Abstract
Background:
Malaria constitutes a major health problem, with children and pregnant women being the most vulnerable to its morbidity and mortality.
Aim:
To determine the demographic factors associated with the use of insecticide-treated nets among children and pregnant women in Nigeria.
Materials and Methods:
The study was based on data drawn from the Nigeria Demographic and Health Survey 2008 on the use of insecticide-treated nets among women and children. The survey was conducted in 34070 households and a total of 10,724 women aged 15-49 years participated in the survey. Data were entered into Minitab version 15 and the chi-square test for independence was performed to show association between variables.
Results:
The results revealed that 49.8% of children and 44% of pregnant women present in households that owe insecticide-treated nets slept under them on the night before the survey. Sleeping under an insecticide-treated nets among children was associated with (P<0.05) the age of a child, geopolitical zone, and wealth quintile while the use of insecticide-treated nets among pregnant women was associated with the education level and wealth quintile of households.
Conclusion:
The study demonstrated that some demographic factors are associated with the use of ITNs among children and pregnant women in Nigeria.
Keywords: Children, Demographic factors, Insecticides-treated nets, Pregnant women
Introduction
Malaria constitutes a major health problem with about 300-500 million clinical cases and more than one million deaths annually. Children and pregnant women are the most vulnerable to malaria morbidity and mortality. Every 40 s, a child dies of malaria resulting in more than 2000 deaths per day among children worldwide.[1] Malaria affects maternal health and pregnancy outcome. It causes anemia in pregnancy which increases the risk of maternal deaths with an estimated 10,000 maternal deaths annually attributed to maternal anemia.[2,3] Malaria in pregnancy also causes low birth weight, preterm delivery, congenital infection, and reproductive loss.[2] Over 90% of malaria burden occurs in Sub-Saharan Africa.[4]
Malaria is endemic in Nigeria, with a prevalence of 919 per 100 000 population and remains one of the leading cause of morbidity and mortality. It accounts for 30% and 11% of child and maternal deaths, respectively.[5] The economic impact of malaria in Nigeria is enormous with about  132 billion lost annually.[6]
132 billion lost annually.[6]
Insecticide-treated nets (ITNs) have been shown to be the most cost effective measures in the prevention of malaria.[7,8] ITNs have been shown to reduce malaria mortality by 17% in children below the age of five.[8] In view of the effectiveness of ITNs, the Roll Back Malaria Partnership (RBM) targets to protect 80% of children and pregnant women at risk for malaria with ITNs by 2015.[9] Nigeria, has also established policy guidelines for the implementation and scaling-up use of ITNs in accordance with the provision of Abuja declaration and its national strategic plan.[5] The Malaria prevention programme in Nigeria was expected to provide about 60 million ITNs by the end of 2010.[10] Consistent use of these nets is important in the prevention of malaria.
Some demographic factors have been identified as important predictors of ITNs use including gender, wealth, access to health care, education, and ethnicity.[11] This study was aimed at determining the demographic factors associated with the use of ITNs among children and pregnant women in Nigeria.
Materials and Methods
Study design
The study was based on data drawn from the Nigeria Demographic and Health Survey (NDHS) 2008. In the survey, women aged 15-49 years from selected households were interviewed. The survey collected data on demography, ownership of an insecticide treated net, number of children who slept under an ITN on the night preceding the survey, and number of women age 15-49 (including women who were pregnant at the time of the survey) who slept under an ITN on the night preceding the survey.
The survey considered an ITN as a factory treated net not requiring any further treatment, or a pretreated net/net soaked with an insecticide within 12 months preceding the survey.
Study population
The survey was conducted in 34,070 households and a total of 10,724 women aged 15-49 years participated in the survey.
