Abstract
Objectives
To investigate whether demographic (age and education) adjustments for the Mini-Mental State Examination (MMSE) attenuate mean score discrepancies between African American and Caucasian adults, and to determine whether demographically-adjusted MMSE scores improve the diagnostic classification accuracy of dementia in African American adults when compared to unadjusted MMSE scores.
Design
Cross-sectional study.
Setting
Community-dwelling adults participating in the Mayo Clinic Alzheimer’s Disease Patient Registry (ADPR) and Alzheimer’s Disease Research Center (ADRC).
Participants
Three thousand two hundred fifty-four adults (2819 Caucasian, 435 African American) aged 60 and older.
Measurements
MMSE at study entry.
Results
African American adults obtained significantly lower unadjusted MMSE scores (23.0 ± 7.4) compared to Caucasian adults (25.3 ± 5.4). This discrepancy persisted despite adjustment of MMSE scores for age and years of education using established regression weights or newly-derived weights. However, controlling for dementia severity at baseline and adjusting MMSE scores for age and quality of education attenuated this discrepancy. Among African American adults, an age- and education-adjusted MMSE cut score of 23/24 provided optimal dementia classification accuracy, but this represented only a modest improvement over an unadjusted MMSE cut score of 22/23. The posterior probability of dementia in African American adults is presented for various unadjusted MMSE cut scores and prevalence rates of dementia.
Conclusion
Age, dementia severity at study entry, and quality of educational experience are important explanatory factors to understand the existing discrepancies in MMSE performance between Caucasian and African American adults. Our findings support the use of unadjusted MMSE scores when screening African American elders for dementia, with an unadjusted MMSE cut score of 22/23 yielding optimal classification accuracy.
Keywords: MMSE, African American, ethnicity, dementia, cognition
INTRODUCTION
The Mini-Mental State Examination (MMSE)1 is one of the most widely used cognitive screening measures in medical settings. It is a sensitive indicator of dementia, but its diagnostic utility tends to diminish when used to evaluate ethnic minorities or highly educated individuals2. Ethnic minorities systematically obtain lower MMSE scores compared to Caucasian adults with a comparable degree of cognitive impairment3,4. This discrepancy may lead a disproportionate number of cognitively-normal ethnic minorities to be inaccurately classified as impaired, and overestimate the level of disease severity in ethnic minorities with dementia.
Mungas and colleagues5 studied 590 Caucasian and Hispanic older adults and showed that adjusting MMSE scores for the effects of age and years of education (MMSEAdj1) attenuated the discrepancy attributable to ethnic group membership. Moreover, MMSEAdj1 scores in Hispanic adults yielded improved sensitivity (SN) and specificity (SP) compared to unadjusted MMSE scores. The authors found a comparable improvement in SN and SP when making this adjustment to MMSE scores from eleven African American elders. However, they urged caution interpreting those findings due to their small sample of African American participants.
The current study examines whether age- and education-adjustments attenuate the known discrepancy in MMSE scores between Caucasian and African American adults. Specifically, we expand the preliminary findings from Mungas et al.5 and apply their regression-based adjustment to our current sample. We also investigate the use of regression weights derived from our sample to adjust MMSE scores for age and years of education, as well as adjustment for quality of education using a proxy indicator of reading achievement. We then evaluate the diagnostic validity of these adjusted MMSE scores for detecting dementia in African American elders. We hypothesize that the use of demographically-adjusted MMSE scores will yield improved diagnostic classification accuracy over unadjusted MMSE scores.
