Abstract
OBJECTIVES
To examine the association between the use of compensatory strategies to successfully complete common daily activities — an indicator of pre-clinical disability— and body mass in pre-clinically disabled older adults.
DESIGN
Cross-sectional observational study.
PARTICIPANTS
Two-hundred and fifty-nine pre-clinically disabled older adults defined as having changed the frequency or manner of performing daily tasks without reporting any difficulty.
MEASUREMENTS
The use of compensatory strategies were objectively evaluated using the MOD scale — a reliable and valid scale for assessing the manner in which common daily activities were completed. Height and weight were measured to classify participants into the following body mass index (BMI) categories: 1) normal: 18.5–24.9kg/m2, 2) overweight: 25.0–29.9kg/m2, 3) obese class I: 30.0–34.9kg/m2, and 4) obese class II: 35.0–39.9kg/m2.
RESULTS
Compared to other BMI categories, individuals with class II obesity demonstrated a significantly higher probability of using ≥ 1 compensatory strategies when rising from a chair (30cm height), kneel to stand, stair ascent, stair descent, and supine to stand tasks. When summarized over all tasks, individuals with class II obesity were 18 times more likely to use extensive compensatory strategies (≥ 6 on MOD scale) compared to normal weight older adults. Similar trends at a lesser magnitude were found in obese and overweight compared to normal weight older adults.
CONCLUSION
Obesity is associated with extensive use of compensatory strategies when performing common daily tasks prior to the onset of perceived difficulty, thus placing them at higher risk of disability compared to their peers with lower body mass.
Keywords: Body mass, Functional task modification, Disablement, preclinical disability, obesity, compensatory strategies
1. Introduction
As life expectancy in the United States continues to rise, the maintenance of physical independence among older adults has emerged as a major public health priority. Obesity in older adults has consistently been found to increase the risk for functional decline and the development of mobility disability in aging populations (Ferraro et al., 2002; Peeters et al., 2004). Additionally, obesity-related disability is associated with significant burden in terms of both quality of life and healthcare costs (Fontaine and Barofsky, 2001). Alarmingly, the number and proportion of older, obese adults has increased dramatically over the past two decades (Flegal et al., 2010). Recent estimates indicate that a disturbing 35% of older adults are obese and another 33% are overweight, placing them at risk for obesity (Flegal et al., 2010). This rise in an older, obese adult population and associated risk of physical disability has led to increased efforts to identify high risk individuals that are ideal recipients for strategies to prevent the onset of disability.
Physical disability in older adults typically occurs through two pathways: catastrophic events (e.g., ischemic stroke, accidents and fractures) or gradual progression over time. Regarding the latter, recent evidence suggests that subtle, but measurable transitions occur prior to the onset of outright disability (Fried et al., 1991; Fried et al., 2001; Petrella and Cress, 2004; Wolinsky et al., 2005). These subtle transitions are signified by the adoption of compensatory strategies to cope with environmental demands (e.g. using the handrail on the stairs or arm rests on a chair to push off). As such, using compensatory strategies marks an initial step that denotes how underlying functional impairments eventually manifest into disabling conditions realized in the environment. Fried and colleagues were the first to describe this transition and labeled it pre-clinical disability – as it provides an early warning sign in the disablement process. Adults who are pre clinically disabled are characterized as individuals who do not perceive difficulty but report modifying the method or frequency of daily tasks (Fried et al., 1996; Fried et al., 1991; Petrella and Cress, 2004). Previous research has demonstrated that older adults who are pre-clinically disabled have significantly lower physical function and are at high risk for outright disability (Fried et al., 2000; Manty et al., 2007; Petrella and Cress, 2004; West et al., 2005).
