Abstract
The ongoing controversy over publication of two studies involving the transmission in ferrets of H5N1 (H5) subtype influenza viruses and the recommendations of the National Science Advisory Board for Biosecurity to redact key details in the manuscripts call for an examination of relevant scientific facts. In addition, there are calls in the media to destroy the viruses, curtail future research in this area, and protect the public from such “frightening” research efforts. Fear needs to be put to rest with solid science and not speculation.
Keywords: avian influenza, moratorium, World Health Organization, case fatality rate, National Science Advisory Board for Biosecurity
Facts
What Are the Studies About?
The two studies discussed here are by Ron Fouchier at Erasmus Medical Center in Rotterdam and Yoshihiro Kawaoka at the University of Wisconsin (not yet published by Science and Nature, respectively). Both senior authors are experienced virologists who have worked for years with highly pathogenic avian influenza viruses. Their respective studies differ in many ways, but both were designed to answer one question of whether H5 influenza viruses can achieve sustainable aerosol transmission in ferrets.
The studies use the age-old method of virus adaptation by repeated passage in cells or in naive animal hosts. H5 viruses (WT or with specific mutations introduced that are known to confer tropism to mammalian tissue) were passaged in ferrets, a well established animal model for the study of influenza transmission (1–5). Ultimately, both studies determined that, indeed, H5 viruses could acquire aerosol transmissibility while maintaining virulence in ferrets.*
The experiments demonstrate the important finding that aerosol transmission between ferrets can be determined by a relatively small number of mutations that do not significantly change virus virulence. Thus, the need for continued surveillance efforts around H5 viruses is clearly reinforced by these works, as is the importance of continuing to develop H5 vaccines and therapeutics (6).
How Relevant Are These Studies for Humans?
The ferret system is an important model for the study of influenza transmission, virulence, and immunity (7–11). Generally, the ferret model provides a more accurate reflection of how influenza viruses affect humans compared with the mouse model (another common system) (12). Ferrets are quite susceptible to infection with influenza viruses. However, it is not clear that all virus strains that replicate in and transmit between ferrets necessarily do so in humans (13, 14). Ferrets are also more likely than humans to have disseminated, multiorgan influenza disease including neurologic sequelae resulting from virus replication in the brain (15–18). Thus, the mutations identified in the studies by Fouchier and Kawaoka could cause the viruses to be more transmissible between humans, but this is simply unknowable from the available data. The viruses may well be more adapted to ferrets, but not more adapted to other mammals; one cannot directly extrapolate from the data to make predictions about humans. In fact, passage of viruses in a different host is the most frequently used strategy to reduce viral virulence in humans. Many live, attenuated virus vaccines have been generated by that approach, including those for poliovirus and yellow fever virus. Further experiments in other mammalian systems would enhance our understanding of the potential for the H5 viruses to transmit between nonferret mammals and/or cause disease in these systems (19–21).
It is known that H5 viruses have been circulating in poultry for at least 50 years (probably much longer) and that they cause natural infection and even transmit between some mammals such as pigs, dogs, and cats (21–24) (Figs. 1 and 2). Despite regular human contact with animal reservoirs and the virus’ propensity to mutate, strains able to cause sustained disease in humans have not emerged. In fact, in humans, only influenza viruses of the subtypes H1, H2, and H3 have circulated during the past 100 years, suggesting that other subtypes may not easily become significant human pathogens.
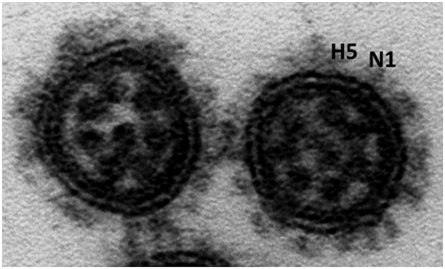
Fig. 1.
EM image of influenza virus particles. Image courtesy of Yi-ying Chou.
Fig. 2.
Influenza viruses can infect many different animal species, including birds, pigs, dogs, cats, ferrets, monkeys, horses, and humans. Animal model systems include mice, ferrets, and guinea pigs.
Why Is it Important to Have the Full Data Published?
With respect to the specific papers by Fouchier and Kawaoka, it would be important for other scientists to replicate portions of these works to test new vaccines/therapeutic agents and for continued studies on the molecular aspects of influenza transmission, a topic that is extremely important yet relatively poorly understood (25–27).
