Abstract
Objective
This study examined the association between alcohol use and sexual behaviors among South African adults who reported current drinking.
Method
Street-intercept surveys were administered to adults residing in neighborhoods in South African townships.
Results
Analyses were restricted to participants reporting current drinking (N = 1,285; mean age = 32; 27% women; 98% Black). Most participants (60%) reported heavy episodic drinking (i.e., 5 or more drinks on a single occasion) at least once per week in the past 30 days. Compared to non-heavy episodic drinkers, participants who reported heavy episodic drinking were more likely to drink before sex (79% vs. 66%) and have sex with a partner who had been drinking (59% vs. 44%). Overall, drinking before sex (self or partner) and heavy episodic drinking was associated with multiple sexual partners, discussing condom use with sexual partner(s), and proportion of protected sex. The frequency of condom use varied among participants with steady, casual, or both steady and casual sexual partners.
Conclusions
Alcohol use among South African adults is associated with sexual risk behaviors, but this association differs by partner type. Findings suggest the need to strengthen alcohol use components in sexual risk reduction interventions especially for participants with both steady and casual sex partners.
Keywords: alcohol, South Africa, sexual risk, heavy episodic drinking, HIV
1. INTRODUCTION
South Africa has the highest prevalence of HIV in the world with an estimated 5.6 million South Africans living with HIV (UNAIDS, 2010). In addition to bearing the heaviest HIV burden, South Africa also has the highest levels of alcohol consumption per adult drinker than any other region in the world (Rehm et al., 2003). According to the 2003 South African Demographic and Health Survey, 30% of South African men and 17% of women report current alcohol use with 12% of men and 14% of women reporting hazardous or harmful levels of alcohol consumption (South African Medical Research Council, 2007). Approximately one-third of South African adults reported heavy episodic drinking (Peltzer & Ramlagan, 2009). Heavy episodic drinking (HED) is defined as drinking 5 or more drinks on a single occasion during the past week (World Health Organization, 2011).
The HIV epidemic in South Africa is associated, in part, with alcohol use (Fisher, Bang, & Kapiga, 2007). Risky alcohol consumption in South Africa has increased in recent years, partially due to the increased consumption of commercial alcoholic beverages with higher alcohol content then traditional homebrews (Parry et al., 2005; Peltzer & Ramlagan, 2009). Environments where alcohol is consumed, such as drinking venues, are frequently associated with sexual behaviors conferring risk for HIV infection (Fritz, Morojele, & Kalichman, 2010). Research shows that participants who meet sexual partners at drinking venues are more likely to have multiple sexual partners and more unprotected sex than those who did not meet their partners at drinking venues (Kalichman, Simbayi, Vermaak, Jooste, & Cain, 2008). Informal alcohol serving establishments, such as small bars and private homes where alcoholic beverages are sold and served, popularly known as “shebeens,” are often places where sex partners meet (Kalichman, Simbayi, Vermaak, Jooste, et al., 2008; Morojele et al., 2006; Weir et al., 2003). Furthermore, sex between new or casual partners often occurs at or around drinking venues (Kalichman, Simbayi, Vermaak, Jooste, et al., 2008; Morojele, et al., 2006; Myer, Matthews, & Little, 2002). Finally, Kalichman et al. (2008) showed that meeting sexual partners in shebeens is associated with problem drinking. The association between alcohol use and sexual risk behaviors suggests that importance of examining high risk alcohol use (i.e., HED) as well as contextual factors (i.e., drinking before sex or partner drinking before sex) associated with sexual risk and prevention behaviors.
Consuming large quantities of alcohol (e.g., HED), but not the frequency of drinking, is associated with having more sexual partners, unprotected sex, and concurrent sexual partners (Kalichman, Simbayi, Kaufman, Cain, & Jooste, 2007). A recent meta-analysis examining the association between alcohol use and HIV from studies conducted in Africa (Fisher, et al., 2007) found drinker status to be associated with HIV infection such that drinkers were 70% more likely to be HIV-positive than non-drinkers. Risk of HIV was notably higher among problem drinkers vs. non-problem drinkers. Baliunas, Rehm, Irving, and Shuper (2010) found the incidence of HIV was associated with overall level of alcohol consumption. Moreover, risk of HIV infection among heavy episodic drinkers was double that of non-heavy episodic drinkers. HED is a risk factor in the transmission of HIV.
Efforts to understand alcohol-related risks must also take into account the context in which alcohol is consumed. Alcohol consumption, before or during sex, is associated with sexual behaviors that may increase the risk of acquiring HIV infection (Baliunas, et al., 2010). For example, Simbayi et al. (2004) found alcohol use before sex was associated with multiple sexual partners and more unprotected sexual occasions among patients at a South African sexually transmitted disease (STD) clinic. Among HIV+ South Africans, drinking before sex was associated with unprotected sex but only when participants consumed greater amounts of alcohol (Kiene et al., 2008). Heavy episodic drinkers may consume more alcohol during sexual events because they drink more alcohol in all contexts. Furthermore, Kiene et al. found drinking before sex was associated with a higher likelihood of unprotected sex when participants reported having sex with a casual rather than a steady sexual partner. Thus, the association between contextual alcohol use and risky sexual behavior may be moderated by sexual partner type.
