Abstract
INTRODUCTION
Exposure to child maltreatment is associated with elevated risk for behavioral disorders in adulthood. One explanation for this life-course association is that child maltreatment increases vulnerability to the effects of subsequent stressors; however, the extent to which maltreatment increases sensitivity to social context has never been examined. We evaluated whether the association between neighborhood physical disorder and binge drinking was modified by child maltreatment exposure.
METHODS
Data were drawn from the Detroit Neighborhood Health Study, a prospective representative sample of predominately African Americans in the Detroit population. Neighborhood physical disorder was measured via systematic neighborhood assessment. Child maltreatment indicators included self-reported physical, sexual, and emotional abuse. Incident binge drinking was defined as at least one episode of ≥5 drinks (men) or ≥4 drinks (women) in the past 30-day period among those with no binge drinking at baseline (N=1,013).
RESULTS
Child maltreatment and neighborhood physical disorder interacted to predict incident binge drinking (B=0.16, p=0.02) and maximum number of past 30-day drinks (B=0.15, p=0.04), such that neighborhood physical disorder predicted problematic alcohol use only among individuals with high exposure to child maltreatment.
CONCLUSION
The results add to the growing literature that African Americans in the U.S. are exposed to an array of stressors that have pernicious consequences for problematic alcohol use. Our results document the need for increased attention to the potential for at-risk alcohol use among populations with a high degree of stress exposure.
Keywords: binge drinking, child maltreatment, neighborhood effects, neighborhood physical disorder, African Americans
1. Introduction
The World Health Organization has called for the development of global strategies to reduce alcohol consumption (Casswell and Thamarangsi, 2009), noting the high social, medical, and economic cost of excessive alcohol consumption worldwide (Jarl et al., 2008; Rehm et al., 2009). Excessive alcohol use is the third leading cause of mortality in the US (Mokdad et al., 2004), and binge drinking, defined as five or more drinks for men and four or more drinks for women per drinking occasion (National Institute on Alcohol Abuse and Alcoholism, 2005) is associated with numerous adverse health outcomes. Acute effects of binge drinking include intentional as well as unintentional injury (Hingson et al., 2002), intimate partner violence (Thompson and Kingree, 2006), unintended pregnancy (Naimi et al., 2006a), and fetal alcohol syndrome (May and Gossage, 2001), and chronic binge drinking is associated with several forms of cancer (Longnecker et al., 1994), disruption in liver function, and premature mortality (Holman et al., 1996). Binge drinking is implicated in over half of the alcohol-attributable deaths in the U.S. (Naimi et al., 2003b).
At the individual level, risk factors for binge drinking include young adulthood, White race/ethnicity, male gender, and psychiatric disorders (Hasin et al., 2007). Substantial evidence indicates that individuals with a history of maltreatment in childhood are at higher risk for at-risk drinking later in life (Hussey et al., 2006; Kessler et al., 1997; MacMillan et al., 2001; Widom et al., 1995). Population-based prospective data have documented high rates of binge drinking and alcohol abuse/dependence among adults reporting experiences of physical and emotional abuse (MacMillan et al., 2001), neglect (Hussey et al., 2006; Widom et al., 1995, 2007), and sexual abuse (Kessler et al., 1997; MacMillan et al., 2001; Molnar et al., 2001) in childhood.
In addition to these individual-level stressors, a growing literature suggests that residence in disorganized and chaotic neighborhoods can be a stressful experience with deleterious implications for mental health, including substance use (Galea et al., 2004; Gmel et al., 2004). Elevated rates of alcohol use (Cerda et al., 2010; Galea et al., 2007; Rice et al., 1998) and binge drinking (Bernstein et al., 2007; Cerda et al., 2010; Hill and Angel, 2005) have been documented consistently among individuals living in neighborhoods characterized by poverty, inequality and physical disorder (with a few notable exceptions (Ennett et al., 1997; Pollack et al., 2005)). Neighborhoods with lower social cohesion have higher rates of alcohol use disorders (Winstanley et al., 2008) and alcohol-related arrests (Duncan et al., 2002) than high-cohesion neighborhoods. Further, disorganized and chaotic neighborhoods have higher alcohol outlet density (Gruenewald et al., 2002; Scribner et al., 1994), more permissive social norms with respect to drinking and drunkenness (Ahern et al., 2008), making the use of alcohol a more accessible and socially sanctioned coping strategy to manage the chronic stress of living in an unsafe and disordered area. (Boardman et al., 2001). In summary, exposure to neighborhood physical disorder is a chronic stressful experience associated with elevated use of alcohol, potentially as a coping strategy to manage stress. However, not all individuals who confront stressful living conditions demonstrate elevated levels of alcohol consumption. Yet we are unaware of previous research examining factors that promote alcohol consumption in the presence of neighborhood physical disorder.
The experience of child maltreatment may be one such effect-modifying factor. Accumulating evidence indicates that child maltreatment increases vulnerability to the deleterious mental health effects of stressors that occur later in development, which has been referred to as “stress sensitization” (Hammen et al., 2000; McLaughlin et al., 2010a). The association between adult stressful life events and risk for mood and anxiety disorders is stronger among individuals with high exposure to child maltreatment (Espejo et al., 2007; Hammen et al., 2000; Kendler et al., 2004; McLaughlin et al., 2010a). Dysregulation in physiological stress response systems is thought to underlie this increased stress sensitivity (Essex et al., 2002; Heim and Nemeroff, 2001; Loman and Gunnar, 2010; Oosterman et al., 2010). Child maltreatment also is associated with increased emotional reactivity (Glaser et al., 2006; McLaughlin et al., 2010b; Wichers et al., 2009) as well as disruptions in the ability to adaptively modulate negative emotions (McLaughlin and Hatzenbuehler, 2009; McLaughlin et al., 2009). These patterns of emotional responses among maltreated individuals may increase liability to alcohol misuse in the context of adult stress. Specifically, individuals who are emotionally reactive and who have limited skills for effectively modulating their emotions may turn to alcohol or other substances to manage negative affect and arousal following stress (Carpenter and Hasin, 1998; Cooper et al., 1995; Ham and Hope, 2003). To date, however, stress sensitization effects have been examined almost exclusively in relation to mood and anxiety disorders (Espejo et al., 2007; Hammen et al., 2000; Kendler et al., 2004; McLaughlin et al., 2010a) with the exception of one study showing that adult stressors were more likely to precipitate acts of interpersonal violence among individuals with high levels of childhood maltreatment (Roberts et al., 2011).
The current study addresses two notable gaps in the literature. First, it is unclear how individual-level characteristics increase vulnerability to binge drinking among those exposed to the chronic stress of living in a disordered neighborhood. Second, the stress sensitization hypothesis has never been examined in predicting at-risk alcohol use, a prevalent and often debilitating health behavior. We address these gaps by examining whether exposure to childhood maltreatment increases susceptibility to at-risk drinking in the context of disordered neighborhood environments in adulthood in a prospective community-based sample of predominately African-American individuals living in Detroit, Michigan. Specifically, we assess whether the relation between neighborhood physical disorder and binge drinking differs according to prior exposure to child maltreatment. Our specific aims are as follows: First, we examine whether neighborhood physical disorder, assessed using a standardized objective measure completed by independent raters, predicts incident binge drinking over the course of one year. Second, we examine whether reports of childhood maltreatment moderate the effect of neighborhood physical disorder on binge drinking. We include rigorous controls not only for established individual-level risk factors such as age, sex, and indicators of socio-economic position, but also for contextual-level confounders. Further, we examine evidence for a similar effect modifying effect for an alternative measure of at-risk drinking: largest number of drinks in the past 12 months. Given documented associations between neighborhood socio-economic position and binge drinking (Jones-Webb et al., 1997; Pollack et al., 2005), we control for average neighborhood income, house price, and percent living below the poverty line. Based on previous research documenting the sensitizing effects of childhood maltreatment on risk for psychopathology following stressful life events in adulthood, we predict that the association of neighborhood physical disorder with incident binge drinking is stronger among individuals with high exposure to child maltreatment than among individuals with low exposure to maltreatment.
