Abstract
Background
Joint instability has been suggested as a risk factor for knee osteoarthritis and a cause of significant functional declines in those with symptomatic disease. However, the relationship between altered knee joint mechanics and self-reports of instability in individuals with knee osteoarthritis remains unclear.
Methods
Fourteen subjects with knee osteoarthritis and complaints of joint instability and 12 control volunteers with no history of knee disease were recruited for this study. Dynamic stereo X-ray technology was used to assess the three-dimensional kinematics of the knee joint during the loading response phase of gait.
Findings
Individuals with concurrent knee osteoarthritis and joint instability demonstrated significantly reduced flexion and internal/external rotation knee motion excursions during the loading response phase of gait (P < 0.01), while the total abduction/adduction range of motion was increased (P < 0.05). In addition, the coronal and transverse plane alignment of the knee joint at initial contact was significantly different (P < 0.05) for individuals with concurrent knee osteoarthritis and joint instability. However, the anteroposterior and mediolateral tibiofemoral joint positions at initial contact and the corresponding total joint translations were similar between groups during the loading phase of gait.
Interpretations
The rotational patterns of tibiofemoral joint motion and joint alignments reported for individuals with concurrent knee osteoarthritis and joint instability are consistent with those previously established for individuals with knee osteoarthritis. Furthermore, the findings of similar translatory tibiofemoral motion between groups suggest that self-reports of episodic joint instability in individuals with knee osteoarthritis may not necessarily be associated with adaptive alterations in joint arthrokinematics.
Keywords: Knee Instability, Knee Osteoarthritis, Arthrokinematics
1. INTRODUCTION
Knee Osteoarthritis (OA) is a common cause of symptoms (Felson et al., 2000, Felson et al., 1987, Felson et al., 1995, Muraki et al., 2009) and a frequent source of functional limitations in the older adults (Ettinger et al., 1994, Guccione et al., 1994). Recently, there has been increased interest in the possible role of joint instability as a risk factor for accelerated rates of disease progression and functional decline in individuals with knee OA. Knee instability has previously been linked to the pathogenesis of knee OA in presence of meniscus or anterior cruciate ligament injuries (Amin et al., 2008, Berthiaume et al., 2005). It has also been reported that a significant number of individuals with knee OA who report episodes of knee instability (such as giving way, buckling, or shifting of their arthritic knees) are adversely affected in their ability to perform weight-bearing functional tasks (Fitzgerald et al., 2004). To date, however, a thorough understanding of the potential underlying alterations in knee joint mechanics in presence of concurrent knee OA and joint instability has not been fully elucidated.
Changes in knee joint kinematics and static alignment have been previously linked to the pathogenesis of knee OA. For instance, symptomatic OA knees have demonstrated significantly reduced sagittal–plane knee joint excursions during gait (Andriacchi et al., 2004, Childs et al., 2004, Messier et al., 1992). In addition, altered coronal and transverse plane tibiofemoral joint rotations (Astephen and Deluzio, 2005, Nagao et al., 1998) and malalignments (Sharma et al., 2000, Sharma et al., 2001, Yagi, 1994, Yagi and Sasaki, 1986) have been linked to an increased incidence of knee OA and rates of disease progression. Such abnormal kinematics and malalignments may contribute to initiation and progression of the disease by elevating joint contact stresses and accelerating the rate of cartilage breakdown (Andriacchi et al., 2004, Yang et al., 2009). It is also suggested that alterations in knee arthrokinematics (i.e. movement between the tibial and femoral joint surfaces) could play a role in the progression of knee OA by altering loads and load distributions between the contact surfaces of the joint (Andriacchi et al., 2004). However, no previous study has characterized the dynamic knee joint arthrokinematics and potential malalignments associated with presence of concurrent knee OA and joint instability.
The lack of current evidence relating instability, joint kinematics, and knee OA is largely due to limitations of commonly available methodology. For example, common video-motion analysis techniques use markers placed on the skin that are prone to excessive movement artifacts and are generally unsuitable for quantifying knee arthrokinematics (Akbarshahi et al., 2010). In addition, placing fixtures on the limb or a pin in the bone will cause movement adaptations that do not necessarily reflect normal function (Andriacchi et al., 2004). More recently, Dynamic Stereo X-ray (DSX) analysis has been suggested as a more accurate method of measuring knee motion during functional activities (Anderst et al., 2009, Tashman and Anderst, 2003, You et al., 2001). The basic premise behind DSX is that high speed bi-plane radiographic images of the knee are combined with subject-specific three dimensional (3D) bone models acquired from high-resolution imaging modalities to determine the relative knee rotations and translations (Akbarshahi et al., 2010, Anderst et al., 2009, Tashman and Anderst, 2003). To this end, dynamic DSX has proven to be a useful and valid tool for non-invasive quantification of dynamic knee joint kinematics in-vivo (Anderst et al., 2009).
Using DSX technology, the purpose of the current study was to investigate the differences in knee joint kinematics during the loading response phase of gait between individuals with concurrent knee OA and joint instability compared to a healthy control group. Loading response was selected as a critical time period associated with high demands on the knee joint as well as a previously reported dynamic alignment change in presence of knee OA (Astephen and Deluzio, 2005, Schipplein and Andriacchi, 1991). We had hypothesized that individuals with knee OA who report episodes of knee instability would exhibit less rotational and greater translational joint motion during the loading response phase of gait. An improved understanding of characteristic alterations in functional knee kinematics in individuals with concurrent knee OA and instability may lead to the development of more effective rehabilitation strategies for this patient population.