Sampling procedure
The respondents for the 2008 NDHS were obtained through a stratified two-stage cluster design. Nigeria is divided into states. Each state is subdivided into local government areas (LGAs), and each LGA is divided into localities.[12] The 2008 NDHS subdivided each locality into convenient areas called census Enumeration Areas (EAs) which constitutes the primary sampling unit referred to as a cluster. In the first stage, 886 clusters, consisting of 286 and 600 clusters from urban and rural areas respectively were selected from localities in each local government area of the country. The second stage involves selecting an average of 41 households per cluster.[12]
Data analysis
Data Analysis was performed in two stages. In the first stage, data drawn from the NDHS were entered into Minitab version 15 statistical software and the chi-square test was performed to show association between the use of ITNs and demographic variables. The second stage involved calculating unadjusted odd ratio (OR) and the respective 95% confidence interval (CI) to determine the strength of association.
Results
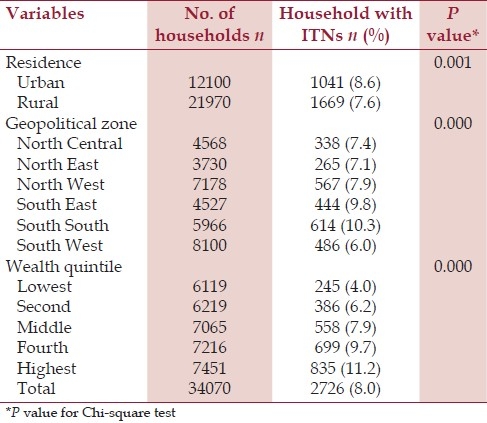
The 2008 NDHS showed that only 8.0% of Nigerian households were in possession of at least one ITN with an average of 0.1 ITN per household. Applying Chi-square test to the results in [Table 1] shows that the ownership of an ITN in Nigeria was associated (P<0.05) with place of residence, geopolitical zone and the wealth quintile of household. Urban households, households from the South East and South South geopolitical zones, and those of the highest wealth quintile possessed a significant (P<0.05) number of ITNs than their corresponding counterparts [Table 1].
Table 1.
Households in possession of at least one ITN
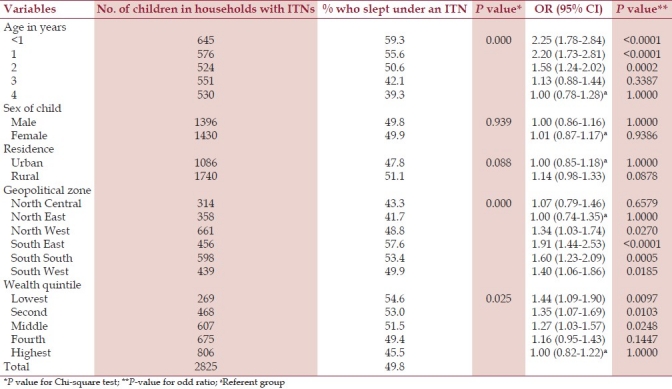
Only 49.8% of the children present in households that owe ITNs slept under an ITN on the night before the survey [Table 2]. Sleeping under an ITN was found to be associated with (P<0.05) the age of a child, geopolitical zone, and wealth quintile of households. The use of an ITN decreases with an increase in the age of a child and wealth quintile of households. Children below 1 year were two times more likely (OR 2.25) to sleep under an ITN than those of 4-year old and those belonging to families with the lowest wealth quintile were 1.4 times more likely to sleep under an ITN than those from the highest wealth quintile.
Table 2.
