Abstract
Introduction/Purpose
In humans, whole body heating and cooling are used to address physiological questions where core temperature is central to the investigated hypotheses. Core temperature can be measured in various locations throughout the human body. The measurement of intestinal temperature is increasingly used in laboratory settings as well as in athletics. However, it is unknown whether intestinal temperature accurately tracks pulmonary artery blood temperature, the gold standard, during thermal stimuli in resting humans, which is the investigated hypothesis.
Methods
This study compared pulmonary artery blood temperature (via thermistor in a pulmonary artery catheter) with intestinal temperature (telemetry pill) during whole-body heat stress (n=8), followed by whole-body cooling in healthy humans (mean ± SD age 24 ± 3 yrs; height 183 ± 8 cm; mass 78.1 ± 8.2 kg). Heat stress and subsequent cooling were performed by perfusing warm followed by cold water through a tube-lined suit worn by each subject.
Results
Prior to heat stress blood temperature (36.69 ± 0.25°C) was less than intestinal temperature (36.96 ± 0.21°C, P = 0.004). The increase in blood temperature after 20 min of heat stress was greater than intestinal temperature (0.70 ± 0.24 vs. 0.47 ± 0.18; P = 0.001). However, the increase in temperatures at the end of heat stress were similar between sites (blood Δ = 1.32 ± 0.20°C vs. intestinal Δ = 1.21 ± 0.36°C; P = 0.30). Subsequent cooling decreased blood temperature (Δ = −1.03 ± 0.34°C) to a greater extent than intestinal temperature (Δ = −0.41 ± 0.30°C, P = 0.04).
Conclusion
In response to the applied thermal provocations, early temperature changes in the intestine are less than the temperature changes in pulmonary artery blood.
Keywords: core temperature, heat stress, cooling, hyperthermia
Introduction
Paragraph Number 1 Whole body heat stress is an experimental intervention where internal body or “core temperature” is central to the investigated hypothesis and/or provides important information for the safety of the evaluated individual. Pulmonary artery blood temperature is considered the gold standard for core temperature measurement as it is a composite of blood temperatures returning to the heart from all regions of the body (5). However, given the invasive nature of this measurement, other minimally invasive approaches to provide an index of core temperature, such as the intestinal telemetric pill, are often preferred.
Paragraph Number 2 The telemetric pill was first used in the 1960’ s (18) and has become an increasingly popular method especially in field settings (8); under the assumption that changes in intestinal temperature reflect core temperature. A good agreement between changes in intestinal, rectal and esophageal temperatures have been reported in a variety of environments (8, 9, 16, 20, 21, 25, 27), including whole body heating and cooling. However, differences in basal temperatures can exist between the measurement sites before the onset of a thermal provocation. Moreover, the rate of temperature change between differing measures of core temperature may vary between the sites during a thermal provocation.
Paragraph Number 3 To prevent unsafe and/or undesirable changes in core temperature, it is important to understand the agreement between pulmonary artery blood and intestinal temperatures in conditions where external temperatures change rapidly, such as during whole body heat stress and subsequent cooling. Whole body cooling is an effective strategy to reduce elevated core temperatures associated with heat injury (1, 2, 11, 14, 28). Under such conditions the tracking of internal temperature is important and therefore an accurate measure of core temperature is necessary. Given the increased use of intestinal telemetric pills to monitor core temperature in collegiate and professional athletics, particularly American football, (7, 12, 15, 17, 24, 26, 32), where heat injuries can occur, an understanding of the accuracy of this device in monitoring core temperature is important.
Paragraph Number 4 Despite the importance of accurately measuring temperature, the agreement between the intestinal pill and other minimally invasive core temperature measures during thermal provocations is equivocal (19, 21). Furthermore, the agreement between pulmonary artery blood and intestinal temperature (using the telemetric pill) during rapid whole body heating and cooling is unknown. Therefore, the purpose of this study was to test the hypothesis that intestinal temperature accurately tracks changes in pulmonary artery blood temperature during whole body heat stress and subsequent cooling in humans.
