Abstract
Acute and chronic environmental and psychosocial stress contributes to the pathogenesis and progression of cardiovascular diseases (CVD). Stress reduction via Transcendental Meditation (TM)® has been shown to lower blood pressure (BP) levels and reduce CVD risk in adults and adolescents. This article reviews recent findings indicating a beneficial BP-lowering impact of TM in hypertensive adults at rest and in pre-hypertensive adolescents at rest, during acute laboratory stress and during normal daily activity. These findings have important implications for inclusion of TM in efforts to prevent and treat cardiovascular diseases and its clinical consequences.
INTRODUCTION
Cardiovascular disease (CVD) afflicts over 70 million Americans. It is the leading cause of death in the US, killing 927,444 Americans in 2002 and costing an estimated $393 billion in 2005 [1]. Like most other diseases, CVD is multi-factorial in nature. Well-established preventable CVD risk factors include elevated serum cholesterol levels [2], high blood pressure (BP) [3], smoking [4], psychological distress/angry temperament [5], metabolic syndrome [6], obesity [7], stress [8] and physical inactivity [9]. Exposure to CVD risk factors during childhood and adolescence has been associated with the development of atherosclerosis later in life [10,11]. These risk factors, all modifiable, can be greatly benefitted by changes in lifestyle [12].
Environmental and psychosocial stress has been thought to play a significant role in the development of essential hypertension (EH) by acting through both acute and long-term BP control mechanisms [13,14]. Stress is defined as a process in which environmental demands tax or exceed the adaptive capacity of an organism, resulting in physiological changes that, over time, may place the individual at risk for disease development [15]. The biobehavioral model of stress-induced hypertension depicted in Fig. 1 incorporates both the acute phase of the stress response, which results in a rapid BP increase, and the chronic phase of the stress response which acts to maintain elevated BP levels as long as physiologically needed to maintain homeostasis. Chronic sympathetic nervous system (SNS) activation has been linked to EH [16]. Stress has been hypothesized as contributing to the development of EH and CVD via a pathway of exaggerated cardiovascular reactivity [13,14,17]. The acute phase of the stress response involves complex neuroendocrine changes characterized by increased sympathetic activation [18]. Animal and human studies have demonstrated that exposure to chronic and acute stress may augment SNS activity resulting in increased levels of catecholamines including norepinephrine (NE) [19]. This results in a rapid rise in BP predominantly due to increased vasoconstriction [20], which increases total peripheral resistance (TPR) [21].
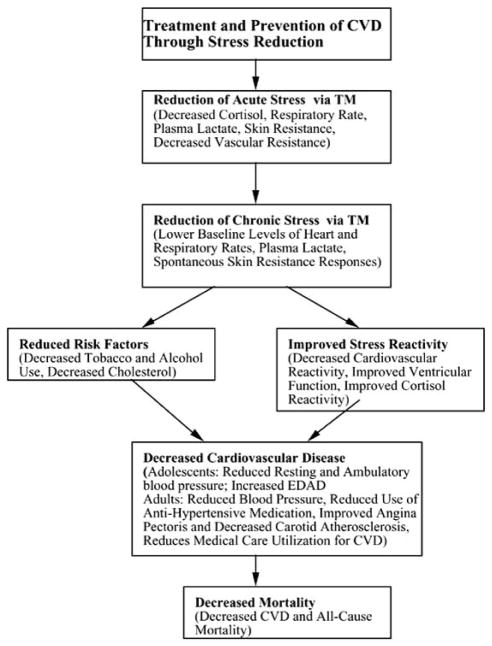
Fig. (1).
A model of the TM’s effects on hypertension and CVD as reviewed in this paper is presented. Chronic environmental and psychosocial stress, and genetic predisposition, contribute to an increase in acute stress-induced SNS arousal resulting in increased neurohormonal activity and hypothalamic pituitary adrenocortical (HPA) axis dysregulation. Such changes result in greater BP responsivity to the stress, vasoconstriction and increased BP levels. Reduction of acute and chronic stress via TM reduces CVD risk factors and impacts on the SNS resulting in reduced BP reactivity to acute stress. Over time, due to decreased cardiovascular reactivity to acute events, there is reduced load upon the heart resulting in decreased BP levels, thereby helping to prevent early onset of EH [13].
TREATMENT AND PREVENTION OF CVD THROUGH STRESS REDUCTION
Exposure to stress results in SNS-mediated increases in BP to cope with the immediate need for an increased blood supply to the brain and body. It is well established that the SNS activation in turn activates the renin-angiotensin-aldosterone system (RAAS), which includes release of the potent vasoconstrictive hormone, angiotensin II, which contributes to the acute rise in BP [19]. This response pattern is associated with concomitant increases in cardiac and vascular wall tension and intravascular shear stress that over time contribute to early vascular and ventricular remodeling which eventually lead to EH [13,14].
The recurrent and/or sustained exaggerated increases in BP responses to stress are associated with concomitant increases in cardiac and vascular wall tension [22,23]. It is hypothesized that over time this leads to secondary CV structural adaptation, that is, vascular and ventricular remodeling to help normalize wall tension [18,22,24]. An early sign of ventricular remodeling is increased left ventricular mass (LVM) which over time may lead to left ventricular hypertrophy (LVH), the strongest predictor of CV morbidity and mortality, other than advancing age [25–27]. Research findings have shown that BP reactivity in youth predicts LVH [28,29]. Importantly, changes in ventricular functioning that may occur concomitant with or prior to ventricular remodeling include increased resting heart rate (HR).
An individual’s acute cardiovascular responses to stress are moderated by numerous psychological/lifestyle factors. For example, anger and hostility have been shown to be related to CV reactivity and a wide range of physical health problems including EH and CVD [30–35]. Similarly, coping styles (i.e., anger suppression, anger expression), perceived environmental stress (i.e., general stress levels, stressful life events, unfair treatment), and coping resources (e.g., family functioning, social support, stress reduction skills) are implicated in pathway. These variables have been associated with resting BP and/or CV reactivity in adolescents and/or young adults [36–40].
Although not entirely consistent [41], several prospective studies observed that BP reactivity predicts hypertension [42–45]. Exaggerated CV reactivity to stress has been hypothesized [13,14,17] as playing a particularly significant role in the development of EH due to exposure to both chronic and acute psychosocial and environmental stress (e.g., verbal/physical conflict with law/authority figures or family members, racism, inadequate economic resources, social disorganization, lower education and occupational status) [46–48]. Over the past decade pediatric studies found exaggerated BP reactivity to laboratory behavioral stressors is an independent predictor of increases in measures of pre-clinical CVD [49]. Increased peripheral vasoconstriction (i.e., TPR) has been implicated as playing an important role in the early development of EH [50]. Importantly, enhanced TPR is frequently the underlying hemodynamic mechanism responsible [51–53].
A functional measure of vascular remodeling is called diminished endothelium-dependent arterial dilation (EDAD) to reactive hyperemia [54]. Diminished EDAD is an index of endothelial dysfunction, a relatively early event in the pathogenesis of CVD [55]. In youth and adults, decreased EDAD of femoral or brachial arteries to reactive hyperemia has been associated with elevated resting BP, smoking, hypercholesterolemia, CVD and EH [54–56]. Exaggerated SBP and/or TPR reactivity to acute stress has been found to be associated with diminished EDAD in normotensive youth and adults [57–59]. Collectively, these morphological and functional alterations in vascular and ventricular function lead to elevations in resting TPR and BP, which further lead to increases in left ventricular mass index and BP reactivity. A self-perpetuating cycle ensues which contributes to the pathogenesis of EH [21].
Evidence for the efficacy of certain nonpharmacologic approaches to preventing and controlling EH is strong [60]. Clinical research, primarily in adults, has shown behavioral interventions to have great promise in reducing BP levels, improving stress-related coping skills, and alleviating psychosocial distress. The benefits of psychosocial-behavioral interventions with respect to hypertension and CHD have been demonstrated in a number of trials in adults [61,62]. Stress reduction programs include those involving meditation, cognitive behavioral skills training, yoga and muscle relaxation. This review is limited to examining applications of the Transcendental Meditation (TM) program in prevention and treatment of EH and CVD.
There are several significant and unique aspects of the findings contained in this review. First and foremost is the wide range of subject populations, i.e., older and younger Caucasian Americans (CAs) and African Americans (AAs). The research endeavor with TM is among the few to extend behavioral stress reduction research to the adolescent population. Studies in youth are important for at least three reasons. (1) Such studies examine the effectiveness of a non-pharmacological therapy on BP reduction prior to the potentially confounding influences of sustained elevated BP that adversely affects the functioning of the organ systems later on in life [63]. (2) Epidemiological studies indicate that BP percentile rankings for age and sex tend to track from late childhood through adolescence into adulthood [64–66]. As such it is important to study individuals at a time when preventive strategies may still be effective prior to development of pathology. (3) Until now, the prevention of EH and CVD has not been a high priority in pediatric patients. As a result, little is known about the factors underlying pediatric EH. Therefore, given that the incidence of EH is increasing at an alarming rate, the prevention of EH and its consequences in the pediatric population has become an important area of investigation. Prevention of EH prior to the onset of target organ damage has been shown to be highly cost-effective [67].
The importance of the findings of this review lie in the concept that wide implementation of a non-pharmacological BP-reducing intervention could potentially have an enormous impact on public health. Even a small downward shift in the distribution of BP in the youth of a few mm Hg could substantially reduce the incidence of EH and related CVD [68]. Such decreases in youth and adolescents with elevated BP, if maintained over time, may potentially decrease long-term risk for hypertension [69]. The results of this review will provide insight into what has now become a very timely and important issue.
THE TRANSCENDENTAL MEDITATION TECHNIQUE (TM)
Chronic environmental stress is not easily altered. However, our model proposes that the effects of stress can be ameliorated via behavioral stress reduction, i.e., changing how the individual responds to stressors to reduce their negative impact on health. One approach which has been found to be particularly fruitful includes the Transcendental Meditation (TM) program.
The TM program requires no change in personal belief, religious or philosophical orientations and is easily learned by adults and adolescents [70]. TM is a simple mental technique that is learned over a standard seven-step course and practiced twenty minutes twice a day. Over 600 studies from over 210 universities and research institutions in 33 countries evaluating its effects have been published since 1970 [71–73]. Research evidence reviewed below indicates that it benefits many of the risk factors that contribute to CVD.