The primary purpose of this study was to use cross-sectional data to examine the association between alcohol use and sexual risk behaviors among South Africans. Specifically, we examined individual (HED) and contextual (self or partner drinking before sex) factors that may influence the association between alcohol use and sexual risk behavior among current drinkers. We expected that both individual and contextual alcohol use would be associated with multiple sexual partners, failure to discuss condom use with sexual partners, and fewer condom-protected events. A secondary purpose was to explore the alcohol-risky sexual behavior association by partner type (steady partners only, casual partners only, or both steady and casual partners). We expected individual alcohol use would predict risky sexual behavior with steady partners, whereas the context of alcohol use would be associated with risky sexual behavior with casual partners given that alcohol use prior to sex is more common with casual rather than steady sexual partners (Myer, et al., 2002). Examining the association between alcohol use and sexual risk behavior can guide intervention development to avert new infections among South Africans who consume alcohol.
2. METHODS
2.1 Participants and Procedures
We restricted our analyses to the 1,285 (out of 1,694) participants who reported using alcohol in the past month (Table 1). Participants (98% Black African; M age = 32, SD = 8.54, range = 19–57 years; 27% women) were residents of a large primarily Xhosa-speaking (predominantly Black African) township in Cape Town, South Africa, who reported consuming alcohol at least once in the past month (76% of the sample). The township, with discrete and geographically demarcated neighborhoods, was located approximately 20 km from Cape Town’s central business district. The township comprise indigenous Africans of Xhosa cultural heritage. We used the PLACE (Priorities for Local AIDS Control Efforts) method, described by Weir et al. (2002; 2003), to identify neighborhoods where the risk for HIV is greatest. Field workers used street intercept methods to sample from eight non-contiguous neighborhoods within the township. Our previous research found that within a township, residents had similar alcohol consumption and sexual risk behavior patterns (Kalichman et al., 2006). Demographic and socioeconomic rates in the neighborhoods are representative of South African townships (98% Black Africans, 55% obtained at least a high school education, 53% were employed, 19% were married, and 78% had at least one child). Two neighborhoods were surveyed from June 3 to June 29, 2008, two were surveyed from November 2 to December 7, 2008, two were surveyed from May 9 to June 29, 2009, and two were surveyed between October 25 and December 20, 2009. Field workers consisted of 12 ethnically-matched residents of the communities who spoke both Xhosa and English.
Table 1.
Characteristics of the sample overall and by heavy episodic drinking status
| Variables | Overall (N =1285) | No Heavy Drinking (n = 516) | Heavy Drinking (n =769) | Test for Differences |
|---|---|---|---|---|
| Demographics | ||||
| Age | 31.62 (8.54) | 31.17 (8.05) | 31.93 (8.84) | t (1280) = −1.57, p =.12 |
| Gender (% women) | 27% | 27% | 26% | χ2 (1) = 0.12, p = .73 |
| Ethnicity (% Black African) | 98% | 98% | 98% | χ2 (1) = 0.03, p = .86 |
|
| ||||
| Type of Sexual Partner | ||||
| Steady, % | 46% | 49% | 44% | χ2 (2) = 3.90, p = .14 |
| Casual, % | 6% | 5% | 7% | |
| Both steady and casual partners, % | 37% | 35% | 39% | |
|
| ||||
| Sexual Risk Factors | ||||
| Participant drank alcohol before sex | 6.37 (9.06) | 5.21 (9.60) | 7.14 (8.61) | t (1245) = −7.13, p <.001 |
| Partner drank alcohol before sex | 3.84 (7.21) | 4.31 (6.16) | 3.13 (8.50) | t (1253) = −5.39, p <.001 |
| Sexual Risk Behaviors | ||||
| Sexual partners (% 2 partners) | 44% | 42% | 45% | χ2 (1) = 1.08, p = .30 |
| Condom use (mean %) | 0.49 (0.38) | 0.53 (0.39) | 0.46 (0.37) | t (1093) = 2.97, p <.01 |
| Frequency of condom use, steady partners | 3.08 (1.96) | 3.34 (2.06) | 2.89 (1.86) | t (1071) = 3.70, p <.001 |
| Participants with both partner types | 2.83 (1.86) | 2.99 (1.94) | 2.74 (1.81) | t (476) = 1.44, p =.15 |
| Frequency of condom use, casual partners | 4.62 (1.75) | 4.81 (1.63) | 4.51 (1.81) | t (555) = 1.98, p =.05 |
| Participants with both partner types | 4.62 (1.75) | 4.44 (1.84) | 4.91 (1.57) | t (475) = 2.85, p <.01 |
| Discussed condom use with sexual partner | 53% | 57% | 50% | χ2 (1) = 6.84, p = .01 |
Note. Unadjusted means (SD) are provided except where noted. Heavy episodic drinking was defined as 5 or more drinks on a single occasion during the past week. Proportions of participants reporting steady, casual, or both steady and casual sexual partners do not sum to 100 because some participants (n = 131) did not report having a steady or a casual sexual partner. Responses to the measures of frequency of condom use with steady and/or casual partners ranged from 1 (never) to 6 (all the time) and included any participant reporting sex with a steady sexual partner (frequency of condom use, steady partners) or any participant reporting sex with a casual sexual partner (frequency of condom use, casual partners) in the past 30 days (i.e., participants could be included in both analyses if they reported having sex with a steady and a casual partner).