Methods
Subjects
Paragraph Number 5 Eight healthy males participated in this study. Subject characteristics were age, 24 ± 3 years; height, 183 ± 8 cm; and weight, 78.1 ± 8.2 kg (mean±SD). Subjects were not taking any medications, were non-smokers, were free of any known cardiovascular, metabolic, or neurological diseases and refrained from alcohol, caffeine, and exercise for 24 h before the study. Subjects were informed of the purpose, procedures and risks of the study before providing their informed written consent. The protocol and consent were approved by the local ethics committee of Copenhagen and conformed to the Declaration of Helsinki.
Instrumentation and Experimental Protocol
Paragraph Number 6 On arrival to the lab, 90-120 min prior to pre-heat stress data collection, subjects swallowed an ingestible telemetry pill for the measurement of intestinal temperature (HQ, Palmetto, FL). With the exception of water ingested while swallowing the telemetry pill, subjects refrained from ingestion of fluids throughout the protocol. A 20-gauge flow-directed pulmonary arterial catheter, fitted with a thermister at the tip, (93A-831H-7.5F, Baxter Healthcare Corp., Irvine, CA) was introduced through the basilic vein of the left arm and advanced into the pulmonary artery. The catheter was flushed with isotonic saline at 3 ml/h. Each subject donned a water-perfused tube lined suit (Med-Eng, Ottawa, Canada) that covered their entire body except for the head, hands, both forearms arms, and feet. The suit permitted the control of whole body skin and internal temperatures by adjusting the temperature of the water perfusing the suit. Heat stress was imposed by perfusing 48-50°C water through the suit for 42 ± 6 min sufficient to elevate pulmonary artery blood temperature by at least 1°C. In six subjects rapid whole-body cooling was employed after the heat stress by perfusing 10-15°C water through the suit until pulmonary artery blood temperature was reduced ~1°C; cooling duration was 11 ± 3 min.
Data Analysis
Paragraph Number 7 Intestinal temperature was sampled via a data-acquisition system (Biopac System, Santa Barbara, CA), while pulmonary artery blood temperature was obtained from the digital readout of a cardiac output computer interfaced with the pulmonary artery catheter. Pulmonary artery blood temperature readings were obtained at ~5 min intervals. The temperatures at pre-heat stress, approximately mid-way through heat stress (20 min), the end of heat stress and the end of cooling, as well as the change in temperature that occurred with each perturbation were evaluated for statistical differences between devices using a paired samples t-test. Changes in pulmonary artery blood and intestinal temperatures during heat stress from normothermia were also compared for limits of agreement using a Bland and Altman plot (3). Linear regression analysis was used to compare the changes in temperature between methods from normothermia during heat stress and from heat stress to subsequent whole body cooling. Correlation coefficients were adjusted for repeated measures (4). Data are reported as mean±SD. Statistical significance was set at P ≤ 0.05.