Before moving forward, there are some semantic issues regarding the term “pre-clinical” disability. Throughout the literature, researchers have use the terms “pre-clinical” and “sub-clinical” interchangeably. Such semantic differences have led to disputes regarding the appropriate terminology, as the use of “pre-“ and “sub-“ have important distinctions. Traditionally, pre-clinical disease refers to a disease that is not yet clinically apparent, but is designed to progress to clinical disease. However, the term subclinical disease is typically reserved for a condition that is not yet clinically apparent and is not destined to become clinically apparent. Based on these descriptions, arguably the term sub-clinical disability is better suited for the stage of disablement under discussion, considering that progression to disability is not inevitable. However, while we acknowledge these terminology distinctions, we choose to use “pre-clinical” disability throughout the current article as it has been historically used in the literature.
Researchers most commonly assess pre-clinical disability using self-report (Fried et al., 2000; Fried et al., 1996; Fried et al., 2001; Petrella and Cress, 2004; Wolinsky et al., 2005). To improve the objective measurement of compensatory strategies, Manini and colleagues developed and validated the Modification (MOD) scale — a semi-Gutman rating scale to categorize the severity of compensatory strategies used during common daily tasks (Manini et al., 2006). Specifically, the MOD scale uses an index designed to quantify the number of task modifications used to facilitate performance during chair rising from different heights, stair ascending and descending, rising from a kneeling and supine position, and lifting and carrying a weighted basket. MOD scale scores are associated with objective measures of physical function and self-reported physical function (Manini et al., 2006). Importantly, the MOD scale, when used in combination with self-report measures, can serve to comprehensively assess the use of compensatory strategies and help to identify persons who are pre-clinically disabled.
The purpose of the current study was to examine the association between the use of compensatory strategies— an indicator of pre-clinical disability— and body mass. Expanding knowledge on this topic would provide an understanding of the increased risk on physical disability that obesity imposes. Due to physical limitations imposed by increased body mass, obesity likely plays an influential role in whether older adults require compensatory strategies to navigate their environment. Therefore, we hypothesize that body mass index will be positively associated with the use of compensatory strategies to successfully complete a battery of common daily tasks.
2. Materials and Methods
2.1 Participants
The data in this report is ancillary to an intervention study with the purpose of recruiting adults who are pre-clinically disabled > 60 years of age. Potential participants were independently living community dwellers recruited through advertisements posted in local newspapers and mass mailings sent to residents over the age of 60 years within a 50-mile radius of the center. Four hundred forty-six participants responded and were screened by telephone. To isolate the influence of the independent variable, obesity, as much as possible and its association with the performance of daily tasks, inclusion and exclusion criteria were identified to best rule out factors that might contribute to the need for participants to use compensatory strategies when performing daily tasks. Thus, during the telephone screen, participants were asked whether a doctor had told them they had any of the following conditions in the last six months: coronary, myocardial infarction, heart attack, valvular disease, or stroke. Additionally, participants were asked whether they currently had any of the following conditions: chronic hepatitis, inflammation of the liver, cirrhosis, neurological condition, symptomatic rheumatoid arthritis or osteoarthritis that limits mobility, anemia, serious emotional problems or mental illness, chronic kidney disease, and fracture and joint replacement in the past 6 months. Twenty-six participants were excluded because they had one or more of the aforementioned conditions. Eighty-four participants were excluded for other reasons including: exercising more than 125 minutes/week (i.e., to rule out the effects of chronic exercise behaviors), moving out of area, and not willing to participate in all of study procedures.
The presence of pre-clinical disability status was determined on the telephone using established criteria originally developed by Fried et al (Fried et al., 1996; Fried et al., 1991; Miller et al., 2006). We defined pre-clinical disability as a change in frequency or modification of daily task performance without having overt difficulty completing a particular task. During the phone interview potential participants were asked “Do you have any difficulty performing …” five tasks, including: walking half a mile, climbing a flight of stairs, stooping, crouching, or kneeling, getting up off the floor, or lifting something as heavy as 10 pounds. Those who reported a little, some or a lot of difficulty were excluded because they had surpassed what we considered a stage of pre-clinical disability and were defined in this study as having a disability. Therefore, potential participants reporting any difficulty walking half a mile, climbing a flight of stairs, stooping, crouching, or kneeling, getting up off the floor, or lifting something as heavy as 10 pounds were not invited for testing (n = 52). For participants not reporting difficulty a follow-up question asked “Compared to when you were 40 years of age, have you modified or changed the frequency in which you…” performed the same five tasks. Individuals who reported modifying or changing the frequency of any the tasks performed were considered to have pre-clinical disability. Fourteen participants had no difficulty and did not change the frequency or modify daily tasks. Two hundred-seventy participants reported no difficulty and changed the frequency or modified daily tasks, and thus were considered to have pre-clinical disability and be eligible for laboratory assessments. The University of Florida Institutional Review Board reviewed and approved the protocol. All participants gave written informed consent prior to their enrollment in the study.