Surveys were administered in the participants’ preferred language. Field workers approached pedestrians or shebeen patrons and requested their participation in a survey, described as “research regarding HIV/AIDS that may benefit your community.” If individuals were interested (5% refusal rate), they provided verbal consent and then completed a nine-page anonymous survey in exchange for a small non-monetary gift (a keychain). Surveys were typically self-administered; however, if a prospective participant did not possess adequate literacy skills, the surveys were administered by the field worker as an interview. All procedures were approved by the Institutional Review Boards of the Human Sciences Research Council, University of Connecticut, and Syracuse University.
2.2 Measures
The survey assessed (a) demographic information (e.g., age, gender, ethnicity), (b) alcohol use, (c) communication patterns with sexual partners, (d) sexual behavior, and (d) additional measures (e.g., attitudes, community norms about sexual and alcohol behaviors) as part of a larger community-level trial.
2.2.1 Alcohol Use
Participants were given culturally adapted definitions of standard drinks (e.g., a single tot or shot of spirits = 1 standard drink) and were asked several questions about their alcohol use. Current alcohol consumption was assessed by asking participants the number of days they drank alcohol in the past 30 days (never to nearly every day). Responses were used to determine the number of participants to be included in the analyses (i.e., any participant who had consumed alcohol at least once in the past month). Frequency of HED was assessed by asking participants “how many times during the past 30 days did you have 5 or more drinks on an occasion” (1 = nearly every day, 2 = 3–4 times per week, 3 = 2 times per week, 4 = once a week, 5 = 2–3 times in past 30 days, 6 = once in past 30 days, 7 = never). Responses to this question were used to categorize people into groups based on whether they had or had not engaged in HED at least once per week in the last 30 days.
2.2.2 Alcohol Use Before Sex
Participants and their partners’ alcohol consumption before sex was assessed by asking participants the number of times they had “drank alcohol (beer, wine) before sex” and the number of times they “had a sex partner who drank alcohol (beer, wine) before sex” during the past 30 days. Responses yielded two count variables representing the frequency of alcohol consumption before sex for self and for partner(s).
2.2.3 Sexual Risk Behaviors
Participants were asked a series of questions regarding their sexual risk behavior (number of sexual partners, discussing condom use with sexual partners, and condom use) during the past 30 days. Number of sexual partners was assessed by asking participants the number of men [women] they had sex with in the past 30 days (total number of partners). The number of sexual partners was recoded as two or more sexual partners (1) and one or fewer (0) in the past 30 days. Communication about condom use with a sexual partner was assessed by asking participants “in the past 30 days, how many times have you talked with a sex partner about using condoms” (total number of events). We recoded these responses to reflect any condom use discussion (1) vs. no condom use discussion (0) with sexual partner(s) in the past 30 days. Condom use (in past 30 days) was assessed by asking participants how often they had (a) vaginal sex with a condom, (b) vaginal sex without a condom, (c) anal sex with a condom, and (d) anal sex without a condom. Responses were used to determine the proportion of protected sexual events in past 30 days (number of times vaginal and anal sex occurred with a condom divided by the total number of vaginal and anal sexual events).
To assess risk behavior by partner type, participants were asked whether they had a “primary/main sex partner (someone you have a relationship with)” and/or a “casual (non-regular) sex partner” (yes, no). Frequency of condom use with either a primary or casual partner was assessed using two separate items: “If YES, how often do you use a condom with this partner?” Responses were never (1), rarely (2), some of the time (3), half of the time (4), most of the time (5), and all of the time (6).
2.3 Data Management and Analysis
Summary statistics (means and standard deviations, frequencies) were used to describe demographic and risk characteristics for the overall sample and by HED status. Because the count variables (number of times self or partner used alcohol before sex) were skewed and clustered at zero, we transformed these variables with a logarithmic function by adding a constant (1) and taking the natural log (Tabachnick & Fidell, 2007). Differences between heavy episodic and non-heavy episodic drinkers were examined using a series of independent t-tests or one-way ANOVAs (for continuous measures) and chi-square analyses (for dichotomous measures).
A series of regression models (linear and logistic) were used to test the association between alcohol use and risk behaviors. Specifically, three separate models were used to examine the overall effects of alcohol use on each risk behavior (multiple sexual partners, discussed condom use with sexual partner(s), and proportion of protected sex). In each model, we controlled for demographic variables (age, gender, and ethnicity). (Because bivariate analyses indicated demographic differences in risk behavior, we include age, gender, and ethnicity in our analyses.) Alcohol use was examined using three variables: drinking before sex (self), drinking before sex (partner), and HED status (1 = HED at least once per week in the past 30 days, 0 = no HED in the past week). All data analyses were conducted using Stata 11.0 (StataCorp, 2009).
