Abstract
Study Design
Analysis of the National Inpatient Sample database from 2000 to 2008.
Objective
To identify if metabolic syndrome is an independent risk factor for increased major perioperative complications, cost, length of stay and non-routine discharge.
Summary of Background Data
Metabolic syndrome is a combination of medical disorders that has been shown to increase the health risk of the general population. No study has analyzed its impact in the perioperative spine surgery setting.
Methods
We obtained the National Inpatient Sample from the Hospital Cost and Utilization Project for each year between 2000 and 2008. All patients undergoing primary posterior lumbar spine fusion were identified and separated into groups with and without metabolic syndrome. Patient demographics and health care system related parameters were compared. The outcomes of major complications, non-routine discharge, length of hospital stay and hospitalization charges were assessed for both groups. Regression analysis was performed to identify if the presence of metabolic syndrome was an independent risk factor for each outcome.
Results
An estimated 1,152,747 primary posterior lumbar spine fusion were performed between 2000 and 2008 in the US. The prevalence of metabolic syndrome as well as the comorbidities of the patients increased significantly over time. Patients with metabolic syndrome had significantly longer length of stay, higher hospital charges, higher rates of non-routine discharges and increased rates of major life-threatening complications compared to patients without metabolic syndrome.
Conclusion
Patients with metabolic syndrome undergoing primary posterior lumbar spinal fusion represent an increasing financial burden on the health care system. Clinicians should recognize that metabolic syndrome represents a risk factor for increased perioperative morbidity.
Keywords: metabolic syndrome, spinal fusion, lumbar spine, complications, risk factors, perioperative
Introduction
Metabolic syndrome (MetS) refers to a combination of medical disorders that increase the risk for cardiovascular morbidity and mortality.1,2 While exact definitions vary, the presence of obesity, hypertension, dyslipidemia and diabetes are components contributing to this disease complex.3–5 Risk factors for the development of this syndrome have been quoted to include old age, a sedentary lifestyle, and genetic predisposition.6
Studies have linked the presence of the MetS to increased health risks in the general population, however research evaluating its impact in the perioperative setting is sparse.7 In particular, there is a paucity of information on perioperative outcomes in patient with MetS undergoing primary posterior lumbar spine fusion (PSF), a procedure that is becoming increasingly popular.8
We therefore sought to elucidate the epidemiology and perioperative impact of MetS in patients undergoing PSF utilizing nationally representative data collected for the largest all payer inpatient database in the United States, the National Inpatient Sample (NIS).
We hypothesized that MetS would be a risk factor for perioperative complications as well as increased cost, length of stay and non-routine discharge.
Materials and Methods
Data Source
NIS data files were commercially obtained from the Hospital Cost and Utilization Project (HCUP) and analyzed for this study. The NIS represents the largest all payer inpatient discharge database in the United States and is sponsored by the Agency for Healthcare Research and Quality (AHRQ). Detailed information on the NIS design can be accessed electronically.9,10 Recognizing its utility to answer valuable clinical questions, a large number of studies addressing issues across the spectrum of medical specialties have been published using the NIS.
Selection of Study Sample and Statistical Methods
Our study sample consists of all data in the NIS for each year between 2000 and 2008. Entries indicating the performance of primary posterior lumbar spine fusion were identified using International Classification of Diseases- 9th revision-Clinical Modification (ICD-9-CM) (81.08). Those listing additional spinal procedures were excluded. Entries with metabolic syndrome (MetS) were defined as those with at least three out of the four following comorbidities: obesity, hypertension, diabetes mellitus and dyslipidemia. This definition was chosen to approximate the definition published by the US National Cholesterol Education Program Adult Treatment Panel III.5 Comorbidities were defined by ICD-9-CM diagnosis codes and the Clinical Classifications Software for Services and Procedures (CCSSP) provided by the AHRQ11 (i.e obesity, hypertension, diabetes mellitus) and appropriate ICD-9-codes (dyslipedemia: ICD-9-CM 272)
Patient characteristics were compared between entries with and without MetS (table 1). Patient demographics included age (continuous as well as categorized as 0–44, 45–64, 65–74, and >75 years), comorbidities (including diabetes, obesity, dyslipidemia, hypertension, chronic pulmonary disease, liver disease, congestive heart failure, neurologic, liver, renal and peripheral vascular disease), indication for the surgical intervention (degenerative disc disease, spondylolisthesis, spinal stenosis, scoliosis, traumatic and oncologic, and other), gender, race (White, Black, Hispanic, Other), and admission type (emergent, elective, urgent and others). Further characteristics studied were healthcare system related parameters including hospital size (small, medium, large), geographic location (rural, urban), and teaching status (teaching, non-teaching). In order to analyze trends in the prevalence of MetS as well as in individual comorbidities associated with this disease complex, bar charts and profile plots by three-year time periods (2000–2002, 2003–2005, 2006–2008) were generated. In addition, we evaluated the incidence of MetS by disposition status after PSF.