2. METHODS
2.1. Subject Selection
Twenty–six subjects were recruited for this study (Table 1). Fourteen subjects with knee OA who reported episodes of knee instability constituted the experimental group. Subjects were included in the knee OA group if they met the American College of Rheumatology classification criteria (Altman et al., 1991) and demonstrated radiographic severity of knee OA of at least grade II or higher according to the Kellgren and Lawrence radiographic severity rating scale (Kellgren and Lawrence, 1957). In addition, knee OA subjects were only included if they had a self-reported knee instability rating of ≤ 3 on the knee stability scale (Fitzgerald et al., 2004). A knee instability rating of ≤ 3 indicates that the subject perceives the symptom of instability to be affecting their ability to perform activities of daily living (Fitzgerald et al., 2004). Subjects with knee OA were subsequently subdivided into either “medial knee OA” or “medial and lateral Knee OA” groups based on their radiographic pattern of compartmental disease. In addition, twelve subjects without knee OA or history of knee instability served as the control group. Subjects were included in the control group if they were free of radiographic knee OA, had no complaints of knee pain, and no complaints or episodes of knee instability during activities of daily living. Prior to participation, all subjects were informed as to the nature of the study and signed an informed consent form approved by the Institutional Review Board of the University of Pittsburgh.
Table 1.
Subject Characteristics Mean (standard deviations)
| Control No OA (N = 12) | Medial Knee OA (N = 7) | Medial & Lateral Knee OA (N = 7) | |
|---|---|---|---|
| Female (%) | 6 (50%) | 3 (43%) | 5 (71%) |
| Age (years) | 70.2 (8.0) | 68.4 (10.0) | 69.4 (5.8) |
| Height (cm) | 173.3 (12.8) | 172.8 (11.5) | 169.3 (7.6) |
| Weight (kg) | 76.7 (20.3) | 92.5 (20.0) | 81.5 (6.2) |
| BMI | 25.3 (4.6) | 31.0 (6.0)* | 28.5 (2.63) |
Significantly different than the control group (p < 0.05)
Subjects were excluded, regardless of group, if they had a past history of traumatic knee injury, lower extremity total joint arthroplasty, cardiovascular disease (e.g. myocardial infarction, coronary artery disease, stroke), uncontrolled hypertension, or neurological disorders that effect lower extremity function (e.g. stroke, peripheral neuropathy, Parkinson’s disease, multiple sclerosis). To ensure safe participation in the study, subjects were also excluded if they required use of an assistive device for ambulation, reported a history of two or more falls within the previous year, or if they reported lack of confidence in ambulating a distance of 100 feet without an assistive device or need of a rest period.
2.2. Testing Procedures
DSX was used to assess 3D tibiofemoral joint kinematics from biplane radiographic images acquired during the loading response phase of gait. The biplane x-ray system contained 2 x-ray gantries that are configured with their beam paths intersecting at 60° in a plane parallel to the floor. Each gantry contained a 100-kW pulsed x-ray generator (CPX 3100CV; EMD Technologies, Quebec, Canada), a 40-cm image intensifier (Thales, France), and a high-speed 4 megapixel digital video camera (Phantom v10, Vision Research, Wayne, New Jersey). The x-ray generators were customized to provide short-duration pulses at very high repetition rates. For the purposes of the current study, radiographs were generated with a 1 ms pulse width at 100 Hz, with a 90kVp/200mA protocol. This experimental approach has been used in previous studies of knee function and is capable of measuring in vivo joint motion with precision of 0.2 mm (Tashman and Anderst, 2003, Tashman et al., 2007).
Subjects were positioned on a treadmill within the biplane x-ray system so that the knee of interest would remain in the system’s 3D imaging volume throughout the loading phase of gait. For subjects with knee OA, the knee in which subjects reported episodes of instability was designated as the test knee. In cases where both knees experienced episodes of instability, the more problematic knee was designated as the test knee. For control subjects, the knee from the dominant lower limb (the limb subjects would prefer to use to kick a ball) was designated as the test knee.
All gait trials were performed on a dual-belt instrumented treadmill (Bertec Corp., Columbus, OH) to measure ground reaction forces. Ground reaction forces were subsequently used to determine the loading response phase of gait defined as the time between initial contact with the ground to the first peak in the vertical ground reaction force curve. A moderately declined walking condition (7% grade) was adopted as the testing protocol and the velocity for the walking trials were standardized for all subjects at 0.75 meters per second based on the participant feedback from a previously conducted pilot study. Declined walking was chosen due to the frequent patient reports of knee instability during this condition. For each data collection session, the biplane x-ray system was triggered manually to record a 500 milisecond time period starting just prior to initial contact to at least 200 ms post initial contact. Data was collected for three individual walking trials and averaged for statistical analysis.
2.3. Quantification of Knee Joint Kinematics
On the same day as laboratory testing, subjects underwent computerized tomography (CT) imaging of the tibiofemoral joint. The CT field of view was approximately 28 × 28 cm, slice thickness ranged from 0.6 to 1.25 mm, and in-plane resolution was approximately 0.55 mm per pixel. The 3D bone models of the distal femur and proximal tibia of each knee joint were reconstructed from the CT images, as previously described in detail (Tashman and Anderst, 2003). Briefly, the tibia and femur were manually segmented from surrounding tissues. Custom software was then used to perform feature-based interpolation to create the reconstructed 3D bone models. A model-based tracking algorithm was employed to determine 3D joint motion by matching the radiographic images with projections through the 3D volumetric bone models derived from CT, as previously described (Anderst et al., 2009).
Subject-specific local anatomical coordinate systems were created for both the femur and tibia (Tashman and Anderst, 2003). The origin of the femoral coordinate system was defined as the point halfway between the center of the medial and lateral femoral condyles. Similarly, the origin of the tibial coordinate system was defined to be the point located halfway between the most medial and lateral aspects of the tibial plateau. Rotations of the tibia relative to the femur were defined with respect to the bone-fixed coordinate systems, and calculated using body-fixed axes in the order of flexion-extension, adduction-abduction, and internal-external rotation (Tashman et al., 2007). Neutral rotations (zero values) were defined as the position where the tibia and femoral coordinate systems were aligned. Anteroposterior (AP) and mediolateral (ML) displacements of the tibia relative to the femur were also quantified using the position vector from the femoral anatomical origin to the tibial anatomical origin, expressed in the tibial coordinate system.
