Abstract
Objective
Co-occurring posttraumatic stress (PTSD) and substance use disorders provide clinical challenges to addiction treatment providers. Interventions are needed that are effective, well-tolerated by patients, and capable of being delivered by typical clinicians in community settings. This is a randomized controlled trial of integrated cognitive behavioral therapy for co-occurring PTSD and substance use disorders.
Methods
Fifty-three participants sampled from seven community addiction treatment programs were randomized to integrated cognitive behavioral therapy plus standard care or individual addiction counseling plus standard care. Fourteen community therapists employed by these programs delivered both manual-guided therapies. Primary outcomes were PTSD symptoms, substance use symptoms and therapy retention. Participants were assessed at baseline, 3- and 6-month follow-up.
Results
Integrated cognitive behavioral therapy was more effective than individual addiction counseling in reducing PTSD re-experiencing symptoms and PTSD diagnosis. Individual addiction counseling was comparably effective to integrated cognitive behavioral therapy in substance use outcomes and on other measures of psychiatric symptom severity. Participants assigned to individual addiction counseling with severe PTSD were less likely to initiate and engage in the therapy than those assigned to integrated cognitive behavioral therapy. In general, participants with severe PTSD were more likely to benefit from integrated cognitive behavioral therapy.
Conclusions
The findings support the promise of efficacy of integrated cognitive behavioral therapy in improving outcomes for persons in addiction treatment with PTSD. Community counselors delivered both interventions with satisfactory adherence and competence. Despite several limitations to this research, a larger randomized controlled trial of integrated cognitive behavioral therapy appears warranted.
Keywords: Co-occurring disorders, PTSD, substance use, integrated treatment, CBT
Co-morbid posttraumatic stress disorder (PTSD) and substance use disorders are prevalent in the community, even more common in clinical settings, and associated with negative treatment and life outcomes (Back et al., 2000; Brady, Back, & Coffey, 2004; Brown, Recupero, & Stout, 1995; Cacciola, Alterman, McKay, & Rutherford, 2001; Dansky et al., 1994; Jacobsen, Southwick, & Kosten, 2001; Mills, Teesson, Ross, Darke, & Shanahan, 2005; Ouimette, Ahrens, Moos, & Finney, 1997). Historically, treatments for these dual disorders have been targeted to one or the other condition, with the expectation that by effectively addressing one as primary, the “secondary” disorder would consequently improve (McGovern, Alterman, Drake, & Dauten, 2009). Despite this widespread practice, no actual data were available to support this rationale. With the growing awareness of the complicating factor of psychiatric disorders in community addiction treatment, significant research has been invested in designing and testing integrated treatments for co-occurring disorders (Frisman et al., 2009; McLellan et al., 1997; Mueser, Noordsy, Drake, Fox, & Barlow, 2003). The preponderance of evidence generally supports the effectiveness of integrated approaches, although the findings are far from unanimous (Drake, Mueser, & Brunette, 2007; Flynn & Brown, 2008; Frisman et al., 2009; McNamara, Schumacher, Milby, Wallace, & Usdan, 2001; Mueser et al., 2003; Nunes & Levin, 2004; Rogers, 2001). One conjecture regarding the mixed findings is that addiction treatment alone may be effective for persons with mild to moderate psychiatric problems (in addition to substance use). But integrated mental health treatments are necessary for more severe co-morbid psychiatric problems (Flynn & Brown, 2008; McGovern & McLellan, 2008).
Within the context of addiction treatment and recovery, clinical and research interest has also focused on the challenges of persons with substance use and PTSD. Unlike mood, anxiety or even psychotic disorders, PTSD is somewhat easier to diagnose, because the symptoms are not typically substance-induced (McGovern et al., 2009). A variety of psychosocial treatments have been developed and tested, most notably Seeking Safety (Najavits, Weiss, & Liese, 1996; Najavits, Weiss, Shaw, & Muenz, 1998), which has been confined to women, and Concurrent Treatment of PTSD and Cocaine Dependence (Brady, Dansky, Back, Foa, & Carroll, 2001; Brady, 2009). Several other approaches have been described in the literature, although the research programs advancing these have not persisted (Donovan, Padin-Rivera, & Kowaliw, 2001; Triffleman, Carroll, & Kellogg, 1999). Only one of these treatments has been studied within the context of randomized controlled trial design, and the results found no definitive outcome advantage over matched relapse prevention (Hien, Cohen, Miele, Litt, & Capstick, 2004) or women’s health education strategies (Hien et al., 2009). In part, these findings may be due to sampling from a less severe PTSD community sample.
A systematic review of these approaches revealed a continued need for an integrated psychosocial treatment approach that would be effective in addressing substance use and PTSD symptoms, well-tolerated by patients, efficacious with both female and male patients, relatively straightforward for typical community counselors to learn and deliver with adherence and competence, and potentially transferred into routine addiction treatment programs (McGovern et al., 2009). Furthermore, a survey of community addiction treatment program directors indicated an implementation preference for coping skills-based versus exposure-based PTSD therapy, which could be more readily implemented by front line addiction counselors (McGovern et al., 2009).
In response, we identified a cognitive behavioral therapy approach previously designed and tested with patients with serious mental illnesses and co-occurring PTSD (Mueser, Rosenberg, Jankowski, Hamblen, & Descamps, 2004). A randomized controlled trial found the intervention efficacious, and particularly so for participants with severe PTSD (Mueser et al., 2008). Severe PTSD has been standardized and defined by a Clinician Administered PTSD Scale score of 65 or greater (Blake et al., 1995; Weathers, Ruscio, & Keane, 1999). Additionally, the intervention was based on a cognitive restructuring approach (not exposure-based) and simply developed for front-line community mental health clinicians to deliver (Mueser, Rosenberg, & Rosenberg, 2009).
We adapted this cognitive behavioral therapy for persons with co-morbid PTSD and substance use. This adaptation, integrated cognitive behavioral therapy, is manual-guided, delivered in eight to twelve individual sessions, and has three primary components: anxiety reduction technique, patient education, and cognitive and behavioral coping skill development.
Within the framework of the National Institute on Drug Abuse (NIDA) stage model of behavioral therapy development (Onken, Blaine, & Battjest, 1997; Rounsaville, Carroll, & Onken, 2001), Stage One Phase One (I) and Phase Two (II) studies have been conducted. To briefly summarize, the findings from Phase I, a small (n=3) open label study suggested that integrated cognitive behavioral therapy was safe, practical and promising in reducing substance use and PTSD symptoms, and it was well-tolerated by patients (McGovern et al., 2009). The Phase II feasibility study involved a single group design, and both a larger number of patients (n=11) and research therapists (n=5). These data also supported the potential efficacy of integrated cognitive behavioral therapy in reducing PTSD and substance use, as well as in maintaining excellent retention rates (McGovern, Lambert-Harris, et al., 2009). Both of these studies were conducted in community addiction treatment programs (intensive outpatient level of care) and sampled newly admitted patients diagnosed with PTSD and substance dependence disorders using structured clinical interviews. Relative to other studies, these patients had more severe PTSD and substance use problems, as assessed by standardized measures (PTSD: Clinician Administered PTSD Scale (Blake et al., 1995); Substance use: Addiction Severity Index (Cacciola, Alterman, McLellan, Lin, & Lynch, 2007; Rosen, Henson, Finney, & Moos, 2000).
In Stage I Phase III of the NIDA stage model, a small randomized controlled pilot trial is necessary to determine the potential efficacy of the experimental treatment relative to a comparison group. This comparison should reveal the outcome advantage of the experimental treatment over usual care or to another matched attention control intervention. For our purposes, we selected a two-group design with integrated cognitive behavioral therapy versus a matched individual attention control, and both delivered within the context of community addiction treatment services as usual.
The present study describes the results of this Stage I Phase III randomized pilot trial. A sample of patients presenting to community addiction treatment were eligible for research participation if they met criteria for PTSD. Consenting participants were randomized to integrated cognitive behavioral therapy plus standard care or individual addiction counseling plus standard care.
This study aims to address the following research questions;
Relative to individual addiction counseling, does integrated cognitive behavioral therapy result in improved patient outcomes on measures of substance use, PTSD and other psychiatric symptoms?
Relative to individual addiction counseling, do participants assigned to integrated cognitive behavioral therapy initiate, engage and complete treatment at different rates?
Do participants with more severe PTSD symptoms respond differently to the integrated cognitive behavioral therapy and individual addiction counseling interventions, relative to those with less severe PTSD?
