Abstract
Osteoporosis is a major health problem worldwide, and is projected to increase exponentially due to the aging of the population. The absolute fracture risk in individual subjects is calculated by the use of algorithms which include bone mineral density (BMD), age, gender, history of prior fracture and other risk factors. This review describes the laboratory investigations into osteoporosis which include serum calcium, phosphate, creatinine, alkaline phosphatase and 25-hydroxyvitamin D and, additionally in men, testosterone. Parathyroid hormone (PTH) is measured in patients with abnormal serum calcium to determine its cause. Other laboratory investigations such as thyroid function testing, screening for multiple myeloma, and screening for Cushing's syndrome, are performed if indicated. Measurement of bone turnover markers (BTMs) is currently not included in algorithms for fracture risk calculations due to the lack of data. However, BTMs may be useful for monitoring osteoporosis treatment. Further studies of the reference BTMs serum carboxy terminal telopeptide of collagen type I (s-CTX) and serum procollagen type I N-terminal propeptide (s-PINP) in fracture risk prediction and in monitoring various treatments for osteoporosis may help expedite their inclusion in routine clinical practice.
Keywords: Osteoporosis, Bisphosphonates, Bone turnover markers, Fracture risk, Monitoring treatment
INTRODUCTION
Osteoporosis is defined as "a disease characterised by low bone mass and microarchitectural deterioration of bone tissue, leading to enhanced bone fragility and consequent increase in fracture risk" [1]. The WHO's diagnostic criterion for osteoporosis is a bone mineral density (BMD) measurement equal to or more than 2.5 SD below the young female (age 20-29 yr) reference mean (T-score ≤-2.5 SD) [2]. Borderline decrease in BMD (T score between -1.0 and -2.5) is designated as osteopenia. Osteoporosis is a silent disease and the health and economic impact of the disease result from fracture, for which subjects with osteoporosis are at an increased risk. Fracture of the femoral neck in the elderly has the most serious consequences. For example, in Korea, hip fractures cause major morbidity and mortality, with long term loss of mobility in half of such patients, 25% of patients requiring long term care and 11-17% of patients dying within a year [3-6]. The direct costs of medical care of hip fractures were over $65 million in 2004 [3].
The impact of osteoporosis is projected to increase exponentially due to the aging of the population. For example, in Korea, 7.2% of the population was aged >65 yr in 2000, but this is expected to double to 15.7% by 2020 [7]. The worldwide incidence of osteoporotic fractures in 2000 was estimated at nine million, with hip fractures contributing 1.6 million [8]. By 2050, the number of hip fractures worldwide is projected to increase to 6.3 million if fracture rates remain constant [9]. However, age-specific fracture rates seem to have reached a plateau or may even be decreasing in some parts of North America, Europe and Australia, while they seem to continue to increase in Asia where current fracture rates are lower than in western countries and contribute about 30% of hip fractures worldwide [8]. Asia is projected to contribute 50% of hip fractures worldwide by 2050 [9]. In Korea, the number of hip fractures in women over 50 yr of age was 250.9/100,000 persons in 2001 and increased by nearly 5% in 3 yr to 262.8/100,000 in 2004 although in men the rate decreased by over 15% from 162.8/100,000 in 2001 to 137.5/100,000 in 2004 [3].
Although BMD is used in the diagnosis of osteoporosis, a low BMD is not the only risk factor for fractures, but is in fact an inefficient tool by itself for identifying those at high risk of fractures. For example, at a population level, more fractures occur in those with osteopenia than in those with osteoporosis simply because there are a much larger number of people with osteopenia than with osteoporosis. Therefore, in selecting patients for treatment, the risk of fracture in individual subjects is now calculated by the use of algorithms which include a number of recognized independent risk factors for fracture in addition to BMD, such as age, sex, body mass index, family history, past history of fracture, secondary causes of osteoporosis such as rheumatoid arthritis, use of medications such as glucocorticoids, smoking and excessive alcohol intake [10]. FRAX® (WHO Fracture risk assessment tool) is such a fracture risk calculator that is freely accessible on the web (www.shef.ac.uk/FRAX/). Since fracture risk varies by ethnicity and/or country of residence, epidemiological data from various countries have been used to provide country-specific fracture risk. Where country-specific data are unavailable, surrogate data may be used. For example, a recent study has suggested that the fracture risk calculation based on Japanese data in the FRAX® calculator might be the most appropriate for Korean women [11].
Although bone turnover predicts fracture independently of BMD, bone turnover markers (BTMs) are not included in the fracture risk calculator (FRAX®) for the following reasons. Several studies have looked at various BTMs and their contribution to fracture risk, but the results of these studies have been inconsistent, not the least due to the use of different markers and different methodologies for their assessment [12-20]. This has led to the recommendation for the standardization of BTM measurements in future studies with the use of serum carboxy terminal telopeptide of collagen type I (s-CTX) as the standard bone resorption marker and serum procollagen type I N-terminal propeptide (s-PINP) as the standard bone formation marker [21]. Most of the positive results with BTMs were for bone resorption markers, with increased resorption marker predicting an increased fracture risk [12-20]. Whilst BTMs predict fracture risk independently of BMD, their relationships to other established risk factors included in the risk calculator need to be clarified. For example, prior fracture is a risk factor for future fractures, and is included in the risk calculator. Fracture leads to an increase in BTMs which is evident even 6 months after the event [22]; bone formation markers may remain raised even at 52 weeks [23], while resorption markers generally return baseline by then [24]. Some of the secondary causes of osteoporosis included in the risk calculator, such as glucocorticoid use and rheumatoid arthritis, can also lead to changes in BTMs. Glucocorticoid treatment leads to a decrease in the bone formation marker osteocalcin and an increase in bone resorption markers [24]. In untreated rheumatoid arthritis, bone resorption markers increase, with patients with active disease having higher levels than patients with non-active disease [25]. Other conditions associated with osteoporosis such as primary hyperparathyroidism and thyrotoxicosis, are also associated with increased bone turnover. Therefore, the extent to which BTMs predict fracture risk independently of those risk factors needs to be defined before BTMs can be included appropriately in fracture risk calculators.
