Abstract
We report a case of giant cell arteritis manifesting as upper limbs ischemia due to a complete occlusion of the left subclavian artery and a high grade stenosis of the right subclavian artery. We decided to use a combined medical, surgical and endovascular treatment followed by long term treatment with methotrexate. After 4 years the patient had no signs or symptoms of relapse. In our personal experience long term treatment with Methotrexate demonstrated a certain efficacy in avoiding relapse of the inflammatory phase and in maintaining stability of results in this kind of disease.
Keywords: Giant cell arteritis, Acute ischemia, Endovascular and surgical treatment; Methotrexate, Cyclophosphamide, Prednisone
1. Introduction
Giant cell arteritis (GCA) is a chronic vasculitis of large and medium size arteries affecting almost exclusively older patients (>50 years). It was first described clinically in 1890 [1], and histologically in 1932 [2].
The temporal arteries are the most commonly affected, with symptoms like: headache, painful thickening of the temporal artery, visual loss and jaw claudication.
Of the extracranial manifestations, the most frequent is stenosis or occlusion of the subclavian and axillary artery, with loss of peripheral pulses of the arm and upper limb claudication [3].
We present a patient with rest pain of the upper limbs and partial necrosis of the fingers due to extra cranial GCA.
2. Case report
A 75-year-old women presented to our department with rest pain of the upper limbs, preceded by two weeks of ingravescent claudication, and partial necrosis of the index finger of the left hand (Fig. 1). A complete absence of the upper limb pulses was found at the physical examination.
Fig. 1.

Partial necrosis of the II finger of the left hand.
Abnormalities in the following blood tests were found: elevated erythrocyte sedimentation rate (ESR) (>30 mm/h) and C-reactive protein concentrations (CRP) (>5 mg/L) which, though not diagnostic, are frequently associated with primary vasculitis.
The duplex ultrasound imaging showed a complete occlusion of the left subclavian artery and a high grade stenosis (80%) of the right subclavian artery.
An angiographic study of the aorta and upper and lower limbs arteries was executed which demonstrated no disease in aorta and lower limbs and the presence of total occlusion of the left subclavian artery (Fig. 2) and a sub occlusive stenosis for 8 cm of the right subclavian artery (Fig. 3).
Fig. 2.
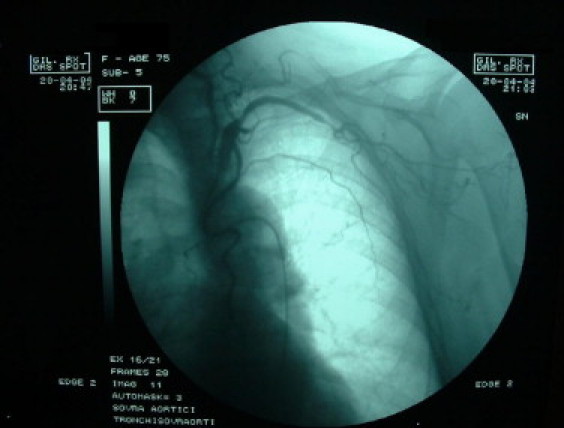
Total occlusion of the left subclavian artery.
Fig. 3.
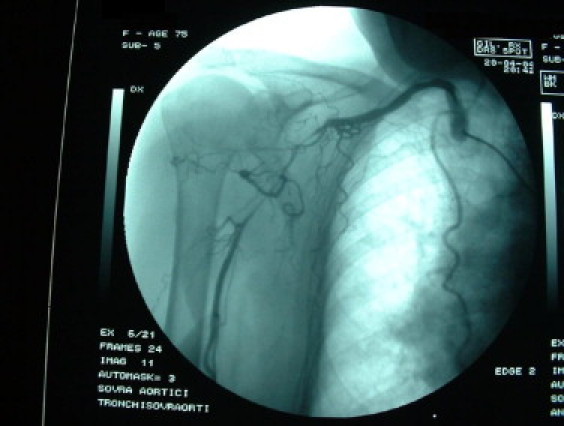
Sub occlusive stenosis of the right subclavian artery.
It was decided to use a combined surgical and endovascular treatment.
As an emergency we performed a left subclavianbrachial by-pass using a venous graft (the internal safenous vein) (Fig. 4) and the second step, after 3 days, was a percutaneous transluminal angioplasty of the right subclavian artery with a right femoral approach (Fig. 5). Angiographic examination showing good results for both (surgical and endovascular) procedures was performed before hospital discharge.
Fig. 4.
