Abstract
Hypertension is a major risk factor for development of stroke, coronary heart disease, heart failure, and end-stage renal disease. In a systematic review of the evidence published from 2004 to 2009, the 2010 Dietary Guidelines Advisory Committee (DGAC) concluded there was moderate evidence of an inverse relationship between the intake of milk and milk products (dairy) and blood pressure. This review synthesizes results from studies published over the past year on the relationship between dairy intake, blood pressure, and hypertension risk. The influence of dairy micronutrients including calcium, vitamin D, potassium, and phosphorous on blood pressure and incident hypertension is examined. Emerging research on bioactive dairy peptides is also reviewed. Lastly, recent evidence on effects of dairy fat content on blood pressure and hypertension risk, and the impact of inclusion of low-fat dairy in dietary patterns is also investigated.
Keywords: Hypertension (HTN), Blood Pressure (BP), Dairy, Calcium, Vitamin D, Lactotripeptides, Dietary Patterns
Introduction
Hypertension (HTN) is highly prevalent and a major risk factor for development of stroke, coronary heart disease, heart failure, and end-stage renal disease in the United States and throughout the world [1, 2]. The American Heart Association (AHA) reports that 33.6% of Americans 20 years and older have HTN and the prevalence of HTN is similar among men and women (34.4% and 32.6%, respectively). An additional 37.4% of American adults have prehypertension. Among African Americans, the incidence of HTN is one of the highest in the world, at >43% [3]. High blood pressure (BP) is the second leading preventable cause of mortality in the United States, after smoking, and BP-associated diseases are the leading causes of morbidity and mortality in the United States and worldwide [4, 5]. The Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7) reports that mortality from both ischemic heart disease and stroke increases linearly with increased BP for persons between the ages of 40 and 90 years [6]. Table 1 provides the JNC 7 stages for classifying BP.
Table 1.
Classification of blood pressure for adult
| Blood pressure classification | SBP/DBP, mm Hg |
|---|---|
| Normal | < 120 / < 80 |
| Prehypertension | SBP 120–139 or DBP 80–89 |
| Hypertension stage 1 | SBP 140–159 or DBP 90–99 |
| Hypertension stage 2 | SBP≥160 or DBP≥100 |
DBP diastolic blood pressure; SBP systolic blood pressure
(From the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report [6].)
Due to the CVD burden associated with increased BP, primary and early interventions are warranted. A healthy lifestyle, including diet, is important in both preventing increased BP over the lifespan and management of BP in people with HTN. Evidence-based national guidelines recommend diets low in salt and high in fruits, vegetables, and low-fat dairy products to reduce BP in hypertensive subjects and decrease HTN risk in healthy individuals [6, 7]. Dairy products contain high biological value protein and essential amino acids, and are a major source of calcium, phosphorous, potassium, and vitamins A and D in the American diet. Dairy products also provide magnesium, riboflavin, folate, vitamin E, and trace minerals iodine, selenium, and zinc. These macro- and micro-nutrients may individually, or in combination, be involved in reducing HTN risk. This article is a 1-year review that includes the 2010 Dietary Guidelines Advisory Committee (DGAC) evidence-based review on the effects of milk and milk products (dairy) on BP and examines areas with the most research published on this topic over the past year.
Methods
The DGAC 2010 conducted an evidence-based systematic review, assisted by United States Department of Agriculture (USDA) Nutrition Evidence Library (NEL) staff, examining the relationship between the intake of milk and milk products and BP. The DGAC systematic reviews were rigorous, transparent, minimized bias, and reproducible. The 2010 DGAC updated the 2005 DGAC review by examining literature published between June 2004 and July 2009. Inclusion criteria were human subjects ages 2 years and above; minimum of 10 subjects per study arm; dropout rate less than 20%; healthy populations and those with elevated chronic disease risk; and English language. Exclusion criteria were studies that considered milk and milk products as part of a larger dietary pattern; milk and milk products in forms not commonly consumed; hospitalized or diseased subjects; animal and in vitro studies; and articles not peer-reviewed. Search terms, databases queried, and validated criteria for assessing study quality can be accessed at http://www.nutritionevidencelibrary.gov. The DGAC search identified a total of 223 articles, and 95 were selected for review. Thirteen studies met the inclusion criteria: one systematic review, one randomized controlled trial (RCT), six prospective cohort studies, and five cross-sectional studies. The 2010 DGAC report can be accessed at http://www.dietaryguidelines.gov.
This 1-year review includes more topics than the 2010 DGAC review and covers data on individuals with HTN, trials of bioactive dairy peptides, and studies on dietary patterns such as the Dietary Approaches to Stop Hypertension (DASH) diet. Searches of Pub Med, Cochrane review, and Embase were conducted for articles published between July 2009 and December 2010. Of 163 total articles, 47 were selected for review, and 13 met the inclusion criteria: one systematic review, nine RCTs, and three prospective cohort studies. The quality of the studies was assessed using the same criteria as the 2010 DGAC review. Other relevant earlier studies are provided for background, context, and comparison with the included studies published over the past year. This article includes the following sections: the DGAC 2010 evidence-based review summary; dairy micronutrients: calcium, vitamin D, potassium, and phosphorous; bioactive dairy peptides; the benefits of low-fat versus high-fat dairy products; and dietary patterns.
2010 DGAC Evidence-Based Review of Dairy Consumption and Blood Pressure
The 2010 DGAC concluded that a moderate body of evidence suggests an inverse relationship between the intake of milk and milk products and BP. A brief summary is presented below.
One methodologically strong systematic review of epidemiologic studies, covering four primary articles on HTN, reported an inverse association between the intake of low-fat dairy products and HTN risk based on a decrease in either systolic blood pressure (SBP) and/or diastolic blood pressure (DBP) [8]. One methodologically strong randomized controlled trial (RCT) conducted among 50 normotensive, overweight men and women (25–64 years of age) in Australia showed that weight loss following energy-restricted, high-protein diets was not affected by high versus moderate dietary calcium or dairy protein versus a mixed protein source [9]. Weight loss was shown to improve both SBP and DBP, independent of dietary protein sources or calcium intake levels.
Six prospective cohort studies conducted in the United States, Spain, and the Netherlands were also reviewed. A methodologically strong report from the Women’s Health Study of 28,886 women (mean age of 54 years) conducted in the United States found that decreased HTN risk was independently associated with low-fat dairy products, calcium, and vitamin D after a 10-year follow-up [10]. The risk of HTN decreased in the higher quintiles of dietary calcium and vitamin D intake, but not with supplemental calcium or vitamin D. There was no association between high-fat dairy and risk of HTN. Of four categories of low-fat dairy products including skim milk, yogurt, cottage cheese, and sherbet, only skim milk was inversely associated with HTN risk. A methodologically strong report from the Seguimiento Universidad de Navarra (SUN) study of 6686 adults (mean age of 37 years) in Spain showed a 54% reduction in HTN in participants with the highest consumption of low-fat dairy compared to the lowest consumption after a 2-year follow-up [11]. No association between whole-fat dairy or total calcium intake and incident HTN was found. A methodologically strong report using data from 2290 elderly subjects (55–80 years of age) at high risk for cardiovascular disease (CVD) from the Prevention with Mediterranean Diet [Prevención con Dieta Mediterránea (PREDIMED)] study in Spain found a statistically significant lowering of SBP in the highest quintile of low-fat dairy intake over 12 months, but no significant relationship between high-fat dairy and BP [12].