PART 1: PREVENTION: BLOOD PRESSURE REDUCTION STUDIES IN YOUTH
Hypertension is no longer considered an adult disease [69]. Blood pressure (BP) levels ‘track’ relative to peers from late childhood onward [74]. These levels may predict hypertension in young adulthood [74,75]. Children in the highest BP quintile are at greater risk to develop EH in early adulthood [74,76]. The incidence of hypertension has risen dramatically in recent years among youth [69], increasing as much as sevenfold among minority populations including African Americans (AAs) in which rates are now estimated at 5–12% [77]. These rates in adolescents are expected to increase together with increases in obesity [78].
CVD ranks as the number two cause of death in children under 15 [1]. In 1997, the National Institutes of Health announced an initiative for pediatric intervention studies for primary prevention of cardiovascular disease (CVD), which may benefit overall health and well-being, and reduce healthcare costs over the life span [79]. However, non-pharmacological interventions (e.g., electrolyte supplementation, diet, physical activity) have met with mixed results, with studies finding minimal to no effect upon BP in nor-motensive youth [75,80]. Sixth Joint National committee Report (JNC-6) failed to support the use of relaxation therapies for the treatment or prevention of hypertension [81], although a TM study was cited as having lowered BP at 3 months [82]. Furthermore, JNC-7 made no mention of relaxation therapies or meditation as a lifestyle modification option to manage hypertension, but rather emphasized weight and sodium reduction, adopting the ‘DASH’ diet, increasing physical activity and moderating alcohol [83]. The omission of relaxation/meditation options for lowering blood pressure in JNC-7 provides impetus for the present review, particularly since JNC-6 cited a TM study. Those with normal (pre-hypertensive) and optimal BP are encouraged to make lifestyle modifications to further reduce their risk of developing CVD [83]. In view of the recommendation of JNC-7 that health-promoting lifestyle modifications be implemented well before BP reaches the “hypertension” range, this review examining effectiveness of a lifestyle technique on BP lowering is highly relevant [83].
IMPACT OF TM ON RESTING BP AND BP REACTIVITY IN HIGH SCHOOL STUDENTS
Studies examining the impact of TM on BP in youth have been conducted by the Georgia Prevention Institute of the Medical College of Georgia. An 8-week pilot study examined resting BP and BP reactivity in adolescents with high normal BP [84]. Thirty-five adolescents (ages 15–18 years) with resting systolic blood pressure between the 85th to 95th percentile for their age, height and gender on 3 consecutive occasions, were randomly assigned to either TM (n=17) or health education control (CTL, n=18) groups. The groups did not differ on anthropomorphic, demographic, or pretest hemodynamic variables. The CTL group received lifestyle education sessions based on NIH guidelines on lowering BP through weight loss, diet and increasing physical activity. The TM group engaged in 15-min meditation sessions twice each day for 2 months including sessions during the school lunch break. Subjects’ cardiovascular function (BP, heart rate, and cardiac output) were measured at minutes 10, 12 and 14 of supine rest and in reaction to a behavioral stressor (simulated car driving) and a social stressor (interview about a stressful event) every minute during the 10-minute stressor period. Assessors were blinded with respect to treatment status. After a two-month TM intervention, subjects were retested on the same protocol. The TM group exhibited a 4.8 mm Hg decrease in resting systolic BP (SBP) (p=.03) from pre- to 2 month post-intervention, compared to an increase of 2.6 mm Hg in the CTL group. The TM group also exhibited greater decreases from pre- to post-intervention SBP, heart rate and cardiac output reactivity (p’s<.03) to the car driving stressor, and in SBP reactivity (p=.03) to the social stressor interview compared to the CTL group. These findings are important in consideration of TM’s effects on hypertension because exaggerated cardiovascular reactivity to chronic stress may detrimentally impact on cardiovascular structure and function, contributing to hypertension and coronary heart disease [23,85].
AMBULATORY BP MONITORING
Ambulatory BP monitoring (ABPM) has been shown to improve prediction of hypertensive complications, be relatively free of placebo effects, highly reproducible and sensitive to small changes in average BP [86]. Multiple readings obtained over 24 hours yield a more reliable measure of overall daytime BP while white coat effects are eliminated [87]. This methodology facilitates observing real-life (at school and at home) BP, assessing the generalization of treatment effects in out-of-laboratory situations [88]. Reproducibility of ambulatory results have been validated in youth [89,90]. Findings in youth have indicated that ambulatory SBP measures are stable across periods of time varying from 1 to 4 years [91]. As compared to measures observed in a controlled laboratory environment, ambulatory BP measures cannot be influenced by laboratory evaluation personnel. Ambulatory BP monitoring has been recommended by JNC --6 and WHO for high reliability due to the 24-hour time series of BP measurements in the natural environment [92]. This approach is free from assessor blinding issues as the monitors can be programmed to measure BP automatically for many measurements during 24 hours. Blinding status becomes a non-issue since edits and calculations are performed automatically by the monitor software and the ABP monitor’s computational programs are run without knowledge of group identification. The results are downloaded directly to computer storage from where daytime and nighttime means are used in the analyses [93]. This approach overcomes problems arising in studies that measure BP a few times in the physician’s office on one day.
IMPACT OF TM ON AMBULATORY BP IN YOUTH
A 16-week random assignment intervention study was conducted with 156 AAs (mean age=16.2 yrs) with high normal SBP (pre-hypertensive, 85th to 95th percentile for their age group i.e., 129.2/75.3 mm Hg) [93]. Subjects were identified via BP screening conducted in the schools and were assigned to TM or CTL following pre-testing. On school days the TM group meditated for 15 minutes each day at school under the daily supervision of a certified TM instructor. On weekends and after school subjects practiced unsupervised at home. Average self reported compliance with TM at home was 75.9%. The CTL group participated in 15-minute cardiovascular health education sessions daily on school days. Ambulatory 24-hr BP measures were recorded at pretest, 2- and 4-month posttests, and 4-month follow-up. The study found decreased daytime SBP (p=.04) and diastolic BP (DBP) (p=.06) in the TM group compared to controls by approximately 4 mm Hg over the four-month intervention period, with a similar SBP decrease maintained at 4 months follow-up [93].
Potential cross-contamination might have existed between the groups if the control and TM subjects were in the same school at the same time. However, interventions (TM and control) were provided separately to all schools over the study period to counterbalance the effect of school environment over the entire study.
IMPACT OF TM ON VASCULAR FUNCTION IN YOUTH
Diminished endothelium-dependent vasodilation to reactive hyperemia (EDAD) is an index of endothelial dysfunction. In youth and adults, decreased EDAD of femoral or brachial arteries to reactive hyperemia has been associated with risk factors for EH and CVD. The above BP study also determined the impact of TM on EDAD in adolescents with high normal blood pressure. 108 AA adolescents (age 16.2± 1.3 years) with high normal systolic blood pressure, were randomly assigned to either 4-month TM or health education control groups. Echocardiographically-derived measures of subjects’ EDAD data were collected at pre-, post-4-month intervention and at 4-month follow up. The subject’s right brachial artery was scanned in longitudinal section using a Hewlett-Packard 5500 with a 7.5 MHz ultrasound vascular transducer for 2 minutes following 4 minutes of arterial occlusion, induced by inflating a BP cuff to 200 mmHg. EDAD was calculated as the percent change from the baseline diameter to the maximum post cuff release diameter. The findings indicated that the TM group exhibited a significant increase in percent change in EDAD adjusted for pre-occlusion arterial diameter compared to the CTL group from pre-intervention to 4 month follow-up (+2.56% vs. −0.53%, p< .05). Significant improvement in EDAD suggests improved vascular function in the TM group compared to CTL in AA adolescents at risk. This finding was viewed as having the highest potential to change clinical practice from the perspective of treatment [94].
The TM program has a side-benefit that through daily practice, skill in managing CVD risk factors eventually leads to reduction in hypertension and CVD. By enhancing skill in stress reduction, one would be less likely to develop hypertension and subsequent health impairments later in life. Substantial benefits could be gained from an empirically validated program that would improve stress reduction skills. Few empirically validated BP-lowering programs are currently available for delivery to the public on a wide basis. Training of TM in childhood, if practice is continued over the long term, may have a beneficial impact upon hypertension risk and related health problems. Thus, the consequences and related economic costs of hypertension may be beneficially impacted if a cardio-protective technique such as TM is made available for youth and becomes a health promoting lifestyle behavior continued throughout life [95].
In summary, the findings indicate that TM has a beneficial effect upon resting and ambulatory BP, CV reactivity to behavioral stress and ventricular function. Whether decreased SNS activity, decreased CV reactivity and improved renal function are physiological pathways linking TM with improved BP control via improved ventricular and vascular function is unknown and requires further study. Most importantly, studies are needed to determine whether different types of behavioral stress reduction programs such as TM, will improve SBP via decreased anger and hostility and improved neurohormonal, renal, vascular and ventricular function, particularly during stress in those at particular risk for development of EH.
PART 2: TREATMENT OF CARDIOVASCULAR RISK FACTORS IN ADULTS
Recommendations of BP-lowering by JNC-7 [83] reflects the inescapable epidemiological fact that BP-related disease cannot be minimized only by treating those with clinical hypertension. Indeed, safe and effective measures to achieve small but significant reductions in BP across entire populations could have a far greater impact in reducing CVD than strategies targeting only higher risk patients. As recommended by JNC-7, the first choice for such measures should be lifestyle/non-pharmacological. TM’s effects in reducing BP in both hypertensive and pre-hypertensive individuals [82,84,93,96–100] coupled with its additional benefits for health-related behaviors and well-being [99,101,102], could be extremely valuable as part of a population strategy for CVD prevention.
Jevning et al. reviewed findings on the impact of TM on acute changes in oxygen consumption, respiration, circulation, tissue metabolism, endocrine, neurotransmitter and autonomic effects, EEG, evoked potential and sensory and motor responses, concluding that the impact of TM is as an integrated response [103]. The review discusses mechanics by which TM reduces baseline levels of stress hormones and suggests that TM provides the physiological basis for a more adaptive response to stress facilitated by a unique deep metabolic rest during which the body’s homeostatic mechanism can normalize malfunctions in the system. The review highlights the need for further research to distinguish TM from other forms of relaxation or stress reduction.
