Abstract
The literature examining trauma among older adults is growing, but little is known about the efficacy of empirically supported interventions for PTSD within this population. Clinical writing on this topic often implies that cognitive-behavioral treatments may be ineffective or inappropriate for older adults with PTSD given physical and/or cognitive vulnerabilities. Review of the limited research in this area, however, provides little support for the claim that cognitive-behavioral interventions are ineffective in treating PTSD among the elderly. In an effort to explicate specific issues related to treatment process and outcome among older survivors of trauma, a case series is presented outlining the treatment of three older adults within the context of a structured, cognitive-behavioral group intervention. Observations from this case series suggests that cognitive-behavioral interventions continue to be useful in treating PTSD with this population. Specific treatment issues unique to older adults are explored and recommendations for future research are discussed.
Keywords: PTSD, older adults, cognitive behavior therapy
Research over the past decade has advanced our understanding of posttraumatic stress disorder (PTSD) considerably, and treatment development efforts have resulted in a number of therapeutic approaches with robust support for their efficacy (Keane, Marshall, & Taft, 2006). Review of this literature, however, indicates that treatment efforts primarily have targeted young to middle-aged adults. As such, our understanding of how to treat PTSD among older adults – generally conceptualized as those individuals age 65 and older – remains in its nascent stages. In this review, we examine literature pertaining to the treatment of PTSD in older adults and highlight the potential strengths of this population. We then present a case series detailing treatment process and outcome in three older individuals within a cognitive-behavioral group intervention. We conclude with a discussion of possible next steps in developing the literature on the treatment of PTSD in older trauma survivors.
PTSD in the General Population and in Older Adults
PTSD is conceptualized as an anxiety disorder developing in response to traumatic events involving actual or threatened death, serious injury, and/or threat to one’s physical integrity (American Psychiatric Association, 2000). Symptoms include re-experiencing the event (e.g., intrusive thoughts, dreams, and/or flashbacks), avoidance of thoughts and/or situations associated with the trauma, numbing of emotional responsiveness (e.g., detachment, flattened or absent affect), and heightened arousal (e.g., exaggerated startle, irritability, disturbed sleep). Approximately 10 – 20% of individuals who experience a traumatic event will go on to develop PTSD, and likelihood of remission is generally considered to be poor in those continuing to meet criteria 1 – 2 years post-event (Norris & Slone, 2007). The chronicity, comorbidity, and social costs associated with this disorder make PTSD a significant public health issue (Solomon & Davidson, 1997).
How does advancing age impact the development and trajectory of PTSD? Large-scale epidemiological research pertaining to the occurrence of PTSD among the elderly is limited, but studies examining smaller subsets of the population demonstrate a robust association between aging and reductions in the prevalence of PTSD. Examinations of reactions to recent, non-combat trauma suggest that older adults evidence lower rates of PTSD and similar, if not better, post-trauma functioning relative to their younger counterparts (Acierno, Ruggiero, Kilpatrick, Resnick, & Galea, 2006; Green, Gleser, Lindy, Grace, & Leonard, 1996; Shore, Vollmer, & Tatum, 1989). Research with combat veterans suggests similar effects (Fontana & Rosenheck, 1994; Frueh et al., 2007). Some researchers posit that the association between age and posttrauma functioning may be a byproduct of methodological factors such as earlier mortality among PTSD samples or reluctance of older generations to acknowledge psychopathology (Cook & Niederehe, 2007). Others suggest that age may simply provide some buffer against the development of post-trauma symptoms (e.g., Fontana & Rosenheck, 1994). At present, both remain plausible explanations given insufficient data in this area. Regardless of the specific mechanisms underlying this particular relationship, it is important to note that the trajectory of symptoms continues to be chronic among older adults who do develop PTSD (Averill & Beck, 2000). As such, treatment issues continue to be an important consideration for this population.
Treatment of PTSD: Controversy in Older Adults
Despite the chronicity associated with PTSD, several therapeutic approaches are supported in the literature. Currently, cognitive-behavioral therapies (CBT) have received the most empirical scrutiny and are considered the preferred treatment for PTSD (APA, 2004; Keane et al., 2006). Principal components of these treatments typically include exposure and cognitive therapies. Exposure therapy for PTSD involves evoking distressing memories of the trauma via controlled exposure to reminders of the event (e.g., Foa, Rothbaum, Riggs, & Murdock, 1991; Blanchard & Hickling, 1997). Exposure can be done both imaginally or in vivo (e.g., reading descriptions of the event, visiting the site of the trauma) and is repeated until distress associated with the memory habituates. Whereas all empirically supported interventions for PTSD include some element of exposure (e.g., Resick & Schnicke, 1992; Shapiro, 1989), Foa et al.’s (1991) prolonged exposure (PE) therapy has received perhaps the most empirical support to date.
Contrasting exposure, cognitive therapy aims to isolate dysfunctional thoughts and assumptions about the trauma which serve to perpetuate distress (e.g., the world is a dangerous place; I am to blame for the trauma). Clients are encouraged to challenge the veracity of these beliefs and to substitute them with more balanced thoughts (e.g., Resick & Schnicke, 1992). In practice, cognitive interventions are generally packaged along with exposure techniques as seen in Resick and Schnicke’s (1992) Cognitive Processing Therapy (CPT). CPT and other cognitive-behavioral programs (e.g., Blanchard et al., 2003; Kubany et al., 2004) consistently evidence superior outcomes relative to wait-list control and/or supportive psychotherapy.