In general, cohort studies from the Netherlands reported a less strong relationship between intake of milk and milk products and BP management. A methodologically strong report from the Rotterdam Study examined HTN risk in 2245 normotensive elderly subjects (≥55 years of age) who did not use HTN medication. At 2-year follow-up, HTN risk was significantly decreased for low-fat dairy consumption, showing low-fat dairy may decrease HTN risk at an older age [13]. However, a second methodologically strong report from the Rotterdam study of 3454 participants (20–65 years of age) found SBP and DBP showed little variation across quintiles with total dairy, whole-fat dairy, or low-fat dairy after 5 years in this young to middle-aged Dutch cohort [14]. Similarly, a methodologically strong report on a 6.4-year follow-up of 1124 elderly subjects (50–75 years) of the Hoorn study found dairy consumption was not associated with changes in SBP or DBP [15].
Five cross-sectional studies conducted in United States, France, and Iran support an inverse association between consumption of milk and milk products and BP levels [16–20]. One methodologically strong study using data from National Health and Nutrition Examination Surveys (NHANES), 1999–2004, found that among 4519 adults (≥18 years) fluid milk was inversely related to SBP and DBP, and yogurt was associated with lower SBP [16]. In contrast, cheese was positively associated with higher SBP. Another methodologically strong study using data from NHANESIII (1988–1994) on 10,872 participants (25–75 years of age) reported that SBP was not different across categories of cheese consumption, but DBP was significantly higher among men in the highest category of cheese consumption compared to non-consumers [17]. In a methodologically strong cross-sectional analysis of almost 5000 participants (25–94 years of age) from the National Heart, Lung and Blood Institute (NHLBI) Family Heart Study, an inverse association between dairy intake and the prevalence of HTN was reported, independent of calcium intake and observed mainly among participants consuming less saturated fat [18]. A methodologically strong cross-sectional analysis of 861 participants (18–74 years of age) in Iran showed an inverse relationship between dairy consumption and HTN [19]. Finally, in a methodologically neutral report from the French cohort of the Multinational Monitoring of Trends and Determinants in Cardiovascular Disease (MONICA) study of 912 men (45–64 years of age), a subgroup analysis of subjects not being treated for HTN showed a highly significant inverse association between HTN and consumption of all dairy products [20].
Dairy Micronutrients: Calcium, Vitamin D, Potassium, and Phosphorous
Calcium and Vitamin D
Bovine milk provides approximately 300 mg calcium per cup (21), representing 30% Daily Value (DV) for this nutrient (DVs were developed by the US Food and Drug Administration to help consumers compare the nutrient contents among products within the context of a total daily diet). Dairy products overall contribute about 80% of the total calcium intake in the American diet. Because a protective role of dairy against risk of HTN has been suggested, a potential role for dietary calcium in prevention of high BP is plausible and has been investigated. Early studies reported an inverse association between calcium consumption and the probability of becoming hypertensive [22]. However, a Cochrane systematic review of calcium supplementation found that evidence of a causal association between calcium supplementation and BP reduction was weak, due to poor quality trials and heterogeneity among trials [23].
The main source of vitamin D in the American diet is fortified milk. Milk in the United States is fortified with approximately 200 IU vitamin D per cup [21] (30% DV); however, other dairy products such as cheese, yogurt, and ice cream are not commonly fortified. Vitamin D is critically linked to calcium status, as 1,25[OH]2D has three major effects on calcium homeostasis: 1) calcium absorption from the small intestine; 2) calcium resorption from bone by osteoclasts; and 3) calcium resorption from the distal renal tubules. Low vitamin D intake can lead to decreased calcium bioavailability and, therefore, also stimulates the parathyroid hormone (PTH) system with results similar to those of low calcium intake. Additionally, low vitamin D activates the renin-angiotensin-aldosterone system, causing increased renin and stimulation of production of angiotensin II and aldosterone, which increase BP directly by vasoconstriction and indirectly by sodium and water retention [24]. This one-year review identified two methodologically strong RCTs on calcium and vitamin D (Table 2) [25•, 26•] and a systematic review from the Agency for Healthcare Research and Quality (AHRQ) on vitamin D and calcium, conducted in support of the Institute of Medicine (IOM) revision of Dietary Reference Intakes (DRI) [27]. One RCT, conducted in the United States, compared consumption of dairy foods, BP, and intracellular calcium in 23 stage 1 hypertensive adults in a randomized crossover trial of 5 weeks per diet phase [25]. The diets included 1) a dairy-rich, high fruit and vegetable diet (total fat and saturated fatty acid [SFA], 30% and 7% of energy, respectively, with 3.4 servings/d of dairy); 2) a high fruit and vegetable diet (total fat and SFA, 30% and 7% of energy, respectively, with 0.4 servings/d of dairy); and 3) a control average Western diet (total fat and SFA, 36% and 15% of energy, respectively, with 0.4 servings/d of dairy). SBP and DBP were significantly decreased following the high dairy, high fruit and vegetable diet or the high fruit and vegetable diet, compared to the average Western diet. Only the high dairy diet significantly lowered serum 1,25[OH]2D and intracellular calcium, compared to the high fruit and vegetable and Western diets, and this change was correlated with a significant decrease in DBP. In subgroup analyses, those in the dairy group with decreased intracellular calcium had a significantly greater decrease in DBP compared to those in the same group who did not show a change in intracellular calcium. The second RCT was a sub-study of a 2-year trial of 167 men over age 50 years in Australia [26•]. The men were randomized to either 400 mL/d of 1% milk fortified with calcium and vitamin D or no additional fortified milk. Results showed that low-fat milk providing 1000 mg calcium and 800 IU of vitamin D per day for 2 years did not change BP in this cohort.
Table 2.
