Abstract
Pollicization substitutes a functioning finger for a deficient thumb. The most indication is thumb hypoplasia with absence or instability of the carpometacarpal joint. However, there are additional causes that may negate thumb function, such as trauma, macrodactyly, multi-fingered hand, and a mirror hand. The technique of pollicization represents a consolidation of contributions from surgeons over the last 100 years. A meticulous stepwise approach from incision to closure is necessary to optimize outcome. Following pollicization, cortical plasticity and motor relearning play a pivotal role in function following pollicization with connections and adjacent sprouting from nearby cortical and/or subcortical territories. Occupational therapy is necessary to encourage large object acquisition followed by smaller objects and ultimately fine pinch. Pollicization is more reliable in patients with isolated thumb hypoplasia and a mobile index finger with robust extrinsic and intrinsic muscle-tendon units compared to and patients with radial forearm deficiencies and diminished index mobility.
Keywords: Pollicization, Thumb hypoplasia, Macrodactyly, Ulnar deficiency, Mirror hand
Pollicization is an amazing operation that combines surgical skill with brain plasticity. The concept is to substitute a functioning finger for a deficient thumb. The deficient thumb is defined as one without ample function to contribute to prehension and grasp. The most common reason is hypoplasia with absence or instability of the carpometacarpal (CMC) joint, which obviates stability and function.1-3) However, there are additional causes that may negate thumb function, such as trauma, macrodactyly, multi-fingered hand, and a mirror hand. The more time I spend caring for children with congenital hand differences, the more likely I am to pursue pollicization as an option to reconstruct the hand impaired by thumb hypoplasia and other ailments. I firmly believe that the best substitute for a deficient thumb with small girth, unstable CMC joint, and/or insufficient extrinsic/intrinsic muscles is a mobile functional index finger. Adrian Flatt, MD (personal communication) has been an inspiration, mentor, and abounding with sage advice. He has extended congenital indications for pollicization to include a thumb smaller than a small finger and I concur! Reconstruction of a small hypoplastic thumb even with a stable CMC joint will pale in comparison to pollicization of a "normal" index finger. This decision requires a "heart to heart" conversation with the parents. The parents make the ultimate decision but the established surgeon has substantial influence. I spend substantial time explaining that "function trumps form" and that thumb ablation and index pollicization will result in enhanced function versus reconstruction of a small scrawny thumb. In addition, people are not very observant and a robust thumb with excellent function has better appearance compared to a small skinny thumb that contributes little to hand function. When in doubt, I recommend the parents discuss this decision with other parents who have made a similar difficult decision. This exchange is facilitated via a list of willing parents and support groups. Of course, cultural influences are important factors to be considered during this decision making process. Parents and society may ultimately negate the concept of thumb ablation and index finger pollicization. The parents are welcome to keep the "thumb", however; I avoid surgery to reconstruct a type IIB hypoplastic thumb as the results of index finger pollicization are far superior.4)
BRAIN PLASTICITY
Cortical plasticity and motor relearning play a pivotal in functional following pollicization. There is a large region of the sensorimotor cortex (SMC) homunculus dedicated to the hand. Researchers are trying to understand the changes in SMC following injury, repair, and reconstruction.5) Techniques include transcranial magnetic stimulation, electroencephalography, magnetoencephalography, functional magnetic resonance imaging (MRI), structural MRI, and positron emission tomography.5-9) Human cortical plasticity is a complex process that involves the unveiling of previously ineffective connections and sprouting of intact afferents from nearby cortical and/or subcortical territories.
Giraux et al.10) have demonstrated that after hand transplantation, the original SMC map for hand activation is restored. The transplantation reverses the SMC loss following the initial hand amputation. Similarly, successful toe transfer produces temporal activation within the SMC cortex consistent with cortical plasticity.11) Functional MRI has demonstrated that a patient learning to use their toe transfer lead to an expansion in their motor cortical representation. Practice magnifies the changes within the SMC cortex. As the new motor skill is mastered, there is a subsequent decrease in the amount of cortical representation.5,11) Functional MRI studies have provided evidence that that motor reorganization continues to evolve over time and may be modified by training and experience for a protracted time.12) These findings suggest that prolonged therapy and training may be necessary to maximize cortical reorganization and functional outcome.
The effects of pollicization have yet to be studied with reference to cortical plasticity. The locale and quantity of homunculus thumb representation before and after pollicization is an intriguing question. Without a doubt, fundamental changes occur in the SMC cortex as the index finger transforms into a thumb. The initial rehabilitation likely involves cortical plasticity with the development of new connections and adjacent sprouting from nearby cortical and/or subcortical territories.
TECHNIQUE
The current technique of pollicization represents a consolidation of contributions from surgeons over the last 100 years.13-15) My personal technique stems from direct interaction with other congenital hand surgeons, especially Marybeth Ezaki, Peter Carter, and Terry Light. Their surgical nuances have been incorporated into my current procedure, which has been fairly consistent for the last 10 years. I must profess that my technique will likely undergo further subtle modifications as I learn more from congenital hand colleagues.
A stepwise approach is used for multiple reasons (Table 1).16) First of all, multiple steps are required for completion of the procedure and this approach avoids "missing" a crucial step. Secondly, I operate at a teaching institution and this methodical approach is "teachable" to interested fellows. I will detail the basic surgical approach and highlight special circumstances that require surgical alterations related to the underlying diagnosis and anatomy encountered.
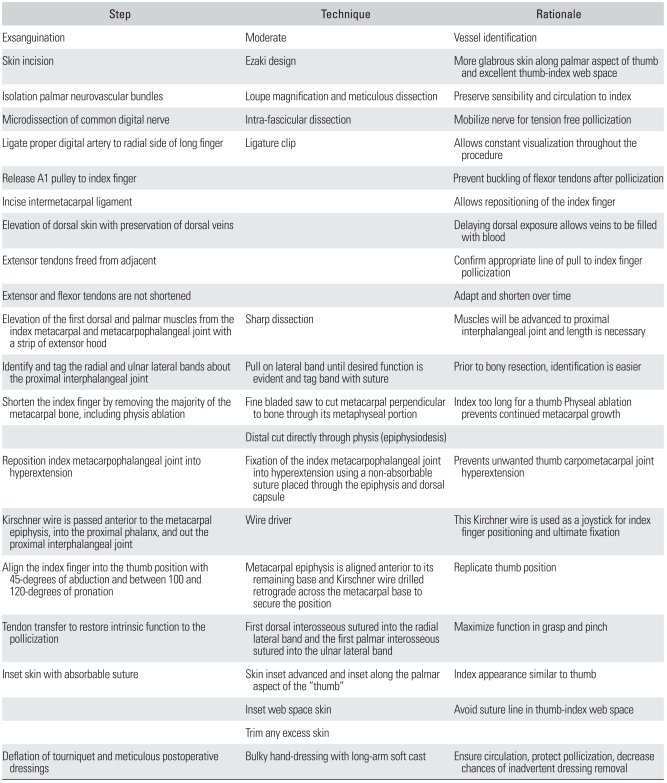
Table 1.
Stepwise Approach to Pollicization
POLLICIZATION FOR THUMB HYPOPLASIA (TYPES IIIB, IV, OR V HYPOPLASIA)
(A video clip is available: Click here to view.)
Following general anesthesia, the child is placed in the supine position. A pediatric tourniquet (Delfi Medical Innovations, Vancouver, Canada) is placed on the upper arm. The pediatric size is smaller in diameter, avoids irritation in the antecubital fossa, and extends the surgical field. Preoperative antibiotics are routinely administered. The extremity is prepped and draped in sterile fashion.
The skin incision must be nimble to allow easy index finger transposition and creation of an adequate thumbindex web space (Figs. 1 and 2). I currently use a modified design by Marybeth Ezaki and Peter Carter that allows more glabrous skin to be placed along the palmar aspect of the index finger.16) This improves the appearance of the index finger once in the thumb position, such that the index looks more like a thumb compared to other incisions.
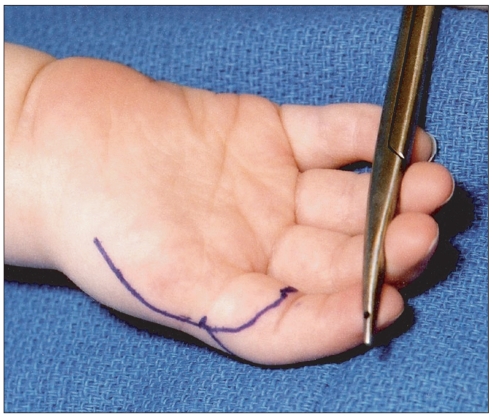
Fig. 1.