2. Methods
2.1. Study sample
Data were drawn from the Detroit Neighborhood Health Study (DNHS), a longitudinal cohort of predominately African-American adults (18+) living in Detroit, Michigan. Wave 1 was conducted between 2008-2009. Participants were selected using a dual-frame probability design, using telephone numbers obtained from the U.S. Postal Service Delivery Sequence Files as well as a list-assisted random-digit-dial frame. Individuals without listed landlines or telephones and individuals with only a cell phone listed were invited to participate through a postal mail effort. A total of 1,547 individuals participated in Wave 1, with an overall participation rate among eligible persons of 53%. Each survey participant was assigned weights that accounted for the method of obtaining contact information and the selection probability of households of different sizes and with a different number of telephone lines, and adjusted the sample to be representative of the Detroit population on a wide range of socio-demographic characteristics. Further information regarding baseline sampling can be found elsewhere (Goldmann et al., in press ; Koenen et al., 2011; Uddin et al., 2010). Wave 2 was conducted one year following Wave 1; a total of 1,054 individuals were re-interviewed (68% of the baseline sample). Those who did not respond were younger (χ2=8.8, p<0.01), less educated (χ2=19.0, p<0.01), more likely to be unemployed (χ2=9.3, p=0.01) and single (χ2=31.6, p<0.01); sample weights were incorporated to account for informative attrition between Waves 1 and 2. The present study focuses on the subset of individuals who reported no history of binge drinking at baseline in order to capture incident cases (N=1,013); sensitivity analyses were performed on the whole sample.
Participants at both waves completed a 40-minute telephone survey. Informed consent was obtained at the beginning of each interview, and respondents were offered $25 for their participation in each interview. The Institutional Review Board of the University of Michigan reviewed and approved the study protocol.
2.2. Measures
2.2.1. Alcohol consumption
Two alcohol outcomes were assessed. Maximum drinks. Participants reported the largest number of drinks consumed on days they drank in the 30-days prior to the interview (range 0 to 20). Binge drinking. Using the maximum drinks variable, binge drinking was defined as consuming five or more drinks (men) or four or more drinks (women) at least once in the 30-days prior to the interview.
2.2.2. Neighborhood physical disorder
Systematic assessments of neighborhood physical environment in a random sample of 138 block groups in all 54 Detroit neighborhoods were conducted by trained independent observers at Wave 1. Observers rated the neighborhood physical environment on 19 items adapted from the New York City IMPACT neighborhood evaluation scale (Ompad et al., 2008). Factor analyses suggested that three items formed a cohesive measure of the external physical environment: 1) presence of buildings with broken windows, boarded up windows, or boarded up doors; 2) presence of buildings with outside damage that can only be corrected by major repairs such as siding, shingles, boards, brick, concrete, and stucco; and 3) presence of entirely vacant buildings. These measures also demonstrated excellent internal consistency (α=0.83). The factor analyses yielded principal component values for each block group, which were then tested for and showed spatial autocorrelation in ArcMap Version 9.2 (ESRI, Redlands, CA) (Moran’s I= 0.14, z-score=4.08, p<0.01). We then used ordinary kriging methods (Koizumi et al., 2009; Kumar et al., 2007) within ArcMap Version 9.2 to predict frequency values for those areas of Detroit that were not evaluated and created maps of these prediction estimates. Predicted values were then averaged by neighborhood. We used these values to create a continuous score representing the physical organization of each respondent neighborhood (mean=−0.12, range −1.52 to 1.23), and then categorized the variable into quartiles to detect potential non-linear relationships with alcohol outcomes. Because our main effect analyses indicated that neighborhood disorganization was monotonically associated with alcohol outcomes, we used a continuous variable for analyses of interaction.
2.2.3. Childhood maltreatment
Childhood maltreatment questions were included at Wave 2 and drawn from the Conflict Tactics Scale (CTS) (Straus, 1979) and the Childhood Trauma Scale (CTQ) (Bernstein et al., 1997). CTS items assessed physical abuse (e.g., “People in my family hit me so hard that it left me with bruises and marks”), and emotional abuse (e.g., “People in my family said hurtful or insulting things to me”) assessed before age 11. Response options were rated on a five point scale and ranged from “never true” (1) to “very often true” (5). CTQ items assessed physical abuse before age 18 (e.g., “Did your parent, step-parent, or adult guardian ever push, grab, or shove you”) with response options ranging from “never” to “more than a few times” and sexual abuse before age 18 (e.g., “Were you ever touched in a sexual way by an adult or older child...”) which was coded as occurring once, multiple times, or never.
CTS physical abuse and emotional abuse questions as well as CTQ physical and sexual abuse questions were recoded into three-level variables indicating whether each abuse type occurred: 1) never, 2) rarely or sometimes, or 3) often. Scores were summed to create a continuous variable ranging from 0 to 22 which was normally distributed in the sample. We also dichotomized the child maltreatment variable at the 75th percentile.
2.2.4. Control variables
Individual-level control variables included age, sex, race/ethnicity, income, education, employment status, and marital status. Variable coding is shown in Table 1. As described above, we controlled for three indicators of neighborhood socio-economic position to document the specific effect of neighborhood physical disorder. Neighborhood-level covariates included three variables assessed at the level of Census tracts (US Bureau of the Census, 2000): percent living below the poverty line, median house value, and median income. These variables were categorized into quartiles. Preliminary analyses indicated that neighborhood disorder measured at the neighborhood level was significantly associated with each Census tract socio-economic indicator at p<0.0001.
Table 1.
Socio-demographic characteristics comparing those with incident binge drinking to those without in a prospective community sample of individuals in Detroit, Michigan (N=1,013)
| N | Incident binge drinking, % (SE) |
No incident binge drinking, % (SE) |
Chi-square, df, p-value |
|
|---|---|---|---|---|
| 26 | 987 | |||
| Sex | ||||
| Male | 401 | 72.1 (10.6) | 45.6 (2.7) | 3.7, 1, 0.04 |
| Female | 612 | 27.9 (10.6) | 54.4 (2.7) | |
| Age | ||||
| 18-34 | 125 | 24.6 (9.1) | 32 (2.9) | 2.6, 5, 0.02 |
| 35-44 | 154 | 4.8 (4.7) | 14.9 (1.7) | |
| 45-54 | 227 | 35 (13.8) | 23.1 (2.1) | |
| 55-64 | 258 | 32.9 (11.9) | 15.6 (1.5) | |
| 65-74 | 139 | 2.7 (2.0) | 9 (1.2) | |
| 75+ | 104 | 0 (0.0) | 5.4 (0.8) | |
| Race/ethnicity | ||||
| Black | 863 | 89.9 (7.1) | 88.4 (1.7) | 1.4, 2, 0.24 |
| White | 111 | 9.1 (7.0) | 7.6 (1.3) | |
| Other | 39 | 1.0 (0.9) | 4.0 (1.2) | |
| Marital status | ||||
| Married | 272 | 17.8 (9.3) | 29.1 (2.2) | 1.1, 2, 0.34 |
| Divorced/Separated/Widowed | 403 | 46.8 (13.1) | 26.1 (2.0) | |
| Never married | 338 | 35.4 (12.1) | 44.8 (2.7) | |
| Education | ||||
| Less than high school | 128 | 6.4 (5.2) | 15.5 (2.0) | 1.4, 2, 0.25 |
| High school or GED | 288 | 59.3 (12.9) | 42.3 (2.7) | |
| More than high school | 597 | 34.3 (12.7) | 42.2 (2.5) | |
| Personal income | ||||
| Less than 25,000 | 276 | 29.1 (11.5) | 33.6 (2.7) | 0.2, 2, 0.85 |
| 25-50,000 | 241 | 33.7 (13.1) | 26.4 (2.4) | |
| 50,000+ | 354 | 37.2 (14.4) | 40.1 (2.7) | |
| Employment | ||||
| Looking for work or unemployed | 156 | 19.8 (9.0) | 25.9 (2.7) | 0.4, 1, 0.53 |
| Other | 857 | 80.2 (9.0) | 74.1 (2.7) |
2.3 Statistical analysis
All analyses were conducted using SAS-callable SUDAAN software (Research Triangle Institute, 2009), and adjusted for the complex survey design as well as attrition weights. Bivariate associations between exposure variables and binge drinking were examined using cross-tabulations, chi-square tests, and multivariate associations were examined using logistic regression. Bivariate and multivariate associations between exposure variables and maximum number of drinks were assessed with Poisson regression due to non-normality of the distribution. Interactions between child maltreatment and neighborhood physical disorder were assessed on the multiplicative scale. Preliminary analyses indicated that continuous measures of childhood maltreatment and neighborhood physical disorder were uncorrelated (Pearson’s correlation coefficient=0.04, p=0.16). Statistical significance was evaluated using 2-sided .05 level tests.