Randomized controlled trials of the effects of dairy intake on blood pressure
| Author (year), quality | Subject characteristics | Intervention | Duration | Outcomes |
|---|---|---|---|---|
| Alonso et al. [44•] (2009) | 45 normotensive men and women | 3.5 servings/day whole- or low-fat dairy (milk and yogurt) | 8-week crossover trial | Whole-fat dairy ↑ SBPa [2.1 mm Hg; 95% CI, 0.1–4.0; P=0.04], NS: DBP |
| Methodologically strong | Age 18–24 y Spain | NS low- versus whole-fat dairy on SBP or DBP | ||
| Daly and Nowson [26•] (2009) | 167 white men with and without HTN | 400 mL/day 1% milk fortified with 1000 mg Ca and 800 IU vitamin D | 2-year parallel trial | NS: SBP or DBP |
| Methodologically strong | Age>50 y | Control group with no additional fortified milk | ||
| Australia | ||||
| De Leeuw et al. [38•] (2009) | 166 prehypertensive men and women | IPP+VPP dairy drinks with increasing dose: 2.3, 4.6, and 9 mg/200 g | 8-week parallel trial | ↓ DBP dose-dependently with IPP+VPP (P<0.05), NS: SBP |
| Methodologically strong | Age 35–70 y | Placebo | ||
| Netherlands | Comparable electrolyte and protein composition | |||
| He et al.[29•] (2010) | 42 men and women with untreated HTN (140–170/90–105 mm Hg) | 10 potassium bicarbonate (KHCO3) capsules/day (potassium: 0.64 g/capsule) | 4-week crossover trial | ↓ 24-hourb SBP across 3 treatments (P=0.043), NS: DBP |
| Methodologically strong | Age 17–75 y | 10 potassium chloride (KCl) capsules/day (potassium: 0.48 g/ capsule) | ||
| United Kingdom | Placebo | |||
| Hilpert et al. [25•] (2009) | 23 untreated stage 1 hypertensive white men and women | Dairy-rich, high fruit and vegetable diet (total fat and SFA, 30% and 7% energy, with 3.4 servings/day dairy) | 5-week crossover trial | ↓ SBP and DBP with high-dairy, high fruit & vegetable diet (−12.0/−7.0 mm Hg) or a high fruit & vegetable diet (−12.3/−7.2 mm Hg) vs control (−9.9/−5.3 mm Hg) (P<0.05) |
| Methodologically strong | Age 22–70 y | High fruit and vegetable diet (total fat and SFA, 30% and 7% energy, with 0.4 servings/day dairy) | ||
| United States | Control Western diet (total fat and SFA, 36% and 15% energy, with 0.4 servings/day dairy) | |||
| Jauhiainen et al. [37•] (2010) | 89 hypertensive subjects | L. helveticus fermented milk product: | 12-week parallel trial | NS: SBP or DBP |
| Methodologically strong | Age 25–55 y | 1 daily 200-mL dose (IPP 1.2 mg+VPP 1.3 mg/100 g) | ||
| Finland | 2 daily 200-mL doses (IPP 5.8 mg+VPP 6.6 mg/100 g) | |||
| Placebo | ||||
| Usinger et al. [40] (2010) | 94 prehypertensive men and women | 150 mL fermented milk (0.55 mg IPP+1.25 mg VPP) | 8-week parallel trial | NS: between-group 24-hour SBP or DBP |
| Methodologically neutral | Age 42–66 y | 300 mL fermented milk (1.1 mg IPP+2.5 mg VPP) | 300-mL group showed significant within-group ↓ in 24-hour SBP and DBP (P<0.05) | |
| Denmark | Placebo | |||
| Usinger et al. [41•] (2010) | 94 prehypertensive men and women | 150 mL fermented milk (0.55 mg IPP+1.25 mg VPP) | 8-week parallel trial | NS: SBP or DBP |
| Methodologically neutral | Age 42–66 y | 300 mL fermented milk (1.1 mg IPP+2.5 mg VPP) | ||
| Denmark | Placebo | |||
| Yamasue et al. [38•] (2010) | 30 hypertensive men and women | 200 mL sour milk with 2.66 mg VPP and 1.88 mg IPP twice daily | 8-week parallel trial | ↓ Night sleep (24-hour) SBP (120 and 119 mm Hg at 4 and 8 weeks) vs baseline (124 mm Hg) (P =0.039 at 4 weeks; P=0.027 at 8 weeks), NS: DBP |
| Methodologically neutral | Age 23–69 y | Control group not taking IPP+VPP | ↓ Morning and evening (24-hour) SBP (133 and 129 mm Hg) vs baseline (136 and 132 mm Hg) at 4 weeks (P=0.008 morning; P=0.019 evening), NS: DBP | |
| Japan |
5-minute rest, sitting blood pressure measurement unless otherwise indicated
24 hour ambulatory blood pressure measurement
DBP—diastolic blood pressure, IPP—isoleucine-proline-proline; NS—not significant; SBP—systolic blood pressure; VPP—valine-proline-proline
The AHRQ report on calcium and BP covered six systematic reviews and 69 RCTs on calcium intake from foods and/or supplements [27]. Meta-analyses within the reviews covered subjects with HTN, without HTN, and the general public with and without HTN. Overall, the AHRQ report concluded that for individuals between 19 and 50 years, the majority of studies show no effect of calcium supplementation on normotensive individuals, but for hypertensive individuals there was significant lowering of SBP, but not DBP. The review also included five longitudinal cohort studies on calcium intake and HTN incidence. Of these, only the Women’s Health Study, with a 10-year follow-up, found a highly significant trend across quintiles of calcium consumption, with significantly higher rates of HTN among women in the lowest quintile of calcium intake [11]. Based on the five longitudinal studies, the AHRQ report concluded that evidence of an association between calcium intake and HTN incidence was inconsistent.
The AHRQ report on vitamin D and HTN and BP included cohort studies on the association between serum 1,25[OH]2D concentrations and incidence of HTN, and RCTs on vitamin D intake and changes in BP [27]. No systematic reviews that evaluated the association of vitamin D intake and HTN risk were identified. The AHRQ synopsis on HTN incidence focused on a combined analysis of subsets from the Health Professionals Follow-Up and the Nurses’ Health studies. This combined analysis showed a higher incidence of HTN at 4 years in men and women with low baseline serum vitamin D (1,25[OH]2D< 37.5 nmol/L); this was also seen in men, but not women, at 8 years. Only three RCTs were identified and these were conducted in Germany, the United Kingdom, and India. These trials varied widely in the dose of vitamin D (800 IU daily to 120,000 IU every 2 weeks), age range and sizes of subject groups, and the SBP and DBP outcomes. No conclusions were reached based on these trials.
Potassium
Milk provides approximately 350 mg of potassium per cup (11% DV) [21]. High dietary potassium intake is associated with lower BP and maintaining adequate intake of dietary potassium (>3500 mg/d) is recommended for the primary prevention of HTN by the JNC 7 [6]. Supplementation with potassium does not appear to provide added benefit, as a Cochrane systematic review on potassium supplementation for the management of HTN concluded that potassium supplementation in hypertensive individuals did not significantly reduce BP [28]. Sodium and potassium have opposing effects on arterial vasodilation. Increased dietary sodium intake leads to decreased endothelial synthesis of nitric oxide (NO), a vasodilator, and increased plasma levels of dimethyl-L-arginine, an inhibitor of NO synthesis. Increased potassium intake raises plasma potassium levels and this is associated with endothelium-dependent vasodilation via stimulation of the sodium pump (Na-K ATPase) and opening of potassium channels of the Na-K ATPase [2].
Over the past year, there have been no new reports on the association between potassium in dairy products and BP or HTN risk. However, a methodologically strong RCT on potassium treatment was identified. This was a 12-week randomized crossover trial with 42 adult men and women with untreated HTN conducted in the United Kingdom (Table 2) [29•]. The interventions included 4-week crossovers of placebo, potassium chloride, and potassium bicarbonate. Although no significant differences in resting BP were reported, a small but significant difference in 24-hour ambulatory and average daytime SBP was reported across the three treatment groups. Additionally, vascular endothelial function, arterial distensibility, and left ventricular diastolic function were significantly improved with both potassium chloride and potassium bicarbonate treatment. The potassium intakes achieved by both treatments were in the range of the Institute of Medicine’s recommendation for potassium, which was raised to 4700 mg/d in the 2005 Dietary Reference Intake (DRI).
Phosphorous
Phosphorous, another mineral abundant in milk, is associated with calcium as a salt of calcium phosphate. One cup of milk contains approximately 230 mg phosphorous (23% DV) [21]. The International Study of Macro- and Micro-Nutrients and BP (INTERMAP), a cross-sectional epidemiologic study of 17 population samples from Japan, China, the United Kingdom, and the United States, found that dietary phosphorous was inversely associated with BP, and correction for dietary and non-dietary confounders did not change this association [30]. In addition, dietary calcium and magnesium, correlated with phosphorous, were inversely associated with BP.