Volar skin design (Courtesy of Shriners Hospital for Children, Philadelphia).
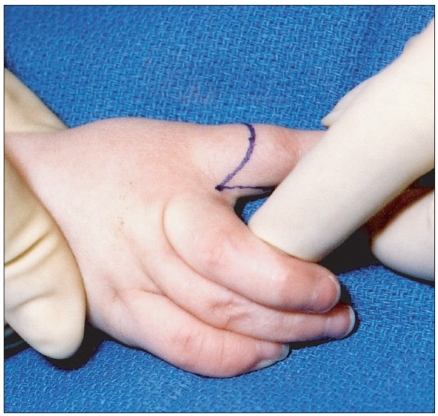
Fig. 2.
Dorsal skin design (Courtesy of Shriners Hospital for Children, Philadelphia).
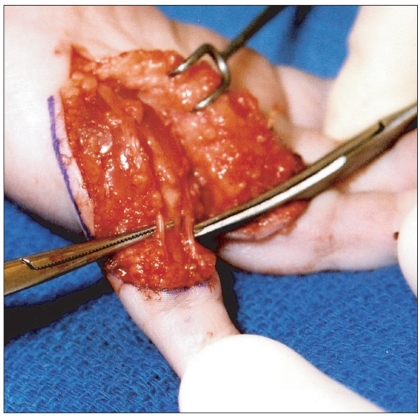
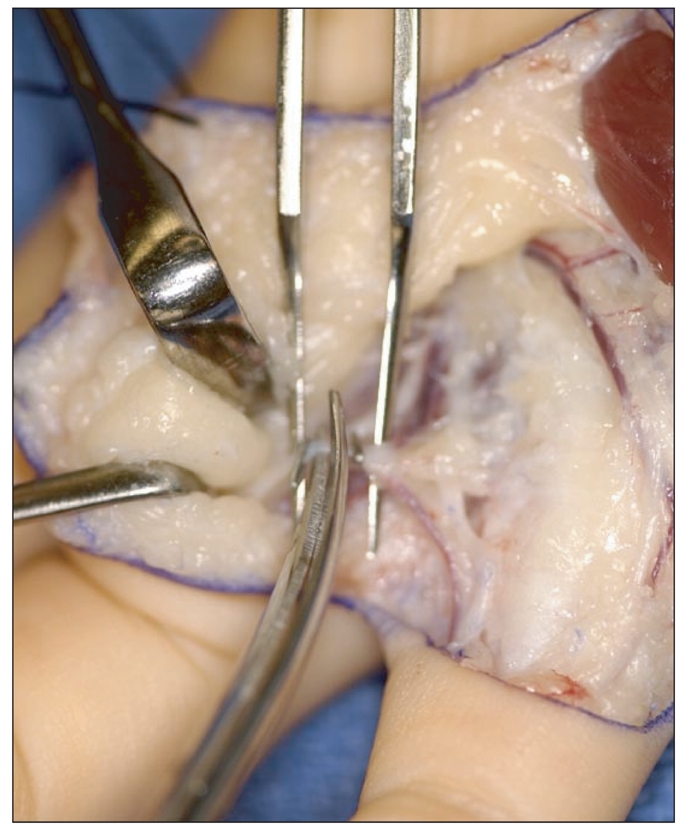
The limb is gently exsanguinated to facilitate identification of the vasculature (Fig. 3). The palmar skin is incised first and the radial neurovascular bundle isolated. In children with a type IV or IIIB thumb hypoplasia, the single vessel within the digit can be traced to radial neurovascular bundle of the index finger (Fig. 4). Dissection then proceeds further ulnar to identify the common digital vessels to the index-long web space. The proper digital nerves to the ulnar side of the index and the radial side of the long finger are isolated. Proximal microdissection is necessary to further separate the proper digital nerves to ease pollicization (Fig. 5). Occasionally, there is a neural loop that encircles the artery that must be addressed to prevent compression of the artery during index transposition. I cut the smaller of the two nooses to eliminate any compression. The proper digital artery to the ulnar side of the index and the radial side of the long finger are also isolated. The proper digital artery to the long finger is ligated to allow tension free index finger pollicization vascularized by the radial digital artery and the common digital artery (Fig. 6). We use ligating clips to mark the ends of the artery as these remain visible and a constant reminder of the vessels locations to prevent inadvertent vessel injury. The common digital artery is traced in a proximal direction. Beware of arterial variations that require additional dissection, such as the common artery originating from the deep arch.
Fig. 3.
Isolation of radial and ulnar neurovascular bundles (Courtesy of Shriners Hospital for Children, Philadelphia).
Fig. 4.
Volar dissection of a type IIIB thumb hypoplasia with tracing of the single vessel to radial neurovascular bundle of the index finger (Courtesy of Shriners Hospital for Children, Philadelphia).
Fig. 5.
Microdissection of the common digital nerve between the index and long (Courtesy of Shriners Hospital for Children, Philadelphia).
Fig. 6.
Ligation of the proper digital artery to the long finger (Courtesy of Shriners Hospital for Children, Philadelphia).
The first annular pulley of the index finger is incised to prevent buckling of the flexor tendons after the digit is shortened (Fig. 7). The intermetacarpal ligament is divided. The dorsal incision is then sharply elevated with conservation of as many dorsal veins as possible (Fig. 8). The index extensor tendons are inspected and any connections released to promote a direct pull to the index finger. I do not shorten the extensor or flexor tendons as these musculotendinous structures adapt over time.
Fig. 7.
Incision of the first annular pulley of the index finger (Courtesy of Shriners Hospital for Children, Philadelphia).
Fig. 8.
Elevation of dorsal incision with preservation of dorsal veins (Courtesy of Shriners Hospital for Children, Philadelphia).
The first dorsal and palmar interossei muscles are traced to their attachments into the extensor hood (Fig. 9). They are released with a portion of the hood in preparation for transfer. The tendons must be carefully isolated from the collateral ligaments about the metacarpophalangeal joint. The neurovascular bundles must be protected during elevation of the interossei. Prior to cutting the metacarpal, the future insertion sites for the tendons transfers are identified within the extensor hood over the proximal interphalangeal joint. A suture placed for later transfer of the first dorsal and first palmar tendons into the radial and ulnar lateral bands, respectively (Fig. 10).
Fig. 9.
First dorsal interosseous released from the extensor hood. (Courtesy of Shriners Hospital for Children, Philadelphia).
Fig. 10.
Sutures placed for later transfer of the first dorsal and first palmar interossei (Courtesy of Shriners Hospital for Children, Philadelphia).
The index finger is shortened by removing of the metacarpal bone from its base to the epiphysis. A fine bladed saw is used to cut the metacarpal base in a perpendicular direction through its metaphyseal portion. A rongeur can widen the base by pedaling the cortex open, which increases the surface area for healing. The metacarpal is dissected in proximal to distal direction and the distal cut is directly through the physis using a knife blade (Fig. 11). Physeal ablation (epiphysiodesis) prevents unwanted growth of the index pollicization.
Fig. 11.
Distal cut of index metacarpal through the physis (Courtesy of Shriners Hospital for Children, Philadelphia).
The normal index metacarpophalangeal joint hyperextends and the normal thumb carpometacarpal joint does not hyperextend. To rectify this discrepancy, the index metacarpophalangeal joint is fixed into hyperextension prior to pollicization. This is accomplished by suturing the metacarpophalangeal joint into hyperextension using a non-absorbable suture material passed through the epiphysis and dorsal capsule (Fig. 12). Subsequently, a Kirschner wire is passed adjacent to the metacarpal epiphysis, into the proximal phalanx, and out the proximal interphalangeal joint using a wire driver. This Kirchner wire is used as a joystick to facilitate index finger positioning. On occasion, interosseous sutures will be used to hold thumb in position (Fig. 13). The index metacarpal epiphysis aligned anterior to its remaining base with carefully positioning into 45-degrees of abduction and between 100 and 120-degrees of pronation. The Kirschner wire is drilled retrograde across the metacarpal base to secure the position. Additional stability is obtained via tendon transfer of the first dorsal interosseous to the radial lateral band and the first palmar interosseous to the ulnar lateral band (Fig. 14). The skin is carefully inset with absorbable suture (Fig. 15). The suture line for the first web space is advanced dorsal to avoid suture material and scar within the first web space. Any redundant skin is excised.