Children who slept under an ITN in households with ITNs
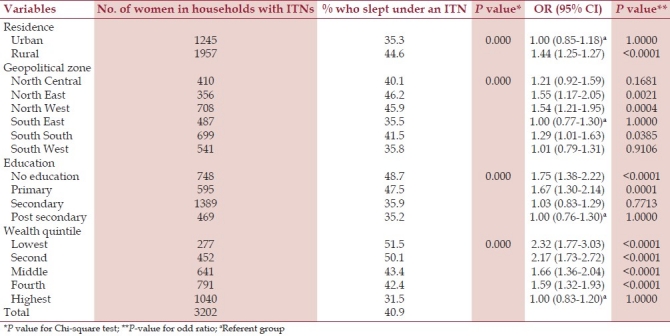
About 41% of women living in households having an ITN slept under an ITN the night before the survey. Sleeping under an ITN among Nigerian women was found to be associated with (P<0.05) place of residence, geopolitical zone, education, and wealth quintile of households [Table 3]. The use of ITNs decreases with increasing education level and wealth quintile. Women without formal education were 1.75 times more likely to sleep under an ITN than those with post secondary education, while those of the lowest wealth quintile were 2.32 times more likely to sleep under a net than those of the highest wealth quintile.
Table 3.
Women who slept under an ITN in households with ITNs
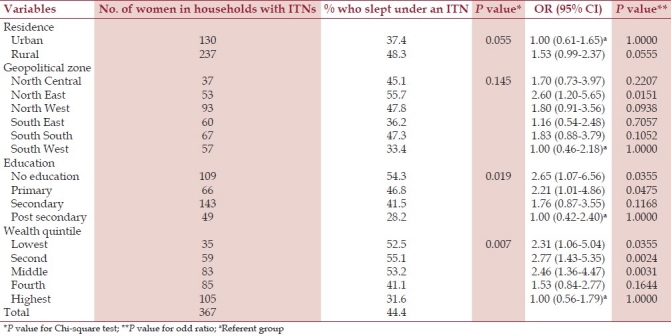
The survey revealed that 44% of pregnant women living in households with an ITN slept under it, a night before the survey. The use of ITNs among pregnant women was associated with the education level and wealth quintile. Those without a formal education (OR 2.65) and from the lowest wealth quintile (OR 2.31) were more likely to use an ITN than those with post secondary education and highest wealth quintile, respectively [Table 4].
Table 4.
Pregnant women who slept under an ITN in households with ITNs
Discussion
The study demonstrated that ITN coverage in Nigeria is low and its utilization among women and children is far from the Roll Back Malaria Partnership (RBM) targets to protect 80% of children and pregnant women at risk for malaria with ITNs by 2015. ITN coverage was very low in rural areas, south-west region and households with the lowest wealth quintile. This suggests that these population groups can be target groups for campaigns to increase coverage. Several strategies have been demonstrated to increase ITN coverage and use including integrated campaign during immunization and mass drug treatment. In Zambia, more than 80% coverage and use of ITN was observed when ITN distribution was integrated with immunization campaigns.[13] A study in central part of Nigeria also showed that widespread coverage of ITNs can be achieved through mass drug administration campaign.[14]
The results of this study showed that about 50% of children less than five years old did not sleep under an ITN the night preceding the survey. This result is similar to that found in other studies in Ethiopia (42%), Ghana (49.8%), and Uganda (46%).[4,9]
The results also revealed that children under the age of 1 (infants) were more likely to sleep under an ITN than their older ones; This findings is in agreement with other findings in sub-Saharan Africa and this shows that infants, especially the breastfeeding ones are likely to sleep under an ITN because they share a bed with their mothers.[3,9] In addition, Eisele et al.,[9] showed that as children grow older, they lose their access to ITN and suggest the need for increasing intra-household access of ITNs.
Although households from the highest wealth quintile have more ITNs in their possession, children from households with the lowest wealth quintile were more likely to sleep under an ITN than those from the highest wealth quintile. This result is in contrast to findings in Uganda where children in wealthy households were more likely to sleep under an ITN than those of poor households.[3] The high use ITNs in households with the lowest wealth quintile may be associated with their perceived vulnerability as perceived vulnerability to malaria have been shown to be higher in poor households.[3] In addition, the fact that a child from poor household is more likely to share a bed with his parent is a possible explanation for the high use of ITN among children in poor homes than those in wealthy homes.