META-ANALYSIS ON PHYSIOLOGICAL EFFECTS AND REVIEWS OF PSYCHOLOGICAL AND PHYSIOLOGICAL MECHANISMS
A meta-analysis of 32 physiological studies by Dillbeck and Orme-Johnson [104] found that TM produces deeper rest than ordinary relaxation, as indicated by greater increases in basal skin resistance, greater decreases in respiration rate, and greater decreases in plasma lactate, a biochemical stress marker. The study also showed that meditators have lower baseline levels of stress outside of the meditation period as indicated by lower measures of sympathetic arousal, (heart rate, respiration rate, spontaneous skin resistance responses, plasma lactate), and finds the TM technique to be more effective than clinically derived methods in reducing several CVD risk factors, i.e., blood pressure [104].
A well-presented model of pathophysiological mechanisms linking psychosocial stress to CVD events is presented by Bairey Merz et al. [105]. Links between psychosocial stress and atherosclerosis, endothelial function, plaque rupture, thrombosis and arrhythmias are presented. Part 2 of this series discusses the effectiveness of TM in treatment and prevention of CVD risk factors including BP, lipids and cholesterol, tobacco and CV reactivity to stress, with helpful tables summarizing the findings [106]. The review discusses TM’s impact on psychological and physiological mechanisms, and highlights reductions in CVD morbidity and mortality, including regression of atherosclerosis, left ventricular hypertrophy and myocardial ischemia.
Part 3 of this series examines clinical and policy implications of research on TM, reviews TM’s impact on medical care utilization, and provides recommendations for health insurance claims and physician reimbursements [107]. The nature and effects of TM which included its origin and standardized instruction, and compliance issues are discussed. The article highlights the need for education of public and health care professionals of TM’s benefits and gives policy recommendations with regard to issues such as services, provision, certification, licensure issues, and reimbursement. Evidence supporting TM for primary and secondary CVD prevention are reviewed and the addition of TM instruction to the health care system is recommended. Concerns related to feasibility of implementation of TM in large-scale settings (e.g., schools, communities, etc.) and availability of specially trained TM teachers were not addressed.
IMPACT ON HYPERTENSION
The efficacy of conventional drug therapy in preventing the most frequent complication of hypertension, i.e., CVD, is less than perfect. For example, anti-hypertensive drug therapy has been associated with tolerability of adverse side effects [108], impaired quality of life concerns [109], and cost effectiveness [110]. However, opinion is mixed regarding patient compliance and BP control [111], and some propound that the relationship has not yet been well established [112]. For these and other reasons the other reasons JNC-7, the National High Blood Pressure Education Program, and the Working Group in Hypertension have recommended non-drug lifestyle modification approaches as first-line definitive or adjunctive treatment for hypertension [83]. Given the inconsistencies that lifestyle interventions have upon BP control and the potential role of psychosocial stress in the development of EH, stress reduction has been shown to be beneficial in the reduction of BP. Adult long-term practitioners of TM have significantly lower BP compared with age group-based population norms [113]. In recent years, well controlled randomized clinical trials (RCT) have been conducted to examine the BP-lowering impact of stress reduction via TM in adults as well as adolescents. Studies with adults have been extensively reviewed previously and will be briefly summarized below [96,106, 107,114–116].
Research on TM and hypertension in adults originated at a number of independent universities, starting in the early 1970’s. Studies with mild and moderate hypertensives were carried out at Harvard Medical School [117], College of Medicine, University of Cincinnati, Cardiovascular Center [118], and Medical College of Allahabad, India [119]. These studies used multiple baseline measures to control for adaptation effects. The group means at baseline of the studies ranged from SBP/DBP 150/94 mm Hg [117] to 157/102 mm Hg [119]. Collectively, these studies [117–119] reported that after a mean of 6 months of TM practice, SBP/DBP decreased by a mean of −12.6/−8.8 mm Hg. Recently larger and better-controlled randomized clinical trials [82,84,93,96–100] have corroborated early findings that TM has a beneficial effect of BP.
A safeguard against potential researcher bias built into randomized studies was that BP data were collected by independent personnel at independent institutions. Studies have been conducted by authors associated with Maharishi University of Management or who practiced TM, in association with independent collaborators from Harvard University and University of Maryland [99], West Oakland Health Center, University of Arkansas, and Haight-Ashbury Free Clinic [97], University of Iowa Hospitals and Clinics [98], More-house School of Medicine, Lake Merritt Heart Care, Haight-Ashbury and West Oakland Health Clinics, and University of Michigan [100].
Data were collected in homes for the elderly in the Boston area [99], West Oakland Health Care Center, an inner city, primary care, community heath clinic in Oakland, California [82,96,97,100], Clinical Research Center of the University of Iowa Hospitals and Clinics [98]. These studies were funded by grants from the National Institute of Mental Health [99], National Institutes of Health, including the National Heart, Lung and Blood Institute [98,100,120], the Retirement Research Foundation and the Lancaster Foundation [97].
In the first randomized clinical trial (RCT) on TM and blood pressure, Alexander et al. [99] studied 73 elderly subjects in the Boston area. The mean age was 80.7 years, and subjects were randomly assigned to the TM program or to inventions designed to match the TM program for contact time with the teacher and expectation-fostering features, or to a third no-treatment control. The active control groups were mindfulness training, which “involved both a structured word-production task and an unstructured creative mental activity task”, and a TM-analog mental relaxation technique. Posttest levels of systolic SBP, adjusting for pretest levels indicated that SBP for the TM group was 4.9 mm Hg lower than mindfulness, 19.6 mm Hg lower than mental relaxation, and 9.9 mm Hg lower than no-treatment. Planned comparison for this pattern of results was significant at p<.01.
In a later RCT on TM and blood pressure, Schneider et al. [97] randomly assigned 127 older African Americans to either TM, Progressive Muscle Relaxation (PMR) or a health education program consisting of dietary and exercise recommendations (HE). Multiple baseline measurements were taken, and after three months of intervention, the unadjusted change in SBP in mm Hg was −10.4 for TM, −4.0 for PMR, and −1.5 for HE. The unadjusted change in DBP in mm Hg was −5.7 for TM, − 2.1 for PMR, and + 6 for HE. Controlling for age produced significant results for TM on SBP when compared to PMR (p<.025) or HE (p<.0005), and for DBP, TM compared to PMR (p<.05) or HE (p<.00005). TM appears to be more efficacious for those who are not on medication, but also simultaneously decreases BP and use of anti-hypertension medication [120], and has been found to reduce the reliance on and desire for drugs in general [121]. A separate subgroup analyses by sex was published by Alexander et al. suggested efficacy of TM for treating hypertension in patients in high as well as low risk categories for six hypertension-related measures of risk: obesity, alcohol use, psychosocial stress, dietary sodium-to-potassium ratio, physical inactivity, and presence of multiple risks [82].
In the third RCT on TM and blood pressure, Wenneberg et al. [98] randomly assigned 66 normotensive 18–34 year old men (mean BP 124.8/70.7 mm Hg) to either TM or to an active control condition modeled after the standard TM course to control for expectancy, instructor attention, and daily time commitment. After four months of treatment, ambulatory DBP decreased by 8.8 mm Hg in high-compliance TM subjects compared to an increase of 2.3 mm Hg in high-compliance controls, but did not change significantly for SBP. A possible interpretation is that TM is effective, but obviously only for those who practice it. The findings raise the practical question of which patients are willing to learn the technique and continue practicing it—a different issue from whether TM is effective or not.
In the fourth RCT on TM and blood pressure, Schneider et al. [120] collaborated with the Haight-Ashbury Free Medical Clinic supported by an NIH grant extending the earlier three-month design [97] to one-year. The study randomly assigned 150 hypertensive African Americans (mean age 49 years; mean 142/95 mm Hg) to TM, Progressive Muscle Relaxation (PMR), or Health Education (HE). Three baseline measurements were taken during each of five sessions spread over one month, and the mean of the 4th and 5th sessions were used as the baseline. The mean change over the year-long intervention for TM was a decrease in SBP/DBP by −3.1/−5.7 mm Hg compared to −0.5/−2.9 mm Hg for PMR or HE, (p’s<0.1 for SBP, p’s<0.01, for DBP). The study found significant within-group BP reductions for TM by the third month, whereas the changes in the other groups did not manifest until after 6 months, providing a longer sustained period of lowered BP for the TM group. The TM group also decreased the use of anti-hypertensive medication relative to PMR (p<.001) and HE (p<.09, trend).
STRESS REDUCTION, CORTISOL AND CVD RISK
Stress affects health adversely through limiting or distorting the normal functioning of adaptive mechanisms [95]. Modifying response to stress has been found to reduce cardiac events [122,123]. TM habituates the nervous system to maintain a more restfully alert resting baseline outside the TM practice [124]. This is indicated by the lower baseline levels outside TM of autonomic measures such as heart and respiration rates [124]. It has been suggested that TM practice facilitates maintenance of a more efficient style of functioning which conserves more energy during non-stressful periods to utilize for coping with stress [115]. In support of this, MacLean et al. reported that TM practice develops a stronger, more adaptive autonomic response to the challenges of stressors, as indicated by improved heart rate, skin resistance, and cortisol responses [125,126].
Cortisol, when produced at appropriate levels, effectively modulates various acute responses to stress [95]. However, chronic stress causes cortisol overproduction, resulting in damaging effects. There is evidence that elevated cortisol levels or impaired cortisol regulation increases atherosclerosis [127], hypertension [128], cancer [129], obesity [130], osteoporosis [131], immunodeficiency [132], hyperlipidemia [133,134], depression [135], some anxiety [136] and aggression-related disorders, such as drug abuse and other addictive disorders [137]. TM practice has been shown to produce a healthy cortisol profile of lower baseline levels and a more robust cortisol response to acute stress. A 27% decline in cortisol concentration during TM reported in studies by Jevning et al. is consistent with complete inhibition of cortisol excretion [138,139]. These findings suggest that adaptive efficiency is a concept that captures TM’s many effects. The strengthening effect of the TM program on the physiology may help to attenuate the negative impact of environmental stressors.
DECREASED SERUM CHOLESTEROL LEVELS
One of the CVD risk factors that normalizes through regular TM practice is serum cholesterol levels. A controlled longitudinal study over an 11-month period found that the TM program reduces serum cholesterol levels. Recent evidence suggests that oxidant stress impacts several functions of the endothelium, including modulation of vasomotor tone [140]. Related to this, 15% lower serum levels of lipid peroxides were found in a study of healthy normotensive TM practitioners compared with matched controls (p<.03). The mechanism for TM’s impact on cholesterol levels is unclear but may involve improved lipid metabolism or better dietary choices, or both [141].