In the past year, one methodologically strong report was identified that examined two prospective cohort studies on phosphorous and HTN (Table 3) [31•]. Alonso et al. [31•] examined phosphorous intake, BP levels, and HTN risk in two prospective US cohort studies, the Atherosclerosis Risk in Communities (ARIC) study and the Multi-Ethnic Study of Atherosclerosis (MESA). The ARIC study included 15,792 middle-aged men and women in four communities in the United States. The MESA study included 6814 middle-aged and elderly men and women from six communities in the United States. After an average 6.2 years of follow-up of the combined cohort, phosphorus from dairy products, but not from other sources, was associated with lower baseline BP and reduced risk of incident HTN. This may indicate that the benefits of phosphorous intake are dependent on interactions with other dairy components.
Table 3.
Prospective cohort studies on association between dairy intake and blood pressure change or hypertension risk
| Author (year), quality | Design/cohort | Outcomes measured | Duration | Findings | Adjustments |
|---|---|---|---|---|---|
| Alonso et al. [45•] (2009) | ARIC study subgroup: | Association between dairy product intake and changes in BP over time assessed by general linear models for repeated measures | 9-year follow-up | ↑ SBP 2.7 mm Hg less (95% CI, −0.3 to 6.0) in whites consuming>3 low-fat milk servings/day vs those consuming<1 serving/week (P for trend=0.01), NS: DBP | Independent variables: age, sex, study center, BMI, waist/hip, physical activity, smoking, total energy, alcohol, Na, K, fruits, vegetables, dairy products, and study visit |
| Methodologically strong | 6912 Caucasian and 1296 African American normotensive men and women | For African-Americans, whole-fat or low-fat dairy NS: DBP or DBP | |||
| Aged 45–64 years | |||||
| United States | |||||
| Alonso et al. [31•] (2010) | ARIC study: | Baseline cross-sectional | Baseline | 3345 diagnoses of HTN | Initial model included quintiles of P intake, with age, sex, and race as adjustment variables |
| Methodologically strong | 15,792 men and women | SBP and DBP longitudinal prospective | Average 6.2- year follow-up combined cohort | Phosphorous (P) inversely associated with ↓ HTN risk (HR: 0.80 [95% CI, 0.80–1.00]; P trend=0.02); adjustment non-dietary (HR 1.01 [95% CI, 0.82–1.23], P trend=0.88 | 2nd model: study site, BMI, waist circumference, education, income, physical activity, glomerular filtration rate, cigarettes, alcohol, and energy intake |
| White and African American | Association of phosphorous intake and HTN risk hazard ratio | P from dairy but not other sources associated with ↓ baseline BP and ↓ HTN risk | 3rd model: Ca, K, Mg, Na, vitamin D, fruits, vegetables, and whole grains | ||
| Aged 45–64 years | HR: 0.86 [95% CI, 0.76–0.97]; P trend=0.01) for P from dairy and 1.04 (95% CI, 0.93–1.17; P trend=0.48) for P from other foods | ||||
| United States | |||||
| MESA Study: | |||||
| 6814 men and women | |||||
| White, African American, Hispanic, and Chinese American | |||||
| Aged 45–84 y | |||||
| United States | |||||
| Toledo et al. [50•] (2010) | SUN study cohort: | Cohort assessed on adherence to 15 different healthy food patterns with score | 4.6-year follow-up | 640 diagnoses of HTN | Cox regression model adjusted for age and sex |
| Methodologically strong | 10,800 men and women initially free of hypertension | Measured HR for HTN risk according to adherence to diet pattern | Higher adherence to DASH associated with ↓ HTN risk; HR=0.48 (95% CI, 0.21–1.09), P trend=0.02 | 2nd model adjusted for BMI, family history of HTN, energy intake, smoking, physical activity | |
| Age 25–54 years | No association between other diet patterns and risk | ||||
| Spain |
BMI body mass index; BP blood pressure; DBP diastolic blood pressure; HTN hypertension; NS not significant; SBP systolic blood pressure
Bioactive Dairy Peptides
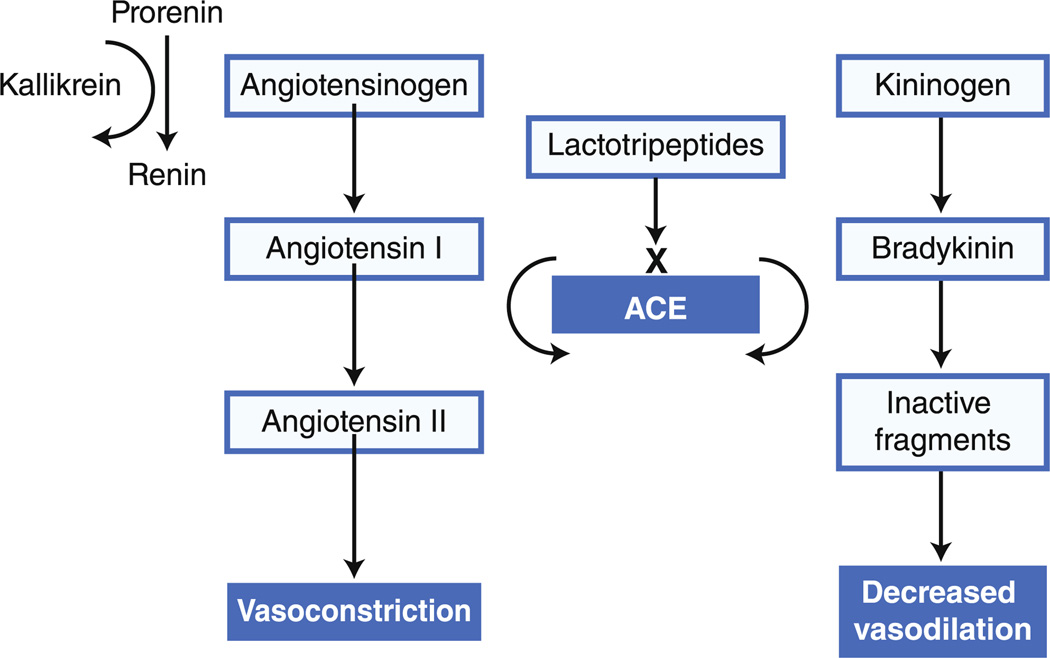
Milk, a good source of high biological value protein, is particularly rich in essential and branched-chain amino acids. Protein metabolites, such as small peptides, have been shown to have bioactive properties that affect BP [32–34]. A significant emerging area of investigation involves these small peptides derived from milk protein, primarily casein and whey protein (casein is about 80% of milk protein). Casein facilitates calcium and phosphate absorption in the small intestine and is the main substrate for production of bioactive peptides. Small dairy peptides are the product of either digestion of milk protein in the human small intestine, with the peptides absorbed intact, or lactobacilli fermentation of milk. Certain of these bioactive molecules, referred to as lactotripeptides, have been studied in detail (eg, Ile-Pro-Pro [IPP] and Val-Pro-Pro [VPP]). These lactotripeptides inhibit angiotensin-converting enzyme (ACE) in vitro and are hypothesized to lower BP via this mechanism (Fig. 1) [32, 33]. Other potential mechanisms for peptides from both milk casein and whey proteins are opioid-like activities that can decrease BP [34]. In 2008, a meta-analysis of 15 RCTs with a total of 826 subjects that examined fermented milk or milk-derived IPP and VPP showed a positive association between lactotripeptides and lower BP. Most of the 15 trials were conducted with hypertensive individuals; however, two studies were conducted among prehypertensive individuals [35]. Another recent review of the evidence from 18 RCTs that tested lactotripeptides IPP and VPP (in either milk drinks or tablets) showed lactotripeptides were effective in reducing elevated BP but not normotensive BP. Effective doses for lactotripeptides ranged from 3.07 to 52.5 mg/d [36].