3. Results
The incidence of binge drinking was 3.48% (SE=0.9). Binge drinking was more common among males (x2=3.7, df=1, p=0.04) and those in middle age (45-64; x2=2.6, df=5, p=0.02) (Table 1). Examining socio-demographic associations with neighborhood physical disorder, those living in disordered neighborhoods were more likely to be never married (x2=5.4, df=2, p=0.005) and make less than $25,000 in the last year (x2=4.3, df=2, p=0.01).
Table 2 shows the main effects of childhood maltreatment and neighborhood physical disorder on binge drinking and maximum drinks. First we examined a continuous variable summing all maltreatment experiences; childhood maltreatment was significantly associated with binge drinking. Each one-unit increase in the childhood maltreatment score was associated with 1.1 times the odds of binge drinking (95% C.I. 1.01-1.23). When maltreatment types were examined individually, sexual abuse was associated with 3.1 times increased odds of binge drinking (95% C.I. 1.04-9.35). The associations between neighborhood physical disorder and alcohol outcomes were not statistically significant.
Table 2.
Main effects of childhood maltreatment and neighborhood physical disorder on incident binge drinking and maximum drinks in the past 30-days among respondents with no binge drinking at the baseline interview in a prospective community sample of individuals in Detroit, Michigan (N=1,013)
| N | % Incident Binge Drinking |
OR (95% C.I.) | OR** (95% C.I.) | Mean maximum drinks in the past 30 days |
Unadjusted incidence density ratio |
Adjusted incidence density ratio** |
|
|---|---|---|---|---|---|---|---|
| Childhood maltreatment |
|||||||
| Cumulative childhood maltreatment |
-- | 1.10 (1.01-1.20) | 1.11 (1.01-1.23) | -- | 1.02 (0.99-1.05) | 1.03 (0.99-1.06) | |
| Physical abuse | 277 | 5.42 | 1.78 (0.58-5.40) | 2.59 (0.83-8.11) | 2.58 | 1.18 (0.95-1.48) | 1.2 (0.95-1.51) |
| No physical abuse | 736 | 3.12 | 1 | 1 | 2.18 | 1 | |
| Emotional abuse | 171 | 5.69 | 1.99 (0.65-6.09) | 1.00 (0.34-2.97) | 2.75 | 1.24 (0.96-1.60) | 1.18 (0.97-1.42) |
| No emotional abuse | 842 | 2.94 | 1 | 1 | 2.22 | 1 | |
| Sexual abuse | 188 | 6.56 | 3.26 (1.18-9.01) | 3.12 (1.04-9.35) | 2.51 | 1.09 (0.81-1.46) | 1.22 (0.92-1.62) |
| No sexual abuse | 825 | 2.11 | 1 | 1 | 2.31 | 1 | |
| Neighborhood physical disorder+ |
|||||||
| Lowest quartile (most disordered) |
257 | 4.52 | 1.14 (0.31-4.27) | 1.72 (0.40-7.44) | 2.76 | 1.28 (0.90-1.81) | 1.28 (0.95-1.72) |
| 2nd quartile | 284 | 2.94 | 0.68 (0.17-2.70) | 1.22 (0.27-5.48) | 2.34 | 1.08 (0.81-1.44) | 1.10 (0.84-1.44) |
| 3rd quartile | 219 | 2.74 | 0.73 (0.16-3.35) | 1.15 (0.28-4.65) | 2.28 | 1.05 (0.79-1.40) | 1.10 (0.86-1.41) |
| Highest quartile (least disordered) |
253 | 3.97 | 1 | 1 | 2.16 | 1 | 1 |
Physical abuse coded positive if greater than 7; emotional neglect coded positive if >2; sexual abuse coded positive if >0; cumulative childhood maltreatment entered as continuous variable
Controlled for age, sex, race, unemployment, education, and income
Higher score is less disordered. Continuous factor score representing three items: presence of buildings with broken windows, boarded up windows, or boarded up doors; presence of buildings with outside damage that can only be corrected by major repairs such as siding, shingles, boards, brick, concrete, and stucco; and presence of entirely vacant buildings.
Table 3 shows the interaction of neighborhood physical disorder and childhood maltreatment predicting binge drinking and maximum number of drinks. In regression models adjusted for demographics and indicators of neighborhood socio-economic position, a significant interaction between neighborhood physical disorder and childhood maltreatment was observed in predicting both binge drinking (β=0.15, SE=0.07, p=0.04) and maximum number of drinks (β=0.05, SE=0.02, p=0.01). As a check on the robustness of the results, we reran these models with prevalent binge drinking (any binge drinking reported at Waves 1 or 2) as the outcome. We continued to observe a significant interaction (β=0.26, SE=0.04, p<0.01), indicating that our results are not limited only to the incident binge drinkers in this sample.
Table 3.
Effect measure modification between neighborhood physical disorder and childhood maltreatment in predicting Wave 2 binge drinking and maximum number of drinks in the past 30 days among those with no binge drinking at baseline in a prospective community sample of individuals in Detroit, Michigan (N=1,013)
| Model 1: Unadjusted | Model 2: Adjusted for demographics+ |
Model 3: Adjusted for demographics and other neighborhood characteristics+ |
|
|---|---|---|---|
| Beta, SE, p-value | Beta, SE, p-value | Beta, SE, p-value | |
| Binge drinking at Wave 2 | |||
| Neighborhood physical disorder* | −1.33 (SE=0.60), p=0.03 | −1.33 (SE=0.60), p=0.03 | −1.21 (SE=0.55), p=0.03 |
| Childhood maltreatment** | 0.06 (SE=0.06), p=0.29 | 0.06 (SE=0.06), p=0.29 | 0.05 (SE=0.06), p=0.43 |
| Interaction between neighborhood disorder and childhood maltreatment |
0.16 (SE=0.07), p=0.02 | 0.16 (SE=0.07), p=0.02 | 0.15 (SE=0.07), p=0.04 |
| Maximum number of drinks at Wave 2 | |||
| Neighborhood physical disorder* | −0.29 (SE=0.12), p=0.01 | −0.71 (SE=0.19), p<0.001 | −0.90 (SE=0.34), p<0.01 |
| Childhood maltreatment | 0.01 (SE=0.01), p=0.25 | −0.01 (SE=0.01), p=0.21 | −0.02 (SE=0.01), p=0.10 |
| Interaction between neighborhood disorder and childhood maltreatment |
0.03 (SE=0.02), p=0.11 | 0.05 (SE=0.02), p=0.004 | 0.05 (SE=0.02), p=0.01 |
Higher score is less disordered. Continuous factor score representing three items: presence of buildings with broken windows, boarded up windows, or boarded up doors; presence of buildings with outside damage that can only be corrected by major repairs such as siding, shingles, boards, brick, concrete, and stucco; and presence of entirely vacant buildings.
Continuous variable with range 0 to 22
Model 2 was adjusted for age, sex, race/ethnicity, income, education, employment status, and marital status. Model three was adjusted for aforementioned variables and additionally controlled for the percent in the census tract that were living below the poverty line, the median house value of the census tract, and the median income of the census tract.
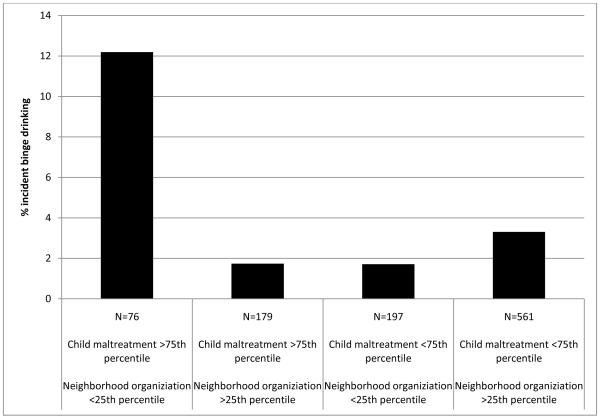
To better understand the direction and magnitude of the interaction, in Figure 1 we stratified by the dichotomized childhood maltreatment variable (dichotomized at the 75th percentile) and examined the associations of the dichotomous neighborhood physical disorder variable with incident binge drinking. The incidence of binge drinking was 12.2% among those with high exposure to childhood maltreatment in the highest quartile of neighborhood physical disorder, compared to 1.74% among those with high childhood maltreatment exposure but in the lowest quartile of neighborhood physical disorder and 1.71% among those in the highest quartile of neighborhood physical disorder but below the 75th percentile on childhood maltreatment. Results were similar for maximum number of drinks (not shown): the mean maximum drinks was 2.74 among those with high exposure to childhood maltreatment in the highest quartile of neighborhood physical disorder, compared to 2.21 among those with high childhood maltreatment exposure but in the lowest quartile of neighborhood physical disorder and 1.85 among those in the highest quartile of neighborhood physical disorder but below the 75th percentile childhood maltreatment.
