Abstract
The rostral ventromedial medulla (RVM) is part of descending circuitry that modulates nociceptive processing at the level of the spinal cord. RVM output can facilitate pain transmission under certain conditions such as inflammation, and thereby contribute to hyperalgesia. Evidence suggests that substance P and activation of neurokinin-1 (NK-1) receptors in the RVM are involved in descending facilitation of nociception. We showed previously that injection of NK-1 receptor antagonists into the RVM attenuated mechanical and heat hyperalgesia produced by intraplantar injection of capsaicin. Furthermore, intraplantar injection of capsaicin excited ON cells in the RVM and inhibited ongoing activity of OFF cells. In the present studies, we therefore examined changes in responses of RVM neurons to mechanical and heat stimuli after intraplantar injection of capsaicin and determined the role of NK-1 receptors by injecting a NK-1 receptor antagonist into the RVM prior to capsaicin. After capsaicin injection, excitatory responses of ON cells and inhibitory responses of OFF cells evoked by mechanical and heat stimuli applied to the injected, but not contralateral, paw were increased. Injection of the NK-1 antagonist L-733,060 did not alter evoked responses of ON or OFF cells but attenuated the capsaicin-evoked enhanced responses of ON cells to mechanical and heat stimuli with less of an effect on the enhanced inhibitory responses of OFF cells. These data support the notion that descending facilitation from RVM contributes to hyperalgesia and that NK-1 receptors, presumably located on ON cells, play an important role in initiating descending facilitation of nociceptive transmission.
Keywords: pain modulation, pain facilitation, descending facilitation, substance P, raphe magnus, nociception, hyperalgesia, electrophysiology
the rostral ventromedial medulla (RVM), which includes the raphe magnus and adjacent nucleus reticularis paragigantocellularis pars α, modulates nociceptive transmission within the dorsal horn of the spinal cord (reviewed by Fields 2000; Mason 2005). Although initial studies focused on descending inhibition (Fields et al. 1983; Mohrland and Gebhart 1980), recent studies indicate that the RVM can facilitate nociceptive transmission (see reviews by Porreca et al. 2002; Suzuki et al. 2004b; Vanegas and Schaible 2004). Behavioral studies have demonstrated facilitation from the RVM in many models associated with hyperalgesia including inflammation (Hamity et al. 2010; Hurley and Hammond 2001; Montagne-Clavel and Oliveras 1994; Ren and Dubner 1996; Watkins et al. 1994), nerve injury (Burgess et al. 2002; Pertovaara et al. 1996), cancer (Donovan-Rodriguez et al. 2006), visceral pain (Coutinho et al. 1998; Zhuo et al. 2002), chronic opioid administration (Bederson et al. 1990; Kaplan and Fields 1991; Vanderah et al. 2001), and intraplantar injection of capsaicin (Pacharinsak et al. 2008).
RVM neurons are classified physiologically as ON, OFF, NEUTRAL, and serotonergic cells (Fields et al. 1983; Gao and Mason 2000). ON cells, which are believed to be pronociceptive, are excited by noxious stimulation, exhibit a burstlike increase in discharge rate just prior to a withdrawal reflex, and are inhibited by morphine. In contrast, OFF cells exhibit a temporal pause in ongoing discharge during noxious stimulation, are excited by morphine, and are thought to inhibit nociceptive transmission (reviewed by Heinricher et al. 2009; Mason 2001). NEUTRAL cells are unaffected by noxious cutaneous stimuli and opioids, and their role in nociceptive modulation is unclear, though they may modulate noxious visceral inputs (Brink and Mason 2003; Brink et al. 2006). Serotonergic cells are a separate group of RVM neurons defined by slow, regular discharge and distinct neurochemistry (Mason 1997).
Electrophysiological studies support a role for increased activity of ON cells in facilitation of nociception. Evoked discharge rates or the proportion of ON cells increased after inflammation (Bederson et al. 1990; Miki et al. 2002), nerve injury (Carlson et al. 2007; Goncalves et al. 2007), intraplantar or intracolonic administration of capsaicin (Budai et al. 2007; Sanoja et al. 2010), chronic morphine (Meng and Harasawa 2007), and acute opioid abstinence (Kaplan and Fields 1991). Although the mechanisms underlying changes in excitability of RVM neurons after injury are unclear, it is likely that multiple neurotransmitter systems play a role. One potential neurotransmitter involved in modulating the excitability of certain RVM neurons is substance P (SP) through activation of neurokinin-1 (NK-1) receptors. NK-1 receptors are found on neurons in the RVM (Budai et al. 2007; Marson and Loewy 1985; Saffroy et al. 1988, 2003), and SP increased excitatory transmission of RVM neurons after inflammation (Zhang and Hammond 2009). In addition, intraplantar administration of capsaicin or iontophoretic application of SP to RVM neurons increased responses of ON cells to iontophoretically applied NMDA (Budai et al. 2007). Moreover, administration of SP into the RVM produced hyperalgesia (Hamity et al. 2010; Lagraize et al. 2010), while NK-1 receptor antagonists attenuated hyperalgesia produced by capsaicin (Pacharinsak et al., 2008) and inflammation (Hamity et al. 2010; Lagraize et al. 2010).
Although these studies suggest that activation of NK-1 receptors within RVM may enhance excitability of ON cells and contribute to descending facilitation of nociceptive transmission, the ability of NK-1 receptors to modulate evoked responses of ON and OFF cells under normal conditions and during hyperalgesia is unknown. Since intraplantar injection of capsaicin in rats produces robust hyperalgesia to mechanical and heat stimuli (Gilchrist et al. 1996) that is attenuated by NK-1 antagonists administered into the RVM (Pacharinsak et al. 2008), we investigated the contribution of NK-1 receptors to changes in response properties of identified RVM neurons after intraplantar injection of capsaicin.
METHODS
Anesthesia and Surgery
Adult male Sprague-Dawley rats (n = 113, 250–375 g; Harlan Industries, Indianapolis, IN) were housed and maintained in a climate-controlled room on a 12:12-h dark-light cycle, with food and water available ad libitum. Each animal was used for one of three electrophysiological experiments: 1) responses of RVM neurons evoked by acute stimuli with preservation of hindlimb withdrawal responses (light anesthesia), 2) responses of RVM neurons evoked by a wide range of noxious stimuli in the absence of withdrawal responses (deep anesthesia), and 3) modulation of responses of RVM neurons by microinjection of NK-1 antagonists into the RVM. All procedures were approved by the Institutional Animal Care and Use Committee at the University of Minnesota and were performed in accordance with the guidelines recommended by the International Association for the Study of Pain.
Rats were initially anesthetized with acepromazine maleate (1–2 mg/kg sc) and ketamine HCl (60 mg/kg sc). A catheter was inserted into the external jugular vein for delivery of supplementary anesthetics during the experiment (methohexital sodium, 30–70 mg·kg−1·h−1). Needle electrodes were inserted into the biceps femoris to record electromyographic (EMG) activity. The EMG activity was not quantified but was used for detecting withdrawal responses. The carotid artery was catheterized for continuous monitoring of blood pressure, and the experiment was terminated if blood pressure fell below 70 mmHg. Rats were placed into a stereotaxic apparatus, a small craniotomy was made over the cerebellum, and dura mater was removed. Core temperature was maintained at ∼37°C with a feedback-controlled heating pad (Harvard Apparatus, Holliston, MA). After surgery, rats were allowed to equilibrate for 1 h. During recording experiments, the infusion rate of methohexital was adjusted and maintained so that rats showed no sign of discomfort, but a withdrawal (EMG) response could be evoked by application of noxious heat (51°C) or mechanical stimuli (pinch) to the paw. After an RVM neuron was classified in the presence of a withdrawal response, the level of anesthesia was deepened for cells whose responses were characterized over a wide range of noxious stimulus intensities and for microinjection studies in order to maintain a constant level of anesthesia over a prolonged period of time. In the absence of withdrawal responses, RVM neurons maintained robust responses to noxious stimuli.
Extracellular Recording from RVM Neurons
Extracellular single unit recordings were obtained with either stainless steel (10 MΩ; Federick Haer, Brunswick, ME) or tungsten (5 MΩ; A-M Systems, Sequim, WA) microelectrodes that were lowered into the RVM with an electronic microdrive (Burleigh Instruments, Fischer, NY). The range of stereotaxic coordinates for all cells studied was AP = −9.9 to −11.5 mm from bregma; DV = +9.4 to +10.6 mm from the cranial surface; L = −1.1 to +1.1 mm from midline (Paxinos and Watson 2005). Neurons were isolated by ongoing discharge, and action potentials were amplified, displayed on a storage oscilloscope, audio-monitored, and discriminated according to amplitude. Only neurons whose action potentials were easily discriminated were studied. Neuronal discharge, EMG activity, stimulus temperature, and time of mechanical stimulation and capsaicin injection were collected with a customized data acquisition program (Lab View, National Instruments, Austin, TX or Spike2, Cambridge Electronic Design, Cambridge, UK) and stored on a computer for off-line analyses. Cells were initially characterized qualitatively according to their responses to a brief pinch to the tail with the experimenter's fingers. Cells were then functionally classified as ON, OFF, or NEUTRAL according to their ongoing spontaneous discharge and their responses evoked by application of noxious heat (51°C for 5 s) applied to the plantar surface of one hind paw. ON and OFF cells were classified by an abrupt increase or decrease, respectively, in discharge in response to noxious heat. Neurons displaying a slow and regular discharge that were likely to be serotonergic (Li and Bayliss 1998; Mason 1997) were not studied. Only one neuron was studied per animal.
