Abstract
Some medical disorders can impair performance, increasing the risk of driving safety errors that can lead to vehicle crashes. The causal pathway often involves a concatenation of factors or events, some of which can be prevented or controlled. Effective interventions can operate before, during, or after a crash occurs at the levels of driver capacity, vehicle and road design, and public policy. A variety of systemic, neurological, psychiatric, and developmental disorders put drivers at potential increased risk of a car crash in the short or long term. Medical diagnosis and age alone are usually insufficient criteria for determining fitness to drive. Strategies are needed for determining what types and levels of reduced function provide a threshold for disqualification in drivers with medical disorders. Evidence of decreased mileage, self-restriction to driving in certain situations, collisions, moving violations, aggressive driving, sleepiness, alcohol abuse, metabolic disorders, and multiple medications may trigger considerations of driver safety. A general framework for evaluating driver fitness relies on a functional evaluation of multiple domains (cognitive, motor, perceptual, and psychiatric) that are important for safe driving and can be applied across many disorders, including conditions that have rarely been studied with respect to driving, and in patients with multiple conditions and medications. Neurocognitive tests, driving simulation, and road tests provide complementary sources of evidence to evaluate driver safety. No single test is sufficient to determine who should drive and who should not.
DR BURNS: Mr P is a 70-year-old right-handed man with a history of idiopathic Parkinson disease, hypertension, and atrial fibrillation. He has Medicare insurance.
Mr P was diagnosed as having idiopathic Parkinson disease 5 years ago. Currently, his main symptom is a right-hand resting tremor. Mr P also has a rapid eye movement sleep disorder with nocturnal movements and daytime sleepiness, as well as occasional double vision.
Mr P is a retired engineer and has enjoyed working on and driving race cars. In 2007, he voluntarily gave up race car driving because he felt that he had lost his “competitive edge” and because he experienced difficulty with depth perception.
Mr P has participated in annual driving evaluations since his diagnosis, with the most recent being administered 1 year prior to interview. At that time he felt that the cognitive aspects of driving were the most difficult for him, that he needed to concentrate very hard while driving, and that he was avoiding more complex environments. On physical examination, he had marked resting tremor of the right hand; visual acuity was 20/35 with normal visual fields, tracking, color vision, and depth perception. The brake reaction test showed that his reaction time was within normal limits at an average of 0.52 with the right foot and 0.45 with the left (<0.55 is within normal limits for the AAA Brake Reaction Timer). On the Trail-Making Test, which measures visual motor ability and attention, his results were in the 10th percentile for his age. He did well on cognitive screening measures, including rules of the road. On a standardized 1-hour on-road evaluation, he controlled the car well, followed the rules of the road, and was observant of others. He had slightly delayed processing and forgot to signal on 2 occasions. Based on this evaluation, he did not demonstrate deficits that would impede his capacity to drive a car. Repeat evaluation in 1 year was recommended.
Mr P has chosen to take minimal medications. He is currently taking digoxin, 250 μg/d; diltiazem, 30 mg/d; finasteride, 5 mg/d; and rasagiline, 1 tablet daily.
MR P: HIS VIEW
Driving has been a significant part of my life in that I've enthusiastically raced for a number of years. Part of the reason for getting into the driving evaluation program several years ago was to have a stable, carefully thought-out test that would be able to evaluate my driving skills. I used the program to make the decision as to when I would stop racing a car on a track. I did stop racing, but I'm still doing street driving at the present time. I have noticed in the last year that it is much more difficult to solve cognitive-type problems than before, including knowing where the rest of the cars are going, being able to keep track of where they are, and looking at road signs and figuring out where you're going, especially in places that you've never been before.
When you go through the driving evaluation program, you sign at the beginning that you are going to live with the findings of the professionals. If you fail to do this, they will turn your name over to the Registry of Motor Vehicles and the registry will deal with it in whatever manner they see fit.
I have decided that if I'm bothering people who are riding in the car because of what I'm doing or how I'm doing it, or if, in a driving evaluation, the evaluators think that my performance on the street is not what it should be, then I'll have to look and, just like in the racing mode, make the decision to not drive any more. Not driving will be a very dramatic and very disturbing thing. It certainly means it will be more difficult trying to get from one place to the other, and having to depend on somebody else to be able to drive you to various different places will most certainly be a burden, to put it mildly.
AT THE CROSSROADS: QUESTIONS FOR DR RIZZO
How do medical disorders place drivers at increased risk? What sources of evidence are available for determining driving competence and what is their accuracy in identifying at-risk drivers? What guidelines exist for at-risk drivers? What interventions can improve driver performance and what is the evidence of their effectiveness? What do you recommend for Mr P?
DR RIZZO: Mr P is a highly educated man and superior driver who could safely race cars. Now he has multiple risk factors for unsafe driving that can lead to a crash, including Parkinson disease with motor and cognitive impairments, vision and sleep disturbances, cardiac dysrhythmia, several medications, and advanced age. A framework for evaluating the fitness of drivers like Mr P relies on a “functional” evaluation of multiple domains (cognitive, motor, perceptual, and psychiatric) that are important for safe driving and can be applied across many disorders, including ones that have rarely been studied with respect to driving, and in patients with multiple conditions and medications. In general, no single test is sufficient to determine who should drive and who should not.
A variety of systemic, neurological, psychiatric, and developmental disorders put drivers at potential increased risk of a car crash; however, diagnosis alone usually is an insufficient criterion for driver decertification, and few diagnoses and treatments have been studied with respect to driving safety. The absence of evidence is an obstacle to accurately advising patients with medical disorders on whether they can drive safely or pose an unacceptably high risk of a crash. Without adequate evidence, physicians and other care-givers must often rely on intuition to restrict driving. Such decisions may unfairly deny individuals their mobility or unwisely sanction driving in crash-prone patients. In addition, states continue to look to clinicians for evidence on driving safety in medical disorders, evidence they often do not have, while clinicians appeal to the state for legal guidance. Further efforts to address the long-standing questions posed by Drachman1 (Who may drive, who may not, and who shall decide?) are clearly needed.2
Chain of Causality of Crashes in Medical Disorders
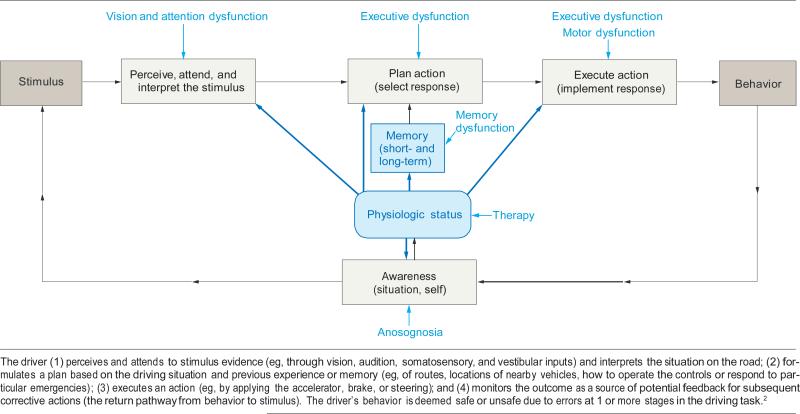
Medical disorders impair patient behavior and performance abilities, increasing the risk of errors that can lead to vehicle crashes (FIGURE).2 The causal pathway often involves a concatenation of factors or events, some of which can be prevented or controlled.3 Effective interventions can operate before, during, or after a crash occurs and at the levels of driver capacity, vehicle and road design, and public policy.4
Figure.