Figure 1.
Incidence of binge drinking at Wave 2 among those low versus high on neighborhood physical disorder and childhood maltreatment exposure among those with no binge drinking at baseline in a prospective community sample of individuals in Detroit, Michigan (N=1,013)
4. Discussion
Exposure to childhood maltreatment modifies the effect of neighborhood physical disorder on risk of binge drinking among this predominately African American community sample in Detroit, MI. Specifically, high levels of neighborhood physical disorder were associated with elevated risk of incident binge drinking, but only among individuals with high exposure to maltreatment in childhood. The interaction of child maltreatment and neighborhood physical disorder predicted alcohol outcomes even after controlling for individual-level risk factors and neighborhood socio-economic indicators, indicating that the physical characteristics of a neighborhood increases risk of binge drinking, but only among those with a pre-existing vulnerability conferred by early-life exposure to maltreatment. These findings are consistent with the theory that stressors experienced in childhood increase vulnerability to the deleterious consequences of stressful life circumstances in adulthood, thereby heightening risk for adverse health consequences in the context of adult stress (Hammen et al., 2000; Kendler et al., 2004; Espejo et al., 2007; McLaughlin et al., 2010).
We document that the one-year incidence of binge drinking in this sample was 2.56%, which is similar to an estimated national one-year incidence of 3.18%, calculated using available data from the follow-up of the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). However, we note that previous studies have documented that the effect of neighborhood poverty on alcohol use is stronger for African Americans compared with Whites (Jones-Webb et al., 1997). Because our sample is predominately African American and representative of the Detroit community, these results may not generalize to other populations with a different distribution of neighborhood factors and other stressors. However, the results add to the growing literature that African Americans in the U.S. are exposed to an array of stressors that have pernicious consequences for problematic alcohol use (Keyes et al., 2011a), despite exhibiting lower rates of alcohol consumption and alcohol use disorders compared with Whites (Hasin et al., 2007). Our results document the need for increased attention to the potential for problematic alcohol use among populations with a high degree of stress exposure.
Our findings are innovative in several respects. To our knowledge, this is the first study to explore the stress sensitization hypothesis using a neighborhood-level exposure. Our results suggest that the stressful experience of living in a neighborhood characterized by physical disorder increases risk for adverse health outcomes among those with high exposure to childhood maltreatment. A similar sensitizing effect of exposure to child maltreatment has been found in predicting mental health outcomes such as mood and anxiety disorders (Espejo et al., 2007; Hammen et al., 2000; Kendler et al., 2004; McLaughlin et al., 2010a), and preliminary evidence suggests a similar sensitizing role of childhood maltreatment in predicting perpetration of interpersonal violence following adult stress exposure (Roberts et al., 2011). This prior research, however, has evaluated adult stressful life events including interpersonal, occupational, financial, and legal events, and no previous literature has documented a stress sensitization effect for alcohol outcomes. Our findings add to a growing body of research supporting the hypothesis that the negative health consequences of stressful experiences in adulthood, including those conferred by social and contextual factors, are heightened by exposure to childhood maltreatment. These findings suggest that exposure to early-life stress creates a diathesis for psychopathology and substance misuse that can be elicited by stress exposure later in life. Finally, our findings support the hypothesis that individual behavior can be influenced by deleterious features of the social environment; when potentiated by exposures endured throughout the life course, this cascade of stress exposure results in adverse mental health outcomes.
We also document main effects of childhood maltreatment on at-risk drinking. Specifically, we found that sexual abuse significantly predicted incident binge drinking, consistent with substantial epidemiologic evidence documenting the pernicious consequences of sexual abuse for substance use outcomes (see review in Keyes et al., 2011b). Further, these findings provide additional support for neighborhood physical disorder as a risk factor for adverse health outcomes in the presence of childhood maltreatment, independent of the neighborhood socio-economic position. Although studies have been mixed on the association between neighborhood physical disorder and crime rates (a hypothesis known as ‘broken windows’ theory) (Cerda et al., 2009), physical disorder is consistently associated with health outcomes such as sexually transmitted infections (Cohen et al., 2003), mental health (Aneshensel and Sucoff, 1996; Kruger et al., 2007), and obesity (Franzini et al., 2009). Our analyses extend previous studies of the neighborhood context by using independent raters rather than inhabitant self-report to characterize the neighborhood environment. Further, we used rigorous controls for neighborhood socio-economic factors, indicating that physical disorder of the neighborhood is associated with elevated risk for the onset of binge drinking patterns over and above the effects of neighborhood poverty and disadvantage. An important next step in this research program is to determine whether these results generalize to other alcohol-related health outcomes, including alcohol use disorders, liver function, and chronicity of heavy drinking. Mechanisms for this effect may be the increase in alcohol outlets among disorganized neighborhoods (Gruenewald et al., 2002; Scribner et al., 1994), fewer social restrictions on drinking and drunkenness (Ahern et al., 2008), or psychological stress generated by efforts to cope with a negative physical environment (Bernstein et al., 2007). However, we also note that individuals who consume alcohol or possess risk factors associated with heavy alcohol consumption may be more likely to live in or move to neighborhoods that are more disorganized; thus, the causal effect of these associations may be reversed. Although these data are consistent with the hypothesis that neighborhood disorganization is a risk factor for binge drinking in the presence of childhood maltreatment, a social selection hypothesis cannot be ruled out.
These results also add to a growing body of literature marking the importance of studying cumulative adversities experienced across the life course to understand adult health outcomes such as binge drinking. Previous studies have shown that the trajectory of socio-economic status from childhood to adulthood influences alcohol-related and other health risks (Fox et al., 2010; Lloyd and Turner, 2008; Pensola and Martikainen, 2003; Pensola and Valkonen, 2000), especially downward mobility (Pensola and Valkonen, 2000), further indicating that adversity is a life course process and that risks interact to increase the risk for adverse health outcomes. Research is also accumulating to document genetic factors that interact with childhood maltreatment experiences in impacting alcohol use and other externalizing behaviors from adolescence to adulthood (Caspi et al., 2002; Enoch et al., 2010; Kaufman et al., 2007; Kim-Cohen et al., 2006; Widom and Brzustowicz, 2006). These same genetic factors also interact with the social environment to raise risk for psychopathology (Koenen et al., 2009), suggesting that the interplay of stressors across the life course and genetic vulnerability provide a compelling pathway for the incidence and persistence of adverse mental health outcomes.
Because both child maltreatment and neighborhood physical disorder are associated with other adverse exposures that increase the risk for problematic alcohol use, our findings highlight just one piece of a complex set of pathways that link the social environment to patterns of alcohol use in adulthood. We note that childhood maltreatment is correlated with a wide range of adversities in childhood including instability in the home (Dube et al. 2002; Dong et al. 2004), poverty (Turner et al. 2006), and parental dysfunction across multiple domains including substance abuse, criminality, and psychopathology (Dinwiddie and Bucholz 1993; Kelleher et al. 1994; Chaffin et al. 1996; Besinger et al. 1999; Conron et al. 2009). Further, maltreatment in childhood raises the risk for other factors throughout the life course that may mediate the associations observed here, including both perpetrating and being the victim of interpersonal violence in adulthood (Desai et al., 2002; Ehrensaft et al., 2003; McKinney et al., 2009) and conduct disorder in adolescence and antisocial personality disorder in adulthood (Iacono et al., 1999; Jessor and Jessor, 1977). These factors were unmeasured in the present data, thus future research should probe these associations further for specificity across multiple domains of childhood maltreatment and mediators through the life course.