Fig. 12.
Metacarpophalangeal joint sutured into hyperextension using a non-absorbable (Courtesy of Shriners Hospital for Children, Philadelphia).
Fig. 13.
Thumb positioned and secured with interosseous sutures (Courtesy of Shriners Hospital for Children, Philadelphia).
Fig. 14.
Intrinsic reconstruction using first dorsal interosseous (Courtesy of Shriners Hospital for Children, Philadelphia).
Fig. 15.

Skin inset and sutured with absorbable suture (Courtesy of Shriners Hospital for Children, Philadelphia).
The tourniquet is deflated and the "thumb" observed for 5 minutes. The arterial circulation usually returns quickly, although vasospasm can result. Time, warm soaks, and patience often leads to resolution. Persistent lack of blood inflow requires exploration for injury. Venous congestion is more common, which can require reapplication of a looser dressing and/or release of any taut suture. The postoperative dressings are critical and follow standard hand dressing practice. A long-arm soft cast (3M Scotchcast Soft Cast Casting Tape, St. Paul, MN, USA) is applied with the elbow flexed to greater than 100-degrees to decrease the chance of inadvertent removal. This fiberglass casting tape does not set to a completely rigid state, but remains slightly flexible when cured. More importantly, the casting material can be unwrapped without a cast saw that is petrifying to the young child. The child is admitted overnight and the arm is elevated to promote venous drainage.
MACRODACTYLY
Macrodactyly is an uncommon congenital difference that is dramatic in presentation. Macrodactyly is commonly associated with lipofibromatosis of the proximal nerve.17,18) Most macrodactyly occurs in a single digit or in a region innervated by a single nerve (a.k.a. nerve territory oriented macrodactyly). The digital growth is either progressive with excessive growth over time or static, which maintains a steady proportion with the rest of the hand. A macrodactylous thumb is usually positioned in extension and abduction (Fig. 16). Longitudinal and appositional bony growth continues until skeletal maturity. Over time, the digit(s) enlarge and motion decreases, which increases functional impairment.
Fig. 16.

Three-year-old girl with progressive macrodactyly of the left thumb and index digits (Courtesy of Shriners Hospital for Children, Philadelphia).
Treatment is difficult and the results are often unimpressive.19) Static macrodactyly can be treated with procedures that limit ongoing growth (epiphysiodesis), reduce digital size (debulking), and/or correct deviation (osteotomy). In contrast, progressive macrodactyly is best treated with early amputation and hand reconstruction. Progressive thumb macrodactyly requires thumb reconstruction via pollicization or free toe transfer.
Pollicization for Macrodactyly
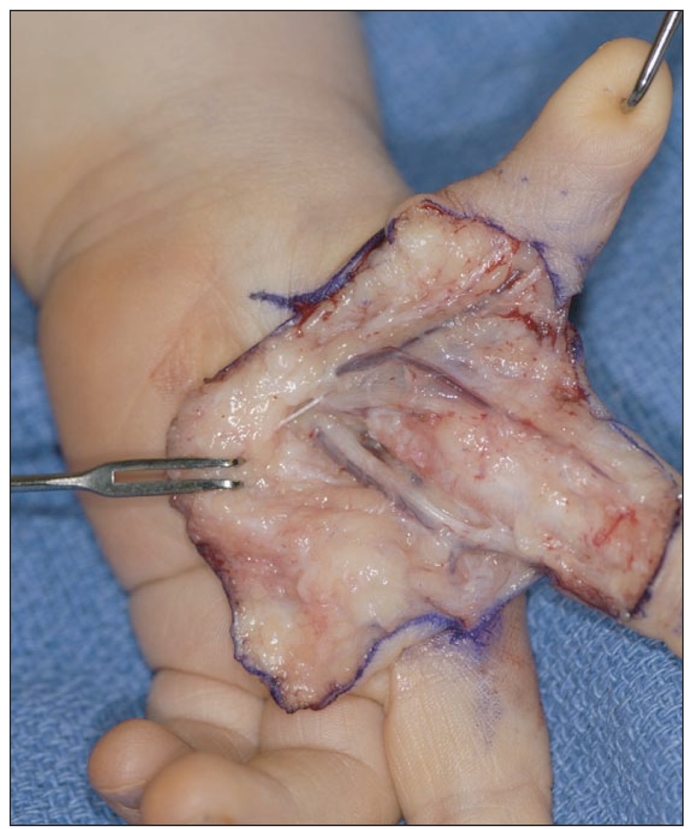
The surgical plan must be nimble as the underlying anatomy is variable. In children with macrodactyly of the index and thumb, long finger macrodactyly may be necessary. Part of the surgical strategy is to obtain independent thumb function by utilizing autonomous motors.14) Fortunately, the tendons are relatively normal in size and can be transferred to achieve independent thumb function. The underlying lipofibromatous median nerve complicates the procedure. Carpal tunnel release and intrafascicular dissection is necessary.
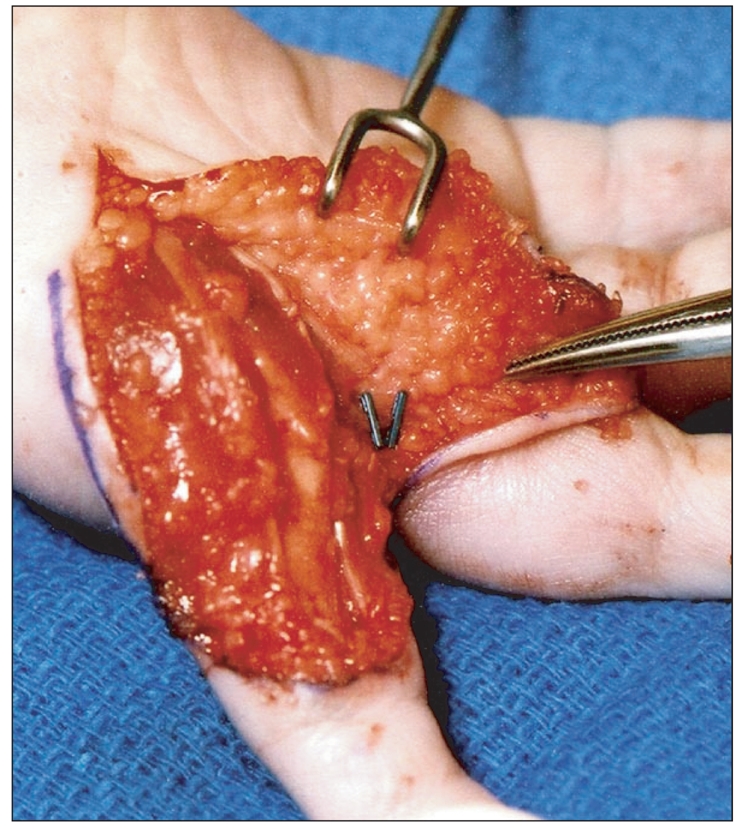
The procedure begins with a large skin incision that incorporates the standard pollicization incision (Figs. 17 and 18). Deeper dissection tries to remove as much of the diseased tissue as possible. The enlarged median nerve is identified as well as the superficial arch (Fig. 19). The nerves and arteries supplying to the thumb and index finger are then divided with a combination of bipolar electrocautery and vessel clips. The carpal tunnel is released, followed by internal neurolysis of the median nerve hamartoma. The digital nerves supplying the long finger are separated from the nerves to the index and thumb and the excessive nerve hamartoma is resected (Fig. 20).
Fig. 17.
Volar skin design (Courtesy of Shriners Hospital for Children, Philadelphia).
Fig. 18.
Dorsal skin design (Courtesy of Shriners Hospital for Children, Philadelphia).
Fig. 19.
Enlarged median nerve and superficial arch isolated (Courtesy of Shriners Hospital for Children, Philadelphia).
Fig. 20.
Digital nerves supplying the long finger are separated from median nerve hamartoma (Courtesy of Shriners Hospital for Children, Philadelphia).