Over the past year, five RCTs were identified on the effects of lactotripeptides on BP (Table 2). A methodologically strong RCT of 89 hypertensive subjects conducted in Finland showed that treatment with high dose tripeptides for 12 weeks resulted in a significant decrease in arterial stiffness, measured as augmentation index (AIx), but no significant change in SBP, DBP, or in endothelial function [37•]. In a methodologically neutral, small RCT in Japan, 30 hypertensive participants were provided sour milk for 8 weeks. Results showed that morning and evening home SBP was significantly decreased at 4 weeks, and night sleep SBP was significantly decreased at 8 weeks. It was also noted that reduced intake of salt may further increase the BP-lowering effects of lactotripeptides in hypertensive subjects [38•]. A methodologically strong, large parallel trial of 166 prehypertensive subjects in the Netherlands showed that lactotripeptides in dairy drinks with comparable electrolyte and protein composition lowered DBP in a dose-dependent manner [39•]. In two separate reports from one methodologically neutral RCT, Usinger et al. measured the effects of fermented milk on ambulatory BP [40] and markers of the renin-angiotensin-aldosterone system [41•] in 94 prehypertensive subjects in Denmark. Participants were randomized to three treatment groups, with daily intake of 150 mL or 300 mL of fermented milk or placebo. The results showed no significant differences between groups in SBP or DBP with repeated 24-hour ambulatory BP measurements and no inhibition of ACE after 8 weeks, although there was a decrease in sympathetic activity. However, the 300-mL milk group showed significant within-group reduction in SBP and DBP at 8 wks by 24-hour ambulatory measures.
Overall, the recently published RCTs on fermented milk or lactotripeptides show variable effects on SBP and DBP and related vascular outcomes in both hypertensive and prehypertensive individuals.
Benefits of Low-Fat versus Whole-Fat Dairy
Possible relative benefits of consuming low-fat dairy versus whole-fat dairy involve decreased saturated fatty acids (SFA) in the milk. SFA present in triglycerides account for 95% of the lipid fraction of whole milk [42]. The main dairy SFA include short-chain butyric (4:0), caprylic (8:0), and capric (10:0) acids, and medium and longer chain lauric (12:0), myristic (14:0), and palmitic (16:0) acids. The medium and longer chain fatty acids increase serum low-density lipoprotein cholesterol and are atherogenic. Atherosclerotic plaque development causes increased vascular endothelial cell dysfunction, increased vascular smooth muscle cell growth, and interstitial collagen synthesis, all of which decrease vascular plasticity and increase vascular resistance.
Many of the large prospective cohort studies included in the 2010 DGAC review covered the literature from 2004 to 2009 and reported benefits from consumption of low-fat versus whole-fat dairy products. The SUN cohort study reported a 54% reduction in incident HTN among individuals with high consumption of low-fat, but not whole-fat, dairy products [12]. In the Women’s Health Study, the risk of HTN was inversely associated with total dairy and low-fat dairy consumption, but not whole-fat dairy consumption [11]. Similarly, middle-aged subjects with high cardiovascular risk in the PREDIMED study exhibited an inverse association between low-fat dairy intake and SBP and a significant decrease in risk of HTN comparing the lowest versus the highest quintile of low-fat dairy intake [12]. No association was found with whole-fat dairy [13]. Other studies that preceded the time range of the 2010 DGAC report included at-risk cohorts not represented in the DGAC review, such as the Coronary Artery Risk Development in Young Adults (CARDIA) study of overweight African Americans and whites. In this study, total dairy intake, particularly low-fat dairy intake, was inversely associated with metabolic syndrome incidence, including high BP, in both groups [43].
The 1-year review identified one methodologically strong RCT (Table 2) and one methodologically strong prospective cohort study on low-fat versus whole-fat dairy (Table 3). The RCT was conducted among 45 normotensive young men and women in Spain who received 3.5 servings/day of whole-fat or low-fat dairy products (milk and yogurt), in addition to their usual diet during an 8-week crossover trial. Whole-fat dairy intake significantly increased SBP and body weight but not DBP. Low-fat dairy, on the other hand, did not change BP or body weight significantly after the intervention. Overall, there was no significant difference in the effect of low-fat versus whole-fat dairy on BP, although whole-fat dairy increased body weight significantly compared to low-fat dairy [44•].
Alonso et al. [45•] reported further results from the ARIC Study, involving an analysis of 6912 Caucasian and 1296 African-American non-hypertensive men and women from four communities in the United States. After 9 years, SBP in Caucasians consuming more than 3 low-fat dairy servings per day increased significantly less than in those consuming less than 1 serving per week. However, among African Americans, neither whole-fat nor low-fat dairy consumption was associated with changes in BP over time. The investigators noted that the results in the African American subgroup should be interpreted cautiously, given the results of other cohort studies, such as the CARDIA study cited above and the DASH trial discussed below.
Dietary Patterns
Examining dietary patterns rather than only individual nutrients or food groups can help determine the effects of a combination of nutrients as they occur together in foods as consumed. The Dietary Approaches to Stop Hypertension (DASH) trial provided landmark evidence that nutrients and also food groups and whole eating patterns can influence blood pressure [46]. This randomized crossover trial tested three patterns: 1) a control Western diet; 2) a diet high in fruits and vegetables; and 3) a combination diet with high fruits and vegetables and low-fat dairy. The combination DASH diet had lower amounts of total fat, SFA, and cholesterol and provided potassium, magnesium, and calcium at levels approximating the 75th percentile of US consumption, with high levels of fiber and protein. There were no differences in sodium intake among the three arms of the trial (~3 g/d). Both the high fruits and vegetables diet and the combination diet decreased BP in prehypertensive and stage 1 HTN individuals, as well as in persons with isolated systolic HTN. The benefits were greatest (ie, the largest) for clinically significant decreases in SBP and DBP in the combination diet group, which added 2 to 3 servings of low-fat dairy per day. A subgroup analysis showed that BP-lowering effects were more pronounced in hypertensive and African American participants [47]. Additionally, decreased sodium intake plus the DASH diet reduced BP even further in stage 1 hypertensive individuals [48], and this was maintained for over 1 year despite a gradual increase in sodium intake over that time period [49].
The 1-year review identified one methodologically strong prospective cohort study, an update of the SUN study that followed 10,800 men and women who were initially free of HTN for a median of 4.6 years in Spain (Table 3) [50•]. Over this period, 640 participants reported a first diagnosis of HTN, and level of adherence to 15 different a priori–defined healthy food patterns was scored. The 15 dietary patterns included the DASH combination diet, five Mediterranean diet–related patterns, the Diet Quality Index-International, the Recommended Food Score, the Quantitative Index for Dietary Diversity (both total energy intake and grams of intake), the Healthy Eating Index, the Alternate Healthy Eating Index, and the Dietary Guidelines for Americans Adherence Index. Overall, adherence to only one dietary pattern, the DASH combination diet pattern, was significantly associated with lower risk for developing HTN. None of the other healthy food patterns, including the five Mediterranean diet–related patterns, showed this inverse association with HTN risk. Additionally, there was no association between lower risk of HTN and whole-fat dairy consumption.