Table 1.
Demographics of patients with and without metabolic syndrome (MetS) undergoing primary posterior lumbar spine fusion from 2000 to 2008.
| Demographics | |||
|---|---|---|---|
| Group | No MetS | MetS | P-value |
| N= | 225347 | 12949 | |
| Weighted N= | 1089802 | 62945 | |
| (%) | 94.5 | 5.5 | |
| Average age (years) | 54.10 (54.04,54.17) | 62.82 (62.63,63.01) | <.0001 |
| Average Comorbidity Index | 0.37 (0.37,0.38) | 1.88 (1.86,1.90) | <.0001 |
| Age group (%) | |||
| 0–44 | 28.2 | 5.7 | <.0001 |
| 45–64 | 43.7 | 47.3 | |
| 65–74 | 17.7 | 32.4 | |
| >75 | 10.3 | 14.6 | |
| Gender(%) | |||
| Male | 44.3 | 41.1 | <.0001 |
| Female | 55.7 | 58.9 | |
| Race(%) | |||
| White | 88.7 | 85.1 | <.0001 |
| Black | 4.4 | 7.7 | |
| Hispanic | 4.2 | 4.3 | |
| Other | 2.6 | 2.9 | |
| Admission Type (%) | |||
| Emergent | 3.3 | 2.6 | <.0001 |
| Elective | 90.4 | 91.8 | |
| Urgent+Other | 6.3 | 5.6 | |
| Hospital Size (%) | |||
| Small | 12.5 | 12.2 | 0.4 |
| Medium | 21.7 | 22.2 | |
| Large | 65.7 | 65.6 | |
| Hospital Location (%) | |||
| Rural | 4.6 | 4.6 | 0.9 |
| Urban | 95.4 | 95.4 | |
| Hospital Teaching Status (%) | |||
| Non-teaching | 46.7 | 46.7 | 1.0 |
| Teaching | 53.3 | 53.3 | |
| Spine Pathology(%) | |||
| Degenerative Disc Disease | 45.9 | 37.7 | <0.0001 |
| Spinal stenosis | 10.0 | 15.0 | |
| Scoliosis | 1.4 | 0.3 | |
| Spondylolisthesis | 5.4 | 5.4 | |
| Trauma | 1.6 | 0.4 | |
| Oncologic | 0.3 | 0.1 | |
| Other | 4.7 | 3.3 | |
| Multiple Indications | 30.7 | 37.7 |
Differences in the frequencies of major complications between MetS and non-MetS entries were analyzed by determining cases that listed Classification of ICD-9-CM diagnosis codes consistent with postoperative cerebral infarction, pulmonary compromise, sepsis, shock/cardiorespiratory arrest, acute myocardial infarction, cardiac complications (except myocardial infarction), pneumonia, and thrombosis/pulmonary embolism based on modified definitions provided in the Complication Screening Package designed for use with administrative data.12 Comorbidity profiles were analyzed by determining the prevalence of a number of disease states as defined in the Comorbidity Software provided by the Agency for Healthcare Research and Quality.11 Additionally, in order to account for overall comorbidity burden, Deyo comorbidity index categories were created.13, 14
Weighted means and percentages were shown for continuous and categorical variables, respectively. Approximately 40% of entries in the race category were not available and were imputed as “white”. This approach has been previously described and is based on the fact that facilities with high rates of missing data for race served populations with higher than average white/black patient ratios.15,16 Of note, in this analysis results did not change significantly when treating missing entries as a separate group.
Multivariate logistic regression analysis was performed to identify if MetS was a risk factor for perioperative major complications and/or mortality, prolonged hospital stay, increased hospital cost and non-routine disposition while controlling for patient age, gender, race, admission type, indication for surgical intervention, and comorbidities, as well as hospital location, size, and teaching status. Among variables considered in the regression model were hospital and patient characteristics as well a surgical indications. Individual comorbidities as well as MetS were also included, taking care not to enter MetS component comorbidities more than once into the regression. When the average length of stay and hospital cost were greater than the 75th percentile, they were defined as prolonged hospital stay and increased hospital cost, respectively. The disposition status was dichotomized to routine and non-routine disposition. Due to the very large sample size in this study, we did not rely on a conventional threshold of statistical significance (i.e., p-value<0.05) to draw conclusions from the study findings. Instead, we reported p-values and use 95% confidence intervals (CI) as a measure of effect size and let the readers evaluate the significance of the findings.