EFFECTS ON TOBACCO AND ALCOHOL USAGE
Cigarette smoking continues to be a major health hazard, and contributes significantly to cardiovascular morbidity and mortality [142]. Research has established a solid relationship between drinking and higher BP [143] and CVD [144]. Effects of TM on tobacco, alcohol, and drug abuse have been reviewed in a number of groups, ranging from the general population to incarcerated drug offenders [145]. A wide range of evidence suggests that the restorative rest produced by TM normalizes the neurochemical imbalances caused by substance abuse [146]. As a result, the physiological basis for craving is thought to decline, which is often accompanied by a decline in substance use [147]. A meta-analysis of 198 studies on behavioral techniques for reducing tobacco, alcohol, and drug consumption suggested that TM had substantially larger effect sizes in reducing harmful substance consumption than other techniques, including relaxation programs, therapeutic probation, pharmacological intervention, educational programs, and unconventional treatments (e.g., acupuncture) [121]. The TM studies also showed that patterns of abstinence were maintained for a longer time. A prospective study of 324 cigarette smokers found that 51% of those who reported full compliance with the TM practice quit smoking after two years, compared to 21% for both partial TM adherents and non-TM controls. The TM program gives no advice to quit smoking [70]. Rather, reduction in smoking is thought to be motivated by the increased sensitivity to the harmful effects of tobacco on the body [148].
ACUTE EFFECTS OF TM ON CV FUNCTION
Increased vasoconstriction has been implicated in the development of EH [50]. Decreased vascular resistance (total peripheral resistance, TPR) is associated with an increase in cardiac output [149]. The acute effect of TM upon CV function was examined in a group of 32 healthy middle aged adults (mean age = 46.7 ± 3.7 yrs) without any history of vascular dysfunction [150]. Long term TM practitioners (mean regular twice daily TM practice = 23.7±5.2 years) were compared to a matched normotensive control group on CV function at rest and during 20 minutes of self-relaxation (eyes closed rest for control group versus TM). The TM group exhibited greater decreases in SBP (−3.0 vs. + 2.1 mmHg, p<.04) and TPR(−1.0 vs. +0.3 mmHg/L/min, p<.03) compared to self-relaxation in the control group. TPR decreased significantly during TM. Decreases in vasoconstrictive tone during TM may be the hemodynamic mechanism responsible for reduction of high BP over time. The results of this study provide a preliminary contribution to the understanding of the underlying hemodynamic mechanisms responsible for beneficial influence of TM upon cardiovascular risk factors.
DECREASED ANGINA PECTORIS AND CAROTID ATHEROSCLEROSIS
A controlled longitudinal study of angina pectoris reported that TM improved exercise tolerance, increased maximum workload, and delayed appearance of electrocardiographic abnormalities during exercise (delayed onset of ST segment depression) in heart patients after 1 year of TM practice [151]. In another study, TM was associated with reduced carotid atherosclerosis in hypertensive African-Americans (AAs) [152].
REDUCED CARDIOVASCULAR MORBIDITY
The results of two large field studies of Blue Cross/Blue Shield of Iowa insurance statistics reported markedly lower medical utilization for TM subjects. The first study examined a group of TM participants that increased in size from 694 to 2,119 over the five-year study period [153]. The TM group was compared to the Blue Cross norm groups comprised of approximately 600,000 members and to five other groups (combined N=22,440) selected by Blue Cross to be of comparable policies, size, and professional membership as the TM group. The TM group’s rate of hospitalization for diseases of the heart and blood vessels was 87% lower than the norm. The overall admissions rate for all causes for the TM group was 55% lower than other groups. The TM group’s average length of hospital stay was 4.5 days compared to 5.4 days for other groups, patient days per 1000 were 61% lower, and TM outpatient visits were 53% lower. Analysis by age categories showed approximately a 50% reduction in inpatient and outpatient admission rates for all causes for the younger TM groups, with even greater reductions of 68% and 74%, respectively, for TM practitioners over 40. Since CVD incidence increases with age, the findings of this study has profound implications for TM with regard to CVD prevention.
COST EFFECTIVENESS OF TM IN TREATING HYPERTENSION
As reviewed above, randomized studies suggest that TM reduces blood pressure in hypertension as effectively as do drug therapies. Cost-effectiveness of managing hypertension comparing TM with the five leading anti-hypertensive drugs was analyzed by Herron et al. [154] This cost-effectiveness comparison in 1996 dollars over a simulated 20-year treatment period reported that TM had the lowest present value cost, and the best health benefits. The study indicated that TM is a cost-effective treatment for hypertension with many side benefits.
CARDIOVASCULAR MORTALITY
Two random assignment studies found that the TM program decreased mortality rates from cardiovascular disease, as well as for death by all causes [155,156]. The first study was a 15-year follow-up of 87 subjects over 80 years old who had been randomly assigned to TM, mindfulness training (MF), mental relaxation (MR) and a no-treatment control (NT). In this study after 3 years survival for the TM patients was 100% compared lower rates for other groups [99]. After 16 years, mean survival time for CVD was higher, and all-cause mortality was significantly lower for the TM group compared to the other groups combined.
In a second study, mortality and cause of death were assessed from vital statistics over 8 years of follow-up on 109 older African American patients with mild hypertension (mean age 67 years) who had participated in a hypertension study [97]. Subjects were randomly assigned to two active stress reduction approaches—the TM program or progressive muscle relaxation (PMR)—or a health education control (EC) program for three months. The adjusted relative risk for CVD mortality of the TM group compared with EC was significantly reduced by 81%. The adjusted relative risk for all-cause mortality of the TM group compared with PMR showed a trend at 57% reduction in the analysis of the 3-month finishers. When patient data from the above two randomized controlled trials was combined in a post-hoc analysis [157], the TM group showed a 23% reduction in all cause mortality compared to combined controls, a 30% reduction in the rate of cardiovascular mortality and a 49% reduction in the rate of cancer mortality. These studies require replication in a larger study but collectively suggest that TM may offer benefit for reducing all-cause and CVD mortality.
If an effective, long-term non-pharmacological approach shown to reduce the incidence of EH and CVD could be applied on a widespread basis, the significance could hardly be underestimated. Recent epidemiologic studies have documented worrisome trends towards increasing BP and obesity levels in adolescents [158]. Since CVD risk factors have been shown to persist into adulthood, this may translate into a CVD epidemic in the future. Health care providers need to assume greater responsibility for the prevention, detection, and intervention relevant to CVD risk factors in adolescents [159]. The urgent need for both population-based and individual approaches to primary prevention of CVD beginning in childhood cannot be over-emphasized [160]. Adolescents should be empowered through education and skill development to assume increasing responsibility for their own health behaviors [161]. School-based interventions including stress reduction can improve the CVD risk profile of children and should be utilized as one means of early primary prevention of CVD [80].
In summary, TM is an easily learned, cost effective means of reducing resting and ambulatory blood pressure and CV reactivity, and improving ventricular function in adolescents at risk for hypertension. In adults with mild or moderate EH, TM decreases blood pressure, reduces the use of anti-hypertensive medication, decreases angina pectoris and carotid atherosclerosis. It markedly reduces medical care utilization for CVD, especially in older individuals, and it significantly decreases CVD and all-cause mortality. The mechanism of TM’s effects appears to be through acute and longitudinal reductions in sympathetic tone and reactivity to stress. It decreases resting heart, respiratory rates and cortisol levels, improves CV function, and decreases stress-related risk factors, including serum cholesterol levels, and alcohol and tobacco use.
Considerable compelling evidence for the efficacy of TM as an approach to preventing and controlling EH and CVD risk has also been documented in extensive reviews [96,106,116,162]. Evidence presented offers a basis for public health policies and clinical approaches that can greatly affect the incidence and consequences of EH and CVD in the population at large [107]. The effective implementation of stress reduction depends to a large extent on the training and motivation of the health care administration. The support and involvement of health professionals, educators, community organizations, industry and government together is necessary to support the adoption of healthy lifestyles for our society for succeeding generations [163]. Intervention through stress reduction in youth and adults is suggested as a future direction for preventive cardiology.
Footnotes
Transcendental Meditation and TM are trademarks registered in the US. Patent and Trademark Office, licensed to Maharishi Vedic Education Development Corporation and are used with permission.