For experiments using combined recording and drug microinjection, extracellular recordings were made with a stainless steel microelectrode attached to a single glass pipette as described previously (Heinricher and Neubert 2004). The tips of the electrode and pipette were ∼300 μm apart, with the pipette having an outer diameter of ∼70 μm. The infusion pipette was connected to a 1-μl Hamilton syringe (Reno, NV) by PE-50 tubing for either vehicle or drug infusion.
Drug Solutions
Capsaicin (Sigma, St. Louis, MO) was dissolved in 5% Tween 80 and saline to a concentration of 0.1% and injected into the plantar skin (10 μg in 10 μl) of one hind paw with a 0.5-ml insulin syringe with a 28-gauge needle. A stock solution (10 mM) of the nonpeptide NK-1 receptor antagonist L-733,060 (Tocris, Ellisville, MO), was prepared in distilled water and on the day of the experiment was dissolved in saline to its final concentration. Injections into the RVM were given at a dose of 1.5 pmol in a volume of 0.5 μl and delivered over a period of 3–5 min.
Evoked Response Measures and Experimental Design
Once a neuron was isolated and classified during light anesthesia, anesthesia was deepened and responses evoked by noxious mechanical and heat stimuli were obtained. A test site (2–3 mm in diameter) was marked on the skin in the middle of each plantar hind paw with a felt-tip pen. Noxious mechanical stimuli were applied to the test sites with a von Frey monofilament with a calibrated bending force of 588 mN (60 g) for a period of 5 s. The response for each cell evoked by stimulation of each hind paw was defined as the mean from three trials. This monofilament was chosen because it reliably evoked withdrawal responses in prior behavioral experiments (Pacharinsak et al. 2008). Heat stimuli were delivered to the plantar hind paws with a Peltier device (Yale Instrumentation, New Haven, CT) with a 1-cm2 contact area. The probe was centered on the test sites, and heat stimuli ranging from 35°C to 51°C, each of 5-s duration, were each delivered in ascending order of 2°C increments from a base temperature of 32°C at a ramp rate of 18°C/s. After baseline responses to mechanical and heat stimuli were obtained, rats received an intraplantar injection of 0.1% capsaicin (10 μg in 10 μl) into the left hind paw (referred to as the ipsilateral paw) and responses to mechanical and heat stimuli were obtained at 15, 30, and 60 min after injection.
For studies of neuronal responses during which a withdrawal reflex was present (light anesthesia), responses were evoked by the mechanical stimulus (60 g von Frey monofilament) and by a restricted set of heat stimuli (45°C and 51°C) applied to each hind paw before and at 15, 30, and 60 min after injection of capsaicin into one hind paw. All stimuli were separated by at least 60 s.
The NK-1 receptor antagonist L-733,060 (or vehicle) was delivered into the RVM to determine the contribution of NK-1 receptors to evoked responses of RVM neurons before and after capsaicin. Responses evoked by mechanical and heat stimuli (as described above) were obtained before and after microinjection into the RVM and at 15, 30, and 60 min after intraplantar injection of capsaicin. All of these experiments were done in the absence of a withdrawal reflex.
Histological Verification of Recording Sites
At the end of each experiment, the recording site was marked by passing current (30 μA for 20 s) through the recording electrode. Animals were euthanized with an overdose of methohexital and perfused intracardially with physiological saline followed by 10% formalin with 1% potassium ferrocyanide. Recording sites were verified histologically in 50- or 100-μm sections. Locations of the microlesions were reconstructed with a stereotaxic atlas (Paxinos and Watson 2005), and experiments with recording sites located outside the RVM were discarded.
Data Analysis
Changes in ongoing discharge evoked by capsaicin were analyzed by determining discharge rates (Hz) in consecutive 15-s bins for 60 s before and for 4 min after capsaicin injection. Baseline ongoing discharge rates were determined as the mean rate for 1 min (4 consecutive 15-s bins) prior to injection. A response to capsaicin for any given cell was defined as a change in discharge rate >20% from the baseline discharge rate. Differences in the mean ongoing activity of ON, OFF, and NEUTRAL cells were determined by one-way ANOVA. Mean discharge rates evoked by capsaicin were divided into consecutive 15-s bins and analyzed with one-way repeated-measures ANOVA and Student-Neuman-Keuls post hoc comparisons. Responses evoked by mechanical and heat stimuli were determined by subtracting the number of spontaneous impulses that occurred for 10 s prior to each stimulus from the number of impulses evoked during the stimulus (5 s) and for 5 s after stimulus presentation. Since OFF cells exhibit ongoing activity that is decreased by noxious stimuli, their evoked responses are described as a negative number of impulses. Responses evoked by mechanical and heat stimuli were analyzed by one-way repeated-measures ANOVA followed by Student-Neuman-Keuls comparisons. Mean heat response thresholds were the lowest stimulus temperature that evoked a significant response above ongoing activity. The effects of L-733,060 (or vehicle) on capsaicin and evoked noxious stimuli responses were analyzed by two-way repeated-measures ANOVA followed by Student-Neuman-Keuls comparisons. A P value of <0.05 was considered significant in all cases. Mean (±SE) values are reported throughout the results unless otherwise stated.
RESULTS
Identification of RVM Neurons
A total of 113 neurons located in the RVM were studied. Of these, responses of 66 neurons were used to characterize responses to noxious mechanical and heat stimuli before and after intraplantar injection of capsaicin and 47 neurons were studied for the effects of the NK-1 receptor antagonist on changes in response properties produced by capsaicin. All RVM neurons were initially classified functionally with the presence of a withdrawal response as ON, OFF, or NEUTRAL cells by their response to 51°C (Fig. 1), the highest heat stimulus used in these studies and a stimulus that always elicited a withdrawal reflex. The mean ± SE number of impulses evoked by 51°C was 87.7 ± 17.4 impulses for ON cells and −30.1 ± 5.4 impulses for OFF cells; NEUTRAL cells were unaffected (1.0 ± 2.2 impulses) by the 51°C stimulus.
Fig. 1.
Functional classification of ON and OFF cells. Representative examples are provided for classifying ON (left) and OFF (right) cells according to their responses evoked by a heat stimulus (Stim) of 51°C applied to the plantar surface of the hind paw. All neurons were initially characterized in the presence of a withdrawal response by simultaneously recording EMG activity from the stimulated limb. ON cells exhibited a robust burst of activity and OFF cells exhibited a pause in ongoing activity that was related in time to the EMG activity.
Effects of Capsaicin on Response Properties of RVM Neurons
Of the 66 neurons studied, 28 (42%) were classified as ON cells, 18 (27%) were classified as OFF cells, and the remaining 20 (30%) were considered NEUTRAL cells. After initial characterization using 51°C heat, most cells (n = 49) were studied during deep anesthesia (absence of withdrawal response) in order to maintain a stable level of anesthesia for a prolonged period of time. However, to ensure that anesthesia depth did not alter cellular responses, 17 neurons (5 ON, 7 OFF, and 5 NEUTRAL cells) were studied exclusively during the presence of a withdrawal reflex. Responses evoked by the mechanical stimulus and by the restricted set of heat stimuli did not differ significantly between light (withdrawal response) and deep (no withdrawal response) anesthesia (Table 1). Therefore, responses of RVM neurons evoked by capsaicin and mechanical stimuli obtained under the different anesthetic conditions were combined, and we analyzed the responses of our entire population of RVM to these stimuli. Responses to heat obtained in the presence of a withdrawal response were not included in our analysis of heat responses of all RVM neurons since only 45°C and 51°C were used under this condition. However, responses to these stimuli did not differ between anesthetic conditions (see Table 1; 51°C before capsaicin and 45°C before and after capsaicin).
Table 1.