Results
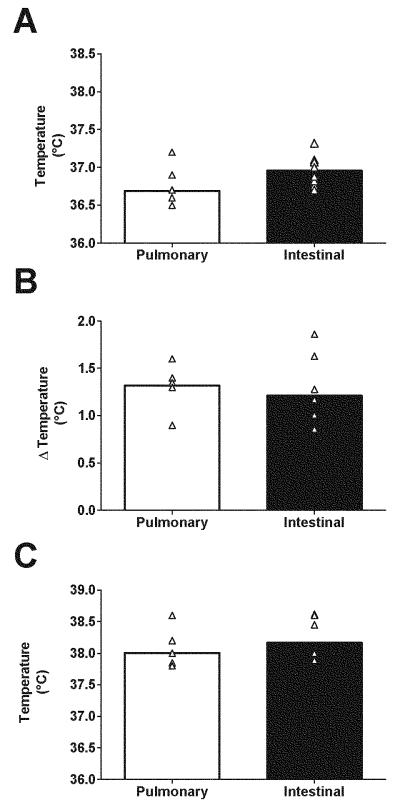
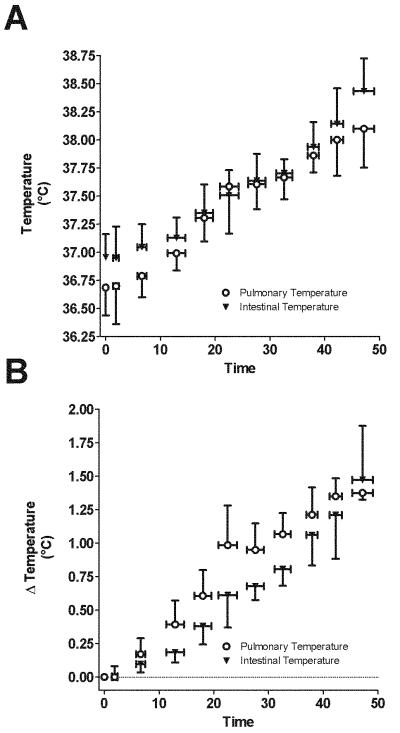
Paragraph Number 8 At pre-heat stress baseline, intestinal temperature was higher than pulmonary artery blood temperature (36.96 ± 0.21 vs. 36.69 ± 0.25 respectively; P = 0.004, Fig. 1a). However, after ~20 min of heat stress the increase in pulmonary artery blood temperature was larger than intestinal temperature (0.70 ± 0.24 vs. 0.47 ± 0.18°C; P = 0.001), yet at the end of heat stress neither the increase from pre-heat stress baseline (pulmonary artery: 1.32 ± 0.20 vs. intestinal: 1.21 ± 0.36, Fig. 1b) nor were pulmonary artery blood and intestinal temperatures (38.01 ± 0.28 vs. 38.17 ± 0.33 respectively; both P > 0.05, Fig.1c) different. The time course of the actual and change in pulmonary artery and intestinal temperatures during whole body heating is shown in Fig. 2a and 2b respectively.
Figure 1. Core temperatures with heat stress.
Pre-heat stress pulmonary artery and intestinal temperatures are illustrated in panel A. Neither the increase in temperatures from pre-heat stress baseline (panel B), nor the actual pulmonary artery and intestinal temperatures at the end of heat stress (panel C), were different between measurement sites at the end of the heat stress (both P > 0.05). Open triangles indicate individual data points while columns depict mean responses. Please note that N=8 for these analyses but some data points are obscured because they overlap other data points.
Figure 2.
Time course of the actual (panel A) and delta (panel B) pulmonary artery blood and intestinal temperatures during whole body heating, Data are mean ± SD from 8 subjects. Note that every subject was not heated for the same duration and thus the number of subjects per averaged data point is less than 8 for the final data points. This results in differences in the final temperatures (for both Panel A and B) relative to that depicted in Figure 1.
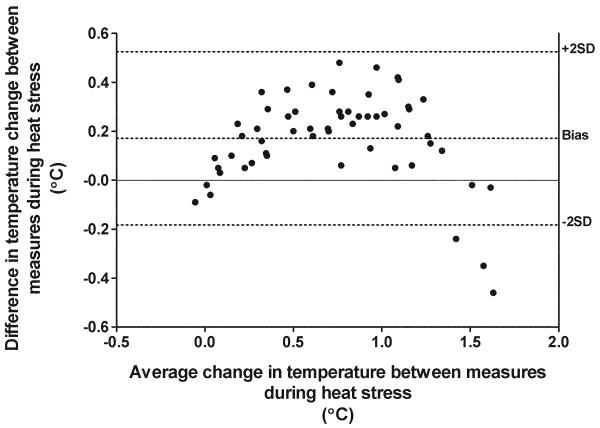
Paragraph Number 9 The Bland-Altman limits of agreement analysis indicated an overall small bias toward pulmonary artery blood temperature (0.17°C) during heat stress. However, this bias was achieved via an inverted “U-shaped” curve (Fig. 3). The upper and lower limits of agreement (2SD) between methods of temperature measurement across heat stress were −0.18 and 0.53°C, respectively.