All statistical analyses were performed using SAS version 9.2 (SAS Institute, Cary, NC). To facilitate analysis of data and to obtain consistent estimates of mean and variance parameters taking into account the complex survey data setting, SAS procedures SURVEYMEANS, SURVEYFREQ, and SURVEYLOGISTIC were utilized for descriptive analyses and modeling efforts.
Results
In the time period studied, we identified 238,296 admissions for PSF in the NIS. This represents an estimated 1,152,747 procedures performed in the US between 2000 and 2008.
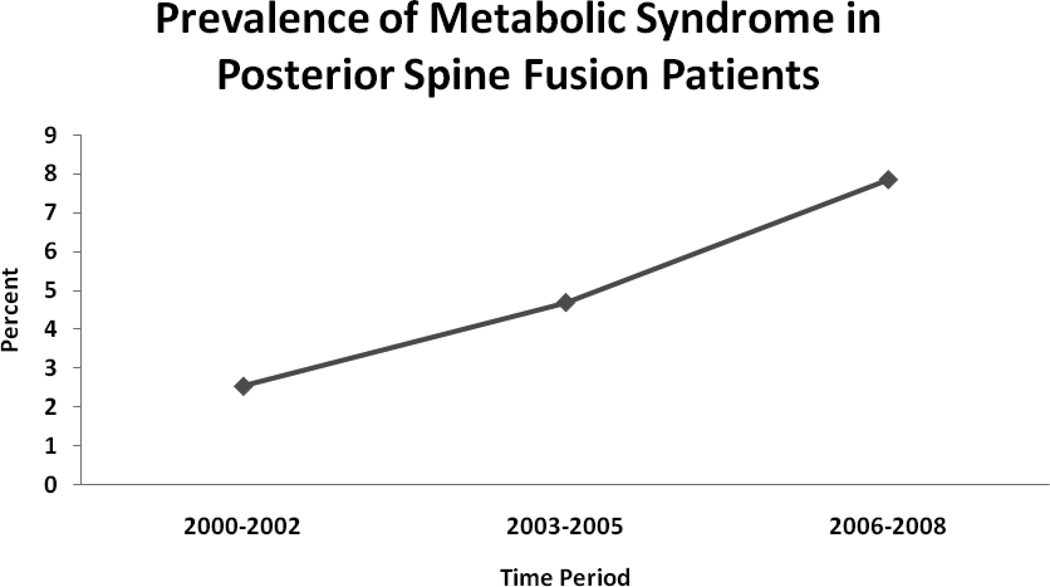
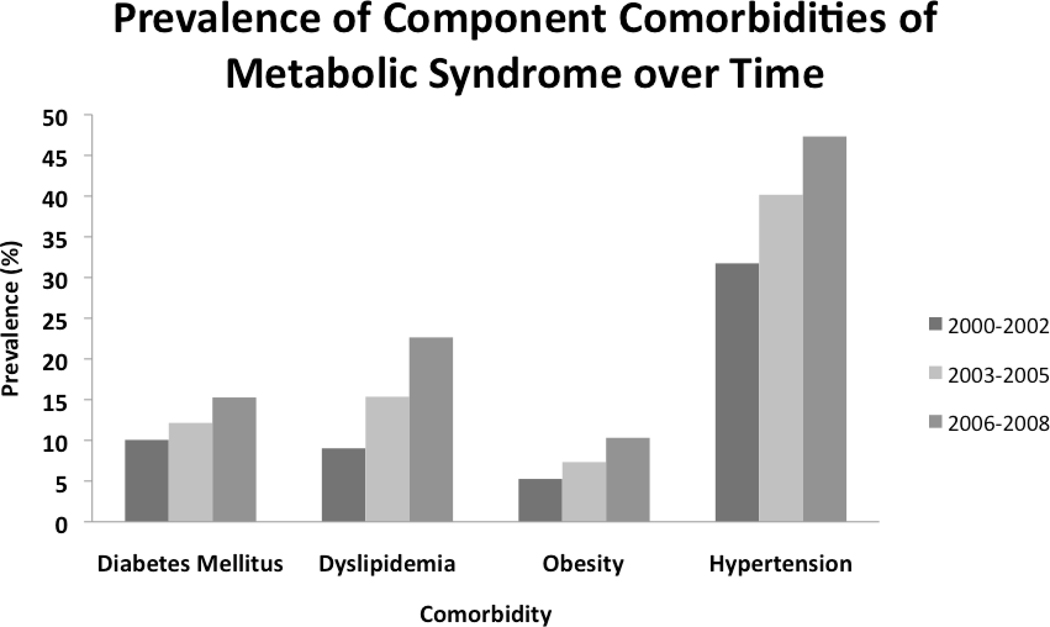
A greater than three-fold increase in the prevalence of MetS among the population undergoing PSF was seen over time. The average prevalence of MetS over the entire study period was 5.5%, with a peak of 9% in 2008 (Figure 1). An increase in the prevalence of MetS component comorbidities was detected between the time periods 2000–2002 and 2006–2008 (Figure 2). The highest proportional increases in comorbidity prevalence were seen for dyslipidemia (151%) and obesity (96%). (Figure 2)
Figure 1.
