Abstract
Purpose
Obesity is a common nutritional problem in both developed and developing countries. The aim of this study was to determine the prevalence of overweightness and obesity using both bioelectrical impedance analysis (BIA) and body mass index (BMI).
Methods
In this cross-sectional study, 288 healthy college students were selected. Socio-economic status questionnaires were completed and subjects’ anthropometric features were measured by a trained nurse. BMI was calculated and body fat mass (BFM) and body fat percent (BF%) were obtained using BIA method by hand-to-hand Omron BF-500 set.
Results
Mean age of the subjects was 21.1±1.7 years. Based on BMI, 2.6% of males and 2.2% of females were obese while 15.7% and 9.6% were diagnosed to be overweight respectively. The correlation between BMI values and BFM were 0.883 and 0.908 in males and females respectively (P<0.001). Furthermore, BF% had a significant correlation with BMI in both males and females (P<0.001).
Conclusion
Our survey demonstrated a lower prevalence of obesity and overweightness in college students compared with Iranian general population, especially in females. Additionally, BIA method was shown to be closely correlated with and as much valuable as BMI in regard to detection of obesity.
Keywords: Body Mass Index, Bioelectrical Impedance, Obesity, Students, Body Fat
INTRODUCTION
Obesity is a common nutritional problem in both developed and developing countries [1–3]. It affects approximately 300 million people and is accompanied by increased mortality and reduced life expectancy [4]. Its prevalence varies in different parts of the world. Factors such as education and socioeconomic status have important impact in both positive and negative ways. Urbanization, less physical activity, increased energy intake, and a modern life style are important risk factors for obesity. According to the increased prevalence of these risk factors, obesity is going to be a major problem in developing countries in the future [5].
A significant increase in the prevalence of obesity has been observed in Middle East. The prevalence of overweightness and obesity [Body Mass Index (BMI)>25] among adults in Kuwait was estimated to be 80.4%. In the age group of 20–24 years nearly 52.3% of males and 49.7% of females had more than 25 kg/m2 BMI [6]. The prevalence of being overweight and obese was estimated to be approximately 40% in Iran [7,8].
BMI classification has been debated in Asian population. A World Health Organization (WHO) study concluded that Asians have a higher percentage of body fat in comparison with white people. Besides, Asian people with risk factors for type II diabetes and cardiovascular disease had lower than 25 kg/m2 BMI. Thus, current cut-off point of overweightness and obesity is not suitable in many Asian populations [9].
Body impedance analysis (BIA), a relatively simple, quick and noninvasive body composition method, is reliable and easy to perform and is widely used to evaluate body composition. Conductance of a small alternating current through the body is measured in this method [10]. As the conductance is mainly determined by the amount of water, which is only present in the fat-free mass, BIA allows calculation of the fat-free mass and BF% accordingly [10].
Erceg DN et al showed that mean BF% calculated by BIA was not significantly different from dual energy x-ray absorptiometry (DXA) and hydrostatic weighing (HW)[11]. A good agreement was also detected between BIA and DXA [12].
The purpose of this study was to determine the prevalence of overweightness and obesity using both BIA and BMI. Furthermore, it was performed to evaluate the correlation between the two methods in a group of students in Shiraz University of Medical Sciences, Shiraz, South of Iran.
METHODS AND SUBJECTS
Subjects
In this cross-sectional study, 288 healthy students (153 males and 135 females) aged 18–27 years from Shiraz University of Medical Sciences were enrolled. They had no history of alcohol consumption or taking medications. The study protocol was approved by Ethics Committee of Shiraz University of Medical Sciences.
Variables and measurements
Socio-economic status questionnaires were completed and subjects’ anthropometric features including weight, height, BMI, waist circumference (WC), hip circumference (HC) and skinfold thickness were measured by a trained nurse. WC was determined by measuring waist diameter at midpoint between iliac crest and lower border of the tenth rib. An average of three measurements was considered as WC. Three skinfold (triceps, subscapular and abdominal) were taken. Skinfolds were measured in triplicate using the Harpenden caliper and the average of the right and left was used. Body weights and heights were measured using Seca digital scale (Germany) and a non-stretchable wall meter respectively. BMI was calculated as body weight in kilogram divided by square of height in meter.