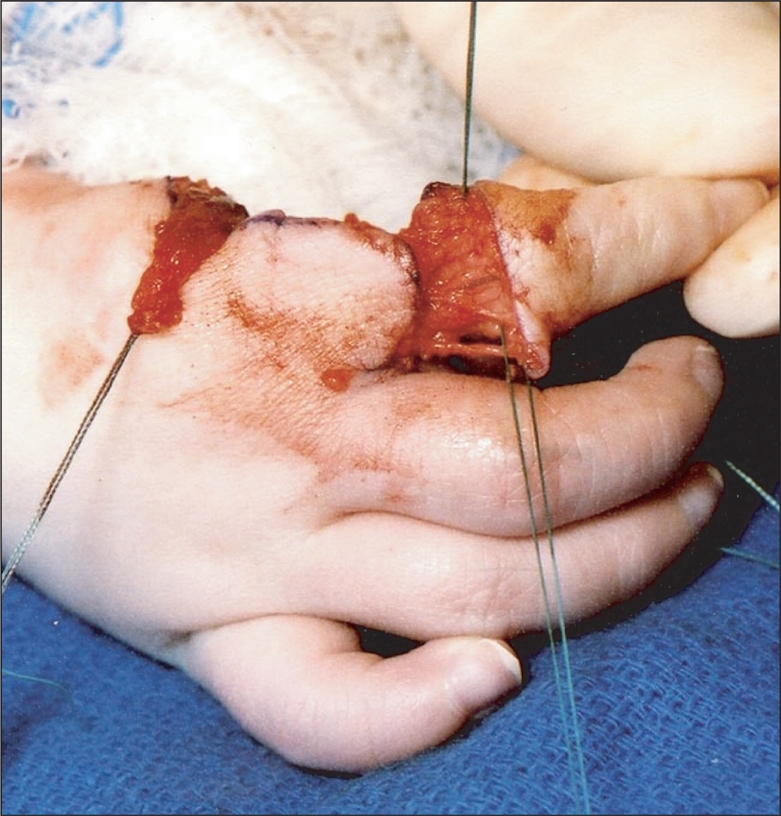
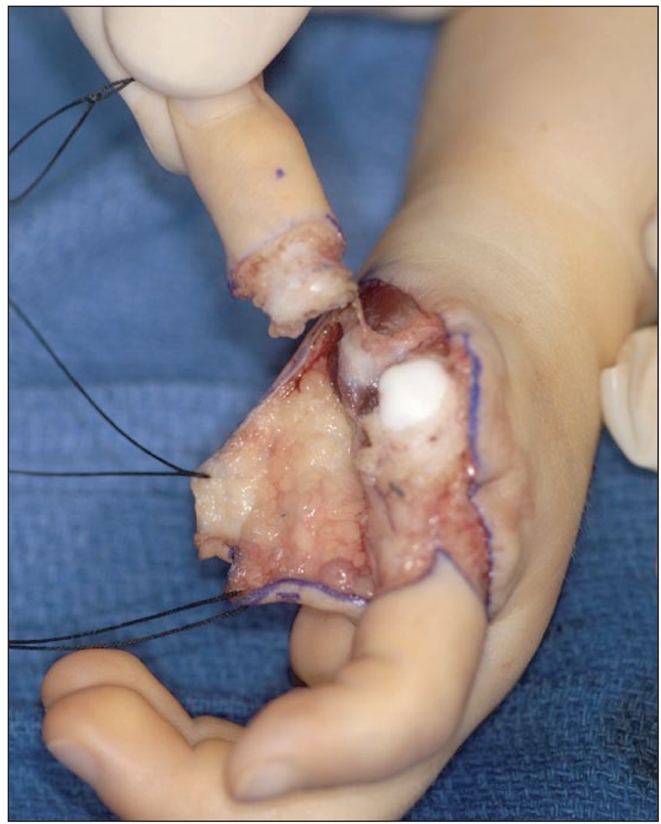
The flexor pollicis longus tendons, as well as the extensor indicis proprius, flexor digitorum superficialis, and flexor digitorum profundus tendons to the index finger are tagged and divided as distal as possible for potential transfers to the thumb. The thumb and all of its associated musculature, including the adductor and the thenar musculature is amputated. Similarly the index finger and its associated musculature are discarded from the remainder of the hand (Fig. 21). The index metacarpal base is retained as a possible base for the long finger.
Fig. 21.
Amputation of thumb and index finger with preservation of the index metacarpal (Courtesy of Shriners Hospital for Children, Philadelphia).
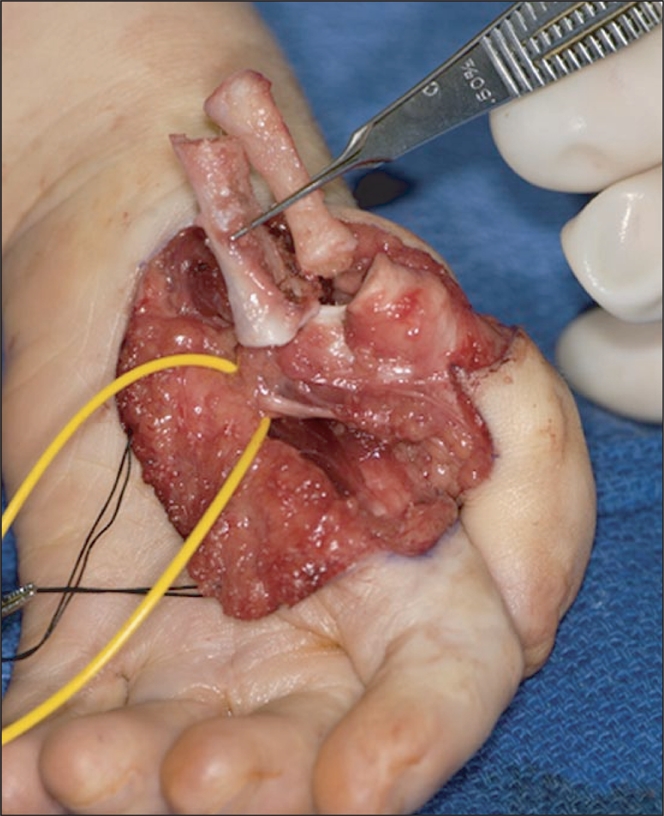
Attention is then directed towards long finger pollicization. The A1 pulley is divided, followed by division of the intermetacarpal ligament and volar and dorsal interosseous fascia. The interossei to the long finger are separated from their insertion preserving the collateral ligaments to the metacarpophalangeal joint. The long finger metacarpal is then divided through its physis performing an epiphysiodesis. The digital vessel to the ring finger is divided and the common long-ring digital vessel is mobilized with the long finger. The common digital nerve is divided in a proximal direction to allow for tension free pollicization. The long finger metacarpal is cut at the base, and the intervening metacarpal segment between the physis and the base is removed (Fig. 22).
Fig. 22.
Long finger metacarpal is removed (Courtesy of Shriners Hospital for Children, Philadelphia).
The index metacarpal base is contoured to accommodate the metacarpal head of the long finger. The long finger metacarpophalangeal joint is positioned into maximal extension and pinned using an antegrade 0.045-inch Kirschner wire driven out of the proximal interphalangeal joint. The metacarpal head of the long finger is then inset into the base of the index metacarpal, and pinned into position by driving the Kirschner wire retrograde into the metacarpal and trapezoid (Fig. 23). The thumb is carefully positioned in approximately 60 degrees of radial abduction, 45 degrees of palmar abduction, and ample pronation. The flexor pollicis longus is transferred either to the flexor digitorum profundus for independent thumb flexion or utilized as an opposition transfer. The dorsal and palmar interossei are transferred to recreate the abductor and adductor functions, respectively. The extensor indicis proprius is transferred to the extensor digitorum communis tendon for independent thumb extension. The skin is carefully inset and standard dressings are applied (Fig. 24).
Fig. 23.
The long finger is inset into the base of the index metacarpal with careful positioning (Courtesy of Shriners Hospital for Children, Philadelphia).
Fig. 24.
Final position after the skin is inset (Courtesy of Shriners Hospital for Children, Philadelphia).
ULNAR DEFICIENCY
Ulnar deficiency is four to ten times less common than radial deficiency.20) This anomaly affects the post-axial border of the limb and can be confused with radial deficiency by the physician not familiar with upper extremity congenital anomalies. The hand can have radial-sided anomalies ranging from a narrow web space to absent thumb.21) Pollicization of the adjacent digit is indicated to enhance function. There are some anatomic variations in ulnar deficiency that can make the procedure more challenging. Underlying neurovascular and bony anomalies must be incorporated into the surgical procedure.