METHODS
Design
This is a randomized controlled trial design consisting of two groups, integrated cognitive behavioral therapy plus standard care versus individual addiction counseling plus standard care. There are two types of standard care: intensive outpatient program and outpatient methadone maintenance. Participants in the integrated cognitive behavioral therapy and individual addiction counseling conditions were assessed at baseline, as well as 3- and 6-months follow-up on primary (substance use, PTSD and retention) and secondary (psychiatric symptom severity and depression) outcomes.
Participants
Subjects were sampled from one of seven participating community intensive outpatient or methadone maintenance programs located in New Hampshire, Vermont and Connecticut. All subjects were new admissions to the community addiction treatment programs.
In order to be eligible for the baseline assessment, participants: 1) Were at least 18 years of age; 2) Were actively enrolled in outpatient addiction services and met criteria for any substance use disorder; 3) Screened positive for PTSD based upon the PTSD Checklist (PCL)(described in measures section below) and revealing a likely Criterion A Traumatic event and a Criteria B, C and D symptom severity score equal to or greater than 44; 4) Provided informed consent to participate in the study. Upon completion of the baseline assessment, participants who met these initial inclusion criteria were potentially eligible for randomization contingent upon the following:1) Diagnosis of PTSD verified by the CAPS and total symptom score equal to or greater than 44; 2) No acute psychotic symptoms (persons with a psychotic disorder were eligible if their symptoms were stable and they were receiving appropriate mental health services); 4) No psychiatric hospitalization or suicide attempt in the past month, unless the hospitalization or attempt was directly related to substance intoxication or detoxification and the person was currently stable; and, 5) Medical and legal situations were stable such that ability to participate in the full duration of the study seemed likely.
Seventy-seven participants initially screened positive for PTSD to determine potential study eligibility. Of the 77 who screened positive on the PCL and who provided informed consent, 53 were objectively verified as eligible for the study based on structured clinical interview. The 24 participants screened positive were not eligible for the study, because they did not meet inclusion criteria (see above). The most common reason for not meeting eligibility criteria was a CAPS score less than 44 and/or not meeting the threshold for CAPS B (Re-experiencing), CAPS C (Avoidance), and/or CAPS D (Arousal) symptoms. Of the 53 enrolled and randomized participants (intent-to-treat), 36 completed at least one treatment session, 33 completed at least two treatment sessions, and 26 completed all treatment sessions. Follow-up data were obtained on 53% of the intent-to-treat sample.
Measures
Clinician Administered PTSD Scale (CAPS) (Blake et al., 1995)
The CAPS is a semi-structured diagnostic interview consisting of 22 items, yielding an overall CAPS Total Score and total scores for 3 subsections: B (re-experiencing), C (avoidance), and D (hyper-arousal), and PTSD Diagnosis. For the current study, we collected this information based on current PTSD symptoms (past 30 days).
Self-Administered Addiction Severity Index (SA-ASI) (McLellan, 1985; Rosen et al., 2000)
The SA-ASI consists of 103 questions assessing problem severity across seven dimensions: medical, employment, alcohol, drug use, legal, family/social and psychiatric. Current problem severity on the alcohol, drug and psychiatric summary composite scores were included as primary outcomes using the same algorithms as those employed for the interviewer administered ASI.
Time Line Follow Back (TLFB) (Sobell, Maisto, Sobell, & Cooper, 1979)
The TLFB is a structured interview to assess frequency and amount of substance use over the past 90 days.
Toxicology measures
Recent alcohol use was detected using the AlcoHawk ABI breathalyzer. Drug metabolites for amphetamine, benzodiazepines, cannabis, cocaine, methamphetamine, and opiates were detected in urine by using the One Step Multi-Drug screen test card with integrated iCup. Urine and breath samples were gathered at all three assessment periods.
Beck Depression Inventory (BDI) (Beck, Steer, & Brown, 1996)
The BDI consists of 21 questions designed to identify depressive symptoms and relative severity.
PTSD Checklist (PCL) (Weathers, Litz, Herman, Huska, & Keane, 1993)
The PCL is a self-report screening measure to assess for the likelihood of a PTSD diagnosis. A score that is greater than or equal to 44 indicates a probable PTSD diagnosis.
Interventions
Integrated cognitive behavioral therapy
Integrated cognitive behavioral therapy is a manual guided individual therapy focusing on PTSD symptoms and substance use. It was designed for integration into routine community addiction treatment programming. All subjects were required to be active in either intensive outpatient or methadone maintenance services. Integrated cognitive behavioral therapy consists of 8 modules: Module 1 (Introduction to Treatment) outlines the therapy approach, goals and mutual expectations. In Module 2 (Crisis & Relapse prevention plan), the clinician and patient review early warning signs, coping strategies and social supports to manage substance use and/or relapse. Module 3 (Breathing Retraining) teaches the patient an anxiety reduction skill. Module 4 (PTSD: Primary symptoms) introduces the three PTSD criterion symptoms (Re-experiencing, Avoidance, Hyper-arousal) and provides patient education and normalization. Module 5 (PTSD: Associated Symptoms) identifies common negative emotions and affects associated with PTSD (a. Fear and anxiety; b. Sadness and depression; c. Guilt and shame; and d. Anger) as well as the interpersonal consequences of PTSD. A significant portion of this module is devoted to examining the interplay between PTSD symptoms and substance use. The cognitive behavioral technique of cognitive restructuring is the focus of Module 6 (Cognitive Restructuring Part I) and Module 7 (Cognitive Restructuring Part II). Module 6 focuses on the basic framework of identifying stressful activating situations, beliefs/thoughts and consequences (emotional or behavioral). Module 7 builds upon this framework and skill development by including steps on disputing the belief (incorporating common styles of thinking handouts) and generating alternative emotions or behaviors. The final module, Module 8 (Generalization training) is designed to bring closure to the therapy relationship, consolidate a plan for continued application of the skills, and consider further treatment options. Integrated cognitive behavioral therapy is delivered in an individual format, within a weekly 45–50 minute session, over approximately 12–14 sessions. Integrated cognitive behavioral therapy has an accompanying client workbook that is used in conjunction with the therapist manual, and also contains practice handout items for homework in between treatment sessions.
Individual Addiction Counseling
Individual addiction counseling is a manual guided individual therapy designed to be integrated into an addiction treatment or methadone maintenance programs. Individual addiction counseling is an adaptation of the Individual Drug Counseling (IDC) treatment used in the NIDA Cocaine Collaborative Study (Mercer & Woody, 1999). Unlike integrated cognitive behavioral therapy, individual addiction counseling targets substance use only and is therefore complementary to a typical community addiction treatment program. Individual addiction counseling consists of 5 modules: 1) Treatment initiation; 2) Early abstinence; 3) Maintaining abstinence; 4) Recovery; and 5) Termination. Individual addiction counseling is delivered in 10–12 weekly sessions. As with integrated cognitive behavioral therapy, individual addiction counseling has patient practice handouts for homework in between treatment sessions.
Standard care
Standard care occurred in either methadone maintenance or intensive outpatient clinics. Two of the seven programs were methadone maintenance and five were intensive outpatient programs. Methadone maintenance clinics provide controlled dispensing of methadone, monthly individual counseling, group counseling, psychiatric evaluation and referral, and some case management services. In general, patients are in methadone maintenance for ongoing care. Intensive outpatient programs operate in two phases, primary intensive outpatient, which includes 5 weeks of 9–12 hours per week group counseling primarily focused on substance use, and continuing care, which includes 2–3 months of weekly one hour group counseling focused on relapse prevention. Psychiatric evaluation and individual counseling are available as needed.
Therapist background, training, and supervision
Fourteen community counselors were cross-trained in both integrated cognitive behavioral therapy and individual addiction counseling interventions. For this study, therapists were crossed (i.e. each therapist delivered both the individual addiction counseling and integrated cognitive behavioral therapy therapies). All therapists were full-time employees of the clinics participating in the study. The majority of the clinicians were female (79% (n=11)) with an average age of 32.6 (sd=26.5). Seven were Caucasian, 6 Hispanic, and 1 African-American. The highest educational levels were: master’s degree (8), bachelor’s degree (4), and high school (2). Six were licensed or certified alcohol and drug counselors (CADC/LADC), 3 were licensed mental health counselors (LMHC), and 5 did not have any certification or licensure. The therapists received a 90 minute didactic training in both integrated cognitive behavioral therapy and individual addiction counseling approaches, and then were supervised in bi-weekly phone (individual) and monthly face-to-face (group) sessions. All therapy sessions were audio-taped for quality assurance and supervision purposes. Members of the research team randomly reviewed tapes and rated sessions for adherence and competency. Adherence/competence measures for both integrated cognitive behavioral therapy and individual addiction counseling were developed for this study and based upon the Yale Adherence and Competence Scale (YACS) system (Corvino et al., 2001). All clinicians in all but 1 case performed at a satisfactory level of adherence and competence.