From a broader perspective, publishing relevant methods and data related to important experimental findings is fundamental to progress in science. Enabling others to repeat published data makes it possible to expand on what is known; the cycle of publication followed by experimental replication and advancement has resulted in the majority of our scientific and medical achievements. With specific reference to influenza viruses, the free flow of data has enabled the timely development of vaccines and other medications for seasonal and pandemic disease, and has, without question, saved millions of lives.
Fear
With the understanding that all parties involved have worthy intentions, it is difficult to ignore some of the incongruities that overshadow discussions related to H5 viruses and the publication of these two manuscripts. Examination of the topics discussed below may relieve some of the fear that is fueling the current debate.
Is the Case Fatality Rate for Human H5 Infections Truly Greater than 50%?
At the heart of this controversy is the notion that the case fatality rate for human H5 infections is in the range of 50% to 80%. This rate is derived from the list of H5 cases that have been “confirmed” under World Health Organization (WHO) guidelines; the list tallies 573 cases in 15 countries (as of December 15, 2011), with nearly 60% of total cases resulting in death (28). The frequency and certainty with which this staggering fatality rate is reported is troubling when one considers how the numbers are generated; in order for a case to be confirmed by WHO, a person must have an acute, febrile respiratory illness (temperature >38 °C/100.3 °F) with known H5 exposure in the 7 days preceding symptom onset and have molecular confirmation of H5 infection by a WHO-approved laboratory (e.g., virus isolation, PCR, serology) (29). This definition does not allow for asymptomatic infections and essentially requires that a person actively seek medical help at a hospital that is equipped to draw samples and ship them to an approved laboratory. Given that rural populations in developing countries are most commonly affected by H5 viruses, it seems unlikely that even a small fraction of the total number of infected cases has been accounted for under the WHO surveillance system. Also, the fatal cases that have been reported are most likely caused by mega-doses of H5 virus inhaled by the patients, who are living in very close contact with infected poultry. Transmission involving small doses of virus (as observed under regular aerosol transmission conditions) may not result in overt disease. Of the 10 largest studies of which we are aware (N ≥ 500) (30–39), which document seroevidence in humans for H5 infections, two studies report no seropositivity and the other eight report rates ranging from 0.2% to 5.6%; the studies are mostly conducted in rural areas where H5 infections have been previously documented (30–39). Even if only a low percentage of the rural population is asymptomatically/subclinically infected, the case fatality rate that is offered by the WHO—and that is driving this controversy—is likely orders of magnitude too high. This suggests that more work should be done to determine an accurate case fatality rate for H5 infections, which takes into account mild and asymptomatic cases.
Why These Papers, Why Now?
The type of work performed in the studies under evaluation is quite common in virology because it is a useful way to study molecular determinants of virus adaptation, pathogenesis, and transmission. The reasoning behind the selection by the National Science Advisory Board for Biosecurity of these specific papers for redaction/censorship seems somewhat arbitrary relative to what has previously been published in the field of influenza.
In 2005, the complete sequences for the 1918 pandemic influenza virus were published in Nature and methods describing the rescue of the 1918 virus were published in Science (40, 41). In 2006, both Science and Nature published reports of specific mutations that enable the H5 viral hemagglutinin to bind human, rather than avian, tissues (42, 43). In 2012, a report from the Centers for Disease Control and Prevention that bears striking resemblance, in principle, to the works by Fouchier and Kawaoka was already published in Virology; it describes mutations in an H5N1 virus that confer airborne transmissibility between ferrets (44). Studies have also been published recently that describe mutations enabling other potential pandemic strains to transmit between ferrets (45, 46) or that make currently circulating virus strains more virulent (47).
These are a small fraction of studies published during the past decade that could have been considered controversial (some were controversial at the time, but all were published in full). We know from studies like these that, for example, the 2009 pandemic vaccine protects against the 1918 pandemic virus and thus the 1918 strain is not a pandemic threat at this time (48), nor would it be of any advantage for a bioterrorist to lay his/her hands on it. Other striking examples of achievements based on the free exchange of potentially controversial information are the elimination of SARS corona virus in only 6 months and the fact that the dangers of HIV have been dramatically reduced by the development of effective antiviral treatments. None of this would have been possible without the uncensored exchange of scientific data.
Could the Data from These Two Papers Realistically Be Used to Generate an H5N1 Biologic Weapon?