Information Processing Model for Understanding Errors That May Lead to Vehicle Crashes in Drivers With Medical Disorders
The relationship between driver behavior and safety errors can be represented as an iceberg in which visible, tip-of-the-iceberg events are safety errors that produce car crashes resulting in fatality, serious injury, mild injury, or (most often) only property damage.5,6 Hidden, below-the-waterline events occur more often and range from more innocuous errors, such as failing to check the rearview mirror on a deserted highway, to more serious errors, such as choosing to drive while impaired or distracted, leading to failure to brake or steer when needed, and producing traffic conflicts, near-crashes (“near-misses”), and, sporadically, traffic citations. Despite producing a devastating public health burden, crashes are relatively infrequent events in a statistical sense.
Medical disorders increase the risk of driver errors that may lead to crashes by causing impairments of attention, perception, response selection and implementation (which depend on memory, decision making, and other executive functions), emotional state, level of arousal or sleepiness, psychomotor factors, general mobility, and awareness of situation and self (metacognition).7-11 Operators normally monitor their performance and internal state, and when feed-back fails to match expectations, they normally detect the discrepancy and take corrective action.12 Drivers with cognitive impairments are less likely to realize their errors or impaired status, a metacognitive failure known as anosognosia, and are more likely to drive, unwittingly, while impaired. Anosognosia is not an all-or-none phenomenon, and subtle, undiagnosed forms of it may hinder patients with a range of perceptual and cognitive impairments, as in patients with sleep disorders, metabolic disorders, or cation effects who are not aware of how sleepy or cognitively impaired they really are.
Exactly how a particular medical disorder affects driving depends on the natural history, time course, severity, stage, and treatment of the disease. Patients with stroke may suddenly become unable to drive but may eventually recover and resume driving, whereas patients with Alzheimer disease or Parkinson disease (like Mr P) may drive safely at first, but with the inevitable progression of their condition, many, if not all, become unfit to ever drive again. Systemic diseases can produce encephalopathy with adverse consequences for driver safety, while fatigue, alcohol, and illicit drugs pose driving safety risks, as do many prescription medicines, (eg, anticonvulsants, antihistamines, antidepressants, antipsychotics and narcotics, and benzodiazepines). Relevant to Mr P, dopaminergic agents can produce adverse effects including psychosis, and higher dopamine equivalents predict a greater likelihood of stopping driving.13
The Federal Motor Carrier Safety Administration (FMCSA) has provided the most comprehensive review of the risk of motor vehicle crash for a variety of medical disorders (TABLE 1).
Table 1.
Federal Motor Carriers Safety Administration (FMCSA) Review of Crash Risk by Medical Disorders (2007-2010)14-18a
| FMCSA Evidence Report Medical Condition (Year) | Increased Crash Risk | Relative Risk (95% Confidence Interval) | No. of Studies With Direct Evidence | Strength of Evidence/Conclusion |
|---|---|---|---|---|
| Diabetes mellitus (2006) | Yes | 1.19 (1.08-1.31) | 13 | Weak |
| Schedule II licit medications (2006) | Cannot determine | 0 | Weak | |
| Cardiovascular disease (2006) | ||||
| Cardiovascular disease | Yes | 1.43 (1.11-1.84) | 8 | Acceptable |
| Hypertension | Yes | Estimate unstable | 2 | Acceptable |
| Seizure disorders (2007) | Yes | 1.13 to 2.16 | 8 | Moderate |
| Obstructive sleep apnea (2007) | Yes | 1.30 to 5.72 | 9 | Strong |
| Renal disease (2007) | Direct: no Indirect: plausible |
2 | Acceptable | |
| Vision (2007) | ||||
| Monocular vision | 4 | Insufficient | ||
| Red-green color deficiencies | 1 | Insufficient | ||
| Visual field loss | Yes | Indeterminate | 12 | Minimally acceptable |
| 240% Reduction in useful field of view | Yes | Indeterminate | 6 | Moderate |
| Cataracts | 4 | Insufficient | ||
| Diplopia | 1 | Insufficient | ||
| Musculoskeletal disease (2007) | ||||
| Amputation of extremity | No | 2 | Minimally acceptable | |
| Inflammatory arthritis | Indeterminate | 3 | Minimally acceptable | |
| Decreased angle of rotation at spine/neck | Indeterminate | 0 | Minimally acceptable | |
| Hearing (2008) | ||||
| Hearing impairment | No | 3 | Acceptable | |
| Vestibular dysfunction | Inconclusive | 1 | Not stated | |
| Psychiatric disease (2008) | ||||
| Psychiatric disease | Inconclusive | 8 | Minimally acceptable | |
| Psychotic disorders | Inconclusive | 4 | Minimally acceptable | |
| Mood disorders | Inconclusive | 3 | Not stated | |
| Anxiety disorders | Inconclusive | 1 | Not stated | |
| Personality disorders | Inconclusive | 3 | Not stated | |
| Benzodiazepine use | Yes | Not provided | 9 | Moderate |
| Antipsychotic use | Inconclusive | 1 | . . . | |
| Antidepressant use | Inconclusive | 7 | Minimally acceptable | |
| Stroke (2009) | Yes | Indeterminate | 3 | Minimally acceptable |
| Parkinson disease (2009) | Yes, for Hoehn and Yahr stages 2 and 3 | Not provided | 3 | Minimally acceptable |
| Multiple sclerosis (2009) | Inconclusive | Indeterminate | 2 | Not stated |
| Traumatic brain injury (2010) | Inconclusive | 1.32 (0.77-2.25) | 5 | Moderate |
Inconclusive indicates insufficient evidence to determine whether risk is increased. Indeterminate indicates could not be determined from the available evidence. If inconclusive or insufficient evidence was available, no crash risk could be estimated.