Body Fat Mass (BFM) and body fat percent (BF%) were obtained using BIA method by hand-to-hand Omron BF-500 set, Japan. Subjects had to fast for at least 5 h, not engage into strenuous physical activity during the previous 12 hours and abstain from consuming caffeine beverages from 24 h before the study.
Central obesity was defined as WHR>0.80 or WC>88 for females and WHR>0.9 or WC>102 for males. The cutoff point of obesity according to American College of Sports Medicine is defined in young adults as body fat > 25% in males and >32% in females[13].
Statistical Analysis
Statistical Analysis was performed using statistical analysis software SPSS version 11.5. The descriptive variables such as mean, median and standard deviations were used. Statistical relationship between BF%, BFM, BMI and anthropometric characteristics was tested by Pearson's correlation coefficient. Independent sample T-test was performed to differentiate between anthropometric characteristics and sex. Chi square test was performed for analysis of statistical relationship between prevalence of obesity and sex. A P-value of less than 0.05 was considered statistically significant.
RESULTS
Mean age of the participants was 21.1±1.7 years (ranging from 18 to 27 years). Demographic characteristics revealed that 153 of the participant (53.1%) were male and 123 of them (42.7%) had physical activity. A total of 179 (62.2%), 36 (12.5%), 61 (21.2%) and 12 (4.2%) were Fars, Turk, Lore and others respectively regarding ethnicity. A significant difference was observed between males and females regarding weight, height, biceps, body fat mass, body fat percent, triceps, subscapular and abdominal thickness and mid-upper arm circumference, whereas it was not significant considering BMI (Table 1). Prevalence of obesity and central obesity based on BMI was not significantly different in males and females. However, the difference in the prevalence of obesity based on body fat percent was statistically significant between males and females (Table 2).
Table 1.
Mean and SD of anthropometric characteristics based on sex
| Anthropometric characteristics | Male Mean (SD) | Female Mean (SD) | P value |
|---|---|---|---|
| Weight (kg) | 67.2 (9.6) | 55.9 (7.4) | <0.001 |
| Height (cm) | 172.0 (5.4) | 159.1 (5.4) | <0.001 |
| Body fat mass (kg) | 10.9 (5.8) | 17.2 (5.8) | <0.001 |
| Body fat percent | 15.6 (6.2) | 30.3 (6.5) | <0.001 |
| Body mass index (kg/m2) | 22.7 (2.8) | 22.1 (3.0) | 0.09 |
| waist circumference (cm) | 79.2 (8.0) | 70.8 (7.4) | <0.001 |
| Mid-upper arm circumference (cm) | 26.2 (2.8) | 24.8 (2.9) | <0.001 |
| Waist-to-hip ratio | 0.85 (0.05) | 0.77 (0.07) | <0.001 |
| Triceps (mm) | 12.3 (4.2) | 21.5 (4.5) | <0.001 |
| Subscapular (mm) | 12.1 (4.4) | 18.1 (5.4) | <0.001 |
| Abdominal (mm) | 14.1 (5.8) | 19.4 (4.3) | <0.001 |
SD: Standard Deviation
Table 2.