3. RESULTS
3.1 Characteristics of the Sample
Overall, 44% of participants reported having two or more sexual partners in the past 30 days (Table 1). About half (46%) of participants had sex only with a steady partner, 6% had sex only with causal partners, and 37% reported having sex with both steady and casual partners; 10% (131/1285) of the sample did not have a sexual partner in the past 30 days (data not tabled). Most participants reported having sex with a partner of the opposite sex (87%), 2% (19 men, 8 women) reported sex with a same sex partner, 2% (18 men, 4 women) reported having sex with both men and women. Approximately half of the participants (53%) reported discussing condom use with a sexual partner at least once in the past 30 days. Condoms were used for 49% of vaginal or anal sex events. Frequency of condom use differed by partner type: condoms were used “most of the time” (M = 4.62) with casual partners and “some of the time” (M = 3.08) with a steady partner.
3.2 Heavy Episodic Drinking
Table 1 reports the overall characteristics of the sample and by HED status. Of the 1,285 participants, 769 (60%) reported HED; rates of HED were similar for men (567/943) and women (202/342). Compared to participants who had not engaged in HED, heavy episodic drinkers reported more sexual occasions preceded by alcohol use (M = 7.14 vs. 5.21), fewer sexual occasions preceded by partners’ alcohol use (M = 3.13 vs. 4.31), more condom-protected vaginal or anal sex events (M = 53% vs. 46%), and less frequent condom use with steady (M = 2.89 vs. 3.34) or casual (M = 4.51 vs. 4.81) sexual partners, all ps <.05. Heavy episodic drinkers (50%) were less likely to report discussing condom use with sexual partner(s) at least once in the past 30 days compared to non-heavy episodic drinkers (57%), p <.01. No other differences in demographic or risk variables between those who had or had not engaged in HED were found (see Table 1).
3.3 Sexual Risk Behaviors
3.3.1 Multiple sexual partners
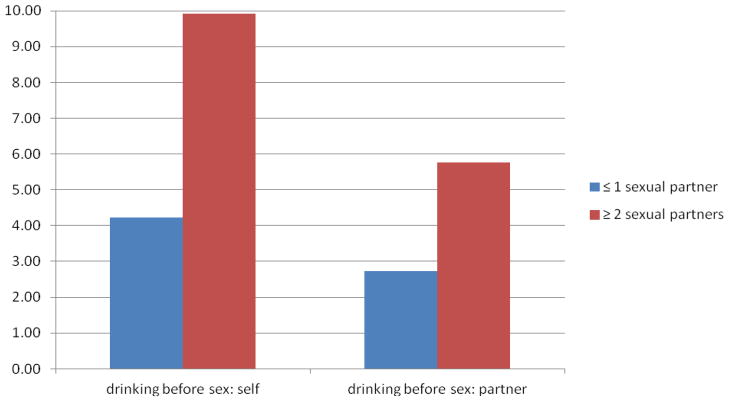
Logistic regression analyses were used to predict the probability of multiple sexual partners from alcohol use (individual and contextual) controlling for demographic variables (age, gender, and ethnicity). Drinking before sex (adjusted OR = 1.99, 95% CI = 1.39, 1.91) and partner drinking before sex (adjusted OR = 1.62, 95% CI = 1.39, 1.91) were associated with multiple sexual partners. Results from subsequent analyses examining differences between participants who did or did not report multiple sexual partners indicated that participants who had 2 or more sexual partners were more likely to drink before sex, t (1128) = 11.26, p <.001, and have a partner who drank before sex, t (1136) = 7.12, p <.001, compared to those who did not report multiple sexual partners (see Figure 1). Heavy episodic drinkers were less likely to report multiple sexual partners than non-heavy episodic drinkers in the analyses (adjusted OR = 0.74, 95% CI = 0.56, 0.98).
Figure 1.
Mean number of times participants or their partner drank alcohol before sex in the past 30 days among those who had or did not have multiple sexual partners.
3.3.2 Discussed condom use with sexual partner(s)
Logistic regression analyses were used to predict the probability of discussing condom use with sexual partner(s) from alcohol use (individual and contextual). Drinking before sex, partner drinking before sex, and HED were all associated with discussing condom use with partners. Participants were more likely to discuss condom use with their partners if they had been drinking before sex (adjusted OR = 1.24, 95% CI = 1.08, 1.42) or had a partner who drank before sex (adjusted OR = 1.30, 95% CI = 1.12, 1.50). HED (adjusted OR = 0.63, 95% CI = 0.49, 0.81) was negatively associated with communication; participants who engaged in HED at least once in the past 30 days were less likely to communicate with partners about condom use. (Data not tabled.)
3.3.3 Condom Use
Linear regression analysis was used to examine the association between alcohol use (individual and contextual) and proportion of condom-protected sexual events. Drinking before sex was a significant predictor of condom use (β = −.12, p <.01); participants who drank before sex were less likely to use a condom. Partner drinking before sex (β = .03, p =.42) and HED status (β = −.05, p =.11) did not predict condom use. (Data not tabled.)