Diabetes
Diabetes is a prime example of the effects of metabolic disorders and encephalopathy on automobile driving. In a meta-analysis, the relative risk of crash among drivers with diabetes was 1.19 (95% confidence interval, 1.08-1.31) vs comparable drivers without diabetes.19 Hypoglycemia and glycemic variability are key risk factors to consider.20 A prospective 12-month study of 452 drivers with type 1 diabetes showed that 52% had 1 and 5% had 6 hypoglycemia-related driving mishaps; these self-reported mishaps were related to driver exposure (mileage) and insulin pump use.21 Tight control of diabetes intended to reduce long-term complications can increase the risk of hypoglycemic episodes and impair cognitive abilities (attention, memory, and decision making)22-24 needed for the safe and continuous performance of complex high-risk tasks such as automobile driving. Furthermore, some drivers with diabetes are unaware of their hypoglycemic status25,26 and may unknowingly expose themselves to excess risk by driving while impaired. A key source of feedback that may help mitigate hypoglycemia and improve driving safety in diabetes is continuous glucose monitoring27 with real-time feedback of low glucose levels via auditory and tactile alarms.28
Sleep Disorders
Excessive daytime sleepiness has many causes in a 24-hour society, underpins a large number of reported motor vehicle collisions (35%-42%),29,30 and may be second only to alcohol in crash causation. Chronic insomnia, narcolepsy, restless leg syndrome, dementia, epilepsy, and medications can all contribute to sleep disturbances, sleep deprivation, and excessive daytime sleepiness.31 Patients with Parkinson disease, like Mr P, may be excessively sleepy because of their disease or dopaminergic therapy.32 Drivers with obstructive sleep apnea are at increased risk of a motor vehicle collision compared with drivers without sleep apnea (relative risk of crash, 2.72; 95% confidence interval, 1.30-5.72; P = .008) because of impairments of vigilance, cognition, and falling asleep at the wheel.33 The treatment for obstructive sleep apnea, continuous positive airway pressure (CPAP), is effective, but adherence is a problem and it is unclear how CPAP-adherent a patient must be (in terms of hours of nightly CPAP for consecutive nights) to become as safe as a comparable driver without sleep apnea or whether there are long-term residual effects of sleep apnea on driver safety. Some sleepy drivers are not aware of their impaired status,34-37 possibly because of related cognitive impairment or an altered frame of reference for fatigue,38 and may be less likely to restrict themselves from driving despite being at increased risk of a crash. Preemptive countermeasures seek to prevent sleepy drivers from entering the road, in the case of commercial motor vehicle drivers through mandated duty cycles, driver logs, and other tools. In-vehicle sleepiness detection devices exist for private and commercial use and can be based on physiologic changes, physical activity and behavioral measures (eg, eye fixation activity, lid aperture/ closure, physiognomy), and model-based predictions of sleepiness.33
Role of Age
The increased crash risk seen at the extremes of age is often depicted as the tails of a U-shaped curve. Licensed drivers aged 60 years or older, the peers of Mr P, have among the highest crash rates per mile of all age groups, approaching the rate of the risky and much less experienced cohort of drivers younger than 25 years.39 The increased crash risk of older drivers is probably due to multiple medical problems and medication use that accompany aging rather than age itself. In addition, older drivers are frailer and more likely to be killed or injured in a car crash than are younger adults. Yet older adults in the United States, Mr P included, favor driving as the main means of travel40,41 and are at increased risk of depression and decreased quality of life when they stop driving.42,43
Evidence of Driving Competence
Several tools provide evidence relevant to driver behavior and performance, including tests of reaction time and sensory perception, standardized neuropsychological tests that are capable of measuring levels of cognitive performance in health or disease (but that are not as good at predicting real-world driving performance), computer-based tests that may use world images (eg, change detection and hazard perception tasks), simulators (including task-focused, non–motion-based, and multicapable motion-based), driving in the real world (on a test track, on a state road test, in an instrumented vehicle), and naturalistic driving (in the driver's own car, over extended time frames). Each tool has its advantages and drawbacks and the one selected to evaluate the medically disordered driver depends on the question being asked (TABLE 2). The tools furnish related results but their ability to predict driving outcomes is attenuated because driving behavior depends strongly on context and individuals may behave differently in the real world.
Table 2.
Advantages and Disadvantages of Different Sources of Evidence of Driving Competency
| Source | Advantages | Disadvantages |
|---|---|---|
| Driving simulation | Safe, without injury risks of road or test track Best means to replicate exactly experimental road conditions under which driver decisions are made Can be used to quantify performance profiles in cognitively impaired drivers (eg, advanced age, Alzheimer disease, Parkinson disease, stroke, traumatic brain injury, multiple sclerosis, obstructive sleep apnea, alcohol/drug use) |
Drivers may behave differently in a simulator, where no injury can occur Testing validity may require laborious detailed comparisons with state records of crashes and moving violations and with real-life performance in an instrumented vehicle or in a state road test Simulator adaptation syndrome |
| State road test2 | Considered gold standard of driver fitness Assesses driving performance under direct supervision of trained expert Performance graded along several dimensions to calculate cutoff score used to designate drivers as safe or unsafe |
Developed to ensure that novice drivers know and apply rules of the road, not to test experienced drivers who may be impaired Few data show that road tests correlate with crash involvement Risk of the road to the driver and examiner Test conditions vary depending on weather, daylight, traffic, and route Driving experts have different biases and grading criteria |
| Instrumented vehicles | Permit quantitative assessment of driver performance under actual road conditions Assessment can incorporate standard maneuvers deemed essential to driving such as turns, observance of traffic signs and signals, maintenance of vehicle control, and response to standard cognitive challenges (eg, route finding; sign identification; multitasking, as in conversation or using in-vehicle telematics devices such as cell phones and navigation devices) while driving Measurements are not subject to human bias that affects interrater reliability on a standard road test |
Risk of the road environment |
| Event recorders | Deployed in driver's own vehicle, these black box systems allow detailed assessment of driver safety in naturalistic settings over extended times without an examiner present May disclose specific situations or settings in which a driver is prone to making safety errors |
Confidentiality of electronic and video data Taxonomies of understanding errors are needed |
| State crash records | Often provide main basis for judging fitness of drivers who have not had road test Are more accurate and impartial than reports of drivers, relatives, and friends Provide details on time of day, road and weather conditions, and crash type, which drivers may forget |
Crashes are uncommon, and unsafe drivers may not have had a crash Some crashes are inevitable, caused by factors extrinsic to the driver Driver reporting of crashes may be unreliable Individuals with faulty memory underreport crashes Injured parties may not remember what happened Single car crashes often have no reliable witnesses No direct observations of actions leading up to a crash Specific details on mechanisms of a crash are generally missing |
Driving Tests
Historically, state road tests have been used as the gold standard of driving ability,2 but they were designed to test whether novice drivers know and can apply the rules of the road, not to predict crash involvement in skilled drivers who may now be impaired. Other sources of evidence on driver performance and behavior and their pros and cons are shown in Table 2.