Figure 3. Limits of agreement between pulmonary artery blood and intestinal temperature during heat stress.
Bland-Altman plot of the differences in the elevation in pulmonary artery blood relative to intestinal temperatures throughout the heat stress (pulmonary artery blood – intestinal temperature). This comparison indicates an overall small bias towards elevated pulmonary artery blood temperature (0.17°C) during the heat stress. The upper and lower limits of agreement between pulmonary artery and intestinal temperature across heat stress were −0.18 and 0.53 °C, respectively. See text for discussion of the shape of this curve. Data are from 8 subjects.
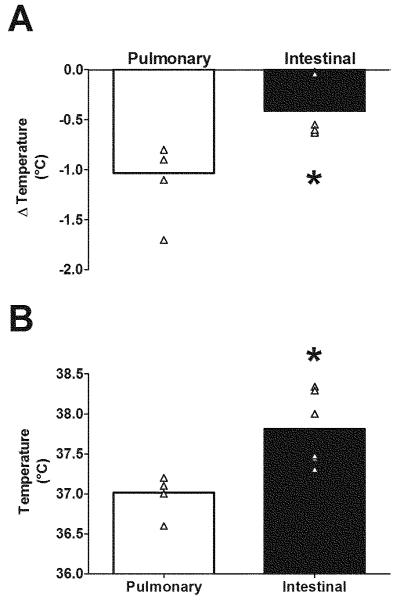
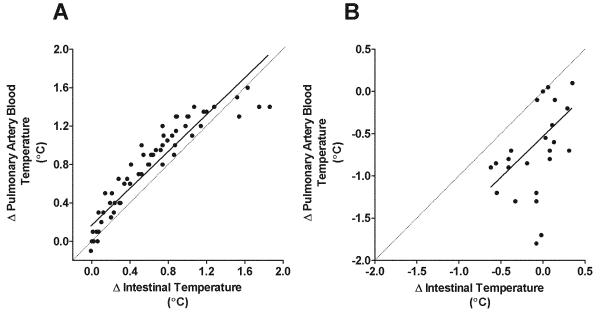
Paragraph Number 10 The decrease in pulmonary artery blood temperature during subsequent whole body cooling was greater (Δ = −1.03 ± 0.34°C) relative to intestinal temperature (−0.41 ± 0.30°C, P = 0.04, Fig. 4a). Consequently at the end of whole body cooling pulmonary artery blood temperature was lower than intestinal temperature (37.01 ± 0.21 vs. 37.81 ± 0.46; P = 0.003, Fig. 4b). The association between changes in pulmonary artery and intestinal temperature were higher during whole body heat stress (r = 0.93, Fig. 5a) than whole body cooling (r = 0.58, Fig. 5b).
Figure 4. Core temperatures with whole body cooling.
Following heat stress, subsequent whole body cooling caused a larger reduction in pulmonary artery temperature than intestinal temperature (P = 0.04; Panel A), which resulted in differences in temperatures the end of the cooling stimulus (P = 0.003; Panel B). These data demonstrate that intestinal temperature lags pulmonary artery temperature during rapid cooling of heat stressed individuals. Open triangles indicate individual data points while columns depict mean responses. Please note that N=6 for these analyses but some data points are obscured because they overlap other data points. * denotes a significant difference between temperature measures (P < 0.05).
Figure 5. Changes in core temperature during heat stress and whole body cooling.
Throughout the heat stress there was a relatively strong relationship between pulmonary artery and intestinal temperatures (r = 0.93), however, this relationship weakens during subsequent whole body cooling (r = 0.58). Solid line depicts the regression between the indicated values. Dashed line represents the line of identity. Values are from 8 subjects for heat stress and 6 subjects for whole body cooling.