3.4 Sexual Risk Behaviors by Partner Type
Because sexual preventive behavior may differ by partner type, exploratory analyses examined the association between alcohol use (individual and contextual) and the frequency of condom use among participants with steady, casual, or both steady and casual partners. In two separate models (stratified by partner type), the frequency of condom use with steady or casual partners was predicted from alcohol use using regression analyses (Table 2). Exploratory analyses included participants who reported having a steady sexual partner (n = 1,073), a casual partner (n = 559), and both steady and casual partners (n = 478). Preliminary analyses comparing participants with steady, casual, or both steady and casual partners on demographic and sexual risk/preventive behaviors revealed significant differences with respect to age, gender, drinking before sex, and partner drinking before sex (Supplemental Table).
Table 2.
Regression analyses examining the effects of alcohol use on past month condom use by partner type
| Participants reporting steady or casual partner only | Participants reporting both steady and casual partners | |||||
|---|---|---|---|---|---|---|
| B (SE) | β | p | B (SE) | β | p | |
| Frequency of Condom Use, Steady Partner | ||||||
| Age | −0.05 (0.01) | −.23 | .00 | −0.04 (0.01) | −.16 | .00 |
| Men | −0.15 (0.20) | −.04 | .45 | 0.05 (0.25) | .01 | .82 |
| Black African | 1.18 (0.59) | .08 | .05 | 1.14 (0.76) | .07 | .13 |
| Participant drank alcohol before sex | −0.28 (0.10) | −.14 | .00 | −0.19 (0.11) | −.10 | .09 |
| Partner drank alcohol before sex | −0.05 (0.10) | −.02 | .64 | 0.10 (0.10) | .06 | .32 |
| Heavy episodic drinking | −0.36 (0.17) | −.09 | .03 | −0.30 (0.18) | −.08 | .10 |
| Frequency of Condom Use, Casual Partner(s) | ||||||
| Age | −0.05 (0.03) | −.23 | .05 | −0.03 (0.01) | −.12 | .01 |
| Men | −0.71 (0.47) | −.17 | .13 | −0.12 (0.23) | −.02 | .62 |
| Black African | 0.32 (1.01) | .04 | .75 | −0.28 (0.72) | −.02 | .70 |
| Participant drank alcohol before sex | −0.46 (0.23) | −.26 | .05 | −0.22 (0.10) | −.12 | .04 |
| Partner drank alcohol before sex | 0.35 (0.22) | .20 | .12 | −0.19 (0.09) | −.12 | .05 |
| Heavy episodic drinking | 1.04 (0.43) | .28 | .02 | −0.34 (0.17) | −.09 | .05 |
Note. Age of participant, drank alcohol before sex, and partner drank alcohol before sex are continuous variables and were centered; all other variables were dummy-coded (men: 1 = men, 0 = women; Black African: 1 =Black African, 0 = other). Heavy episodic drinking was defined as 5 or more drinks on a single occasion during the past week. Analyses included participants who reported having sex with only a steady partner or only a casual partner(s) (steady OR casual partner only) or those who reported having sex with both steady and casual partners (both steady and casual partners).
Participants with steady sexual partners reported a lower frequency of condom use when they drank before sex and when they were heavy drinkers. Among participants with both steady and casual sex partners, drinking before sex (self or partner) or HED was not associated with the frequency of condom use with steady partners. With a casual partner(s), drinking before sex was associated with a lower frequency of condom use whereas HED was associated with a greater frequency of condom use with casual partners. Among participants reporting both steady and casual sexual partners, drinking before sex, partner’s drinking before sex, and HED status were associated with the frequency of condom use with casual partners. Participants reported less frequent condom use with casual partners if they had consumed alcohol before sex, their partner had consumed alcohol before sex, and if they engaged in HED.
4. DISCUSSION
In this study, we examined the association between alcohol use (individual and contextual) and sexual risk behavior in South Africa – the country with the highest per capita rates of HIV infection and alcohol consumption in the world. Overall, results indicated that alcohol use was a significant predictor of sexual risk behaviors but the associations were complex, and varied by individual and contextual alcohol use factors. Consistent with prior research among South African STD clinic patients (Kalichman, Simbayi, Jooste, & Cain, 2007; Simbayi, et al., 2004), shebeen patrons (Morojele, et al., 2006), and HIV-positive patients (Kiene, et al., 2008), drinking before sex was associated with risky sexual behaviors (i.e., multiple sexual partners and fewer condom-protected events). Contrary to our expectations, regression analyses showed that heavy episodic drinkers were less likely to have multiple sexual partners.
Analyses stratified by partner type revealed even more complex patterns. These analyses showed that participants were less likely to use a condom with a steady partner if the respondent had been drinking before sex or if the respondent engaged in HED. Infrequent condom use with steady sexual partners was expected, given the familiarity with (and presumed knowledge about) the partner, the threat to trust created by introducing condom use, and the simple habit of non-condom use. Nonetheless, alcohol use does introduce risk in steady relationships for two reasons. The first is that partner exclusivity cannot be assumed; indeed, the literature documents that “monogamy” is no protection against HIV unless both partners are mutually adherent (Newmann et al., 2000). Second, research indicates that alcohol use is associated with sexual coercive behavior and intimate partner violence (Silverman, Decker, Saggurti, Balaiah, & Raj, 2008). That is, research has shown that when men consume alcohol, their steady sexual partners feel pressure to engage in high-risk sexual activity (Woolf-King & Maisto, 2011), often due to a fear of violent consequences (Mittal, Senn, & Carey, 2011). Our finding that alcohol use contributes to the infrequent use of condoms with steady sexual partners warrants further investigation.