LABORATORY INVESTIGATIONS IN OSTEOPOROSIS
Laboratory investigations in patients with osteoporosis are undertaken to rule out or to detect common causes of osteoporosis in order to treat them. Further targeted investigations may be performed if indicated by clinical presentation, or if the first line investigations are normal but the severity of osteoporosis is unusual for the age and gender. The following first-line measurements may be routinely indicated in the investigation of patients with osteoporosis [26]: Serum total calcium, albumin (to calculate albumin adjusted calcium) and phosphate to detect conditions associated with hypercalcemia such as primary hyperparathyroidism or hypocalcemia and consequent secondary hyperparathyroidism causing bone loss; although albumin adjustment for serum calcium is not universally performed, this practice may be useful to correct total calcium measurements skewed by abnormal albumin levels. Alternatively, ionized calcium measurement gives a more accurate measure of calcium homeostasis. Serum creatinine and estimated glomerular filtration rate (GFR) are useful to detect renal failure which can affect bone health. Serum alkaline phosphatase (ALP) measurement is useful to detect conditions including Paget's disease, metastatic bone disease and osteomalacia, etc. Total ALP is adequate for demonstrating gross increases in bone formation such as those found in most patients with active Paget's disease, osteomalacia, fracture healing or metastatic bone disease, but is not sensitive enough to detect changes in bone remodeling seen in most cases of uncomplicated osteoporosis. Although gamma-glutamyl transpeptidase (GGT) is suggested by some to distinguish an increase in liver ALP from bone ALP, this is neither sensitive nor specific for this purpose. If changes in bone formation need to be determined with sensitivity, or distinguished from an increase in total ALP due to liver disease, a specific bone formation marker such as PINP could be measured.
Vitamin D nutrition should be determined by measuring serum 25-hydroxy vitamin D [25(OH)D]. Although there is controversy about the optimum level of 25(OH)D for bone health; while 50 nmol/L is considered acceptable, others have suggested 75 nmol/L as desirable for optimum bone health [27, 28]. If the higher cut-off is used, then the vast majority of menopausal women (76.8%) would be considered to have sub-optimal vitamin D nutrition [28]. A reference interval study performed in one of the authors' laboratory in Seoul showed that the central 95th percentile of 25(OH) D levels in a healthy population above 40 yr of age was 25-70 nmol/L (unpublished data, Lee JH). Others have found that 22% of postmenopausal Korean women have a 25(OH)D level <50 nmol/L [29]. 25(OH)D levels decrease in winter due to a reduction in sun exposure; Park et al. have reported that the mean serum 25(OH)D of Korean postmenopausal women during wintertime was 30.5 nmol/L [30], and So et al. found that the prevalence of serum 25(OH)D <50 nmol/L, during wintertime was 90.1% [31]. Therefore we suggest that 50 nmol/L, recommended by the US Institute of Medicine [27], is a more realistic and attainable goal than a higher level for serum 25(OH)D. Current automated assays for 25(OH)D have been associated with analytical problems including method related bias. Therefore properly standardized liquid chromatography (LC)/mass spectrometry (MS) is the desirable method for measuring 25(OH)D [32].
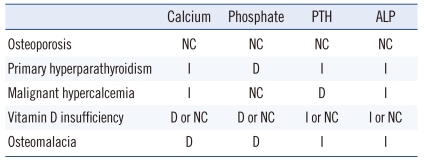
PTH measurement would be required if serum calcium is abnormal, to help investigate the cause of the calcium abnormality (Table 1). Appropriate sample handling is important for PTH measurement [33]. A full examination of blood and erythrocyte sedimentation rate (ESR) would be useful for general health and for inflammatory diseases which often increase bone loss. Serum protein electrophoresis and free light chains in older patients would be useful to exclude multiple myeloma which causes major bone loss. Other secondary causes such as thyrotoxicosis can be excluded with thyroid function tests, and in men hypogonadism is screened with a serum testosterone. In women, the diagnosis of menopause is made clinically and does not warrant estradiol measurement. If Cushing's syndrome is suggested clinically, then screening tests could be performed: 24 hr urine cortisol, midnight salivary cortisol or overnight dexamethasone suppression test. Rarer conditions, if suspected, could be specifically tested; e.g. celiac disease (which is commonly seen in people of European ancestry, but also in parts of Africa, the Middle East and South Asia) with tissue transglutaminase antibody (together with IgA) or systemic mastocytosis with serum tryptase and/or urine methyl histamine. BTMs are not routinely recommended for the assessment of osteoporosis for the reasons stated above. However, if treatment for osteoporosis is to be initiated and monitoring with BTMs is intended, baseline measurement of fasting morning s-CTX and/or s-PINP may be undertaken.
Table 1.
Biochemical changes in bone diseases
Abbreviations: NC, not changed; I, increased; D, decreased; PTH, parathyroid hormone; ALP, alkaline phosphatase.