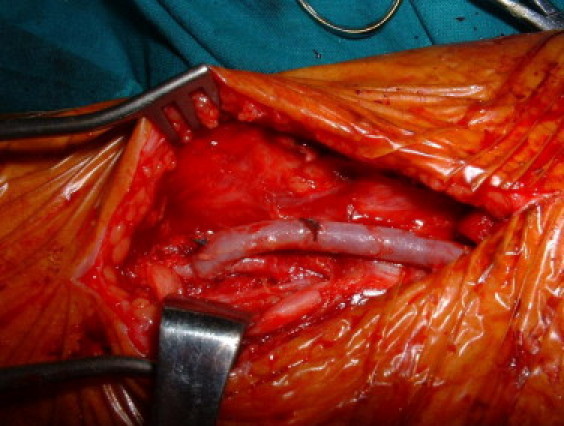
Left subclavian-brachial by-pass using a venous graft. Brachial anastomosis.
Fig. 5.
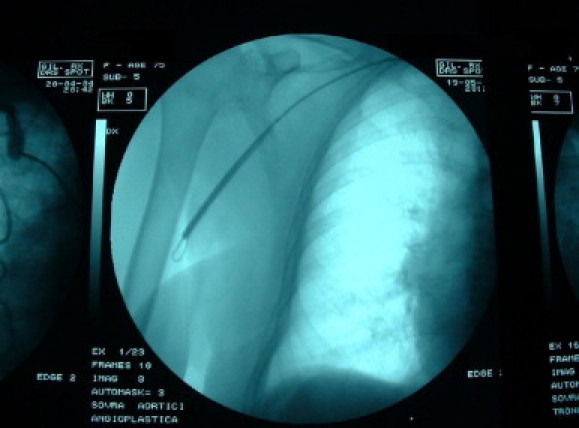
Angioplasty of the right subclavian artery.
Surgical specimens of subclavian and brachial arteries showed histopathologic features of GCA (lymphoplasmacytic panarteritis with a variable number of giant cells).
After surgical and endovascular procedures medical treatment was instituted.
Medical treatment consisted of prednisone 50 mg/day (25 mg twice/day) for 1 month, and then prednisone was decreased to 20 mg/day (10 mg twice/day) for 1 month and to 10 mg/day (5 mg twice/day) for 2 months.
We used cyclophosphamide for 3 months (2 mg/kg/day) and then methotrexate (7.5 mg/day once a week) in long-term therapy for 1 year (the same treatment in use at our department for patients with Takayasu's arteritis [4]).
During treatment (every month for 7 months and every 2 months subsequently), the following blood tests were performed: ESR and CRP as indices of inflammatory activity, blood cell count, and hepatic procollagen type III amino-terminal propeptide PIIINP for monitoring inflammation state and side effects of steroid and cytotoxic drugs.
After two months of steroid therapy ESR and CRP decreased normal range and remained low during cyclophosphamide and methotrexate treatment.
The patient was reviewed every 6 month after methotrexate long term treatment and after 4 years the patient had no signs or symptoms of relapse (Figs. 6 and 7).
Fig. 6.
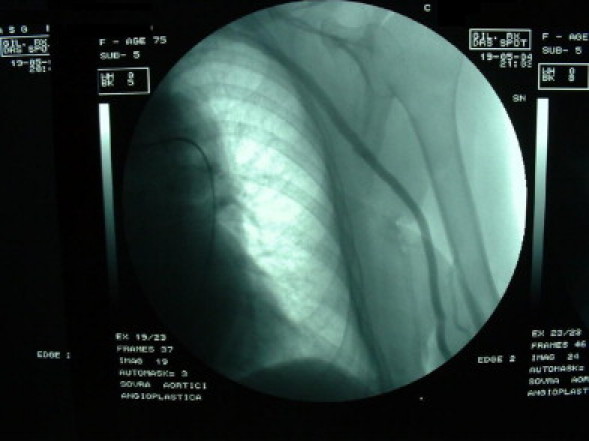
Control of the left subclavian artery after 1 month of procedure.
Fig. 7.
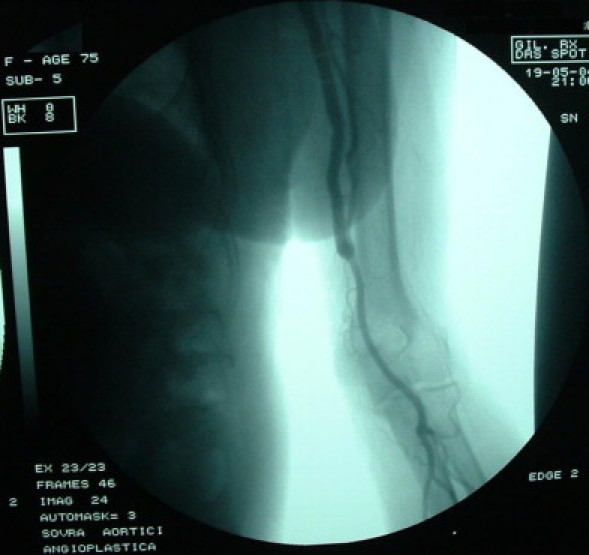
Control of the left brachial artery after 1 month of procedure.