In addition, modern vehicles now allow detailed information from the driver's own car to be collected over extended time frames.44 Speed and performance measures can be reported via the vehicle's on-board diagnostics port, lane-tracking video can assess lane-keeping behavior, radar systems can measure proximity, following distance, and lane-merging behavior,45 global positioning systems can show where and when a driver drives, and cell phone use can be tracked to assess a driver. Aspects of these data can be examined in a road test conducted in an instrumented vehicle or using an event recorder deployed in the driver's own vehicle over extended times.
Neurocognitive, Perceptual, and Self-report Tools
Standardized neuropsychological tests provide quantitative estimates of specific cognitive abilities, and have been found to predict driving performance to varying degrees in different patient populations as well as in older drivers. Raw scores (eg, uncorrected for age or education) tend to be better predictors than adjusted scores of driver performance on the road, where raw ability matters more.46 Impaired performance on some of these tasks (eg, Rey-Complex Figure Test, Trail-Making Test [performed by Mr P], composite measures [eg, “Cogstat”]) may be predictive of driving safety risk7,47 and of real-world driver errors, even in the absence of neurological disease.7,47,48
Use of neuropsychiatric tests alone needs to be cautious because multiple factors attenuate the relationship between test performance and driving, including decisions such as what vehicle to drive, how often and where to drive and under what road conditions, choosing to be distracted (eg, by eating, texting, conversing on cell phones), and how a driver values speed over safety. And while poor performance on laboratory tests would appear to predict greater likelihood of crashes and moving violations, the impaired driver might avert these outcomes by restricting his or her driving.
Various questionnaires assess relevant factors such as age, education, sex, general health, vision status, mobility, and chronic health conditions. The psychological state of a driver can be screened using the General Health Questionnaire49 and the Beck Depression Inventory.50 Chronic sleep disturbances can be assessed from self-report on the Epworth Sleepiness Scale.51,52 Frequency of driving can be assessed using a Driving Habits Questionnaire.53 The Dula Dangerous Driving Index measures self-reported likelihood to drive dangerously; each subscale (total, aggressive driving, negative emotional driving, and risky driving) shows strong internal reliability54 and scores have been linked to drunk driving, aggressive driving, and speeding violations.
Visual assessment can include tests of letter acuity (eg, the Early Treatment Diabetic Retinopathy Study chart55) and contrast sensitivity.56 Useful field of view reduction in patients who have normal visual fields can be demonstrated using visual tasks under differing attention loads.53 Overall visual health can be assessed with the National Eye Institute Visual Functioning Questionnaire–25.57 The FMCSA conducted a comprehensive review of how well visual tests (of acuity, contrast sensitivity, visual fields, and color) and disorders (age-related macular degeneration, cataract, glaucoma, diabetic retinopathy) predict driving outcomes.58
Guidelines for At-Risk Drivers
The American Medical Association/National Highway Traffic Safety Administration,59,60 American Academy of Ophthalmology,61 American Association of Motor Vehicle Administrators,62 FMCSA, and American Academy of Neurology have guidelines for at-risk drivers with visual, cognitive, or medical impairments based on current peer-reviewed evidence, previous guidelines, and standards of medical practice (TABLE 3). These guidelines by necessity are based on minimal quantitative data linking medical disorders and driving outcomes and “treatment” of unsafe driving (eg, restricting driving, educational interventions, on-board assistive devices, therapy for disease).
Table 3.
Recommendations in Driving Guidelines Published by Medical Organizations and the US Governmenta
| AMA/NHTSA59,60 | FMCSA (USDOT)58 | AAO61 | AAMVA/NHTSA62 | AAN63 | |
|---|---|---|---|---|---|
| Medical condition | |||||
| Vision | |||||
| Monocular vision | + | I | + | ||
| Red-green color deficiencies | + | I | + | + | |
| Visual field loss | + | + | + | + | |
| Reduced useful field of view | + | + | + | ||
| Cataracts | + | I | + | ||
| Diplopia | + | I | + | ||
| Hearing | |||||
| Hearing impairment | + | + | + | ||
| Vestibular dysfunction | + | I | |||
| Cardiovascular disease | |||||
| Cardiovascular disease | + | + | + | ||
| Hypertension | + | + | + | ||
| Cerebrovascular disease | + | + | + | ||
| Neurological diseases | + | + | + | + | |
| Psychiatric disease | |||||
| Psychotic disorders | + | I | + | ||
| Mood disorders | + | I | + | ||
| Anxiety disorders | + | I | + | ||
| Personality disorders | + | I | + | ||
| Benzodiazepine use | + | + | + | ||
| Antipsychotic use | + | I | + | ||
| Antidepressant use | + | I | + | ||
| Metabolic disorders | + | + | + | ||
| Musculoskeletal disease | |||||
| Amputation of extremity | + | I | + | ||
| Inflammatory arthritis | + | I | + | ||
| Decreased angle of rotation at spine/neck | + | I | + | ||
| Peripheral vascular diseases | + | ||||
| Renal disease | + | + | |||
| Respiratory diseases | + | + | |||
| Effects of anesthesia and surgery | + | ||||
| Miscellaneous conditions | + | + | |||
| Medications | + | I | + | ||
| Multiple risk factors | + | + | |||
+ indicates that recommendations are available; I, recommendations are inconclusive. The American Medical Association/National Highway Traffic Safety Administration (AMA/NHTSA), American Association of Motor Vehicle Administrators (AAMVA)/NHTSA, and American Academy of Ophthalmology (AAO) guidelines rely on professional opinions and literature reviews of the best available articles. The American Academy of Neurology (AAN) uses standardized evidence grading schema that range from class 1 (randomized clinical trials) to class 4 (observational studies with no controls that have less reliability for practice).64 The Federal Motor Carrier Safety Administration (FMCSA)/US Department of Transportation (USDOT) Evidence Reports are based on systematic reviews of the literature and are presented in more detail in Table 1.