1. Measurement of BTMs
1) s-CTX
The reference bone resorption marker is s-CTX. The antibody used in immunoassays for CTX in serum is raised against the β-isomerized octapeptide (EKAH(β)DGGR) on the non-helical carboxy terminal telopeptide of the type I collagen molecule [34]; Currently, two automated immunoassays are available: Beta-CrossLaps Roche Elecsys (ECLIA, Roche Diagnostics, Mannheim, Germany) and CTX-1 (CrossLaps) IDS-iSYS (CLIA, Immunodiagnostic Systems, Tyne and Wear, UK). While both immunoassays use antibodies raised against the same epitope, there seems to be some bias despite good correlation between the results produced by the two assays (personal communication, UK NEQAS for Immunology, Immunochemistry & Allergy). An ELISA for s-CTX is also available (Immunodiagnostic Systems, Tyne and Wear, UK). S-CTX is influenced by renal function; it also shows significant diurnal variability with a peak in the early morning and a nadir in the afternoon, and food intake leads to a decrease in level [34]. Therefore, sample collection needs to be standardized, and performed in a fasting state in the morning. Whilst serum or plasma can be used, the best stability is obtained in EDTA plasma.
2) s-PINP
There are two forms of PINP in blood: the "intact" or trimeric molecule and the monomer [34]. Assays which are currently available measure either the trimeric form (intact assay) only or both forms (total PINP). The total PINP assay (automated) is available on Elecsys (Roche Diagnostics). The intact PINP assay automated is available on IDS-iSYS (Immunodiagnostic Systems); a radioimmunoassay for intact PINP is also available (UniQ PINP RIA Orion Diagnostica, Epsoo, Finland). Whilst results from current assays for PINP are comparable to the results from 'healthy' osteoporosis subjects with normal renal function, there is a potential for heterogeneity in patients with renal failure or metastatic bone disease, as it is claimed that the monomeric fragments may accumulate in these conditions [35, 36]. Pre-analytical advantages of PINP include a low diurnal and intra-individual variability, and stability at room temperature. Serum or plasma is acceptable. A working group of the International Federation of Clinical Chemistry (IFCC) and International Osteoporosis Foundation (IOF) is planning for the standardization of commercial assays for s-CTX and s-PINP in collaboration with commercial manufacturers [21].
BIOCHEMICAL EFFECTS OF OSTEOPOROSIS TREATMENT
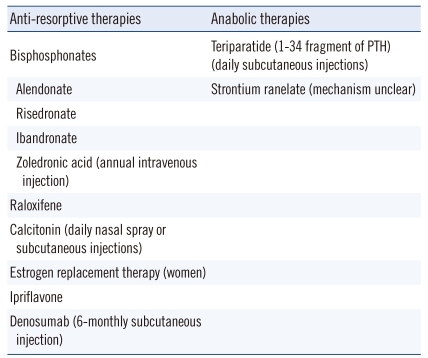
There are now a number of effective treatments available for osteoporosis, as shown by randomized controlled trials, to decrease fracture risk significantly in the spine, hip and other skeletal sites. These treatments are listed in Table 2, and are generally classified either as anti-resorptive agents which have an inhibitory effect on osteoclasts or as anabolic agents which have a primary stimulatory effect on osteoblasts (note that the action of strontium ranelate is not clear even though listed under anabolic agents).
Table 2.
Treatments currently available for osteoporosis (orally administered unless otherwise indicated)
Abbreviation: PTH, parathyroid hormone.
Calcium and vitamin D have a modest effect on reducing bone loss or improving BMD and decreasing fracture risk, especially in subjects with inadequate calcium or vitamin D nutrition, such as institutionalized elderly patients [26]. However, in patients requiring treatment calcium and vitamin D are generally used as adjuncts to drug therapy.
Bisphosphonates (alendronate, risedronate and zoledronic acid), the most common drugs for osteoporosis are analogues of pyrophosphate and potent inhibitors of osteoclast-mediated bone resorption with major effects on bone remodeling and calcium metabolism. They are extensively used in the treatment of osteoporosis as well as other bone diseases such as Paget's disease (found mainly in western Europeans), osteogenesis imperfecta (a rare genetic disorder due to mutations in the type 1 collagen genes COL1A1 and COL1A2), osteolytic bone disease of malignancy, and hypercalcemia. The biochemical responses to bisphosphonate therapy are manifold and of interest to clinicians who prescribe these drugs; the appreciation of the effects of bisphosphonates on biochemical measurements is vitally important for the appropriate interpretation of laboratory investigations performed during the routine therapeutic use of such drugs.
During treatment with bisphosphonates, the early inhibition of bone resorption induces a decrease in serum calcium which stimulates the secretion of PTH [37-40]. The increase in PTH in turn causes an increase in 1,25-dihydroxyvitamin D. Thus, a serum PTH which is mildly raised above the upper limit of the reference interval with normal or low serum calcium, is not an uncommon finding in bisphosphonate-treated patients with metabolic bone disease, especially when there is suboptimal calcium or vitamin D nutrition. The reduction in serum calcium occurs within days to weeks of initiation of oral bisphosphonate treatment and earlier with intravenous therapy. These changes may persist for many weeks to months following the institution of treatment and may be prominent in vitamin D insufficient patients.
Fasting urinary calcium excretion is usually within the reference interval in patients with osteoporosis. Following treatment with bisphosphonates there is a decrease in urine calcium excretion due to the reduction of calcium egress from the bone as well as the increased PTH action on the renal tubules to increase reabsorption of calcium. This urinary calcium conservation may be accentuated in subjects with inadequate calcium intake and vitamin D deficiency. It should be noted that calcium supplementation is generally prescribed together with bisphosphonate therapy.