Conclusion
The study therefore demonstrated that some demographic factors are associated with the use of ITNs among children and pregnant women in Nigeria. Sleeping under an ITN among Nigerian children was associated with the age of a child, geopolitical zone, and wealth quintile of households while the use of ITNs among Nigerian pregnant women was associated with the education level and wealth quintile.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Sachs J, Malaney P. The economic and social burden of malaria. Nature. 2002;415:680–5. doi: 10.1038/415680a. [DOI] [PubMed] [Google Scholar]
- 2.Pell C, Straus L, Andrew EV, Menaca A, Pool R. Social and cultural factors affecting uptake of interventions for malaria in pregnancy in Africa: A systematic review of the qualitative research. PLoS One. 2011;6:e22452. doi: 10.1371/journal.pone.0022452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mugisha F, Arinatwe J. Sleeping arrangements and mosquito net use among under-fives: results from the Uganda demographic and health survey. Malar J. 2003;2:40. doi: 10.1186/1475-2875-2-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dagne G, Deressa G. Knowledge and utilisation of insecticide-treated mosquito nets among freely supplied households in Wonago Woreda, Southern Ethiopia. Ethiop J Health Dev. 2008;22:34–41. [Google Scholar]
- 5.Abebe E, Mosanya ME, Amajoh C, Otsemobor O, Ezedinachi EN, Afolabi BM, et al. Nigeria roll back malaria consultative mission: Essential actions to support the attainment of the Abuja targets. 2003. Oct 20-25, [Last cited on 2011 Nov 05]. Available from: http://www.rollbackmalaria.org/partnership/country/docs/WAfrica/reaping_nigeria.pdf .
- 6.A road map for impact on malaria in Nigeria. Abuja: Federal Ministry of Health, National Malaria Programme; 2006. National Malaria Control Programme. [Google Scholar]
- 7.Insecticide-Treated Mosquito Nets: a WHO position statement. Geneva: World Health Organization; 2008. World Health Organization. [Google Scholar]
- 8.Lengeler C. Insecticide-treated bed nets and curtains for preventing malaria. Cochrane Database Syst Rev. 2004:CD000363. doi: 10.1002/14651858.CD000363.pub2. [DOI] [PubMed] [Google Scholar]
- 9.Eisele TP, Keating J, Littrel M, Larsen D, Macintyre K. Assessment of insecticide-treated bednet use among children and pregnant women across 15 countries using standardized national surveys. Am J Trop Med Hyg. 2009;80:209–14. [PubMed] [Google Scholar]
- 10.Malaria prevention program in Nigeria aims at universal bed net coverage. Washington: World Bank; 2009. World Bank. [Google Scholar]
- 11.Macintyre K, Keating J, Okbaldt YB, Zerom M, Sosler S, Ghebremeskel T, et al. Rolling out insecticide-treated nets in Eritrea: Examining the determinants of possession and use in malarious zones during the rainy season. Trop Med Int Health. 2006;11:824–33. doi: 10.1111/j.1365-3156.2006.01637.x. [DOI] [PubMed] [Google Scholar]
- 12.Nigeria Demographic and health survey 2008. Abuja: National Population Commission; 2009. National Population Commission and ICF Macro. [Google Scholar]
- 13.Grabowsky M, Farrel N, Hawley W, Chimumbwa J, Hoyer S, Wolkon A, et al. Integrating insecticide-treated bednets into a measles vaccination campaign achieves high, rapid and equitable coverage with direct and voucher-based methods. Trop Med Int Health. 2005;10:1151–60. doi: 10.1111/j.1365-3156.2005.01502.x. [DOI] [PubMed] [Google Scholar]
- 14.Blackburn BG, Eigege A, Gotau H, Gerlong G, Miri E, Hawley WA, et al. Successful integration of insecticide-treated bednet distribution with mass drug administration in central Nigeria. Am J Trop Med Hyg. 2006;75:650–5. [PubMed] [Google Scholar]