Discussion
Paragraph Number 11 The major finding from this study is that while pulmonary artery blood and intestinal temperatures were not different at the end of the whole body heat stress, the increase in pulmonary artery blood temperature was more rapid than intestinal temperature in the early stages of the heat stress. Likewise, during whole-body cooling following heating, the reduction in pulmonary artery blood temperature was appreciably greater than intestinal temperature. These data indicate that there are differences between pulmonary artery blood and intestinal temperatures during the early stages of a whole body heat stress and also during rapid cooling following the heat stress. While there is a significant body of research investigating the agreement between temperature measures during thermal provocations, often showing that intestinal pill temperature responds slowly to thermal provocations, the present data specifically indicate slower changes in intestinal temperature relative to the gold standard (i.e., pulmonary artery blood temperature) in response to the employed thermal provocations. These data further highlight the differences in temperature between sites during these common experimental perturbations, thereby showing that “core temperature” is dependent upon the measurement site.
Paragraph Number 12 In normothermic resting humans temperatures likely vary in different regions of the body, as was evident in the present study (Fig. 1a). However, the primary focus of this project was to investigate whether changes in intestinal temperature were similar to changes in pulmonary artery temperature during thermal provocations. During passive whole body heating, ingestible pill based measures of intestinal temperature have been compared to esophageal, auditory meatus, and rectal temperatures (21, 27). In the present study we found that at the end of whole body heating there was only a small, non-significant difference between pulmonary artery blood and intestinal temperatures (~0.16°C). This is similar to that reported by O’ Brien et al. (27), in which the differences between esophageal and intestinal temperatures to a mild thermal provocation were also small (~0.25°C). Our findings expand upon these results and show that pulmonary artery blood and intestinal temperatures are similar following a moderate, but more severe passive heat stress, than previously investigated (27). The relationship between temperatures during the heat stress is illustrated in figure 5a, where these changes were closely correlated (r = 0.93; Fig. 5). Despite this overall agreement between these methods during heating, there was a discrepancy between measures during the initial 20 min of heating where the increase in pulmonary artery blood temperature was larger than the intestine. This difference is in line with the discrepant increases between esophageal and intestinal temperatures following a short period (~20 min) of hot water immersion (21).
Paragraph Number 13 The temperature profile throughout whole body heating is illustrated by the inverted ‘u’ shape of the Bland-Altman plot (Fig. 3). When evaluated over the entire heating period, the small bias depicted in Figure 3 indicates that the changes in pulmonary artery blood temperature were slightly larger than the intestine. However, it is important to note that during the early stages of the heat stress, the upward portion of the inverted ‘u’ was due to the aforementioned greater increase in pulmonary artery blood relative to intestinal temperature. Near the end of the heat stress the downward portion of the inverted ‘u’ was due to a greater increase in intestinal relative to pulmonary artery blood temperature primarily in one subject, in whom there was a marked increase in intestinal temperature (from 37.9 to 38.6°C) with less of an increase in pulmonary artery blood temperature (from 37.8 to 38°C). These discrepancies can also be seen in Fig. 5a where the plot of changes in pulmonary artery blood against intestinal temperature during heat stress deviates from the line of identity.
Paragraph Number 14 Following the development of hyperthermia or heat illness, either through exercise or other forms of heat exposure, it may be necessary to rapidly reduce body temperature including critical areas of the body, including the brain and central nervous system, to avoid neuronal damage; and also the intestines to avoid increased gut permeability associated with heat illness (6). Following the development of hyperthermia, whole body cooling causes large and rapid reductions in esophageal temperature (31) that are greater compared to rectal (19) and intestinal temperatures (21). Although the importance of this cooling has previously been addressed (10), in such circumstances where rectal temperature is often used as a measure of “core” temperature (13), the agreement between pulmonary artery blood and intestinal temperatures was unknown. We found that during whole body cooling the reduction in pulmonary artery blood temperature (and therefore the blood temperature perfusing the brain) was appreciably greater than intestinal temperature (Fig. 4a); being approximately double the reduction of intestinal temperature during the same time period, which remained closer to ~38°C following cooling. The difference between temperature measures is also highlighted by the weak relationship shared between changes in pulmonary artery blood and intestinal temperatures during cooling (r = 0.58; Fig. 5b). The discrepancy between pulmonary artery blood and intestinal pill temperatures have important implications for the monitoring of ‘core’ temperatures during cooling subsequent to exercise induced hyperthermic injury, as the development of hypothermia should be avoided. This is particularly important in athletic events where the intestinal pill is commonly used. Therefore, if rapid cooling is deemed necessary to treat dangerously hyperthermic temperatures measured at the intestine, the magnitude of the reduction in blood temperature perfusing regions such as the brain and central nervous system is likely substantially greater relative to the intestine.