The reductions in renal phosphate threshold and in serum phosphate which follow treatment with bisphosphonates are attributed to the effects of PTH on renal tubules as a consequence of secondary hyperparathyroidism [41]. On the other hand, in hypoparathyroid patients who are unable to mount a PTH response, bisphosphonates have been shown to induce a marked and sustained increase in serum phosphate and renal tubular reabsorption of phosphate [42].
The hypocalcemic response to bisphosphonates mentioned above, although usually mild, can on occasions be severe enough to be symptomatic and warrant clinical intervention. Most reports of symptomatic hypocalcemia have involved cancer patients presenting with paresthesia and tetany a few days (up to 2 weeks) after treatment with intravenous bisphosphonates [43, 44]. Patients with hypoparathyroidism would be especially at risk of this complication, since they would not be able to counteract the hypocalcemic effects of bisphosphonate action.
BTMS FOR MONITORING OSTEOPOROSIS TREATMENT
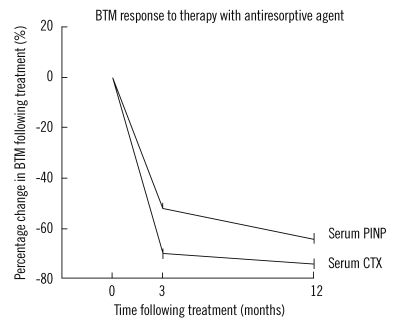
The changes in BTMs following therapy are well documented. There is a decrease in BTMs following initiation of anti-resorptive therapy, reflecting inhibition of osteoclastic activity [45-53]. For example, with bisphosphonate treatment, there is a decrease in bone resorption markers within days following intravenous therapy, and within weeks following oral therapy [45-53]. The decrease in resorption markers is followed by a later decline in bone formation markers which also reach their nadir or plateau (Fig. 1) [54].
Fig. 1.
The direction and magnitude of changes in a marker of bone resorption (serum CTX) and a marker of formation (serum PINP) in response to treatment with oral alendronate therapy [Drawn based on reference 54].
Abbreviations: BTM, bone turnover marker; CTX, carboxy terminal telopeptide of collagen type I; PINP, procollagen type I N-terminal propeptide.
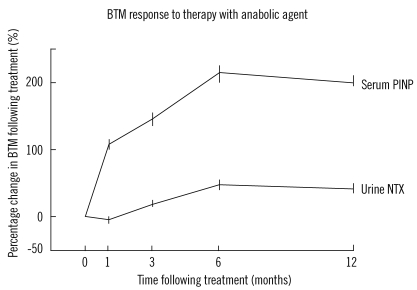
In the case of anabolic agents such as teriparatide, after initiation of treatment there is an increase in BTMs, with the bone formation marker first followed by in resorption marker (Fig. 2) [55, 56]. In the case of strontium ranelate, there is a small increase in bone formation markers and a small decrease in bone resorption markers [57]. The use of biochemical markers of bone remodeling in the monitoring of patients on treatment for osteoporosis is generally well-recognized [34, 58]. However, optimum treatment targets specific to various therapies and the benefits of monitoring in terms of improvement in fracture outcomes or in adherence to oral therapies are not established [21].
Fig. 2.
The direction and magnitude of changes in a marker of bone resorption (urine NTX) and a marker of formation (serum PINP) in response to treatment with daily teriparatide injections [Drawn based on reference 55].
Abbreviations: BTM, bone turnover marker; NTX, cross-linked N-telopeptides of type I collagen; PINP, procollagen type I N-terminal propeptide.
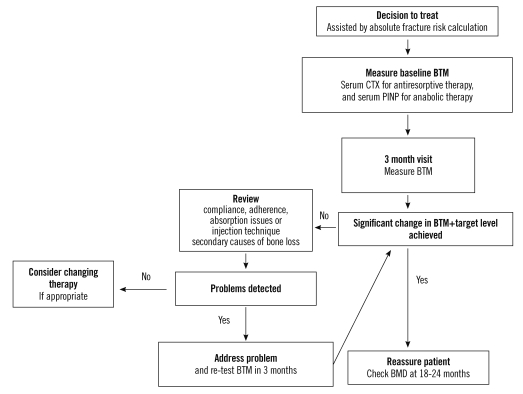
The theoretical basis for the use of BTMs in monitoring osteoporosis treatment is as follows. The aim of treatment is to reduce fracture risk. Fracture events are not common and in any case one does not want to wait untill the patient develops a fracture to determine failure of therapy. Therefore, a surrogate marker is required to confirm efficacy of treatment. The changes in BMD and BTMs following the initiation of osteoporosis treatment independently correlate with fracture risk reduction [59]. However, the change in BTMs following treatment explains a greater proportion of treatment effect than the change in BMD does, in terms of fracture risk reduction [60, 61]. Also, the change in BMD is small and slow whereas the changes in BTMs are large and occur early after initiation of therapy. Repeat BMD is not advocated within 12 months after initiation of therapy as the changes do not generally attain significance within that time, and in fact 18-24 months may be appropriate for repeat BMD measurements [26]. BTMs on the other hand show significant change by 3-6 months. For example, bone resorption markers can be measured 3 months after initiation of oral bisphosphonates, and bone formation markers 6 months after start of therapy [30, 57]. Significant changes in BTMs may be seen even earlier with intravenous bisphosphonates. The objective in anti-resorptive therapy is to reduce BTM levels, if they are increased, into the pre-menopausal range, or even better, to below the premenopausal mean. In patients with pre-treatment BTMs within the premenopausal range, a decrease greater than the least significant change (LSC) confirms the effect of the medication [57]. The relatively large intra-individual variation in BTMs is often cited as a problem in their application in practice [62]. This variation is less in blood than in urine. Also, the LSC for BTMs is generally calculated using 95% confidence, which is traditionally used in research (i.e. LSC=2.77×CV) [57]. However, this level of confidence is not the normal in clinical decision making and may not be needed for the application of BTMs in practice; a 90% or even 80% confidence may be acceptable [21, 34]. At this level of confidence together with a one-tailed test (since the direction of change following each currently available treatments is known), LSC may be calculated as 1.81×CV or 1.19×CV respectively. This level of change would be seen in most compliant patients following initiation of therapy with anti-resorptives such as bisphosphonate or the new anti-resorptive agent denosumab, as well as anabolic agents such as teriparatide therapy. An algorithm that may guide the use of BTMs in monitoring osteoporosis therapy is shown in Fig. 3. The role of BTMs in monitoring strontium ranelate treatment is less clear as the changes in BTMs with this medication are small.