Comparison of response properties of RVM neurons during light and deep anesthesia
| ON | OFF | NEUTRAL | |
|---|---|---|---|
| Ongoing discharge | L 1.8 ± 0.6 Hz | L 14.0 ± 5.0 Hz | L 11.5 ± 2.9 Hz |
| D 1.2 ± 0.6 Hz | D 11.4 ± 2.2 Hz | D 17.5 ± 3.1 Hz | |
| Response to 51°C | L 59.1 ± 19.0 spikes | L −22.8 ± 4.7 spikes | L NR |
| D 93.9 ± 20.7 spikes | D −35.8 ± 8.8 spikes | D NR | |
| Peak response to capsaicin | L 13.6 ± 3.6 Hz | L 5.1 ± 2.5 Hz | L NR |
| D 19.6 ± 4.3 Hz | D 3.0 ± 1.0 Hz | D NR | |
| Response to 60 g VF before capsaicin | L 2.5 ± 1.7 spikes | L −4.4 ± 3.2 spikes | L NR |
| D 2.7 ± 6.8 spikes | D −1.7 ± 1.1 spikes | D NR | |
| Response to 60 g VF 15 min after capsaicin | L 26.6 ± 7.1 spikes | L −25.1 ± 5.8 spikes | L NR |
| D 33.8 ± 8.0 spikes | D −27.1 ± 8.2 spikes | D NR | |
| Response to 45°C before capsaicin | L 5.2 ± 4.4 spikes | L −1.9 ± 2.4 spikes | L NR |
| D 1.3 ± 1.3 spikes | D −1.1 ± 1.1 spikes | D NR | |
| Response to 45°C 15 min after capsaicin | L 44.2 ± 10.6 spikes | L −30.9 ± 8.5 spikes | L NR |
| D 55.7 ± 15.9 spikes | D −37.7 ± 10.5 spikes | D NR |
Values are means ± SE. Ongoing discharge is level of spontaneous activity soon after cell was classified. RVM, rostral ventromedial medulla; L, light anesthesia; D, deep anesthesia; VF, von Frey monofilament; NR, no response.
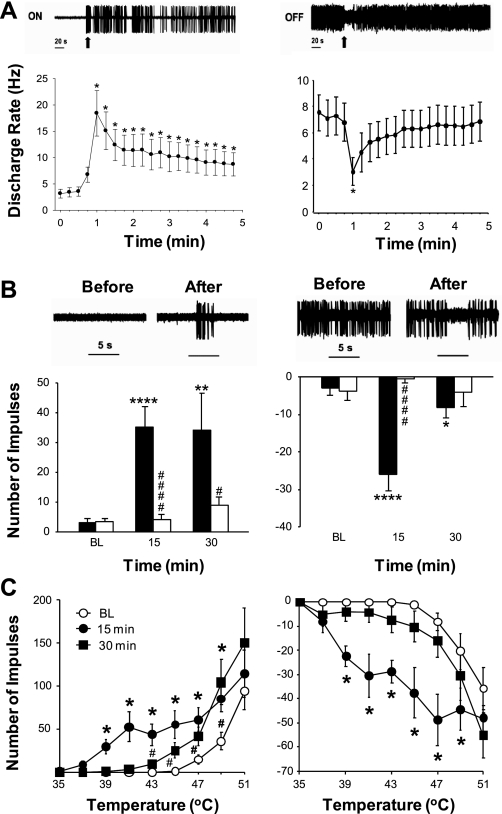
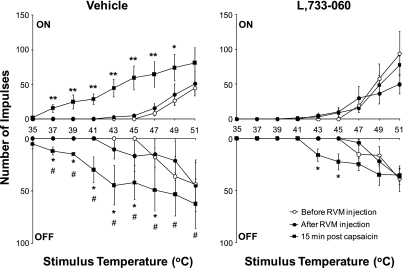
Intraplantar injection of capsaicin into one hind paw increased the ongoing discharge rates of ON cells and decreased the ongoing discharge rates of OFF cells (Fig. 2A), while the discharge rates of NEUTRAL cells did not change (data not shown). For both ON and OFF cells, the peak discharge typically occurred within the first 15 s after injection of capsaicin. Mean discharge rates for ON cells increased from 4.6 ± 1.5 Hz for the 45-s period before to 18.4 ± 4.3 Hz for the 15-s period immediately after capsaicin injection (P < 0.001). The mean discharge rates for OFF cells decreased from 7.3 ± 0.8 Hz before capsaicin to 3.0 ± 1.0 Hz for the 15-s period immediately after injection of capsaicin (P < 0.001). The durations of the responses to capsaicin differed between ON and OFF cells. Discharge rates of ON cells remained elevated for at least 4 min after capsaicin injection, whereas discharge of OFF cells returned to baseline levels within 1 min after injection.
Fig. 2.
Enhanced responses of ON (left) and OFF (right) cells before and after intraplantar injection of capsaicin. A, top: examples of responses of single ON (left) and OFF (right) cells to intraplantar injection of capsaicin. Each example shows discharge for 5 min, including 60 s before injection. Arrows indicate time of capsaicin injection. Bottom: mean (±SE) discharge rates for ON (left) and OFF (right) cells before and after capsaicin. The injection was given at the 1 min time point. *Significant difference from the mean discharge rate for 60 s prior to injection (P < 0.001 for ON cells; P < 0.05 for OFF cells). B: responses evoked by the von Frey monofilament (60 g) before and after capsaicin. Top: responses of individual ON (left) and OFF (right) cells before and at 15 min after capsaicin. The monofilament was applied for 5 s at the time indicated by the horizontal bar. Bottom: mean (±SE) number of impulses evoked by the monofilament before (BL) and at 15 and 30 min after capsaicin for all ON and OFF cells. Responses evoked by stimulation of the ipsilateral paw are shown by the filled bars, and responses evoked by stimulation of the contralateral paw are shown by the open bars. Significant difference from BL: *P < 0.05, **P < 0.005, ****P < 0.001. Significant difference from the contralateral paw: #P < 0.05, ####P < 0.001. C: mean (±SE) numbers of impulses evoked by heat stimuli of 35–51°C before (BL) and at 15 and 30 min after capsaicin for all ON and OFF cells. Significant difference from BL: *P < 0.01 at 15 min after capsaicin injection, #P < 0.01 at 30 min after capsaicin injection.
NEUTRAL cells did not exhibit any changes in ongoing discharge rates after capsaicin injection. The mean ongoing activity of NEUTRAL cells was 11.8 ± 2.2 Hz before and 13.4 ± 2.6 Hz during the first 15 s after capsaicin injection. In addition, NEUTRAL cells never became responsive to mechanical or heat stimuli either after intraplantar injection of capsaicin or after injection of vehicle or L-733,060 into the RVM. Therefore, NEUTRAL cells are not discussed further in detail.
None of the ON or OFF cells responded to the 60 g von Frey monofilament applied to the hind paw before injection of capsaicin, and this mechanical stimulus did not evoke a withdrawal reflex in lightly anesthetized rats. However, 15 min after injection of capsaicin, ON and OFF cells exhibited responses to this von Frey monofilament (Fig. 2B). Responses of ON cells increased from 3.0 ± 1.3 impulses before to 35.1 ± 6.8 impulses at 15 min after capsaicin injection (P < 0.001), while responses of OFF cells decreased from −3.1 ± 1.7 impulses before capsaicin injection to −26.0 ± 4.5 impulses after (P < 0.02). Responses of ON cells remained elevated for at least 60 min (data not shown), whereas responses of OFF cells returned to baseline values by 30 min after capsaicin. Importantly, the increase in evoked activity of both ON and OFF cells after injection of capsaicin occurred only in response to stimuli applied to the ipsilateral (capsaicin injected) paw, as responses evoked by the 60 g von Frey filament to the contralateral paw were not different from baseline values (Fig. 2B).
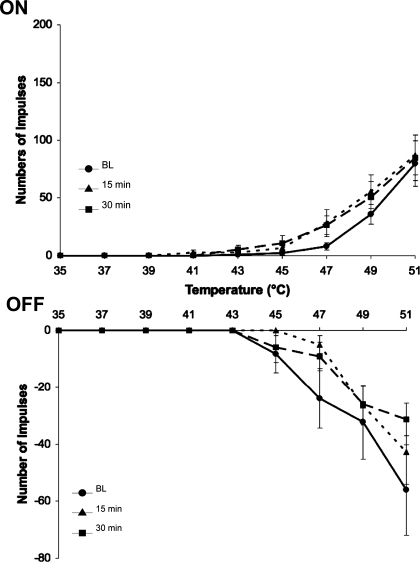
Injection of capsaicin also increased the responses of ON and OFF cells evoked by heat stimuli (Fig. 2C). Prior to capsaicin ON cells were excited, and OFF cells were inhibited, by heat stimuli of 47°C, 49°C, and 51°C, and these excitatory and inhibitory responses increased as a function of stimulus intensity. At 15 min after injection of capsaicin, mean heat response thresholds of ON cells decreased from 48.8 ± 0.4°C to 38.8 ± 0.4°C (P < 0.001). Similarly, the mean response threshold for OFF cells decreased from 48.6 ± 0.7°C to 38.3 ± 0.3°C at 15 min after capsaicin injection (P < 0.005). In addition to a decrease in response threshold, ON and OFF cells exhibited enhanced responses to suprathreshold stimuli after injection of capsaicin (Fig. 2C). Importantly, injection of capsaicin did not alter responses of ON or OFF cells evoked by heat stimuli applied to the contralateral paw (Fig. 3). There were no changes in response thresholds, and responses evoked by suprathreshold heat stimuli remained unchanged at 15 and 30 min after capsaicin injection.
Fig. 3.