Procedure
All subjects completed the PTSD Checklist (PCL) at admission to standard care settings. Subjects who were potentially eligible for the study (PCL total score of 44 or greater) were approached by the site coordinator to determine interest in the study. If a subject was interested in participating, a research interviewer would meet with the subject to discuss the study in detail and to obtain written informed consent. This study was conducted in strict accordance with all human subject protections and good clinical practices (e.g., Helsinki Declaration, Belmont Principles, and Nuremberg Code) and was approved by the Trustees of Dartmouth College Committee for the Protection of Human Subjects (CPHS) and the State of New Hampshire Department of Health and Human Services CPHS.
If a subject was determined to be eligible for the study at the baseline assessment, s/he was randomly assigned to one of two interventions, integrated cognitive behavioral therapy or individual addiction counseling, in addition to the treatment s/he would ordinarily receive. Both interventions were delivered over an 8 to 12 week timeframe. At 3-month post-baseline, all participants were re-assessed using the same primary outcome measures conducted at baseline, whether or not s/he completed treatment. Finally, all randomized participants were assessed at 6-month post-baseline using the same measures as at the 3-month follow-up. The research interviewers were blinded to treatment assignment at randomization, but not at the follow-up assessments.
Participants were paid for their participation in the study: At baseline $30, at the completion of the 3-month follow-up $40, and $50 at the completion of the 6-month follow-up.
Data analysis
Data were analyzed using SPSS (17.0) (SPSS, 2008). Baseline participant characteristics were analyzed using chi-square for categorical variables and t-test for continuous variables. Generalized Estimating Equations (GEE) analyses were use to examine change over time in PTSD severity and diagnosis (CAPS), substance use severity (ASI Drug composite scores, ASI Alcohol composite scores, and TLFB alcohol and drug use in the past 90 days), and psychiatric severity (ASI psychiatric composite score and BDI). The GEE models data, including categorical and continuous outcome data, without excluding subjects based on missing data points or drop out. Analysis of covariance (ANCOVA) was used to generate effect sizes between groups on the above mentioned primary outcomes with the exception of PTSD Diagnosis, positive alcohol breathalyzer, and positive urine drug screen. Since PTSD diagnosis, positive alcohol breathalyzer, and urine drug screen are categorical variables, we approximated the effect size by transforming the proportion of PTSD positive diagnoses, at endpoint into an Arcsine value and calculated the difference between the two groups to determine the effect size (Lipsey, 1990). The same calculations were used to determine effect size for positive alcohol breathalyzer and positive urine drug screen. There was no significant site difference found on primary outcomes, therefore, site was not treated as a covariate.
RESULTS
Participant characteristics
The average age of participants was 39.09 (sd=11.32) in integrated cognitive behavioral therapy and 35.48 (sd=9.44) years in individual addiction counseling. The majority of participants were Caucasian. Half of the integrated cognitive behavioral therapy participants were male (n=16), while only 33.3% of the individual addiction counseling were male (n=7). All participants in the study were assessed positive for PTSD using the CAPS. On average, both groups scored in the severe range of PTSD based upon the CAPS total scores. CAPS B Re-experiencing, CAPS C Avoidance, and CAPS D Arousal were also remarkable for a high level of PTSD symptom severity. Chronologically, the majority of participants experienced one or more traumatic life events and then began using substances. The most common traumatic event was childhood sexual assault followed by childhood physical assault and adult sexual assault (see Table 1).
Table 1.
Demographics and baseline characteristics (n=53)
| ICBT (n=32) |
IAC (n=21) |
|
|---|---|---|
| Age Mean(sd) | 39.09 (11.32) | 35.48 (9.44) |
| Gender (Male) | 50.0% (16) | 33.3% (7) |
| Race (Caucasian/White) | 87.5% (28) | 95.2% (20) |
| PTSD Positive | 100.0% (32) | 100.0% (21) |
| CAP Score Total Mean(sd) | 75.75 (19.94) | 84.10 (22.57) |
| CAPS B Re-experiencing Mean(sd) | 22.50 (7.07) | 24.86 (8.45) |
| CAPS C Avoidance Mean(sd) | 30.00 (9.36) | 32.38 (10.69) |
| CAPS D Arousal Mean(sd) | 23.25 (8.68) | 26.86 (7.79) |
| Trauma Types | ||
| Childhood Sexual Assault | 71.9% (23) | 61.9% (13) |
| Childhood Physical Assault | 21.9% (7) | 14.3% (3) |
| Adult Sexual Assault | 6.3% (2) | 14.3% (3) |
| Adult Physical Assault | 0.0% (0) | 4.8% (1) |
| Accident | 0.0% (0) | 4.8% (1) |
| Trauma Sequence | ||
| Trauma > Substance use | 21.9% (7) | 14.3% (3) |
| Trauma > Substance use > Trauma > Substance use | 68.8% (22) | 81.0% (17) |
| Substance use > Trauma | 9.4% (3) | 4.8% (1) |
| Positive urine drug screen | 46.9% (15) | 47.6% (10) |
| Positive alcohol breathalyzer | 6.3% (2) | 0.0% (0) |
| 3-month Timeline Follow Back | ||
| Mean number of days drinking | 23.03 (27.57) | 15.69 (20.10) |
| Mean number of days using drugs | 36.28 (35.54) | 26.21 (23.87) |
| ASI Composite Scores | ||
| Alcohol | .25 (.29) | .24 (.22) |
| Drug | .19 (.15) | .20 (.09) |
| Psychiatric | .49 (.18) | .56 (.15) |
Note. ICBT = integrated cognitive behavioral therapy; IAC = individual addiction counseling; CAPS = Clinician Administered PTSD Scale; ASI = Addiction Severity Index.
As shown in Table 1, approximately half of the participants tested positive for drug use at baseline. However, none of the participants had a positive alcohol breathalyzer in the individual addiction counseling group, and only 6.3% were positive for alcohol among the integrated cognitive behavioral therapy group. At the initial assessment, participants in the integrated cognitive behavioral therapy group reported drinking slightly more days than the individual addiction counseling group in the past 90 days. A similar pattern was reported for drug use in the past 90 days among the groups. However, these differences between the groups were not significant.
On the ASI, we found comparable alcohol, drug, and psychiatric composite scores for the groups (see Table 1).
There were no significant differences found between groups on any baseline characteristics.
Retention
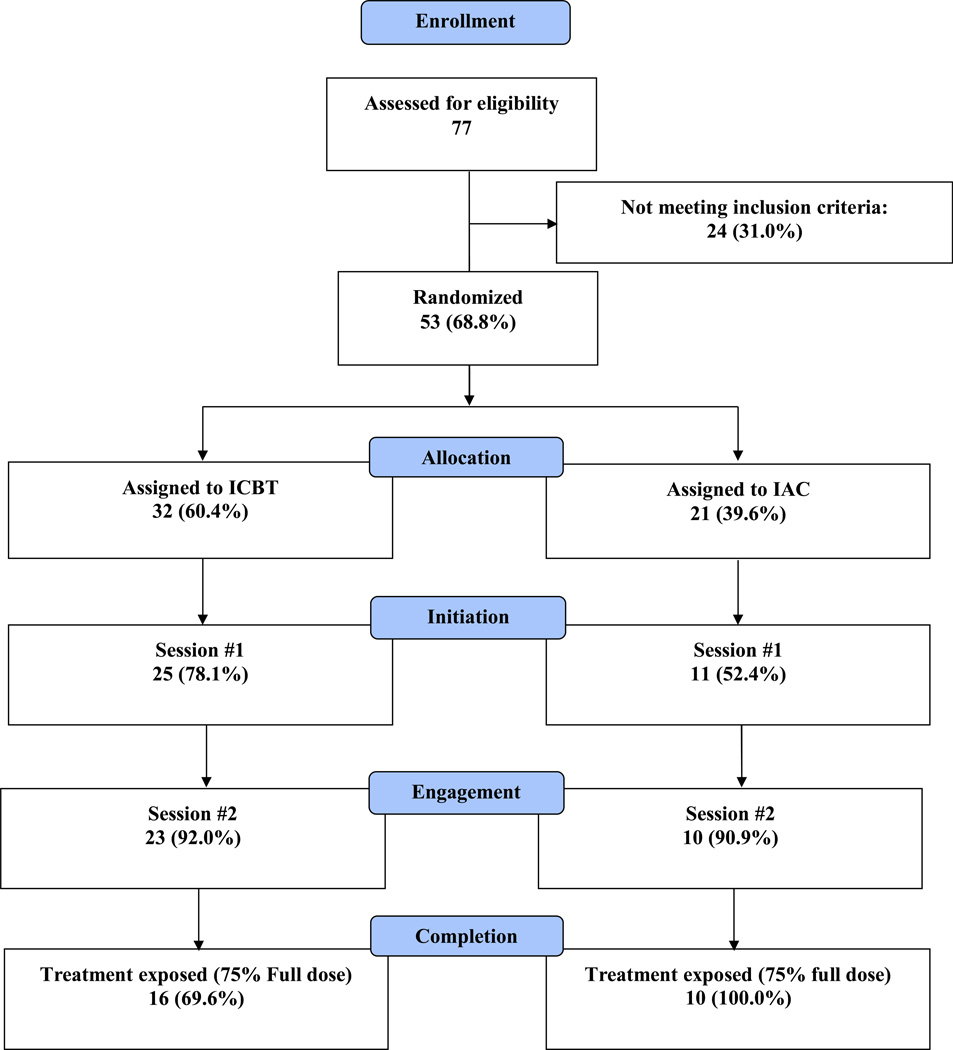
Retention data were approached at three levels: 1) Initiation: Once randomized, attending at least one session (i.e. starting therapy); 2) Engagement: Once initiated, engaging in therapy for at least two sessions (i.e. continuing therapy); and 3) Completion: Once continuing, completing a sufficient dose (75% of sessions) of sessions (i.e. finishing therapy).