METHODS
Participants
Archival data of 4248 patients from the Mayo Clinic Alzheimer’s Disease Research Center (ADRC) and Alzheimer’s Disease Patient Registry (ADPR) were reviewed. Information on age, gender, education, self-reported ethnicity, diagnosis, and baseline MMSE scores were available for 3254 individuals aged 60 and older (1169 males, 2085 females), including 2819 Caucasians (86.6%) and 435 African Americans (13.4%). The sample included 2048 cognitively-normal adults (see Ivnik et al.6 for criteria used to define normal cognition) and 1206 patients with dementia, diagnosed via consensus among ADRC/ADPR investigators and using published diagnostic criteria. Diagnoses included 864 (71.6%) patients with probable or possible Alzheimer’s disease, 112 (9.3%) with Lewy body dementia, 76 (6.3%) with vascular-related dementia, 53 (4.4%) with frontotemporal dementia, and 101 (8.4%) with other dementia etiologies. The MMSE was administered as part of a dementia battery that also included the Clinical Dementia Rating (CDR)7 scale and a measure of word reading from the Wide Range Achievement Test (WRAT-3)8. This index of word reading achievement serves as a proxy for the quality of a person’s educational experience, and is particularly useful when evaluating African American adults9,10. MMSE scores did not contribute to the baseline consensus diagnosis.
All data were obtained in compliance with the Mayo Clinic Institutional Review Board.
Statistical Analyses
Continuous data were analyzed using independent t-tests, with degrees of freedom adjusted for inequality of variance where appropriate. Categorical data were analyzed using chi-square tests. MMSEAdj1 scores were derived using the regression equation published by Mungas and colleagues5, which adjusts MMSE scores for age and years of education. Because regression weights tend to be sample-specific, we derived a new correction based on our sample (MMSEAdj2) using the same methodology. To obtain this correction, unadjusted MMSE scores were regressed onto age and years of education, and the regression weights of these predictors were inserted into the equation: MMSEAdj2 = MMSE − [.386 × (education − 12)] + [.058 × (age − 70)].
To evaluate the role of quality of education on MMSE scores, we used age and years of education (step 1), standard scores from the WRAT-3 reading test (step 2), and ethnicity (step 3) in a hierarchical model predicting MMSE scores. WRAT-3 data were available for 1761 participants (1418 Caucasian, 343 African American). Then we derived demographic corrections (MMSEAdj3) using age and WRAT-3 reading scores. Education (years) was excluded from this model due to the expected multicollinearity with WRAT-3 scores. The resulting equation was: MMSEAdj3 = MMSE - [0.176 × (Reading score − 100)] + [0.078 × (age − 70)].
The diagnostic classification accuracy of each demographic adjustment in African American adults was evaluated through logistic regression and receiver operating characteristic (ROC) curves. The positive likelihood ratio (LR+) was estimated as the proportion of African Americans with dementia scoring below an MMSE cut score (sensitivity) to the proportion of African Americans with normal cognition scoring below the cut score (1 – specificity). The posterior probability of dementia at various MMSE cut scores and prevalence rates (.10, .20, and .30) was obtained by converting each prevalence rate to pretest odds (prevalence/1 – prevalence), multiplying the pretest odds by LR+, and converting those odds to probability (posttest odds/(1 + posttest odds).
RESULTS
Participant information
The total sample had a mean age ± standard deviation (SD) of 76.4 ± 7.3 years and mean education of 13.2 ± 3.3 years. African American adults were younger (73.0 ± 7.4) than Caucasian adults (77.0 ± 7.1) (p < .001). African Americans also reported fewer years of education (11.6 ± 3.7) than Caucasian adults (13.5 ± 3.1) (p < .001). Compared to individuals with dementia, elders without dementia were significantly younger (p < .001) and more educated (p < .001). The proportion of African American and Caucasian participants with diagnoses of dementia was 32.6% and 37.7%, respectively (p < .05).