Responses of rostral ventromedial medulla (RVM) neurons to heat stimuli applied to the paw contralateral to the capsaicin injection. Response threshold and response evoked by heat stimuli applied to the noninjected paw remained unchanged for ON (top) and OFF (bottom) cells at 15 and 30 min after intraplantar injection of capsaicin.
These data demonstrate that intraplantar injection of capsaicin increased ongoing activity of ON cells, caused a brief inhibition of ongoing activity of OFF cells, and increased responses of ON and OFF cells evoked by mechanical and heat stimuli.
Modulation of Evoked Responses of RVM Neurons by NK-1 Receptors
The same protocol as described in the experiment above was used with the addition of microinjection of either vehicle or the NK-1 receptor antagonist L-733,060 into the RVM 30 min before the capsaicin injection. Of the 47 neurons studied for these experiments, 22 (47%) were classified as ON cells (vehicle n = 10; L-733,060 n = 12), 10 (21%) were OFF cells (vehicle n = 4; L-733,060 n = 6), and 15 (32%) were NEUTRAL cells (vehicle n = 7; L-733,060 n = 8).
Responses evoked by capsaicin.
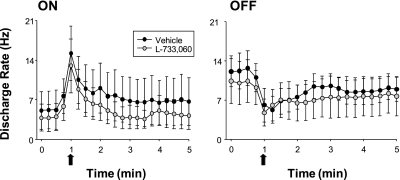
As shown in Fig. 4, the magnitude and duration of responses of ON and OFF cells evoked by intraplantar injection of capsaicin were similar after pretreatment with vehicle or L-733,060 into the RVM. Eleven of 12 ON cells tested with the NK-1 receptor antagonist were excited by the injection of capsaicin (compared to 9 of 10 in saline controls), while all 9 OFF cells (vehicle n = 4; L-733,060 n = 5) exhibited similar inhibition of ongoing activity after the capsaicin injection. Discharge rates of ON cells after capsaicin injection increased from 6.6 ± 3.1 to 15.2 ± 4.8 Hz at 15 s after injection for the vehicle-treated group and from 5.9 ± 2.6 to 13.1 ± 4.5 Hz for the group treated with L-733,060. Discharge rates of OFF cells decreased after injection of capsaicin from 11.0 ± 2.5 to 6.1 ± 3.0 Hz at 15 s after injection for the vehicle-treated group and from 9.2 ± 3.8 to 4.7 ± 2.4 Hz for the L-733,060-treated group. Thus capsaicin-evoked responses of ON and OFF cells were not altered by the NK-1 receptor antagonist.
Fig. 4.
Effects of vehicle or L-733,060 injected into the RVM on responses of ON (left) and OFF (right) cells evoked by intraplantar injection of 10 μg of capsaicin: mean (±SE) ongoing discharge rates (Hz) for 60 s before and for 4 min after capsaicin (bin width is 15 s). Arrows indicate time of capsaicin injection. Responses of ON and OFF cells to capsaicin were not altered by the NK-1 receptor antagonist L-733,060.
Responses evoked by mechanical stimuli.
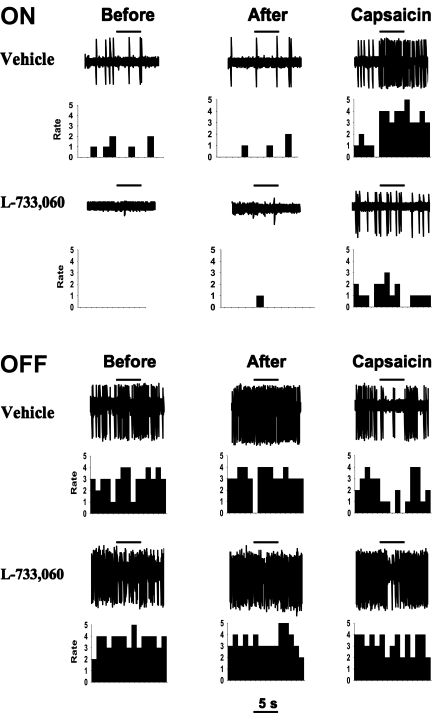
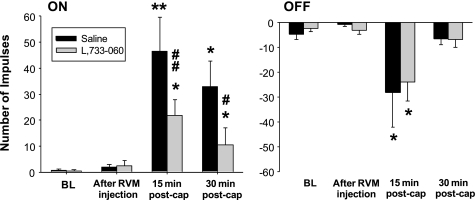
Prior to any injection none of the ON or OFF cells exhibited consistent responses to the 60 g von Frey monofilament, and this was not altered after injection of vehicle or L-733,060 into the RVM. The increases in responses of ON and OFF cells after intraplantar injection of capsaicin were attenuated by pretreatment with L-733,060, but not vehicle, into the RVM. This is shown for individual ON and OFF cells in Fig. 5.
Fig. 5.
Examples of responses of 2 individual ON (top) and OFF (bottom) cells to mechanical stimulation of the hind paw before any injection (Before), after injection of vehicle or L-733,060 into the RVM (After), and 15 min after injection of capsaicin (Capsaicin). Evoked responses of the ON and OFF cells were not altered after injection of vehicle or L-733,060 into the RVM, but the enhanced responses after injection of capsaicin were attenuated by L-733,060. Horizontal lines indicate times of mechanical stimulation (60 g von Frey monofilament), which was delivered to the capsaicin-injected paw.
Before capsaicin (and after injection of vehicle or L-733,060 into the RVM), mean responses of all ON cells evoked by mechanical stimulation were similar for the vehicle- and L-733,060-treated groups. As shown in Fig. 6, pretreatment with L-733,060 attenuated the increase in responses of ON cells at 15 min after injection of capsaicin. After pretreatment with vehicle, responses of ON cells increased from 1.9 ± 1.0 impulses before capsaicin injection to 46.4 ± 13.2 impulses at 15 min after, whereas the increase in responses of ON cells following pretreatment with L-733,060 was less (2.5 ± 2.0 impulses before to 21.8 ± 6.2 impulses at 15 min after capsaicin injection; P < 0.05). The enhanced responses of ON cells persisted for at least 30 min but were lower in the group pretreated with L-733,060.
Fig. 6.
Effects of vehicle or L-733,060 injected into the RVM on responses of all RVM neurons evoked by mechanical stimulation (60 g von Frey monofilament): mean (±SE) number of impulses evoked by mechanical stimulation for ON (left) and OFF (right) cells before any injection (BL), at 15 min after injection of vehicle (saline) or L-733,060 into the RVM, and at 15 and 30 min after intraplantar injection of capsaicin. Significant difference from baseline: *P < 0.05, **P < 0.005. Significant difference from the vehicle-treated group: #P < 0.05, ##P < 0.01. Pretreatment of the RVM with vehicle or L-733,060 alone had no effect on mechanically evoked responses of ON and OFF cells, and L-733,060 attenuated the enhanced responses of ON cells but not OFF cells.
Unlike ON cells, pretreatment with L-733,060 did not alter the enhanced inhibitory responses of OFF cells to mechanical stimuli after capsaicin. At 15 min after capsaicin, responses of OFF cells treated with L-733,060 (−23.9 ± 7.7 impulses) did not differ from those after pretreatment with vehicle (−28.3 ± 13.8 impulses) (Fig. 6). Responses of OFF cells returned to baseline values by 30 min after capsaicin in both treatment groups.
Responses of ON and OFF cells evoked by mechanical stimulation of the contralateral control paw were not altered after capsaicin or after any injection into the RVM.
Responses evoked by heat stimuli.
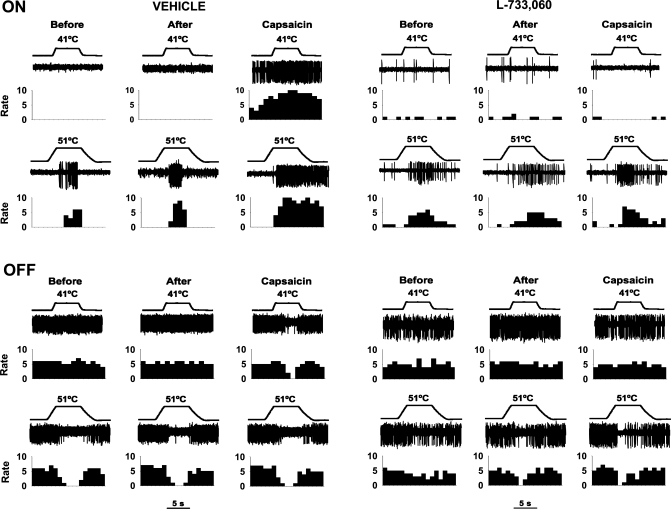
Prior to any injection, ON and OFF cells were responsive to heat stimuli of 47°C or greater, and responses were not changed after injection of vehicle or L-733,060 into the RVM. The increased responses of ON and OFF cells to heat stimuli after capsaicin were blocked by the NK-1 antagonist, and this is illustrated for individual ON and OFF cells in Fig. 7. After pretreatment with vehicle, ON cells exhibited a lower heat response threshold (from 48.5 ± 0.5°C to 38.0 ± 0.7°C; P < 0.05) at 15 min after capsaicin and large increases in evoked responses to heat stimuli. In contrast, after pretreatment with L-733,060 response thresholds of ON cells were unchanged after capsaicin (48.7 ± 0.5°C before and 47.3 ± 0.5°C at 15 min after capsaicin) and responses to suprathreshold stimuli were not increased (Fig. 8). Thus injection of L-733,060 into the RVM abolished the sensitization of ON cells to heat that is normally observed after intraplantar injection of capsaicin.