Paragraph Number 15 The mechanism for the discrepancy in the rate of temperature change between pulmonary artery blood and intestinal temperatures, both early during the heat stress and subsequent whole body cooling, is unknown but can be speculated upon. Whole body heat stress induces large increases in skin temperature owing to the high water temperature running through the water perfused suit. This increase in skin temperature is accompanied by rapid elevations in skin blood flow (22). This increase of blood flow through warm skin causes a rapid increase in cutaneous blood temperature which then returns to the heart and increases pulmonary artery blood temperature. In contrast to the skin, splanchnic blood flow decreases during whole-body heat stress (29). Such a response will reduce the rate of delivery of warmed blood to the splanchnic region, likely delaying the elevation in intestinal temperature measured with the pill, relative to pulmonary blood temperature. A similar mechanism may explain the slower reduction in intestinal temperature during cooling, given the expectation that blood temperature will cool at a faster rate that intestinal temperature, recognizing that the capacity to cool skin blood becomes minimized as local skin cooling causes cutaneous vasoconstriction (23). Moreover, during rapid cooling following a heat stress, the elevation of splanchnic blood flow to pre-heat stress levels, and thus changes in splanchnic temperatures due to the cooling stimulus, is likewise relatively slow (30).
Paragraph Number 16 A limitation of the present study is that pill temperature was likely sampled from slightly different locations, given that the pill is expected to travel slightly within the intestines during the data collection period. This is in contrast to temperature measures from the pulmonary artery, which are obtained from a fixed location. That said, it is unlikely that the differences in the change in temperature between devices both early during heat stress and following whole body cooling were a result of potentially small changes in pill position within the intestine
Paragraph Number 17 In summary, the present data provide evidence that early during whole-body heat stress the elevation in intestinal temperature lags pulmonary artery blood temperature. However, as the exposure to heat stress continues these temperature differences are minimized such that actual temperatures between these sites are not different at the end of a heat stress sufficient to elevate pulmonary artery blood temperature by ~1.3°C. Perhaps more profound is the large difference in the temperature profiles during subsequent rapid whole body cooling, in which intestinal temperature appreciably lags pulmonary artery blood temperature. These latter results have important implications towards an understanding of the responsiveness of rapid cooling on “core temperature” of individuals who are experiencing a hyperthermic injury. Furthermore, these data highlight that changes in temperature during a thermal provocation likely vary and depend upon the measurement site,
Acknowledgements
This study was supported by NIH Grants HL61388 & HL84072. Morton Overgaard was supported by a grant from Mr Jakob Ehrenreich and Grethe Ehrenreichs.