Despite evidence for the efficacy of CBT in treating PTSD, similar research has not appeared within geriatric research. This literature is best characterized by case studies (e.g., Burgmer & Heuft, 2004; Maercker, 2002), summaries of clinical experience (e.g., Bonwick, 1998; Bonwick & Morris, 1996), and uncontrolled clinical trials (e.g., Games & Hayden, 1991; Lipton & Schaffer, 1986). Interestingly, some in this literature express reservations regarding the utility of CBT in older trauma populations. Many question the safety of exposure-based interventions given concerns that any associated physiological and emotional reactivity may exacerbate age-related health conditions (e.g., Hankin, 1997; Hyer & Woods, 1998; Shapiro, 1995). Some caution that older adults may be less amenable to cognitive interventions due to age-related declines in cognitive capacity (e.g., Cook, Ruzek, & Cassidy, 2003; Flint, 2004). Others suggest that older adults are less “psychologically minded” and less responsive to psychosocial treatment in general (e.g., Burgmer & Heuft, 2004). At present, these concerns are limited to clinical speculation given the absence of systematic research examining the efficacy of CBT specifically among older trauma survivors. A subset of the available case literature, however, seems to imply that the success of CBT with older adults may be tenuous at best.
Whereas provision of mental-health services to the aged sometimes involves additional logistic considerations (e.g., potential age-related health complications, transportation issues; APA, 1998), reservations regarding the utility of CBT in this population may be largely unfounded. The APA Working Group on the Older Adult (1998) notes that although the likelihood of cognitive disorders increases with age, normal age-related declines in cognitive ability typically are not sufficiently severe to impact routine functioning. Furthermore, research demonstrating the efficacy of CBT for both depression and generalized anxiety among older adults (Ayers et al., 2007; Mohlman, 2004; Scogin & McElreath, 1994) challenges the notion that CBT is ineffective with this population. Available case studies also indicate that exposure-based interventions may be used safely and successfully with older adults, even those with serious health issues (e.g., Markowitz, 2007; Russo et al., 2003). Markowitz (2007) describes the use of graded exposure with an 82-year old World War II veteran diagnosed with chronic PTSD. Despite an extensive history of cardiovascular illness (i.e., four myocardial infarctions, quadruple bypass surgery, angioplasty, several catheterizations and stent placements), this client evidenced significant reductions in PTSD symptomology following exposure therapy augmented with anti-anxiety medication (i.e., escitalopram). As with any client, it is the responsibility of the clinician to carefully consider the strengths and limitations of CBT on a case-by-case basis. However, there is little evidence to suggest that advanced age should preclude older adults from receiving the most efficacious treatments currently available for PTSD.
Case Example of Group CBT with Older Adults
To illustrate therapeutic process of CBT in older adults, we present data collected within the context of a cognitive-behavioral group intervention targeting motor-vehicle accident (MVA) related PTSD (Beck & Coffey, 2005; Beck, Coffey, Foy, Keane, & Blanchard, 2009). Specifically, we provide a series of case studies taken from a treatment group containing a subset of three older gentlemen. A number of points should be emphasized in outlining these vignettes:
Although the present data were not collected as part of a systematic study examining treatment outcome in older trauma survivors, they do provide a unique opportunity to explore therapeutic process in older adults participating in structured group CBT. Several authors suggest that interpersonal relationships developed within the context of group therapy may be especially beneficial in the treatment of PTSD (e.g., Bonwick, 1998; Boehnlein & Sparr, 1993). Examples of case studies detailing group interventions for PTSD among elderly clients are available in the existent literature, but these reports are limited largely to supportive group therapies for aging combat veterans (Bonwick, 1998; Boehnlein & Sparr, 1993; Games & Hayden, 1991; Lipton & Schaffer, 1986). Examining process and treatment outcome in response to a structured, cognitive-behavioral group intervention extends the existing case literature.
Additionally, the individuals presented in these vignettes were seeking treatment for post-trauma symptoms subsequent to recent trauma exposure (i.e., serious MVA). The preponderance of literature regarding the treatment of PTSD in older adults pertains to those exposed to war-related trauma occurring many years prior to treatment. However, trauma exposure is not confined to any specific demographic and can occur throughout the lifespan. These vignettes examine a clinical population that has largely been overlooked in the PTSD literature.
Description of Treatment
Beck et al.’s (2009; Beck & Coffey, 2005) group CBT (GCBT) is based on Blanchard and Hickling’s (1997) individual treatment program for MVA-related PTSD. GCBT consists of 14 weekly sessions each lasting 2 hours. Homework exercises serve a central role throughout treatment and focus primarily on exposure and cognitive techniques. The initial session is used for introductions, to provide guidelines for group therapy (e.g., confidentiality), and to review the rationale for treatment. Didactic materials pertaining to the role of avoidance in maintaining fear and anxiety are presented in Session 2, and group members begin to create individualized fear hierarchies. Fear hierarchies are used to guide between-session exposure exercises assigned for the duration of therapy. In Session 4, group members are asked to compose a detailed description of their MVA to be used as an additional exposure tool. The MVA narrative is read aloud as between-session homework following Session 5. Members are encouraged to modify these narratives as additional details of the event are recalled. Exposure exercises using the MVA narrative are continued as between-session assignments until distress associated with the trauma memory has extinguished.
Cognitive therapy is introduced in Session 6 and emphasizes developing positive self-talk. Session 7 pertains to identification of cognitive errors and techniques for challenging dysfunctional beliefs. Session 8 completes the cognitive portion of GCBT and emphasizes the practical application of cognitive skills. The remaining sessions involve strategies for managing anger and depression (Sessions 9 & 10), rebuilding social support systems (Sessions 11 & 12), and relapse prevention (Sessions 13 & 14). Homework assignments in final sessions continue to emphasize skills obtained in Sessions 1 – 8.
Blanchard and Hickling’s (1997) treatment program served as the basic framework for Beck et al.’s (2009) intervention, but a number of modifications were incorporated to accommodate the group format. GCBT places a strong emphasis on group-building to encourage a supportive atmosphere and to capitalize on the inherent support network of the group. Therapeutic techniques are introduced at a slower pace to accommodate group discussion and to review members’ experience with tools used during between-session homework. Anxiety management techniques (i.e., mindfulness training: Sessions 2–14; progressive muscle relaxation: Sessions 4–7) also are incorporated to help manage distress associated with transportation to and from therapy. Finally, GCBT is administered by two therapists, a choice guided by previous experience treating PTSD in group settings (Schnurr, Friedman, Lavori, & Hsieh, 2001). A detailed description of treatment development and session-by-session activities are provided in Beck and Coffey (2005). Data from a randomized controlled pilot study examining the efficacy of GCBT (Beck et al., 2009) are presented as a reference for the current case series. Individuals included in the larger pilot study ranged in age from 22 to 69 with a mean of 43.3 (SD = 12.8).1
Group Members2
Matthew
Matthew was 72-year old Caucasian male residing with his wife of 43 years. Matthew was retired but held a seasonal position at a local country club. A veteran of the Vietnam War, he reported witnessing a number of combat-related traumas but denied any ongoing distress as a result of these experiences. Matthew had been diagnosed with and successfully treated for colon cancer two years earlier. He reported no ongoing physical complications or medication use associated with this diagnosis.