2.2. Objective measures of compensatory strategies
We objectively measured modifications in a laboratory setting using a reliable and valid performance scale developed to specifically rank the severity of compensatory strategies used during a battery of 8 tasks – The MOD scale (full details of the MOD scale are described in Manini et al 2006, 2007 (Manini et al., 2006; Manini et al., 2007). Participants performed a chair rise from three different seat pan heights (43cm, 38cm, and 30cm), a kneel to stand, stair ascent, stair descent, a supine to stand, and lifting and carrying a laundry basket filled with 10% of a participant’s body mass. The MOD scale ranked participants’ performance on each task from 0–5 according to the severity of compensatory strategy to complete the task. Previous research has demonstrated that the MOD scale has good test-retest reliability (interclass correlation coefficient > 0.90), compares well with established measures of functional and muscular performance (Manini et al., 2006), and is sensitive to change during a behavioral intervention (Manini et al., 2007).
Scores on the MOD scale were summed and expressed descriptively from 0 to 40 where a higher total MOD score represented greater use of compensatory strategies to complete the tasks or inability to perform the tasks. For analysis purposes, we also dichotomized individuals at a total MOD ≥ 6, which represents a MOD score at the highest third of the sample (N=82). This cutoff score highlights individuals using severe modifications on at least two tasks or consistently using less severe modifications on several tasks.
2.3. Measurement of BMI
Height and weight were measured with participants wearing light clothing and without shoes. A wall-mounted stadiometer (Seca Inc Hanover, MD) graduated in centimeters with a horizontal measuring block was used to measure height recorded to the nearest 0.1 cm as participants stood erect looking forward. Weight was measured in kilograms using a standard certified scale (Detecto Inc. Webb City, Missouri). BMI was calculated with following formula: kilograms/(height in meters)2. According to standards of the World Health Organization, participants were classified into the following BMI categories: 1) normal: 18.5–24.9 kg/m2, 2) overweight: 25.0–29.9 kg/m2, 3) obese class I: 30.0–34.9 kg/m2, and 4) obese class II: 35.0–39.9 kg/m2.
2.4. Data Analysis
Comparisons of baseline characteristics across groups were evaluated using Chi-square for categorical variables (gender, race) and analysis of variance (ANOVA) for continuous variables (age). Comparisons in MOD scores between BMI categories for each task were performed using one-way ANOVAs. The predicted probability (adjusted age, race and gender) for having a MOD score ≥ 1 was calculated for each BMI category across all tasks performed. Next, we examined the association between MOD scale score and BMI using multivariate regressions. Logistic regression was used to examine 1) the association between BMI expressed in kg/m2 and total MOD score that ranged from 0 to 40 and 2) the dichotomized total MOD score (MOD ≥ 6), which represented the highest third (coded as one) or lowest two-thirds (coded as zero) of the total MOD distribution. Models were acquired with and without adjustments for covariates which included age, gender, and race. Statistical significance for all analyses was set at p ≤ 0.05. Statistical analyses were done using STATA SE (Version 10.0; College Station, TX).
3. Results
Eleven participants did not undertake some tasks and the results reflect only those who completed all tasks (N=259). Table 1 summarizes data across each BMI category. There were no significant differences in gender or race groups across BMI categories. However, obese class I and class II adults were younger than other BMI categories (p < 0.001). Additionally, MOD scores were generally higher with increasing BMI on the kneel to stand, stair ascent, stair descent, and supine to stand. On average, individuals with class II obesity exhibited approximately 3 additional compensatory strategies when compared to other BMI categories.