Results should be interpreted with study limitations in mind. Childhood maltreatment is retrospectively self-reported by respondents, which potentially introduces bias into the results (Green et al.; Hardt and Rutter, 2004). Longitudinal studies have documented that child abuse reports, including childhood sexual abuse, are unstable over time (Widom, 1996, 1997). Studies testing the validity of retrospective self-report generally find few false positives, indicating that the consequence of unstable reporting is that the prevalence of childhood maltreatment assessed at only one time point is likely underestimated (Fergusson et al., 2000; Widom, 1996, 1997). Further, several independent cohort studies with both prospective and retrospective assessment of childhood maltreatments have reported that risk association estimates are stable regardless of the timing of assessment (Fergusson et al., 2000; Hardt et al., 2010). Thus, although the estimates provided in these data should be interpreted with caution, the associations reported here are unlikely to be artifacts of assessment timing. Additionally, neighborhood physical disorder is based on values for some Detroit block groups predicted using the values of the 138 block groups that we assessed. It is possible, though unlikely, that these values do not accurately describe the level of disorder in these block groups. However, there was strong evidence of spatial clustering of neighborhood physical disorder, which gives us confidence in our ability to using kriging techniques to predict block group values. The block groups randomly selected for evaluation were also chosen in such a way as to represent various different types of areas (based on population characteristics and density). Additionally, sensitivity analyses using only the observed neighborhood physical disorder values (rather than inclusion of predicted values) indicated that the magnitude and direction of interaction effects were similar. Further, neighborhood-level control variables were measured at the census tract level, which potentially comprises several block groups. Thus, we may have residual confounding if there is block-group heterogeneity of socio-economic indicators within the census tract group. However, all census tract indicators were strongly and significantly associated with block-level neighborhood disorganization, thus the impact of this potential residual confounding is likely minimal. Further, there is the possibility of neighborhood selection bias associated with childhood maltreatment, given that individuals with maltreatment histories may cluster within lower socio-economic neighborhoods. However, our analyses indicated that there was no correlation between maltreatment and neighborhood physical disorder in these data. Finally, we note that the participation rate at Wave 1 was 53%; thus, our findings are generalizable to populations who tend to respond to survey research of this kind. While we do not have information on whether participation was associated with the relevant study variables, this limitation should be kept in mind while interpreting the results.
Despite these limitations, the present study capitalized on the strengths of a longitudinally assessed community sample of individuals to document a negative synergistic effect of child maltreatment and neighborhood physical disorder in heightening risk for the onset of problematic patterns of alcohol consumption. Existing evidence increasingly suggests that neighborhood deprivation has deleterious effects on a wide range of poor health outcomes, including mental health problems such as depression (Latkin and Curry, 2003; Ross, 2000) and drug use disorders (Boardman et al., 2001) as well as physical health outcomes including heart disease (Diez-Roux et al., 1997, 2001; Sundquist et al., 2004) and obesity (Franzini et al., 2009). Future research should examine the potential sensitizing effect of childhood maltreatment and exposure to other adversities in the association of neighborhood characteristics with these outcomes in order to better understand the public health consequences of exposure to stress over the life-course.
Acknowledgements
We thank Rebecca M. Coulborn for overseeing DNHS specimen collection, Janie Slayden for coordinating the overall DNHS project, and Amy Weckle and Richelo Soliven for handling the DNHS specimen processing and laboratory technical assistance; the many Detroit residents who chose to participate in the DNHS; and Allison Aiello, Jorge Delva, Larry Gant, Bob Marans, and Trivellore Raghunathan for contributing to the conceptual development of the DNHS.
Role of Funding Source. This study was supported by National Institutes of Health Grants DA022720, DA022720-S1, MH088283, MH078152, as well as MH082729 (to S.G.), MH070627 and MH078928 (to K.C.K.), and MH092526 (to K.M.). NIDA and NIMH had no further role in the study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributors. Katherine Keyes conceived of the present analysis, lead the statistical analysis efforts, and wrote the initial drafts of the manuscript. Sandro Galea and Karestan Koenen designed the study, led data collection efforts, supervised the present analysis and provided critical revisions to the manuscript. Monica Uddin was involved with data collection and provided critical revisions to the manuscript. Emily Goldmann supervised field work during the data collection and was involved with data analysis and in providing critical revisions to the manuscript. Katie McLaughlin were involved with data analysis and provided critical revisions to the manuscript.
Conflict of Interest. None
Author Disclosures. None
References
- Ahern J, Galea S, Hubbard A, Midanik L, Syme SL. “Culture of drinking” and individual problems with alcohol use. Am. J. Epidemiol. 2008;167:1041–1049. doi: 10.1093/aje/kwn022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aneshensel CS, Sucoff CA. The neighborhood context of adolescent mental health. J. Health Soc. Behav. 1996;37:293–310. [PubMed] [Google Scholar]
- Bernstein DP, Ahluvalia T, Pogge D, Handelsman L. Validity of the Childhood Trauma Questionnaire in an adolescent psychiatric population. J. Am. Acad. Child Adolesc. Psychiatry. 1997;36:340–348. doi: 10.1097/00004583-199703000-00012. [DOI] [PubMed] [Google Scholar]
- Bernstein KT, Galea S, Ahern J, Tracy M, Vlahov D. The built environment and alcohol consumption in urban neighborhoods. Drug Alcohol Depend. 2007;91:244–252. doi: 10.1016/j.drugalcdep.2007.06.006. [DOI] [PubMed] [Google Scholar]
- Boardman JD, Finch BK, Ellison CG, Williams DR, Jackson JS. Neighborhood disadvantage, stress, and drug use among adults. J. Health Soc. Behav. 2001;42:151–165. [PubMed] [Google Scholar]
- Carpenter KM, Hasin DS. A prospective evaluation of the relationship between reasons for drinking and DSM-IV alcohol-use disorders. Addict. Behav. 1998;23:41–46. doi: 10.1016/s0306-4603(97)00015-4. [DOI] [PubMed] [Google Scholar]
- Caspi A, McClay J, Moffitt TE, Mill J, Martin J, Craig IW, Taylor A, Poulton R. Role of genotype in the cycle of violence in maltreated children. Science. 2002;297:851–854. doi: 10.1126/science.1072290. [DOI] [PubMed] [Google Scholar]
- Casswell S, Thamarangsi T. Reducing harm from alcohol: call to action. Lancet. 2009;373:2247–2257. doi: 10.1016/S0140-6736(09)60745-5. [DOI] [PubMed] [Google Scholar]
- Cerda M, Diez-Roux AV, Tchetgen ET, Gordon-Larsen P, Kiefe C. The relationship between neighborhood poverty and alcohol use: estimation by marginal structural models. Epidemiology. 2010;21:482–489. doi: 10.1097/EDE.0b013e3181e13539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cerda M, Tracy M, Messner SF, Vlahov D, Tardiff K, Galea S. Misdemeanor policing, physical disorder, and gun-related homicide: a spatial analytic test of “broken-windows” theory. Epidemiology. 2009;20:533–541. doi: 10.1097/EDE.0b013e3181a48a99. [DOI] [PubMed] [Google Scholar]
- Chaffin M, Kelleher K, Hollenberg J. Onset of physical abuse and neglect: psychiatric, substance abuse, and social risk factors from prospective community data. Child Abuse Negl. 1996;20:191–203. doi: 10.1016/s0145-2134(95)00144-1. [DOI] [PubMed] [Google Scholar]
- Cohen DA, Mason K, Bedimo A, Scribner R, Basolo V, Farley TA. Neighborhood physical conditions and health. Am. J. Public Health. 2003;93:467–471. doi: 10.2105/ajph.93.3.467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conron KJ, Beardslee W, Koenen KC, Buka SL, Gortmaker SL. A longitudinal study of maternal depression and child maltreatment in a national sample of families investigated by child protective services. Arch. Pediatr. Adolesc. Med. 2009;163:922–930. doi: 10.1001/archpediatrics.2009.176. [DOI] [PubMed] [Google Scholar]
- Cooper ML, Frone MR, Russell M, Mudar P. Drinking to regulate positive and negative emotions: a motivations model of alcohol use. J. Person. Soc. Psychol. 1995;69:990–1005. doi: 10.1037//0022-3514.69.5.990. [DOI] [PubMed] [Google Scholar]