Pollicization for Ulnar Deficiency
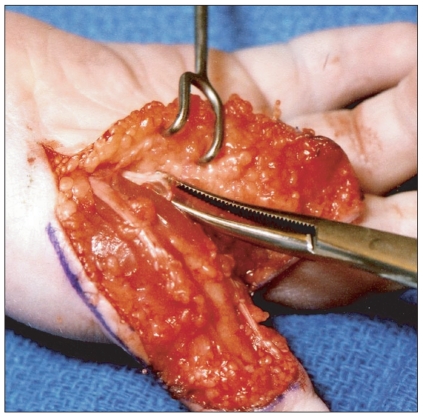
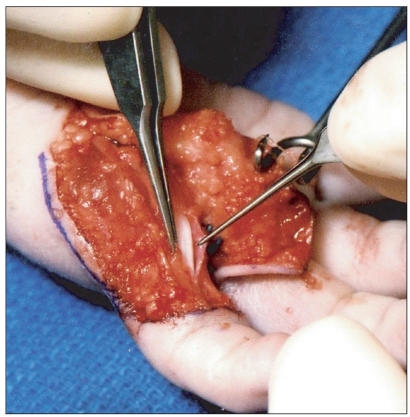
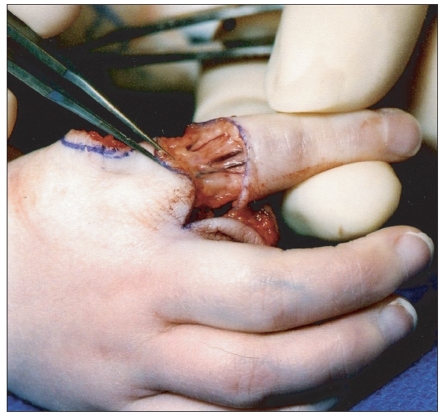
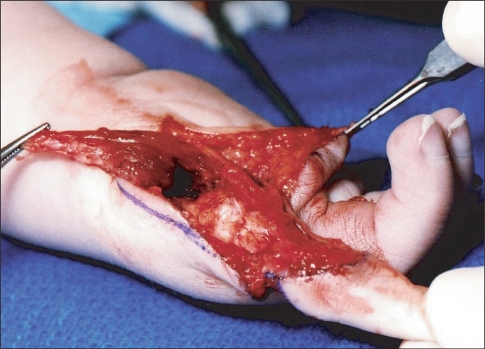
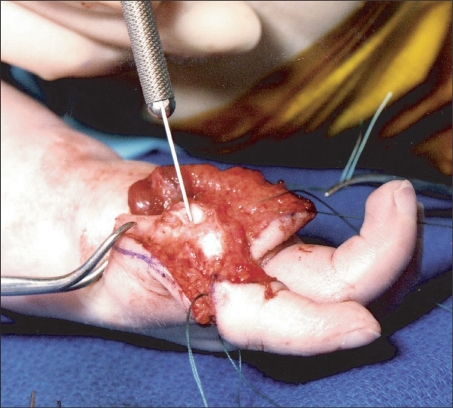
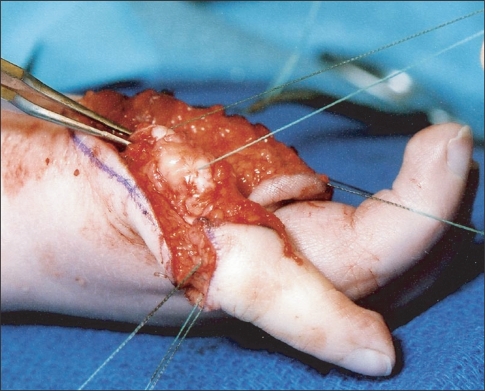
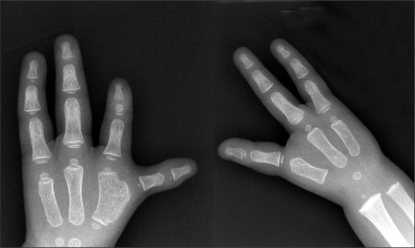
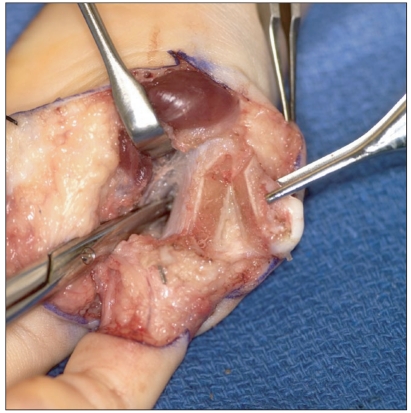
Preoperative clinical and X-ray evaluations are mandatory prior to surgery. Underlying bony abnormalities can be incorporated into the pollicization (Fig. 25). In cases with a hypoplastic thumb, the skin incision must be modified to incorporate thumb ablation (Figs. 26 and 27). Following skin incision, the neurovascular bundles are identified. The hypoplastic thumb is mobilized on its neurovascular bundle. Any substantial muscles are preserved and used to augment the index finger following pollicization (Fig. 28). The radial digital artery to the index finger is isolated and protected. The A1 pulley is opened and the ulnar neurovascular bundle is identified. The radial digital artery to the long finger is ligated (Fig. 29). The neurovascular structures are mobilized in a proximal direction to prevent any kinking during index finger transposition into the thumb position. The dorsal flap is elevated with preservation of dorsal vein for venous outflow. The hypoplastic thumb is amputated (Fig. 30). In cases with osseous anomalies, creative thinking is necessary to optimize bony support. Bifid metacarpals create a unique problem and osteotomy is necessary. The osteotomy must consider any double physis and avoid unintentional physeal arrest. The bifid metacarpal does provide a wide base for thumb policization (Fig. 31). The index metacarpal is shortened and a distal metacarpal epiphysiodesis performed (Fig. 32). A widened base allows fixation with two Kirschner wires for additional stability. The standard musculotendinous reconstruction is performed with augmentation of any muscles that were salvaged from the hypoplastic thumb (Fig. 33). The skin is inset and sutured with 5-0 plain suture (Figs. 34 and 35). Some skin contouring is always necessary. Following complete closure, the tourniquet is deflated to ensure good capillary refill is returned to all digits. Subsequently, a long-arm thumb spica cast is applied with the thumb exposed for neurovascular monitoring.
Fig. 25.
Three-year-old girl with bilateral ulnar deficiencies and a left hypoplastic thumb with a bifid metacarpal (Courtesy of Shriners Hospital for Children, Philadelphia).
Fig. 26.
Volar skin incision incorporating thumb ablation (Courtesy of Shriners Hospital for Children, Philadelphia).
Fig. 27.
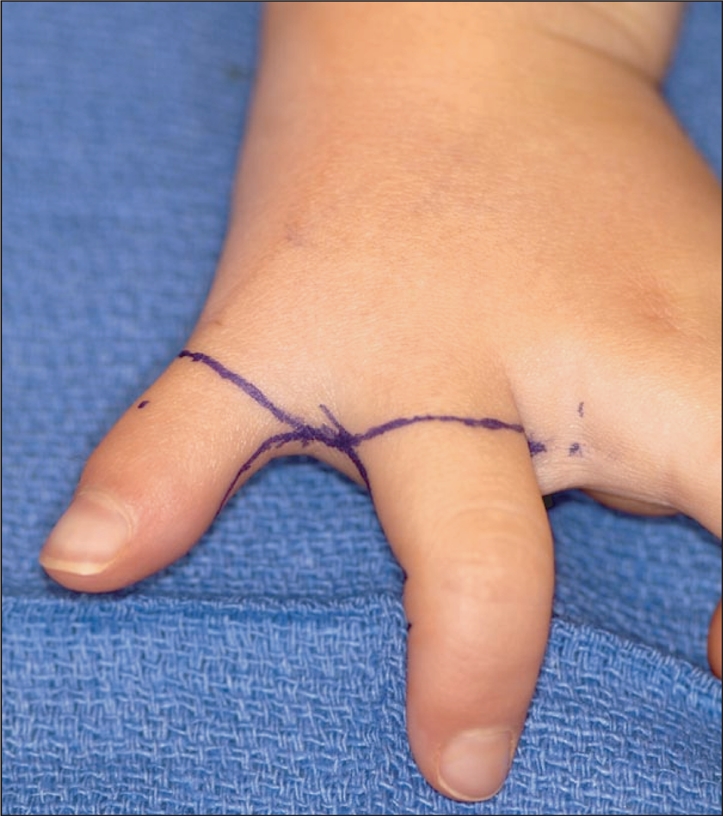
Dorsal skin incision (Courtesy of Shriners Hospital for Children, Philadelphia).