As expected, and consistent with prior research (Brown & Vanable, 2007; Kiene, Barta, Tennen, & Armeli, 2009; Scott-Sheldon et al., 2009), the frequency of condom use with casual partners was lower if the participant drank before sex. Explanations for this association typically invoke the alcohol myopia model (Steele & Josephs, 1990), such that when intoxicated, people are less able to attend to or process multiple situational cues and focus solely on the most salient cues. This research suggests the need to provide interventions that (a) reduce alcohol use prior to sexual encounters and (b) promote better condom use when drinking. The value of this approach is supported by results from Kalichman et al. (2008), who implemented a skills-based alcohol-related HIV risk-reduction intervention in South Africa. In this study, intervention participants reduced their sexual risk behavior relative to the control groups; however, these reductions were found only for light drinkers (vs. heavy drinkers) indicating the need for more refinement for heavy drinking patrons.
Heavy episodic drinkers seem to be a unique sub-set of alcohol users who may require special attention. In the current study, contrary to expectation, condom use was greater if participants were heavy episodic drinkers. There are several possible explanations for this unexpected finding. For example, it is possible that heavy drinking patrons simply had more opportunities to use condoms because they had more sexual encounters. Exploratory analyses provided little support for this explanation. An alternative explanation is that heavy drinking patrons were more likely to have sex with partners whom they did not know well, whereas non-heavy drinking counterparts had partners with whom they were better acquainted, and therefore with partners who were perceived to be less risky. Our data do not allow us to test this explanation. A third explanation involves the context of different drinking patterns; that is, heavy episodic alcohol use may be associated with more condom use because it occurs in the vicinity of public drinking places (e.g., bars or shebeens) where condom use may be more normative. Each of these hypotheses warrants investigation, perhaps using qualitative research to examine the quantitative results that emerged from our data.
Several limitations of our methods should be kept in mind when interpreting the findings. First, data were gathered from self-reports, which are imperfect indicators of behavior. To minimize socially desirable responding (Weinhardt, Forsyth, Carey, Jaworski, & Durant, 1998), field staff emphasized that all data were anonymous. Second, the respondents sampled may not be representative of the larger community; however, we used street intercept surveys, a methodology that provides access to the widest range of community members and minimizes the self-selection bias often seen with clinical or other recruitment strategies (Miller, Wilder, Stillman, & Becker, 1997). Third, our data are cross-sectional and do not support causal inferences. Event-level data can provide stronger evidence regarding the association between alcohol use and risky sexual behavior (Weinhardt & Carey, 2000).
5. CONCLUSION
This research carries implications for sexual risk and alcohol use reduction; in particular, these findings suggest that risk reduction strategies in South Africa should address the important role of alcohol use in the context of sex. Interventionists might seek to increase awareness of the effects of alcohol use on risk perception, decision-making, and interpersonal and self-management skills (cf. (Kalichman, Simbayi, Vermaak, Cain, et al., 2008). Implementing sexual risk reduction interventions at drinking venues may reach those at greatest need but will be cleverly implemented; that is, they are more likely to be welcomed by shebeen owners if they do not jeopardize alcohol sales. Interventions might focus on both individual as well as community level sexual risk reduction. The latter may be achieved, for example, by making condoms available and by modifying norms associated with risky sexual behavior (especially in the vicinity of drinking venues). Implementing intervention strategies in frequently attended drinking venues that service people engaging in unsafe sexual behaviors can help to reduce the impact of the HIV epidemic in South Africa.
Supplementary Material
HIGHLIGHTS.
Alcohol use is associated with sexual risk behaviors among South Africans.
The alcohol-risky behavior association varies by individual and contextual factors.
Findings suggests the need to include alcohol content in HIV prevention programs.
Acknowledgments
This project was supported by the National Institute on Alcohol Abuse and Alcoholism (R01 AA017399 to Seth C. Kalichman). This project was partially supported by the National Institute of Mental Health (K01MH087219 to Ofer Harel). We thank the participants, staff, and our research team.
Footnotes
Conflict of Interest. All authors declare that they have no conflicts of interest.
Contributors. Authors contributed to the manuscript in the following manner:
Study concept and design: Scott-Sheldon, MP Carey, KB Carey
Acquisition of data: Cain, Mehlomakulu, Mwaba
Analysis and interpretation of data: Scott-Sheldon, MP Carey, KB Carey, Cain, Harel, Mehlomakulu, Mwaba, Simbayi, and Kalichman
Drafting of the manuscript: Scott-Sheldon, MP Carey, KB Carey
Critical revision of the manuscript: Scott-Sheldon, MP Carey, KB Carey, Cain, Harel, Mehlomakulu, Mwaba, Simbayi, and Kalichman
Statistical analysis: Scott-Sheldon
Obtaining funding: Kalichman, MP Carey, KBCarey
Administrative, technical, or material support: Cain
Study supervision: Kalichman
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Lori A. J. Scott-Sheldon, Centers for Behavioral and Preventive Medicine, The Miriam Hospital, and Department of Psychiatry and Human Behavior, Alpert Medical School, Brown University, Providence, RI.