Prevalence of metabolic syndrome between 2000 and 2008 among admissions for primary posterior lumbar spine fusion.
Figure 2.
Prevalence of metabolic syndrome component comorbidities in admissions for primary posterior lumbar spine fusion over time.
Table 1 shows the demographics for patient with and without MetS undergoing PSF. Several patient characteristics differed between MetS and non-MetS admissions.
The average age was higher for MetS patients and rates of MetS were disproportionately high in age groups of 45–74 compared to those aged less than 44 years and over 75 years. MetS was disproportionately prevalent among female PSF patients. Patients of minority race groups were more frequently affected by MetS. For example, among PSF admissions, black race was 75% more likely among MetS versus non-MetS patients. Prevalence of MetS did not differ among hospitals based on teaching status, size or location. Admissions of patients with MetS for PSF were more frequently of an elective nature. MetS patients were disproportionately likely to have spinal stenosis as an indication for surgery and more frequently had multiple indications compared to non-MetS patients.
Table 2 lists the prevalence of comorbidities in MetS and non-MetS admissions. The presence of MetS was associated with higher rates for all studied comorbidities, which was also reflected in a higher average comorbidity index (Table 2).
Table 2.
Comorbidities of admissions with and without metabolic syndrome (MetS).
| Comorbidities | |||
|---|---|---|---|
| Comorbidity | No MetS | MetS | P-value |
| Congestive Heart Failure | 1.5 | 3.9 | <.0001 |
| Chronic Lung Disease | 12.6 | 16.6 | <.0001 |
| Liver Disease | 0.7 | 0.9 | 0.0101 |
| Neurologic Disorders | 2.7 | 2.5 | 0.3119 |
| Peripheral Vascular Disease | 1.4 | 4 | <.0001 |
| Renal Disease | 0.7 | 3.5 | <.0001 |
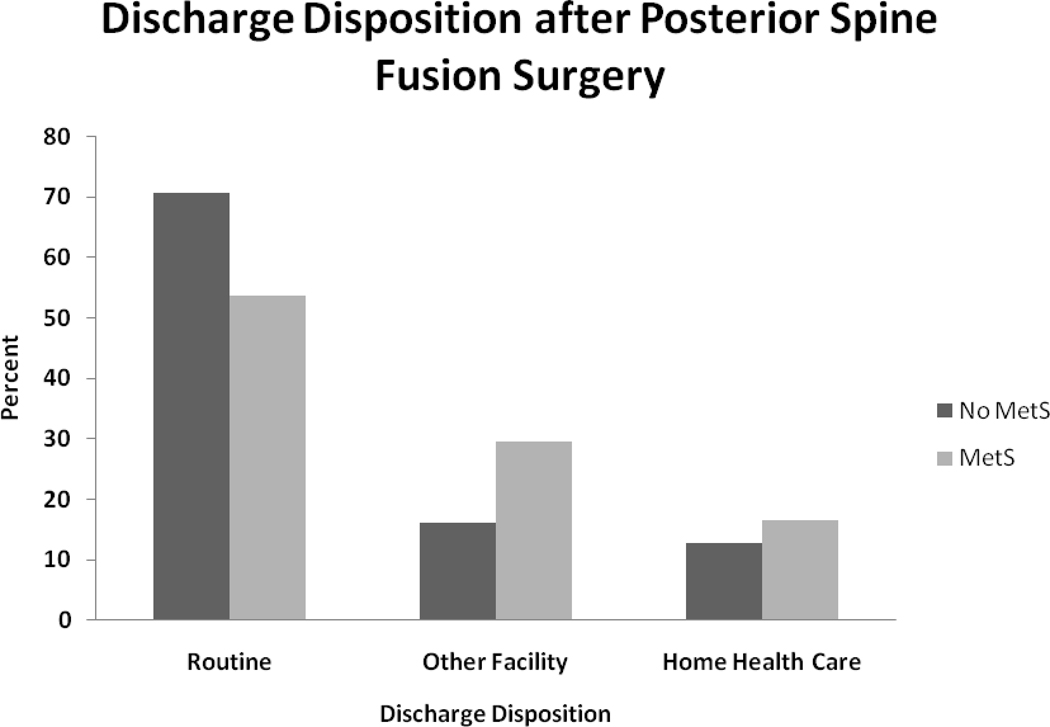
Length of stay was slightly, but significantly longer for HMS patients after PSF 4.69 days (CI 4.64; 4.75) versus 4.55 days (CI 4.54; 4.57), (P<0.0001). Moreover, MetS patients were less frequently discharged to their home and more frequently to another health care facility (P<0.0001) when compared to non-MetS patients (Figure 3). Median hospital charges were higher for MetS versus non-MetS patients for PSF ($23,215 versus $21,739, P<0.0001).