2.4. Statistical Analysis
Group differences for tibiofemoral rotations and translations were compared at initial contact, as well as for the total excursions of the joint within the loading response phase of gait (i.e. the first 200 ms of stance). In order to evaluate the group differences in the initial contact position of the tibiofemoral joint, the AP and ML position values were normalized to the AP and ML dimensions of the tibial plateau to account for individual variations in anthropometrics. In addition, joint excursions were defined as the difference between the maximum and minimum values for each variable within the loading response phase of gait. A one-way analysis of variance with post hoc Bonferroni adjustments were used to determine the statistically significant group differences for each variable of interest (Stata 11, StataCorp LP, College Station, USA). Level of significance was set at p < 0.05.
3. RESULTS
3.1. Alignment at Initial Contact
Knee flexion angle at initial contact was similar between groups (Table 2, Figure 1). However, significant differences in coronal plane motion were found between groups. The medial and lateral knee OA group demonstrated a more abducted alignment (mean (SD), 3.8 (3.2)°) compared to the control group (mean (SD), -0.8 (1.9)°; p < 0.01) and the medial knee OA group (mean (SD), -2.8 (2.5)°; p < 0.01) who demonstrated a more adducted alignment (Table 2, Figure 2). Transverse plane position of the tibiofemoral joint was also significantly different between groups at initial contact. The medial and lateral knee OA group demonstrated a more internally rotated alignment (mean (SD), 4.0 (4.1)°) compared to the control group (mean (SD), -4.4 (7.2)°; P < 0.05) and the medial knee OA group (mean (SD), -4.8 (8.7)°; p < 0.05) who demonstrated a more externally rotated alignment (Table 2, Figure 3). Finally, the normalized AP and ML position of the tibia with respect to the femur were similar between all 3 groups at initial contact (Table 2, Figures 4-5).
Table 2.
Means and standard deviations for the knee alignment at initial contact and the total joint excursions for rotations and translations during the loading phase of gait.
| Control No OA (n = 12) | Medial Knee OA (n = 7) | Medial & Lateral Knee OA (n = 7) | |
|---|---|---|---|
| Flexion (angle) | |||
| Initial Contact (degrees) | 3.3 (3.7) | 6.7(8.0) | 7.4 (5.9) |
| Joint Excursion (degrees) | 17.4 (4.7) | 9.7 (3.4)* | 9.3 (4.9)* |
| Abduction (+) /Adduction (-) | |||
| Initial Contact (degrees) | -0.8 (1.9) | -2.8 (2.5) | 3.8 (3.2)*† |
| Joint Excursion (degrees) | -1.0 (0.5) | -2.2 (0.7)* | 1.9 (1.1)* |
| Internal Rotation (+) /External Rotation (-) | |||
| Initial Contact (degrees) | -4.4 (7.2) | -4.8 (8.7) | 4.0 (4.1)*† |
| Joint Excursion (degrees) | 7.4 (2.2) | 4.7 (1.2)* | 3.1 (0.9)* |
| Anterior Translation (+) / Posterior Translation (-) | |||
| Initial Contact†† | -0.01 (0.1) | 0.01 (0.1) | 0.05 (0.1) |
| Joint Excursion (mm) | 3.4 (0.9) | 3.4 (1.2) | 3.4 (1.2) |
| Lateral Translation (+) / Medial Translation (-) | |||
| Initial Contact†† | 0.03 (0.02) | 0.04 (0.03) | 0.06 (0.04) |
| Joint Excursion (mm) | -1.2 (0.7) | 1.2 (0.3) | -1.1 (0.6) |
Significantly different than the control group (p < 0.05)
Significantly different than the Medial OA group (p < 0.05)
Antroposterior and mediolateral joint positions at initial contact are reported as normalized values with respect to the tibial plateau dimensions in the corresponding plane.
Figure 1.
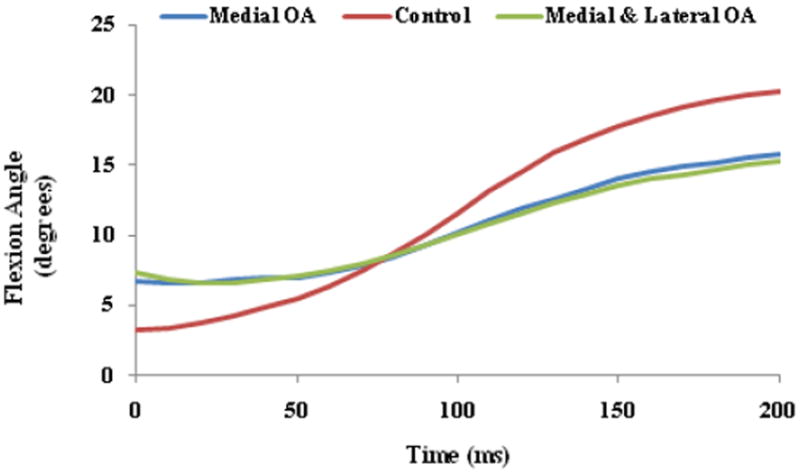
Ensemble average sagittal plane tibiofemoral rotations during the loading response phase of gait.
Figure 2.