Initiation
Of those who were eligible for study treatment (n=53), 32 were randomized to integrated cognitive behavioral therapy and 21 were randomized to individual addiction counseling. Seventy-eight percent (n=25) attended at least one integrated cognitive behavioral therapy session, while 52.4% (n=11) attended at least one individual addiction counseling session (see Figure 1). The number of participants receiving at least one session of integrated cognitive behavioral therapy was significantly greater than those attending at least one individual addiction counseling session (χ2=3.86, df=1, p=.05). At baseline, we found a significant age difference between those who attended session one of integrated cognitive behavioral therapy and those who did not (t=−2.47, df=30, p=.02). Attendees of at least one integrated cognitive behavioral therapy session were significantly older (42.70 (sd=9.89) vs. 29.89 (sd=9.73)). There were no other significant differences found on baseline measures among the integrated cognitive behavioral therapy group.
FIGURE 1.
ICBT and IAC retention: initiation, engagement, and completion.
With respect to individual addiction counseling, those who did not attend at least one session had significantly higher CAPS total scores (94.80 (sd=20.49) vs. 74.36 (sd=20.54)) (t=2.28, df=19, p=.03), CAPS D Arousal (30.50 (sd=7.29) vs. 23.55 (sd=6.93)) (t=2.24, df=19, p=.04), ASI alcohol composite scores (.40 (sd=.19) vs. .12 (sd=.16)) (t=3.68, df=18, p=.00), and days of alcohol use in the past 90 days (27.85 (sd=18.81) vs. 4.64 (sd=14.40)(t=3.19, df=19, p=.01).
No significant age, gender, drug composite score, psychiatric composite score or BDI differences were found among those who attended one individual addiction counseling session and those who did not receive at least one session.
To summarize, most participants (78.1%) randomized to integrated cognitive behavioral therapy attended the first session, whereas about half (52.4%) randomized to individual addiction counseling started treatment. The differences are found in PTSD and alcohol problem severity. Those with more severe PTSD and more severe alcohol issues did not initiate individual addiction counseling but the same pattern was not found with integrated cognitive behavioral therapy.
Engagement
Ninety-two percent (n=23) of the integrated cognitive behavioral therapy participants engaged in treatment (completed session 2), versus 90.9% (n=10) of the individual addiction counseling participants (see Figure 1). There was no significant difference in rate of treatment engagement between the groups. Of those who engaged in integrated cognitive behavioral therapy, the only difference found was age. The participants who engaged in integrated cognitive behavioral therapy treatment were 42.69 (sd=9.89) versus 29.89 (sd=9.73) for non-engagers (t=−3.31, df=30, p=.00). In individual addiction counseling there were a number of significant differences found, including CAPS Total Score, ASI alcohol composite score, and days of alcohol use (past 90 days). Those who did not engage in individual addiction counseling treatment had significantly greater CAPS Total scores (94.64 (sd=19.44) vs. 72.50 (sd=20.65), ASI Alcohol composite scores (.36 (sd=.22) vs. .13 (sd=.16)) and days of alcohol use (25.32 (sd=19.72) vs. 5.10 (sd=15.09)) than those who engaged (t=2.53, df=19, p=.02; t=2.72, df=18, p=.01; t=2.62,df=19, p=.02).
In summary, there were no significant differences in the rates of engagement between integrated cognitive behavioral therapy and individual addiction counseling. But those subjects who did not engage in individual addiction counseling had more severe PTSD and alcohol symptoms.
Completion
For both integrated cognitive behavioral therapy and individual addiction counseling, completion or sufficient treatment exposure was set a priori at 75% of sessions, in other words, attending at least 8 of the 12 total sessions.
Sixty-nine percent (16) of participants engaged in integrated cognitive behavioral therapy completed treatment, while 100% (10) of participants engaged in individual addiction counseling completed (see Figure 1). Those who engaged in individual addiction counseling were significantly more likely to complete than those who engaged in integrated cognitive behavioral therapy (χ2=3.86, df=1, p=.05). Integrated cognitive behavioral therapy non-completers had a significantly higher ASI drug composite score (.31 (sd=.17) vs. .13 (sd=.11)) and days of drug use (56.86 (sd=31.16) vs. 22.13 (sd=30.67)) at baseline (t=2.96, df=20, p.01; t=2.39, df=21, p=.03) than integrated cognitive behavioral therapy completers. In summary, of those continuing in therapy, individual addiction counseling had better completion rate than integrated cognitive behavioral therapy. Participants not completing integrated cognitive behavioral therapy were more likely to have more severe drug use severity.
Primary Outcomes
PTSD
PTSD severity and diagnosis were evaluated using the CAPS. As shown in Table 2, there was a significant group effect on CAPS total score (χ2=4.14, df=1, p=.04), CAPS B Re-experiencing score (χ2=6.81, df=1, p=.01), CAPS D Arousal score (χ2=4.75, df=1, p=.03), and days of drug use (χ2=5.04, df-1, p=.03). We found a small effect size for CAPS total score (−0.17) and CAPS D Arousal (−0.35), and a moderate effect size on CAPS B Re-experiencing (−0.40). Over time, both groups significantly decreased overall CAPS total scores (χ2=96.54, df=2, p=.00), CAPS B Re-experiencing score (χ2=82.28, df=2, p=.00), CAPS C Avoidance score (χ2=56.47, df=2, p=.00), CAPS D Arousal score (χ2=34.14, df=2, p=.00) and PTSD diagnosis (χ2=61.76, df=2, p=.00).
Table 2.