Figure 3.
Disposition status after primary posterior lumbar spine fusion of patients with and without metabolic syndrome.
MetS admissions were associated with an increased incidence of in-hospital major life-threatening complications compared to non-MetS patients (Table 3). The biggest differences were seen for cardiac and pulmonary complications.
Table 3.
Major complications of admissions with and without metabolic syndrome (MetS) undergoing primary posterior lumbar spine fusion.
| Complications | |||
|---|---|---|---|
| Complications | No MetS | MetS | P value |
| Cerebrovascular Event | 0.1 | 0.2 | 0.3489 |
| Pulmonary Complication | 1.2 | 1.6 | 0.0006 |
| Sepsis | 0.4 | 0.2 | 0.0216 |
| Shock | 0.1 | 0.1 | 0.8254 |
| Myocardial Infarction | 0.3 | 0.6 | <.0001 |
| Cardiac Complications | 2.9 | 5.1 | <.0001 |
| Pneumonia | 1.3 | 1.5 | 0.0308 |
| Venous Thromboembolism | 0.4 | 0.4 | 0.4148 |
| Death | 0.2 | 0.1 | 0.2394 |
| Total | 5.6 | 8.5 | <.0001 |
When controlling for the indication for surgery, admission type, hospital (bed size, teaching status and location), and patient related covariates (age, gender, race and comorbidities), MetS was a risk factor for increased cost (i.e. =/> 75th percentile ($30,263)) (1.25 (CI 1.19; 1.31), P<0.0001) and non-routine disposition (1.55 (CI 1.49; 1.62), P<0.0001). Furthermore, MetS increased the odds for prolonged hospital stay (i.e. =/> 75th percentile (4.7 days)) (1.09 (CI 1.05; 1.14), P<0.0001) and the development of a major complication (1.11 (CI 1.03, 1.20), P=0.0054).
Discussion
Using data from a nationally representative database collected between 2000 and 2008, we have shown that MetS is an independent risk factor for increased length of hospital stay, non-routine disposition, increased cost and the development of major complications after PSF.
We were able to identify a significant increase in the prevalence of MetS among patients undergoing PSF over time. Furthermore, we showed an increase in MetS component comorbidities over the course of the study period with a near doubling in the prevalence of obesity and a 2.5 fold increase in the prevalence of dyslipidemia. Recent studies suggest that the prevalence of MetS in the United States is between 13 and 40%. 17–19 The frequency of MetS among PSF patients has not yet reached the levels seen in the general population, however we show that the prevalence in this patient population tripled between 2000 and 2008, and had reached 9% by 2008. The implications for the future are not clear, but the number and proportion of spinal fusion patients with MetS is likely to continue to rise given the worsening worldwide obesity epidemic and an aging population.