The answer is simply no. It would be unrealistic to assume that these ferret viruses could be successfully used against humans. Even if the viruses were transmissible between humans and were to cause disease in humans, viable vaccine candidates for H5 viruses do exist and available influenza medications have good activity against H5 strains (49, 50). Additionally, safely generating a stock of highly virulent influenza virus based on raw sequence information would require (i) access to a sophisticated laboratory setting, (ii) proficiency in relevant concepts of molecular biology, and (iii) experience with laboratory methods related to influenza viruses (e.g., rescue by reverse genetics, growth and harvesting of the virus, storage).
In contrast to the expertise and resources that would be required to use nucleic acid sequences for virus production, passing a virus in animals (or humans) to adapt it to a mammalian host would require no training or data, and could likely be done very quickly. Still, this approach is extremely unlikely to be successful. As mentioned earlier, passing viruses in animals typically results in attenuation of the disease phenotype and, perhaps most importantly, this experiment has been and is going on every day in a natural setting. So far, of the likely millions of mammals that have hosted H5 viruses, none of the strains that have emerged are real human pathogens. It would be very difficult for a bioterrorist to come up with a human virus strain that is transmissible and still highly virulent. Under natural conditions, however, there is virtually unlimited allowance for generation of capable viruses, the opportunities for infection of humans are plentiful, and the evolutionary pressures of selection are great. If anyone could do it, Nature could.
Footnotes
The authors declare no conflict of interest.
*Details of the manuscripts have already been disclosed to many in the field of influenza virology; for example, one of us (P.P.) was sent one of the manuscripts in September 2011 as a courtesy and to elicit comments.
References
- 1.Itoh Y, et al. In vitro and in vivo characterization of new swine-origin H1N1 influenza viruses. Nature. 2009;460:1021–1025. doi: 10.1038/nature08260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Maines TR, et al. Transmission and pathogenesis of swine-origin 2009 A(H1N1) influenza viruses in ferrets and mice. Science. 2009;325:484–487. doi: 10.1126/science.1177238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Van Hoeven N, et al. Human HA and polymerase subunit PB2 proteins confer transmission of an avian influenza virus through the air. Proc Natl Acad Sci USA. 2009;106:3366–3371. doi: 10.1073/pnas.0813172106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Memoli MJ, et al. An early ‘classical’ swine H1N1 influenza virus shows similar pathogenicity to the 1918 pandemic virus in ferrets and mice. Virology. 2009;393:338–345. doi: 10.1016/j.virol.2009.08.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Maines TR, et al. Lack of transmission of H5N1 avian-human reassortant influenza viruses in a ferret model. Proc Natl Acad Sci USA. 2006;103:12121–12126. doi: 10.1073/pnas.0605134103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Steel J. New strategies for the development of H5N1 subtype influenza vaccines: Progress and challenges. BioDrugs. 2011;25:285–298. doi: 10.1007/BF03256169. [DOI] [PubMed] [Google Scholar]
- 7.Maines TR, et al. Avian influenza (H5N1) viruses isolated from humans in Asia in 2004 exhibit increased virulence in mammals. J Virol. 2005;79:11788–11800. doi: 10.1128/JVI.79.18.11788-11800.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Belser JA, et al. Pathogenesis of avian influenza (H7) virus infection in mice and ferrets: Enhanced virulence of Eurasian H7N7 viruses isolated from humans. J Virol. 2007;81:11139–11147. doi: 10.1128/JVI.01235-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Leigh MW, Connor RJ, Kelm S, Baum LG, Paulson JC. Receptor specificity of influenza virus influences severity of illness in ferrets. Vaccine. 1995;13:1468–1473. doi: 10.1016/0264-410x(95)00004-k. [DOI] [PubMed] [Google Scholar]