Footnotes
Conflict of Interest: James Pearson – none declared; Matthew S. Ganio – none declared; Thomas Seifert – none declared; Morten Overgaard – none declared; Niels H. Secher – none declared; Craig G. Crandall – none declared
There are no conflicts of interest. The results of the present study do not constitute endorsement by ACSM
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Armstrong LE, Casa DJ, Millard-Stafford M, Moran DS, Pyne SW, Roberts WO. American College of Sports Medicine position stand. Exertional heat illness during training and competition. Med Sci Sports Exerc. 2007;39(3):556–72. doi: 10.1249/MSS.0b013e31802fa199. [DOI] [PubMed] [Google Scholar]
- 2.Binkley HM, Beckett J, Casa DJ, Kleiner DM, Plummer PE. National Athletic Trainers’ Association position statement: Exertional heat illnesses. J Athl Train. 2002;37(3):329–43. [PMC free article] [PubMed] [Google Scholar]
- 3.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1(8476):307–10. [PubMed] [Google Scholar]
- 4.Bland JM, Altman DG. Calculating correlation coefficients with repeated observations: Part 1--Correlation within subjects. BMJ. 1995;310(6977):446. doi: 10.1136/bmj.310.6977.446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bligh J. Temperature regulation in mammals and other vertebrates. North-Holland; London: 1973. pp. 80–84. [Google Scholar]
- 6.Bouchama A, Knochel JP. Heat stroke. N Engl J Med. 2002;346(25):1978–88. doi: 10.1056/NEJMra011089. [DOI] [PubMed] [Google Scholar]
- 7.Byrne C, Lee JK, Chew SA, Lim CL, Tan EY. Continuous thermoregulatory responses to mass-participation distance running in heat. Med Sci Sports Exerc. 2006;38(5):803–10. doi: 10.1249/01.mss.0000218134.74238.6a. [DOI] [PubMed] [Google Scholar]
- 8.Byrne C, Lim CL. The ingestible telemetric body core temperature sensor: a review of validity and exercise applications. Br J Sports Med. 2007;41(3):126–33. doi: 10.1136/bjsm.2006.026344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Casa DJ, Becker SM, Ganio MS, Brown CM, Yeargin SW, Roti MW, Siegler J, Blowers JA, Glaviano NR, Huggins RA, Armstrong LE, Maresh CM. Validity of devices that assess body temperature during outdoor exercise in the heat. J Athl Train. 2007;42(3):333–42. [PMC free article] [PubMed] [Google Scholar]
- 10.Casa DJ, Kenny GP, Taylor NA. Immersion treatment for exertional hyperthermia: cold or temperate water? Med Sci Sports Exerc. 2010;42(7):1246–52. doi: 10.1249/MSS.0b013e3181e26cbb. [DOI] [PubMed] [Google Scholar]
- 11.Casa DJ, McDermott BP, Lee EC, Yeargin SW, Armstrong LE, Maresh CM. Cold water immersion: the gold standard for exertional heatstroke treatment. Exerc Sport Sci Rev. 2007;35(3):141–9. doi: 10.1097/jes.0b013e3180a02bec. [DOI] [PubMed] [Google Scholar]
- 12.Castellani JW, Delany JP, O’Brien C, Hoyt RW, Santee WR, Young AJ. Energy expenditure in men and women during 54 h of exercise and caloric deprivation. Med Sci Sports Exerc. 2006;38(5):894–900. doi: 10.1249/01.mss.0000218122.59968.eb. [DOI] [PubMed] [Google Scholar]
- 13.Clowes GH, Jr., O’Donnell TF., Jr. Heat stroke. N Engl J Med. 1974;291(11):564–7. doi: 10.1056/NEJM197409122911106. [DOI] [PubMed] [Google Scholar]
- 14.Costrini A. Emergency treatment of exertional heatstroke and comparison of whole body cooling techniques. Med Sci Sports Exerc. 1990;22(1):15–8. [PubMed] [Google Scholar]
- 15.Edwards AM, Clark NA. Thermoregulatory observations in soccer match play: professional and recreational level applications using an intestinal pill system to measure core temperature. Br J Sports Med. 2006;40(2):133–8. doi: 10.1136/bjsm.2005.021980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fortney SM, Mikhaylov V, Lee SM, Kobzev Y, Gonzalez RR, Greenleaf JE. Body temperature and thermoregulation during submaximal exercise after 115-day spaceflight. Aviat Space Environ Med. 1998;69(2):137–41. [PubMed] [Google Scholar]