Certain demographic characteristics were positively associated with MetS in PSF patients. Middle-aged patients (age groups between 45 and 74), women, and patients of Black race were found to be overly represented among admissions with MetS compared to those without the syndrome. Of note, several studies of overall MetS prevalence in the United States indicate a higher prevalence of MetS in men compared to women and non-hispanic white men compared to Black men.17–19 While MetS may be more common in men overall, our data suggests that female gender is significantly associated with MetS in the PSF patient population. Research indicates higher rates of MetS in non-hispanic Black women and Mexican-American women compared to non-hispanic white women, which is in concordance with race distributions in our analysis.20
The MetS population undergoing PSF presents with a unique surgical, medical, and pathological profile. Patients with MetS are disproportionately likely to be undergoing elective surgery, suggesting the opportunity for more careful selection and optimization of patients for this procedure. Preselection may enable the limitation of this invasive procedure to patients with adequate health status. This is particularly important as we found that MetS was associated with higher rates of congestive heart failure, chronic lung disease, liver disease, peripheral vascular disease, and renal disease. The aforementioned attributes of PSF patients with MetS present distinct challenges in perioperative management above and beyond control of the component diagnoses (dyslipidemia, obesity, hypertension, and diabetes).21 More careful selection of surgical candidates may explain the lower overall rates of MetS found among PSF admissions compared to the general population.
On pathological examination MetS patients were more likely to have spinal stenosis and to have multiple indications for surgery. The cause of the association between MetS and spinal stenosis is unclear and warrants further exploration. One possible explanation for our findings is that surgeons may be more likely to proceed with surgery on patients with comorbidities associated with MetS when the patients present with multiple indications and/or high risk spinal stenosis. MetS patients with a single diagnosis such as scoliosis or degenerative disc disease may be more likely to be managed non-surgically than patients without MetS. MetS patients with multiple indications for posterior spinal fusion may benefit from staged procedures, shortened OR times, and minimally invasive approaches in an effort to minimize associated morbidity.
Patients with metabolic syndrome have multiple risk factors for atherosclerosis and are known to be at increased risk for cardiovascular disease and related mortality as well as all-cause mortality.1,2 Obesity has been paradoxically associated with improved outcome after non-cardiac surgery, however several studies have shown that patients with MetS are at increased perioperative risk. Glance et. al found that perioperative mortality was doubled among super-obese patients with MetS after noncardiac surgery and cardiac adverse events were 2–2.5 fold higher in all patients with MetS undergoing noncardiac surgery.22 In that study, musculoskeletal procedures accounted for 5.33% of the surgeries evaluated.22
Few studies have specifically examined the outcomes of patients with MetS after orthopedic surgery. In this work, with univariate analysis, we found patients with metabolic syndrome to have increased rates of major complications after PSF, including cardiac and pulmonary complications. After controlling for covariates MetS emerged as an independent risk factor for life-threatening complications after PSF. It is also important to note that most comorbidities which were also associated with increased risk for adverse outcome (data not shown) had a higher prevalence among MetS patients undergoing PSF. While these comorbidities do not contribute to the official definitions of MetS, they are linked to the presence of this disease complex by virtue of their high prevalence and therefore cannot be discounted in the overall risk assessment of the MetS patient.
MetS has been correlated with prolonged length of hospital stay after coronary artery bypass grafting.23 In addition, an evaluation of men underoing gastric bypass surgery for morbid obesity found MetS to be the single largest risk factor for prolonged length of stay.24 In this study, we evaluated the impact of MetS on length of stay, cost, and discharge status after PSF. After multivariate analysis, we found MetS patients to have significantly longer hospital stays, higher average hospital charges, and more frequent discharges with home health care or to secondary healthcare facilities.
The excess cost associated with non-routine disposition for MetS patients could not be measured in this study, but is undoubtedly significant. Moreover, evidence suggests that functional outcomes after hip and knee arthroplasty are worse in patients with MetS, possibly due to a pre-existing systemic pro-inflammatory state.25 As the percentage of patients with MetS undergoing spine surgery rises, research into the long-term functional outcomes of these patients and the costs of long-term care and rehabilitation are warranted.
Our study is limited by a number of factors inherent to secondary analysis of large administrative databases. Clinical information available in the NIS, including data on intraoperative events, is limited and our analysis must be interpreted accordingly. Further, information on the levels of surgery is not available for the majority of cases and could therefore not be included as a factor in this analysis. Because of the nature of the NIS, only in-patient data are available and thus complications and events after discharge are not captured. Furthermore, readmissions cannot be discerned from this database. Thus, conclusions should be limited to the acute perioperative setting with the notion that complications and cost are likely underestimated. Other databases, i.e. the Medicare database, contain such longitudinal information and could be used to answer these questions, however they have other limitations, in this case the inclusion of patients above Medicare eligible age. While it cannot be excluded that data entry may be subject to some form of coding or reporting bias, there is no reason to believe that reporting should differ between patients within the database. Both MetS and non-MetS discharges are likely to be exposed to the same bias within the same data collection construct, thus comparative analysis should be unlikely to be affected by such bias. Further, our data on MetS has to be interpreted in the context of the definition used in this study, which is based on the use of ICD-9-codes and was chosen to approximate the definition put forth by the US National Cholesterol Education Program Adult Treatment Panel III. It should be noted, however, that several definitions of MetS exist in the literature.3–5 Finally, we would like to mention that it was beyond the scope of this study to compare outcomes of surgical and non-surgical treatment of spine disease in patients with and without MetS.