- Cunradi CB. Neighborhoods, alcohol outlets and intimate partner violence: addressing research gaps in explanatory mechanisms. Int. J. Environ. Res. Public Health. 2010;7:799–813. doi: 10.3390/ijerph7030799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Desai A, Arias I, Thompson MP, Basile KC. Childhood victimization and subsequent revictimization assessed in a nationally representative sample of women and men. Violence Vict. 2002;17:639–653. doi: 10.1891/vivi.17.6.639.33725. [DOI] [PubMed] [Google Scholar]
- Diez-Roux AV, Nieto FJ, Muntaner C, Tyroler HA, Comstock GW, Shahar E, Cooper LS, Watson RL, Szklo M. Neighborhood environments and coronary heart disease: a multilevel analysis. Am. J. Epidemiol. 1997;146:48–63. doi: 10.1093/oxfordjournals.aje.a009191. [DOI] [PubMed] [Google Scholar]
- Diez Roux AV, Merkin SS, Arnett D, Chambless L, Massing M, Nieto FJ, Sorlie P, Szklo M, Tyroler HA, Watson RL. Neighborhood of residence and incidence of coronary heart disease. N. Engl. J. Med. 2001;345:99–106. doi: 10.1056/NEJM200107123450205. [DOI] [PubMed] [Google Scholar]
- Dinwiddie SH, Bucholz KK. Psychiatric diagnoses of self-reported child abusers. Child Abuse Negl. 1993;17:465–476. doi: 10.1016/0145-2134(93)90021-v. [DOI] [PubMed] [Google Scholar]
- Dong M, Anda RF, Felitti VJ, Dube SR, Williamson DF, Thompson TJ, Loo CM, Giles WH. The interrelatedness of multiple forms of childhood abuse, neglect, and household dysfunction. Child Abuse Negl. 2004;28:771–784. doi: 10.1016/j.chiabu.2004.01.008. [DOI] [PubMed] [Google Scholar]
- Dube SR, Anda RF, Felitti VJ, Edwards VJ, Williamson DF. Exposure to abuse, neglect, and household dysfunction among adults who witnessed intimate partner violence as children: implications for health and social services. Violence Vict. 2002;17:3–17. doi: 10.1891/vivi.17.1.3.33635. [DOI] [PubMed] [Google Scholar]
- Duncan SC, Duncan TE, Strycker LA. A multilevel analysis of neighborhood context and youth alcohol and drug problems. Prev. Sci. 2002;3:125–133. doi: 10.1023/a:1015483317310. [DOI] [PubMed] [Google Scholar]
- Ehrensaft MK, Cohen P, Brown J, Smailes E, Chen H, Johnson JG. Intergenerational transmission of partner violence: a 20-year prospective study. J. Consult. Clin. Psychol. 2003;71:741–753. doi: 10.1037/0022-006x.71.4.741. [DOI] [PubMed] [Google Scholar]
- Ennett ST, Flewelling RL, Lindrooth RC, Norton EC. School and neighborhood characteristics associated with school rates of alcohol, cigarette, and marijuana use. J. Health Soc. Behav. 1997;38:55–71. [PubMed] [Google Scholar]
- Enoch MA, Steer CD, Newman TK, Gibson N, Goldman D. Early life stress, MAOA, and gene-environment interactions predict behavioral disinhibition in children. Genes Brain Behav. 2010;9:65–74. doi: 10.1111/j.1601-183X.2009.00535.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Espejo EP, Hammen CL, Connolly NP, Brennan PA, Najman JM, Bor W. Stress sensitization and adolescent depressive severity as a function of childhood adversity: a link to anxiety disorders. J. Abnorm. Child Psychol. 2007;35:287–299. doi: 10.1007/s10802-006-9090-3. [DOI] [PubMed] [Google Scholar]
- Essex MJ, Klein MH, Cho E, Kalin NH. Maternal stress beginning in infancy may sensitize children to later stress exposure: effects on cortisol and behavior. Biol. Psychiatry. 2002;52:776–784. doi: 10.1016/s0006-3223(02)01553-6. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Horwood LJ, Woodward LJ. The stability of child abuse reports: a longitudinal study of the reporting behaviour of young adults. Psychol. Med. 2000;30:529–544. doi: 10.1017/s0033291799002111. [DOI] [PubMed] [Google Scholar]
- Foran HM, O’Leary KD. Alcohol and intimate partner violence: a meta-analytic review. Clin. Psychol. Rev. 2008;28:1222–1234. doi: 10.1016/j.cpr.2008.05.001. [DOI] [PubMed] [Google Scholar]
- Fox HC, Bergquist KL, Peihua G, Rajita S. Interactive effects of cumulative stress and impulsivity on alcohol consumption. Alcohol. Clin. Exp. Res. 2010;34:1376–85. doi: 10.1111/j.1530-0277.2010.01221.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franzini L, Elliott MN, Cuccaro P, Schuster M, Gilliland MJ, Grunbaum JA, Franklin F, Tortolero SR. Influences of physical and social neighborhood environments on children’s physical activity and obesity. Am. J. Public Health. 2009;99:271–278. doi: 10.2105/AJPH.2007.128702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freisthler B, Lascala EA, Gruenewald PJ, Treno AJ. An examination of drug activity: effects of neighborhood social organization on the development of drug distribution systems. Subst. Use Misuse. 2005;40:671–686. doi: 10.1081/ja-200055373. [DOI] [PubMed] [Google Scholar]
- Galea S, Ahern J, Tracy M, Rudenstine S, Vlahov D. Education inequality and use of cigarettes, alcohol, and marijuana. Drug Alcohol Depend. 2007;90(Suppl. 1):S4–15. doi: 10.1016/j.drugalcdep.2006.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galea S, Nandi A, Vlahov D. The social epidemiology of substance use. Epidemiol. Rev. 2004;26:36–52. doi: 10.1093/epirev/mxh007. [DOI] [PubMed] [Google Scholar]
- Gil-Gonzalez D, Vives-Cases C, Alvarez-Dardet C, Latour-Perez J. Alcohol and intimate partner violence: do we have enough information to act? Eur. J. Public Health. 2006;16:279–285. doi: 10.1093/eurpub/ckl016. [DOI] [PubMed] [Google Scholar]
- Glaser JP, van Os J, Portegijs PJ, Myin-Germeys I. Childhood trauma and emotional reactivity to daily life stress in adult frequent attenders of general practitioners. J. Psychosom. Res. 2006;61:229–236. doi: 10.1016/j.jpsychores.2006.04.014. [DOI] [PubMed] [Google Scholar]
- Gmel G, Rehm J, Room R. Contrasting individual level and aggregate level studies in alcohol research? Combining them is the answer! Addict. Res Theory. 2004;12:1–10. [Google Scholar]
- Goldman E, Aiello AE, Uddin M, Delva J, Koenen KC, Gant LM, Galea S. Pervasive exposure to violence and posttraumatic stress disorder in a predominantly African-American urban community: the Detroit Neighborhood Health Study. under review. [DOI] [PMC free article] [PubMed]
- Grant BF, Goldstein RB, Chou SP, Huang B, Stinson FS, Dawson DA, Saha TD, Smith SM, Pulay AJ, Pickering RP, Ruan WJ, Compton WM. Sociodemographic and psychopathologic predictors of first incidence of DSM-IV substance use, mood and anxiety disorders: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. Mol. Psychiatry. 2009;14:1051–1066. doi: 10.1038/mp.2008.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green JG, McLaughlin KA, Berglund PA, Gruber MJ, Sampson NA, Zaslavsky AM, Kessler RC. Childhood adversities and adult psychiatric disorders in the national comorbidity survey replication I: associations with first onset of DSM-IV disorders. Arch. Gen. Psychiatry. 2010;67:113–123. doi: 10.1001/archgenpsychiatry.2009.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gruenewald PJ, Johnson FW, Treno AJ. Outlets, drinking and driving: a multilevel analysis of availability. J. Stud. Alcohol. 2002a;63:460–468. doi: 10.15288/jsa.2002.63.460. [DOI] [PubMed] [Google Scholar]
- Ham LS, Hope DA. College students and problematic drinking: a review of the literature. Clin. Psychol. Rev. 2003;23:719–759. doi: 10.1016/s0272-7358(03)00071-0. [DOI] [PubMed] [Google Scholar]
- Hammen C, Henry R, Daley SE. Depression and sensitization to stressors among young women as a function of childhood adversity. J. Consult. Clin. Psychol. 2000a;68:782–787. [PubMed] [Google Scholar]
- Hardt J, Rutter M. Validity of adult retrospective reports of adverse childhood experiences: review of the evidence. J. Child Psychol. Psychiatry. 2004;45:260–273. doi: 10.1111/j.1469-7610.2004.00218.x. [DOI] [PubMed] [Google Scholar]
- Hardt J, Vellaisamy P, Schoon I. Sequelae of prospective versus retrospective reports of adverse childhood experiences. Psychol. Rep. 2010;107:425–440. doi: 10.2466/02.04.09.10.16.21.PR0.107.5.425-440. [DOI] [PubMed] [Google Scholar]
- Hasin DS, Stinson FS, Ogburn E, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch. Gen. Psychiatry. 2007;64:830–842. doi: 10.1001/archpsyc.64.7.830. [DOI] [PubMed] [Google Scholar]
- Heim C, Nemeroff CB. The role of childhood trauma in the neurobiology of mood and anxiety disorders: preclinical and clinical studies. Biol. Psychiatry. 2001;49:1023–1039. doi: 10.1016/s0006-3223(01)01157-x. [DOI] [PubMed] [Google Scholar]
- Hill TD, Angel RJ. Neighborhood disorder, psychological distress, and heavy drinking. Soc. Sci. Med. 2005;61:965–975. doi: 10.1016/j.socscimed.2004.12.027. [DOI] [PubMed] [Google Scholar]
- Hingson R, Heeren T, Zakocs RC, Kopstein A, Wechsler H. Magnitude of alcohol-related mortality and morbidity among U.S. college students ages 18-24. J. Stud. Alcohol. 2002;63:136–144. doi: 10.15288/jsa.2002.63.136. [DOI] [PubMed] [Google Scholar]
- Holman CDJ, English DR, Milne E, Winter MG. Meta-analysis of alcohol and all-cause mortality: a validation of NHMRC recommendations. Med. J. Australia. 1996;164:141–145. doi: 10.5694/j.1326-5377.1996.tb122011.x. [DOI] [PubMed] [Google Scholar]
