PubMed] [Google Scholar]
- 8.Ghosh R, Pepe P. The critical care cascade: a systems approach. Curr Opin Crit Care. 2009;15(4):279–283. doi: 10.1097/MCC.0b013e32832faef2. [DOI] [PubMed] [Google Scholar]
- 9.Mosley I, Nicol M, Donnan G, et al. The impact of ambulance practice on acute stroke care. Stroke. 2007;38(10):2765–2770. doi: 10.1161/STROKEAHA.107.483446. [DOI] [PubMed] [Google Scholar]
- 10.Sivagangabalan G, Ong AT, Narayan A, et al. Effect of prehospital triage on revascularization times, left ventricular function, and survival in patients with ST-elevation myocardial infarction. Am J Cardiol. 2009;103(7):907–912. doi: 10.1016/j.amjcard.2008.12.007. [DOI] [PubMed] [Google Scholar]
- 11.Wang HE, Weaver MD, Shapiro NI, et al. Opportunities for Emergency Medical Services care of sepsis. Resuscitation. 81(2):193–197. doi: 10.1016/j.resuscitation.2009.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Seymour CW, Band RA, Cooke CR, et al. Out-of-hospital characteristics and care of patients with severe sepsis: A cohort study. J Crit Care. 2010 doi: 10.1016/j.jcrc.2010.02.010. [EPUB] Apr 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jansen TC, van Bommel J, Mulder PG, et al. The prognostic value of blood lactate levels relative to that of vital signs in the pre-hospital setting: a pilot study. Crit Care. 2008;12(6):R160. doi: 10.1186/cc7159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Seymour CW, Cooke CR, Mikkelsen ME, et al. Out-of-hospital fluid in severe sepsis: effect on early resuscitation in the emergency department. Prehosp Emerg Care. 14(2):145–152. doi: 10.3109/10903120903524997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Robson W, Nutbeam T, Daniels R. Sepsis: a need for prehospital intervention? Emerg Med J. 2009;26(7):535–538. doi: 10.1136/emj.2008.064469. [DOI] [PubMed] [Google Scholar]
- 16.Rubulotta FM, Ramsay G, Parker MM, et al. An international survey: Public awareness and perception of sepsis. Crit Care Med. 2009;37(1):167–170. doi: 10.1097/ccm.0b013e3181926883. [DOI] [PubMed] [Google Scholar]
- 17.Poeze M, Ramsay G, Gerlach H, et al. An international sepsis survey: a study of doctors’ knowledge and perception about sepsis. Crit Care. 2004;8(6):R409–413. doi: 10.1186/cc2959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Levy MM, Fink MP, Marshall JC, et al. 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Intensive Care Med. 2003;29(4):530–538. doi: 10.1007/s00134-003-1662-x. [DOI] [PubMed] [Google Scholar]
- 19.Wang HE, Devereaux RS, Yealy DM, et al. National variation in United States sepsis mortality: a descriptive study. Int J Health Geogr. 2010;9:9. doi: 10.1186/1476-072X-9-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Johnson NJ, Backlund E, Sorlie PD, et al. Marital status and mortality: the national longitudinal mortality study. Ann Epidemiol. 2000;10(4):224–238. doi: 10.1016/s1047-2797(99)00052-6. [DOI] [PubMed] [Google Scholar]
- 21.Angus DC, Linde-Zwirble WT, Lidicker J, et al. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med. 2001;29(7):1303–1310. doi: 10.1097/00003246-200107000-00002. [DOI] [PubMed] [Google Scholar]
- 22.Rivers E, Nguyen B, Havstad S, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345(19):1368–1377. doi: 10.1056/NEJMoa010307. [DOI] [PubMed] [Google Scholar]
- 23.Otero RM, Nguyen HB, Huang DT, et al. Early goal-directed therapy in severe sepsis and septic shock revisited: concepts, controversies, and contemporary findings. Chest. 2006;130(5):1579–1595. doi: 10.1378/chest.130.5.1579. [DOI] [PubMed] [Google Scholar]