Michael P. Carey, Centers for Behavioral and Preventive Medicine, The Miriam Hospital, and Department of Psychiatry and Human Behavior, Alpert Medical School, Brown University, Providence, RI.
Kate B. Carey, Center for Alcohol and Addiction Studies, Brown University, Providence, RI.
Demetria Cain, Center for Health, Intervention, and Prevention, University of Connecticut, USA.
Ofer Harel, Center for Health, Intervention, and Prevention, University of Connecticut, USA.
Vuyelwa Mehlomakulu, HIV/AIDS, STIs and TB, Human Sciences Research Council, Cape Town, South Africa.
Kelvin Mwaba, HIV/AIDS, STIs and TB, Human Sciences Research Council, Cape Town, South Africa.
Leickness C. Simbayi, HIV/AIDS, STIs and TB, Human Sciences Research Council, Cape Town, South Africa.
Seth C. Kalichman, Center for Health, Intervention, and Prevention, University of Connecticut, USA.
References
- Baliunas D, Rehm J, Irving H, Shuper P. Alcohol consumption and risk of incident human immunodeficiency virus infection: a meta-analysis. Int J Public Health. 2010;55(3):159–166. doi: 10.1007/s00038-009-0095-x. [DOI] [PubMed] [Google Scholar]
- Brown JL, Vanable PA. Alcohol use, partner type, and risky sexual behavior among college students: Findings from an event-level study. Addict Behav. 2007;32(12):2940–2952. doi: 10.1016/j.addbeh.2007.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher JC, Bang H, Kapiga SH. The association between HIV infection and alcohol use: a systematic review and meta-analysis of African studies. Sexually Transmitted Diseases. 2007;34(11):856–863. doi: 10.1097/OLQ.0b013e318067b4fd. [DOI] [PubMed] [Google Scholar]
- Fritz K, Morojele N, Kalichman S. Alcohol: the forgotten drug in HIV/AIDS. Lancet. 2010;376(9739):398–400. doi: 10.1016/S0140-6736(10)60884-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalichman SC, Simbayi LC, Jooste S, Cain D. Frequency, quantity, and contextual use of alcohol among sexually transmitted infection clinic patients in Cape Town, South Africa. American Journal of Drug and Alcohol Abuse. 2007;33(5):687–698. doi: 10.1080/00952990701522716. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Simbayi LC, Kagee A, Toefy Y, Cain D, Cherry C. Association of poverty, substance use, and HIV transmission risk behaviors in three South African communities. Social Science and Medicine. 2006;62:1641–1649. doi: 10.1016/j.socscimed.2005.08.021. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Simbayi LC, Kaufman M, Cain D, Jooste S. Alcohol use and sexual risks for HIV/AIDS in sub-Saharan Africa: systematic review of empirical findings. Prev Sci. 2007;8(2):141–151. doi: 10.1007/s11121-006-0061-2. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Simbayi LC, Vermaak R, Cain D, Smith G, Mthebu J, Jooste S. Randomized trial of a community-based alcohol-related HIV risk-reduction intervention for men and women in Cape Town South Africa. Annals of Behavioral Medicine. 2008;36(3):270–279. doi: 10.1007/s12160-008-9067-2. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Simbayi LC, Vermaak R, Jooste S, Cain D. HIV/AIDS risks among men and women who drink at informal alcohol serving establishments (Shebeens) in Cape Town, South Africa. Prevention Science. 2008;9(1):55–62. doi: 10.1007/s11121-008-0085-x. [DOI] [PubMed] [Google Scholar]
- Kiene SM, Barta WD, Tennen H, Armeli S. Alcohol, helping young adults to have unprotected sex with casual partners: findings from a daily diary study of alcohol use and sexual behavior. J Adolesc Health. 2009;44(1):73–80. doi: 10.1016/j.jadohealth.2008.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiene SM, Simbayi LC, Abrams A, Cloete A, Tennen H, Fisher JD. High rates of unprotected sex occurring among HIV-positive individuals in a daily diary study in South Africa: the role of alcohol use. J Acquir Immune Defic Syndr. 2008;49(2):219–226. doi: 10.1097/QAI.0b013e318184559f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller KW, Wilder LB, Stillman FA, Becker DM. The feasibility of a street-intercept survey method in an African-American community. Am J Public Health. 1997;87:655–658. doi: 10.2105/ajph.87.4.655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mittal M, Senn TE, Carey MP. Fear of Violent Consequences and Condom Use among Women Attending a STD Clinic. 2011. Manuscript submitted for publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morojele NK, Kachieng’a MA, Mokoko E, Nkoko MA, Parry CD, Nkowane AM, Saxena S. Alcohol use and sexual behaviour among risky drinkers and bar and shebeen patrons in Gauteng province, South Africa. Soc Sci Med. 2006;62(1):217–227. doi: 10.1016/j.socscimed.2005.05.031. [DOI] [PubMed] [Google Scholar]