It is likely that the rate of MetS in this study is underestimated as only cases for which a component diagnosis code was listed were eligible for inclusion. Thus, the true impact of MetS on outcomes may be higher. Indeed, it should be mentioned that the number of possible diagnosis codes that can be enetered is limited in any data base and may thus lead to under reporting of diseases that are considered less acute for any given hospitalization. Therefore, comorbidities like obesity or hypertension are likely to have even higher prevalence than that reported here.
In conclusion, this study provides evidence that patients with MetS undergoing PSF have an increased hospital length of stay, higher costs, and higher need for post-hospitalization care and increased risk for major perioperative complications. Further research into long-term post-operative outcomes for these patients is warranted.
Key points.
The prevalence of metabolic syndrome among primary posterior spine fusion patients tripled between the time periods 2000–2002 and 2006–2008.
Patients with metabolic syndrome undergoing primary posterior lumbar spine fusion present with higher rates of comorbidities.
Following primary posterior lumbar spine fusion, patients with metabolic syndrome have increased perioperative complications, hospital length of stay, cost of hospitalization, and need for post-hospitalization care.
Acknowledgments
Financial disclosure: This study was performed with funds from the Hospital for the Department of Anesthesiology at the Hospital for Special Surgery (Stavros G. Memtsoudis) and Center for Education and Research in Therapeutics (CERTs) (AHRQ RFA-HS-05-14) (Ya-lin Chiu and Madhu Mazumdar) and Clinical Translational Science Center (CTSC) (NIH UL1-RR024996) (Yan Ma and Madhu Mazumdar).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Attribute to: Departments of Anesthesiology and Public Health and Biostatistics Hospital for Special Surgery, Weill Medical College of Cornell University.
IRB: As the data used in this study are sufficiently de-identified this project was exempt from review by the institutional review board.
No conflicts of interest arise from any part of this study for any of the authors.
The manuscript submitted does not contain information about medical device(s)/drug(s). Federal and Institutional funds were received to support this work. No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript.
References
- 1.Isomaa B, Almgren P, Tuomi T, et al. Cardiovascular morbidity and mortality associated with the metabolic syndrome. Diabetes Care. 2001;24:683–689. doi: 10.2337/diacare.24.4.683. [DOI] [PubMed] [Google Scholar]
- 2.Lakka HM, Laaksonen DE, Lakka TA, et al. The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men. JAMA. 2002;288:2709–2716. doi: 10.1001/jama.288.21.2709. [DOI] [PubMed] [Google Scholar]
- 3.Grundy SM, Brewer HB, Jr, Cleeman JI, et al. Definition of metabolic syndrome: report of the National Heart, Lung, and Blood Institute/American Heart Association conference on scientific issues related to definition. Circulation. 2004;109:433–438. doi: 10.1161/01.CIR.0000111245.75752.C6. [DOI] [PubMed] [Google Scholar]
- 4.Alberti KG, Zimmet P, Shaw J, et al. IDF Epidemiology Task Force Consensus Group. The metabolic syndrome- a new worldwide definition. Lancet. 2005;366:1059–1062. doi: 10.1016/S0140-6736(05)67402-8. [DOI] [PubMed] [Google Scholar]
- 5.Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III) JAMA. 2001;285:2486–2497. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 6.Pollex RL, Hegele RA. Genetic determinants of the metabolic syndrome. Nat Clin Pract Cardiovasc Med. 2006;3:482–489. doi: 10.1038/ncpcardio0638. [DOI] [PubMed] [Google Scholar]
- 7.Glance LG, Wissler R, Mukamel DB, et al. Perioperative outcomes among patients with the modified metabolic syndrome who are undergoing noncardiac surgery. Anesthesiology. 2010;113:859–872. doi: 10.1097/ALN.0b013e3181eff32e. [DOI] [PubMed] [Google Scholar]