Matthew’s accident occurred approximately 4 years prior to the initial assessment. An oncoming vehicle swerved across his lane, and Matthew struck the oncoming car. He was knocked unconscious and broke several ribs. A 15 year-old passenger in the oncoming vehicle was killed in the collision. Since the MVA, Matthew reported intrusive memories of the event, flashbacks, and distress in response to reminders of the MVA. He acknowledged avoiding the crash site, irritability, and exaggerated startle responses. Although he did not endorse a sufficient number of avoidance and numbing symptoms to meet full DSM-IV criteria for PTSD, Matthew’s symptom presentation was consistent with a diagnosis of partial-PTSD. Partial-PTSD is defined by the presence of at least one symptom in each diagnostic cluster (i.e., reexperiencing, avoidance/numbing, hyperarousal) with either three or more avoidance/numbing symptoms or two or more hyperarousal symptoms (Blanchard et al. 1996).
John
John was a 69-year old Caucasian male residing with his wife of 44 years. John was employed part-time at an accounting firm. He reported no additional Criterion-A trauma but did acknowledge loosing a close friend in an MVA 22 years earlier. John reported no major health concerns or medication use.
John’s accident occurred 3 years prior to the initial assessment. While driving through a local neighborhood, a motorist failed to stop at an intersection and struck John’s driver’s side door. John did not seek immediate medical care but reported soreness in his neck that persisted for several years. He reported unpleasant dreams of the MVA as well as emotional and physiological distress when reminded of the event. He refused to speak about the MVA and would not drive or ride as a passenger on certain roads or after dark. John reported a pervasive sense that “[he] could be gone tomorrow” and had made arrangements for his funeral. He acknowledged difficulty concentrating, excessive concern for his safety, and exaggerated startle responses. In addition to a diagnosis of PTSD, John reported an excessive preoccupation with order and symmetry. He denied any distress as a function of these symptoms, but the time dedicated to organizing his home and workspace warranted an additional diagnosis of Obsessive Compulsive Disorder.
David
David was a 67-year-old Caucasian male residing with his wife of 39 years. David worked full-time as the foreman of a construction company. He endorsed a number of additional Criterion-A events including childhood physical abuse, physical assault as an adult, and traumatic injury while on a construction site. David was diagnosed with Type II diabetes and was using medication to manage this disorder.
David’s accident occurred approximately 4 years prior to the initial assessment. While driving in poor weather conditions, David’s vehicle slid off of the road and rolled down a small embankment. David sustained a concussion and a broken arm as a consequence of the accident. He reported intrusive recollections of the event as well as occasional flashbacks. He refused to speak about the MVA and reported efforts to avoid thinking of the trauma. David refused to drive or ride as a passenger on interstates or 4-lane highways. He acknowledged diminished interest in his usual activities as well as substantial sleeping difficulties. David reported increased irritability and acknowledged hypervigilance in most driving-related situations. David also evidenced low-level symptoms of Dysthymia but did not meet criteria for any other disorder.
Additional group members
The treatment group also included two middle-aged individuals. The first was a 48-year old Caucasian female whose accident occurred 6 months prior to the initial assessment. She received a primary diagnosis of PTSD with comorbid Major Depressive Disorder, Panic Disorder, and Generalized Anxiety Disorder. The second was a 53-year old Native American male. His MVA occurred 2 years prior to treatment. He was diagnosed with PTSD as well as Generalized Anxiety Disorder and Major Depressive Disorder.
Assessment
Diagnoses of PTSD and comorbid disorders were established via clinical interview conducted during the initial assessment (pre-treatment) and one month following the completion of the program (post-treatment). PTSD diagnoses were established using the Clinician-Administered PTSD Scale (CAPS; Blake et al., 1990). CAPS items also were summed to provide a continuous index of PTSD severity (CAPS severity; scores ranging from 0 to 136). Interviews were conducted by advanced graduate students supervised by the second author. As a reference for the reliability of CAPS diagnoses, approximately 30% (n = 55) of the cases from the Beck et al. (2009) clinical trial (completed prior to the present group) were randomly chosen for review by an independent clinician. Agreement for diagnosis of PTSD was excellent (k=0.86).
Diagnoses of comorbid mood and anxiety disorders were established using the Anxiety Disorder Interview Schedule for DSM-IV (ADIS-IV; DiNardo, Brown, & Barlow, 1994). As with the CAPS, 30% (n = 55) of interviews from the larger clinical trial were randomly selected and rated by an independent interviewer. Agreement between clinicians across comorbid mood and anxiety disorders ranged from good (major depressive disorder; k = 0.74) to excellent (generalized anxiety disorder; k = 0.96).