Primary outcomes (n=53)
| Group Effect | |||||||
|---|---|---|---|---|---|---|---|
| Outcome | Condition | Baseline | 3 months | 6 months | df | χ2 | ES |
| Continuous variables1 | |||||||
| CAPS Total Score | ICBT | 75.75(19.94) | 36.08(19.19) | 46.50(21.75) | 1 | 4.14* | –0.17 |
| IAC | 84.10(22.57) | 52.60(21.86) | 49.75(28.64) | ||||
| CAPS B Re-experiencing | ICBT | 22.50(7.07) | 10.69(4.73) | 12.07(6.81) | 1 | 6.81** | –0.40 |
| IAC | 24.86(8.45) | 16.10(7.03) | 14.38(8.55) | ||||
| CAPS C Avoidance | ICBT | 30.00(9.36) | 13.54(8.92) | 17.14(11.62) | 1 | 0.26 | 0.11 |
| IAC | 32.38(10.69) | 18.00(12.89) | 15.88(15.29) | ||||
| CAPS D Arousal | ICBT | 23.25(8.68) | 11.85(9.61) | 17.29(6.72) | 1 | 4.75* | –0.35 |
| IAC | 26.86(7.79) | 18.50(5.66) | 19.50(8.00) | ||||
| ASI Alcohol Composite | ICBT | .25(.29) | .07(.15) | .11(.20) | 1 | 0.00 | 0.75 |
| IAC | .24(.22) | .05(.07) | .03(.06) | ||||
| ASI Drug Composite | ICBT | .19(.15) | .12(.10) | .10(.09) | 1 | 0.02 | 0.03 |
| IAC | .20(.09) | .11(.08) | .10(.10) | ||||
| Alcohol Use (Days) | ICBT | 23.03(27.57) | 1.31(2.43) | 8.14(23.75) | 1 | 0.74 | 0.63 |
| IAC | 15.69(20.10) | 0.20(0.63) | 0.25(0.71) | ||||
| Drug Use (Days) | ICBT | 36.28(35.54) | 16.15(32.00) | 12.68(25.87) | 1 | 5.04* | 0.41 |
| IAC | 37.56(10.36) | 25.70(17.01) | 26.24(16.14) | ||||
| ASI Psychiatric Composite | ICBT | .49(.18) | .28(.22) | .35(.19) | 1 | 2.64 | –0.42 |
| IAC | .56(.15) | .42(.21) | .42(.17) | ||||
| BDI | ICBT | 21.10(10.19) | 13.35(9.83) | 19.68(12.74) | 1 | 3.45 | –0.47 |
| IAC | 37.56(10.36) | 25.70(17.01) | 26.24(16.14) | ||||
| Categorical variables2 | |||||||
| PTSD Diagnosis - Positive | ICBT | 32(100.0) | 4(30.8) | 7(50.0) | 1 | 0.57 | 0.52 |
| IAC | 21(100.0) | 5(50.0) | 2(25.0) | ||||
| Positive alcohol breathalyzer | ICBT | 2(6.3) | 0(0.0) | 0 (0.0) | 1 | 1.25 | –0.74 |
| IAC | 0(0.0) | 1(10.0) | 1(12.5) | ||||
| Positive urine drug screen | ICBT | 15(46.9) | 9(75.0) | 6(46.2) | 1 | 0.11 | –0.08 |
| IAC | 10(47.6) | 7(77.8) | 4(50.0) | ||||
Values are means and standard deviation;
Values are given as number and percent;
p<=.001;
p=.01;
p=.05
Note. ICBT = integrated cognitive behavioral therapy; IAC = individual addiction counseling; CAPS = Clinician Administered PTSD Scale; ASI = Addiction Severity Index; BDI = Beck Depression Inventory.
There was a significant interaction effect between groups over time on the CAPS B Re-experiencing score (χ2=6.09, df=2, p=.05) as well as PTSD Diagnosis (χ2=5.91, df=2, p=.05). A greater proportion of the integrated cognitive behavioral therapy group no longer had a PTSD diagnosis by 6-month follow-up than the individual addiction counseling group, and integrated cognitive behavioral therapy had significantly greater reductions in re-experiencing symptoms.
Substance use
The ASI alcohol and drug composite scores, toxicology measures and the TLFB were used to measure substance use severity. A significant decrease in both ASI alcohol and drug composite scores over time was found (χ2=27.15, df=2, p=.00; χ2=17.95, df=2, p=.00). Consistent with the findings from the ASI composite scores, on the TLFB subjects reported a significant reduction in alcohol and drug use over time (χ2=34.31, df=2, p=.00; χ2=24.16, df=2, p=.00). There was a moderate effect size on drug use days between integrated cognitive behavioral therapy and individual addiction counseling (see Table 2). Both groups also significantly decreased drug use as verified by urine drug screen (χ2=8.50, df=2, p=.01).
Psychiatric symptoms
Overall psychiatric symptom severity was assessed using the ASI psychiatric severity composite score and BDI. There was a significant decrease in ASI psychiatric composite scores and BDI scores over time for both the integrated cognitive behavioral therapy and individual addiction counseling groups (χ2=22.21, df=2, p=.00; χ2=32.32, df=2, p=.00). We found no significant group by time effects.
Severe PTSD subsample
PTSD
Relative to the entire sample, a greater reduction in PTSD symptoms in the more severe PTSD subsample (37) was observed on: CAPS Total Score (χ2=5.97, df=1, p=.02), CAPS B Re-experiencing score (χ2=21.61, df=1, p=.00), and CAPS D Arousal score (χ2=6.03, df=1, p=.01). We found a large effect size between the integrated cognitive behavioral therapy and individual addiction counseling groups on CAPS total score (−1.82), CAPS B Re-experiencing (−1.97), and CAPS D Arousal (−1.23). Over time, both groups significantly decreased CAPS Total Score (χ2=86.46, df=2, p=.00), CAPS B Re-experiencing (χ2=98.94, df=2, p=.00), CAPS C Avoidance (χ2=47.92, df=2, p=.00), CAPS D Arousal (χ2=27.81, df=2, p=.00), and PTSD diagnosis (χ2=14.93, df=2, p=.00).
Substance use
As with PTSD symptoms, participants in the more severe subsample significantly reduced substance severity over time as measured by ASI alcohol composite score (χ2=17.43, df=2, p=.00), ASI drug composite score (χ2=9.36, df=2, p=.01), days of alcohol use (TLFB)(χ2=27.18, df=2, p=.00), and days of drug use (TLFB)(χ2=16.91, df=2, p=.00). There was a significantly greater decrease in days of alcohol use among the individual addiction counseling group (18 days vs. 14 days) (χ2=7.29, df=2, p=.03) versus integrated cognitive behavioral therapy. However, there was a significantly greater reduction in reported days of drug use among the integrated cognitive behavioral therapy group (31 days vs. 10 days) (χ2=9.29, df=2, p=.01) than the individual addiction counseling group (effect size: −1.53) (See Table 3).
Table 3.
Primary outcomes: Severe PTSD subsample (n=37)
| Group Effect | |||||||
|---|---|---|---|---|---|---|---|
| Outcome | Condition | Baseline | 3 months | 6 months | df | χ2 | ES |
| Continuous variables1 | |||||||
| CAPS Total Score | ICBT | 84.57(16.08) | 43.57(19.72) | 48.00(23.53) | 1 | 5.97* | –1.82 |
| IAC | 97.50(13.82) | 60.50(17.46) | 78.00(19.93) | ||||
| CAPS B Re-experiencing | ICBT | 24.83(6.65) | 10.71(4.15) | 11.56(7.60) | 1 | 21.61*** | –1.97 |
| IAC | 29.57(5.16) | 18.00(3.16) | 22.00(3.61) | ||||
| CAPS C Avoidance | ICBT | 32.52(8.02) | 16.00(10.95) | 17.44(12.42) | 1 | 0.86 | –1.03 |
| IAC | 37.79(8.08) | 19.25(12.69) | 29.67(15.50) | ||||
| CAPS D Arousal | ICBT | 27.22(6.08) | 16.86(8.24) | 19.00(7.25) | 1 | 6.03** | –1.23 |
| IAC | 30.14(6.55) | 23.25(4.11) | 26.33(6.43) | ||||
| ASI Alcohol Composite | ICBT | .27(.29) | .10(.20) | .16(.23) | 1 | 0.07 | 0.76 |
| IAC | .32(.21) | .05(.08) | .06(.10) | ||||
| ASI Drug Composite | ICBT | .19(.17) | .10(.09) | .07(.08) | 1 | 4.01* | –1.53 |
| IAC | .23(.09) | .18(.05) | .18(.11) | ||||
| Alcohol Use (Days) | ICBT | 26.04(29.11) | 1.71(3.15) | 12.11(29.43) | 1 | 0.04 | 0.79 |
| IAC | 18.46(20.84) | 0.00(0.00) | 0.67(1.15) | ||||
| Drug Use (Days) | ICBT | 37.22(34.16) | 15.14(33.47) | 5.83(13.47) | 1 | 0.12 | –0.59 |
| IAC | 23.11(19.69) | 7.50(13.70) | 13.33(11.93) | ||||
| ASI Psychiatric Composite | ICBT | .55(.18) | .36(.20) | .30(.18) | 1 | 6.10** | –1.54 |
| IAC | .58(.15) | .45(.06) | .54(.02) | ||||
| BDI | ICBT | 33.40(11.18) | 12.93(10.74) | 18.38(9.36) | 1 | 11.23*** | –1.60 |
| IAC | 40.77(7.86) | 40.50(10.66) | 35.33(16.17) | ||||
| Categorical variables2 | |||||||
| PTSD Diagnosis Positive | ICBT | 23(100.0) | 4(57.1) | 5(55.6) | 1 | 0.59 | –0.23 |
| IAC | 14(100.0) | 2(50.0) | 2(66.7) | ||||
| Positive alcohol breathalyzer | ICBT | 2(8.7) | 0(0.0) | 0(0.0) | 1 | 0.37 | –1.22 |
| IAC | 0(0.0) | 1(25.0) | 1(33.3) | ||||
| Positive urine drug screen | ICBT | 10(43.5) | 5(83.3) | 4(50.0) | 1 | 0.64 | 0.35 |
| IAC | 5(35.7) | 1(33.3) | 1(33.3) | ||||
Values are means and standard deviation;
Values are given as number and percent;
p<=.001;
p=.01;
p=.05
Note. ICBT = integrated cognitive behavioral therapy; IAC = individual addiction counseling; CAPS = Clinician Administered PTSD Scale; ASI = Addiction Severity Index; BDI = Beck Depression Inventory.