Fig. 3.
An algorithm for the use of bone turnover markers (BTMs) in the monitoring of osteoporosis treatment [Based on references 58 and 63].
Further studies are needed to determine optimum monitoring protocols for different therapies, including optimum treatment targets for reference standard BTMs, s-PINP, and s-CTX. The standardization of commercial assays for their measurement will assist in determining universally applicable cut-offs and targets which can then be included in guidelines. There is also the need for evidence that the use of BTMs in monitoring therapy will improve adherence and fracture outcomes.
CONCLUSION
We have shown that although changes in laboratory indices are not major in osteoporosis, and the measurement of BTMs is not useful for the diagnosis of osteoporosis, laboratory investigations are useful in excluding or identifying secondary causes of osteoporosis. Although BTMs are independent predictors of fracture risk, their inclusion in fracture risk calculations will have to await further data to clarify their contribution to fracture risk and interactions with other risk factors. Changes in BTMs may be useful in monitoring osteoporosis treatment to confirm compliance with oral therapies, and efficacy of treatment. Further studies with reference BTMs are needed to clarify treatment targets for various therapies and optimal monitoring regimes.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Consensus Development Conference: diagnosis, prophylaxis and treatment of osteoporosis. Am J Med. 1993;94:646–650. doi: 10.1016/0002-9343(93)90218-e. [DOI] [PubMed] [Google Scholar]
- 2.Kanis JA, McCloskey EV, Johansson H, Oden A, Melton LJ, 3rd, Khaltaev N. A reference standard for the description of osteoporosis. Bone. 2008;42:467–475. doi: 10.1016/j.bone.2007.11.001. [DOI] [PubMed] [Google Scholar]
- 3.Lim S, Koo BK, Lee EJ, Park JH, Kim MH, Shin KH, et al. Incidence of hip fractures in Korea. J Bone Miner Metab. 2008;26:400–405. doi: 10.1007/s00774-007-0835-z. [DOI] [PubMed] [Google Scholar]
- 4.Moon YW, Yoon BK, Min YK, Chang MJ, Jung SM, Lim SJ, et al. Mortality, second fracture, and functional recovery after hip fracture surgery in elderly Koreans. Korean J Bone Metab. 2008;15:41–47. [Google Scholar]
- 5.Lee SR, Kim SR, Chung KH, Ko DO, Cho SH, Ha YC, et al. Mortality and activity after hip fracture: a prospective study. J Korean Orthop Assoc. 2005;40:423–427. [Google Scholar]
- 6.Kho DH, Kim KH, Shin JY, Lee JH, Kim DH. Postoperative mortality rate of hip fracture in elderly patients. J Korean Fract Soc. 2006;19:117–121. [Google Scholar]
- 7.Statistics Korea. [Updated on Dec 2011]. https://www.index.go.kr/egams/stts/jsp/potal/stts/PO_STTS_IdxMain.jsp?idx_cd=1010&bbs=INDX_001.