Regression-based demographic adjustments
Caucasian participants obtained significantly higher unadjusted MMSE scores than African American participants, and this discrepancy was evident in the cognitively normal and dementia subsamples (Table 1). Application of the demographic adjustments based on age and years of education (MMSEAdj1 and MMSEAdj2) did not attenuate these group differences in mean MMSE scores. In a hierarchical regression model, quality of education as indexed by WRAT-3 reading scores accounted for significant, unique variance in the prediction of MMSE scores, over and above age and years of education (R2 change = 0.13, p < .001). With age, years of education, and quality of education in the model, ethnicity contributed significant, albeit quite modest incremental variance (R2 change = 0.01, p < .001). Because quality of education appeared to be uniquely associated with the MMSE, we then adjusted MMSE scores for age and quality of education (MMSEAdj3). As shown in Table 1, with this adjustment MMSE scores were not significantly different between cognitively-normal Caucasian and African American adults. However, MMSE scores for Caucasian adults with dementia remained significantly higher than scores for African Americans with dementia.
Table 1.
Mean unadjusted and adjusted MMSE scores by diagnostic status and ethnic group.
| Caucasian | African American | |||
|---|---|---|---|---|
| Mean ± Standard Deviation |
Mean ± Standard Deviation |
t | p | |
| All Participants | ||||
| MMSE | 25.3 ± 5.37 | 23.0 ± 7.44 | 6.11 | <.001 |
| MMSEAdj1 | 25.0 ± 5.39 | 23.1 ± 6.69 | 5.59 | <.001 |
| MMSEAdj2 | 25.1 ± 5.31 | 23.3 ± 6.89 | 5.08 | <.001 |
| MMSEAdj3 | 26.1 ± 4.20 | 27.0 ± 3.98 | −3.50 | <.001 |
| Cognitively Normal | ||||
| MMSE | 28.2 ± 1.60 | 27.3 ± 1.95 | 7.85 | <.001 |
| MMSEAdj1 | 27.8 ± 2.05 | 26.9 ± 2.11 | 7.09 | <.001 |
| MMSEAdj2 | 27.9 ± 1.77 | 27.3 ± 1.89 | 5.16 | <.001 |
| MMSEAdj3 | 28.3 ± 1.75 | 28.4 ± 1.98 | −0.35 | .724 |
| Dementia | ||||
| MMSE | 20.3 ± 5.77 | 14.0 ± 6.48 | 11.05 | <.001 |
| MMSEAdj1 | 20.3 ± 5.93 | 15.3 ± 6.12 | 9.45 | <.001 |
| MMSEAdj2 | 20.4 ± 5.83 | 15.1 ± 6.11 | 10.11 | <.001 |
| MMSEAdj3 | 22.7 ± 4.59 | 20.6 ± 4.67 | 3.32 | <.001 |
Note. MMSEAdj1 = Age and education (years) adjustment based on Mungas et al.5; MMSEAdj2 = age and education (years) adjustment based on Mayo Clinic sample; MMSEAdj3 = age and quality of education (reading score) adjustment based on Mayo Clinic sample.
Demographic adjustments in dementia-matched sample
Because African American adults often present for clinical evaluation at a more advanced stage of cognitive impairment than their Caucasian counterparts, and in light of the persistent discrepancy in MMSE scores noted earlier despite demographic adjustments, we explored whether dementia severity at study entry represented a potential confounder. Indeed, baseline CDR global scores were higher for African American than Caucasian adults (p < .05), with 24.4% of African Americans obtaining a CDR global score ≥ 1 compared to 16.8% of Caucasians.
The two ethnicity groups were matched by baseline CDR global scores and the unadjusted and adjusted MMSE scores were re-examined. Despite matching on dementia severity, unadjusted MMSE scores remained significantly different between Caucasian (25.2 ± 6.2) and African American (23.5 ± 7.0) participants (p < .001). Moreover, this discrepancy in mean MMSE scores was not attenuated when applying adjustments based on age and years of education. The MMSEAdj3 correction using age and quality of education did attenuate group differences (p = .26), resulting in a mean adjusted MMSE score of 26.7 ± 4.4 for Caucasian and 27.0 ± 4.0 for African American adults. The nonsignificant difference in MMSEAdj3 scores was also evident within the cognitively-normal and dementia subsamples. This finding highlights the key roles of quality of education and baseline dementia severity in explaining the existing discrepancies in MMSE scores between Caucasian and African American older adults.