Fig. 7.
Examples of responses of 2 individual ON (top) and OFF (bottom) cells evoked by heat stimuli of 41°C and 51°C delivered to the hind paw before any injection (Before), after injection of vehicle (left) or L-733,060 (right) into the RVM (After), and after injection of capsaicin (Capsaicin). Injection of vehicle into the RVM (left) did not alter responses of these ON or OFF cells to heat, and responses were increased after injection of capsaicin. Injection of L-733,060 into the RVM (right) also did not alter responses of ON and OFF cells to heat but decreased the enhanced responses to heat produced by injection of capsaicin.
Fig. 8.
Effects of vehicle and L-7733,060 injected into the RVM on responses of all RVM neurons evoked by heat stimuli. Mean (±SE) number of impulses of ON (top) and OFF (bottom) cells before RVM injection, 15 min after injection of vehicle (left) or L-737,060 (right) into the RVM, and at 15 min after intraplantar injection of capsaicin. L-733,060 alone did not alter responses of ON or OFF cells to heat and blocked or attenuated the capsaicin-induced increases in responses of ON and OFF cells, respectively. Significant difference from baseline (before RVM injection): *P < 0.05, **P < 0.005. Significant difference in responses of OFF cells after capsaicin following pretreatment with vehicle or L-733,060: #P < 0.05.
The increase in the inhibitory responses of OFF cells evoked by heat stimuli after capsaicin was partially attenuated by pretreatment with L-733,060 (Fig. 8). After pretreatment with vehicle heat response thresholds decreased from 48.5 ± 1.2°C to 37.5 ± 0.6°C at 15 min after capsaicin, whereas thresholds decreased from 49.0 ± 0.5°C to 43.0 ± 1.0°C at 15 min after capsaicin in rats pretreated with L-733,060 (P < 0.05). Also, the increase in the inhibitory responses evoked by suprathreshold stimuli after capsaicin was attenuated after pretreatment with L-733,060 compared with vehicle pretreatment (2-way ANOVA with repeated measures, P < 0.05).
In addition to attenuating enhanced responses of ON and OFF cells to heat produced by capsaicin, L-733,060 produced a rightward shift in the cumulative percentage of ON and OFF cells that were responsive to lower heat stimulus temperatures after capsaicin. For example, at 15 min after capsaicin, ∼85% of ON cells were excited by 39°C in the vehicle-treated group, while none of the ON cells were excited by this temperature in the L-733,060-treated group. Similar results were found for OFF cells. For example, at 15 min after intraplantar injection of capsaicin, each of the OFF cells from vehicle-treated rats exhibited an inhibition in ongoing activity during application of 39°C, while none of the OFF cells was inhibited by 39°C in animals pretreated with L-733,060. Importantly, injection of vehicle or L-733,060 alone did not alter the percentage of ON and OFF cells that were responsive to heat.
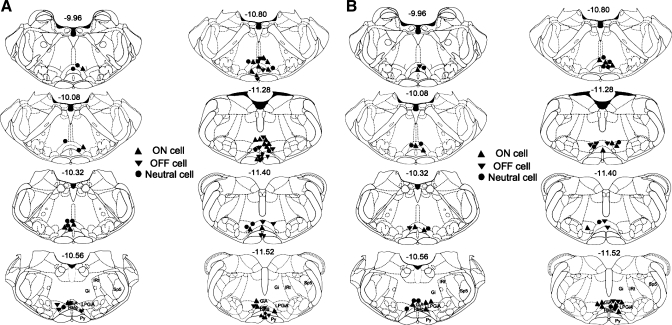
Location of Recording Sites in the RVM
Anatomical reconstructions of recording sites in the RVM are shown in Fig. 9. The locations of recording sites for ON, OFF, and NEUTRAL cells (n = 66) obtained in naive rats (Fig. 9A) were similar to those obtained in the combined recording and microinjection studies (n = 47) (Fig. 9B). Recording sites were distributed from the level of the trapezoid body to that of the inferior olive. There was no obvious pattern of distribution for functional cell types and no differences in distribution between the treatment groups.
Fig. 9.
Location of recording sites in the RVM. A: recording sites for ON, OFF, and NEUTRAL cells from RVM in both light (gray symbols) and deep (black symbols) anesthesia. B: recording sites from RVM cells for combined injection and recording experiments. The rostro-caudal coordinates are relative to bregma, and for B the microinjection pipette is not shown but is located ≤300 μm away. In some cases, the location of a cell has been shifted ≤100 μm for clarity. RMg, nucleus raphe magnus; Gi, nucleus gigantocellularis; GiA, nucleus gigantocellularis pars α; IRt, intermediate reticular nucleus; LPGiA, lateral paragigantocellularis nucleus pars α; Py, pyramidal tract; Sp5, spinal trigeminal tract. Images are adapted from Paxinos and Watson (2005). Copyright Elsevier.
DISCUSSION
The present study examined modulation of capsaicin-evoked changes in response properties of ON, OFF, and NEUTRAL cells in the RVM by NK-1 receptors. Capsaicin produced a long-lasting excitation of ON cells and a short-lasting inhibition of the ongoing activity of OFF cells and enhanced the excitatory responses for ON cells and the inhibitory responses for OFF cells evoked by mechanical and heat stimuli. After capsaicin, responses of both ON and OFF cells were evoked by stimulus intensities that did not elicit responses before injection. These data demonstrate an increase in descending facilitatory output and a decrease in inhibitory output (ON and OFF cells, respectively) from the RVM after intraplantar injection of capsaicin. Importantly, NK-1 receptors play a role primarily in the increased responses of ON cells, as microinjection of the NK-1 receptor antagonist L-733,060 attenuated the enhanced responses of ON cells, with a lesser effect on OFF cells, after capsaicin. We believe that the effects of L-733,060 occurred through NK-1 receptors since we had shown earlier that excitation of ON cells by SP were blocked by L-733,060 (Budai et al. 2007). The present results support and extend our previous behavioral (Pacharinsak et al., 2008) and electrophysiological (Budai et al. 2007) studies indicating that NK-1 receptors in the RVM, presumably located on a subset of ON cells, play a major role in driving descending facilitation of nociceptive transmission.
Although all of the neurons examined in this study were initially classified functionally during the presence of a withdrawal response (EMG activity), the majority of our experiments were conducted in the absence of withdrawal responses. We were concerned about the potential effect of deep anesthesia on the functional classification of RVM neurons and changes in their evoked responses. It has been shown that high concentrations of isoflurane can blunt or eliminate responses of ON and OFF cells, making them appear to be NEUTRAL cells (Leung and Mason 1995). Furthermore, responses of ON and OFF cells were smaller in the absence of withdrawal responses regardless of isoflurane concentration (Jinks et al. 2004). Importantly, barbiturates produce a greater inhibition of spinal motoneurons than dorsal horn neurons, including ascending projection neurons (Paik et al. 1989; Soja et al. 2002). In our study, all cells were initially classified in the presence of a stimulus-evoked withdrawal response and, importantly, none of the neurons exhibited a change in their functional response characteristics after transition to deep anesthesia. Furthermore, the magnitudes and time courses of evoked responses did not differ from those obtained in the presence of a withdrawal response. Thus the anesthesia used in our studies was at a level that eliminated motor responses but preserved responses of RVM neurons. Our studies are consistent with previous electrophysiological studies of RVM neurons under deep anesthesia with barbiturates or urethane (Hernandez and Vanegas 2001; Jiang and Behbehani 2001; Sanoja et al. 2010).
Relation Between Cellular Activity in the RVM and Capsaicin-Evoked Hyperalgesia
Our results show that the time course of changes in response properties of RVM neurons correlates well with behavioral measures of hyperalgesia produced by intraplantar injection of capsaicin (Pacharinsak et al. 2008). Although capsaicin enhanced the responses of RVM neurons to both mechanical and heat stimuli, there were differences in their respective time courses. In both rats and humans, the duration of mechanical hyperalgesia following injection of capsaicin into the skin outlasts the hyperalgesia to heat (Gilchrist et al. 1996; LaMotte et al. 1991; Pacharinsak et al. 2008; Simone et al. 1987, 1989). Similarly, the enhanced responses of ON cells to heat lasted <30 min, whereas the increase in responses to mechanical stimulation persisted throughout the 60-min testing period (data not shown). In contrast, responses of OFF cells evoked by both mechanical and heat stimuli returned to baseline values within 30 min after capsaicin. These results suggest that enhanced responses of both ON and OFF cells to heat may contribute to heat hyperalgesia after capsaicin, whereas activity of ON cells alone may contribute to the long duration of mechanical hyperalgesia.