- 10.Campbell D, Sweet C, Smith H. Comparisons of virulence of influenza virus recombinants in ferrets in relation to their behaviour in man and their genetic constitution. J Gen Virol. 1979;44:37–44. doi: 10.1099/0022-1317-44-1-37. [DOI] [PubMed] [Google Scholar]
- 11.Belser JA, et al. Pathogenesis and transmission of triple-reassortant swine H1N1 influenza viruses isolated before the 2009 H1N1 pandemic. J Virol. 2011;85:1563–1572. doi: 10.1128/JVI.02231-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Belser JA, Szretter KJ, Katz JM, Tumpey TM. Use of animal models to understand the pandemic potential of highly pathogenic avian influenza viruses. Adv Virus Res. 2009;73:55–97. doi: 10.1016/S0065-3527(09)73002-7. [DOI] [PubMed] [Google Scholar]
- 13.Smith JH, et al. Comparative pathology in ferrets infected with H1N1 influenza A viruses isolated from different hosts. J Virol. 2011;85:7572–7581. doi: 10.1128/JVI.00512-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ma W, et al. Identification of H2N3 influenza A viruses from swine in the United States. Proc Natl Acad Sci USA. 2007;104:20949–20954. doi: 10.1073/pnas.0710286104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zitzow LA, et al. Pathogenesis of avian influenza A (H5N1) viruses in ferrets. J Virol. 2002;76:4420–4429. doi: 10.1128/JVI.76.9.4420-4429.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.JA Lednicky, et al. Ferrets develop fatal influenza after inhaling small particle aerosols of highly pathogenic avian influenza virus A/Vietnam/1203 (H5N1) Virol J. 2010;7:231. doi: 10.1186/1743-422X-7-231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bodewes R, Rimmelzwaan GF, Osterhaus ADME. Animal models for the preclinical evaluation of candidate influenza vaccines. Expert Rev Vaccines. 2010;9:59–72. doi: 10.1586/erv.09.148. [DOI] [PubMed] [Google Scholar]
- 18.Yen HL, et al. Inefficient transmission of H5N1 influenza viruses in a ferret contact model. J Virol. 2007;81:6890–6898. doi: 10.1128/JVI.00170-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lowen AC, Mubareka S, Tumpey TM, García-Sastre A, Palese P. The guinea pig as a transmission model for human influenza viruses. Proc Natl Acad Sci USA. 2006;103:9988–9992. doi: 10.1073/pnas.0604157103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rigoni M, et al. The mouse model is suitable for the study of viral factors governing transmission and pathogenesis of highly pathogenic avian influenza (HPAI) viruses in mammals. Vet Res. 2010;41:66. doi: 10.1051/vetres/2010038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kuiken T, et al. Avian H5N1 influenza in cats. Science. 2004;306:241. doi: 10.1126/science.1102287. [DOI] [PubMed] [Google Scholar]
- 22.Burgos S, Burgos SA. Reports of avian influenza H5N1 in cats and dogs. Int J Poult Sci. 2007;6:1003. [Google Scholar]
- 23.World Health Organization . Avian Influenza A(H5N1)—Update 31: Situation (Poultry) in Asia: Need for a Long-Term Response, Comparison with Previous Outbreaks. Geneva: WHO; 2004. [PubMed] [Google Scholar]
- 24.Nidom CA, et al. Influenza A (H5N1) viruses from pigs, Indonesia. Emerg Infect Dis. 2010;10:1515–1523. doi: 10.3201/eid1610.100508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tellier R. Aerosol transmission of influenza A virus: A review of new studies. J R Soc Interface. 2009;6(suppl 6):S783–S790. doi: 10.1098/rsif.2009.0302.focus. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Myers KP, Olsen CW, Gray GC. Cases of swine influenza in humans: A review of the literature. Clin Infect Dis. 2007;44:1084–1088. doi: 10.1086/512813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Subbarao K, Joseph T. Scientific barriers to developing vaccines against avian influenza viruses. Nat Rev Immunol. 2007;7:267–278. doi: 10.1038/nri2054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.World Health Organization Cumulative Number of Confirmed Human Cases for Avian Influenza A(H5N1) Reported to WHO, 2003–2011. 2011. Available at http://www.who.int/entity/influenza/human_animal_interface/EN_GIP_20111215CumulativeNumberH5N1cases.pdf. Accessed January 6, 2010.
- 29.World Health Organization WHO Case Definitions for Human Infections with Influenza A(H5N1) Virus. 2006. Available at http://www.who.int/influenza/resources/documents/case_definition2006_08_29/en/index.html. Accessed January 6, 2010.