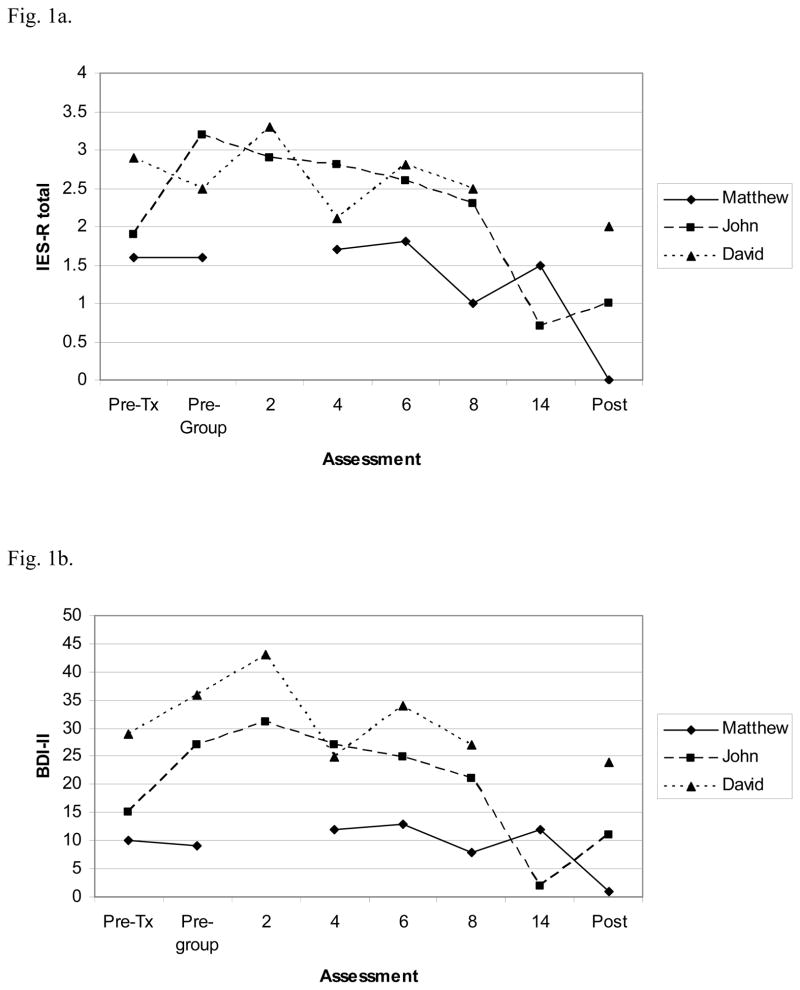
Self-report measures of PTSD and depressive symptoms were administered during pre-and post-treatment and periodically throughout group. Trajectory of PTSD severity was monitored using the Impact of Event Scale–Revised (IES-R; Weiss & Marmar, 1997). IES-R scores reflect the average rated distress associated with the trauma over the previous week. Total scores range from 0 to 4. The Beck Depression Inventory II (BDI-II; Beck, Steer, & Brown, 1996) was used to assess ongoing symptoms of depression with scores ranging from 0 to 63.
All individuals completed the CAPS, ADIS, IES-R, and BDI-II at the initial assessment. Due to a period of latency between pre-treatment assessment and the initial group session (to allow a sufficient number of people to be assessed and consented to GCBT)3, an individual pre-group session was scheduled with each group member one week prior to the beginning of GCBT. Members provided IES-R and BDI-II ratings at the pre-group meeting and during Sessions 2, 4, 6, 8, and 14. Four weeks after the completion of the program, participants completed post-treatment assessments. All procedures were in compliance with the local institutional review board.
Outcome: Pre- and Post-Treatment Assessment
PTSD diagnoses, CAPS total, IES-R, and BDI-II scores at pre- and post-treatment are presented in Table 1. Means and standard deviations from the Beck et al. (2009) trial are provided as a reference for the current case series. Interview and self-report data reveal some variability among the three men. Consistent with diagnostic interviews, Matthew evidenced the lowest scores on all three measures at pre-treatment. Although his IES-R and BDI-II scores were comparable to those observed in the Beck et al. trial (i.e., close to 1 SD), his CAPS severity score was considerably lower than the average reported in that study. John’s pre-treatment scores were comparable to Matthew’s across all three assessment measures. David evidenced the most severe psychopathology with an IES-R score notably larger than that reported in the Beck et al. trial.
Table 1.
PTSD severity, depression, and diagnostic status pre- and post-treatment for case series and Beck et al. (2009) pilot
| CAPS | IES-R | BDI-II | PTSD Dx | ||
|---|---|---|---|---|---|
| Matthew | Pre | 32 | 1.6 | 10 | Partial PTSD |
| Post | 13 | 0 | 1 | None | |
|
| |||||
| John | Pre | 33 | 1.9 | 15 | Full PTSD |
| Post | 10 | 1.0 | 11 | None | |
|
| |||||
| David | Pre | 60 | 2.9 | 29 | Full PTSD |
| Post | 16 | 2.0 | 24 | None | |
|
| |||||
| GCBT† | Pre | 57.3 (15.5) | 1.8 (0.7) | 22.4 (10.7) | Full PTSD: 100% |
| Post | 28.9 (19.9) | 1.0 (0.9) | 16.6 (12.4) | Full PTSD: 11.7% | |
Note: PRE = pre-treatment; POST = post-treatment; CAPS = Clinician-Administered PTSD Scale severity; IES-R = Impact of Events Scale Revised total; BDI-II = Beck Depression Inventory II; PTSD Dx = PTSD diagnostic status; Full PTSD = full DSM-IV criteria; Partial PTSD = 1 reexperiencing symptom and ≥ 3 avoidance/numbing symptoms or ≥ 2 hyperarousal symptoms with at least 1 symptom in each diagnostic cluster
GCBT = Beck et al. (2009) pilot data (N = 17); standard deviations for group scores in parenthesess
Assessment at one month post-treatment evidenced considerable reductions in CAPS severity across all three men. John and David no longer met criteria for PTSD at post-treatment. Matthew, although failing to meet formal DSM-IV criteria at the initial assessment, no longer qualified for partial PTSD at post-treatment. Matthew also evidenced substantial reductions in IES-R and BDI scores. John and David evidenced more modest improvements on these measures. In sum, these data suggest that overall treatment outcome for this group of older adults was positive and comparable to that observed in Beck et al.’s clinical trial.