Thus individual addiction counseling had differential impact on days of alcohol use (more favorable), and integrated cognitive behavioral therapy had a more positive impact on days of drug use in the severe PTSD subsample.
Psychiatric symptoms
Finally, there was a significant group effect on ASI psychiatric composite score (χ2=6.10, df=1, p=.01; effect size: −1.54). Both groups significantly reduced the ASI psychiatric composite score over time (χ2=26.79, df=2, p=.00). The integrated cognitive behavioral therapy group had a significantly greater reduction in ASI psychiatric composite scores over time than the individual addiction counseling group (χ2=14.88, df=2, p=.00). In addition, the individual addiction counseling group had a significantly higher BDI score (more symptomatic) than the integrated cognitive behavioral therapy group (χ2=11.23, df=1, p=.00) (see Table 3).
In summary, for the more severe PTSD subsample, PTSD outcomes were more substantial than in the less severe sample. The integrated cognitive behavioral therapy had better outcomes relative to individual addiction counseling for this subsample in drug use severity, depression and overall psychiatric severity. Individual addiction counseling had a more favorable impact on alcohol use severity.
DISCUSSION
Summary of findings
The first research question entailed the differential outcomes between the integrated cognitive behavioral therapy and individual addiction counseling conditions. Analyses revealed that both treatments had a favorable impact on PTSD, substance use and psychiatric symptoms from baseline to follow-up. Statistical and clinically significant reductions in PTSD symptom severity were examined via the CAPS total and section scores. A clinically meaningful reduction in PTSD has been determined to be 15 points or more (Weathers et al., 1999). The integrated cognitive behavioral therapy group had a close to an average 40 point reduction in CAPS total score from baseline to post-treatment, and an average 30 point reduction was maintained at 3-month follow-up. The individual addiction counseling group had an average 30 point reduction post-treatment and 25 point decrease maintained at follow-up.
The integrated cognitive behavioral therapy approach was superior to individual addiction counseling in terms of reduction of CAPS B Re-experiencing symptoms as well as in overall decrease in positive PTSD diagnoses.
Both integrated cognitive behavioral therapy and individual addiction counseling had a significant impact on reduction of PTSD severity. But integrated cognitive behavioral therapy had a more potent impact on PTSD diagnosis and re-experiencing symptom severity. Thus, patients with a PTSD diagnosis realize significantly greater benefit from the integrated cognitive behavioral therapy treatment, and more effective skills to deal with one of the more distressing phenomenon of the disorder: re-experiencing symptoms.
Both conditions were similarly effective in reducing substance use, and these findings converged across all three measures (ASI, TLFB, toxicology). Individual addiction counseling and integrated cognitive behavioral therapy were likewise equivalently successful in reducing psychiatric symptoms as measured by the ASI and BDI.
Since individual addiction counseling targets substance use and integrated cognitive behavioral therapy targets both substance use and PTSD, it is entirely plausible that substance use outcomes might be equivalent across the two interventions. This may in fact be the case in the short-term, however other researchers have recently found in a longer follow-up period, that positive changes in PTSD symptoms serve to predicate substance use outcomes (e.g.Hien et al, 2010). Therefore a longer term follow-up of participants receiving integrated cognitive behavioral therapy or individual addiction counseling may have found differences between the treatments in substance use outcomes.
With respect to retention, we segmented this variable into three categories: initiation, continuation and completion. The individual addiction counseling condition had a 100% completion rate relative to integrated cognitive behavioral therapy which had 69.6% of the sample completing sufficient dose. For both treatments exposure to 8 sessions was a sufficient dose of “completion”.
However, the groups were very different in initiation and engagement. Participants with severe PTSD and alcohol problems were much less likely to initiate individual addiction counseling than integrated cognitive behavioral therapy. Being randomized to individual addiction counseling precipitated attrition in 50% of individual addiction counseling cases vs. 20% with integrated cognitive behavioral therapy. Of those engaged (continuing to the second session), 92% continued in integrated cognitive behavioral therapy versus 90.9% in individual addiction counseling. Clearly, there was little equipoise in this study, as significant differences in treatment preferences emerged. This difference seemed to center around patients with severe PTSD desiring treatment that would directly address this concern.
We followed the logic of Flynn & Brown (2008) and also attempted to replicate the better response to integrated cognitive behavioral therapy among a more severe PTSD subsample as found by Mueser et al (2008). In this study, we replicated the finding that participants with CAPS total scores of 65 or more experienced greater change than those with mild to moderate PTSD across both integrated cognitive behavioral therapy and individual addiction counseling approaches. For this subgroup, the differences may have actually transpired in who initiated and continued in the respective therapies: more severe PTSD participants entered integrated cognitive behavioral therapy but not individual addiction counseling. Nonetheless, there were also differences found in changes on drug use severity and psychiatric symptom severity (ASI psychiatric composite score and BDI). Integrated cognitive behavioral therapy outcomes on these variables were significantly better than with individual addiction counseling. Interestingly, among this more severe PTSD subgroup, individual addiction counseling was more effective than integrated cognitive behavioral therapy with alcohol symptom severity.
In summary, the results of this small randomized controlled trial support the promise in efficacy of integrated cognitive behavioral therapy for persons with co-occurring PTSD, particularly if one considers patient preference, as well as increasing treatment options for a more severe PTSD subsample.
Again, given the significant short-term impact of integrated cognitive behavioral therapy on PTSD symptom severity, there may be longer term implications for substance use outcomes. In studies by Back et al (2006), and more recently by Hien et al (2010), change in PTSD symptoms was found to be a precursor to change in substance use. A longer term follow-up (i.e. beyond 3-months post-treatment) may have replicated these findings.
Limitations
As with many pilot trials, the present study was statistically under-powered and may have lacked sufficient sample size to detect actual differences between the groups. Kraemer and colleagues (2006) discussed the data analytic challenges in conducting small pilot trials in advance of larger randomized controlled trials. These considerations include estimating effect size, controlling for mediators and moderators and contending with subjects lost to treatment and follow-up assessment. This study suffered these typical liabilities. Of particular concern is the low follow-up rate (53%), which reduces the power and the ability to detect differences between treatment conditions. The low follow-up rate was mainly due significant housing instability and geographic movement of the research participants, but also the lack of dedicated research personnel to maintain ongoing contact with the participants, as well as insufficient contact information collected at baseline assessment. Although GEE is useful in statistically estimating follow-up scores using within intent to treat analyses, future research must clearly improve follow-up rates to adequately answer questions about efficacy. Having greater resources for research personnel to maintain ongoing contact with the participants is essential. Additional methods should also be utilized such as requesting several collateral contacts (e.g., extended family, friends, parole officers, etc.), and deploying multiple formats for contact (e.g. phone, email, social network sites).
Despite these limitations and the liability of a small sample size, significant group and interaction effects were observed. Integrated cognitive behavioral therapy has a significant and positive impact on PTSD symptom severity, substance use and other psychiatric symptoms. Individual addiction counseling is also an effective treatment. For less severe PTSD and co-morbid substance use, particularly alcohol use disorders, it has a clear benefit.
Future research
Within the framework of the stage model of behavioral therapy development, this research reports on the results of the Stage I Phase III randomized controlled pilot trial. Integrated cognitive behavioral therapy was compared to a matched attention control, individual addiction counseling, and found to be equally effective on some outcome variables, more effective on others, and emerged as a patient preference.
Based upon therapist adherence and competence ratings, integrated cognitive behavioral therapy appears feasible for typical community addiction counselors to learn and deliver. This finding suggests important downstream implementation advantages for the translation of integrated cognitive behavioral therapy into routine community practice settings. Previous studies have found significant barriers to counselors’ capacity to learn and deliver CBT for substance use disorders (Morgenstern, Blanchard, Morgan, Labouvie, & Hayaki, 2001; Sholomskas et al., 2005). Future research with integrated cognitive behavioral therapy can address ingredients to the selection, training and supervision of community clinicians.