- 8.Gray DT, Deyo RA, Kreuter W, et al. Population-based trends in volumes and rates of ambulatory lumbar spine surgery. Spine. 2006;31:1957–1963. doi: 10.1097/01.brs.0000229148.63418.c1. [DOI] [PubMed] [Google Scholar]
- 9.HCUP Databases. Healthcare Cost and Utilization Project (HCUP) Rockville, MD: Agency for Healthcare Research and Quality; 2008. [Accessed March 15, 2010]. Available at Accessed http://www.hcup-us.ahrq.gov/nisoverview.jsp. [Google Scholar]
- 10.Introduction to the HCUP National Inpatient Sample (NIS) 2006. Rockville, MD: Agency for Healthcare Research and Quality, Healthcare Cost and Utilization Project (HCUP); 2008. [Accessed March 15, 2010]. Available at http://www.hcup-us.ahrq.gov/db/nation/nis/2006NIS_INTRODUCTION.pdf. [Google Scholar]
- 11.HCUP Comorbidity Software. Healthcare Cost and Utilization Project (HCUP) Rockville, MD: Agency for Healthcare Research and Quality; 2009. [Accessed October 15, 2010]. (at www.hcup-us.ahrq.gov/toolssoftware/comorbidity/comorbidity.jsp.) [Google Scholar]
- 12.Iezzoni LI, Daley J, Heeren T, et al. Identifying complications of care using administrative data. Medical Care. 1994;32:700–715. doi: 10.1097/00005650-199407000-00004. [DOI] [PubMed] [Google Scholar]
- 13.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 14.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–619. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 15.Memtsoudis SG, Ma Y, González Della Valle A, Mazumdar M, Gaber-Baylis LK, MacKenzie CR, Sculco TP. Perioperative outcomes after unilateral and bilateral total knee arthroplasty. Anesthesiology. 2009;111:1206–1216. doi: 10.1097/ALN.0b013e3181bfab7d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kozak LJ. Underreporting of race in the National Hospital Discharge Survey. Adv Data. 1995;265:1–12. [PubMed] [Google Scholar]
- 17.Ford ES, Li C, Zhao G. Prevalence and correlates of metabolic syndrome based on a harmonious definition among adults in the US. J Diabetes. 2010;2:180–193. doi: 10.1111/j.1753-0407.2010.00078.x. [DOI] [PubMed] [Google Scholar]
- 18.Mozumdar A, Liguori G. Persistent increase of prevalence of metabolic syndrome among US adults: NHANES III to NHANES 1999–2006. Diabetes Care. 2011;34:216–219. doi: 10.2337/dc10-0879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vega GL, Barlow CE, Grundy SM. Prevalence of the metabolic syndrome as influenced by the measure of obesity employed. Am J Cardiol. 2010;105:1306–1312. doi: 10.1016/j.amjcard.2009.12.048. [DOI] [PubMed] [Google Scholar]
- 20.Ervin RB. Prevalence of metabolic syndrome among adults 20 years of age and over, by sex, age, race and ethnicity, and body mass index: United States, 2003–2006. Natl Health Stat Report. 2009;5:1–7. [PubMed] [Google Scholar]
- 21.Watson K. Surgical risk in patients with metabolic syndrome: focus on lipids and hypertension. Curr Cardiol Rep. 2006;8:433–438. doi: 10.1007/s11886-006-0101-3. [DOI] [PubMed] [Google Scholar]
- 22.Glance LG, Wissler R, Mukamel DB, et al. Perioperative outcomes among patients with the modified metabolic syndrome who are undergoing noncardiac surgery. Anesthesiology. 2010;113:859–872. doi: 10.1097/ALN.0b013e3181eff32e. [DOI] [PubMed] [Google Scholar]
- 23.Brackbill ML, Sytsma CS, Sykes K. Perioperative outcomes of coronary artery bypass grafting: effects of metabolic syndrome and patient's sex. Am J Crit Care. 2009;18(5):468–473. doi: 10.4037/ajcc2009718. [DOI] [PubMed] [Google Scholar]
- 24.Ballantyne GH, Svahn J, Capella RF, et al. Predictors of prolonged hospital stay following open and laparoscopic gastric bypass for morbid obesity: body mass index, length of surgery, sleep apnea, asthma, and the metabolic syndrome. Obes Surg. 2004;14:1042–1050. doi: 10.1381/0960892041975460. [DOI] [PubMed] [Google Scholar]
- 25.Gandhi R, Razak F, Davey JR, et al. Metabolic syndrome and the functional outcomes of hip and knee arthroplasty. J Rheumatol. 2010;37:1917–1922. doi: 10.3899/jrheum.091242. [DOI] [PubMed] [Google Scholar]