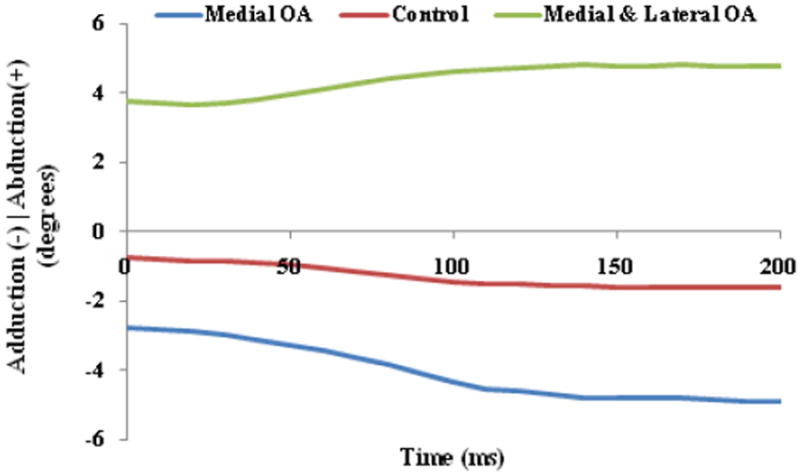
Ensemble average coronal plane tibiofemoral rotations during the loading response phase of gait.
Figure 3.
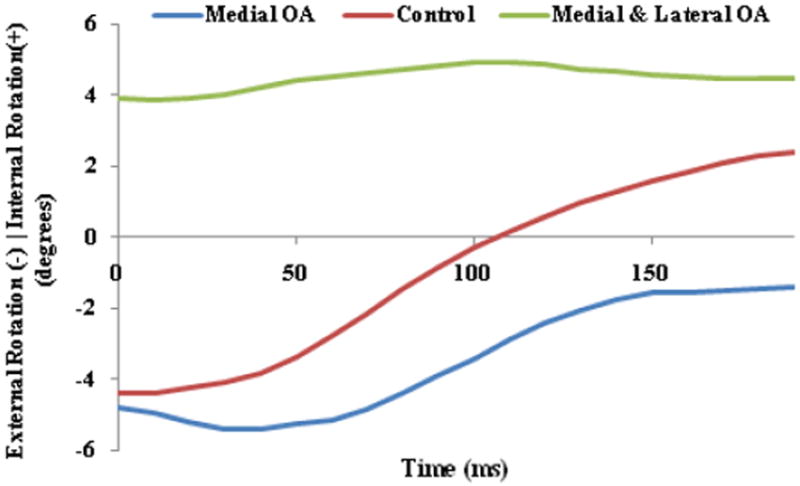
Ensemble average transverse plane tibiofemoral rotations during the loading response phase of gait.
Figure 4.
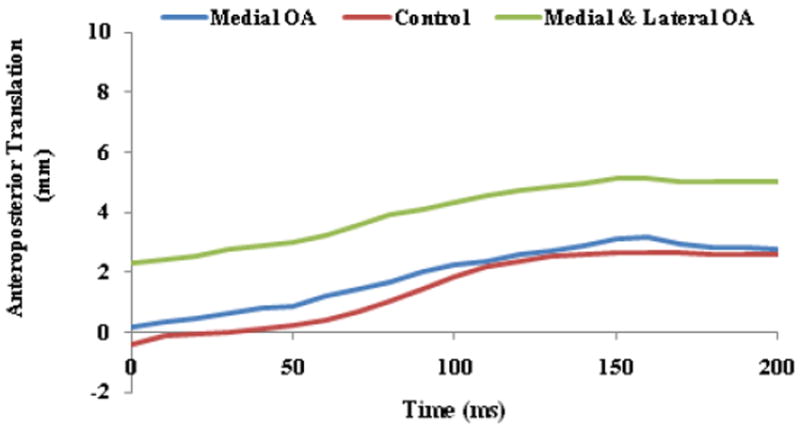
Ensemble average anteroposterior tibiofemoral translation during the loading response phase of gait.
Figure 5.
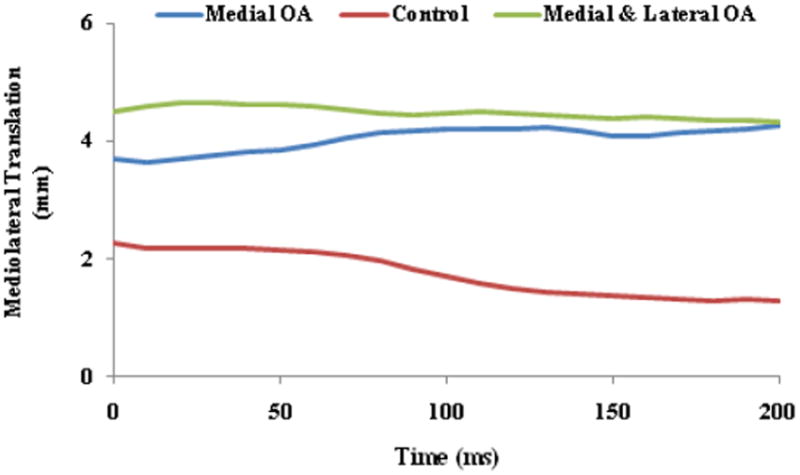
Ensemble average mediolateral tibiofemoral translation during the loading response phase of gait.
3.2. Joint Excursions
The total tibiofemoral joint flexion excursion (Table 2, Figure 1) was significantly greater for the control group (mean (SD), 17.4 (4.7)°) compared to the medial OA group (mean (SD), 9.7 (3.4)°; p < 0.01) and the medial and lateral OA group (mean (SD), 9.3 (4.9)°; p < 0.01). Conversely, the control group demonstrated a decreased pattern of coronal plane joint excursion (mean (SD), -1.0 (0.5)°) compared to the medial knee OA group (mean (SD), -2.2 (0.7)°; p < 0.01) who moved into more adduction as well as the medial and lateral knee OA group (mean (SD), 1.9 (1.1)°; p < 0.05) who moved into more abduction (Table 2, Figure 2). Similar to the pattern demonstrated for flexion, the control group also demonstrated higher tibiofemoral joint excursions in the transverse plane (mean (SD), 7.4 (2.2)°) compared to the medial knee OA group (mean (SD), 4.7 (1.2)°; p < 0.01) who moved into less external rotation and the medial and lateral knee OA group (mean (SD), 3.1 (0.9)°; p < 0.01) who remained internally rotated (Table 2, Figure 3). However, the AP and ML displacement excursions were similar between all groups (Table 2, Figures 4-5).