Fig. 28.
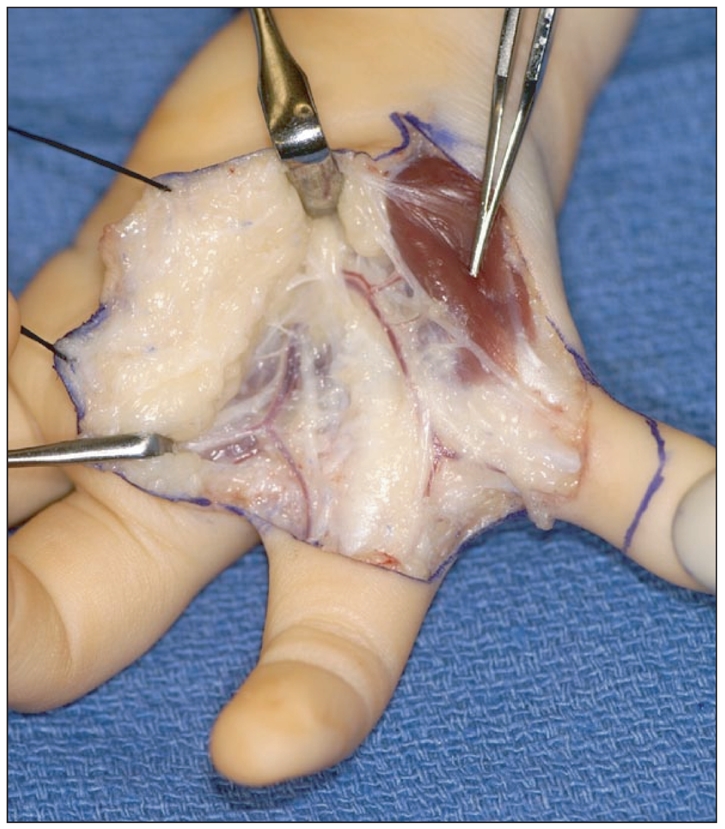
Isolation of neurovascular bundles and residual abductor pollicis brevis to be incorporated into the pollicization (Courtesy of Shriners Hospital for Children, Philadelphia).
Fig. 29.
Ligation of the radial digital artery to the long finger (Courtesy of Shriners Hospital for Children, Philadelphia).
Fig. 30.
Amputation of the thumb and its phalanges (Courtesy of Shriners Hospital for Children, Philadelphia).
Fig. 31.
Resection of the radial portion of the bifid metacarpal with preservation of a large base (Courtesy of Shriners Hospital for Children, Philadelphia).
Fig. 32.

Shortening of the index metacarpal for pollicization (Courtesy of Shriners Hospital for Children, Philadelphia).
Fig. 33.
Fixation with two Kirschner wires and abductor reconstruction (Courtesy of Shriners Hospital for Children, Philadelphia).
Fig. 34.

Skin countering of the first web space (Courtesy of Shriners Hospital for Children, Philadelphia).
Fig. 35.

Closure with 5-0 plain suture (Courtesy of Shriners Hospital for Children, Philadelphia).
MULTI-FINGERED HAND
The multi-fingered hand presents with multiple variations on a single theme. In other words, the hand has an excessive number of fingers and no thumb. There is a distinction between a multi-fingered hand and a mirror hand. The multi-fingered hand has a normal forearm segment while the mirror hand has ulnar dimelia.22) The multi-fingered can occur with syndactyly and/or polydactyly. In cases of polydactyly, there is usually five or six fingers. The surgical treatment must be individualized to the particular hand with the ultimate goal of making the best thumb possible. Pollicization techniques are variable and each hand has a unique set of challenges.
Pollicization for Multi-Fingered Hand
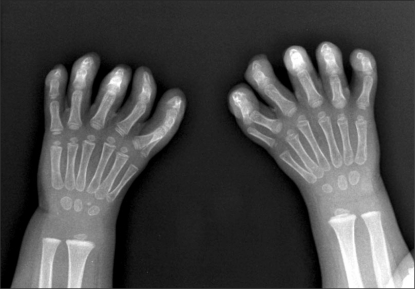
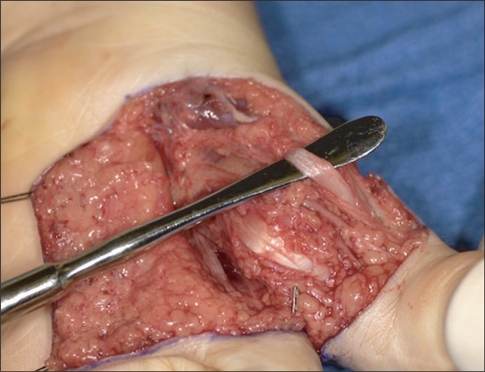
Clinical examination and X-rays occasionally supports pollicization of two radial digits when they are combined within a syndactyly and separation would result in a substandard thumb (Figs. 36 and 37). The volar skin is incised and the neurovascular bundle isolated. There is often a large artery between the two digits that must be preserved (Fig. 38). The common artery to the ulnar side of the radial two digits is isolated and the proper digital artery to the next adjacent digit is ligated. The A1 pulleys are incised and the intermetacarpal ligament between the radial two digits and adjacent ulnar digit divided (Fig. 39).
Fig. 36.
X-ray of 3-year-old girl with bilateral 6 fingered hands (Courtesy of Shriners Hospital for Children, Philadelphia).
Fig. 37.

Clinical examination demonstrates conjoined motion of the two radial digits (Courtesy of Shriners Hospital for Children, Philadelphia).
Fig. 38.

Volar dissection and identification of neurovascular structures (Courtesy of Shriners Hospital for Children, Philadelphia).
Fig. 39.
Incision of A1 pulleys (Courtesy of Shriners Hospital for Children, Philadelphia).
Dorsal dissection is performed with preservation of dorsal veins. The interossei are elevated with a portion of the extensor hood. Any interosseous muscle between the metacarpals is excised or incorporated into the subsequent muscular reconstruction.
Bony reduction is complicated and both metacarpals are removed with the distal cut through the physis (Fig. 40). If the metacarpophalangeal joints are located at different levels, then a single metacarpophalangeal joint is used to from the carpometacarpal joint. Otherwise, both metacarpophalangeal joints can be incorporated into the carpometacarpal joint reconstruction.
Fig. 40.
Excision of both metacarpals (Courtesy of Shriners Hospital for Children, Philadelphia).
A 0.045 Kirschner wire was drilled through the metacarpal head and out through the proximal interphalangeal joint. The two radial digits are positioned into the thumb position and the K-wire drilled retrograde across the metacarpal base. Intrinsic reconstruction is performed using the available muscles. The goal is to reconstruct the abductor pollicis brevis and the adductor pollicis. The first palmar interossei is often used to reconstruct the adductor pollicis. If there is a first dorsal interosseous, this muscle can be used for abductor reconstruction. Otherwise, the previous muscle between the two metacarpals can be used to reconstruct the abductor by advancing the tendon into the extensor hood. The skin is inset with 5-0 plain suture. A standard dressing and long-arm spica cast is applied (Fig. 41). The subsequent X-rays yield a bizarre bony arrangement, however; clinical function is remarkable (Figs. 42 and 43).
Fig. 41.

Postoperative appearance after intrinsic reconstruction and skin closure (Courtesy of Shriners Hospital for Children, Philadelphia).
Fig. 42.
Subsequent postoperative X-rays following bilateral pollicization (Courtesy of Shriners Hospital for Children, Philadelphia).
Fig. 43.
Left thumb position and pinch function (Courtesy of Shriners Hospital for Children, Philadelphia).
MIRROR HAND
Mirror hand is described by symmetric duplication of fingers within the hand attributed to replication of the zone of polarizing activity or its signaling molecule, sonic hedgehog protein, from the posterior margin of the limb bud to the anterior aspect (Fig. 44).23) The forearm has two ulnae that support duplicated ulnar carpal elements and the radius is absent. The soft tissue anatomy is peculiar and complex.24)
Fig. 44.