Our results support the notion that an increase in the net output from ON cells is pronociceptive and contributes to hyperalgesia through descending modulation of nociceptive transmission in the spinal cord. The net output of RVM neurons on dorsal horn neuronal activity under normal conditions and after nerve injury has been shown to be facilitatory since application of local anesthetic to the RVM decreased evoked responses of nociceptive neurons in the spinal cord (Bee and Dickenson 2007). Moreover, spontaneous and evoked activity of ON cells was increased and inhibition of OFF cells was enhanced after topical application of mustard oil (Kincaid et al. 2006; Xu et al. 2007), inflammation produced by complete Freund's adjuvant (Miki et al. 2002), and nerve injury (Carlson et al. 2007; Goncalves et al. 2007). In those studies, models of persistent hyperalgesia were used and changes in neuronal responses of RVM neurons could be due to changes in gene expression. For example, persistent inflammation has been shown to upregulate NMDA receptors in the RVM (Miki et al. 2002). It is unknown whether the enhanced responses of RVM neurons after capsaicin injection are due to changes in gene expression, particularly since changes in excitability of RVM neurons are observed nearly immediately after capsaicin.
Mechanisms Underlying Increased Output of ON Cells
The mechanisms underlying the enhanced excitation and inhibition of ON and OFF cells in the RVM, respectively, remain unclear. One possibility is that changes in response properties of RVM neurons purely reflect an increase in nociceptive inputs following injection of capsaicin. It is known that intradermal injection of capsaicin produces sensitization of nociceptive spinal neurons whereby their responses evoked by mechanical and heat stimuli are increased (Khasabov et al. 2002; Simone et al. 1991; see review by Cervero 2009). Moreover, evoked responses of RVM neurons after capsaicin were only increased by stimulation of the injected paw. This is consistent with behavioral studies showing that mechanical hyperalgesia occurred only in the paw injected with capsaicin (Gilchrist et al. 1996). Responses of ON and OFF cells to stimuli applied to the contralateral paw were not altered, supporting the notion that the enhanced responses of RVM neurons reflect an increase in ascending nociceptive input. A similar relation between enhanced responsiveness after injury and the area of skin stimulated has been observed after mustard oil (Kincaid et al. 2006) and nerve injury (Carlson et al. 2007).
However, in addition to an increase in nociceptive input, neurons in the RVM might also become sensitized. Earlier studies demonstrated cellular changes in the RVM following persistent inflammation (Guan et al. 2002, 2003, 2004; Guo et al. 2006; Imbe et al. 2005, 2007). We have shown that after intraplantar injection of capsaicin ON cells, but not OFF cells, exhibited greater responses to iontophoretic application of NMDA (Budai et al. 2007). This was likely due to activation of NMDA receptors located on ON cells, suggesting that, in addition to an increase in nociceptive input to the RVM, ON cells may also develop an increase in excitability.
Our earlier studies suggested that ON cells, but not OFF cells, expressed NK-1 receptors, since iontophoretic application of SP excited ON cells but had no effect on OFF cells (Budai et al. 2007). However, the enhanced inhibitory response of OFF cells after capsaicin was partially reduced by the NK-1 receptor antagonist, suggesting a functional interaction between ON and OFF cells through a NK-1 receptor-dependent mechanism. Also, blocking NK-1 receptors partially reversed the capsaicin-enhanced inhibitory responses of OFF cells to heat, but not to mechanical stimuli, as shown in recent studies (Hamity et al. 2010; Lagraize et al. 2010). These results further support the notion that the expression and functions of NK-1 receptors related to ON and OFF cells differ.
Importantly, injection of L-733,060 alone did not alter responses of RVM neurons to mechanical or heat stimuli. This is consistent with our behavioral studies (Pacharinsak et al. 2008) and others (Hamity et al. 2010; Lagraize et al. 2010) showing that withdrawal responses were not altered after administration of L-733,060 into the RVM. These results indicate that SP and NK-1 receptors do not exert ongoing modulation of RVM neurons but rather are primarily involved in enhancing the responses of RVM neurons after injury.
Neurotransmitters Involved in Descending Facilitation
A wide variety of neurotransmitter systems participate in descending facilitation of nociceptive transmission from the RVM. Administration of neurotensin (Neubert et al. 2004), cholecystokinin (CCK) (Kovelowski et al. 2000), and brain-derived neurotrophic factor (Guo et al. 2006) into the RVM produced mechanical and/or heat hyperalgesia. Moreover, administration of neurotensin (Neubert et al. 2004) or CCK (Heinricher and Neubert 2004) into the RVM excited ON cells, and CCK microinjected into RVM reduced chronic opioid-induced hyperalgesia (Xie et al. 2005). In addition, glial activation within the RVM and their neuronal interactions may also contribute to persistent pain (Roberts et al. 2009; Wei et al. 2008).
SP has also been implicated previously in descending facilitation of nociceptive transmission. SP and NK-1 receptors have been identified in the RVM (Budai et al. 2007; Marson and Loewy 1985; Saffroy et al. 1988, 2003), and nearly half of the NK-1-expressing neurons from RVM project to the dorsal horn of the spinal cord (Pinto et al. 2008). Dickenson and colleagues originally proposed a pathway through which excitation of NK-1-expressing neurons in the superficial spinal dorsal horn leads to descending facilitation (Suzuki et al. 2002) via serotonin and 5-HT3 receptors in the spinal cord (Suzuki et al. 2004a, 2004b; see also Lagraize et al. 2010). Indeed, the majority of spinal dorsal horn neurons that express NK-1 receptors send projections to supraspinal structures (Todd et al. 2002) and are necessary for encoding of intense noxious stimuli (Suzuki et al. 2003) and for the development of hyperalgesia (Mantyh et al. 1997; Nichols et al. 1999) and central sensitization (Khasabov et al. 2002, 2005; Suzuki et al. 2002).
Conclusions
Results of the present studies demonstrate that responses of ON and OFF cells in the RVM are enhanced after intraplantar injection of capsaicin, and this occurs, at least in part, through activation of NK-1 receptors. Capsaicin-evoked excitation and sensitization of ON cells, and to a lesser extent the enhanced inhibitory responses of OFF cells, correlated well with nocifensive behavior and hyperalgesia observed in earlier behavioral studies (Gilchrist et al. 1996; Pacharinsak et al. 2008). Additional studies are needed to determine the effects of NK-1 receptor activation in the RVM on response properties of nociceptive neurons in the spinal cord. Identification of the neurochemical mechanisms in the RVM and in the spinal cord that drive descending facilitation of nociceptive transmission may lead to novel approaches for pain management.
GRANTS
This work was supported by National Institutes of Health Grants DA-011471 and CA-091007 (D. A. Simone) and DA-023576 (D. L. Hammond) and University of Minnesota Faculty Grant-in-Aid 21169 (S. G. Khasabov). T. S. Brink was supported by the National Institute of Dental and Craniofacial Research (T32-DE-007288).
DISCLOSURES
No conflicts of interest, financial or otherwise, are declared by the author(s).
AUTHOR CONTRIBUTIONS
Author contributions: T.S.B., C.P., and D.A.S. conception and design of research; T.S.B., C.P., S.G.K., and D.A.S. performed experiments; T.S.B., C.P., and S.G.K. analyzed data; T.S.B., C.P., S.G.K., A.J.B., and D.A.S. interpreted results of experiments; T.S.B. and C.P. prepared figures; T.S.B., C.P., S.G.K., A.J.B., and D.A.S. edited and revised manuscript; C.P. drafted manuscript; S.G.K., A.J.B., and D.A.S. approved final version of manuscript.
ACKNOWLEDGMENTS
The authors thank Dr. Mary M. Heinricher for sharing technical expertise and for providing technical training for the combined recording and injecting approach and Drs. Donna L. Hammond and Glenn Giesler for comments on an early version of the manuscript. We also thank Keta Desai for technical assistance during these experiments.
Present addresses: T. S. Brink, Neuromodulation Research, Medtronic Inc., 7000 Central Ave. NE, Minneapolis MN 55432; C. Pacharinsak, Dept. of Comparative Medicine, Stanford University School of Medicine, Stanford, CA 94305.