- Myer L, Matthews C, Little F. Condom Use and Sexual Behaviors Among Individuals Procuring Free Male Condoms in South Africa: A Prospective Study. Sexually Transmitted Diseases. 2002;29(4):239–241. doi: 10.1097/00007435-200204000-00009. [DOI] [PubMed] [Google Scholar]
- Newmann S, Sarin P, Kumarasamy N, Amalraj E, Rogers M, Madhivanan P, Solomon S. Marriage, monogamy and HIV: a profile of HIV-infected women in south India. Int J STD AIDS. 2000;11(4):250–253. doi: 10.1258/0956462001915796. [DOI] [PubMed] [Google Scholar]
- Parry CD, Pluddemann A, Steyn K, Bradshaw D, Norman R, Laubscher R. Alcohol use in South Africa: findings from the first Demographic and Health Survey (1998) Journal of Studies on Alcohol. 2005;66(1):91–97. doi: 10.15288/jsa.2005.66.91. [DOI] [PubMed] [Google Scholar]
- Peltzer K, Ramlagan S. Alcohol use trends in South Africa. Journal of Social Sciences. 2009;18:1–12. [Google Scholar]
- Rehm J, Rehn N, Room R, Monteiro M, Gmel G, Jernigan D, Frick U. The global distribution of average volume of alcohol consumption and patterns of drinking. European Addiction Research. 2003;9(4):147–156. doi: 10.1159/000072221. [DOI] [PubMed] [Google Scholar]
- Scott-Sheldon LA, Carey MP, Vanable PA, Senn TE, Coury-Doniger P, Urban MA. Alcohol consumption, drug use, and condom use among STD clinic patients. J Stud Alcohol Drugs. 2009;70(5):762–770. doi: 10.15288/jsad.2009.70.762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverman JG, Decker MR, Saggurti N, Balaiah D, Raj A. Intimate partner violence and HIV infection among married Indian women. JAMA. 2008;300(6):703–710. doi: 10.1001/jama.300.6.703. [DOI] [PubMed] [Google Scholar]
- Simbayi LC, Kalichman SC, Jooste S, Mathiti V, Cain D, Cherry C. Alcohol use and sexual risks for HIV infection among men and women receiving sexually transmitted infection clinic services in Cape Town, South Africa. J Stud Alcohol. 2004;65(4):434–442. doi: 10.15288/jsa.2004.65.434. [DOI] [PubMed] [Google Scholar]
- South African Medical Research Council. South Africa Demographic and Health Survey 2003. Pretoria, South Africa: Department of Health; 2007. [Google Scholar]
- StataCorp. Stata Statistical Software: Release 11. College Station, TX: StataCorp LP; 2009. [Google Scholar]
- Steele CM, Josephs RA. Alcohol myopia. It’s prized and dangerous effects. American Psychologist. 1990;45:921–933. doi: 10.1037//0003-066x.45.8.921. [DOI] [PubMed] [Google Scholar]
- Tabachnick BG, Fidell LS. Using multivariate statistics. 5. Boston, MA: Allyn and Bacon; 2007. [Google Scholar]
- UNAIDS. Global Report: UNAIDS Report on the Global AIDS Epidemic. 2010 Retrieved September 19, 2011, from http://www.unaids.org/globalreport/Global_report.htm.
- Weinhardt LS, Carey MP. Does alcohol lead to sexual risk behavior? Findings from event-level research. Annual Review of Sex Research. 2000;11:125–157. [PMC free article] [PubMed] [Google Scholar]
- Weinhardt LS, Forsyth AD, Carey MP, Jaworski BC, Durant LE. Reliability and validity of self-report measures of HIV-related sexual behavior: Progress since 1990 and recommendations for research and practice. Arch Sex Behav. 1998;27(2):155–180. doi: 10.1023/a:1018682530519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weir SS, Morroni C, Coetzee N, Spencer J, Boerma JT. A pilot study of a rapid assessment method to identify places for AIDS prevention in Cape Town, South Africa. Sex Transm Infect. 2002;78(Suppl 1):i106–113. doi: 10.1136/sti.78.suppl_1.i106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weir SS, Pailman C, Mahlalela X, Coetzee N, Meidany F, Boerma JT. From people to places: focusing AIDS prevention efforts where it matters most. AIDS. 2003;17(6):895–903. doi: 10.1097/01.aids.0000050809.06065.e0. [DOI] [PubMed] [Google Scholar]
- Woolf-King SE, Maisto SA. Alcohol use and high-risk sexual behavior in Sub-Saharan Africa: a narrative review. Archives of Sexual Behavior. 2011;40(1):17–42. doi: 10.1007/s10508-009-9516-4. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Global status report on alcohol and health. 2011 Retrieved November 21, 2011, from http://www.who.int/substance_abuse/publications/global_alcohol_report/msbgsruprofiles.pdf.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.