Table 1.
Baseline Characteristics and Descriptive Statistics of Scores on MOD Scale of Participants Stratified by BMI Category.a
| Total (n = 259) | Normal (n = 68) | Overweight (n = 92) | Class I Obesity (n = 57) | Class II Obesity (n = 42) | Group difference p-value | |
|---|---|---|---|---|---|---|
| Characteristics | ||||||
| Age, mean (SD), y | 67.6 (7.0) | 69.68 (8.1) | 68.4 (7.1) | 65.9 (5.7) | 64.8 (5.1) | <0.001 |
| Gender, No male (%) | 116 (45.0) | 23 (33.8) | 45 (48.9) | 25 (44.6) | 23 (54.8) | 0.132 |
| Race, No Caucasian (%) | 228 (88.7) | 64 (94.1) | 77 (84.6) | 50 (89.3) | 37 (88.1) | 0.315 |
| 43 cm chair rise, MOD score | 0.39 (.73) | 0.38 (.73) | 0.35 (.70) | 0.40 (.68) | 0.50 (.83) | 0.732 |
| 38 cm chair rise, MOD score | 0.62 (.73) | 0.48 (.76) | 0.66 (.87) | 0.70 (.84) | 0.62 (.79) | 0.456 |
| 30 cm chair rise, MOD score | 0.78 (1.00) | 0.66 (.97) | 0.76 (1.01) | 0.72 (.96) | 1.10 (1.05) | 0.150 |
| Kneel to stand, MOD score | 0.94 (1.14) | 0.76 (1.05) | 0.82 (1.13) | 0.96 (1.13) | 1.48 (1.21) | 0.007 |
| Stair ascent, MOD score | 0.35 (.86) | 0.28 (.73) | 0.26 (.71) | 0.25 (.61) | 0.81 (1.37) | 0.002 |
| Stair descent, MOD score | 0.61 (1.10) | 0.59 (1.00) | 0.55 (1.07) | 0.35 (.72) | 1.09 (1.52) | 0.008 |
| Supine to stand, MOD score | 1.20 (1.23) | 0.85 (1.11) | 1.19 (1.25) | 1.19 (1.20) | 1.79 (1.20) | 0.002 |
| Lift & carry, MOD score | 0.16 (.64) | 0.15 (.65) | 0.13 (.47) | 0.21 (.73) | 0.19 (.83) | 0.883 |
| Total MOD, MOD score | 5.53 (5.68) | 4.64 (5.20) | 5.26 (6.05) | 5.10 (4.93) | 8.14 (5.96) | 0.011 |
Values are expressed as number (percentage) or mean (standard deviation) unless otherwise stated.
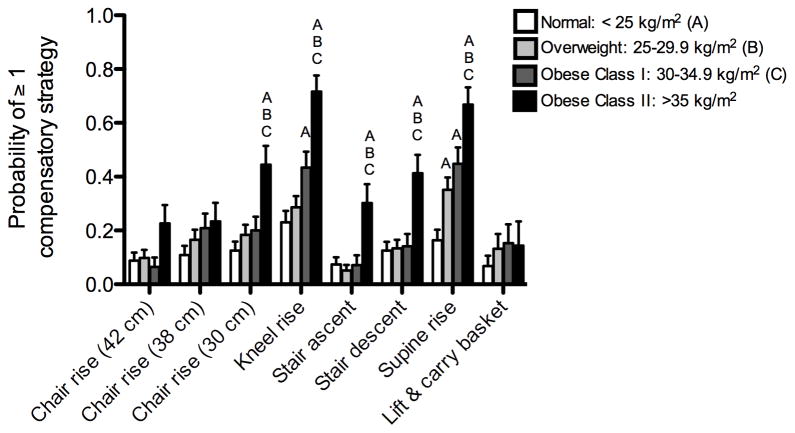
Figure 1 illustrates the adjusted probability of using ≥ 1 compensatory strategy on the MOD scale. As demonstrated by Figure 1, individuals with class II obesity were more likely to use compensatory strategies when rising from a chair with a seat height of 30 cm than individuals categorized normal weight (p = 0.001), overweight (p = 0.008) and obese class I (p = 0.029). For the kneel rise, class II obesity was associated with a higher probability of using one or more compensatory strategies compared to individuals categorized as normal weight (p < 0.001) overweight (p < 0.001) and obese class I (p = 0.008). Additionally, class I obesity had a higher probability of using one or more compensatory strategies than the normal weight group (p = 0.027). Individuals categorized as obese class II were more likely to use compensatory strategies while ascending and descending the stairs compared to normal (p < 0.02), overweight (p < 0.02) and obese class I (p < 0.02) groups. The obese class II group had a higher likelihood of using one or more compensatory strategies while rising from a supine position on the floor than all other groups (all p-values < 0.04). Individuals categorized as overweight and obese class I were more likely to use compensatory strategies rising from the floor than the normal weight group (p values < 0.05). No significant differences were noted for rising from chairs with a height of 42 cm and 38 cm, and lifting then carrying a weighted basket.