References
- 1.American Heart Association. Heart Disease and Stroke Statistics —2005 Update. Dallas, TX: American Heart Association; 2005. [Google Scholar]
- 2.White AD, Hames CG, Tyroler HA. Serum cholesterol and 20-year mortality in black and white men and women aged 65 and older in the Evans County Heart Study. Ann Epidemiol. 1992;2:85–89. doi: 10.1016/1047-2797(92)90041-n. [DOI] [PubMed] [Google Scholar]
- 3.Stamler J, Stamler R, Neaton JD. Blood pressure, systolic and diastolic, and cardiovascular risks. US population data. Arch Intern Med. 1993;153:598–615. doi: 10.1001/archinte.153.5.598. [DOI] [PubMed] [Google Scholar]
- 4.Keil JE, Sutherland SE, Hames CG, et al. Coronary disease mortality and risk factors in black and white men. Results from the combined Charleston, SC, and Evans County, Georgia, heart studies. Arch Intern Med. 1995;155:1521–1527. [PubMed] [Google Scholar]
- 5.Williams JE, Nieto FJ, Sanford CP, Tyroler HA. Effects of an angry temperament on coronary heart disease risk : The Atherosclerosis Risk in Communities Study. Am J Epidemiol. 2001;154:230–235. doi: 10.1093/aje/154.3.230. [DOI] [PubMed] [Google Scholar]
- 6.Sorrentino MJ. Implications of the metabolic syndrome: the new epidemic. Am J Cardiol. 2005;96:3E–7E. doi: 10.1016/j.amjcard.2005.05.008. [DOI] [PubMed] [Google Scholar]
- 7.Reaven G, Abbasi F, McLaughlin T. Obesity, insulin resistance, and cardiovascular disease. Recent Prog Horm Res. 2004;59:207–223. doi: 10.1210/rp.59.1.207. [DOI] [PubMed] [Google Scholar]
- 8.Lewis S. Broken heart syndrome: perspectives from East and West. Adv Mind Body Med. 2005;21:3–5. [PubMed] [Google Scholar]
- 9.Eisenmann JC. Physical activity and cardiovascular disease risk factors in children and adolescents: an overview. Can J Cardio. 2004;20:295–301. [PubMed] [Google Scholar]
- 10.Raitakari OT, Juonala M, Kahonen M, et al. Cardiovascular risk factors in childhood and carotid artery intima-media thickness in adulthood: the Cardiovascular Risk in Young Finns Study. JAMA. 2003;290:2277–2283. doi: 10.1001/jama.290.17.2277. [DOI] [PubMed] [Google Scholar]
- 11.Li S, Chen W, Srinivasan SR, et al. Childhood cardiovascular risk factors and carotid vascular changes in adulthood: the Bogalusa Heart Study. JAMA. 2003;290:2271–2276. doi: 10.1001/jama.290.17.2271. [DOI] [PubMed] [Google Scholar]
- 12.Grundy SM, Cleeman JI, Merz CN, et al. Program. CCotNCE. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III Guidelines. J Am Coll Cardiol. 2004;44:720–732. doi: 10.1016/j.jacc.2004.07.001. [DOI] [PubMed] [Google Scholar]
- 13.Snieder H, Harshfield G, Barbeau P, Pollock D, Pollock J, Treiber F. Dissecting the genetic architecture of the cardiovascular and renal stress response. Biol Psychol. 2002;61:73–95. doi: 10.1016/s0301-0511(02)00053-4. [DOI] [PubMed] [Google Scholar]
- 14.Treiber FA, Davis H, Turner JR. Cardiovascular responsivity to stress and preclinical manifestations of cardiovascular disease in youth. In: Hayman L, McMahon M, Turner JR, editors. Health and Behavior in Childhood and Adolescence: Cross-disciplinary Perspectives. New York: Lawrence Erlbaum Associates, Inc; 2001. [Google Scholar]
- 15.Cohen S, Kessler RC, Underwood Gordon L. Strategies for measuring stress in studies of psychiatric and physical disorders. In: Cohen S, Kessler RC, Underwood Gordon L, editors. Measuring stress. New York: Oxford University Press; 1995. pp. 3–26. [Google Scholar]
- 16.Esler M. The sympathetic system and hypertension. Am J Hypertens. 2000;13:99S–105S. doi: 10.1016/s0895-7061(00)00225-9. [DOI] [PubMed] [Google Scholar]
- 17.Manuck SB. Cardiovascular reactivity in cardiovascular disease: “Once more unto the breach”. Intern J Behav Med. 1994;1:4–31. doi: 10.1207/s15327558ijbm0101_2. [DOI] [PubMed] [Google Scholar]
- 18.Julius S, Nesbitt S. Sympathetic overactivity in hypertension. A moving target. Am J Hypertens. 1996;9:113S–120S. doi: 10.1016/0895-7061(96)00287-7. [DOI] [PubMed] [Google Scholar]
- 19.Guyton AC, Hall JE. Textbook of Medical Physiology. 9. Philadelphia: W.B. Saunders Company; 1996. [Google Scholar]
- 20.Luft FC, Grim CE, Fineberg N, Weinberger MC. Effects of volume expansion and contraction in normotensive whites, blacks, and subjects of different ages. Circulation. 1979;59:643–650. doi: 10.1161/01.cir.59.4.643. [DOI] [PubMed] [Google Scholar]
- 21.Anderson NB. Ethnic differences in resting and stress-induced cardiovascular and humoral activity. In: Schneiderman N, Weiss SM, Kaufman PG, editors. Handbook of Research Methods in Cardiovascular Behavioral Medicine. New York: Plenum Press; 1989. [Google Scholar]
- 22.Folkow B. The structural factor in hypertension. In: Laragh JH, Brenner SM, editors. Hypertension: Pathophysiology, diagnosis and management. New York: Raven Press; 1990. pp. 5–58. [Google Scholar]
- 23.Folkow B. “Structural factor” in primary and secondary hypertension. Hypertension. 1990;16:89–101. doi: 10.1161/01.hyp.16.1.89. [DOI] [PubMed] [Google Scholar]
- 24.Weber KT, Sun Y, Guarda E. Structural remodeling in hypertensive heart disease and the role of hormones. Hypertension. 1994;23:869–877. doi: 10.1161/01.hyp.23.6.869. [DOI] [PubMed] [Google Scholar]
- 25.Levy D, Garrison RJ, Savage DD, Kannel WB, Castelli WP. Prognostic implications of echocardiographically determined left ventricular mass in the Framingham Heart Study. N Engl J Med. 1990;322:1561–1566. doi: 10.1056/NEJM199005313222203. [DOI] [PubMed] [Google Scholar]
- 26.Koren MJ, Devereux RB, Casale PN, Savage DD, Laragh JH. Relation of left ventricular mass and geometry to morbidity and mortality in uncomplicated essential hypertension. Ann Intern Med. 1991;114:345–352. doi: 10.7326/0003-4819-114-5-345. [DOI] [PubMed] [Google Scholar]
- 27.Casale PN, Devereux RB, Milner M, et al. Value of echocardiographic measurement of left ventricular mass in predicting cardiovascular morbid events in hypertensive men. Ann Intern Med. 1986;105:173–178. doi: 10.7326/0003-4819-105-2-173. [DOI] [PubMed] [Google Scholar]
- 28.Papavassiliou DP, Treiber FA, Strong WB, Malpass MD, Davis H. Anthropometric, demographic, and cardiovascular predictors of left ventricular mass in young children. Am J Cardiol. 1996;78:323–326. doi: 10.1016/0002-9149(96)00286-x. [DOI] [PubMed] [Google Scholar]
- 29.Murdison KA, Treiber FA, Mensah G, Davis H, Thompson W, Strong WB. Prediction of left ventricular mass in youth with family histories of essential hypertension. Am J Med Sci. 1998;315:118–123. doi: 10.1097/00000441-199802000-00008. [DOI] [PubMed] [Google Scholar]
- 30.Suls J, Wan CK. The relationship between trait hostility and cardiovascular reactivity: a quantitative review and analysis. Psycho-physiology. 1993;30:615–626. doi: 10.1111/j.1469-8986.1993.tb02087.x. [DOI] [PubMed] [Google Scholar]
- 31.Suls J, Wan CK, Costa PTJ. Relationship of trait anger to resting blood pressure: a meta-analysis. Health Psychol. 1995;14:444–456. doi: 10.1037//0278-6133.14.5.444. [DOI] [PubMed] [Google Scholar]
- 32.Rutledge T, Hogan BE. A quantitative review of prospective evidence linking psychological factors with hypertension development. Psychosom Med. 2002;64:758–766. doi: 10.1097/01.psy.0000031578.42041.1c. [DOI] [PubMed] [Google Scholar]
- 33.Anderson NB, Myers HF, Pickering T, Jackson JS. Hypertension in blacks: Psychosocial and biological perspectives. J Hypertens. 1989;7:161–172. [PubMed] [Google Scholar]
- 34.Johnson EH, Broman CL. The relationship of anger expression to health problems among black Americans in a national survey. J Behav Med. 1987;10:103–116. doi: 10.1007/BF00846419. [DOI] [PubMed] [Google Scholar]
- 35.Johnson EH. The Deadly Emotions: The Role of Anger, Hostility and Aggression in Health and Emotional Well-Being. New York: praeger Publishing Corp; 1990. [Google Scholar]
- 36.Johnson EH, Spielberger CD, Worden TJ, Jacobs GA. Emotional and familial determinants of elevated blood pressure in black and white adolescent males. J Psychosom Res. 1987;31:287–300. doi: 10.1016/0022-3999(87)90048-1. [DOI] [PubMed] [Google Scholar]
- 37.Johnson EH, Schork NF, Spielberger CD. Emotional and familial determinants of elevated blood pressure in black and white adolescent females. J Psychosomatic Res. 1987;31:731–741. doi: 10.1016/0022-3999(87)90022-5. [DOI] [PubMed] [Google Scholar]
- 38.Musante L, Turner JR, Treiber FA, Davis H, Strong WB. Moderators of ethnic differences in vasoconstrictive reactivity in youth. Ethn Dis. 1996;6:224–234. [PubMed] [Google Scholar]