Prevalence of obesity and central obesity based on sex
| Male Number (%) | Female Number (%) | P value | ||
|---|---|---|---|---|
| Body Mass Index (kg/m2) | <18.5 | 6 (3.9) | 5 (3.7) | 0.5 |
| 18.5-24.9 | 119 (77.8) | 114 (84.4) | ||
| 25-29.9 | 24 (15.7) | 13 (9.6) | ||
| >30 | 4 (2.6) | 3 (2.2) | ||
| Waist-to-hip ratio | Normal | 123 (82.0) | 105 (78.4) | 0.4 |
| Central obesity | 27 (18.0) | 29 (21.6) | ||
| Waist circumference | Normal | 148 (98.7) | 128 (95.5) | 0.1 |
| Central obesity | 2 (1.3) | 6 (4.5) | ||
| Body fat percent | Normal | 138 (91.4) | 82 (61.7) | <0.001 |
| Obese | 13 (8.6) | 51 (38.3) | ||
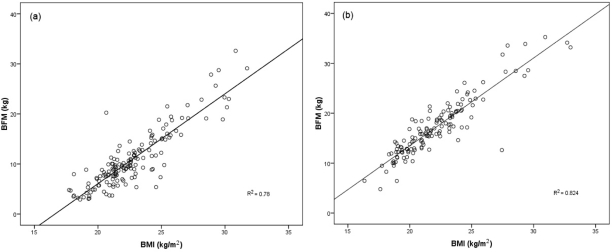
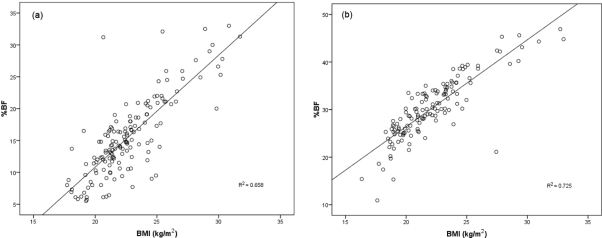
Table 3 demonstrates the correlation between various anthropometric characteristics. The correlation between BMI values and BFM were 0.883 and 0.908 in males and females respectively (P<0.001; Fig 1). Furthermore, BF% had a significant correlation with BMI in males and females (P<0.001; Fig. 2).
Table 3.
The correlation between anthropometric characteristics based on sex
| Groups | BMI | BF% | BFM | Triceps | Subscapular | Abdominal | |
|---|---|---|---|---|---|---|---|
| Male | BMI | 1 | 0.81* | 0.88* | 0.64* | 0.80* | 0.72* |
| BF% | 0.81* | 1 | 0.97* | 0.65* | 0.74* | 0.75* | |
| BFM | 0.88* | 0.97* | 1 | 0.68* | 0.79* | 0.78* | |
| Triceps | 0.64* | 0.65* | 0.68* | 1 | 0.74* | 0.73* | |
| Subscapular | 0.77* | 0.74* | 0.79* | 0.74* | 1 | 0.81* | |
| Abdominal | 0.72* | 0.75* | 0.78* | 0.73* | 0.81* | 1 | |
| Female | BMI | 1 | 0.85* | 0.91* | 0.68* | 0.65* | 0.39* |
| BF% | 0.85* | 1 | 0.96* | 0.69* | 0.64* | 0.42* | |
| BFM | 0.91* | 0.96* | 1 | 0.69* | 0.63* | 0.39* | |
| Triceps | 0.68* | 0.69* | 0.69* | 1 | 0.70* | 0.55* | |
| Subscapular | 0.65* | 0.64* | 0.63* | 0.70* | 1 | 0.62* | |
| Abdominal | 0.39* | 0.42* | 0.39* | 0.55* | 0.62* | 1 | |
BMI: body mass index; BF%: body fat percent; BFM: body fat mass
Correlation is significant at the 0.01 level.
Fig. 1.
Correlation between body mass index (BMI) and body fat mass (BFM) in males (a) and females (b)
Fig. 2.
Correlation between body mass index (BMI) and body fat percent (%BF) in males (a) and females (b)
DISCUSSION
An alarming increase in prevalence and incidence of obesity has been demonstrated in the World Health Organization's Global Disease Burden report, which estimates that being overweight is the 10th leading burden of disease worldwide [16]. Obesity has been shown to be a major determinant of high blood pressure, elevated cholesterol, metabolic syndrome and clearly an important primordial risk factor for cardiovascular diseases [7,14].