Figure 1.
The adjusted (adjusted for age, gender and race) probability of using ≥ 1 compensatory strategy on each task of the MOD scale across BMI categories. Statistically significant differences are expressed with letters: A = significant difference compared to Normal (p < 0.05). B = significant difference compared to Overweight (p < 0.05). C = significant difference compared to Obese class 1 (p < 0.05).
Table 2 illustrates the results from logistic regression analyses. In the adjusted model, each unit of BMI was associated with an increase in 0.16 MOD score (p < 0.001). Logistic regression analyses revealed that having class II obesity was significantly associated with a high probability of using ≥ 6 compensatory strategies (all p values were < .001). Following adjustments for age, gender, and race, participants in the class II obesity category were 18.69 times more likely to use ≥ 6 compensatory strategies compared to participants in the normal BMI category. In the adjusted model, being overweight (p=.056) or class I obese (p=.065) conferred a higher odds of using ≥ 6 compensatory strategies that approached statistical significance. Additional analyses found no interaction between BMI category and age, gender, or race on the probability of using ≥ 6 compensatory strategies.
Table 2.
Odds Ratio of Logistic Regression Models
| Odds Ratio (95% CI) | Odds Ratio (95% CI) | |
|---|---|---|
| Unadjusted | Adjusteda | |
| Per unit BMIb | 1.07 (1.03–1.13) | 1.16 (1.09–1.23) |
| BMI categories | ||
| <24.9 kg/m2 | 1.0 | 1.0 |
| 25.0–29.9 kg/m2 | 1.47 (0.71–3.04) | 2.28 (0.98–5.31) |
| 30.0–34.9 kg/m2 | 1.15 (0.501–2.64) | 2.48 (0.94–6.54) |
| >35 kg/m2 | 4.71 (2.04–10.89 | 18.69 (6.44–54.19) |
| p-value for trend | 0.002 | <0.001 |
Adjusted for age, gender, and race
BMI is used a continuous variable in the model.
BMI = Body Mass Index
4. Discussion
The results from this study provide novel information and support our hypothesis regarding the relationship between obesity and using compensatory strategies on common daily tasks in older adults who are pre-clinically disabled. The data indicate that class II obesity in this population is an important predictor for using compensatory strategies to complete a physical task even after accounting for age, gender, and race. In particular, compensatory strategies were most prevalent among this group when performing the low chair rise, kneel to stand, stair ascent and descent, and supine to stand tasks. Importantly, we observed that obese individuals need to perform numerous compensatory strategies despite their report of having no difficulty performing the same tasks. Moreover, these individuals were thoroughly screened for several potentially disabling disease conditions (e.g., severe osteoarthritis, cardiovascular disease) and represented relatively healthy older adults. Furthermore, adults with class I and II obesity were younger than the overweight and normal weight adults indicating that age-related changes were unlikely to explain the findings. Overall, the data suggest that obese individuals who report no outright difficulty executing physical tasks are successfully performing these tasks in a manner that predisposes them to a high risk of future disability.