Conclusions
The 2010 DGAC Report reviewed literature from 2004 to 2009 and concluded there was moderate evidence of an inverse relationship between the intake of milk and milk products and blood pressure. This updated, 1-year review (2009–2010) reports on vitamin D, calcium, potassium, phosphorous, bioactive small peptides, low-fat dairy products, and low-fat dairy dietary patterns and provides further evidence that dairy intake may improve BP and decrease HTN risk. The unique dairy micronutrient composition together with low sodium, high protein, and bioactive lactotripeptides may offer combined protective effects.
The 2010 DGAC advocated new RCTs to determine whether dairy products alter blood pressure, noting the potential for confounding adding complexity to this research. Also, additional investigation is warranted on potential impact of bioactive small peptides derived from milk proteins. Results from current RCTs on fermented milk or lactotripeptides are variable. Finally, ongoing analyses from the DASH study showed long-term BP benefits from adherence to the combination diet with low-fat dairy, but not all studies and populations report similar results. Because dairy fat is primarily saturated fat, including medium and longer chain fatty acids that are atherogenic and potentially counter the benefits of dairy consumption, further research is required to determine risk/benefit of dairy-specific SFA within the overall context of the eating pattern.
Fig. 1.
Role of angiotensin-converting enzyme (ACE) in reninangiotensin and kininogen-bradykinin system. ACE removes the C-terminal dipeptide from the decapeptide angiotensin I to produce angiotensin II. Angiotensin II is a vasoconstrictor and stimulates aldosterone release, which leads to sodium and water retention by the kidneys and increased blood volume. ACE also inactivates the vasodilator bradykinin by cleaving the C-terminal dipeptide and releasing inactive fragments, further contributing to increased blood pressure. Lactotripeptides competitively bind to the active site of ACE and inhibit ACE activity
Footnotes
Disclosure The authors report no potential conflicts of interest relevant to this article.
Contributor Information
Mary M. McGrane, Email: mary.mcgrane@cnpp.usda.gov, US Department of Agriculture, Center for Nutrition Policy and Promotion, 3101 Park Center Drive, Room 1034, Alexandria, VA 22302 1594, USA.
Eve Essery, Email: Eve.Essery@cnpp.usda.gov, US Department of Agriculture, Center for Nutrition Policy and Promotion, 3101 Park Center Drive, Room 1034, Alexandria, VA 22302 1594, USA.
Julie Obbagy, Email: Julie.Obbagy@cnpp.usda.gov, US Department of Agriculture, Center for Nutrition Policy and Promotion, 3101 Park Center Drive, Room 1034, Alexandria, VA 22302 1594, USA.
Joan Lyon, Email: lyonnessj@hughes.net, US Department of Agriculture, Center for Nutrition Policy and Promotion, 3101 Park Center Drive, Room 1034, Alexandria, VA 22302 1594, USA.
Patricia MacNeil, Email: patricia.macneil@cnpp.usda.gov, US Department of Agriculture, Center for Nutrition Policy and Promotion, 3101 Park Center Drive, Room 1034, Alexandria, VA 22302 1594, USA.
Joanne Spahn, Email: Joanne.spahn@fns.usda.gov, US Department of Agriculture, Center for Nutrition Policy and Promotion, 3101 Park Center Drive, Room 1034, Alexandria, VA 22302 1594, USA.
Linda Van Horn, Email: lvanhorn@northwestern.edu, Department of Preventive Medicine, Northwestern University, 680 N Lake Shore Drive Ste 1400, Chicago, IL 60611, USA.
References
Papers of particular interest, published recently, have been highlighted as:
• Of importance
- 1.Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988–2008. JAMA. 2010;303(20):2043–2050. doi: 10.1001/jama.2010.650. [DOI] [PubMed] [Google Scholar]
- 2.Lawes CM, Vander Hoorn S, Rodgers A. International Society of Hypertension. Global burden of blood-pressure-related disease, 2001. Lancet. 2008;371(9623):1513–1518. doi: 10.1016/S0140-6736(08)60655-8. [DOI] [PubMed] [Google Scholar]
- 3.Lloyd-Jones D, Adams RJ, Brown TM, et al. American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics–2010 update: a report from the American Heart Association. Circulation. 2010;121(7):e46–e215. doi: 10.1161/CIRCULATIONAHA.109.192667. [DOI] [PubMed] [Google Scholar]
- 4.Danaei G, Ding EL, Mozaffarian D, et al. The preventable causes of death in the United States: comparative risk assessment of dietary, lifestyle, and metabolic risk factors. PLoS Med. 2009;6(4) doi: 10.1371/journal.pmed.1000058. e1000058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Appel LJ, Frohlich ED, Hall JE, et al. The Importance of Population-Wide Sodium Reduction as a Means to Prevent Cardiovascular Disease and Stroke: A Call to Action From the American Heart Association. Circulation. 2011 Jan 13; doi: 10.1161/CIR.0b013e31820d0793. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 6.Chobanian AV, Bakris GL, Black HR, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289:2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 7.Whelton PK, He J, Appel LJ, et al. National High Blood Pressure Education Program Coordinating Committee. Primary prevention of hypertension: clinical and public health advisory from The National High Blood Pressure Education Program. JAMA. 2002;288(15):1882–1888. doi: 10.1001/jama.288.15.1882. [DOI] [PubMed] [Google Scholar]
- 8.Alvarez-León EE, Román-Viñas B, Serra-Majem L. Dairy products and health: a review of the epidemiological evidence. Br J Nutr. 2006;96 Suppl 1:S94–S99. doi: 10.1079/bjn20061709. [DOI] [PubMed] [Google Scholar]
- 9.Bowen J, Noakes M, Clifton PM. Effect of calcium and dairy foods in high protein, energy-restricted diets on weight loss and metabolic parameters in overweight adults. Int J Obes (Lond) 2005;29(8):957–965. doi: 10.1038/sj.ijo.0802895. [DOI] [PubMed] [Google Scholar]
- 10.Wang L, Manson JE, Buring JE, et al. Dietary intake of dairy products, calcium, and vitamin D and the risk of HTN in middle-aged and older women. HTN. 2008;51(4):1073–1079. doi: 10.1161/HYPERTENSIONAHA.107.107821. [DOI] [PubMed] [Google Scholar]
- 11.Alonso A, Beunza JJ, Delgado-Rodríguez M, et al. Low-fat dairy consumption and reduced risk of HTN: The Seguimiento Universidad de Navarra (SUN) cohort. Am J Clin Nutr. 2005 Nov;82(5):972–979. doi: 10.1093/ajcn/82.5.972. [DOI] [PubMed] [Google Scholar]
- 12.Toledo E, Delgado-Rodríguez M, Estruch R, et al. Low-fat dairy products and blood pressure: Follow-up of 2290 older persons at high cardiovascular risk participating in the PREDIMED study. Br J Nutr. 2009;101(1):59–67. doi: 10.1017/S0007114508981496. [DOI] [PubMed] [Google Scholar]
- 13.Engberink MF, Hendriksen MA, Schouten EG, et al. Inverse association between dairy intake and HTN: The Rotterdam Study. Am J Clin Nutr. 2009;89(6):1877–1883. doi: 10.3945/ajcn.2008.27064. [DOI] [PubMed] [Google Scholar]
- 14.Engberink MF, Geleijnse JM, de Jong N, et al. Dairy intake, blood pressure, and incident HTN in a general Dutch population. J. Nutr. 2009;139(3):582–587. doi: 10.3945/jn.108.093088. [DOI] [PubMed] [Google Scholar]
- 15.Snijder MB, van Dam RM, Stehouwer CD, et al. A prospective study of dairy consumption in relation to changes in metabolic risk factors: The Hoorn Study. Obesity (Silver Spring) 2008;16(3):706–709. doi: 10.1038/oby.2007.93. [DOI] [PubMed] [Google Scholar]
- 16.Beydoun MA, Gary TL, Caballero BH, et al. Ethnic differences in dairy and related nutrient consumption among US adults and their association with obesity, central obesity, and the metabolic syndrome. Am J Clin Nutr. 2008;87(6):1914–1925. doi: 10.1093/ajcn/87.6.1914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Houston DK, Driver KE, Bush AJ, et al. The association between cheese consumption and cardiovascular risk factors among adults. J Hum Nutr Diet. 2008;21(2):129–140. doi: 10.1111/j.1365-277X.2008.00853.x. [DOI] [PubMed] [Google Scholar]
- 18.Djoussé L, Pankow JS, Hunt SC, et al. Influence of saturated fat and linolenic acid on the association between intake of dairy products and blood pressure. HTN. 2006;48(2):335–341. doi: 10.1161/01.HYP.0000229668.73501.e8. [DOI] [PubMed] [Google Scholar]
- 19.Azadbakht L, Mirmiran P, Esmaillzadeh A, et al. Dairy consumption is inversely associated with the prevalence of the metabolic syndrome in Tehranian adults. Am J Clin Nutr. 2005;82(3):523–530. doi: 10.1093/ajcn.82.3.523. [DOI] [PubMed] [Google Scholar]
- 20.Ruidavets JB, Bongard V, Simon C, et al. Independent contribution of dairy products and calcium intake to blood pressure variations at a population level. J Hypertens. 2006;24(4):671–681. doi: 10.1097/01.hjh.0000217849.10831.16. [DOI] [PubMed] [Google Scholar]
- 21.U.S. Department of Agriculture, Agricultural Research Service. USDA National Nutrient Database for Standard Reference, Release 23. Nutrient Data Laboratory Home Page. 2010 http://www.arsusda.gov/ba/bhnrc/ndl.