- Hussey JM, Chang JJ, Kotch JB. Child maltreatment in the United States: prevalence, risk factors, and adolescent health consequences. Pediatrics. 2006;118:933–942. doi: 10.1542/peds.2005-2452. [DOI] [PubMed] [Google Scholar]
- Iacono WG, Carlson SR, Taylor J, Elkins IJ, McGue M. Behavioral disinhibition and the development of substance-use disorders: findings from the Minnesota Twin Family Study. Dev. Psychopathol. 1999;11:869–900. doi: 10.1017/s0954579499002369. [DOI] [PubMed] [Google Scholar]
- Jarl J, Johansson P, Eriksson A, Eriksson M, Gerdtham UG, Hemstrom O, Selin KH, Lenke L, Ramstedt M, Room R. The societal cost of alcohol consumption: an estimation of the economic and human cost including health effects in Sweden, 2002. Eur. J. Health Econ. 2008;9:351–360. doi: 10.1007/s10198-007-0082-1. [DOI] [PubMed] [Google Scholar]
- Jessor R, Jessor SL. Problem behaviour and psychosocial development: a longitudinal study of youth. Academic Press; New York: 1977. [Google Scholar]
- Jones-Webb R, Snowden L, Herd D, Short B, Hannan P. Alcohol-related problems among black, Hispanic and white men: the contribution of neighborhood poverty. J. Stud. Alcohol. 1997;58:539–545. doi: 10.15288/jsa.1997.58.539. [DOI] [PubMed] [Google Scholar]
- Kaufman J, Yang BZ, Douglas-Palumberi H, Crouse-Artus M, Lipschitz D, Krystal JH, Gelernter J. Genetic and environmental predictors of early alcohol use. Biol. Psychiatry. 2007;61:1228–1234. doi: 10.1016/j.biopsych.2006.06.039. [DOI] [PubMed] [Google Scholar]
- Kelleher K, Chaffin M, Hollenberg J, Fischer E. Alcohol and drug disorders among physically abusive and neglectful parents in a community-based sample. Am. J. Public Health. 1994;84:1586–1590. doi: 10.2105/ajph.84.10.1586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Kuhn JW, Prescott CA. Childhood sexual abuse, stressful life events and risk for major depression in women. Psychol. Med. 2004;34:1475–1482. doi: 10.1017/s003329170400265x. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Davis CG, Kendler KS. Childhood adversity and adult psychiatric disorder in the US National Comorbidity Survey. Psychol. Med. 1997;27:1101–1119. doi: 10.1017/s0033291797005588. [DOI] [PubMed] [Google Scholar]
- Keyes KM, Barnes DM, Bates LM. Stress, coping, and depression: testing a new hypothesis in a prospectively studied general population sample of U.S.-born Whites and Blacks. Soc. Sci. Med. 2011a;72:650–659. doi: 10.1016/j.socscimed.2010.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes KM, Hatzenbuehler ML, Hasin DS. Stressful life experiences, alcohol consumption, and alcohol use disorders: the epidemiologic evidence for four main types of stressors. Psychopharmacology (Berl.) 2011b doi: 10.1007/s00213-011-2236-1. ePub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim-Cohen J, Caspi A, Taylor A, Williams B, Newcombe R, Craig IW, Moffitt TE. MAOA, maltreatment, and gene-environment interaction predicting children’s mental health: new evidence and a meta-analysis. Mol. Psychiatry. 2006;11:903–913. doi: 10.1038/sj.mp.4001851. [DOI] [PubMed] [Google Scholar]
- Koenen KC, Aiello AE, Bakshis E, Amstadter AB, Ruggiero KJ, Acierno R, Kilpatrick DG, Gelernter J, Galea S. Modification of the association between serotonin transporter genotype and risk of posttraumatic stress disorder in adults by county-level social environment. Am. J. Epidemiology. 2009;169:704–711. doi: 10.1093/aje/kwn397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koenen KC, Uddin M, Aiello AE, Wildman D, Goldmann E, Galea S. Methylation of SLC6A4 modifies the effect of cumulative traumatic burden on risk for posttraumatic stress disorder. Depress. Anxiety. 2011 doi: 10.1002/da.20825. ePub May 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koizumi N, Rothbard AB, Kuno E. Distance matters in choice of mental health program: policy implications for reducing racial disparities in public mental health care. Admin. Policy Ment. Health a Ment. Health Services Res. 2009;36:424–431. doi: 10.1007/s10488-009-0233-z. [DOI] [PubMed] [Google Scholar]
- Kozaric-Kovacic D, Ljubin T, Grappe M. Comorbidity of posttraumatic stress disorder and alcohol dependence in displaced persons. Croat. Med. J. 2000;41:173–178. [PubMed] [Google Scholar]
- Kruger DJ, Reischl TM, Gee GC. Neighborhood social conditions mediate the association between physical deterioration and mental health. Am. J. Community Psychol. 2007;40:261–271. doi: 10.1007/s10464-007-9139-7. [DOI] [PubMed] [Google Scholar]
- Kumar A, Maroju S, Abhishek B. Application of ArcGIS geostatistical analyst for interpolating environmental data from observations. Environ. Progress. 2007;26:220–225. [Google Scholar]
- Latkin CA, Curry AD. Stressful neighborhoods and depression: a prospective study of the impact of neighborhood disorder. J. Health Soc. Behav. 2003;44:34–44. [PubMed] [Google Scholar]
- Leventhal T, Brooks-Gunn J. The neighborhoods they live in: the effects of neighborhood residence on child and adolescent outcomes. Psychol. Bull. 2000;126:309–337. doi: 10.1037/0033-2909.126.2.309. [DOI] [PubMed] [Google Scholar]
- Lloyd DA, Turner RJ. Cumulative lifetime adversities and alcohol dependence in adolescence and young adulthood. Drug Alcohol Depend. 2008;93:217–26. doi: 10.1016/j.drugalcdep.2007.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loman MM, Gunnar MR. Early experience and the development of stress reactivity and regulation in children. Neurosci. Biobehav. Rev. 2010;34:867–876. doi: 10.1016/j.neubiorev.2009.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Longnecker MP. Alcoholic beverage consumption in relation to risk of breast cancer: meta-analysis and review. Cancer Causes Control. 1994;5:73–82. doi: 10.1007/BF01830729. [DOI] [PubMed] [Google Scholar]
- Lyons MJ, Goldberg J, Eisen SA, True W, Tsuang MT, Meyer JM, Henderson WG. Do genes influence exposure to trauma? A twin study of combat. Am. J. Med. Genet. 1993;48:22–27. doi: 10.1002/ajmg.1320480107. [DOI] [PubMed] [Google Scholar]
- May PA, Gossage JP. Estimating the prevalence of fetal alcohol syndrome: a summary. Alcohol Res. Health. 2001;25:159–67. [PMC free article] [PubMed] [Google Scholar]
- MacMillan HL, Fleming JE, Streiner DL, Lin E, Boyle MH, Jamieson E, Duku EK, Walsh CA, Wong MY, Beardslee WR. Childhood abuse and lifetime psychopathology in a community sample. Am. J. Psychiatry. 2001;158:1878–1883. doi: 10.1176/appi.ajp.158.11.1878. [DOI] [PubMed] [Google Scholar]
- McKinney CM, Caetano R, Ramisetty-Mikler S, Nelson S. Childhood family violence and perpetration and victimization of intimate partner violence: findings from a national population-based study of couples. Ann. Epidemiol. 2009;19:25–32. doi: 10.1016/j.annepidem.2008.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, Conron KJ, Koenen KC, Gilman SE. Childhood adversity, adult stressful life events, and risk of past-year psychiatric disorder: a test of the stress sensitization hypothesis in a population-based sample of adults. Psychol. Med. 2010a;40:1647–1658. doi: 10.1017/S0033291709992121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, Hatzenbuehler ML. Mechanisms linking stressful life events and mental health problems in a prospective, community-based sample of adolescents. J. Adolesc. Health. 2009;44:153–160. doi: 10.1016/j.jadohealth.2008.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, Hatzenbuehler ML, Hilt LM. Emotion dysregulation as a mechanism linking peer victimization to internalizing symptoms in adolescents. J. Consult. Clin. Psychol. 2009;77:894–904. doi: 10.1037/a0015760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, Kubzansky LD, Dunn EC, Waldinger R, Vaillant G, Koenen KC. Childhood social environment, emotional reactivity to stress, and mood and anxiety disorders across the life course. Depress. Anxiety. 2010b;27:1087–1094. doi: 10.1002/da.20762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States, 2000. JAMA. 2004;291:1238–1245. doi: 10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- Molnar BE, Buka SL, Kessler RC. Child sexual abuse and subsequent psychopathology: results from the National Comorbidity Survey. Am. J. Public Health. 2001;91:753–760. doi: 10.2105/ajph.91.5.753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naimi TS, Brewer RD, Mokdad A, Denny C, Serdula MK, Marks JS. Binge drinking among US adults. JAMA. 2003b;289:70–75. doi: 10.1001/jama.289.1.70. [DOI] [PubMed] [Google Scholar]
- Naimi TS, Lipscomb LE, Brewer RD, Gilbert BC. Binge drinking in the preconception period and the risk of unintended pregnancy: implications for women and their children. Pediatrics. 2003a;111:1136–1141. [PubMed] [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism Helping Patients Who Drink Too Much: A Clinican’s Guide. 2005 NIH Publication No 07-3769, accessed on:, available at: http://pubsniaaanihgov/publications/practitioner/cliniciansguide2005/guidepdf.