The present findings corroborate previous evidence demonstrating a consistent association between heightened body mass and compromised ability to perform mobility tasks, particularly those involving the lower body or transferring body weight (Vincent et al., 2010b; Sharkey et al., 2006; Apovian et al., 2002). For example, Sharkey et al. found that higher BMIs were associated with a progressive increase for the inability to perform a repeated chair rise test (Sharkey et al., 2006). Additionally, Apovian and colleagues found that the median time for climbing a standard set of stairs was almost 30% higher among individuals with class I or II obesity compared to normal weight individuals (Apovian et al., 2002). Prospective longitudinal studies have also supported the notion that disability risk is higher for obese compared to non-obese persons (Ferraro et al., 2002; Peeters et al., 2004). Adding to this body of knowledge, the current study documented for the first time the association between obesity and the earliest signs of functional limitations becoming apparent in a variety of environmental situations that involve completing daily tasks. These results suggest that obesity class I and II result in an extensive use of compensatory strategies on common daily tasks prior to the onset of perceived difficulty performing those tasks, thus placing obese older adults with class I and II at higher risk of disablement compared to their peers with lower BMIs.
Several mechanisms might account for why obesity is closely related to using compensatory strategies. First, as body mass increases, the energy and strength required to position the body increases correspondingly (Ko et al., 2010; Messier et al., 2011). In particular, excess body mass produces biomechanical burden to the lower extremity joints (Ko et al., 2010; Lai et al., 2008). For example, Browning et al. demonstrated that total knee generative mechanical work expenditure is higher in older obese adults compared to non-obese older adults (Browning and Kram, 2007). The exacerbated load and energy burdens placed on the lower limb joints likely trigger activity avoidance or modification of daily task performance. Additionally, as aging is generally associated with progressive muscle weakness and increased muscular fat infiltration (Delmonico et al., 2009), the combination of obesity and age-related muscle weakness may encourage task modification in older adults (Manini and Clark, 2011).
Interestingly, the current study found no relationship between obesity and the upper-body related task: the lift and carry of a weighted basket. This finding is in line with previous work showing that obese individuals have a higher likelihood of experiencing lower-extremity mobility difficulties than upper-extremity mobility difficulties (Weil et al., 2002). Additional research has suggested that across the spectrum of physical tasks, activities involving the lower-extremities are significantly more difficult to maintain during the progression of disability compared to activities primarily involving the upper-extremities (Ferrucci et al., 1998). Data from the current study support these notions and suggest that class I and II obesity is especially detrimental to performing tasks that require the lower-extremity region even in older adults who report no difficulty performing common daily tasks.
This study has a number of limitations. First, because the current study was cross-sectional, the findings cannot establish whether obesity is a cause or consequence of increased use of compensatory strategies during common daily tasks. Second, compensatory strategies can involve not only modifying the method, but also the frequency of daily task performance —the current study only examined alterations in the method of performance. Given that excess weight could also trigger a fear of movement leading to task avoidance (Vincent et al., 2010a), a relationship might also exist between obesity and frequency of performing daily tasks in adults who are pre-clinically disabled. Finally, the study population was predominantly healthy Caucasians between 60 and 100 years of age, which limits generalizability to other age and ethnic groups.
In conclusion, the findings from the current study demonstrate that obesity represents a key factor involved in whether compensatory strategies are used to facilitate successful completion of physical tasks in older adults who report no signs of difficulty. This finding was most pronounced in older adults with class II obesity and was magnified in lower-extremity tasks that included the kneel to stand, stair ascent/descent, and supine to stand tasks. Additional research is necessary to determine the mechanisms underlying the association between extensive use of compensatory strategies and obesity in pre-clinical disability.
Acknowledgments
Sources of funding: This research was supported by National Institutes of Health (5R21AG031974-02 to T.M.M.) and in part by the NIA Claude D. Pepper Center (P30AG028740 to T.M.M.). The sponsors of the project had no role in the study.