Outcome: Trajectory Across Therapy
Pre- and post-treatment data suggest an overall positive response to GCBT. Scores collected throughout the course of treatment provide a detailed picture of how these changes occurred. Consistent with low levels of initial symptomology, Matthew’s IES-R and BDI-II data indicate a fairly flat treatment response (see Fig. 1a & 1b). Matthew was perhaps the most verbally engaged of the three older adults in this group and was generally compliant with homework assignments. Because his symptoms of avoidance were relatively minor in comparison to those of John and David, he moved quickly through his fear hierarchy. Matthew’s success on these assignments was encouraging, but care was taken to prevent other members from judging their own progress as inadequate by comparison. Matthew did struggle with the MVA narrative, and processing emotions associated with the fatality required several sessions. He seemed the most adept at mastering the cognitive techniques, however, and used these tools to challenge feelings of guilt and self-blame. As indicated by his scores at post-assessment, Matthew continued to utilize skills obtained in group, and his IES-R and BDI-II scores were negligible at the post-assessment.
Figure 1.
Fig. 1a. IES-R scores across treatment for case group; Missing data points represent missed sessions
Fig. 1b. BDI-II scores across treatment for case group; Missing data points represent missed sessions
John evidenced a much different trajectory. Unlike Matthew, John demonstrated a marked increase in symptoms of PTSD and depression from pre-treatment to pre-group (see Fig. 1a & 1b). This exacerbation of symptomology may reflect anticipatory anxiety related to beginning treatment, an increase in symptomology sometimes associated with initiating exposure therapy, episodic waxing and waning of symptoms characteristic of chronic PTSD, underreporting at the initial assessment, or a combination of all of these factors. Despite a substantial increase in self-reported depression and PTSD, John attended sessions without fail and his compliance with exposure homework was exemplary. His successful progression through his fear hierarchy is reflected in the steadily decreasing scores on the IES-R. John struggled to integrate the principles of cognitive therapy into his homework, but these difficulties did not appear to be qualitatively different from younger individuals participating in the larger treatment trial. Comparison of John’s pre- and post-treatment IES-R and BDI-II scores suggest moderate reductions in self-reported symptomology, but the trajectory of these scores over the course of therapy more clearly illuminate the progress made by this client. Although John’s symptoms of OCD continued unabated at post-assessment, he declined referrals for continued services.
David, the most severe of the three older adults at pre-treatment, also demonstrated the poorest compliance. He missed several of the initial treatment sessions and failed to complete homework assignments. Assignments that were attempted were incomplete or deviated from instructions provided within sessions. His erratic compliance over the first eight weeks is reflected in the trajectory of his scores (see Fig. 1a & 1b). David also evidenced the greatest degree of on-going life stress, reporting issues related to work and his two adult children. Frustration with these stressors almost invariantly manifested as irritability. Although David at no point directed his anger towards the therapists or other group members, his interactions during sessions often were terse and his non-verbal behavior conveyed hostility. David’s attendance and group participation improved somewhat in the final five sessions (Sessions 10 – 14). Coincidentally, Session 10 provided instruction on anger management strategies (e.g., assertiveness training), and David reported several successes using these techniques. He also demonstrated greater focus in completing his fear hierarchy during the final weeks. David evidenced substantial reductions in his overall distress and did not meet criteria for any psychological disorder at post-treatment.
Impact of Advanced Age on Outcome & Process
A number of important points should be noted given the criticisms of cognitive-behavioral interventions with older trauma survivors. In-group discussion and review of weekly homework indicated no greater difficulty with exposure or cognitive-based interventions than members in the larger Beck et al. (2009) clinical trial. All three men participated in weekly, between-session exposure exercises with no evidence of physical complications. These results are consistent with previous case studies suggesting the efficacy of exposure therapy among older trauma survivors (e.g., Markowitz, 2007; Russo et al., 2003). Admittedly, the men in this group evidenced few acute health concerns to be aggravated by exposure-related arousal. Markowitz’ (2007) case study, however, demonstrates that exposure therapy can be effectively adapted even among older individuals with substantial health issues. An important commonality between Markowitz’ approach and the current group protocol is that both emphasized controlled, graduated exposure. In contrast with other methods (e.g., flooding, implosive therapy), the present exposures were conducted at a pace dictated by the client while maintaining therapeutic effects. This graded approach may allow older trauma survivors to capitalize on the well-documented benefits of exposure therapy while avoiding the risk of undue physiological burden that may accompany more extreme variations of exposure.
Client responses to cognitive techniques were varied. The underlying premise of cognitive therapy involves developing an awareness of automatic thoughts and beliefs and monitoring how these impact both emotions and behavior. In-session discussions and review of homework assignments suggested that Matthew, the oldest of the three, was able to employ these techniques relatively flexibly. John, by contrast, struggled with the cognitive components of treatment. Variability within this group appeared to be more a function of individual difference than age and seemed no different than younger participants’ struggles with the complexities of cognitive therapy. Although these conclusions are based largely on clinical inference, observations made in this case series suggest that age was not a systematic influence on the efficacy of cognitive therapy.
Data from this case series suggests that cognitive-behavioral interventions continue to be a powerful therapeutic tool in older survivors of trauma; however, the potential benefits of the group format are somewhat unclear. The APA (1998) acknowledges that older adults may benefit from a greater emphasis on the rationale, structure, and goals of treatment relative to younger adults more familiar with psychosocial therapies. The APA group also suggests that slowing the pace of therapy and repetition of basic concepts may improve outcome in older adults. Although not a unique feature of group therapy per se, Beck et al. (2009; Beck & Coffey, 2005) incorporated these suggestions in the service of adapting Blanchard and Hickling’s (1997) treatment to a group format, and it is possible that these modifications contributed to observed treatment effects. The group format also may have been beneficial in that discussions of trauma-related interference and symptom management were naturally placed within an age-relevant context. Having multiple older individuals in the same group may provide a forum for problem-solving trauma-related issues unique to individuals in that age range. By contrast, the group format limits the extent to which clinicians may emphasize person-specific issues within session, and a structured approach likely restricts the time that can be given to any specific treatment component (e.g., cognitive restructuring). The present case series has little basis to evaluate the impact of group format within this population, and the unique effects of treatment format should be considered as an area of exploration for future research.