In addition, the American Academy of Neurology practice guidelines use an algorithm for cognitively impaired drivers.63 A Clinical Dementia Rating (CDR) score of 0.5 to 1.0 should prompt evaluation of driver risk factors, namely caregiver report of marginal or unsafe skills (level B evidence); history of citations, history of crashes, driving less than 60 miles per week, situation avoidance, aggression or impulsivity, or Mini-Mental State Examination score of less than 24 (level C evidence); and other factors (alcohol and medication use, sleep disorders, visual impairment, and motor impairment). A driver with a CDR score of 2 is judged to have an unacceptably high risk for driving and risk mitigation strategies are advised, such as encouraging family support for alternate transportation, professional driving evaluation, voluntary surrender of driving privileges, or referral for a state-administered driving test.
Interventions to Improve Driving Performance
A rigorous study showed that a comprehensive 1-to-1 driver safety training program did not reduce older driver crash rates.65 Cognitive interventions with speed-of-processing and attention training may help mitigate crash risk in some of these drivers,66,67 yet it may be difficult to train the brain of a person with progressive neurodegenerative impairment (such as Mr P) to improve performance in a sustained and meaningful way. Instead, other approaches include modifying environmental exposure and behavioral interventions to enhance drivers’ knowledge and awareness of their own actual driving safety errors so that they avoid the hazardous situations in which these errors are most likely to occur. In the future, on-board driver-assist and collision warning devices potentially could mitigate the risk of cognitively impaired drivers.
RECOMMENDATIONS FOR MR P
Mr P is at increased risk of unsafe driving because of multiple medical factors, including Parkinson disease, atrial fibrillation, and medications, and associated declines in cognitive performance, motor function, and behavior. Mr P has already begun to restrict his exposure to driving.
Most, if not all, patients with neurodegenerative disorders eventually have to stop driving altogether, and clinicians should be able to knowledgeably discuss this prospect with patients like Mr P and their families soon after diagnosis. With forewarning and preparation, a patient with a progressive disorder can begin to reduce driving over time, preparing for likely eventual cessation.
A clinician has a moral responsibility to recommend what is best for a patient, although patients may disagree with advice to curtail driving. Mandatory reporting laws for driving risk vary by jurisdiction, and clinicians, patients, and their families must know their local laws. A clinician needs to judge the risks that a patient poses, how reluctant the patient is to cease driving, any legal guidelines in terms of ability, and the effects of limiting or ceasing driving on the patient's independence. Alternatives to driving can be explored.68
Mr P may wish to continue driving for now, albeit with recommended restrictions. He has a highly educated and involved spouse and access to sophisticated medical care and driving specialists to advise him. Based on the American Academy of Neurology guidelines (admittedly designed for dementia, not Parkinson disease), Mr P should have a 6-month reassessment.
QUESTIONS AND DISCUSSION
QUESTION: Sometimes a physician suspects that a patient is an unsafe driver and recommends a driving evaluation. What can be done if the patient refuses the test or doesn't want to stop driving no matter what?
DR RIZZO: We don't want to coerce patients to take tests they don't want or can't afford. Private driving tests are often not covered by insurance. If the clinical evidence raises questions of driver fitness, a physician may refer a person to a state's department of motor vehicles for a driving test. The driver is more likely to show up if license renewal depends on taking the test. State driving tests are included in the licensing fee. It is possible to make a convincing argument for driver testing based on family report, driving history, and clinical evidence, including disease severity and cognitive test scores. Most patients respect the opinion of a caring person in a white coat and would strive to avoid potential risks understood in terms of crashes and injuries to themselves, passengers, and family members. Alternate transportation planning is helpful, but sometimes the family has to hide the car keys.
QUESTION: Could you specify the level of performance on a cognitive test, such as the Trail-Making Test, in terms of the risk of drunk driving with a blood alcohol concentration (BAC) of 0.08% or some other gauge of driver risk?
DR RIZZO: Population-based crash rates are often given in terms of crashes per 1 million or 100 million miles traveled. Relative risk of an alcohol-related motor vehicle crash varies widely69 and increases exponentially at around a BAC of 0.08%,70 making it hard to draw the line for acceptable crash risk on a test such as the Trail-Making Test based on BAC. Male teenage drivers have the greatest level of driver risk accepted by society and might provide a threshold for acceptable risk in terms of mileage-adjusted crash rates. Yet, self-estimates of driving mileage on which these estimates depend are often inaccurate, and we cannot confidently specify the test scores that correspond to this threshold. This supports an argument for measuring behavior in the real world using event-triggered “black box” recorders.
QUESTION: How far developed are these event recorders and what do they cost?
DR RIZZO: Event recorders are available now and are being used to examine the safety of novice teenage drivers, professionals (including truck and bus drivers), and patients.71-76 Such a device typically costs a few hundred dollars, and there may be a recurring fee for cellular transmission or analysis of data. Service costs are evolving but currently range between $1000 and $2000 per year. A “black box” recorder may disclose that a driver is prone to making safety errors on a particular roadway segment or driving task or for a certain amount of time after taking or missing a dose of a particular drug. The information could be used to develop specific strategies and to inform individualized interventions (including situation awareness and avoidance, education, and treatment), putting this intervention in line with the promise of personalized medicine.
Acknowledgement
We would like to thank the patient for sharing his story. Research supported by NIH NIA RO1 AG 17177, NIA R01 AG026027 and NIA RO1 AG 15071 and NHLBI RO1 HL091917
Footnotes
This conference took place at the Neurology Grand Rounds at the Beth Israel Deaconess Medical Center, Boston, Mass, on December 2nd, 2009.