- 8.Cooper C, Cole ZA, Holroyd CR, Earl SC, Harvey NC, Dennison EM, et al. Secular trends in the incidence of hip and other osteoporotic fractures. Osteoporos Int. 2011;22:1277–1288. doi: 10.1007/s00198-011-1601-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cooper C, Campion G, Melton LJ., 3rd Hip fractures in the elderly: a world-wide projection. Osteoporos Int. 1992;2:285–289. doi: 10.1007/BF01623184. [DOI] [PubMed] [Google Scholar]
- 10.Kanis JA, Johnell O, Oden A, Johansson H, McCloskey E. FRAX and the assessment of fracture probability in men and women from the UK. Osteoporos Int. 2008;19:385–397. doi: 10.1007/s00198-007-0543-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee DY, Lim SJ, Moon YW, Min YK, Choi D, Yoon BK, Park YS. Determination of an applicable FRAX model in Korean women. J Korean Med Sci. 2010;25:1657–1660. doi: 10.3346/jkms.2010.25.11.1657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tromp AM, Ooms ME, Popp-Snijders C, Roos JC, Lips P. Predictors of fractures in elderly women. Osteoporos Int. 2000;11:134–140. doi: 10.1007/PL00004174. [DOI] [PubMed] [Google Scholar]
- 13.Ross PD, Kress BC, Parson RE, Wasnich RD, Armour KA, Mizrahi IA. Serum bone alkaline phosphatase and calcaneus bone density predict fractures: a prospective study. Osteoporos Int. 2000;11:76–82. doi: 10.1007/s001980050009. [DOI] [PubMed] [Google Scholar]
- 14.van Daele PL, Seibel MJ, Burger H, Hofman A, Grobbee DE, van Leeuwen JP, et al. Case-control analysis of bone resorption markers, disability, and hip fracture risk: the Rotterdam study. BMJ. 1996;312:482–483. doi: 10.1136/bmj.312.7029.482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chapurlat RD, Garnero P, Bréart G, Meunier PJ, Delmas PD. Serum type I collagen breakdown product (serum CTX) predicts hip fracture risk in elderly women: the EPIDOS study. Bone. 2000;27:283–286. doi: 10.1016/s8756-3282(00)00325-2. [DOI] [PubMed] [Google Scholar]
- 16.Garnero P, Sornay-Rendu E, Claustrat B, Delmas PD. Biochemical markers of bone turnover, endogenous hormones and the risk of fractures in postmenopausal women: the OFELY Study. J Bone Miner Res. 2000;15:1526–1536. doi: 10.1359/jbmr.2000.15.8.1526. [DOI] [PubMed] [Google Scholar]
- 17.Greenfield DM, Hannon RA, Eastell R. The association between bone turnover and fracture risk: The Sheffield Osteoporosis study. In: Eastell R, Baumann M, Hoyle N, Wieczorek L, editors. Bone markers - biochemical and clinical perspectives. Cachan: Lavoisier; 2001. pp. 225–226. [Google Scholar]
- 18.Garnero P, Cloos P, Sornay-Rendu E, Qvist P, Delmas PD. Type I collagen racemization and isomerization and the risk of fracture in postmenopausal women: the OFELY prospective study. J Bone Miner Res. 2002;17:826–833. doi: 10.1359/jbmr.2002.17.5.826. [DOI] [PubMed] [Google Scholar]
- 19.Meier C, Nguyen TV, Center JR, Seibel MJ, Eisman JA. Bone resorption and osteoporotic fractures in elderly men: the dubbo osteoporosis epidemiology study. J Bone Miner Res. 2005;20:579–587. doi: 10.1359/JBMR.041207. [DOI] [PubMed] [Google Scholar]
- 20.Bauer DC, Garnero P, Harrison SL, Cauley JA, Eastell R, Ensrud KE, et al. Biochemical markers of bone turnover, hip bone loss, and fracture in older men: the MrOS study. J Bone Miner Res. 2009;24:2032–2038. doi: 10.1359/JBMR.090526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vasikaran S, Eastell R, Bruyère O, Foldes AJ, Garnero P, Griesmacher A, et al. Markers of bone turnover for the prediction of fracture risk and monitoring of osteoporosis treatment: a need for international reference standards. Osteoporos Int. 2011;22:391–420. doi: 10.1007/s00198-010-1501-1. [DOI] [PubMed] [Google Scholar]
- 22.Veitch SW, Findlay SC, Hamer AJ, Blumsohn A, Eastell R, Ingle BM. Changes in bone mass and bone turnover following tibial shaft fracture. Osteoporos Int. 2006;17:364–372. doi: 10.1007/s00198-005-2025-y. [DOI] [PubMed] [Google Scholar]
- 23.Ingle BM, Hay SM, Bottjer HM, Eastell R. Changes in bone mass and bone turnover following ankle fracture. Osteoporos Int. 1999;10:408–415. doi: 10.1007/s001980050247. [DOI] [PubMed] [Google Scholar]
- 24.Lane NE, Lukert B. The science and therapy of glucocorticoid-induced bone loss. Endocrinol Metab Clin North Am. 1998;27:465–483. doi: 10.1016/s0889-8529(05)70017-7. [DOI] [PubMed] [Google Scholar]
- 25.Deodhar AA, Woolf AD. Bone mass measurement and bone metabolism in rheumatoid arthritis: a review. Br J Rheumatol. 1996;35:309–322. doi: 10.1093/rheumatology/35.4.309. [DOI] [PubMed] [Google Scholar]
- 26.Clinical guideline for the prevention and treatment of osteoporosis in postmenopausal women and older men (RACGP) [Updated on Feb 2010]. http://www.racgp.org.au/guidelines/musculoskeletaldiseases/osteoporosis.