The next step of research in the stage model of behavioral therapy development is the Stage II efficacy study. This stage overcomes many of the obvious limitations in the current study (small sample size, adequate resources for follow-up) and involves a large randomized controlled trial (RCT). A large RCT study of integrated cognitive behavioral therapy is presently underway. In addition, many community providers, as well as providers in the Veterans Affairs (VA) system of care, continue to seek solutions for patients with co-occurring PTSD and substance use disorders. Studies of integrated cognitive behavioral therapy are also in progress with U.S. Veterans, including an adaptation of integrated cognitive behavioral therapy for delivery in a group therapy format. Given the high rates of this co-morbidity among community and military populations, the need remains for more effective treatment options.
ACKNOWLEDGMENTS
This research was supported by K23DA16574, R01DA27650 and R01DA30102 (McGovern). The authors wish to acknowledge the patients and staff at Dartmouth-Hitchcock Medical Center Addiction Treatment Program (Lebanon, New Hampshire), Farnum Recovery Center (Manchester, New Hampshire), the Hartford Dispensary (Hartford and New Britain, Connecticut), Brattleboro Retreat (Brattleboro, Vermont), Clara Martin Center (Wilder, Vermont) and WestBridge Inc. (Manchester, New Hampshire). Kim Mueser, Stanley Rosenberg, Stephanie Acquilano, Beth Dickinson and Whitney Kling of the Dartmouth Psychiatric Research Center were key to the execution of this research.
Footnotes
DISCLOSURES
The authors report no financial relationships with commercial interests.
Contributor Information
Mark P. McGovern, Department of Psychiatry, Dartmouth Medical School, Lebanon, New Hampshire, USA
Chantal Lambert-Harris, Dartmouth Psychiatric Research Center, Dartmouth Medical School, Concord, New Hampshire, USA
Arthur I. Alterman, Department of Psychiatry, University of Pennsylvania, Philadelphia, Pennsylvania, USA
Haiyi Xie, Department of Community and Family Medicine, Dartmouth Medical School, Lebanon, New Hampshire, USA
Andrea Meier, Dartmouth Psychiatric Research Center, Dartmouth Medical School, Lebanon, New Hampshire, USA
REFERENCES
- Back S, Dansky BS, Coffey SF, Saladin ME, Sonne S, Brady KT. Cocaine dependence with and without post-traumatic stress disorder: A comparison of substance use, trauma history and psychiatric comorbidity. The American Journal on Addictions / American Academy of Psychiatrists in Alcoholism and Addictions. 2000;9(1):51–62. doi: 10.1080/10550490050172227. [DOI] [PubMed] [Google Scholar]
- Back SE, Brady KT, Sonne SC, Verduin ML. Symptom improvement in co-occurring PTSD and alcohol dependence. The Journal of Nervous and Mental Disease. 2006;194(9):690–696. doi: 10.1097/01.nmd.0000235794.12794.8a. [doi]; 00005053 200609000-00009 [pii] [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK. Manual for the beck depression inventory-II. San Antonio Texas: Psychological Corporation; 1996. [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, Keane TM. The development of a clinician-administered PTSD scale. Journal of Traumatic Stress. 1995;8(1):75–90. doi: 10.1007/BF02105408. [DOI] [PubMed] [Google Scholar]
- Brady KT. Treatments for PTSD or combined PTSD and drug abuse; NIDA Conference on Addressing Substance Abuse Comorbidities among Military Personnel, Veterans, and their Families; Bethesda MD: 2009. [Google Scholar]
- Brady KT, Dansky BS, Back SE, Foa EB, Carroll KM. Exposure therapy in the treatment of PTSD among cocaine-dependent individuals: Preliminary findings. Journal of Substance Abuse Treatment. 2001;21(1):47–54. doi: 10.1016/s0740-5472(01)00182-9. [DOI] [PubMed] [Google Scholar]
- Brady KT, Back SE, Coffey SF. Substance abuse and posttraumatic stress disorder. Current Directions in Psychological Science. 2004;13(5):206–209. [Google Scholar]
- Brown PJ, Recupero PR, Stout R. PTSD substance abuse comorbidity and treatment utilization. Addictive Behaviors. 1995;20(2):251–254. doi: 10.1016/0306-4603(94)00060-3. [DOI] [PubMed] [Google Scholar]
- Cacciola JS, Alterman AI, McLellan AT, Lin YT, Lynch KG. Initial evidence for the reliability and validity of a "lite" version of the addiction severity index. Drug and Alcohol Dependence. 2007;87(2–3):297–302. doi: 10.1016/j.drugalcdep.2006.09.002. 10.1016/j.drugalcdep.2006.09.002 [doi] [DOI] [PubMed] [Google Scholar]
- Cacciola JS, Alterman AI, McKay JR, Rutherford MJ. Psychiatric comorbidity in patients with substance use disorders: Do not forget axis II disorders. Psychiatric Annals. 2001;31:321–331. [Google Scholar]
- Corvino J, Carroll KM, Nuro K, Nich C, Sifry R, Frankforter T, Rounsaville BJ. Yale adherence and competence scale (YACS) guidelines. New Haven CT: Yale University Psychotherapy Development Center; 2001. [Google Scholar]
- Dansky BS, Saladin M, Brady K, Killeen T, Becker S, Roitzsch JD, Resnick H, Kilpatrick D. The nature of victimization among inpatient substance abusers; Poster presentation at the Annual Meeting of the Southeastern Psychological Association; New Orleans, LA: 1994. [Google Scholar]
- Donovan B, Padin-Rivera E, Kowaliw S. "Transcend": Initial outcomes from a posttraumatic stress disorder/substance abuse treatment program. Journal of Traumatic Stress. 2001;14(4):757–772. doi: 10.1023/A:1013094206154. [DOI] [PubMed] [Google Scholar]
- Drake RE, Mueser KT, Brunette MF. Management of persons with co-occurring severe mental illness and substance use disorder: Program implications. World Psychiatry : Official Journal of the World Psychiatric Association (WPA) 2007;6(3):131–136. [PMC free article] [PubMed] [Google Scholar]
- Flynn PM, Brown BS. Co-occurring disorders in substance abuse treatment: Issues and prospects. Journal of Substance Abuse Treatment. 2008;34(1):36–47. doi: 10.1016/j.jsat.2006.11.013. PMC2200799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frisman LK, Mueser KT, Covell NH, Lin H, Crocker A, Drake RE, Essock SM. Use of integrated dual disorder treatment via assertive community treatment versus clinical case management for persons with co-occurring disorders and antisocial personality disorder. Journal of Nervous and Mental Disease. 2009;197(11):822–828. doi: 10.1097/NMD.0b013e3181beac52. [DOI] [PubMed] [Google Scholar]
- Hien DA, Wells EA, Jiang H, Suarez-Morales L, Campbell AN, Cohen LR, Nunes EV. Multisite randomized trial of behavioral interventions for women with co-occurring PTSD and substance use disorders. Journal of Consulting and Clinical Psychology. 2009;77:607–619. doi: 10.1037/a0016227. PMC2795638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hien DA, Cohen LR, Miele GM, Litt LC, Capstick C. Promising treatments for women with comorbid PTSD and substance use disorders. The American Journal of Psychiatry. 2004;161(8):1426–1432. doi: 10.1176/appi.ajp.161.8.1426. [doi]; 161/8/1426 [pii] [DOI] [PubMed] [Google Scholar]
- Hien DA, Jiang H, Campbell ANC, Hu M, Miele GM, Cohen LR, Nunes EV. Do treatment improvements in PTSD severity affect substance use outcomes? A secondary analysis from a randomized clinical trial in NIDA's clinical trials network. The American Journal of Psychiatry. 2010;167(1):95–101. doi: 10.1176/appi.ajp.2009.09091261. PMC2806486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobsen LK, Southwick SM, Kosten TR. Substance use disorders in patients with posttraumatic stress disorder: A review of the literature. American Journal of Psychiatry. 2001;158(8):1184–1190. doi: 10.1176/appi.ajp.158.8.1184. [DOI] [PubMed] [Google Scholar]
- Kraemer HC, Mintz J, Noda A, Tinklenberg J, Yesavage JA. Caution regarding the use of pilot studies to guide power calculations for study proposals. Archives of General Psychiatry. 2006;63(5):484–489. doi: 10.1001/archpsyc.63.5.484. http://archpsyc.ama-assn.org/cgi/reprint/63/5/484. [DOI] [PubMed] [Google Scholar]