REFERENCES
- 1.Drachman DA. Who may drive? who may not? who shall decide? Ann Neurol. 1988;24(6):787–788. doi: 10.1002/ana.410240614. [DOI] [PubMed] [Google Scholar]
- 2.Rizzo M, Kellison IL. The brain on the road. In: Grant I, Marcotte TD, editors. Neuropsychology of Everyday Functioning: The Science and Practice of Neuropsychology. Guilford Press; New York, NY: 2010. pp. 168–208. [Google Scholar]
- 3.Runyan CW. Using the Haddon matrix: introducing the third dimension. Inj Prev. 1998;4(4):302–307. doi: 10.1136/ip.4.4.302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Haddon W., Jr A logical framework for categorizing highway safety phenomena and activity. J Trauma. 1972;12(3):193–207. doi: 10.1097/00005373-197203000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Heinrich HW, Petersen D, Roos NR, Brown J, Hazlett S. Industrial Accident Prevention: A Safety Management Approach. McGraw-Hill Companies; New York, NY: 1980. [Google Scholar]
- 6.Maycock G. Accident liability—the human perspective. In: Rothengatter T, Carbonell VE, editors. Traffic and Transport Psychology: Theory and Application. Pergamon; New York, NY: 1997. pp. 65–76. [Google Scholar]
- 7.Dawson JD, Anderson SW, Uc EY, Dastrup E, Rizzo M. Predictors of driving safety in early Alzheimer disease. Neurology. 2009;72(6):521–527. doi: 10.1212/01.wnl.0000341931.35870.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Marottoli RA, Cooney LM, Jr, Wagner R, Doucette J, Tinetti ME. Predictors of automobile crashes and moving violations among elderly drivers. Ann Intern Med. 1994;121(11):842–846. doi: 10.7326/0003-4819-121-11-199412010-00003. [DOI] [PubMed] [Google Scholar]
- 9.Rizzo M, McGehee DV, Dawson JD, Anderson SN. Simulated car crashes at intersections in drivers with Alzheimer disease. Alzheimer Dis Assoc Disord. 2001;15(1):10–20. doi: 10.1097/00002093-200101000-00002. [DOI] [PubMed] [Google Scholar]
- 10.Rizzo M, Reinach S, McGehee D, Dawson J. Simulated car crashes and crash predictors in drivers with Alzheimer disease. Arch Neurol. 1997;54(5):545–551. doi: 10.1001/archneur.1997.00550170027011. [DOI] [PubMed] [Google Scholar]
- 11.Uc EY, Rizzo M, Anderson SW, Sparks JD, Rodnitzky RL, Dawson JD. Driving with distraction in Parkinson disease. Neurology. 2006;67(10):1774–1780. doi: 10.1212/01.wnl.0000245086.32787.61. [DOI] [PubMed] [Google Scholar]
- 12.Wickens C, editor. Engineering, Psychology and Human Performance. 2nd ed. Harper Collins; New York, NY: 1992. [Google Scholar]
- 13.Uc EY, Rizzo M, Dastrup E, Liu D, Anderson S, Dawson J. Real-life driving outcomes in mild-moderate Parkinson's disease. Neurology. 2010;74(suppl 2):A58. [Google Scholar]
- 14.Tregear SJ, Tiller M, Federal Motor Carrier Safety Administration [February 16, 2011];Executive Summary: Diabetes and Commercial Motor Vehicle Driver Safety. 2006 September 8; http://www.fmcsa.dot.gov/rules-regulations/TOPICS/mep/report/Final-Diabetes-Executive-Summary-prot.pdf.
- 15.Tregear SJ, Tiller M, Price N, Federal Motor Carrier Safety Administration [February 16, 2011];Executive Summary: Cardiovascular Disease and Commercial Motor Vehicle Driver Safety. 2007 April 10; http://www.fmcsa.dot.gov/rules-regulations/TOPICS/mep/report/Final-Executive-Summary-prot.pdf.
- 16.Tiller M, Tregear S, Fontanarossa J, Price N, Federal Motor Carrier Safety Administration [February 16, 2011];Executive Summary: Seizure Disorders and Commercial Motor Vehicle Driver Safety. 2007 November 30; http://www.fmcsa.dot.gov/rules-regulations/TOPICS/mep/report/Final-Seizure-Executive-Summary-prot.pdf.
- 17.Tregear SJ, Tiller M, Fontanarrosa J, Price N, Akafomo C, Federal Motor Carrier Safety Administration [February 16, 2011];Executive Summary: Obstructive Sleep Apnea and Commercial Motor Vehicle Driver Safety. 2007 July 12; http://www.fmcsa.dot.gov/rules-regulations/TOPICS/mep/report/Sleep-Apnea-Final-Executive-Summary-prot.pdf.
- 18.Reston JT, Tregear S, Federal Motor Carrier Safety Administration [February 16, 2011];Executive Summary: Traumatic Brain Injury and Commercial Motor Vehicle Driver Safety. 2009 March 30; http://www.fmcsa.dot.gov/rules-regulations/TOPICS/mep/report/TraumaticBrainInjury_ExecutiveReport.pdf.
- 19.Tregear SJ, Rizzo M, Tiller M, et al. Proceedings of Driving Assessment 2007: The Fourth International Driving Symposium on Human Factors in Driver Assessment, Training, and Vehicle Design. University of Iowa; Iowa City: 2007. Diabetes and motor vehicle crashes: a systematic evidence-based review and meta-analysis. pp. 343–350. [Google Scholar]
- 20.Bragd J, Adamson U, Bäcklund LB, Lins PE, Moberg E, Oskarsson P. Can glycaemic variability, as calculated from blood glucose self-monitoring, predict the development of complications in type 1 diabetes over a decade? Diabetes Metab. 2008;34(6 pt 1):612–616. doi: 10.1016/j.diabet.2008.04.005. [DOI] [PubMed] [Google Scholar]
- 21.Cox DJ, Ford D, Gonder-Frederick L, et al. Driving mishaps among individuals with type 1 diabetes: a prospective study. Diabetes Care. 2009;32(12):2177–2180. doi: 10.2337/dc08-1510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lobmann R, Smid HG, Pottag G, Wagner K, Heinze HJ, Lehnert H. Impair ment and recovery of elementary cognitive function induced by hypoglycemia in type-1 diabetic patients and healthy controls. J Clin Endocrinol Metab. 2000;85(8):2758–2766. doi: 10.1210/jcem.85.8.6737. [DOI] [PubMed] [Google Scholar]
- 23.Weinger K, Kinsley BT, Levy CJ, et al. The perception of safe driving ability during hypoglycemia in patients with type 1 diabetes mellitus. Am J Med. 1999;107(3):246–253. doi: 10.1016/s0002-9343(99)00221-1. [DOI] [PubMed] [Google Scholar]
- 24.Wright RJ, Frier BM, Deary IJ. Effects of acute insulin-induced hypoglycemia on spatial abilities in adults with type 1 diabetes. Diabetes Care. 2009;32(8):1503–1506. doi: 10.2337/dc09-0212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cryer PE. Diverse causes of hypoglycemia-associated autonomic failure in diabetes. N Engl J Med. 2004;350(22):2272–2279. doi: 10.1056/NEJMra031354. [DOI] [PubMed] [Google Scholar]
- 26.Heller SR, Macdonald IA. The measurement of cognitive function during acute hypoglycaemia: experimental limitations and their effect on the study of hypoglycaemia unawareness. Diabet Med. 1996;13(7):607–615. doi: 10.1002/(SICI)1096-9136(199607)13:7<607::AID-DIA159>3.0.CO;2-I. [DOI] [PubMed] [Google Scholar]
- 27.Tamborlane WV, Beck RW, Bode BW, et al. Juvenile Diabetes Research Foundation Continuous Glucose Monitoring Study Group. Continuous glucose monitoring and intensive treatment of type 1 diabetes. N Engl J Med. 2008;359(14):1464–1476. doi: 10.1056/NEJMoa0805017. [DOI] [PubMed] [Google Scholar]