- 39.Wright LB, Treiber FA, Davis H, et al. Relationship between family environment and children’s hemodynamic responses to stress: A longitudinal evaluation. Behav Med. 1993;19:115–121. doi: 10.1080/08964289.1993.9935180. [DOI] [PubMed] [Google Scholar]
- 40.Wright LB, Treiber F, Davis H, Bunch C, Strong WB. The role of maternal hostility and family environment upon cardiovascular functioning among youth two years later: socioeconomic and ethnic differences. Ethn Dis. 1998;8:367–376. [PubMed] [Google Scholar]
- 41.Eich RH, Jacobsen EC. Vascular reactivity in medical students followed for 10 yr. J Chron Dis. 1967;20:583–592. doi: 10.1016/0021-9681(67)90035-5. [DOI] [PubMed] [Google Scholar]
- 42.Matthews KA, Woodall KL, Allen MT. Cardiovascular reactivity to stress predicts future blood pressure status. Hypertension. 1993;22:479–485. doi: 10.1161/01.hyp.22.4.479. [DOI] [PubMed] [Google Scholar]
- 43.Menkes MS, Matthews KA, Krantz DS, et al. Cardiovascular reactivity to the cold pressor test as a predictor of hypertension. Hypertension. 1989;14:524–530. doi: 10.1161/01.hyp.14.5.524. [DOI] [PubMed] [Google Scholar]
- 44.Falkner B, Kushner H, Onesti G, Angelakos ET. Cardiovascular characteristics in adolescents who develop essential hypertension. Hypertension. 1981;3:521–527. doi: 10.1161/01.hyp.3.5.521. [DOI] [PubMed] [Google Scholar]
- 45.Jackson AS, Squires WG, Grimes G, Beard EF. Prediction of future resting hypertension from exercise blood pressure. J Card Rehabilit. 1983;3:263–268. [Google Scholar]
- 46.Anderson NB, Armstead CA. Toward understanding the association of socioeconomic status and health: a new challenge for the biopsychosocial approach. Psychosomatic Med. 1995;57:213–225. doi: 10.1097/00006842-199505000-00003. [DOI] [PubMed] [Google Scholar]
- 47.Clark R, Anderson NB, Clark V, Williams DR. Racism as a stressor for African Americans. A biopsychosocial model. Am Psychol. 1999;54:805–816. doi: 10.1037//0003-066x.54.10.805. [DOI] [PubMed] [Google Scholar]
- 48.Anderson NB, McNeilly M, Myers H. Toward understanding race difference in autonomic reactivity. In: Turner JR, Sherwood A, Light KC, editors. Individual Differences in Cardiovascular Response to Stress. New York: Plenum Press; 1992. pp. 125–145. [Google Scholar]
- 49.Treiber FA, Kamarck T, Schneiderman N, Sheffield D, Kapuku G, Taylor T. Cardiovascular reactivity and development of preclinical and clinical disease states. Psychosom Med. 2003;65:46–62. doi: 10.1097/00006842-200301000-00007. [DOI] [PubMed] [Google Scholar]
- 50.Anderson NB. Racial differences in stress-induced cardiovascular reactivity and hypertension: current status and substantive issues. Psychol Bull. 1989;105:89–105. doi: 10.1037/0033-2909.105.1.89. [DOI] [PubMed] [Google Scholar]
- 51.Saab PG, Llabre MM, Hurwitz BE, Schneiderman N, et al. Myocardial and peripheral vascular responses to behavioral challenges and their stability in black and white. Americans Psychophysiology. 1992;29:384–397. doi: 10.1111/j.1469-8986.1992.tb01712.x. [DOI] [PubMed] [Google Scholar]
- 52.Treiber FA, Davis H, Musante L, Raunikar RA, Strong WB, McCaffrey F. Ethnicity, gender, family history of myocardial infarction, and hemodynamic responses to laboratory stressors in children. Health Psychol. 1993;12:6–15. doi: 10.1037//0278-6133.12.1.6. [DOI] [PubMed] [Google Scholar]
- 53.Treiber FA, McCaffrey F, Musante L, et al. Ethnicity, family history of hypertension and patterns of hemodynamic reactivity in boys. Psychosomatic Med. 1993;55:70–77. doi: 10.1097/00006842-199301000-00012. [DOI] [PubMed] [Google Scholar]
- 54.Celermajer DS, Sorensen KE, Gooch VM, et al. Non-invasive detection of endothelial dysfunction in children and adults at risk of atherosclerosis. Lancet. 1992;340:1111–1115. doi: 10.1016/0140-6736(92)93147-f. [DOI] [PubMed] [Google Scholar]
- 55.Luscher TF, Vanhoutte PM. The Endothelium: Modulator of Cardiovascular Function. Boca Raton, Fla: CRC Press; 1990. [Google Scholar]
- 56.Celermajer DS, Sorensen KE, Bull C, Robinson J, Deanfield JE. Endothelium-dependent dilation in the systemic arteries of asymptomatic subjects relates to coronary risk factors and their interaction. J Am Coll Cardiol. 1994;24:1468–1474. doi: 10.1016/0735-1097(94)90141-4. [DOI] [PubMed] [Google Scholar]
- 57.Kapuku G, Treiber FA, Davis HC, Mensah GA. Endothelial function and hemodynamic responsivity to stress in youth. Psychosom Med. 2000;62:150. [Google Scholar]
- 58.Treiber F, Papavassiliou D, Gutin B, et al. Determinants of endothelium-dependent femoral artery vasodilation in youth. Psychosomatic Med. 1997;59:376–381. doi: 10.1097/00006842-199707000-00007. [DOI] [PubMed] [Google Scholar]
- 59.Hartley B, Treiber F, Ludwig D, Kapuku G. Correlates of femoral artery flow mediated dilation in a multi-ethnic sample of 12- to 26-year-olds. Ethn Dis. 2004;14:227–232. [PubMed] [Google Scholar]
- 60.Labarthe D, Ayala C. Nondrug interventions in hypertension prevention and control. Cardiol Clin. 2002;20:249–263. doi: 10.1016/s0733-8651(01)00003-0. [DOI] [PubMed] [Google Scholar]
- 61.Linden W, Chambers L. Clinical effectiveness of non-drug treatment for hypertension: A meta-analysis. Ann Behav Med. 1994;16:35–45. [Google Scholar]
- 62.Linden W, Stossel C, Maurice J. Psychological interventions for patients with coronary artery disease. Arch Intern Med. 1996;156:745–752. [PubMed] [Google Scholar]
- 63.Davis PH, Dawson JD, Riley WA, Lauer RM. Carotid intimal-medial thickness is related to cardiovascular risk factors measured from childhood through middle age: The Muscatine Study. Circulation. 2001;104:2815–2819. doi: 10.1161/hc4601.099486. [DOI] [PubMed] [Google Scholar]
- 64.Berenson GS, Wattigney WA, Tracy RE. Atherosclerosis of the aorta and coronary arteries and cardiovascular risk factors in persons aged 6 to 30 years and studied at necropsy (The Bogalusa Heart Study) Am J Cardiol. 1992;70:851–858. doi: 10.1016/0002-9149(92)90726-f. [DOI] [PubMed] [Google Scholar]
- 65.Berenson GS, Wattigney WA, Bao W, Nicklas TA, Jiang X, Rush JA. Epidemiology of early primary hypertension and implications for prevention: the Bogalusa Heart Study. J Hum Hypertens. 1994;8:303–311. [PubMed] [Google Scholar]
- 66.Berenson GS, Srinivasan SR, Bao W. Precursors of cardiovascular risk in young adults from a biracial (black-white) population: the Bogalusa Heart Study. Ann N Y Acad Sci. 1997;817:189–198. doi: 10.1111/j.1749-6632.1997.tb48206.x. [DOI] [PubMed] [Google Scholar]
- 67.Probstfield JL. How cost-effective are new preventive strategies for cardiovascular disease? Am J Cardiol. 2003;91:22G–27G. doi: 10.1016/s0002-9149(03)00229-7. [DOI] [PubMed] [Google Scholar]
- 68.Cook NR, Cohen J, Hebert PR, Taylor JO, Hennekens CH. Implications of small reductions in diastolic blood pressure for primary prevention. Arch Intern Med. 1995;155:701–709. [PubMed] [Google Scholar]
- 69.Muntner P, He J, Cutler JA, Wildman RP, Whelton PK. Trends in blood pressure among children and adolescents. JAMA. 2004;291:2107–2113. doi: 10.1001/jama.291.17.2107. [DOI] [PubMed] [Google Scholar]
- 70.Roth R. Maharishi Mahesh Yogi’s Transcendental Meditation. Washington, DC: Primus; 1994. [Google Scholar]
- 71.Orme-Johnson DW, Farrow J, editors. Scientific Research on the Transcendental Meditation program: Collected Papers. Vol. 1. Rheinweiler, West Germany: MERU Press; 1977. [Google Scholar]
- 72.Chalmers R, Clements G, Schenkluhn H, Weinless M, editors. Scientific Research on the Transcendental Meditation program: Collected Papers. 2–4. Vlodrop, The Netherlands: MVU Press; 1990. [Google Scholar]
- 73.Wallace RK, Orme-Johnson DW, Dillbeck MC, editors. Scientific Research on the Transcendental Meditation Program: Collected Papers. Vol. 5. Fairfield, Iowa: MIU Press; 1990. [Google Scholar]
- 74.Bao W, Threefoot SA, Srinivasan SR, Berenson GS. Essential hypertension predicted by tracking of elevated blood pressure from childhood to adulthood: the Bogalusa Heart Study. Am J Hypertens. 1995;8:657–665. doi: 10.1016/0895-7061(95)00116-7. [DOI] [PubMed] [Google Scholar]
- 75.Alpert BS, Murphy JK, Treiber FA. Essential hypertension: Approaches to prevention in children. Med Exer Nutr Health. 1994;3:296–307. [Google Scholar]
- 76.Lambrechtsen J, Rasmussen F, Hansen HS, Jacobsen IA. Tracking and factors predicting rising in ‘tracking quartile’ in blood pressure from childhood to adulthood: Odense Schoolchild Study. J Hum Hypertens. 1999;13:385–391. doi: 10.1038/sj.jhh.1000836. [DOI] [PubMed] [Google Scholar]
- 77.International Pediatric Hypertension Association. Blood Pressure Facts. 2005 www.pediatrichypertension.org.