Many simple anthropometric measurements such as BMI based on height and weight are implemented to assess the body composition. Considering the variations of body composition in different ethnicities, the appropriateness of current BMI cutoffs in Asian populations, despite their widely accepted applications, has been questioned [9,15,16]. A widely accepted method for estimation of body composition is BIA, which is relatively simple, quick and noninvasive [11,17]. It can be applied to determine body composition in both healthy subjects [18–20] and patients being monitored [21–23].
Our investigation revealed that 2.6% of males and 2.2% of females were obese, while 15.7% and 9.6% were diagnosed to be overweight respectively. These findings are similar to the first National Non- Communicable Disease Risk Factor Surveillance survey, in which the prevalence of BMI ≥ 25 kg/m2 (obesity and overweightness) was estimated to be 22.3% and 42.8% in age groups of 15-24 and 15-64 respectively [24]. Another study conducted in northern Iran concluded that the prevalence of BMI ≥ 25 kg/m2 in 20-29-year-old age group was 31.5% in males and 36.9% in females [7]. The results of the third National Surveillance of Risk Factors of Non-communicable Diseases showed the prevalence of obesity and overweightness to be 36.2% and 58.6% in 25-34-year-old and 25-64-year-old age groups respectively [25]. Prevalence of obesity (BMI>30) in recent decade was estimated to be 13.7 and 27.3 for males and females with more than 18 years of age respectively [26]. Rapid nutritional transition and a changing lifestyle pattern are considered to be the leading causes of the current increase in the prevalence of obesity.
The prevalence of central obesity based on WC and WHR criteria has also been calculated in the present study. Although a higher prevalence of central obesity was observed in males, the difference was not statistically significant. In general, the prevalence of central obesity by WC criteria (1.3% for males and 4.5% for females) was lower than WHR criteria (18.0% for males and 21.6% for females). The rate calculated by WC criteria, reported by Hajian-Tilaki et al was 5.0% and 24.7% in males and females of the 20–29-year-old age group respectively [7]. According to the first nationwide survey of prevalence of obesity in adult Iranians, 3.2% of men and 18.1% of women were obese in the 20-29-year-old age group [24].
In general, our observation has established that there is a significant correlation between BFM and BMI and to a lower degree between BF% and BMI. Furthermore, this correlation was greater in women (r=0.86) compared with men (r=0.81), although it did not reach a statistical significance. (Table 3, Fig. 1 and 2). The correlation of BFM and BF% with thickness of triceps, subscapular and abdominal skinfolds and BMI was significant (P<0.001). Amani reported a similar correlation between BF% and BFM obtained from BIA method and BMI (r=0.86 and 0.77 respectively) [27]. In another investigation by Pecoraro et al. a significant correlation was detected between BFM measured by BIA and BMI (r=0.92) [28]. Additionally, Gallagher et al. showed a similar correlation between BF% obtained from DXA and BMI [29].
A limitation of the present study was the fact that it was conducted only in a university students’ population. Obviously, these indices should be evaluated in other populations as well.
CONCLUSION
Our survey demonstrated a lower prevalence of obesity and overweightness in university students compared with national reports of Iranian general population, especially females. This could have resulted from a better nutrition, diet and more exercise. Moreover, BIA was shown to be closely correlated with and as much valuable as BMI in detection of obesity. According to our results, BIA can be used easily and it is reliable to detect obesity in Iranian population.
ACKNOWLEDGMENTS
This work was financially supported by the Vice Chancellor for Research of Shiraz University of Medical Science. The authors declare that they have no conflicts of interest.
Conflict of interests: No conflict of interests amongst authors.