Footnotes
Conflict of interest statement
The authors report no conflict of interest regarding any financial and personal relationships with other people or organizations that could in appropriately influence their work.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Apovian CM, Frey CM, Wood GC, Rogers JZ, Still CD, Jensen GL. Body mass index and physical function in older women. Obes Res. 2002;10:740–747. doi: 10.1038/oby.2002.101. [DOI] [PubMed] [Google Scholar]
- Browning RC, Kram R. Effects of obesity on the biomechanics of walking at different speeds. Med Sci Sports Exercise. 2007;39:1632–1641. doi: 10.1249/mss.0b013e318076b54b. [DOI] [PubMed] [Google Scholar]
- Delmonico MJ, Harris TB, Visser M, Park SW, Conroy MB, Velasquez-Mieyer P, Boudreau R, Manini TM, Nevitt M, Newman AB, Goodpaster BH. Longitudinal study of muscle strength, quality, and adipose tissue infiltration. Am J Clin Nutr. 2009;90:1579–1585. doi: 10.3945/ajcn.2009.28047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferraro KF, Su YP, Gretebeck RJ, Black DR, Badylak SF. Body mass index and disability in adulthood: a 20-year panel study. Am J Public Health. 2002;92:834–840. doi: 10.2105/ajph.92.5.834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrucci L, Guralnik JM, Cecchi F, Marchionni N, Salani B, Kasper J, Celli R, Giardini S, Heikkinen E, Jylha M, Baroni A. Constant hierarchic patterns of physical functioning across seven populations in five countries. The Gerontologist. 1998;38:286–294. doi: 10.1093/geront/38.3.286. [DOI] [PubMed] [Google Scholar]
- Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999–2008. JAMA. 2010;303:235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- Fontaine KR, Barofsky I. Obesity and health-related quality of life. Obes Rev. 2001;2:173–182. doi: 10.1046/j.1467-789x.2001.00032.x. [DOI] [PubMed] [Google Scholar]
- Fried LP, Bandeen-Roche K, Chaves PH, Johnson BA. Preclinical mobility disability predicts incident mobility disability in older women. J Gerontol A Biol Sci Med Sci. 2000;55:M43–52. doi: 10.1093/gerona/55.1.m43. [DOI] [PubMed] [Google Scholar]
- Fried LP, Bandeen-Roche K, Williamson JD, Prasada-Rao P, Chee E, Tepper S, Rubin GS. Functional decline in older adults: expanding methods of ascertainment. J Gerontol A Biol Sci Med Sci. 1996;51A:M206–214. doi: 10.1093/gerona/51a.5.m206. [DOI] [PubMed] [Google Scholar]
- Fried LP, Herdman SJ, Kuhn KE, Rubin G, Turano K. Preclinical disability: hypotheses about the bottom of the iceberg. J Aging Health. 1991;3:285–300. [Google Scholar]
- Fried LP, Young Y, Rubin G, Bandeen-Roche K. Self-reported preclinical disability identifies older women with early declines in performance and early disease. J Clin Epidemiology. 2001;54:889–901. doi: 10.1016/s0895-4356(01)00357-2. [DOI] [PubMed] [Google Scholar]
- Ko S, Stenholm S, Ferrucci L. Characteristic gait patterns in older adults with obesity--results from the Baltimore Longitudinal Study of Aging. J Biomech. 2010;43:1104–1110. doi: 10.1016/j.jbiomech.2009.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai PP, Leung AK, Li AN, Zhang M. Three-dimensional gait analysis of obese adults. Clin Biomech. 2008;23(Suppl 1):S2–6. doi: 10.1016/j.clinbiomech.2008.02.004. [DOI] [PubMed] [Google Scholar]