- 78.Guillaume M, Björntorp P. Obesity in children. Horm Metab Res. 1996;28:573–581. doi: 10.1055/s-2007-979856. [DOI] [PubMed] [Google Scholar]
- 79.Minutes of meeting September 8–9, 1997. Department of Health and Human Services, National Institutes of Health, National Heart, Lung, and Blood Institute; 1998. NIH Special Emphasis Panel on Intervention Studies in Children and Adolescents to Prevent Cardiovascular Disease. [Google Scholar]
- 80.Resnicow K, Robinson TN. School-based cardiovascular disease prevention studies: review and synthesis. AEP. 1997;7:S14–S31. [Google Scholar]
- 81.Kaplan NM. The 6th Joint National Committee report (JNC-6): New guidelines for hypertension therapy from the USA. Keio J Med. 1998;47:99–105. doi: 10.2302/kjm.47.99. [DOI] [PubMed] [Google Scholar]
- 82.Alexander CN, Schneider RH, Staggers F, et al. Trial of stress reduction for hypertension in older African Americans (part II): sex and risk subgroup analysis. Hypertension. 1996;28:228–237. doi: 10.1161/01.hyp.28.2.228. [DOI] [PubMed] [Google Scholar]
- 83.Chobanian AV, Bakris GL, Black HR, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: The JNC 7 Report. J Am Med Associ. 2003;289:2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 84.Barnes VA, Treiber FA, Davis H. Impact of Transcendental Meditation on cardiovascular function at rest and during acute stress in adolescents with high normal blood pressure. J Psychosomatic Res. 2001;51:597–605. doi: 10.1016/s0022-3999(01)00261-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Pickering TG. Mental stress as a causal factor in the development of hypertension and cardiovascular disease. Curr Hypertens Rep. 2001;3:249–254. doi: 10.1007/s11906-001-0047-1. [DOI] [PubMed] [Google Scholar]
- 86.O’Brien E, Staessen J. Normotension and hypertension as defined by 24-ambulatory blood pressure monitoring. Blood Pressure. 1995;4:266–282. doi: 10.3109/08037059509077607. [DOI] [PubMed] [Google Scholar]
- 87.McAlister FA, Straus SE. Evidence based treatment of hypertension. Measurement of blood pressure: an evidence based review. BMJ. 2001;322:908–911. doi: 10.1136/bmj.322.7291.908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Fahrenberg J, Myrtek M. Ambulatory Assessment: Computer-assisted Psychological and Psychophysiological Methods in Monitoring and Field Studies. Gottingen, Germany: Hogrefe and Huber; 1996. [Google Scholar]
- 89.Barnes VA, Johnson MH, Dekkers JC, Treiber FA. Reproducibility of ambulatory blood pressure measures in African American adolescents. Ethn Dis. 2002;12:240–245. [PMC free article] [PubMed] [Google Scholar]
- 90.Barnes VA, Johnson MH, Treiber FA. Temporal stability of twenty-four-hour ambulatory hemodynamic bioimpedance measures in African American adolescents. Blood Pressure Monitoring. 2004;9:173–177. doi: 10.1097/00126097-200408000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Treiber FA, Murphy JK, Davis H, Rauniker A, Pflieger K, Strong WB. Pressor reactivity, ethnicity, and 24-hour ambulatory monitoring in children from hypertensive families. Behav Med. 1994;20:133–142. doi: 10.1080/08964289.1994.9934628. [DOI] [PubMed] [Google Scholar]
- 92.Smith DHG. Ambulatory blood pressure monitoring. In: Weber MA, editor. Hypertension Medicine. Totowa, NJ: Humana Press; 2001. pp. 181–190. [Google Scholar]
- 93.Barnes VA, Johnson MH, Treiber FA. Impact of Transcendental Meditation on ambulatory blood pressure in African American adolescents. Am J Hypertension. 2004;17:366–369. doi: 10.1016/j.amjhyper.2003.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Barnes VA, Malhotra S, Treiber FA. Impact of Transcendental Meditation on vascular function in African American adolescents. Psychosomatic Med. 2005;67:A31. [Google Scholar]
- 95.Barnes VA, Schneider RH, Alexander CN, Staggers F. Stress, stress reduction and hypertension in African Americans: An updated review. J Natl Med Associ. 1997;89:464–476. [PMC free article] [PubMed] [Google Scholar]
- 96.Schneider RH, Alexander CN, Salerno J, Rainforth M, Nidich SI. Stress reduction in the prevention and treatment of cardiovascular disease in African Americans: a review of controlled research on the Transcendental Meditation (TM) program. J Soc Behav Person. 2005;17:159–180. [Google Scholar]
- 97.Schneider RH, Staggers F, Alexander CN, et al. A randomized controlled trial of stress reduction for hypertension in older African Americans. Hypertension. 1995;26:820–827. doi: 10.1161/01.hyp.26.5.820. [DOI] [PubMed] [Google Scholar]
- 98.Wenneberg SR, Schneider RH, Walton KG, et al. A controlled study on the effects of Transcendental Meditation on cardiovascular reactivity and ambulatory blood pressure. Intern J Neurosci. 1997;89:15–28. doi: 10.3109/00207459708988461. [DOI] [PubMed] [Google Scholar]
- 99.Alexander CN, Langer EJ, Newman RI, Chandler HM, Davies JL. Transcendental Meditation, mindfulness, and longevity: An experimental study with the elderly. J Person Soc Psychol. 1989;57:950–964. doi: 10.1037//0022-3514.57.6.950. [DOI] [PubMed] [Google Scholar]
- 100.Kondwani KA, Schneider RH, Alexander CN, et al. Left ventricular mass regression with the Transcendental Meditation technique and a health education program in hypertensive African Americans. J Soc Behav Person. 2005;17:181–200. [Google Scholar]
- 101.Alexander CN, Robinson P, Orme-Johnson DW, Schneider RH, Walton KG. Effects of Transcendental Meditation compared to other methods of relaxation and meditation in reducing risk factors, morbidity and mortality. Homeostasis. 1994;35:243–264. [Google Scholar]
- 102.Eppley K, Abrams AI, Shear J. Differential effects of relaxation techniques on trait anxiety: A meta-analysis. J Clin Psychol. 1989;45:957–974. doi: 10.1002/1097-4679(198911)45:6<957::aid-jclp2270450622>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- 103.Jevning R, Wallace RK, Biedebach M. The physiology of meditation: A review. A wakeful hypometabolic integrated response. Neurosci Biobehav Rev. 1992;16:415–424. doi: 10.1016/s0149-7634(05)80210-6. [DOI] [PubMed] [Google Scholar]
- 104.Orme-Johnson DW, Walton KG. All approaches of preventing or reversing effects of stress are not the same. Am J Health Promot. 1998;12:297–299. doi: 10.4278/0890-1171-12.5.297. [DOI] [PubMed] [Google Scholar]
- 105.Bairey Merz CN, Dwyer J, Nordstrom CK, Walton KG, Salerno JW, Schneider RH. Psychosocial stress and cardiovascular disease: pathophysiological links. Behav Med. 2002;27:141–147. doi: 10.1080/08964280209596039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Walton KG, Schneider RH, Nidich SI, Salerno JW, Nordstrom CK, Bairey Merz CN. Psychosocial stress and cardiovascular disease Part 2: Effectiveness of the Transcendental Meditation program in treatment and prevention. Behav Med. 2002;28:106–123. doi: 10.1080/08964280209596049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Walton KG, Schneider RH, Salerno JW, Nidich SI. Psychosocial stress and cardiovascular disease Part 3: Clinical and policy implications of research on the Transcendental Meditation program. Behav Med. 2005;30:173–183. doi: 10.3200/BMED.30.4.173-184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Bucca C. Take the side-effects of drugs into account. Lancet. 2004;364:1285. doi: 10.1016/S0140-6736(04)17149-3. [DOI] [PubMed] [Google Scholar]
- 109.Bremner AD. Antihypertensive medication and quality of life--silent treatment of a silent killer? Cardiovasc Drugs Ther. 2002;16:353–364. doi: 10.1023/a:1021790112182. [DOI] [PubMed] [Google Scholar]
- 110.Ambrosioni E. Pharmacoeconomics of hypertension management: the place of combination therapy. Pharmacoeconomics. 2001;19:337–347. doi: 10.2165/00019053-200119040-00002. [DOI] [PubMed] [Google Scholar]
- 111.Krousel-Wood M, Thomas S, Muntner P, Morisky D. Medication adherence: a key factor in achieving blood pressure control and good clinical outcomes in hypertensive patients. Curr Opin Cardiol. 2004;19:357–362. doi: 10.1097/01.hco.0000126978.03828.9e. [DOI] [PubMed] [Google Scholar]
- 112.Wetzels GE, Nelemans P, Schouten JS, Prins MH. Facts and fiction of poor compliance as a cause of inadequate blood pressure control: a systematic review. J Hypertens. 2004;22:1849–1855. doi: 10.1097/00004872-200410000-00002. [DOI] [PubMed] [Google Scholar]
- 113.Wallace RK, Silver J, Mills PJ, Dillbeck MC, Wagoner DE. Systolic blood pressure and long-term practice of the Transcendental Meditation and TM-Sidhi programs: Effects of TM on systolic blood pressure. Psychosom Med. 1983;45:41–46. doi: 10.1097/00006842-198303000-00006. [DOI] [PubMed] [Google Scholar]
- 114.Walton KG, Schneider RH, Nidich SI. Review of controlled research on the transcendental meditation program and cardiovascular disease: risk factors, morbidity, and mortality. Cardiol Rev. 2004;12:262–266. doi: 10.1097/01.crd.0000113021.96119.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Walton KG, Pugh NDC, Gelderloos P, Macrea P. Stress reduction and preventing hypertension: Preliminary support for a psychoneuroendocrine mechanism. J Altern Complement Med. 1995;1:263–283. doi: 10.1089/acm.1995.1.263. [DOI] [PubMed] [Google Scholar]
- 116.Schneider RH, Alexander CN, Wallace RK. In: search of an optimal behavioral treatment for hypertension: A review and focus on Transcendental Meditation. In: Johnson EH, Gentry WD, Julius S, editors. Personality, Elevated Blood, and Essential Hypertension. Washington: Hemisphere Publishing Corporation; 1992. pp. 291–318. [Google Scholar]
- 117.Benson H, Wallace RK. Decreased blood pressure in hypertensive subjects who practiced meditation. Circulation. 1972;45 & 46:516. doi: 10.1016/0021-9681(74)90083-6. [DOI] [PubMed] [Google Scholar]
- 118.Blackwell B, Hanenson IB, Bloomfield SS, Magenheim HG, Nidich SI, Gartside P. Effects of Transcendental Meditation on blood pressure: A controlled pilot experiment. Psychosom Med. 1975;37:86 (abstract). [Google Scholar]
- 119.Agarwal BL, Kharbanda A. Effect of transcendental meditation on mild and moderate hypertension. J Assoc Physicians India. 1981;29:591–596. [PubMed] [Google Scholar]