- 24.Millin MG, Gullett T, Daya MR. EMS management of acute stroke--out-of-hospital treatment and stroke system development (resource document to NAEMSP position statement). Prehosp Emerg Care. 2007;11(3):318–325. doi: 10.1080/10903120701347885. [DOI] [PubMed] [Google Scholar]
- 25.Carr BG, Conway PH, Meisel ZF, et al. Defining the Emergency Care Sensitive Condition: A Health Policy Research Agenda in Emergency Medicine. Ann Emerg Med. 2009;56(1):49–51. doi: 10.1016/j.annemergmed.2009.12.013. [DOI] [PubMed] [Google Scholar]
- 26.Seymour CW, Kahn JM, Cooke CR, Watkins TD, Heckbert SR, Rea TD. Prediction of critical illness during out-of-hospital emergency care. JAMA. 2010;304(7):747–754. doi: 10.1001/jama.2010.1140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Peelen L, de Keizer NF, Peek N, et al. The influence of volume and intensive care unit organization on hospital mortality in patients admitted with severe sepsis: a retrospective multicentre cohort study. Crit Care. 2007;11(2):R40. doi: 10.1186/cc5727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dellinger RP, Levy MM, Carlet JM, et al. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock: 2008. Crit Care Med. 2008;36(1):296–327. doi: 10.1097/01.CCM.0000298158.12101.41. [DOI] [PubMed] [Google Scholar]
- 29.Yeh EL, Cone DC. Cancellation of responding ALS units by BLS providers: a national survey. Prehosp Emerg Care. 2000;4(3):227–233. doi: 10.1080/10903120090941245. [DOI] [PubMed] [Google Scholar]
- 30.Cone DC, Wydro GC. Can basic life support personnel safely determine that advanced life support is not needed? Prehosp Emerg Care. 2001;5(4):360–365. doi: 10.1080/10903120190939517. [DOI] [PubMed] [Google Scholar]
- 31.Stiell IG, Nesbitt LP, Pickett W, et al. The OPALS Major Trauma Study: impact of advanced life-support on survival and morbidity. CMAJ. 2008;178(9):1141–1152. doi: 10.1503/cmaj.071154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lammers RL, Byrwa MJ, Fales WD, et al. Simulation-based assessment of paramedic pediatric resuscitation skills. Prehosp Emerg Care. 2009;13(3):345–356. doi: 10.1080/10903120802706161. [DOI] [PubMed] [Google Scholar]
- 33.Williams I, Mears G, Raisor C, et al. An emergency medical services toolkit for improving systems of care for stroke in North Carolina. Prev Chronic Dis. 2009;6(2):A67. [PMC free article] [PubMed] [Google Scholar]
- 34.Snider JB, Moreno R, Fuller DJ, et al. The effect of simple interventions on paramedic aspirin administration rates. Prehosp Emerg Care. 2004;8(1):41–45. doi: 10.1080/312703002211. [DOI] [PubMed] [Google Scholar]
- 35.Brice JH, Evenson KR, Lellis JC, et al. Emergency medical services education, community outreach, and protocols for stroke and chest pain in North Carolina. Prehosp Emerg Care. 2008;12(3):366–371. doi: 10.1080/10903120802100100. [DOI] [PubMed] [Google Scholar]
- 36.Culley LL, Rea TD, Murray JA, et al. Public access defibrillation in out-of-hospital cardiac arrest: a community-based study. Circulation. 2004;109(15):1859–1863. doi: 10.1161/01.CIR.0000124721.83385.B2. [DOI] [PubMed] [Google Scholar]
- 37.Kellerman SE, Herold J. Physician response to surveys. A review of the literature. Am J Prev Med. 2001;20(1):61–67. doi: 10.1016/s0749-3797(00)00258-0. [DOI] [PubMed] [Google Scholar]
- 38.Schmuhl P, Van Duker H, Gurley KL, et al. Reaching emergency medical services providers: is one survey mode better than another? Prehosp Emerg Care. 14(3):361–369. doi: 10.3109/10903121003760184. [DOI] [PubMed] [Google Scholar]
- 39.Davy JA, Kincaid JF, Smith KJ, Trawick MA. An examination of the role of attitudinal characteristics and motivation on the cheating behavior of business students. Ethics & Behavior. 2007;17(3):281–302. [Google Scholar]