- 27.Ross AC, Manson JE, Abrams SA, Aloia JF, Brannon PM, Clinton SK, et al. The 2011 report on dietary reference intakes for calcium and vitamin D from the Institute of Medicine: what clinicians need to know. J Clin Endocrinol Metab. 2011;96:53–58. doi: 10.1210/jc.2010-2704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Glendenning P, Taranto M, Noble JM, Musk AA, Hammond C, Goldswain PR, et al. Current assays overestimate 25-hydroxyvitamin D3 and underestimate 25-hydroxyvitamin D2 compared with HPLC: need for assay-specific decision limits and metabolite-specific assays. Ann Clin Biochem. 2006;43:23–30. doi: 10.1258/000456306775141650. [DOI] [PubMed] [Google Scholar]
- 29.Glendenning P, Laffer LL, Weber HK, Musk AA, Vasikaran SD. Parathyroid hormone is more stable in EDTA plasma than in serum. Clin Chem. 2002;48:766–767. [PubMed] [Google Scholar]
- 30.Chung SH, Kim TH, Lee HH. Relationship between Vitamin D level and bone mineral density in postmenopausal women from Bucheon area. J Korean Soc Osteoporos. 2009;7:198–202. [Google Scholar]
- 31.Kim H, Ku SY, Kim SH, Choi YM, Moon SY, Kim JG. A study on vitamin D insufficiency in postmenopausal Korean women. J Korean Soc Osteoporos. 2003;1:12–21. [Google Scholar]
- 32.Park HM, Kim JG, Choi WH, Lim SK, Kim GS. The vitamin D nutritional status of postmenopausal women in Korea. Korean J Bone Metab. 2003;10:47–55. [Google Scholar]
- 33.So JS, Park HM. Relationship between parathyroid hormone, vitamin D and bone turnover markers in Korean postmenopausal women. Korean J Obstet Gynecol. 2004;47:153–160. [Google Scholar]
- 34.Brown JP, Albert C, Nassar BA, Adachi JD, Cole D, Davison KS, et al. Bone turnover markers in the management of postmenopausal osteoporosis. Clin Biochem. 2009;42:929–942. doi: 10.1016/j.clinbiochem.2009.04.001. [DOI] [PubMed] [Google Scholar]
- 35.Koivula MK, Ruotsalainen V, Björkman M, Nurmenniemi S, Ikäheimo R, Savolainen K, et al. Difference between total and intact assays for N-terminal propeptide of type I procollagen reflects degradation of pN-collagen rather than denaturation of intact propeptide. Ann Clin Biochem. 2010;47:67–71. doi: 10.1258/acb.2009.009110. [DOI] [PubMed] [Google Scholar]
- 36.Marin L, Koivula MK, Jukkola-Vuorinen A, Leino A, Risteli J. Comparison of total and intact aminoterminal propeptide of type I procollagen assays in patients with breast cancer with or without bone metastases. Ann Clin Biochem. 2011;48:447–451. doi: 10.1258/acb.2011.011040. [DOI] [PubMed] [Google Scholar]
- 37.Douglas DL, Duckworth T, Russell RG, Kanis JA, Preston CJ, Preston FE, et al. Effect of dichloromethylene diphosphonate in Paget's disease of bone and in hypercalcaemia due to primary hyperparathyroidism or malignant disease. Lancet. 1980;1:1043–1047. doi: 10.1016/s0140-6736(80)91496-8. [DOI] [PubMed] [Google Scholar]
- 38.Fraser WD, Logue FC, Gallacher SJ, O'Reilly DS, Beastall GH, Ralston SH, et al. Direct and indirect assessment of the parathyroid hormone response to pamidronate therapy in Paget's disease of bone and hypercalcaemia of malignancy. Bone Miner. 1991;12:113–121. doi: 10.1016/0169-6009(91)90040-7. [DOI] [PubMed] [Google Scholar]
- 39.Chesnut CH, 3rd, Harris ST. Short-term effect of alendronate on bone mass and bone remodeling in postmenopausal women. Osteoporos Int. 1993;3(Suppl 3):S17–S19. doi: 10.1007/BF01623003. [DOI] [PubMed] [Google Scholar]
- 40.Maalouf NM, Heller HJ, Odvina CV, Kim PJ, Sakhaee K. Bisphosphonate-induced hypocalcemia: report of 3 cases and review of literature. Endocr Pract. 2006;12:48–53. doi: 10.4158/EP.12.1.48. [DOI] [PubMed] [Google Scholar]
- 41.McCloskey EV, Yates AJ, Gray RE, Hamdy NA, Galloway J, Kanis JA. Diphosphonates and phosphate homeostasis in man. Clin Sci (Lond) 1988;74:607–612. doi: 10.1042/cs0740607. [DOI] [PubMed] [Google Scholar]
- 42.Vasikaran SD, O'Doherty DP, McCloskey EV, Gertz B, Kahn S, Kanis JA. The effect of alendronate on renal tubular reabsorption of phosphate. Bone Miner. 1994;27:51–56. doi: 10.1016/s0169-6009(08)80186-9. [DOI] [PubMed] [Google Scholar]
- 43.Jodrell DI, Iveson TJ, Smith IE. Symptomatic hypocalcaemia after treatment with high-dose aminohydroxypropylidene diphosphonate. Lancet. 1987;1:622. doi: 10.1016/s0140-6736(87)90255-8. [DOI] [PubMed] [Google Scholar]
- 44.Chong G, Hoang T, Davis ID. Symptomatic hypocalcaemia following intravenous pamidronate in cancer patients. Aust N Z J Med. 1999;29:96–97. doi: 10.1111/j.1445-5994.1999.tb01601.x. [DOI] [PubMed] [Google Scholar]
- 45.Garnero P, Shih WJ, Gineyts E, Karpf DB, Delmas PD. Comparison of new biochemical markers of bone turnover in late postmenopausal osteoporotic women in response to alendronate treatment. J Clin Endocrinol Metab. 1994;79:1693–1700. doi: 10.1210/jcem.79.6.7989477. [DOI] [PubMed] [Google Scholar]