- Lipsey MW. Design sensitivity: Statistical power for experimental research. Newbury Park: Sage Publication; 1990. [Google Scholar]
- McGovern MP, Alterman AI, Drake KM, Dauten AP. Co-occurring PTSD and substance use disorders in addiction treatment settings. In: Mueser KT, Rosenberg SD, Rosenberg HJ, editors. Treatment of posttraumatic stress disorders in special populations: A cognitive restructuring program. Washington DC: American Psychological Association Press; 2009. [Google Scholar]
- McGovern MP, McLellan AT. The status of addiction treatment research with co-occurring substance use and psychiatric disorders. Journal of Substance Abuse Treatment. 2008;34(1):1–2. doi: 10.1016/j.jsat.2007.03.007. http://www.sciencedirect.com/science/article/B6T90-4P00S19-4/2/9b819ed7e832828b9db1332a9c35b0b7. [DOI] [PubMed] [Google Scholar]
- McGovern MP, Lambert-Harris C, Acquilano S, Xie H, Alterman AI, Weiss RD. A cognitive behavioral therapy for co-occurring substance use and posttraumatic stress disorders. Addictive Behaviors. 2009;34(10):892–897. doi: 10.1016/j.addbeh.2009.03.009. PMC2720425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLellan A, Grissom GR, Zanis D, Randall M, Brill P, O'Brien CP. Problem-service 'matching' in addiction treatment: A prospective study in 4 programs. Archives of General Psychiatry. 1997;54(8):730–735. doi: 10.1001/archpsyc.1997.01830200062008. [DOI] [PubMed] [Google Scholar]
- McLellan AT. New data from the addiction severity index: Reliability and validity in three centers. Journal of Nervous and Mental Disease. 1985;173(7):412–423. doi: 10.1097/00005053-198507000-00005. [DOI] [PubMed] [Google Scholar]
- McNamara C, Schumacher JE, Milby JB, Wallace D, Usdan S. Prevalence of nonpsychotic mental disorders does not affect treatment outcome in a homeless cocaine-dependent sample. The American Journal of Drug and Alcohol Abuse. 2001;27:91–106. doi: 10.1081/ada-100103120. [DOI] [PubMed] [Google Scholar]
- Mercer D, Woody G. Individual drug counseling. Rockville MD: National Institute on Drug Abuse; 1999. [Google Scholar]
- Mills KL, Teesson M, Ross J, Darke S, Shanahan M. The costs and outcomes of treatment for opioid dependence associated with posttraumatic stress disorder. Psychiatric Services. 2005;56(8):940–945. doi: 10.1176/appi.ps.56.8.940. 10.1176/appi.ps.56.8.940 [doi]: http://ps.psychiatryonline.org/cgi/reprint/56/8/940. [DOI] [PubMed] [Google Scholar]
- Morgenstern J, Blanchard KA, Morgan TJ, Labouvie E, Hayaki J. Testing the effectiveness of cognitive-behavioral treatment for substance abuse in a community setting: Within treatment and posttreatment findings. Journal of Consulting and Clinical Psychology. 2001;69(6):1007–1017. doi: 10.1037//0022-006x.69.6.1007. http://www.csa.com/ids70/gateway.php?mode=pdf&doi=10.1037%2F0022-006X.69.6.1007&db=psycinfo-set-c&s1=09d17a93e63e929b2fe4ee4a025436b7&s2=da3b4ccae91e4574c852cab6671d31b7. [DOI] [PubMed] [Google Scholar]
- Mueser KT, Noordsy DL, Drake RE, Fox L, Barlow DH. Integrated treatment for dual disorders: A guide to effective practice. New York, NY, US: Guilford Press; 2003. [Google Scholar]
- Mueser KT, Rosenberg SD, Jankowski MK, Hamblen JL, Descamps M. A cognitive-behavioral treatment program for posttraumatic stress disorder in persons with severe mental illness. American Journal of Psychiatric Rehabilitation. 2004;7(2):107–146. [Google Scholar]
- Mueser KT, Rosenberg SD, Rosenberg HJ. An overview of the cognitive restructuring for posttraumatic stress disorder program. Washington DC, US: American Psychological Association; 2009. [Google Scholar]
- Mueser KT, Rosenberg SD, Xie H, Jankowski MK, Bolton EE, Lu W, Wolfe R. A randomized controlled trial of cognitive-behavioral treatment for posttraumatic stress disorder in severe mental illness. Journal of Consulting and Clinical Psychology. 2008;76(2):259–271. doi: 10.1037/0022-006X.76.2.259. http://www.csa.com/ids70/gateway.php?mode=pdf&doi=10.1037%2F0022-006X.76.2.259&db=psycinfo-set-c&s1=09d17a93e63e929b2fe4ee4a025436b7&s2=e85ec7af2d7cf528805b550080df1c70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Najavits LM, Weiss RD, Liese BS. Group cognitive-behavioral therapy for women with PTSD and substance use disorder. Journal of Substance Abuse Treatment. 1996;13(1):13–22. doi: 10.1016/0740-5472(95)02025-x. [DOI] [PubMed] [Google Scholar]
- Najavits LM, Weiss RD, Shaw SR, Muenz LR. "Seeking safety": Outcome of a new cognitive-behavioral psychotherapy for women with posttraumatic stress disorder and substance dependence. Journal of Traumatic Stress. 1998;11(3):437–456. doi: 10.1023/A:1024496427434. [DOI] [PubMed] [Google Scholar]
- Nunes EV, Levin FR. Treatment of depression in patients with alcohol or other drug dependence: A meta-analysis. JAMA: The Journal of the American Medical Association. 2004;291(15):1887–1896. doi: 10.1001/jama.291.15.1887. http://jama.ama-assn.org/cgi/content/abstract/291/15/1887. [DOI] [PubMed] [Google Scholar]
- Onken LS, Blaine JD, Battjest R. Behavioral therapy research: A conceptualization of a process. In: Henngler SW, Amentos R, editors. Innovative approaches for difficult to treat populations. Washington, DC: American Psychiatric Press; 1997. pp. 477–485. [Google Scholar]
- Ouimette PC, Ahrens C, Moos RH, Finney JW. Posttraumatic stress disorder in substance abuse patients: Relationship to 1-year posttreatment outcomes. Psychology of Addictive Behaviors. 1997;11(1):34–47. [Google Scholar]
- Rogers JV. The integrated approach for the dually diagnosed: Concurrent individual and group psychotherapy with a dually diagnosed Mexican male in early recovery. 2001 (ProQuest Information & Learning). (Electronic; Print). (AAI3013722; 2001-95020-357. [Google Scholar]
- Rosen CS, Henson BR, Finney JW, Moos RH. Consistency of self-administered and interviewer-based addiction severity index composite scores. Addiction. 2000;95(3):419–425. doi: 10.1046/j.1360-0443.2000.95341912.x. [DOI] [PubMed] [Google Scholar]
- Rounsaville BJ, Carroll KM, Onken LS. A stage model of behavioral therapies research: Getting started and moving on from stage I. Clinical Psychology: Science & Practice. 2001;8:133–142. [Google Scholar]
- Sholomskas DE, Syracuse-Siewert G, Rounsaville BJ, Ball SA, Nuro KF, Carroll KM. We don't train in vain: A dissemination trial of three strategies of training clinicians in cognitive-behavioral therapy. Journal of Consulting and Clinical Psychology. 2005;73(1):106–115. doi: 10.1037/0022-006X.73.1.106. http://www.csa.com/ids70/gateway.php?mode=pdf&doi=10.1037%2F0022-006X.73.1.106&db=psycinfo-set-c&s1=09d17a93e63e929b2fe4ee4a025436b7&s2=12e01b82a36a5a7c4e76bed87ef0d684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell LC, Maisto SA, Sobell MB, Cooper AM. Reliability of alcohol abusers’ self-reports of drinking behavior. Behavioral Research and Therapy. 1979;17:157–160. doi: 10.1016/0005-7967(79)90025-1. [DOI] [PubMed] [Google Scholar]
- SPSS, Inc. SPSS 17.0 for windows. Chicago, IL: 2008. [Google Scholar]
- Triffleman E, Carroll K, Kellogg S. Substance dependence posttraumatic stress disorder therapy: An integrated cognitive-behavioral approach. Journal of Substance Abuse Treatment. 1999;17(1–2):3–14. doi: 10.1016/s0740-5472(98)00067-1. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Ruscio AM, Keane TM. Psychometric properties of nine scoring rules for the clinician-administered posttraumatic stress disorder scale. Psychological Assessment. 1999;11(2):124–133. [Google Scholar]
- Weathers FW, Litz BT, Herman DS, Huska JA, Keane TM. The PTSD Checklist: Reliability, validity, and diagnostic utility; Paper presented at the Annual Meeting of the International Society for Traumatic Stress Studies; San Antonio, TX: 1993. October. [Google Scholar]