MMSE and dementia classification accuracy in African American older adults
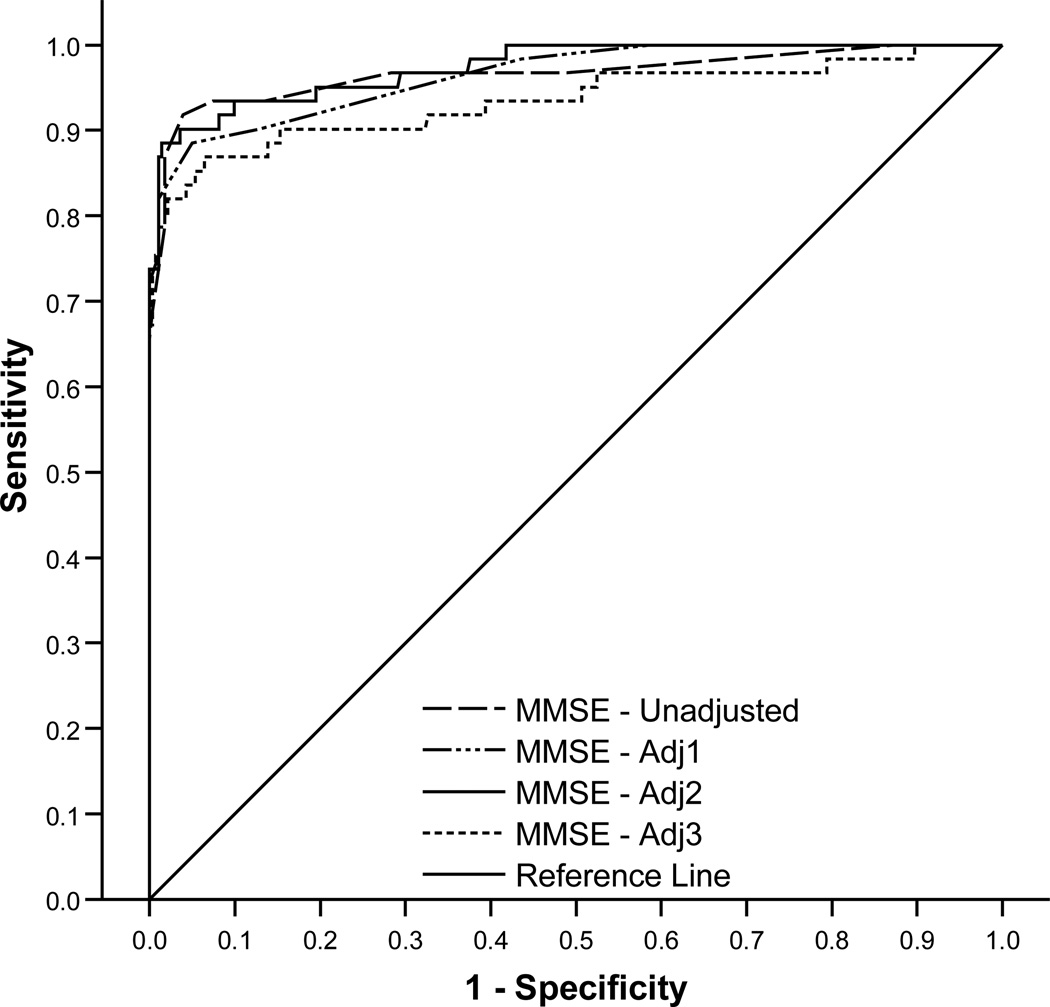
Overall, a cut score of 23/24 in the MMSEAdj2 provided the highest classification accuracy of dementia (0.963), with high sensitivity (0.92) and specificity (0.98). This demographic adjustment, however, yielded only a modest gain in accuracy compared to the unadjusted MMSE cut score of 22/23 (accuracy = .959). Classification accuracy obtained from the MMSEAdj1 and MMSEAdj3 scores was suboptimal across cut scores. In ROC analyses, the areas under the curve were 0.98 for the unadjusted MMSE and MMSEAdj2 scores, 0.97 for the MMSEAdj1 scores, and 0.94 for the MMSEAdj3 scores (Figure 1). When applying these analyses to African American participants in the CDR-matched subsample, the results were nearly identical to those described above and shown in Figure 1.