- 17.Fowkes Godek S, Godek JJ, Bartolozzi AR. Thermal Responses in Football and Cross-Country Athletes During Their Respective Practices in a Hot Environment. J Athl Train. 2004;39(3):235–40. [PMC free article] [PubMed] [Google Scholar]
- 18.Fox RH, Goldsmith R, Wolff HS. The use of a radio pill to measure deep body temperature. The Journal of Physiology. 1962;160(Suppl):22P–3P. [Google Scholar]
- 19.Gagnon D, Lemire BB, Casa DJ, Kenny GP. Cold-water immersion and the treatment of hyperthermia: using 38.6 degrees C as a safe rectal temperature cooling limit. J Athl Train. 2010;45(5):439–44. doi: 10.4085/1062-6050-45.5.439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gant N, Atkinson G, Williams C. The validity and reliability of intestinal temperature during intermittent running. Med Sci Sports Exerc. 2006;38(11):1926–31. doi: 10.1249/01.mss.0000233800.69776.ef. [DOI] [PubMed] [Google Scholar]
- 21.Gibson TM, Redman PJ, Belyavin AJ. Prediction of oesophageal temperatures from core temperatures measured at other sites in man. Clin Phys Physiol Meas. 1981;2(4):247–52. doi: 10.1088/0143-0815/2/4/001. [DOI] [PubMed] [Google Scholar]
- 22.Johnson JM, Brengelmann GL, Rowell LB. Interactions between local and reflex influences on human forearm skin blood flow. J Appl Physiol. 1976;41(6):826–31. doi: 10.1152/jappl.1976.41.6.826. [DOI] [PubMed] [Google Scholar]
- 23.Kellogg DL., Jr. In vivo mechanisms of cutaneous vasodilation and vasoconstriction in humans during thermoregulatory challenges. J Appl Physiol. 2006;100(5):1709–18. doi: 10.1152/japplphysiol.01071.2005. [DOI] [PubMed] [Google Scholar]
- 24.Laursen PB, Suriano R, Quod MJ, Lee H, Abbiss CR, Nosaka K, Martin DT, Bishop D. Core temperature and hydration status during an Ironman triathlon. Br J Sports Med. 2006;40(4):320–5. doi: 10.1136/bjsm.2005.022426. discussion 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lee SM, Williams WJ, Fortney Schneider SM. Core temperature measurement during supine exercise: esophageal, rectal, and intestinal temperatures. Aviat Space Environ Med. 2000;71(9):939–45. [PubMed] [Google Scholar]
- 26.Mekjavic B, Golden FS, Eglin M, Tipton MJ. Thermal status of saturation divers during operational dives in the North Sea. Undersea Hyperb Med. 2001;28(3):149–55. [PubMed] [Google Scholar]
- 27.O’Brien C, Hoyt RW, Buller MJ, Castellani JW, Young AJ. Telemetry pill measurement of core temperature in humans during active heating and cooling. Med Sci Sports Exerc. 1998;30(3):468–72. doi: 10.1097/00005768-199803000-00020. [DOI] [PubMed] [Google Scholar]
- 28.O’Donnell TF, Jr., Clowes GH., Jr. The circulatory abnormalities of heat stroke. N Engl J Med. 1972;287(15):734–7. doi: 10.1056/NEJM197210122871502. [DOI] [PubMed] [Google Scholar]
- 29.Rowell LB, Brengelmann GL, Blackmon JR, Murray JA. Redistribution of blood flow during sustained high skin temperature in resting man. J Appl Physiol. 1970;28(4):415–20. doi: 10.1152/jappl.1970.28.4.415. [DOI] [PubMed] [Google Scholar]
- 30.Rowell LB, Detry JR, Profant GR, Wyss C. Splanchnic vasoconstriction in hyperthermic man--role of falling blood pressure. J Appl Physiol. 1971;31(6):864–9. doi: 10.1152/jappl.1971.31.6.864. [DOI] [PubMed] [Google Scholar]
- 31.Taylor NA, Caldwell JN, Van den Heuvel AM, Patterson MJ. To cool, but not too cool: that is the question--immersion cooling for hyperthermia. Med Sci Sports Exerc. 2008;40(11):1962–9. doi: 10.1249/MSS.0b013e31817eee9d. [DOI] [PubMed] [Google Scholar]
- 32.White LJ, Jackson F, McMullen MJ, Lystad J, Jones JS, Hubers RH. Continuous core temperature monitoring of search and rescue divers during extreme conditions. Prehosp Emerg Care. 1998;2(4):280–4. doi: 10.1080/10903129808958880. [DOI] [PubMed] [Google Scholar]