- 22.McCarron DA, Morris CD, Henry HJ, et al. Blood pressure and nutrient intake in the United States: an analysis of the Health and Nutrition Examination Survey I. Science. 1984;224:1392–1398. doi: 10.1126/science.6729459. [DOI] [PubMed] [Google Scholar]
- 23.Dickinson HO, Nicolson DJ, Cook JV, et al. Calcium supplementation for the management of primary hypertension in adults. Cochrane Database Syst Rev. 2006 Apr 19;(2) doi: 10.1002/14651858.CD004639.pub2. CD004639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pilz S, Tomaschitz A, Ritz E, et al. Vitamin D status and arterial hypertension: a systematic review. Medscape Nat Rev Cardiol. 2009;6(10):621–630. doi: 10.1038/nrcardio.2009.135. [DOI] [PubMed] [Google Scholar]
- 25. Hilpert KF, West SG, Bagshaw DM, et al. Effects of dairy products on intracellular calcium and blood pressure in adults with essential HTN. J Am Coll Nutr. 2009;28(2):142–149. doi: 10.1080/07315724.2009.10719765.. This RCT compared consumption of dairy foods, BP, intracellular calcium in 23 stage 1 hypertensive adults in a 5-week crossover trial conducted in the United States The diets included 1) a dairyrich, high fruit and vegetable diet; 2) a high fruit and vegetable diet; 3) an average Western diet. SBP and DBP were significantly decreased following either the high dairy, high fruit and vegetable diet or the high fruit and vegetable diet compared to the Western diet. Only the high dairy diet significantly lowered 1,25[OH]2D and intracellular calcium.
- 26. Daly RM, Nowson CA. Long-term effect of calcium-vitamin D(3) fortified milk on blood pressure and serum lipid concentrations in healthy older men. Eur J Clin Nutr. 2009;63(8):993–1000. doi: 10.1038/ejcn.2008.79.. This RCT was a substudy of a 2-year trial of 167 men over 50 years of age in Australia. The men were randomized to either 400 mL/day of 1% milk fortified with calcium and vitamin D or control group with no additional fortified milk. Results showed that low-fat milk providing 1000 mg calcium and 800 IU of vitamin D per day for 2 years did not change BP in this cohort.
- 27.Chung M, Balk EM, Brendel M, et al. Evidence Report/Technology Assessment No. 183. Rockville, MD: Agency for Healthcare Research and Quality; 2009. Aug, Vitamin D and Calcium: Systematic Review of Health Outcomes. (Prepared by Tufts Evidence-based Practice Center under Contract, No. 290-2007-10055-I). AHRQ Publication, No. 09-E015. [PMC free article] [PubMed] [Google Scholar]
- 28.Dickinson HO, Nicolson D, Campbell F, et al. Potassium supplementation for the management of primary hypertension in adults. Cochrane Database of Systematic Reviews. 2006;(Issue 3) doi: 10.1002/14651858.CD004641.pub2. Art. No.: CD004641. [DOI] [PubMed] [Google Scholar]
- 29. He FJ, Marciniak M, Carney C, et al. Effects of potassium chloride and potassium bicarbonate on endothelial function, cardiovascular risk factors, and bone turnover in mild hypertensives. HTN. 2010;55(3):681–688. doi: 10.1161/HYPERTENSIONAHA.109.147488.. This is RCT on potassium and HTN involving a 12-week randomized crossover trial with 42 adult men and women with untreated HTN. The RCT was conducted to test potassium chloride and potassium bicarbonate treatment, with a 4-week crossover of placebo, potassium chloride, and potassium bicarbonate. No significant differences in BP were reported, but vascular endothelial function, arterial distensibility, and left ventricular diastolic function were significantly improved with both potassium chloride and potassium bicarbonate supplementation.
- 30.Elliott P, Kesteloot H, Appel LJ, et al. INTERMAP Cooperative Research Group. Dietary phosphorus and blood pressure: international study of macro- and micro-nutrients and blood pressure. Hypertension. 2008;51(3):669–675. doi: 10.1161/HYPERTENSIONAHA.107.103747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Alonso A, Nettleton JA, Ix JH, et al. Dietary Phosphorus, Blood Pressure, and Incidence of HTN in the Atherosclerosis Risk in Communities Study and the Multi-Ethnic Study of Atherosclerosis HTN. 2010;55:776–784. doi: 10.1161/HYPERTENSIONAHA.109.143461.. This article examined phosphorous intake, BP levels, and HTN risk in two prospective US cohort studies: the Atherosclerosis Risk in Communities (ARIC) study and the Multi-Ethnic Study of Atherosclerosis (MESA). The ARIC study included 15,792 middle-aged men and women in four communities. The more recent MESA study included 6814 middle-aged and elderly men and women from six communities. After an average 6.2 years of follow-up of the combined cohort, phosphorus from dairy products, but not from other sources, was associated with lower baseline BP and reduced risk of incident HTN.