Figure 1.
Receiver operating characteristic (ROC) curves for unadjusted and adjusted MMSE scores in African Americans.
Note. ROC curves displayed for subsample with all 3 MMSE score adjustments (n=343).
Posterior probability of dementia in African American older adults using unadjusted MMSE scores
Although age- and education-adjustments (MMSEAdj2) yielded a very modest improvement in dementia classification accuracy over the unadjusted MMSE scores, it is likely that many clinicians will use the unadjusted cut score due to its ease of scoring. To facilitate this use, we next provide the posterior probability of dementia as a function of various unadjusted MMSE cut scores and dementia prevalence rates (Table 2). For instance, in a setting with 10% prevalence, an unadjusted MMSE score of 22 suggests that the individual has an 86% probability of dementia.
Table 2.
Posterior probabilities for unadjusted MMSE scores in African Americans at dementia prevalence rates of .10, .20, and .30.
| Cut score | LR+ | Prevalence | Pretest Odds | Posttest Odds | Posterior Probability |
|---|---|---|---|---|---|
| 20/21 | 272.3 | 0.10 | 0.11 | 30.3 | 0.97 |
| 0.20 | 0.25 | 68.1 | 0.99 | ||
| 0.30 | 0.43 | 116.7 | 0.99 | ||
| 21/22 | 50.9 | 0.10 | 0.11 | 5.7 | 0.85 |
| 0.20 | 0.25 | 12.7 | 0.93 | ||
| 0.30 | 0.43 | 21.8 | 0.96 | ||
| 22/23 | 53.4 | 0.10 | 0.11 | 5.9 | 0.86 |
| 0.20 | 0.25 | 13.4 | 0.93 | ||
| 0.30 | 0.43 | 22.9 | 0.96 | ||
| 23/24 | 22.9 | 0.10 | 0.11 | 2.5 | 0.72 |
| 0.20 | 0.25 | 5.7 | 0.85 | ||
| 0.30 | 0.43 | 9.8 | 0.91 | ||
| 24/25 | 11.6 | 0.10 | 0.11 | 1.3 | 0.56 |
| 0.20 | 0.25 | 2.9 | 0.74 | ||
| 0.30 | 0.43 | 5.0 | 0.83 | ||
| 25/26 | 6.3 | 0.10 | 0.11 | 0.7 | 0.41 |
| 0.20 | 0.25 | 1.6 | 0.61 | ||
| 0.30 | 0.43 | 2.7 | 0.73 |
Note. LR=Likelihood ratio.
DISCUSSION
In our sample of 3254 adults aged 60 and older, adjustment for age and quality of education attenuates the significant discrepancy in MMSE scores between cognitively-normal Caucasian and African American elders. Moreover, controlling for age, quality of education, and dementia severity at study entry eliminates the significant discrepancy in MMSE scores across all study participants. These findings underscore the key role that quality, not just quantity, of educational experience has in shaping overall cognitive ability, particularly for African American adults. In our sample, quality of education accounted for 13% of the unique variance in MMSE scores over and above age and years of education.