- Manini TM, Clark BC. Dynapenia and Aging: An Update. J Gerontol A Biol Sci Med Sci. 2011 doi: 10.1093/gerona/glr010. Epub Mar 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manini TM, Cook SB, VanArnam T, Marko M, Ploutz-Snyder L. Evaluating task modification as an objective measure of functional limitation: repeatability and comparability. J Gerontol A Biol Sci Med Sci. 2006;61:718–725. doi: 10.1093/gerona/61.7.718. [DOI] [PubMed] [Google Scholar]
- Manini TM, Marko M, Van Arnam T, Cook SB, Fernhall B, Burke JM, Ploutz-Snyder L. Efficacy of resistance and task-specific exercise in older adults who modify tasks of everyday life. J Gerontol A Biol Sci Med Sci. 2007;62:616–623. doi: 10.1093/gerona/62.6.616. [DOI] [PubMed] [Google Scholar]
- Manty M, Heinonen A, Leinonen R, Tormakangas T, Sakari-Rantala R, Hirvensalo M, von Bonsdorff MB, Rantanen T. Construct and predictive validity of a self-reported measure of preclinical mobility limitation. Arch Phys Med Rehabil. 2007;88:1108–1113. doi: 10.1016/j.apmr.2007.06.016. [DOI] [PubMed] [Google Scholar]
- Messier SP, Legault C, Loeser RF, Van Arsdale SJ, Davis C, Ettinger WH, DeVita P. Does high weight loss in older adults with knee osteoarthritis affect bone-on-bone joint loads and muscle forces during walking? Osteoarthritis and Cartilage. 2011;19:272–280. doi: 10.1016/j.joca.2010.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller DK, Andresen EM, Malmstrom TK, Miller JP, Wolinsky FD. Test-retest reliability of subclinical status for functional limitation and disability. J Gerontol B Psychol Sci Soc Sci. 2006;61:S52–56. doi: 10.1093/geronb/61.1.s52. [DOI] [PubMed] [Google Scholar]
- Peeters A, Bonneux L, Nusselder WJ, De Laet C, Barendregt JJ. Adult obesity and the burden of disability throughout life. Obes Res. 2004;12:1145–1151. doi: 10.1038/oby.2004.143. [DOI] [PubMed] [Google Scholar]
- Petrella JK, Cress ME. Daily ambulation activity and task performance in community-dwelling older adults aged 63–71 years with preclinical disability. J Gerontol A Biol Sci Med Sci. 2004;59:264–267. doi: 10.1093/gerona/59.3.m264. [DOI] [PubMed] [Google Scholar]
- Sharkey JR, Ory MG, Branch LG. Severe elder obesity and 1-year diminished lower extremity physical performance in homebound older adults. J Am Geriatrics Soc. 2006;54:1407–1413. doi: 10.1111/j.1532-5415.2006.00842.x. [DOI] [PubMed] [Google Scholar]
- Vincent HK, Lamb KM, Day TI, Tillman SM, Vincent KR, George SZ. Morbid obesity is associated with fear of movement and lower quality of life in patients with knee pain-related diagnoses. PM & R : The Journal of Injury, Function, and Rehabilitation. 2010a;2:713–722. doi: 10.1016/j.pmrj.2010.04.027. [DOI] [PubMed] [Google Scholar]
- Vincent HK, Vincent KR, Lamb KM. Obesity and mobility disability in the older adult. Obes Rev. 2010b;11:568–579. doi: 10.1111/j.1467-789X.2009.00703.x. [DOI] [PubMed] [Google Scholar]
- Weil E, Wachterman M, McCarthy EP, Davis RB, O’Day B, Iezzoni LI, Wee CC. Obesity among adults with disabling conditions. JAMA. 2002;288:1265–1268. doi: 10.1001/jama.288.10.1265. [DOI] [PubMed] [Google Scholar]
- West SK, Munoz B, Rubin GS, Bandeen-Roche K, Broman AT, Turano KA. Compensatory strategy use identifies risk of incident disability for the visually impaired. Arch of Ophthalmology. 2005;123:1242–1247. doi: 10.1001/archopht.123.9.1242. [DOI] [PubMed] [Google Scholar]
- Wolinsky FD, Miller DK, Andresen EM, Malmstrom TK, Miller JP. Further evidence for the importance of subclinical functional limitation and subclinical disability assessment in gerontology and geriatrics. J Gerontol B Psychol Sci Soc Sci. 2005;60:S146–151. doi: 10.1093/geronb/60.3.s146. [DOI] [PubMed] [Google Scholar]