Three-year-old girl with mirror hand and seven fingers (Courtesy of Shriners Hospital for Children, Philadelphia).
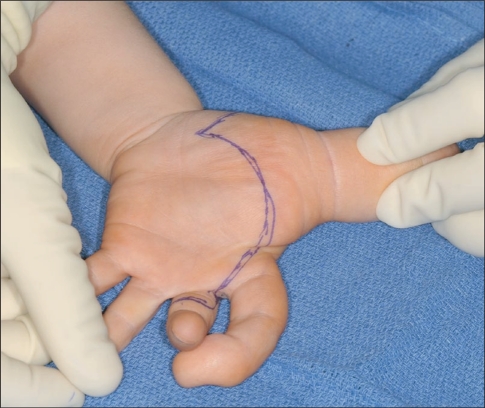
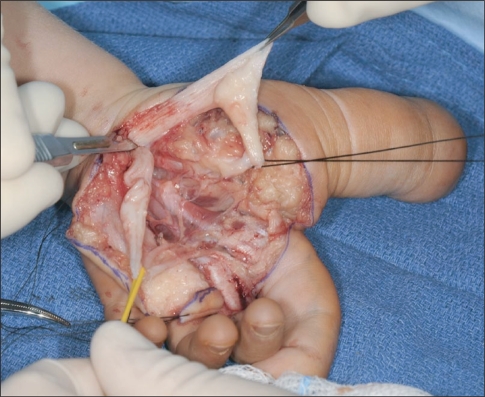
Pollicization for Mirror Hand
The absent thumb is managed by pollicization.25) The most mobile radial finger is selected for pollicization and the remaining radial fingers are removed (Figs. 45-47). An experienced occupational therapist can help decide which finger to utilize. A similar skin design and surgical technique is utilized. Many of the surgical points highlighted for the multi-fingered hand apply to mirror hand pollicization. The underlying anatomy can be confusing and diligent dissection is necessary. There are a plethora of muscles and tendons that can be used to augment the pollicization. The surgeon must select those muscles that can augment thumb function and avoid using too many muscles that will compete for function. Careful positioning is necessary for optimal prehension.
Fig. 45.
Ablation of the two less mobile radial digits (Courtesy of Shriners Hospital for Children, Philadelphia).
Fig. 47.

Appearance after pollicization (Courtesy of Shriners Hospital for Children, Philadelphia).
REHABILITATION
The cast and Kirschner wire is removed four to five weeks after surgery and a short arm thumb spica splint is fabricated. Occupational therapy is started with an emphasis on thumb usage. The initial goal is large object acquisition followed by smaller objects and ultimately fine pinch. Activities for encouraging grasp pattern include tearing up paper, picking up pencils, opening containers, playing with small objects (cars and blocks), coloring/scribbling, pulling sticker apart, and picking up leaves (Fig. 48). Standard wound care is also performed consisting of scar massage and soft ening techniques.
Fig. 48.
Activities for encouraging pinch pattern include playing with stickers (Courtesy of Shriners Hospital for Children, Philadelphia).
The splint is worn all day splint all day except for quiet supervised play activities, scar massage, bathing, and therapy for four weeks. The splint time is gradually diminished during weeks five through twelve and then discontinued. As thumb motion increases, strengthening is slowly added to the therapy regimen. Activities for strengthening included playing with dough, riding toys, holding objects with handles (bucket), and grasping balls (tennis ball/baseball).
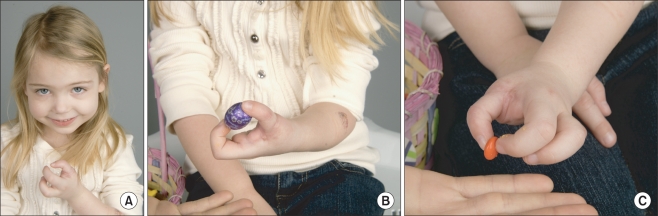
OUTCOME
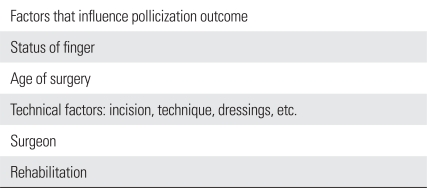
There are a variety of factors that affect outcome (Table 2). The principal factor is the preoperative status of the index digit and the presence or absence of adequate muscles/tendon units.1,2,13,26-30) A mobile index finger with robust extrinsic and intrinsic muscle-tendon units will make an excellent thumb that participates in grasp and mobility for pinch (Fig. 49). In contrast, an index finger with limited active and passive motion may provide stability for gross grasp but is unlikely to be used for pinch. In these cases, the child is more agile with scissoring pinch between the remaining fingers. For this reason, pollicization is more reliable in patients with isolated thumb hypoplasia compared to and patients with radial forearm deficiencies and diminished index mobility.1,2,28,30)
Table 2.
Pollicization Factors
Fig. 49.
Three-year-old with ulnar deficiency depicted in Fig. 25 (Courtesy of Shriners Hospital for Children, Philadelphia). (A) Left thumb position. (B) Gross grasp pattern. (C) Fine pinch pattern.
Another factor is age at time of surgery. The precise age to perform surgery is debatable. Younger surgery takes advantage of brain plasticity and ease of incorporation into daily activities. These "young" factors are mitigated by the anatomical size of the neurovascular and musculocutaneous structures. I recommend pollicization at about one year of age to allow for some hand growth, while optimizing the positive aspects of youth. Late presentation is not a contraindication for pollicization, however; the adolescent is often surprised about the change is his or her hand. Preoperative discussion will limit the astonishment following dressing removal.
Technical factors that influence outcome include surgical technique and the choice of bone and tendon realignment. The technique requires a stepwise approach to craft the thumb in optimum position with adequate muscle-tendons unit for mobilization. Similarly, surgical experience has a positive influence on the outcome. Pollicization is a relatively uncommon procedure that requires considerably repetition to gain adequate experience to the circumvent variations in anatomy. I perform about 15-20 pollicizations per year and feel comfortable in tackling a standard pollicization for hypoplastic thumbs as well as pollicizations for abnormal circumstances, such as polysyndactyly and macrodactyly. Pollicization is NOT for the pediatric surgeon or adult hand surgeon. These cases should be performed by a pediatric hand surgeon familiar with the intricacies of the procedure.
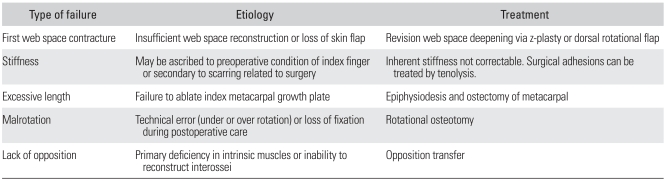
COMPLICATIONS
Pollicization is an intricate procedure that has multiple pitfalls that result in suboptimal function. Early complications are related to arterial and venous blood flow. Inadvertent arterial injury requires microsurgical repair. Venous problems are more common as the dorsal venous plexus is tenuous and preservation is difficult in more complex pollicization procedures. Transient venous congestion requires elevation, loosening of the dressings, removal of dorsal sutures, and even evacuation of hematoma. More severe cases may require unconventional measures, such as leech therapy.
Long-term complications are more prevalent. Any unsatisfactory outcome requires an analytical approach to find the root of the problem (Table 3). Additional surgery may or may not be available to improve the status and function of the thumb.31,32)
Table 3.
Pollicization Pitfalls and Complications
Fig. 46.
Polllicization of the most mobile radial digit (Courtesy of Shriners Hospital for Children, Philadelphia).
ACKNOWLEDGEMENTS
The author would like to acknowledge Brian W. O'Doherty, Coordinator of Visual Media Services. His photographic excellence was necessary for completion of this manuscript.
Footnotes
No potential conflict of interest relevant to this article was reported.
Supplementary Material
A video clip is available on the electronic version of this paper at the CiOS web site, www.ecios.org.