REFERENCES
- 1.Caballero B. A nutrition paradox–underweight and obesity in developing countries. N Engl J Med. 2005;352:1514–6. doi: 10.1056/NEJMp048310. [DOI] [PubMed] [Google Scholar]
- 2.Ayatollahi SMT, Heydari ST. Obesity indices among infants and their parents, Shiraz, Iran. Iran J Med Sci. 2004;29:161–7. [Google Scholar]
- 3.Heydari ST, Vakili MA, Emamghorashi F. Longitudinal pattern and reference values of obesity indices of infants in Jahrom (Southern Region of), Iran. Iran J Pediatr. 2008;18:38–46. [Google Scholar]
- 4.Fontaine KR, Redden DT, Wang C, et al. Years of life lost due to obesity. JAMA. 2003;289:187–93. doi: 10.1001/jama.289.2.187. [DOI] [PubMed] [Google Scholar]
- 5.Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser. 2000;894(i-xii):1–253. [PubMed] [Google Scholar]
- 6.Al Rashdan I, Al Nesef Y. Prevalence of overweight, obesity, and metabolic syndrome among adult Kuwaitis: results from community-based national survey. Angiology. 2010;61:42–8. doi: 10.1177/0003319709333226. [DOI] [PubMed] [Google Scholar]
- 7.Hajian-Tilaki KO, Heidari B. Prevalence of obesity, central obesity and the associated factors in urban population aged 20-70 years, in the north of Iran: a population-based study and regression approach. Obes Rev. 2007;8:3–10. doi: 10.1111/j.1467-789X.2006.00235.x. [DOI] [PubMed] [Google Scholar]
- 8.Rashidy-Pour A, Malek M, Eskandarian R, Ghorbani R. Obesity in the Iranian population. Obes Rev. 2009;10:2–6. doi: 10.1111/j.1467-789X.2008.00536.x. [DOI] [PubMed] [Google Scholar]
- 9.Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–63. doi: 10.1016/S0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]
- 10.Bioelectrical impedance analysis in body composition measurement: National Institutes of Health Technology Assessment Conference Statement. Am J Clin Nutr. 1996;64:524S–32S. doi: 10.1093/ajcn/64.3.524S. [DOI] [PubMed] [Google Scholar]
- 11.Erceg DN, Dieli-Conwright CM, Rossuello AE, et al. The Stayhealthy bioelectrical impedance analyzer predicts body fat in children and adults. Nutr Res. 2010;30:297–304. doi: 10.1016/j.nutres.2010.04.009. [DOI] [PubMed] [Google Scholar]
- 12.Gupta N, Balasekaran G, Victor Govindaswamy V, et al. Comparison of body composition with bioelectric impedance (BIA) and dual energy X-ray absorptiometry (DEXA) among Singapore Chinese. J Sci Med Sport. 2011;14(1):33–5. doi: 10.1016/j.jsams.2010.04.005. [DOI] [PubMed] [Google Scholar]
- 13.Whaley MH, Brubaker PH, Otto RM, editors. American College of Sports Medicine. ACSM's Guidelines for Exercise Testing and Prescription. 7 ed. Philadelphia: Lippincott Williams and Wilkins; 2005. pp. 70–4. [Google Scholar]
- 14.Kelly T, Yang W, Chen CS, et al. Global burden of obesity in 2005 and projections to 2030. Int J Obes (Lond) 2008;32:1431–7. doi: 10.1038/ijo.2008.102. [DOI] [PubMed] [Google Scholar]
- 15.Deurenberg-Yap M, Schmidt G, van Staveren WA, Deurenberg P. The paradox of low body mass index and high body fat percentage among Chinese, Malays and Indians in Singapore. Int J Obes Relat Metab Disord. 2000;24:1011–7. doi: 10.1038/sj.ijo.0801353. [DOI] [PubMed] [Google Scholar]
- 16.Razak F, Anand SS, Shannon H, et al. Defining obesity cut points in a multiethnic population. Circulation. 2007;115:2111–8. doi: 10.1161/CIRCULATIONAHA.106.635011. [DOI] [PubMed] [Google Scholar]