- 120.Schneider RH, Alexander CN, Staggers F, et al. A randomized controlled trial of stress reduction in the treatment of hypertension in African Americans over one year. Am J Hypertension. 2005;18:88–89. doi: 10.1016/j.amjhyper.2004.08.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Alexander CN, Robinson P, Rainforth M. Treating and preventing alcohol, nicotine and drug abuse through Transcendental Meditation Technique: A review and statistical analysis. In: O’Connell DF, Alexander CN, editors. Self Recovery—Treating Addictions Using Transcendental Meditation and Maharishi Ayur-Veda. Binghamton, NY: Harrington Park Press; 1994. pp. 13–88. [Google Scholar]
- 122.Blumenthal JA, Jiang W, Babyak MA, et al. Stress management and exercise training in cardiac patients with myocardial ischemia: Effects on prognosis and evaluation of mechanisms. Archiv Intern Med. 1997;157:2213–2223. [PubMed] [Google Scholar]
- 123.Blumenthal JA, Babyak M, Wei J, et al. Usefulness of psychosocial treatment of mental stress-induced myocardial ischemia in men. Am J Cardiol. 2002;89:164–168. doi: 10.1016/s0002-9149(01)02194-4. [DOI] [PubMed] [Google Scholar]
- 124.Dillbeck MC, Orme-Johnson DW. Physiological differences between Transcendental Meditation and rest. Am Psychol. 1987;42:879–881. [Google Scholar]
- 125.MacLean CR, Walton KG, Wenneberg SR, et al. Effects of the Transcendental Meditation program on adaptive mechanisms: changes in hormone levels and responses to stress after 4 months. Psychoneuroendocrinology. 1997;22:277–295. doi: 10.1016/s0306-4530(97)00003-6. [DOI] [PubMed] [Google Scholar]
- 126.MacLean CR, Walton KG, Wenneberg SR, et al. Altered responses of cortisol, GH, TSH and testosterone to acute stress after four months’ practice of Transcendental Meditation (TM) Ann N Y Acad Sci. 1994;746:381–384. doi: 10.1111/j.1749-6632.1994.tb39261.x. [DOI] [PubMed] [Google Scholar]
- 127.Tedeschi-Reiner E, Reiner Z, Ivekovic R, Novak-Laus K, Pintaric I. Plasma cortisol in men--relationship with atherosclerosis of retinal arteries. Coll Antropol. 2002;26:615–619. [PubMed] [Google Scholar]
- 128.Quinkler M, Stewart PM. Hypertension and the cortisol-cortisone shuttle. J Clin Endocrinol Metab. 2003;88:2384–2392. doi: 10.1210/jc.2003-030138. [DOI] [PubMed] [Google Scholar]
- 129.Cizza G, Chrousos GP. Adrenocorticotrophic hormone-dependent Cushing’s syndrome. Cancer Treat Res. 1997;89:25–40. doi: 10.1007/978-1-4615-6355-6_2. [DOI] [PubMed] [Google Scholar]
- 130.Moyer AE, Rodin J, Grilo CM, Cummings N, Larson LM, Rebuffé-Scrive M. Stress-induced cortisol response and fat distribution in women. Obesity Res. 1994;2:255–261. doi: 10.1002/j.1550-8528.1994.tb00055.x. [DOI] [PubMed] [Google Scholar]
- 131.Ferrari P. Cortisol and the renal handling of electrolytes: role in glucocorticoid-induced hypertension and bone disease. Best Pract Res Clin Endocrinol Metab. 2003;17:575–589. doi: 10.1016/s1521-690x(03)00053-8. [DOI] [PubMed] [Google Scholar]
- 132.Mayo J, Collazos J, Martinez E, Ibarra S. Adrenal function in the human immunodeficiency virus-infected patient. Arch Intern Med. 2002;162:1095–1098. doi: 10.1001/archinte.162.10.1095. [DOI] [PubMed] [Google Scholar]
- 133.Peeke PM, Chrousos G. Hypercortisolism and obesity. Ann N Y Acad Sci. 1995;771:665–676. doi: 10.1111/j.1749-6632.1995.tb44719.x. [DOI] [PubMed] [Google Scholar]
- 134.Varma VK, Rushing JT, Ettinger WHJ. High density lipoprotein cholesterol is associated with serum cortisol in older people. J Am Geriatr Soc. 1995;43:1345–1349. doi: 10.1111/j.1532-5415.1995.tb06612.x. [DOI] [PubMed] [Google Scholar]
- 135.Brown ES, Varghese FP, McEwen BS. Association of depression with medical illness: does cortisol play a role? Biol Psychiatry. 2004;55:1–9. doi: 10.1016/s0006-3223(03)00473-6. [DOI] [PubMed] [Google Scholar]
- 136.Gulley LR, Nemeroff CB. The neurobiological basis of mixed depression-anxiety states. J Clin Psychiatry. 1993;54:16–19. [PubMed] [Google Scholar]
- 137.Van Praag HM. Anxiety/aggression-driven depression. A paradigm of functionalization and verticalization of psychiatric diagnosis. Prog Neuropsychopharmacol Biol Psychiatry. 2001;25:893–924. doi: 10.1016/s0278-5846(01)00151-8. [DOI] [PubMed] [Google Scholar]
- 138.Jevning R, Wilson AF, Smith WR. The transcendental meditation technique, adrenocortical activity, and implications for stress. Experientia. 1978;34:618–619. doi: 10.1007/BF01936994. [DOI] [PubMed] [Google Scholar]
- 139.Jevning R, Wilson AF, Smith WR. Adrenocortical activity during meditation. Horm Behavior. 1978;10:54–60. doi: 10.1016/0018-506x(78)90024-7. [DOI] [PubMed] [Google Scholar]
- 140.Cai H, Harrison DG. Endothelial dysfunction in cardiovascular diseases: the role of oxidant stress. Circ Res. 2000;87:840–844. doi: 10.1161/01.res.87.10.840. [DOI] [PubMed] [Google Scholar]
- 141.Cooper MJ, Aygen MM. A relaxation technique in the management of hypercholesterolemia. J Human Stress. 1979;5:24–27. doi: 10.1080/0097840x.1979.10545991. [DOI] [PubMed] [Google Scholar]
- 142.Ambrose JA, Barua RS. The pathophysiology of cigarette smoking and cardiovascular disease: an update. J Am Coll Cardiol. 2004;43:1731–1737. doi: 10.1016/j.jacc.2003.12.047. [DOI] [PubMed] [Google Scholar]
- 143.Klatsky AL. Alcohol and cardiovascular disease—more than one paradox to consider. Alcohol and hypertension: does it matter? Yes J Cardiovasc Risk. 2003;10:21–24. doi: 10.1097/01.hjr.0000051960.68260.79. [DOI] [PubMed] [Google Scholar]
- 144.Rehm J, Sempos CT, Trevisan M. Alcohol and cardiovascular disease—more than one paradox to consider. Average volume of alcohol consumption, patterns of drinking and risk of coronary heart disease—a review. J Cardiovasc Risk. 2003;10:15–20. doi: 10.1097/01.hjr.0000051961.68260.30. [DOI] [PubMed] [Google Scholar]
- 145.O’Connell DF, Alexander CN, editors. Self Recovery—Treating Addictions Using Transcendental Meditation and Maharishi Ayur-Veda. Binghamton, NY: Harrington Park Press; 1994. [Google Scholar]
- 146.Walton KG, Levitsky D. A neuroendocrine mechanism for the reduction of drug use and addictions by Transcendental Meditation. In: O’Connell DF, Alexander CN, editors. Self Recovery—Treating Addictions Using Transcendental Meditation and Maharishi Ayur-Veda. Binghamton, NY: Harrington Park Press; 1994. pp. 89–118. [Google Scholar]
- 147.Hawkins MA. Effectiveness of the Transcendental Meditation program in criminal rehabilitation and substance abuse recovery: A review of the research. J Offender Rehabilit. 2002;36:47–65. [Google Scholar]
- 148.Royer A. The role of the Transcendental Meditation Technique in promoting smoking cessation: A longitudinal study. In: O’Connell DF, Alexander CN, editors. Self Recovery—Treating Addictions Using Transcendental Meditation and Maharishi Ayur-Veda. Binghamton, NY: Harrington Park Press; 1994. pp. 221–242. [Google Scholar]
- 149.Jevning R, Wilson AF, Smith WR, Morton ME. Redistribution of blood flow in acute hypometabolic behavior. Am J Physiol. 1978;235:R89–R92. doi: 10.1152/ajpregu.1978.235.1.R89. [DOI] [PubMed] [Google Scholar]
- 150.Barnes VA, Treiber FA, Turner JR, Davis H, Strong WB. Acute effects of Transcendental Meditation on hemodynamic functioning in middle aged adults. Psychosom Med. 1999;61:525–531. doi: 10.1097/00006842-199907000-00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Zamarra JW, Schneider RH, Besseghini I, Robinson DK, Salerno JW. Usefulness of the Transcendental Meditation Program in the treatment of patients with coronary artery disease. Am J Cardiol. 1996;77:867–870. doi: 10.1016/S0002-9149(97)89184-9. [DOI] [PubMed] [Google Scholar]
- 152.Castillo-Richmond A, Schneider R, Alexander C, et al. Effects of stress reduction on carotid atherosclerosis in hypertensive African Americans. Stroke. 2000;31:568–573. doi: 10.1161/01.str.31.3.568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Orme-Johnson DW. Medical care utilization and the Transcendental Meditation program. Psychosom Med. 1987;49:493–507. doi: 10.1097/00006842-198709000-00006. [DOI] [PubMed] [Google Scholar]
- 154.Herron RE, Hillis SL, Mandarino JV, Orme-Johnson DW, Walton KG. The impact of the Transcendental Meditation program on government payments to physicians in Quebec. Am J Health Promot. 1996;10:183–191. doi: 10.4278/0890-1171-10.3.208. [DOI] [PubMed] [Google Scholar]
- 155.Alexander CN, Barnes VA, Schneider RH, et al. A randomized controlled trial of stress reduction on cardiovascular and all cause mortality: Results of 8 year and 15 year follow-ups. Circulation. 1996;93:19. Abstract. [Google Scholar]
- 156.Barnes VA, Schneider RH, Alexander CN, Rainforth M, Staggers F, Salerno J, Kondwani KA. Impact of Transcendental Meditation on mortality in older African Americans with hypertension—eight year follow-up. J Soc Behav Personal. 2005;17:201–216. [Google Scholar]
- 157.Schneider RH, Alexander CN, Staggers F, et al. Long-term effects of stress reduction on mortality in persons >/=55 years of age with systemic hypertension. Am J Cardiol. 2005;95:1060–1064. doi: 10.1016/j.amjcard.2004.12.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.McCrindle BW. Cardiovascular risk factors in adolescents: relevance, detection, and intervention. Adolesc Med. 2001;12:147–162. [PubMed] [Google Scholar]
- 159.Rocchini AP. Raising heart-healthy children. Pediatr Int. 1999;41:597–602. doi: 10.1046/j.1442-200x.1999.01151.x. [DOI] [PubMed] [Google Scholar]
- 160.Harrell JS, Pearce PF, Hayman LL. Fostering prevention in the pediatric population. J Cardiovasc Nurs. 2003;18:144–149. doi: 10.1097/00005082-200304000-00011. [DOI] [PubMed] [Google Scholar]
- 161.Washington RL. Interventions to reduce cardiovascular risk factors in children and adolescents. Am Fam Physician. 1999;59:2211–2218. [PubMed] [Google Scholar]
- 162.Walton KG, Fields JZ, Levitsky DK, Harris DA, Pugh ND, Schneider RH. Lowering cortisol and CVD risk in postmenopausal women: a pilot study using the Transcendental Meditation program. Ann N Y Acad Sci. 2005;1032:211–215. doi: 10.1196/annals.1314.023. [DOI] [PubMed] [Google Scholar]
- 163.Lawrence M, Arbeit M, Johnson CC, Berenson GS. Prevention of adult heart disease beginning in childhood: intervention programs. Cardiovasc Clin. 1991;21:249–262. [PubMed] [Google Scholar]