4. DISCUSSION
The purpose of this study was to evaluate whether individuals with concurrent knee OA and complaints of joint instability exhibit different knee joint kinematics during the loading response phase of gait compared to individuals with healthy, asymptomatic knees. For the purposes of this study, knee instability was defined as episodic reports of knee giving way, buckling, or shifting that adversely affected the participant’s ability to perform weight-bearing functional tasks (Fitzgerald et al., 2004). Consistent with our original hypothesis, our results indicate that individuals with knee OA and reports of joint instability demonstrate significant reductions in their sagittal and transverse plane rotational knee joint excursions. On average, individuals with concurrent knee OA and joint instability in the current study exhibited approximately 45% less knee flexion and 47% less transverse plane rotation arc of motion during the loading response phase of gait compared to the control group (Table 2; Figures 1 and 3). It is conceivable that the decreased rotational joint motion may represent a compensatory attempt to avoid pain and/or to stabilize an unstable knee joint during the loading response phase of gait (Childs et al., 2004). However, this movement strategy may be problematic in the long term as it may lead to increased compressive loading and reduction of the shock absorption capabilities of the joint (Childs et al., 2004, Messier et al., 1992, Mundermann et al., 2005). Additionally, reduced sagittal and transverse plane motion of the tibiofemoral joint may also interfere with the ability of the knee joint to distribute the contact forces over a greater area which may in turn contribute to cumulative localized loading and an increased rate of disease progression. It is also interesting to note that individuals with both medial and lateral compartment involvement demonstrated the least amount of sagittal and transverse plane rotational joint excursions in comparison to the control group and those with uni-compartmental disease. Therefore, compartmental distribution of the disease may be associated with specific patterns of altered rotational knee joint motion.
On the other hand, inconsistent with our original hypothesis, individuals with concurrent knee OA and instability exhibited an increased amount of rotational knee joint excursion in the coronal plane compared to those in the control group. Whereas individuals in the medial OA group exhibited an average 2.8° increase in knee adduction, those in the medial and lateral knee OA group moved into more abduction by an average of 1.9° during the loading response phase of gait (Figure 2). It is plausible that the malalignment of the tibiofemoral joint at initial contact may have predisposed the knee joint to these movement patterns. More specifically, if the tibiofemoral joint was in an adducted position at initial contact, then this knee malalignment became accentuated in the corresponding direction throughout the loading response phase of gait. Similarly, if the tibiofemoral joint was in an abducted position at initial contact, then the knee joint became more abducted throughout the loading phase of gait. In comparison, with an average 1.0° of coronal plane rotational arc of motion, the control group maintained a near neutral alignment throughout the loading response phase of gait. As normal gait pattern is associated with minimal coronal plane motion (Perry, 1992), the functional consequence of this dynamic alignment change is an alteration in the normal angle of force transmission in the knee joint (Englund, 2010) and a change in joint forces and moments in the corresponding motion planes (Teixeira and Olney, 1996). Such characteristic change in dynamic alignment could in turn lead to compartment-specific patterns of disease progression and cartilage breakdown. The notion of accelerated knee OA progression in presence of dynamic coronal plane knee malalignment is supported by the work of Astephen and Deluzio (Astephen and Deluzio, 2005) who suggested that the most discriminating principal component of severe knee OA gait pattern is represented by a coronal plane change in alignment during the stance phase of the gait cycle.
Contrary to our hypothesis, individuals with concurrent knee OA and complaints of joint instability demonstrated similar knee joint arthrokinematics compared to our control group. This finding was unexpected as we had hypothesized that reported history of knee instability would be associated with excessive translatory motion of the tibiofemoral joint during the performance of a functional activity. This hypothesis was based on the premise that joint laxity resulting from reduced tension in the joint capsule and ligaments of the knee that occur due to progressive degenerative changes would make the joint more vulnerable to excessive translations during the increasing stability demands of declined gait (Sharma et al., 1999). However, the AP and ML position of the tibia with respect to the femur at initial contact and the excursions of the joints in the associated motion planes were similar between all three groups. As the current study only evaluated knee arthrokinematics during a single task of declined gait, the possibility of excessive translatory motion cannot be completely ruled out for other high demanding activities such as stair climbing. In addition, as no episodes of instability were reported during data collection, we are unable to comment on whether knee joint arthokinematics may differ during an actual episode of instability compared to a period without instability. Therefore, these interesting findings should be further substantiated in future research attempts under different experimental conditions.