Whereas many aspects of treatment were typical of other groups, process issues were noted that seemed unique to older members. Fatigue was a considerable issue for these individuals. Group sessions were conducted in the evening to accommodate client schedules. Older members often would evidence drowsiness towards the end of session and would occasionally doze off during mindfulness meditation and relaxation exercises. Activities were subsequently modified in an attempt to promote alertness (e.g., conducting exercises without dimming the lights), but difficulties with fatigue in the later hour of session can be understood as a failure to appreciate age-specific characteristics of older adults’ schedules.
The present group also was unique in that older participants did not seem to seek support from other members to the same degree as individuals included in the larger pilot trial. The availability of social resources inherent in group interventions is cited as a potential benefit of the format, and existing literature on group interventions for PTSD, although largely limited to veteran samples, almost invariably note a sense of camaraderie between members (e.g., Beck & Coffey, 2005; Lipton & Schaffer, 1986). Indicators of therapeutic engagement (i.e., California Psychotherapy Alliance Scales; Marmar, Gaston, Gallagher, & Thompson, 1989) in the present group were comparable to those of the larger clinical trial, and older members were friendly and generally engaged during session. However, older participants evidenced little motivation to develop “friendships” outside of the group. This observation is unlikely a function of the GCBT program or a characteristic trait of MVA survivors specifically. Other groups conducted over the course of the larger clinical study evidenced several strong friendships that continued beyond the treatment setting. The absence of strong inter-group relationships also is unlikely to be a characteristic of male group members or older adults in general given evidence of strong group bonds in existing case studies of older male groups (e.g., Boehnlein & Sparr, 1993; Bonwick, 1998; Games & Hayden, 1991). The relative lack of external support-seeking observed in the present group may have been a multiplicative function of these factors or simply a unique feature of this particular group of individuals.
As with any case study, generalization to the population of older trauma survivors should be made with care. Participants in this group evidenced symptoms of PTSD associated with relatively recent trauma. Treatment effects and clinical issues for this subset of the population may be somewhat different than those for individuals experiencing chronic symptoms associated with earlier trauma (e.g., combat veterans). Participants in this particular group were similar to those in the larger clinical trial with regard to marital status, education, income, and degree of overall social support. In contrast, older group members evidenced a disproportionately high level of employment and somewhat lower levels of overall psychological comorbidity. As such, general functioning in this group is likely higher than what may be expected among older trauma survivors encountered in hospital or outpatient settings. Although not unique to older survivors of trauma, social, physical, and psychological factors contributing global impairment should be considered when evaluating the ecological validity of these observations.
Future Directions
Because the literature concerning PTSD in the elderly remains in its early stages, continued research on any number of topics is welcome. A number of specific areas seem particularly relevant given the present review. The association of advanced age with lower rates of PTSD and greater post-trauma functioning appear to be relatively robust across studies and trauma samples (e.g., Acierno, et al., 2006; Frueh et al., 2007). Notwithstanding potential method effects, what factors account for this relationship? Aldwin (1991) proposes that older adults may use more constructive coping strategies in response to stress than do younger adults, but this hypothesis remains to be explored within the trauma literature. Isolation of specific factors serving to buffer older adults, or those which increase vulnerability in younger adults, may assist the ongoing refinement of trauma interventions.
With respect to the treatment of PTSD in older adults specifically, randomized-controlled research would be ideal for examining the efficacy of CBT as well as factors proposed to moderate its utility in older trauma survivors. Incorporating indices of cognitive functioning would be especially helpful in differentiating the impact of chronological age on treatment outcome from the effects of cognitive ability more generally. This may be particularly important in addressing the effectiveness of cognitive-oriented therapies with this population. Designs including individuals across a greater range of adulthood also may allow researchers to examine age as a continuous moderator of treatment outcome and begin to address the influence of factors such as “psychological mindedness.” Aging veteran populations from World War II, the Korean War, and Vietnam make this an increasingly viable option for researchers.
The growing population of elderly combat veterans may provide more opportunity to examine the effects of age on treatment outcome, but investigators would be remiss to overlook survivors of more recent, non-combat trauma. The majority of the existing treatment literature is specific to survivors of war-related trauma, and failure to fully examine the effects of trauma mode and time since exposure may unduly limit generalizability of results. Individuals with a history of PTSD persisting over a period of decades (i.e., older veterans) may be expected to be more treatment resistant than those with less time to develop avoidance behaviors associated with the maintenance of the disorder. Examination of treatment efficacy across modes of trauma and time since exposure may elucidate specific factors that arise as barriers to treatment and help to identify optimal windows of intervention.
Finally, it seems prudent for future work in this area to consider the degree of client agedness. We have consistently operationalized “older adults” as those ages 65 and over, but Cook and Niederehe (2007) offer compelling arguments to differentiate between young-old (65 –74), middle-old (75 – 84), and old-old (> 85). Older adults include a heterogeneous collection of individuals, and considerations made for clients at age 95 will be different than for those at age 65. Specification of particular age subgroups will serve to improve the clarity of this literature.
Our understanding of PTSD among older adults remains limited but is growing. Existing opinion in this area often seems to imply that older trauma survivors may be unable or too vulnerable to appreciate the benefits of treatments known to be effective in younger populations. The available data, by contrast, suggests that older adults actually may be more psychologically robust to the effects of trauma than their younger counterparts. In addition, little evidence exists to suggest that older clients are less amenable to current state-of-the-art treatments for PTSD. As with any clinical case, practitioners should take care to acknowledge and to be sensitive to age-specific issues. However, clinicians would be remiss to allow advanced age to lower the accepted standard of care for older survivors of trauma.
Acknowledgments
This research was supported in part by grants from the National Institute of Mental Health awarded to J. Gayle Beck (MH64777) and Joshua D. Clapp (F31 MH083385) The authors would like to thank Sarah A. Palyo, Ph.D. for her role as co-therapist for the current treatment group
Footnotes
The Beck et al. (2009) pilot study included two groups containing an older adult, each age 69.