- 30.Bridges CB, et al. Risk of influenza A (H5N1) infection among poultry workers, Hong Kong, 1997-1998. J Infect Dis. 2002;185:1005–1010. doi: 10.1086/340044. [DOI] [PubMed] [Google Scholar]
- 31.Buchy P, et al. Kinetics of neutralizing antibodies in patients naturally infected by H5N1 virus. PLoS ONE. 2010;5:e10864. doi: 10.1371/journal.pone.0010864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cavailler P, et al. Seroprevalence of anti-H5 antibody in rural Cambodia, 2007. J Clin Virol. 2010;48:123–126. doi: 10.1016/j.jcv.2010.02.021. [DOI] [PubMed] [Google Scholar]
- 33.Dejpichai R, et al. Seroprevalence of antibodies to avian influenza virus A (H5N1) among residents of villages with human cases, Thailand, 2005. Emerg Infect Dis. 2009;15:756–760. doi: 10.3201/eid1505.080316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Santhia K, et al. Avian influenza A H5N1 infections in Bali Province, Indonesia: A behavioral, virological and seroepidemiological study. Influenza Other Respir Viruses. 2009;3:81–89. doi: 10.1111/j.1750-2659.2009.00069.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schultsz C, et al. Prevalence of antibodies against avian influenza A (H5N1) virus among Cullers and poultry workers in Ho Chi Minh City, 2005. PLoS ONE. 2009;4:e7948. doi: 10.1371/journal.pone.0007948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Vong S, et al. Risk factors associated with subclinical human infection with avian influenza A (H5N1) virus—Cambodia, 2006. J Infect Dis. 2009;199:1744–1752. doi: 10.1086/599208. [DOI] [PubMed] [Google Scholar]
- 37.Khuntirat BP, et al. Evidence for subclinical avian influenza virus infections among rural Thai villagers. Clin Infect Dis. 2011;53:e107–e116. doi: 10.1093/cid/cir525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lu CY, et al. Potential infections of H5N1 and H9N2 avian influenza do exist in Guangdong populations of China. Chin Med J (Engl) 2008;121:2050–2053. [PubMed] [Google Scholar]
- 39.Wang M, Fu CX, Zheng BJ. Antibodies against H5 and H9 avian influenza among poultry workers in China. N Engl J Med. 2009;360:2583–2584. doi: 10.1056/NEJMc0900358. [DOI] [PubMed] [Google Scholar]
- 40.Taubenberger JK, et al. Characterization of the 1918 influenza virus polymerase genes. Nature. 2005;437:889–893. doi: 10.1038/nature04230. [DOI] [PubMed] [Google Scholar]
- 41.Tumpey TM, et al. Characterization of the reconstructed 1918 Spanish influenza pandemic virus. Science. 2005;310:77–80. doi: 10.1126/science.1119392. [DOI] [PubMed] [Google Scholar]
- 42.Stevens J, et al. Structure and receptor specificity of the hemagglutinin from an H5N1 influenza virus. Science. 2006;312:404–410. doi: 10.1126/science.1124513. [DOI] [PubMed] [Google Scholar]
- 43.Yamada S, et al. Haemagglutinin mutations responsible for the binding of H5N1 influenza A viruses to human-type receptors. Nature. 2006;444:378–382. doi: 10.1038/nature05264. [DOI] [PubMed] [Google Scholar]
- 44.Chen LM, et al. In vitro evolution of H5N1 avian influenza virus toward human-type receptor specificity. Virology. 2012;422:105–113. doi: 10.1016/j.virol.2011.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kimble JB, Sorrell E, Shao H, Martin PL, Perez DR. Compatibility of H9N2 avian influenza surface genes and 2009 pandemic H1N1 internal genes for transmission in the ferret model. Proc Natl Acad Sci USA. 2011;108:12084–12088. doi: 10.1073/pnas.1108058108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pappas C, et al. Receptor specificity and transmission of H2N2 subtype viruses isolated from the pandemic of 1957. PLoS ONE. 2010;5:e11158. doi: 10.1371/journal.pone.0011158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Houng HSH, et al. Emergent 2009 influenza A (H1N1) viruses containing HA D222N mutation associated with severe clinical outcomes in the Americas. J Clin Virol. 2012;53:12–15. doi: 10.1016/j.jcv.2011.09.004. [DOI] [PubMed] [Google Scholar]
- 48.Medina RA, et al. Pandemic 2009 H1N1 vaccine protects against 1918 Spanish influenza virus. Nat Commun. 2010;1:28. doi: 10.1038/ncomms1026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Chen GL, Subbarao K. Live attenuated vaccines for pandemic influenza. Curr Top Microbiol Immunol. 2009;333:109–132. doi: 10.1007/978-3-540-92165-3_5. [DOI] [PubMed] [Google Scholar]
- 50.Galli G, et al. Adjuvanted H5N1 vaccine induces early CD4+ T cell response that predicts long-term persistence of protective antibody levels. Proc Natl Acad Sci USA. 2009;106:3877–3882. doi: 10.1073/pnas.0813390106. [DOI] [PMC free article] [PubMed] [Google Scholar]