REFERENCES
- Bederson JB, Fields HL, Barbaro NM. Hyperalgesia during naloxone-precipitated withdrawal from morphine is associated with increased on-cell activity in the rostral ventromedial medulla. Somatosens Mot Res 7: 185–203, 1990 [DOI] [PubMed] [Google Scholar]
- Bee LA, Dickenson AH. Rostral ventromedial medulla control of spinal sensory processing in normal and pathophysiological states. Neuroscience 147: 786–793, 2007 [DOI] [PubMed] [Google Scholar]
- Brink TS, Hellman KM, Lambert AM, Mason P. Raphe magnus neurons help protect reactions to visceral pain from interruption by cutaneous pain. J Neurophysiol 96: 3423–3432, 2006 [DOI] [PubMed] [Google Scholar]
- Brink TS, Mason P. Raphe magnus neurons respond to noxious colorectal distension. J Neurophysiol 89: 2506–2515, 2003 [DOI] [PubMed] [Google Scholar]
- Budai D, Khasabov SG, Mantyh PW, Simone DA. NK-1 receptors modulate the excitability of ON cells in the rostral ventromedial medulla. J Neurophysiol 97: 1388–1395, 2007 [DOI] [PubMed] [Google Scholar]
- Burgess SE, Gardell LR, Ossipov MH, Malan TP, Jr, Vanderah TW, Lai J, Porreca F. Time-dependent descending facilitation from the rostral ventromedial medulla maintains, but does not initiate, neuropathic pain. J Neurosci 22: 5129–5136, 2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlson JD, Maire JJ, Martenson ME, Heinricher MM. Sensitization of pain-modulating neurons in the rostral ventromedial medulla after peripheral nerve injury. J Neurosci 27: 13222–13231, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cervero F. Spinal cord hyperexcitability and its role in pain and hyperalgesia. Exp Brain Res 196: 129–137, 2009 [DOI] [PubMed] [Google Scholar]
- Coutinho SV, Urban MO, Gebhart GF. Role of glutamate receptors and nitric oxide in the rostral ventromedial medulla in visceral hyperalgesia. Pain 78: 59–69, 1998 [DOI] [PubMed] [Google Scholar]
- Donovan-Rodriguez T, Urch CE, Dickenson AH. Evidence of a role for descending serotonergic facilitation in a rat model of cancer-induced bone pain. Neurosci Lett 393: 237–242, 2006 [DOI] [PubMed] [Google Scholar]
- Fields HL. Pain modulation: expectation, opioid analgesia and virtual pain. Prog Brain Res 122: 245–253, 2000 [DOI] [PubMed] [Google Scholar]
- Fields HL, Bry J, Hentall I, Zorman G. The activity of neurons in the rostral medulla of the rat during withdrawal from noxious heat. J Neurosci 3: 2545–2552, 1983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao K, Mason P. Serotonergic raphe magnus cells that respond to noxious tail heat are not ON or OFF cells. J Neurophysiol 84: 1719–1725, 2000 [DOI] [PubMed] [Google Scholar]
- Gilchrist HD, Allard BL, Simone DA. Enhanced withdrawal responses to heat and mechanical stimuli following intraplantar injection of capsaicin in rats. Pain 67: 179–188, 1996 [DOI] [PubMed] [Google Scholar]
- Goncalves L, Almeida A, Pertovaara A. Pronociceptive changes in response properties of rostroventromedial medullary neurons in a rat model of peripheral neuropathy. Eur J Neurosci 26: 2188–2195, 2007 [DOI] [PubMed] [Google Scholar]
- Guan Y, Guo W, Robbins MT, Dubner R, Ren K. Changes in AMPA receptor phosphorylation in the rostral ventromedial medulla after inflammatory hyperalgesia in rats. Neurosci Lett 366: 201–205, 2004 [DOI] [PubMed] [Google Scholar]
- Guan Y, Guo W, Zou SP, Dubner R, Ren K. Inflammation-induced upregulation of AMPA receptor subunit expression in brain stem pain modulatory circuitry. Pain 104: 401–413, 2003 [DOI] [PubMed] [Google Scholar]
- Guan Y, Terayama R, Dubner R, Ren K. Plasticity in excitatory amino acid receptor-mediated descending pain modulation after inflammation. J Pharmacol Exp Ther 300: 513–520, 2002 [DOI] [PubMed] [Google Scholar]
- Guo W, Robbins MT, Wei F, Zou S, Dubner R, Ren K. Supraspinal brain-derived neurotrophic factor signaling: a novel mechanism for descending pain facilitation. J Neurosci 26: 126–137, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamity MV, White SR, Hammond DL. Effects of neurokinin-1 receptor agonism and antagonism in the rostral ventromedial medulla of rats with acute or persistent inflammatory nociception. Neuroscience 165: 902–913, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heinricher MM, Neubert MJ. Neural basis for the hyperalgesic action of cholecystokinin in the rostral ventromedial medulla. J Neurophysiol 92: 1982–1989, 2004 [DOI] [PubMed] [Google Scholar]
- Heinricher MM, Tavares I, Leith JL, Lumb BM. Descending control of nociception: specificity, recruitment and plasticity. Brain Res Rev 60: 214–225, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hernandez N, Vanegas H. Encoding of noxious stimulus intensity by putative pain modulating neurons in the rostral ventromedial medulla and by simultaneously recorded nociceptive neurons in the spinal dorsal horn of rats. Pain 91: 307–315, 2001 [DOI] [PubMed] [Google Scholar]
- Hurley RW, Hammond DL. Contribution of endogenous enkephalins to the enhanced analgesic effects of supraspinal mu opioid receptor agonists after inflammatory injury. J Neurosci 21: 2536–2545, 2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imbe H, Okamoto K, Okamura T, Kumabe S, Nakatsuka M, Aikawa F, Iwai-Liao Y, Senba E. Effects of peripheral inflammation on activation of ERK in the rostral ventromedial medulla. Brain Res 1063: 151–158, 2005 [DOI] [PubMed] [Google Scholar]
- Imbe H, Okamoto K, Aikawa F, Kimura A, Donishi T, Tamai Y, Iwai-Liao Y, Senba E. Effects of peripheral inflammation on activation of p38 mitogen-activated protein kinase in the rostral ventromedial medulla. Brain Res 1134: 131–139, 2007 [DOI] [PubMed] [Google Scholar]
- Jiang M, Behbehani MM. Physiological characteristics of the projection pathway from the medial preoptic to the nucleus raphe magnus of the rat and its modulation by the periaqueductal gray. Pain 94: 139–147, 2001 [DOI] [PubMed] [Google Scholar]
- Jinks SL, Carstens E, Antognini JF. Isoflurane differentially modulates medullary on and off neurons while suppressing hind-limb motor withdrawals. Anesthesiology 100: 1224–1234, 2004 [DOI] [PubMed] [Google Scholar]
- Kaplan H, Fields HL. Hyperalgesia during acute opioid abstinence: evidence for a nociceptive facilitating function of the rostral ventromedial medulla. J Neurosci 11: 1433–1439, 1991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khasabov SG, Ghilardi JR, Mantyh PW, Simone DA. Spinal neurons that express NK-1 receptors modulate descending controls that project through the dorsolateral funiculus. J Neurophysiol 93: 998–1006, 2005 [DOI] [PubMed] [Google Scholar]
- Khasabov SG, Rogers SD, Ghilardi JR, Peters CM, Mantyh PW, Simone DA. Spinal neurons that possess the substance P receptor are required for the development of central sensitization. J Neurosci 22: 9086–9098, 2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kincaid W, Neubert MJ, Xu M, Kim CJ, Heinricher MM. Role for medullary pain facilitating neurons in secondary thermal hyperalgesia. J Neurophysiol 95: 33–41, 2006 [DOI] [PubMed] [Google Scholar]
- Kovelowski CJ, Ossipov MH, Sun H, Lai J, Malan TP, Porreca F. Supraspinal cholecystokinin may drive tonic descending facilitation mechanisms to maintain neuropathic pain in the rat. Pain 87: 265–273, 2000 [DOI] [PubMed] [Google Scholar]
- Lagraize SC, Guo W, Yang K, Wei F, Ren K, Dubner R. Spinal cord mechanisms mediating behavioral hyperalgesia induced by neurokinin-1 tachykinin receptor activation in the rostral ventromedial medulla. Neuroscience 171: 1341–1356, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaMotte RH, Shain CN, Simone DA, Tsai EF. Neurogenic hyperalgesia: psychophysical studies of underlying mechanisms. J Neurophysiol 66: 190–211, 1991 [DOI] [PubMed] [Google Scholar]
- Leung CG, Mason P. Effects of isoflurane concentration on the activity of pontomedullary raphe and medial reticular neurons in the rat. Brain Res 699: 71–82, 1995 [DOI] [PubMed] [Google Scholar]
- Li YW, Bayliss DA. Presynaptic inhibition by 5-HT1B receptors of glutamatergic synaptic inputs onto serotonergic caudal raphe neurones in rat. J Physiol 510: 121–134, 1998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mantyh PW, Rogers SD, Honore P, Allen BJ, Ghilardi JR, Li J, Daughters RS, Lappi DA, Wiley RG, Simone DA. Inhibition of hyperalgesia by ablation of lamina I spinal neurons expressing the substance P receptor. Science 278: 275–279, 1997 [DOI] [PubMed] [Google Scholar]