- 32.Ricci I, Artacho R, Olalla M. Milk protein peptides with angiotensin I-converting enzyme inhibitory (ACEI) activity. Crit Rev Food Sci Nutr. 2010;50(5):390–402. doi: 10.1080/10408390802304198. [DOI] [PubMed] [Google Scholar]
- 33.Savica V, Bellinghieri G, Kopple JD. The effect of nutrition on blood pressure. Annu Rev Nutr. 2010;30:365–401. doi: 10.1146/annurev-nutr-010510-103954. [DOI] [PubMed] [Google Scholar]
- 34.Jauhiainen T, Korpela R. Milk peptides and blood pressure. J Nutr. 2007;137(3) Suppl 2:825S–829S. doi: 10.1093/jn/137.3.825S. [DOI] [PubMed] [Google Scholar]
- 35.Pripp AH. Effect of peptides derived from food proteins on blood pressure: a meta-analysis of randomized controlled trials. Food Nutr Res. 2008;52 doi: 10.3402/fnr.v52i0.1641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Boelsma E, Kloek J. Lactotripeptides and antihypertensive effects: a critical review. Br J Nutr. 2009;101(6):776–786. doi: 10.1017/S0007114508137722. [DOI] [PubMed] [Google Scholar]
- 37. Jauhiainen T, Rönnback M, Vapaatalo H, et al. Long-term intervention with Lactobacillus helveticus fermented milk reduces augmentation index in hypertensive subjects. Eur J Clin Nutr. 2010;64(4):424–431. doi: 10.1038/ejcn.2010.3.. This RCT of 89 hypertensive subjects conducted in Finland showed that treatment with high-dose tripeptides for 12 weeks resulted in a significant decrease in arterial stiffness, measured as augmentation index (AIx), but no change in endothelial function. There were no significant changes in blood pressure between groups.
- 38. Yamasue K, Morikawa N, Mizushima S, et al. The blood pressure lowering effect of lactotripeptides and salt intake in 24-h ambulatory blood pressure measurements. Clin Exp Hypertens. 2010;32(4):214–220. doi: 10.3109/10641963.2010.491885.. In this RCT in Japan, 30 hypertensive participants were provided sour milk for 8 weeks and the BP-lowering effects of lactotripeptides were documented. It was noted that reduced intake of salt may further increase the BP-lowering effects of lactotripeptides in hypertensive subjects.
- 39. de Leeuw PW, van der Zander K, Kroon AA, et al. Dose-dependent lowering of blood pressure by dairy peptides in mildly hypertensive subjects. Blood Press. 2009;18(1–2):44–50. doi: 10.1080/08037050902761209.. This RCT of 166 prehypertensive subjects in the Netherlands, with IPP and VPP dairy drinks for 8 weeks, showed that lactotripeptides in dairy drinks with comparable electrolyte and protein composition lowered DBP in a dose-dependent manner.
- 40.Usinger L, Ibsen H, Linneberg A, et al. Human in vivo study of the renin-angiotensin-aldosterone system and the sympathetic activity after 8 weeks daily intake of fermented milk. Clin Physiol Funct Imaging. 2010;30(2):162–168. doi: 10.1111/j.1475-097X.2009.00921.x. [DOI] [PubMed] [Google Scholar]
- 41. Usinger L, Jensen LT, Flambard B, et al. The antihypertensive effect of fermented milk in individuals with prehypertension or borderline hypertension. J Hum Hypertens. 2010;24(10):678–683. doi: 10.1038/jhh.2010.4.. In two separate reports from one RCT, the authors measured the effects of fermented milk on ambulatory BP and markers of the rennin-angiotensin-aldosterone system in 94 prehypertensive subjects in Denmark. Participants were randomized to three treatment groups with daily intake of 150 mL or 300 mL of fermented milk or placebo. The results showed no significant differences between groups in SBP or DBP with repeated 2- hour ambulatory BP measurements and no inhibition of ACE after 8 weeks, although there was a decrease in sympathetic activity. Although there were no statistically significant differences between the groups, the group with highest fermented milk intake showed reduced BP across the 8-week period of the trial.
- 42.Huang TC, Kuksis A. A comparative study of the lipids of globule membrane and fat core and of the milk serum of cows. Lipids. 1967;2(6):453–460. doi: 10.1007/BF02533171. [DOI] [PubMed] [Google Scholar]
- 43.Pereira MA, Jacobs DR, Jr, Van Horn L, et al. Dairy consumption, obesity, and the insulin resistance syndrome in young adults: the CARDIA Study. JAMA. 2002;287:2081–2089. doi: 10.1001/jama.287.16.2081. [DOI] [PubMed] [Google Scholar]
- 44. Alonso A, Zozaya C, Vázquez Z, et al. The effect of low-fat versus whole-fat dairy product intake on blood pressure and weight in young normotensive adults. J Hum Nutr Diet. 2009;22(4):336–342. doi: 10.1111/j.1365-277X.2009.00967.x.. This RCT was conducted among 45 normotensive young men and women who alternatively received 3.5 servings/day of whole-fat or low-fat dairy products during an 8-week crossover trial. Whole-fat dairy intake significantly increased SBP and body weight but not DBP. Low-fat dairy did not change BP or body weight significantly. Overall, there was no significant difference in the effect of low-fat versus whole-fat dairy, on, BP, although whole-fat dairy increased body weight significantly compared to low-fat dairy.
- 45. Alonso A, Steffen LM, Folsom AR. Dairy intake and changes in blood pressure over 9 years: the ARIC study. Eur J Clin Nutr. 2009;63(10):1272–1275. doi: 10.1038/ejcn.2009.50.. The authors reported further results from the Atherosclerosis Risk in Communities (ARIC) Study, involving a bi-racial analysis among 6912 white and 1296 African American non-hypertensive men and women. After a 9-year follow-up period, whites consuming more than 3 low-fat dairy servings per day had significantly lower increase in BP than those consuming less than 1 serving per week. However, among African Americans, low-fat dairy product consumption was not associated with changes in BP over time.
- 46.Appel LJ, Moore TJ, Obarzanek E, et al. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N Engl J Med. 1997;336(16):1117–1124. doi: 10.1056/NEJM199704173361601. [DOI] [PubMed] [Google Scholar]
- 47.Svetkey LP, Simons-Morton D, Vollmer WM, et al. Effects of Dietary Patterns on Blood Pressure–Subgroup Analysis of the Dietary Approaches to Stop Hypertension (DASH) randomized clinical trial. Arch Intern Med. 1999;159:285–293. doi: 10.1001/archinte.159.3.285. [DOI] [PubMed] [Google Scholar]
- 48.Svetkey LP, Simons-Morton DG, Proschan MA, et al. Effect of the dietary approaches to stop HTN diet and reduced sodium intake on blood pressure control. J Clin Hypertens. 2004;6:373–381. doi: 10.1111/j.1524-6175.2004.03523.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ard JD, Coffman CJ, Lin PH, et al. One-year follow-up study of blood pressure and dietary patterns in Dietary Approaches to Stop Hypertension (DASH)-sodium participants. Am J Hypertens. 2004;17:1156–1162. doi: 10.1016/j.amjhyper.2004.07.005. [DOI] [PubMed] [Google Scholar]
- 50. Toledo E, de A Carmona-Torre F, Alonso A, et al. Hypothesis-oriented food patterns and incidence of HTN: 6-year follow-up of the SUN (Seguimiento Universidad de Navarra) prospective cohort. Public Health Nutr. 2010;13(3):338–349. doi: 10.1017/S1368980009991066.. The authors 10,800 men and women who were initially free of HTN for a median of 4.6 years. Over this period: 640 participants reported a first diagnosis of HTN and level of adherence to 15 different healthy food patterns was scored. Overall, adherence to only one dietary pattern, the DASH combination diet pattern, was significantly associated with a lower risk for developing HTN.