- National Institute on Drug Abuse . Epidemiologic Trends in Drug Abuse. Vol. 1: Proceedings of the Community Epidemiology Work Group. Highlights and Executive Summary. U.S. Department of Health and Human Services; Washington, DC: 2005. NIH Publication No. 07-5879A. [Google Scholar]
- Ompad DC, Galea S, Marshall G, Fuller CM, Weiss L, Beard JR, Chan C, Edwards V, Vlahov D. Sampling and recruitment in multilevel studies among marginalized urban populations: the IMPACT studies. J. Urban Health. 2008;85:268–280. doi: 10.1007/s11524-008-9256-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oosterman M, De Schipper JC, Fisher P, Dozier M, Schuengel C. Autonomic reactivity in relation to attachment and early adversity among foster children. Dev. Psychopathol. 2010;22:109–118. doi: 10.1017/S0954579409990290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pensola TH, Martikainen P. Cumulative social class and mortality from various causes of adult men. J. Epidemiol. Community Health. 2003;57:745–751. doi: 10.1136/jech.57.9.745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pensola TH, Valkonen T. Mortality differences by parental social class from childhood to adulthood. J. Epidemiol. Community Health. 2000;54:525–9. doi: 10.1136/jech.54.7.525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollack CE, Cubbin C, Ahn D, Winkleby M. Neighbourhood deprivation and alcohol consumption: does the availability of alcohol play a role? Int. J. Epidemiol. 2005;34:772–780. doi: 10.1093/ije/dyi026. [DOI] [PubMed] [Google Scholar]
- Rankin BH, Quane JM. Social contexts and urban adolescent outcomes: the interrelated effects of neighborhoods, families, and peers on African-American youth. Soc. Probl. 2002;49:79–100. [Google Scholar]
- Rehm J, Mathers C, Popova S, Thavorncharoensap M, Teerawattananon Y, Patra J. Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. Lancet. 2009;373:2223–2233. doi: 10.1016/S0140-6736(09)60746-7. [DOI] [PubMed] [Google Scholar]
- Research Triangle Institute SAS-Callable SUDAAN software. (version 10.0.1) 2009 accessed on: http://www.rti.org/sudaan/
- Rice N, Carr-Hill R, Dixon P, Sutton M. The influence of households on drinking behaviour: a multilevel analysis. Soc. Sci. Med. 1998;46:971–979. doi: 10.1016/s0277-9536(97)10017-x. [DOI] [PubMed] [Google Scholar]
- Roberts AL, McLaughlin KA, Conron KJ, Koenen KC. Adult stressors, history of childhood adversity, and risk of perpetration of intimate partner violence among men and women. Am. J. Prev. Med. 2011;40:128–138. doi: 10.1016/j.amepre.2010.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross CE. Neighborhood disadvantage and adult depression. J. Health Soc. Behav. 2000;41:177–187. [Google Scholar]
- Scribner RA, MacKinnon DP, Dwyer JH. Alcohol outlet density and motor vehicle crashes in Los Angeles County cities. J. Stud. Alcohol. 1994;55:447–453. doi: 10.15288/jsa.1994.55.447. [DOI] [PubMed] [Google Scholar]
- Straus MA. Measuring intrafamily conflict and violence: the Conflict Tactics (CT) Scales. J. Marriage Fam. 1979;41:75–88. [Google Scholar]
- Sundquist K, Winkleby M, Ahlen H, Johansson SE. Neighborhood socioeconomic environment and incidence of coronary heart disease: a follow-up study of 25,319 women and men in Sweden. Am. J. Epidemiol. 2004;159:655–662. doi: 10.1093/aje/kwh096. [DOI] [PubMed] [Google Scholar]
- Thompson MP, Kingree JB. The roles of victim and perpetrator alcohol use in intimate partner violence outcomes. J. Interpers. Violence. 2006;21:163–177. doi: 10.1177/0886260505282283. [DOI] [PubMed] [Google Scholar]
- Turner HA, Finkelhor D, Ormrod R. The effect of lifetime victimization on the mental health of children and adolescents. Soc. Sci. Med. 2006;62:13–27. doi: 10.1016/j.socscimed.2005.05.030. [DOI] [PubMed] [Google Scholar]
- Uddin M, Koenen KC, Aiello AE, Wildman DE, de Los Santos R, Galea S. Epigenetic and inflammatory marker profiles associated with depression in a community-based epidemiologic sample. Psychol. Med. 2010:1–11. doi: 10.1017/S0033291710001674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- US Bureau of the Census American Factfinder. 2000. Census 2000. Summary File 1.
- Wichers M, Geschwind N, Jacobs N, Kenis G, Peeters F, Derom C, Thiery E, Delespaul P, van Os J. Transition from stress sensitivity to a depressive state: Longitudinal Twin Study. Br. J .Psychiatry. 2009;195:498–503. doi: 10.1192/bjp.bp.108.056853. [DOI] [PubMed] [Google Scholar]
- Widom CS. Accuracy of adult recollection of chilhood victimization: part I. childhood physical abuse. Psychol. Assess. 1996;8:412–421. [Google Scholar]
- Widom CS. Accuracy of adult recollection of childhood victimization: part 2. childhood sexual abuse. Psychol. Assess. 1997;9:34–46. [Google Scholar]
- Widom CS, Brzustowicz LM. MAOA and the “cycle of violence:” childhood abuse and neglect, MAOA genotype, and risk for violent and antisocial behavior. Biol. Psychiatry. 2006;60:684–689. doi: 10.1016/j.biopsych.2006.03.039. [DOI] [PubMed] [Google Scholar]
- Widom CS, Ireland T, Glynn PJ. Alcohol abuse in abused and neglected children followed-up: are they at increased risk? J. Stud. Alcohol. 1995;56:207–217. doi: 10.15288/jsa.1995.56.207. [DOI] [PubMed] [Google Scholar]
- Widom CS, Marmorstein NR, White HR. Childhood victimization and illicit drug use in middle adulthood. Psychol. Addict. Behav. 2006;20:394–403. doi: 10.1037/0893-164X.20.4.394. [DOI] [PubMed] [Google Scholar]
- Widom CS, White HR, Czaja SJ, Marmorstein NR. Long-term effects of child abuse and neglect on alcohol use and excessive drinking in middle adulthood. J. Stud. Alcohol Drugs. 2007;68:317–326. doi: 10.15288/jsad.2007.68.317. [DOI] [PubMed] [Google Scholar]
- Winstanley EL, Steinwachs DM, Ensminger ME, Latkin CA, Stitzer ML, Olsen Y. The association of self-reported neighborhood disorganization and social capital with adolescent alcohol and drug use, dependence, and access to treatment. Drug Alcohol Depend. 2008;92:173–182. doi: 10.1016/j.drugalcdep.2007.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]