- Marson L, Loewy AD. Topographic organization of substance P and monoamine cells in the ventral medulla of the cat. J Auton Nerv Syst 14: 271–285, 1985 [DOI] [PubMed] [Google Scholar]
- Mason P. Contributions of the medullary raphe and ventromedial reticular region to pain modulation and other homeostatic functions. Annu Rev Neurosci 24: 737–777, 2001 [DOI] [PubMed] [Google Scholar]
- Mason P. Ventromedial medulla: pain modulation and beyond. J Comp Neurol 493: 2–8, 2005 [DOI] [PubMed] [Google Scholar]
- Mason P. Physiological identification of pontomedullary serotonergic neurons in the rat. J Neurophysiol 77: 1087–1098, 1997 [DOI] [PubMed] [Google Scholar]
- Meng ID, Harasawa I. Chronic morphine exposure increases the proportion of on-cells in the rostral ventromedial medulla in rats. Life Sci 80: 1915–1920, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miki K, Zhou QQ, Guo W, Guan Y, Terayama R, Dubner R, Ren K. Changes in gene expression and neuronal phenotype in brain stem pain modulatory circuitry after inflammation. J Neurophysiol 87: 750–760, 2002 [DOI] [PubMed] [Google Scholar]
- Mohrland JS, Gebhart GF. Effects of focal electrical stimulation and morphine microinjection in the periaqueductal gray of the rat mesencephalon on neuronal activity in the medullary reticular formation. Brain Res 201: 23–37, 1980 [DOI] [PubMed] [Google Scholar]
- Montagne-Clavel J, Oliveras JL. Are ventromedial medulla neuronal properties modified by chronic peripheral inflammation? A single-unit study in the awake, freely moving polyarthritic rat. Brain Res 657: 92–104, 1994 [DOI] [PubMed] [Google Scholar]
- Neubert MJ, Kincaid W, Heinricher MM. Nociceptive facilitating neurons in the rostral ventromedial medulla. Pain 110: 158–165, 2004 [DOI] [PubMed] [Google Scholar]
- Nichols ML, Allen BJ, Rogers SD, Ghilardi JR, Honore P, Luger NM, Finke MP, Li J, Lappi DA, Simone DA, Mantyh PW. Transmission of chronic nociception by spinal neurons expressing the substance P receptor. Science 286: 1558–1561, 1999 [DOI] [PubMed] [Google Scholar]
- Pacharinsak C, Khasabov SG, Beitz AJ, Simone DA. NK-1 receptors in the rostral ventromedial medulla contribute to hyperalgesia produced by intraplantar injection of capsaicin. Pain 139: 34–46, 2008 [DOI] [PubMed] [Google Scholar]
- Paik KS, Nam SC, Chung JM. Different classes of cat spinal neurons display differential sensitivity to sodium pentobarbital. J Neurosci Res 23: 107–115, 1989 [DOI] [PubMed] [Google Scholar]
- Paxinos G, Watson C. The Rat Brain in Stereotaxic Coordinates. Amsterdam: Elsevier Academic, 2005 [Google Scholar]
- Pertovaara A, Wei H, Hamalainen MM. Lidocaine in the rostroventromedial medulla and the periaqueductal gray attenuates allodynia in neuropathic rats. Neurosci Lett 218: 127–130, 1996 [DOI] [PubMed] [Google Scholar]
- Pinto M, Sousa M, Lima D, Tavares I. Participation of μ-opioid, GABAB, and NK1 receptors of major pain control medullary areas in pathways targeting the rat spinal cord: implications for descending modulation of nociceptive transmission. J Comp Neurol 510: 175–187, 2008 [DOI] [PubMed] [Google Scholar]
- Porreca F, Ossipov MH, Gebhart GF. Chronic pain and medullary descending facilitation. Trends Neurosci 25: 319–325, 2002 [DOI] [PubMed] [Google Scholar]
- Ren K, Dubner R. Enhanced descending modulation of nociception in rats with persistent hindpaw inflammation. J Neurophysiol 76: 3025–3037, 1996 [DOI] [PubMed] [Google Scholar]
- Roberts J, Ossipov MH, Porreca F. Glial activation in the rostral ventromedial medulla promotes descending facilitation to mediate inflammatory hpersensitivity. Eur J Neurosci 30: 229–241, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saffroy M, Beaujouan JC, Torrens Y, Besseyre J, Bergstrom L, Glowinski J. Localization of tachykinin binding sites (NK1, NK2, NK3 ligands) in the rat brain. Peptides 9: 227–241, 1988 [DOI] [PubMed] [Google Scholar]
- Saffroy M, Torrens Y, Glowinski J, Beaujouan JC. Autoradiographic distribution of tachykinin NK2 binding sites in the rat brain: comparison with NK1 and NK3 binding sites. Neuroscience 116: 761–773, 2003 [DOI] [PubMed] [Google Scholar]
- Sanoja R, Tortorici V, Fernandez C, Price TJ, Cervero F. Role of RVM neurons in capsaicin-evoked visceral nociception and referred hyperalgesia. Eur J Pain 14: 120.e121–120.e129, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simone DA, Baumann TK, LaMotte RH. Dose-dependent pain and mechanical hyperalgesia in humans after intradermal injection of capsaicin. Pain 38: 99–107, 1989 [DOI] [PubMed] [Google Scholar]
- Simone DA, Ngeow JY, Putterman GJ, LaMotte RH. Hyperalgesia to heat after intradermal injection of capsaicin. Brain Res 418: 201–203, 1987 [DOI] [PubMed] [Google Scholar]
- Simone DA, Sorkin LS, Oh U, Chung JM, Owens C, LaMotte RH, Willis WD. Neurogenic hyperalgesia: central neural correlates in responses of spinothalamic tract neurons. J Neurophysiol 66: 228–246, 1991 [DOI] [PubMed] [Google Scholar]
- Soja PJ, Taepavarapruk N, Pang W, Cairns BE, McErlane SA, Fragoso MC. Transmission through the dorsal spinocerebellar, and spinoreticular tracts: wakefulness versus thiopental anesthesia. Anesthesiology 97: 1178–1188, 2002 [DOI] [PubMed] [Google Scholar]
- Suzuki R, Hunt SP, Dickenson AH. The coding of noxious mechanical and thermal stimuli of deep dorsal horn neurones is attenuated in NK1 knockout mice. Neuropharmacology 45: 1093–1100, 2003 [DOI] [PubMed] [Google Scholar]
- Suzuki R, Morcuende S, Webber M, Hunt SP, Dickenson AH. Superficial NK1-expressing neurons control spinal excitability through activation of descending pathways. Nat Neurosci 5: 1319–1326, 2002 [DOI] [PubMed] [Google Scholar]
- Suzuki R, Rahman W, Hunt SP, Dickenson AH. Descending facilitatory control of mechanically evoked responses is enhanced in deep dorsal horn neurones following peripheral nerve injury. Brain Res 1019: 68–76, 2004a [DOI] [PubMed] [Google Scholar]
- Suzuki R, Rygh LJ, Dickenson AH. Bad news from the brain: descending 5-HT pathways that control spinal pain processing. Trends Pharmacol Sci 12: 613–617, 2004b [DOI] [PubMed] [Google Scholar]
- Todd AJ, Puskar Z, SPike RV, Hughes C, Watt C, Forrest L. Projection neurons in lamina I of rat spinal cord with the neurokinin 1 receptor are selectively innervated by substance P-containing afferents and respond to noxious stimulation. J Neurosci 22: 4103–4113, 2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vanderah TW, Suenaga NM, Ossipov MH, Malan TP, Jr, Lai J, Porreca F. Tonic descending facilitation from the rostral ventromedial medulla mediates opioid-induced abnormal pain and antinociceptive tolerance. J Neurosci 21: 279–286, 2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vanegas H, Schaible HG. Descending control of persistent pain: inhibitory or facilitatory? Brain Res Brain Res Rev 46: 295–309, 2004 [DOI] [PubMed] [Google Scholar]
- Watkins LR, Wiertelak EP, Goehler LE, Mooney-Heiberger K, Martinez J, Furness L, Smith KP, Maier SF. Neurocircuitry of illness-induced hyperalgesia. Brain Res 639: 283–299, 1994 [DOI] [PubMed] [Google Scholar]
- Wei F, Guo W, Zou S, Ren K, Dubner R. Supraspinal glial-neuronal interactions contribute to descending pain facilitation. J Neurosci 28: 10482–10495, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie JY, Herman DS, Stiller CO, Gardell LR, Ossipov MH, Lai J, Porreca F, Vanderah TW. Cholecystokinin in the rostral ventromedial medulla mediates opioid-induced hyperalgesia and antinociceptive tolerance. J Neurosci 25: 409–416, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu M, Kim CJ, Neubert MJ, Heinricher MM. NMDA receptor-mediated activation of medullary pro-nociceptive neurons is required for secondary thermal hyperalgesia. Pain 127: 253–262, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang L, Hammond DL. Substance P enhances excitatory synaptic transmission on spinally projecting neurons in the rostral ventromedial medulla after inflammatory injury. J Neurophysiol 102: 1139–1151, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhuo M, Sengupta JN, Gebhart GF. Biphasic modulation of spinal visceral nociceptive transmission from the rostroventral medial medulla in the rat. J Neurophysiol 87: 2225–2236, 2002 [DOI] [PubMed] [Google Scholar]