As we did not observe excessive joint translations in our cohort, it could be possible that other factors such as momentary inhibition of the quadriceps muscle or altered neuromuscular control could be responsible for the reported isolated episodes of knee instability in this patient population. Muscle activity is critical in determining the mechanical stiffness and dynamic stability of diarthrodial joints (Sharma and Pai, 1997). In fact, it is plausible that increased co-contraction of agonist and antagonist muscles crossing the knee joint may have been responsible for the absence of the hypothesized excessive knee joint translations in our subjects with reports of episodic knee instability. However, if muscle contractions are not properly coordinated, the joint could exceed its boundaries of normal motion (O’Connor and Brandt, 1993) and as a result an instantaneous episode of instability could be perceived. As joint stability depends in part on sensory proprioceptive input and an appropriate motor output (Hurley and Newham, 1993), factors that can influence the dynamics of the neuromuscular system could play a role in making the knee joint vulnerable to momentary episodes of instability. For instance, episodic exacerbation of joint symptoms due to pain can lead to significant reflex inhibition and restriction of proper activation of the musculature surrounding the knee joint (so-called arthrogenous muscle inhibition) (Hopkins et al., 2001, Palmieri-Smith et al., 2007). Altered knee joint mechanics resulting from momentary arthrogenous muscle inhibition may in turn render the joint unstable during high demands of various functional activities. In addition, acute impairments in the ability to exert force or power such as those reported for neuromuscular fatigue could also play a role in episodic knee instability (Allman and Rice, 2002). However, since we did not monitor muscle activation patterns or strength in our study, future efforts should evaluate the potential role of muscle inhibition and altered neuromuscular function in individuals with concurrent knee OA and reports of instability.
It is important to note that the altered patterns of tibiofemoral joint rotational motion reported in the current study are similar to what has previously been established for individuals with knee OA without reports of joint instability. For instance, Childs and colleague (Childs et al., 2004) reported that knee flexion is reduced by 4-6° during the loading phase of gait in individuals with knee OA compared to age and gender matched control subjects. In addition, coronal plane findings for our medial knee OA group is very similar to those reported by Gok and colleagues (Gok et al., 2002) who reported an increased dynamic varus malalignment during the loading response phase of gait in individuals with medial knee OA. Therefore, it could be argued that the kinematic differences reported in the current study may be indicative of characteristic gait adaptations due to knee OA rather than joint instability. Thus, a limitation of the current study is that the exact contribution of either knee OA or joint instability to the reported alterations in knee joint kinematics cannot be readily elucidated. To fully understand the potential mechanisms responsible for episodes of knee joint instability, future research efforts should consider evaluating the kinematic differences in OA knees between individual with and without reports of instability. However, from a clinical perspective, if the ultimate goal of a rehabilitation program is to restore normal joint mechanics, it could be argued that an appropriate intervention strategy for this patient population would be one resulting in modification of the altered knee joint kinematics towards a pattern demonstrated by the control group. Alternatively, as these kinematic alterations could potentially be compensatory mechanisms for improving joint stability or reducing symptoms, it is unclear whether improving knee joint kinematics would lead to better patient-related outcomes. Thus, it is also plausible that a more successful intervention may be one that assists the natural compensation strategy used by patients. Further research is needed to clarify whether different treatment strategies should be considered for knee OA in individuals with and without complaints of instability.
An additional limitation of this investigation is our small sample size. We fully acknowledge that the low power of the current study limits our ability to formulate clear-cut conclusions. However, the large standard deviations of the tibiofemoral joint rotational data and the similarities in the tibiofemoral translations reported for our small cohort may indicate that detecting differences may be unlikely unless a very large sample size is used. In addition, reports of joint instability in presence of knee OA is most likely a multi-factorial problem that may be the result of factors such as increased capsuloligamentous laxity, structural damage to the knee, and altered lower extremity muscular strength and neuromuscular control (Fitzgerald et al., 2004). Therefore, future investigations should also consider the potential role of these factors and their possible interactions in influencing knee joint mechanics in individuals with concurrent knee OA and joint instability.
5. CONCLUSIONS
Consistent with previous reports of altered tibiofemoral joint kinematics reported for Individuals with knee OA, our cohort of subjects with concurrent knee OA and reports of joint instability demonstrated significantly reduced flexion and internal/external rotational knee motion excursions during the loading response phase of declined gait while the abduction/adduction motion excursions were increased. Additionally, subjects with concurrent knee OA and joint instability also demonstrated altered coronal and transverse plane knee alignments at initial contact. However, the AP and ML tibiofemoral joint alignments at initial contact and the corresponding total joint translations during the loading response phase of declined gait were not altered. This is the first study to report that perceived episodic joint instability in individuals with knee OA may not necessarily be associated with adaptive changes in knee joint arthrokinematics. However, the possibility of excessive translatory motion of the tibiofemoral joint in presence of concurent knee OA and joint instability cannot be completely ruled out. Further research is needed to determine if reductions in passive joint stability, altered neuromuscular control, or a combination of the two are associated with subjective complaints of episodic knee joint instability in individuals with OA.
Acknowledgments
This publication was made possible by Grant Number 1 UL1 RR024153 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NCRR or NIH. Information on NCRR is available at http://www.ncrr.nih.gov/. Information on Re-engineering the Clinical Research Enterprise can be obtained from http://nihroadmap.nih.gov/clinicalresearch/overview-translational.asp. The funding source had no role in the study design, data collection, analysis or writing of this manuscript.