The names and personal details of group members have been changed to protect confidentiality
Average latency from pre-treatment assessment to beginning of GCBT for the current group was 9 weeks
References
- Acierno R, Ruggiero KJ, Kilpatrick DG, Resnick HS, Galea S. Risk and protective factors for psychopathology among older versus younger adults after the 2004 Florida hurricanes. American Journal of Geriatric Psychiatry. 2006;14:1051–1059. doi: 10.1097/01.JGP.0000221327.97904.b0. [DOI] [PubMed] [Google Scholar]
- Aldwin CM. Does age affect the stress and coping process? Implications of age differences in perceived control. Journal of Gerontology: Psychological Sciences. 1991;46:174–180. doi: 10.1093/geronj/46.4.p174. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. Washington DC: Author; 2000. text revision. [Google Scholar]
- American Psychiatric Association. Practice guideline for the treatment of patients with acute stress disorder and posttraumatic stress disorder. 2004 http://www.psychiatryonline.com/pracGuide/loadGuidelinePdf.aspx?file=ASD_PTSD_05-15-06. [PubMed]
- American Psychological Association Working Group on the Older Adult. Guidelines for psychological practice with older adults. Professional Psychology: Research and Practice. 1998;29:413–427. [Google Scholar]
- Averill PM, Beck JG. Posttraumatic stress disorder in older adults: A conceptual review. Journal of Anxiety Disorders. 2000;14:133–156. doi: 10.1016/s0887-6185(99)00045-6. [DOI] [PubMed] [Google Scholar]
- Ayers CR, Sorrell JT, Thorp SR, Wetherell JL. Evidence-based psychological treatments for late-life anxiety. Psychology and Aging. 2007;22:8–17. doi: 10.1037/0882-7974.22.1.8. [DOI] [PubMed] [Google Scholar]
- Beck JG, Coffey SF. Group Cognitive Behavioral Treatment for PTSD: Treatment of motor vehicle accident survivors. Cognitive and Behavioral Practice. 2005;12:267–277. doi: 10.1016/s1077-7229(05)80049-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck JG, Coffey SF, Foy DW, Keane TM, Blanchard EB. Group Cognitive Behavior Therapy for Posttraumatic Stress Disorder: An initial randomized pilot study. Behavior Therapy. 2009;40:82–92. doi: 10.1016/j.beth.2008.01.003. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown G. Manual for the Beck Depression Inventory II. (BDI-II) San Antonio, TX: Psychological Cooperation; 1996. [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Klauminzer G, Charney DS, Keane TM. Clinician-Administered PTSD Scale (CAPS) Boston, MA: National Center for Post-traumatic Stress Disorder, Behavioral Science Division; 1990. [Google Scholar]
- Blanchard EB, Hickling EJ. After the crash. Washington, DC: American Psychological Association; 1997. [Google Scholar]
- Blanchard EB, Hickling EJ, Barton KA, Taylor AE, Loos WR, Jones-Alexander J. One-year prospective follow-up of motor vehicle accident victims. Behaviour Research and Therapy. 1996;34:775–786. doi: 10.1016/0005-7967(96)00038-1. [DOI] [PubMed] [Google Scholar]
- Blanchard EB, Hickling EJ, Devineni T, Veazey CH, Galovski TE, Mundy E, et al. A controlled evaluation of cognitive behavioral therapy for posttraumatic stress disorder in motor vehicle accident survivors. Behaviour Research and Therapy. 2003;41:79–96. doi: 10.1016/s0005-7967(01)00131-0. [DOI] [PubMed] [Google Scholar]
- Boehnlein JK, Sparr LF. Group treatment with WWII ex-POW’s: Long-term posttraumatic adjustment in a geriatric population. American Journal of Psychotherapy. 1993;47:273–281. doi: 10.1176/appi.psychotherapy.1993.47.2.273. [DOI] [PubMed] [Google Scholar]
- Bonwick RJ, Morris PLP. Review: Post-Traumatic Stress Disorder in elderly war veterans. International Journal of Geriatric Psychiatry. 1996;11:1071–1076. [Google Scholar]
- Bonwick R. Letters to the editor: Group treatment programme for elderly war veterans with PTSD. International Journal of Geriatric Psychiatry. 1998;13:64–67. doi: 10.1002/(sici)1099-1166(199801)13:1<64::aid-gps730>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- Burgmer M, Heuft G. Occurrence and treatment of post-traumatic stress disorder in an elderly patient after a traffic accident. International Journal of Geriatric Psychiatry. 2004;19:185–188. doi: 10.1002/gps.1047. [DOI] [PubMed] [Google Scholar]
- Cook JM, Niederehe G. Trauma in older adults. In: Friedman M, Keane T, Resick P, editors. Handbook of PTSD: Science and Practice. New York: Guilford Press; 2007. pp. 252–276. [Google Scholar]
- Cook JM, Ruzek JI, Cassidy E. Possible association of posttraumatic stress disorder with cognitive impairment among older adults. Psychiatric Services. 2003;54:1223–1225. doi: 10.1176/appi.ps.54.9.1223. [DOI] [PubMed] [Google Scholar]
- DiNardo PA, Brown TA, Barlow DH. Anxiety Disorders Interview Schedule for DSM-IV (ADIS-IV) Albany, NY: Graywind Publications; 1994. [Google Scholar]
- Flint AJ. Anxiety disorders. In: Sadavoy J, Jarvik L, Grossberg G, Meyers B, editors. Comprehensive Textbook of Geriatric Psychiatry. 3. New York: W. W. Norton; 2004. pp. 678–699. [Google Scholar]
- Foa EB, Rothbaum BO, Riggs D, Murdock T. Treatment of posttraumatic stress disorder in rape victims: A comparison between cognitive-behavioral procedures and counseling. Journal of Consulting and Clinical Psychology. 1991;59:715–723. doi: 10.1037//0022-006x.59.5.715. [DOI] [PubMed] [Google Scholar]