3. Discussion
Giant cell arteritis (GCA) is a chronic vasculitis of large and medium sized arteries that almost exclusively affects elderly patients. GCA is also a heterogeneous disease with a wide range of clinical manifestations, although none that is pathognomonic because many arteries throughout the body may be affected producing symptoms and signs that are common to other medical and surgical conditions. The most common extracranial manifestation of GCA is stenosis or occlusion of the subclavian and axillary artery, with loss of arm pulses and upper limb claudication [5–7].
Symptoms and signs of systemic inflammation are present in almost all patient [8].
The relative merits of angioplasty and surgery in chronic arteritis is a topic of continuing debate. Angioplasty and surgery are both effective but the duration of results is controversial because of the natural history of the disease (progressive vascular involvement especially in areas previously unaffected). However, the problems of surgical procedure in these cases include frequent graft reocclusion, anastomotic site aneurysm and those of endovascular procedure include early restenosis.
For medical treatment there is no consensus on the dose and duration of steroid treatment after a histologic diagnosis of giant cell arteritis. Most clinicians recommend treatment with steroids in the active phase of disease. The active phase is determined by either symptomatic vasculitis or elevated markers of inflammation [9]. We administered the same treatment for patients with Takayasu's arteritis in use at our department: prednisone 50 mg/day (25 mg twice/day) for 1 month, and then decreased to 20 mg/day (10 mg twice/day) for 1 month and to 10 mg/day (5 mg twice/day) for 2 months; cyclophosphamide for 3 months (2 mg/kg/day) and then methotrexate (7.5 mg/day once a week) in longterm therapy for 1 year.
The patient after 4 years had no signs or symptoms of relapse.
It is very difficult in a case of this kind of arteritis to maintain the stability of results both for surgical or endovascular procedures but in our personal experience combining both procedures associated with long term treatment with methotrexate demonstrated a certain efficacy in avoiding relapse of the inflammatory phase and in maintaining stability of results.
Conflicts of interest statement
None declared.
Funding
None.
Ethical approval
Written consent has been obtained from the patient and is available should the editor ask to see it.
Contributor Information
Stefano de Franciscis, Email: defranci@unicz.it.
Giuseppe Roscitano, Email: giuseppe.roscitano@virgilio.it.
Raffaele Serra, Email: rserra@unicz.it.
Gianluca Buffone, Email: buffonegianluca@yahoo.it.
Attilio Cotroneo, Email: attiliocotroneo@tiscali.it.
Andrea de Franciscis, Email: sangioacchino@hotmail.com.
Diego Mastrangelo, Email: dielo@hotmail.it.
Francesco Spinelli, Email: fspinelli@unime.it.
References
- 1.Hutchinson J. Diseases of the arteries. On a peculiar form of thrombotic arteritis of the aged which is sometimes productive of gangrene. Arch Surg (Lond) 1890;1:323–329. [Google Scholar]
- 2.Horton B.T., Magath T.B., Brown G.E. An undescribed form of arteritis of the temporal vessels. Mayo Clin Proc. 1932;7:700–701. [Google Scholar]
- 3.Ostberg G. Temporal arteritis in a large necropsy series. Ann Rheum Dis. 1971;30:224–235. doi: 10.1136/ard.30.3.224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.de Franciscis S., Serra R., Luongo A., Sabino G., Puzziello A. The management of Takayasu's arteritis: personal experience. Ann Vasc Surg. 2007;21(November (6)):754–760. doi: 10.1016/j.avsg.2007.03.021. [DOI] [PubMed] [Google Scholar]
- 5.Salvarani C., Cantini F., Boiardi L., Hunder G.G. Polymyalgia rheumatica and giantcell arteritis. N Engl J Med. 2002;347:261–271. doi: 10.1056/NEJMra011913. [DOI] [PubMed] [Google Scholar]
- 6.Klein R.G., Hunder G.G., Stanson A.W., Sheps S.G. Large artery involvement in giant cell (temporal) arteritis. Ann Int Med. 1975;83:806–812. doi: 10.7326/0003-4819-83-6-806. [DOI] [PubMed] [Google Scholar]
- 7.Weyand C.M., Goronzy J.J. Medium- and large-vessel vasculitis. N Engl J Med. 2003;349:160–169. doi: 10.1056/NEJMra022694. [DOI] [PubMed] [Google Scholar]
- 8.Weyand Weyand C.M. The Dunlop–Dottridge lecture: the pathogenesis of giant cell arteritis. J Rheumatol. 2000;27:517–522. [PubMed] [Google Scholar]
- 9.Zehr K.J., Mathur A., Orszulak T.A., Mullany C.J., Hartzell V.S. Surgical treatment of ascending aortic aneurysms in patients with giant cell aortitis. Ann Thorac Surg. 2005;79:1512–1517. doi: 10.1016/j.athoracsur.2004.10.039. [DOI] [PubMed] [Google Scholar]