This study was approved by the Health Sciences Institutional Review Board, University of Pittsburgh, Pittsburgh, PA, USA.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- AKBARSHAHI M, SCHACHE AG, FERNANDEZ JW, BAKER R, BANKS S, PANDY MG. Non-invasive assessment of soft-tissue artifact and its effect on knee joint kinematics during functional activity. J Biomech. 2010;43:1292–301. doi: 10.1016/j.jbiomech.2010.01.002. [DOI] [PubMed] [Google Scholar]
- ALLMAN BL, RICE CL. Neuromuscular fatigue and aging: central and peripheral factors. Muscle Nerve. 2002;25:785–96. doi: 10.1002/mus.10116. [DOI] [PubMed] [Google Scholar]
- ALTMAN R, ALARCON G, APPELROUTH D, BLOCH D, BORENSTEIN D, BRANDT K, BROWN C, COOKE TD, DANIEL W, FELDMAN D, et al. The American College of Rheumatology criteria for the classification and reporting of osteoarthritis of the hip. Arthritis Rheum. 1991;34:505–14. doi: 10.1002/art.1780340502. [DOI] [PubMed] [Google Scholar]
- AMIN S, GUERMAZI A, LAVALLEY MP, NIU J, CLANCY M, HUNTER DJ, GRIGORYAN M, FELSON DT. Complete anterior cruciate ligament tear and the risk for cartilage loss and progression of symptoms in men and women with knee osteoarthritis. Osteoarthritis Cartilage. 2008;16:897–902. doi: 10.1016/j.joca.2007.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ANDERST W, ZAUEL R, BISHOP J, DEMPS E, TASHMAN S. Validation of three-dimensional model-based tibio-femoral tracking during running. Med Eng Phys. 2009;31:10–6. doi: 10.1016/j.medengphy.2008.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ANDRIACCHI TP, MUNDERMANN A, SMITH RL, ALEXANDER EJ, DYRBY CO, KOO S. A framework for the in vivo pathomechanics of osteoarthritis at the knee. Ann Biomed Eng. 2004;32:447–57. doi: 10.1023/b:abme.0000017541.82498.37. [DOI] [PubMed] [Google Scholar]
- ASTEPHEN JL, DELUZIO KJ. Changes in frontal plane dynamics and the loading response phase of the gait cycle are characteristic of severe knee osteoarthritis application of a multidimensional analysis technique. Clin Biomech (Bristol, Avon) 2005;20:209–17. doi: 10.1016/j.clinbiomech.2004.09.007. [DOI] [PubMed] [Google Scholar]
- BERTHIAUME MJ, RAYNAULD JP, MARTEL-PELLETIER J, LABONTE F, BEAUDOIN G, BLOCH DA, CHOQUETTE D, HARAOUI B, ALTMAN RD, HOCHBERG M, MEYER JM, CLINE GA, PELLETIER JP. Meniscal tear and extrusion are strongly associated with progression of symptomatic knee osteoarthritis as assessed by quantitative magnetic resonance imaging. Ann Rheum Dis. 2005;64:556–63. doi: 10.1136/ard.2004.023796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CHILDS JD, SPARTO PJ, FITZGERALD GK, BIZZINI M, IRRGANG JJ. Alterations in lower extremity movement and muscle activation patterns in individuals with knee osteoarthritis. Clin Biomech (Bristol, Avon) 2004;19:44–9. doi: 10.1016/j.clinbiomech.2003.08.007. [DOI] [PubMed] [Google Scholar]
- ENGLUND M. The role of biomechanics in the initiation and progression of OA of the knee. Best Pract Res Clin Rheumatol. 2010;24:39–46. doi: 10.1016/j.berh.2009.08.008. [DOI] [PubMed] [Google Scholar]
- ETTINGER WH, DAVIS MA, NEUHAUS JM, MALLON KP. Long-term physical functioning in persons with knee osteoarthritis from NHANES. I: Effects of comorbid medical conditions. J Clin Epidemiol. 1994;47:809–15. doi: 10.1016/0895-4356(94)90178-3. [DOI] [PubMed] [Google Scholar]
- FELSON DT, LAWRENCE RC, DIEPPE PA, HIRSCH R, HELMICK CG, JORDAN JM, KINGTON RS, LANE NE, NEVITT MC, ZHANG Y, SOWERS M, MCALINDON T, SPECTOR TD, POOLE AR, YANOVSKI SZ, ATESHIAN G, SHARMA L, BUCKWALTER JA, BRANDT KD, FRIES JF. Osteoarthritis: new insights. Part 1: the disease and its risk factors. Ann Intern Med. 2000;133:635–46. doi: 10.7326/0003-4819-133-8-200010170-00016. [DOI] [PubMed] [Google Scholar]
- FELSON DT, NAIMARK A, ANDERSON J, KAZIS L, CASTELLI W, MEENAN RF. The prevalence of knee osteoarthritis in the elderly. The Framingham Osteoarthritis Study. Arthritis Rheum. 1987;30:914–8. doi: 10.1002/art.1780300811. [DOI] [PubMed] [Google Scholar]
- FELSON DT, ZHANG Y, HANNAN MT, NAIMARK A, WEISSMAN BN, ALIABADI P, LEVY D. The incidence and natural history of knee osteoarthritis in the elderly. The Framingham Osteoarthritis Study. Arthritis Rheum. 1995;38:1500–5. doi: 10.1002/art.1780381017. [DOI] [PubMed] [Google Scholar]
- FITZGERALD GK, PIVA SR, IRRGANG JJ. Reports of joint instability in knee osteoarthritis: its prevalence and relationship to physical function. Arthritis Rheum. 2004;51:941–6. doi: 10.1002/art.20825. [DOI] [PubMed] [Google Scholar]
- GOK H, ERGIN S, YAVUZER G. Kinetic and kinematic characteristics of gait in patients with medial knee arthrosis. Acta Orthop Scand. 2002;73:647–52. doi: 10.1080/000164702321039606. [DOI] [PubMed] [Google Scholar]