References
- 1.Manske PR, McCaroll HR., Jr Index finger pollicization for a congenitally absent or nonfunctioning thumb. J Hand Surg Am. 1985;10(5):606–613. doi: 10.1016/s0363-5023(85)80192-1. [DOI] [PubMed] [Google Scholar]
- 2.Kozin SH, Weiss AA, Webber JB, Betz RR, Clancy M, Steel HH. Index finger pollicization for congenital aplasia or hypoplasia of the thumb. J Hand Surg Am. 1992;17(5):880–884. doi: 10.1016/0363-5023(92)90460-7. [DOI] [PubMed] [Google Scholar]
- 3.Lister G. Reconstruction of the hypoplastic thumb. Clin Orthop Relat Res. 1985;(195):52–65. [PubMed] [Google Scholar]
- 4.Foucher G, Medina J, Navarro R. Microsurgical reconstruction of the hypoplastic thumb, type IIIB. J Reconstr Microsurg. 2001;17(1):9–15. doi: 10.1055/s-2001-12683. [DOI] [PubMed] [Google Scholar]
- 5.Anastakis DJ, Malessy MJ, Chen R, Davis KD, Mikulis D. Cortical plasticity following nerve transfer in the upper extremity. Hand Clin. 2008;24(4):425–444. doi: 10.1016/j.hcl.2008.04.005. [DOI] [PubMed] [Google Scholar]
- 6.Chen R. Studies of human motor physiology with transcranial magnetic stimulation. Muscle Nerve Suppl. 2000;9:S26–S32. doi: 10.1002/1097-4598(2000)999:9<::aid-mus6>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 7.Barker AT, Jalinous R, Freeston IL. Non-invasive magnetic stimulation of human motor cortex. Lancet. 1985;1(8437):1106–1107. doi: 10.1016/s0140-6736(85)92413-4. [DOI] [PubMed] [Google Scholar]
- 8.Gevins A, Leong H, Smith ME, Le J, Du R. Mapping cognitive brain function with modern high-resolution electroencephalography. Trends Neurosci. 1995;18(10):429–436. doi: 10.1016/0166-2236(95)94489-r. [DOI] [PubMed] [Google Scholar]
- 9.Friston KJ, Frith CD, Liddle PF, Frackowiak RS. Comparing functional (PET) images: the assessment of significant change. J Cereb Blood Flow Metab. 1991;11(4):690–699. doi: 10.1038/jcbfm.1991.122. [DOI] [PubMed] [Google Scholar]
- 10.Giraux P, Sirigu A, Schneider F, Dubernard JM. Cortical reorganization in motor cortex after graft of both hands. Nat Neurosci. 2001;4(7):691–692. doi: 10.1038/89472. [DOI] [PubMed] [Google Scholar]
- 11.Manduch M, Bezuhly M, Anastakis DJ, Crawley AP, Mikulis DJ. Serial fMRI of adaptive changes in primary sensorimotor cortex following thumb reconstruction. Neurology. 2002;59(8):1278–1281. doi: 10.1212/wnl.59.8.1278. [DOI] [PubMed] [Google Scholar]
- 12.Chen R, Anastakis DJ, Haywood CT, Mikulis DJ, Manktelow RT. Plasticity of the human motor system following muscle reconstruction: a magnetic stimulation and functional magnetic resonance imaging study. Clin Neurophysiol. 2003;114(12):2434–2446. doi: 10.1016/s1388-2457(03)00283-9. [DOI] [PubMed] [Google Scholar]
- 13.Buck-Gramcko D. Pollicization of the index finger: method and results in aplasia and hypoplasia of the thumb. J Bone Joint Surg Am. 1971;53(8):1605–1617. [PubMed] [Google Scholar]
- 14.Littler JW. On making a thumb: one hundred years of surgical effort. J Hand Surg Am. 1976;1(1):35–51. doi: 10.1016/s0363-5023(76)80024-x. [DOI] [PubMed] [Google Scholar]
- 15.McCarroll HR. Congenital anomalies: a 25-year overview. J Hand Surg Am. 2000;25(6):1007–1037. doi: 10.1053/jhsu.2000.6457. [DOI] [PubMed] [Google Scholar]
- 16.Kozin SH. Deformities of the thumb. In: Wolfe SW, Hotchkiss RN, Pederson WC, Kozin SH, editors. Green's operative hand surgery. 6th ed. Philadelphia, PA: Elsevier Churchill Livingstone; 2010. pp. 1371–1404. [Google Scholar]
- 17.Brodwater BK, Major NM, Goldner RD, Layfield LJ. Macrodystrophia lipomatosa with associated fibrolipomatous hamartoma of the median nerve. Pediatr Surg Int. 2000;16(3):216–218. doi: 10.1007/s003830050728. [DOI] [PubMed] [Google Scholar]
- 18.Al-Qattan MM. Lipofibromatous hamartoma of the median nerve and its associated conditions. J Hand Surg Br. 2001;26(4):368–372. doi: 10.1054/jhsb.2001.0579. [DOI] [PubMed] [Google Scholar]
- 19.Ishida O, Ikuta Y. Long-term results of surgical treatment for macrodactyly of the hand. Plast Reconstr Surg. 1998;102(5):1586–1590. doi: 10.1097/00006534-199810000-00038. [DOI] [PubMed] [Google Scholar]
- 20.Kozin SH. Upper-extremity congenital anomalies. J Bone Joint Surg Am. 2003;85(8):1564–1576. doi: 10.2106/00004623-200308000-00021. [DOI] [PubMed] [Google Scholar]
- 21.Cole RJ, Manske PR. Classification of ulnar deficiency according to the thumb and first web. J Hand Surg Am. 1997;22(3):479–488. doi: 10.1016/S0363-5023(97)80016-0. [DOI] [PubMed] [Google Scholar]
- 22.Al-Qattan MM, Al-Thunayan A, De Cordier M, Nandagopal N, Pitkanen J. Classification of the mirror hand-multiple hand spectrum. J Hand Surg Br. 1998;23(4):534–536. doi: 10.1016/s0266-7681(98)80140-x. [DOI] [PubMed] [Google Scholar]
- 23.Riddle RD, Johnson RL, Laufer E, Tabin C. Sonic hedgehog mediates the polarizing activity of the ZPA. Cell. 1993;75(7):1401–1416. doi: 10.1016/0092-8674(93)90626-2. [DOI] [PubMed] [Google Scholar]
- 24.Barton NJ, Buck-Gramcko D, Evans DM. Soft-tissue anatomy of mirror hand. J Hand Surg Br. 1986;11(3):307–319. doi: 10.1016/0266-7681(86)90151-8. [DOI] [PubMed] [Google Scholar]
- 25.Barton NJ, Buck-Gramcko D, Evans DM, Kleinert H, Semple C, Ulson H. Mirror hand treated by true pollicization. J Hand Surg Br. 1986;11(3):320–336. doi: 10.1016/0266-7681(86)90152-x. [DOI] [PubMed] [Google Scholar]
- 26.Manske PR, Rotman MB, Dailey LA. Long-term functional results after pollicization for the congenitally deficient thumb. J Hand Surg Am. 1992;17(6):1064–1072. doi: 10.1016/s0363-5023(09)91063-2. [DOI] [PubMed] [Google Scholar]
- 27.Clark DI, Chell J, Davis TR. Pollicisation of the index finger: a 27-year follow-up study. J Bone Joint Surg Br. 1998;80(4):631–635. doi: 10.1302/0301-620x.80b4.8613. [DOI] [PubMed] [Google Scholar]
- 28.Ogino T, Ishii S. Long-term results after pollicization for congenital hand deformities. Hand Surg. 1997;2(2):79–85. [Google Scholar]
- 29.Sykes PJ, Chandraprakasam T, Percival NJ. Pollicisation of the index finger in congenital anomalies: a retrospective analysis. J Hand Surg Br. 1991;16(2):144–147. doi: 10.1016/0266-7681(91)90164-j. [DOI] [PubMed] [Google Scholar]
- 30.Vekris MD, Beris AE, Lykissas MG, Soucacos PN. Index finger pollicization in the treatment of congenitally deficient thumb. Ann Plast Surg. 2011;66(2):137–142. doi: 10.1097/SAP.0b013e3181e6cfd9. [DOI] [PubMed] [Google Scholar]
- 31.Ogino T, Minami A, Fukuda K. Abductor digitiminimi opponensplasty in hypoplastic thumb. J Hand Surg Br. 1986;11(3):372–377. doi: 10.1016/0266-7681(86)90160-9. [DOI] [PubMed] [Google Scholar]
- 32.Latimer J, Shah M, Kay S. Abductor digitiminimi transfer for the restoration of opposition in children. J Hand Surg Br. 1994;19(5):653–658. doi: 10.1016/0266-7681(94)90137-6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A video clip is available on the electronic version of this paper at the CiOS web site, www.ecios.org.