- 46.Schlosser K, Scigalla P. Biochemical markers as surrogates in clinical trials in patients with metastatic bone disease and osteoporosis. Scand J Clin Lab Invest Suppl. 1997;227:21–28. [PubMed] [Google Scholar]
- 47.Braga de Castro Machado A, Hannon R, Eastell R. Monitoring alendronate therapy for osteoporosis. J Bone Miner Res. 1999;14:602–608. doi: 10.1359/jbmr.1999.14.4.602. [DOI] [PubMed] [Google Scholar]
- 48.Bell NH, Bilezikian JP, Bone HG, 3rd, Kaur A, Maragoto A, Santora AC. Alendronate increases bone mass and reduces bone markers in postmenopausal African-American women. J Clin Endocrinol Metab. 2002;87:2792–2797. doi: 10.1210/jcem.87.6.8575. [DOI] [PubMed] [Google Scholar]
- 49.Greenspan SL, Parker RA, Ferguson L, Rosen HN, Maitland-Ramsey L, Karpf DB. Early changes in biochemical markers of bone turnover predict the long-term response to alendronate therapy in representative elderly women: a randomized clinical trial. J Bone Miner Res. 1998;13:1431–1438. doi: 10.1359/jbmr.1998.13.9.1431. [DOI] [PubMed] [Google Scholar]
- 50.Garnero P, Gineyts E, Arbault P, Christiansen C, Delmas PD. Different effects of bisphosphonate and estrogen therapy on free and peptidebound bone cross-links excretion. J Bone Miner Res. 1995;10:641–649. doi: 10.1002/jbmr.5650100418. [DOI] [PubMed] [Google Scholar]
- 51.Rosen HN, Dresner-Pollak R, Moses AC, Rosenblatt M, Zeind AJ, Clemens JD, et al. Specificity of urinary excretion of cross-linked N-telopeptides of type I collagen as a marker of bone turnover. Calcif Tissue Int. 1994;54:26–29. doi: 10.1007/BF00316285. [DOI] [PubMed] [Google Scholar]
- 52.Rosen HN, Moses AC, Garber J, Ross DS, Lee SL, Greenspan SL. Utility of biochemical markers of bone turnover in the follow-up of patients treated with bisphosphonates. Calcif Tissue Int. 1998;63:363–368. doi: 10.1007/s002239900541. [DOI] [PubMed] [Google Scholar]
- 53.McClung MR, Lewiecki EM, Cohen SB, Bolognese MA, Woodson GC, Moffett AH, et al. Denosumab in postmenopausal women with low bone mineral density. N Engl J Med. 2006;354:821–831. doi: 10.1056/NEJMoa044459. [DOI] [PubMed] [Google Scholar]
- 54.Rosen CJ, Hochberg MC, Bonnick SL, McClung M, Miller P, Broy S, et al. Treatment with once-weekly alendronate 70 mg compared with onceweekly risedronate 35 mg in women with postmenopausal osteoporosis: a randomized double-blind study. J Bone Miner Res. 2005;20:141–151. doi: 10.1359/JBMR.040920. [DOI] [PubMed] [Google Scholar]
- 55.McClung MR, San Martin J, Miller PD, Civitelli R, Bandeira F, Omizo M, et al. Opposite bone remodeling effects of teriparatide and alendronate in increasing bone mass. Arch Intern Med. 2005;165:1762–1768. doi: 10.1001/archinte.165.15.1762. [DOI] [PubMed] [Google Scholar]
- 56.Body JJ, Gaich GA, Scheele WH, Kulkarni PM, Miller PD, Peretz A, et al. A randomized double-blind trial to compare the efficacy of teriparatide [recombinant human parathyroid hormone (1-34)] with alendronate in postmenopausal women with osteoporosis. J Clin Endocrinol Metab. 2002;87:4528–4535. doi: 10.1210/jc.2002-020334. [DOI] [PubMed] [Google Scholar]
- 57.Meunier PJ, Roux C, Seeman E, Ortolani S, Badurski JE, Spector TD, et al. The effects of strontium ranelate on the risk of vertebral fracture in women with postmenopausal osteoporosis. N Engl J Med. 2004;350:459–468. doi: 10.1056/NEJMoa022436. [DOI] [PubMed] [Google Scholar]
- 58.Bergmann P, Body JJ, Boonen S, Boutsen Y, Devogelaer JP, Goemaere S, et al. Evidence-based guidelines for the use of biochemical markers of bone turnover in the selection and monitoring of bisphosphonate treatment in osteoporosis: a consensus document of the Belgian Bone Club. Int J Clin Pract. 2009;63:19–26. doi: 10.1111/j.1742-1241.2008.01911.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Riggs BL, Melton LJ, 3rd, O'Fallon WM. Drug therapy for vertebral fractures in osteoporosis: evidence that decreases in bone turnover and increases in bone mass both determine antifracture efficacy. Bone. 1996;18(3 Suppl):197S–201S. doi: 10.1016/8756-3282(95)00502-1. [DOI] [PubMed] [Google Scholar]
- 60.Delmas PD, Seeman E. Changes in bone mineral density explain little of the reduction in vertebral or nonvertebral fracture risk with anti-resorptive therapy. Bone. 2004;34:599–604. doi: 10.1016/j.bone.2003.12.022. [DOI] [PubMed] [Google Scholar]
- 61.Delmas PD. Markers of bone turnover for monitoring treatment of osteoporosis with antiresorptive drugs. Osteoporos Int. 2000;11(Suppl 6):S66–S76. doi: 10.1007/s001980070007. [DOI] [PubMed] [Google Scholar]
- 62.Hannon R, Eastell R. Preanalytical variability of biochemical markers of bone turnover. Osteoporos Int. 2000;11(Suppl 6):S30–S44. doi: 10.1007/s001980070004. [DOI] [PubMed] [Google Scholar]
- 63.Eastell R, Krege JH, Chen P, Glass EV, Reginster JY. Development of an algorithm for using PINP to monitor treatment of patients with teriparatide. Curr Med Res Opin. 2006;22:61–66. doi: 10.1185/030079905X75096. [DOI] [PubMed] [Google Scholar]