- GUCCIONE AA, FELSON DT, ANDERSON JJ, ANTHONY JM, ZHANG Y, WILSON PW, KELLY-HAYES M, WOLF PA, KREGER BE, KANNEL WB. The effects of specific medical conditions on the functional limitations of elders in the Framingham Study. Am J Public Health. 1994;84:351–8. doi: 10.2105/ajph.84.3.351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HOPKINS JT, INGERSOLL CD, KRAUSE BA, EDWARDS JE, CORDOVA ML. Effect of knee joint effusion on quadriceps and soleus motoneuron pool excitability. Med Sci Sports Exerc. 2001;33:123–6. doi: 10.1097/00005768-200101000-00019. [DOI] [PubMed] [Google Scholar]
- HURLEY MV, NEWHAM DJ. The influence of arthrogenous muscle inhibition on quadriceps rehabilitation of patients with early, unilateral osteoarthritic knees. Br J Rheumatol. 1993;32:127–31. doi: 10.1093/rheumatology/32.2.127. [DOI] [PubMed] [Google Scholar]
- KELLGREN JH, LAWRENCE JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MESSIER SP, LOESER RF, HOOVER JL, SEMBLE EL, WISE CM. Osteoarthritis of the knee: effects on gait, strength, and flexibility. Arch Phys Med Rehabil. 1992;73:29–36. [PubMed] [Google Scholar]
- MUNDERMANN A, DYRBY CO, ANDRIACCHI TP. Secondary gait changes in patients with medial compartment knee osteoarthritis: increased load at the ankle, knee, and hip during walking. Arthritis Rheum. 2005;52:2835–44. doi: 10.1002/art.21262. [DOI] [PubMed] [Google Scholar]
- MURAKI S, OKA H, AKUNE T, MABUCHI A, EN-YO Y, YOSHIDA M, SAIKA A, SUZUKI T, YOSHIDA H, ISHIBASHI H, YAMAMOTO S, NAKAMURA K, KAWAGUCHI H, YOSHIMURA N. Prevalence of radiographic knee osteoarthritis and its association with knee pain in the elderly of Japanese population-based cohorts: the ROAD study. Osteoarthritis Cartilage. 2009;17:1137–43. doi: 10.1016/j.joca.2009.04.005. [DOI] [PubMed] [Google Scholar]
- NAGAO N, TACHIBANA T, MIZUNO K. The rotational angle in osteoarthritic knees. Int Orthop. 1998;22:282–7. doi: 10.1007/s002640050261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’CONNOR BL, BRANDT KD. Neurogenic factors in the etiopathogenesis of osteoarthritis. Rheum Dis Clin North Am. 1993;19:581–605. [PubMed] [Google Scholar]
- PALMIERI-SMITH RM, KREINBRINK J, ASHTON-MILLER JA, WOJTYS EM. Quadriceps inhibition induced by an experimental knee joint effusion affects knee joint mechanics during a single-legged drop landing. Am J Sports Med. 2007;35:1269–75. doi: 10.1177/0363546506296417. [DOI] [PubMed] [Google Scholar]
- PERRY J. Gait analysis: normal and pathological function. Thorofare, N.J.: SLACK inc; 1992. [Google Scholar]
- SCHIPPLEIN OD, ANDRIACCHI TP. Interaction between active and passive knee stabilizers during level walking. J Orthop Res. 1991;9:113–9. doi: 10.1002/jor.1100090114. [DOI] [PubMed] [Google Scholar]
- SHARMA L, LOU C, CAHUE S, DUNLOP DD. The mechanism of the effect of obesity in knee osteoarthritis: the mediating role of malalignment. Arthritis Rheum. 2000;43:568–75. doi: 10.1002/1529-0131(200003)43:3<568::AID-ANR13>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- SHARMA L, LOU C, FELSON DT, DUNLOP DD, KIRWAN-MELLIS G, HAYES KW, WEINRACH D, BUCHANAN TS. Laxity in healthy and osteoarthritic knees. Arthritis Rheum. 1999;42:861–70. doi: 10.1002/1529-0131(199905)42:5<861::AID-ANR4>3.0.CO;2-N. [DOI] [PubMed] [Google Scholar]
- SHARMA L, PAI YC. Impaired proprioception and osteoarthritis. Curr Opin Rheumatol. 1997;9:253–8. doi: 10.1097/00002281-199705000-00013. [DOI] [PubMed] [Google Scholar]
- SHARMA L, SONG J, FELSON DT, CAHUE S, SHAMIYEH E, DUNLOP DD. The role of knee alignment in disease progression and functional decline in knee osteoarthritis. JAMA. 2001;286:188–95. doi: 10.1001/jama.286.2.188. [DOI] [PubMed] [Google Scholar]
- TASHMAN S, ANDERST W. In-vivo measurement of dynamic joint motion using high speed biplane radiography and CT: application to canine ACL deficiency. J Biomech Eng. 2003;125:238–45. doi: 10.1115/1.1559896. [DOI] [PubMed] [Google Scholar]
- TASHMAN S, KOLOWICH P, COLLON D, ANDERSON K, ANDERST W. Dynamic function of the ACL-reconstructed knee during running. Clin Orthop Relat Res. 2007;454:66–73. doi: 10.1097/BLO.0b013e31802bab3e. [DOI] [PubMed] [Google Scholar]
- TEIXEIRA LF, OLNEY SJ. Relationship between alignment and kinematic and kinetic measures of the knee of osteoarthritic elderly subjects in level walking. Clin Biomech (Bristol, Avon) 1996;11:126–134. doi: 10.1016/0268-0033(95)00057-7. [DOI] [PubMed] [Google Scholar]
- YAGI T. Tibial torsion in patients with medial-type osteoarthrotic knees. Clin Orthop Relat Res. 1994:52–6. [PubMed] [Google Scholar]
- YAGI T, SASAKI T. Tibial torsion in patients with medial-type osteoarthritic knee. Clin Orthop Relat Res. 1986:177–82. [PubMed] [Google Scholar]
- YANG N, NAYEB-HASHEMI H, CANAVAN PK. The combined effect of frontal plane tibiofemoral knee angle and meniscectomy on the cartilage contact stresses and strains. Ann Biomed Eng. 2009;37:2360–72. doi: 10.1007/s10439-009-9781-3. [DOI] [PubMed] [Google Scholar]
- YOU BM, SIY P, ANDERST W, TASHMAN S. In vivo measurement of 3-D skeletal kinematics from sequences of biplane radiographs: application to knee kinematics. IEEE Trans Med Imaging. 2001;20:514–25. doi: 10.1109/42.929617. [DOI] [PubMed] [Google Scholar]