From a clinical diagnostic standpoint, it is important to know whether these demographic adjustments improve our existing ability to identify dementia in African American adults. We find that optimal dementia classification is obtained when using age- and education-adjustments; specifically, an MMSE cut score of 23/24 derived from our regression formula. However, this represents only a minimal gain in classification accuracy compared to an unadjusted MMSE cut score of 22/23. As such, clinicians may find that the unadjusted MMSE score is preferable to demographically-adjusted scores in settings where calculation of the latter is not time efficient. To this end, we provide a table with estimates of the posterior probability of dementia for African American adults at various MMSE cut scores and rates of dementia prevalence.
Overall, the current study indicates that age, dementia severity at study entry, and quality of educational experience are important explanatory factors to understand the existing discrepancies in MMSE performance between Caucasian and African American older adults. Although adjustments for age and education maximize classification accuracy of dementia in African American adults, the use of unadjusted MMSE cut scores yields sufficiently high classification accuracy to support their use in clinical practice.
ACKNOWLEDGMENTS
This study was supported by the National Institutes of Health (NS054722, AG016574, AG006786).
Sponsor’s Role: Sponsors had no role in the design, methods, analysis, or manuscript preparation of this study.
Footnotes
Conflict of Interest
The authors report no conflict of interest related to this study.
Author Contributions
O. Pedraza, J.H. Clark, S.E. O’Bryant, and J.A. Lucas contributed to the study conception and statistical analyses. All authors contributed equally to the interpretation of the data and preparation of the final manuscript.
REFERENCES
- 1.Folstein MF, Folstein SE, McHugh PR. Mini-mental state: A practical method for grading the cognitive state of patients. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 2.O'Bryant SE, Humphreys JD, Smith GE, et al. Detecting dementia with the Mini-Mental State Examination in highly educated individuals. Arch Neurol. 2008;65:963–967. doi: 10.1001/archneur.65.7.963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bohnstedt M, Fox PJ, Kohatsu ND. Correlates of Mini-Mental Status Examination scores among elderly demented patients: The influence of race-ethnicity. J Clin Epidemiol. 1994;47:1381–1387. doi: 10.1016/0895-4356(94)90082-5. [DOI] [PubMed] [Google Scholar]
- 4.Escorber JI, Burnam A, Karno M, et al. Use of the Mini-Mental State Examination (MMSE) in a community population of mixed ethnicity: Cultural and linguistic factors. J Nerv Ment Dis. 1986;174:607–614. doi: 10.1097/00005053-198610000-00005. [DOI] [PubMed] [Google Scholar]
- 5.Mungas D, Marshall SC, Weldon M, et al. Age and education correction of Mini-Mental State Examination for English and Spanish-speaking elderly. Neurology. 1996;46:700–706. doi: 10.1212/wnl.46.3.700. [DOI] [PubMed] [Google Scholar]
- 6.Ivnik RJ, Malec JF, Smith GE, et al. Mayo’s Older Americans Normative Studies: WAIS-R norms for ages 56 to 97. Clin Neuropsychol. 1992;6:1–30. [Google Scholar]
- 7.Morris JC. Clinical Dementia Rating: A reliable and valid diagnostic and staging measure for dementia of the Alzheimer’s type. Int Psychogeriatr. 1997;9:173–178. doi: 10.1017/s1041610297004870. [DOI] [PubMed] [Google Scholar]
- 8.Wilkinson GS. WRAT-3: Wide Range Achievement Test Administration Manual. Washington, DC: Wide Range Inc.; 1993. [Google Scholar]
- 9.Manly JJ, Jacobs DM, Touradji P, et al. Reading level attenuates differences in neuropsychological test performance between African American and White elders. J Int Neuropsychol Soc. 2002;8:341–348. doi: 10.1017/s1355617702813157. [DOI] [PubMed] [Google Scholar]
- 10.Manly JJ, Byrd DA, Touradji P, et al. Acculturation, reading level, and neuropsychological test performance among African American elders. Appl Neuropsychol. 2004;11:37–46. doi: 10.1207/s15324826an1101_5. [DOI] [PubMed] [Google Scholar]