- 17.Lintsi M, Kaarma H, Kull I. Comparison of hand-to-hand bioimpedance and anthropometry equations versus dual-energy X-ray absorptiometry for the assessment of body fat percentage in 17–18-year-old conscripts. Clin Physiol Funct Imaging. 2004;24:85–90. doi: 10.1111/j.1475-097X.2004.00534.x. [DOI] [PubMed] [Google Scholar]
- 18.Kitano T, Kitano N, Inomoto T, Futatsuka M. Evaluation of body composition using dual-energy X-ray absorptiometry, skinfold thickness and bioelectrical impedance analysis in Japanese female college students. J Nutr Sci Vitaminol (Tokyo) 2001;47:122–5. doi: 10.3177/jnsv.47.122. [DOI] [PubMed] [Google Scholar]
- 19.Deurenberg P, Andreoli A, Borg P, et al. The validity of predicted body fat percentage from body mass index and from impedance in samples of five European populations. Eur J Clin Nutr. 2001;55:973–9. doi: 10.1038/sj.ejcn.1601254. [DOI] [PubMed] [Google Scholar]
- 20.Lloret LC, Ciangura C, Bouillot J, et al. Validity of Leg-to-Leg Bioelectrical Impedance Analysis to Estimate Body Fat in Obesity. Obes Surg. 2010 doi: 10.1007/s11695-010-0296-7. [Epub ahead of print] [PMID:20936394] [DOI] [PubMed] [Google Scholar]
- 21.Piccoli A, Codognotto M, Di Pascoli L, et al. Body mass index and agreement between bioimpedance and anthropometry estimates of body compartments in anorexia nervosa. JPEN J Parenter Enteral Nutr. 2005;29:148–56. doi: 10.1177/0148607105029003148. [DOI] [PubMed] [Google Scholar]
- 22.Lazzer S, Bedogni G, Agosti F, et al. Comparison of dual-energy X-ray absorptiometry, air displacement plethysmography and bioelectrical impedance analysis for the assessment of body composition in severely obese Caucasian children and adolescents. Br J Nutr. 2008;100:918–24. doi: 10.1017/S0007114508922558. [DOI] [PubMed] [Google Scholar]
- 23.Ha L, Hauge T, Iversen PO. Body composition in older acute stroke patients after treatment with individualized, nutritional supplementation while in hospital. BMC Geriatr. 2010;10:75. doi: 10.1186/1471-2318-10-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Janghorbani M, Amini M, Willett WC, et al. First nationwide survey of prevalence of overweight, underweight, and abdominal obesity in Iranian adults. Obesity (Silver Spring) 2007;15:2797–808. doi: 10.1038/oby.2007.332. [DOI] [PubMed] [Google Scholar]
- 25.Esteghamati A, Meysamie A, Khalilzadeh O, et al. Third national Surveillance of Risk Factors of Non-Communicable Diseases (SuRFNCD-2007) in Iran: methods and results on prevalence of diabetes, hypertension, obesity, central obesity, and dyslipidemia. BMC Public Health. 2009;9:167. doi: 10.1186/1471-2458-9-167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mirzazadeh A, Sadeghirad B, Haghdoost A, et al. The prevalence of obesity in Iran in recent decade; a systematic review and meta-analysis study. Iran J Public Health. 2009;38(3):1–11. [Google Scholar]
- 27.Amani R. Comparison between bioelectrical impedance analysis and body mass index methods in determination of obesity prevalence in Ahvazi women. Eur J Clin Nutr. 2007;61:478–82. doi: 10.1038/sj.ejcn.1602545. [DOI] [PubMed] [Google Scholar]
- 28.Pecoraro P, Guida B, Caroli M, et al. Body mass index and skinfold thickness versus bioimpedance analysis: fat mass prediction in children. Acta Diabetol. 2003;40:S278–81. doi: 10.1007/s00592-003-0086-y. [DOI] [PubMed] [Google Scholar]
- 29.Gallagher D, Heymsfield SB, Heo M, et al. Healthy percentage body fat ranges: an approach for developing guidelines based on body mass index. Am J Clin Nutr. 2000;72:694–701. doi: 10.1093/ajcn/72.3.694. [DOI] [PubMed] [Google Scholar]