- 28.McGarraugh G. Alarm characterization for continuous glucose monitors used as adjuncts to self-monitoring of blood glucose. J Diabetes Sci Technol. 2010;4(1):41–48. doi: 10.1177/193229681000400106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dingus TA, Hardee HL, Wierwille WW. Development of models for on-board detection of driver impairment. Accid Anal Prev. 1987;19(4):271–283. doi: 10.1016/0001-4575(87)90062-5. [DOI] [PubMed] [Google Scholar]
- 30.Leger D. The cost of sleep-related accidents: a report for the National Commission on Sleep Disorders Research. Sleep. 1994;17(1):84–93. doi: 10.1093/sleep/17.1.84. [DOI] [PubMed] [Google Scholar]
- 31.Volna’ J, Šonka K. Medical factors of falling asleep behind the wheel. Prague Med Rep. 2006;107(3):290–296. [PubMed] [Google Scholar]
- 32.Arnulf I, Leu S, Oudiette D. Abnormal sleep and sleepiness in Parkinson's disease. Curr Opin Neurol. 2008;21(4):472–477. doi: 10.1097/WCO.0b013e328305044d. [DOI] [PubMed] [Google Scholar]
- 33.Tregear SJ, Reston JT, Schoelles K, Phillips B. Obstructive sleep apnea and risk of motor vehicle crash: systematic review and meta-analysis. J Clin Sleep Med. 2009;5(6):573–581. [PMC free article] [PubMed] [Google Scholar]
- 34.Chin K, Fukuhara S, Takahashi K, et al. Response shift in perception of sleepiness in obstructive sleep apnea-hypopnea syndrome before and after treatment with nasal CPAP. Sleep. 2004;27(3):490–493. [PubMed] [Google Scholar]
- 35.Dement WC, Carskadon MA, Richardson G. Excessive daytime sleepiness in the sleep apnea syndrome. In: Guilleminault C, Tilkian A, Dement WC, editors. Sleep Apnea Syndromes. Vol. 27. Alan R Liss; New York, NY: 1978. pp. 465–484. [Google Scholar]
- 36.Engleman HM, Martin SE, Deary IJ, Douglas NJ. Effect of CPAP therapy on daytime function in patients with mild sleep apnoea/hypopnoea syndrome. Thorax. 1997;52(2):114–119. doi: 10.1136/thx.52.2.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Furuta H, Kaneda R, Kosaka K, Arai H, Sano J, Koshino Y. Epworth Sleepiness Scale and sleep studies in patients with obstructive sleep apnea syndrome. Psychiatry Clin Neurosci. 1999;53(2):301–302. doi: 10.1046/j.1440-1819.1999.00511.x. [DOI] [PubMed] [Google Scholar]
- 38.Stutts JC, Wilkins JW, Vaughn BV. Why Do People Have Drowsy Driving Crashes? AAA Foundation for Traffic Safety; Washington, DC: 1999. p. 5944. [Google Scholar]
- 39.National Highway Traffic Safety Administration . Traffic Safety Facts 2007: Older Population. National Highway Traffic Safety Administration; Washington, DC: 2008. Report DOT HS 810 992. [Google Scholar]
- 40.Fonda SJ, Wallace RB, Herzog AR. Changes in driving patterns and worsen ing depressive symptoms among older adults. J Gerontol B Psychol Sci Soc Sci. 2001;56(6):S343–S351. doi: 10.1093/geronb/56.6.s343. [DOI] [PubMed] [Google Scholar]
- 41.Jette AM, Branch LG. A ten-year follow-up of driving patterns among community-dwelling elderly. Hum Factors. 1992;34(1):25–31. doi: 10.1177/001872089203400104. [DOI] [PubMed] [Google Scholar]
- 42.DeCarlo DK, Scilley K, Wells J, Owsley C. Driving habits and health-related quality of life in patients with age-related maculopathy. Optom Vis Sci. 2003;80(3):207–213. doi: 10.1097/00006324-200303000-00010. [DOI] [PubMed] [Google Scholar]
- 43.Marottoli RA, Mendes de Leon CF, Glass TA, et al. Established Populations for Epidemiologic Studies of the Elderly. Driving cessation and increased depressive symptoms: prospective evidence from the New Haven EPESE. J Am Geriatr Soc. 1997;45(2):202–206. doi: 10.1111/j.1532-5415.1997.tb04508.x. [DOI] [PubMed] [Google Scholar]
- 44.Rizzo M, Jermeland J, Severson J. Instrumented vehicles and driving simulators. Gerontechnology. 2002;1(4):291–296. [Google Scholar]
- 45.Pietras TA, Shi Q, Lee JD, Rizzo M. Traffic-entry behavior and crash risk for older drivers with impairment of selective attention. Percept Mot Skills. 2006;102(3):632–644. doi: 10.2466/pms.102.3.632-644. [DOI] [PubMed] [Google Scholar]
- 46.Barrash J, Stillman A, Anderson SW, Uc EY, Dawson JD, Rizzo M. Prediction of driving ability with neuropsychological tests: demographic adjustments diminish accuracy. J Int Neuropsychol Soc. 2010;16(4):679–686. doi: 10.1017/S1355617710000470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Uc EY, Rizzo M, Johnson AM, Dastrup E, Anderson SW, Dawson JD. Road safety in drivers with Parkinson disease. Neurology. 2009;73(24):2112–2119. doi: 10.1212/WNL.0b013e3181c67b77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Reger MA, Welsh RK, Watson GS, Cholerton B, Baker LD, Craft S. The relationship between neuropsychological functioning and driving ability in dementia: a meta-analysis. Neuropsychology. 2004;18(1):85–93. doi: 10.1037/0894-4105.18.1.85. [DOI] [PubMed] [Google Scholar]
- 49.Goldberg D, GHQ . The Selection of Psychiatric Illness by Questionnaire. Oxford University Press; London, England: 1972. [Google Scholar]
- 50.Beck AT, Steer RA, Ball R, Ranieri WF. Comparison of Beck Depression Inventories IA and II in psychiatric outpatients. J Pers Assess. 1996;67(3):588–597. doi: 10.1207/s15327752jpa6703_13. [DOI] [PubMed] [Google Scholar]
- 51.Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14(6):540–545. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 52.Johns MW. Reliability and factor analysis of the Epworth Sleepiness Scale. Sleep. 1992;15(4):376–381. doi: 10.1093/sleep/15.4.376. [DOI] [PubMed] [Google Scholar]
- 53.Ball K, Owsley C, Sloane ME, Roenker DL, Bruni JR. Visual attention problems as a predictor of vehicle crashes in older drivers. Invest Ophthalmol Vis Sci. 1993;34(11):3110–3123. [PubMed] [Google Scholar]
- 54.Dula CS, Ballard ME. Development and evaluation of a measure of dangerous, aggressive, negative emotional, and risky driving. J Appl Soc Psychol. 2006;33(2):263–282. [Google Scholar]
- 55.Ferris FL, III, Kassoff A, Bresnick GH, Bailey I. New visual acuity charts for clinical research. Am J Ophthalmol. 1982;94(1):91–96. [PubMed] [Google Scholar]
- 56.Pelli DG, Robson JG, Wilkins AJ. The design of a new letter chart for measuring contrast sensitivity. Clin Vision Sci. 1988;2(3):187–199. [Google Scholar]
- 57.Mangione CM, Lee PP, Gutierrez PR, Spritzer K, Berry S, Hays RD, National Eye Institute Visual Function Questionnaire Field Test Investigators Development of the 25-item National Eye Institute visual function questionnaire. Arch Ophthalmol. 2001;119(7):1050–1058. doi: 10.1001/archopht.119.7.1050. [DOI] [PubMed] [Google Scholar]
- 58.Berson F, Owsley C, Peli E, Federal Motor Carrier Safety Administration [February 16, 2011];Expert Panel Recommendations: Vision and Commercial Motor Vehicle Driver Safety. 2008 March 14; http://www.fmcsa.dot.gov/rules-regulations/TOPICS/mep/report/MEP-Recommendations-Vision-v2-prot.pdf.