- Fontana A, Rosenheck R. Traumatic war stressors and psychiatric symptoms among World War II, Korean, and Vietnam War veterans. Psychology and Aging. 1994;9:27–33. doi: 10.1037//0882-7974.9.1.27. [DOI] [PubMed] [Google Scholar]
- Frueh BC, Grubaugh AL, Acierno R, Elhai JD, Magruder KM. Age differences in posttraumatic stress disorder, psychiatric disorders, and healthcare service use among veterans in Veterans Affairs primary care clinics. American Journal of Geriatric Psychiatry. 2007;15:660–672. doi: 10.1097/JGP.0b013e3180487cc2. [DOI] [PubMed] [Google Scholar]
- Games JE, Hayden CT. Abating the trauma of World War II and Korean Conflict combat veterans. VA Practitioner. 1991;8:69–71. [Google Scholar]
- Green BL, Gleser GC, Lindy JD, Grace MC, Leonard A. Age-related reactions to the Buffalo Creek dam collapse: Effects in the second decade. In: Miller T, editor. Clinical Disorders and Stressful Life Events. Madison, CT: International Universities Press; 1996. pp. 283–305. [Google Scholar]
- Hankin CS. Treatment of older adults with posttraumatic stress disorder. In: Maercker A, editor. Treatment of PTSD. New York: Springer; 1997. pp. 357–384. [Google Scholar]
- Hyer L, Woods MG. Phenomenology and treatment of trauma in later life. In: Follette V, Ruzek J, Abueg F, editors. Cognitive-Behavioral Therapies for Trauma. New York: Guilford Press; 1998. pp. 383–414. [Google Scholar]
- Keane TM, Marshall AD, Taft CT. Posttraumatic Stress Disorder: Etiology, epidemiology, and treatment outcome. Annual Review of Psychology. 2006;2:161–197. doi: 10.1146/annurev.clinpsy.2.022305.095305. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry. 1995;52:1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Kubany ES, Hill EE, Owens JA, Iannce-Spencer C, McCaig MA, Tremayne KJ. Cognitive trauma therapy for battered women with PTSD (CTT-BW) Journal of Consulting and Clinical Psychology. 2004;72:3–18. doi: 10.1037/0022-006X.72.1.3. [DOI] [PubMed] [Google Scholar]
- Lipton MI, Schaffer WR. Post-Traumatic Stress Disorder in the older veteran. Military Medicine. 1986;151:522–524. [PubMed] [Google Scholar]
- Maercker A. Life-Review Technique in the treatment of PTSD in elderly patients; Rationale and three single case studies. Journal of Clinical Gereopsychology. 2002;8:239–249. [Google Scholar]
- Markowitz JD. Post-Traumatic Stress Disorder in an elderly combat veteran: A case report. Military Medicine. 2007;172:659–662. doi: 10.7205/milmed.172.6.659. [DOI] [PubMed] [Google Scholar]
- Mohlman J. Psychosocial treatment of late-life generalized anxiety disorder: Current status and future directions. Clinical Psychology Review. 2004;24:149–169. doi: 10.1016/j.cpr.2004.01.001. [DOI] [PubMed] [Google Scholar]
- Norris FH, Slone LB. The epidemiology of trauma and PTSD. In: Friedman M, Keane T, Resick P, editors. Handbook of PTSD: Science and Practice. New York: Guilford Press; 2007. pp. 78–98. [Google Scholar]
- Resick PA, Schnicke MK. Cognitive processing therapy for sexual assault victims. Journal of Consulting and Clinical Psychology. 1992;60:748–756. doi: 10.1037//0022-006x.60.5.748. [DOI] [PubMed] [Google Scholar]
- Russo SA, Hersen M, Van Hasselt VB. Treatment of reactivated Post-Traumatic Stress Disorder: Imaginal exposure in an older adult with multiple traumas. Behavior Modification. 2003;25:94–115. doi: 10.1177/0145445501251006. [DOI] [PubMed] [Google Scholar]
- Scogin F, McElreath L. Efficacy of psychosocial treatments for geriatric depression: A quantitative review. Journal of Consulting and Clinical Psychology. 1994;6:69–74. doi: 10.1037//0022-006x.62.1.69. [DOI] [PubMed] [Google Scholar]
- Shapiro F. Eye movement desensitization: A new treatment for post-traumatic stress disorder. Journal of Behavior Therapy and Experimental Psychiatry. 1989;20:211–217. doi: 10.1016/0005-7916(89)90025-6. [DOI] [PubMed] [Google Scholar]
- Shapiro F. Eye Movement Desensitization and Reprocessing: Basic Principles, Protocols, and Procedures. New York: Guildford Press; 1995. [Google Scholar]
- Schnurr PP, Friedman MJ, Lavori PW, Hsieh FY. Design of Department of Veterans Affairs Cooperative Study no. 420: Group treatment of posttraumatic stress disorder. Controlled Clinical Trials. 2001;22:74–88. doi: 10.1016/s0197-2456(00)00118-5. [DOI] [PubMed] [Google Scholar]
- Shore JH, Vollmer WM, Tatum EI. Community patterns of posttraumatic stress disorders. Journal of Nervous and Mental Disease. 1989;177:681–685. doi: 10.1097/00005053-198911000-00004. [DOI] [PubMed] [Google Scholar]
- Solomon SD, Davidson JRT. Trauma: Prevalence, impairment, service use, and cost. Journal of Clinical Psychiatry. 1997;58 (Suppl 9):5–11. [PubMed] [Google Scholar]
- Tarrier N, Pilgrim H, Sommerfield C, Faragher B, Reynolds M, Graham E, et al. A randomized trial of cognitive therapy and imaginal exposure in the treatment of chronic posttraumatic stress disorder. Journal of Consulting and Clinical Psychology. 1999;67:13–18. doi: 10.1037//0022-006x.67.1.13. [DOI] [PubMed] [Google Scholar]
- Weiss DS, Marmar CR. The Impact of Events Scale-Revised. In: Wilson J, Keane T, editors. Assessing Psychological Trauma and PTSD. New York: Guilford Press; 1997. pp. 399–411. [Google Scholar]