- 59.American Medical Association/National Highway Traffic Administration . Physicians’ Guidelines for Assessing and Counseling Older Drivers. Dept of Transportation; Washington, DC: 2003. [Google Scholar]
- 60.Carr D, Schwartberg J, Manning L, Sempek K. Physician's Guide to Assessing and Counseling Older Drivers. 2nd ed. National Highway Traffic Safety Administration; Washington, DC: 2010. [Google Scholar]
- 61.American Academy of Ophthalmology [April 1, 2010];Policy Statement: Vision Requirements for Driving. 2006 March; http://www.aao.org/about/policy/upload/AAODrivingPolicyWebcopy.pdf.
- 62.American Association of Motor Vehicle Administrators. National Highway Traffic Safety Administration . Driver Fitness Medical Guidelines. National Highway Traffic Safety Administration; Washington, DC: 2009. [Google Scholar]
- 63.Iverson DJ, Gronseth GS, Reger MA, Classen S, Dubinsky RM, Rizzo M, Quality Standards Subcommittee of the American Academy of Neurology Practice parameter update: evaluation and management of driving risk in dementia: report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2010;74(16):1316–1324. doi: 10.1212/WNL.0b013e3181da3b0f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Edlund W, Gronseth G, So Y, Franklin G, editors. Clinical Practice Guideline Process Manual. 2004 Edition American Academy of Neurology; St Paul, MN: 2005. [Google Scholar]
- 65.Owsley C, McGwin G, Jr, Phillips JM, McNeal SF, Stalvey BT. Impact of an educational program on the safety of high-risk, visually impaired, older drivers. Am J Prev Med. 2004;26(3):222–229. doi: 10.1016/j.amepre.2003.12.005. [DOI] [PubMed] [Google Scholar]
- 66.Ball K, Edwards JD, Ross LA. The impact of speed of processing training on cognitive and everyday functions. J Gerontol B Psychol Sci Soc Sci. 2007;62(Spec No. 1):19–31. doi: 10.1093/geronb/62.special_issue_1.19. [DOI] [PubMed] [Google Scholar]
- 67.Edwards JD, Bart E, O'Connor ML, Cissell G. Ten years down the road: predictors of driving cessation. Gerontologist. 2010;50(3):393–399. doi: 10.1093/geront/gnp127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Carr DB, Ott BR. The older adult driver with cognitive impairment: “it's a very frustrating life.”. JAMA. 2010;303(16):1632–1641. doi: 10.1001/jama.2010.481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Zador PL, Krawchuk SA, Voas RB. An alcohol-related relative risk of driver fatalities and driver involvement in fatal crashes in relation to driver age and gender: an update using 1996 data. J Stud Alcohol. 2000;61(3):387–395. doi: 10.15288/jsa.2000.61.387. [DOI] [PubMed] [Google Scholar]
- 70.Borkenstein R, Crowther R, Shumate R, Ziel W, Zylman R. The role of the drinking driver in traffic accidents (the Grand Rapids Study). Blutalkohol. 1974;11(suppl 1):1–132. [Google Scholar]
- 71.Rizzo M, Robinson S, Neale VL. The brain in the wild. In: Parasuraman R, Rizzo M, editors. Neuroergonomics: The Brain at Work. Oxford University Press; Oxford, England: 2007. pp. 113–128. [Google Scholar]
- 72.Dingus TA, Klauer SG, Neale VL, et al. The 100-Car Naturalistic Driving Study, Phase II: Results of the 100-Car Field Experiment. [February 18, 2011];Report DOT HS. 2006 April; 810 593. http://ntl.bts.gov/lib/jpodocs/repts_ te/14302.htm.
- 73.Neale VL, Dingus TA, Klauer SG, Sudweeks J, Goodman M. An Overview of the 100-Car Naturalistic Study and Findings. National Highway Traffic Safety Administration. 2005 Paper 05-0400. [Google Scholar]
- 74.Carney C, McGehee DV, Lee JD, Reyes ML, Raby M. Using an event-triggered video intervention system to expand the supervised learning of newly licensed adolescent drivers. Am J Public Health. 2010;100(6):1101–1106. doi: 10.2105/AJPH.2009.165829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.McGehee DV, Raby M, Carney C, Lee JD, Reyes ML. Extending parental mentoring using an event-triggered video intervention in rural teen drivers. J Safety Res. 2007;38(2):215–227. doi: 10.1016/j.jsr.2007.02.009. [DOI] [PubMed] [Google Scholar]
- 76.Hickman JS, Hanowski RJ, Ajayi O. Proceedings of Driving Assessment 2009: The Fifth International Driving Symposium on Human Factors in Driver Assessment, Training and Vehicle Design. Vol. 2009. University of Iowa; Iowa City: Evaluation of an onboard safety monitoring device in commercial vehicle operations. pp. 38–45. [Google Scholar]