Abstract
This article builds upon Traumatic Brain Injury Common Data Elements (TBI CDE) version 1.0 and the pediatric CDE Initiative by emphasizing the essential role of psychosocial risk and protective factors in pediatric TBI research. The goals are to provide a compelling rationale for including psychosocial risk and protective factors in addition to socioeconomic status (SES), age, and sex in the study design and analyses of pediatric TBI research and to describe recommendations for core common data elements in this domain. Risk and protective factor research is based on the ecological theory of child development in which children develop through a series of interactions with their immediate and more distant environments. Home, school, religious, and social influences are conceptualized as risk and/or protective factors. Child development and TBI researchers have interpreted risk and protective variables as main effects or as interactions and have used cumulative risk indices and moderation models to describe the relationship among these variables and outcomes that have to do with development and with recovery from TBI. It is likely that the number, type, and interaction among risk and protective factors each contribute unique variance to study outcomes. Longitudinal designs in TBI research will be essential to understanding the reciprocal relationships between risk/protective factors and the recovery/outcome made by the child. The search for effective interventions to hasten TBI recovery mandates the need to target modifiable risks and to promote protective factors in the child's environment.
Key words: additive model, moderation model, psychosocial protective factors, psychosocial risk factors, TBI research
Introduction
In considering the potentially far-reaching outcomes of pediatric traumatic brain injury (TBI) (see the companion article published in this issue by McCauley et al.), it became apparent that there was a host of critically important psychosocial risk and protective factors that influence the course of recovery from childhood TBI. This companion article was developed to provide a rationale for including the assessment of risk and protective factors in future pediatric TBI research and to identify core measures in this domain. The supplemental and emerging measures identified by the Pediatric Common Data Elements Working Group provide a range of risk and protective variables that will contribute to a range of childhood TBI studies.
This article focuses on risk and protective factors identified for cognitive, behavioral, and social development and recovery following TBI. Although risk and protective factors also exist as circumstances leading to the injury (see Gerring et al., 2009), discussion of that literature is beyond the scope of the current article. The goals of the current article are as follows: 1) to provide an initial basic framework for understanding social-environmental influences on recovery following TBI; 2) to ground the discussion in the broader developmental literature on environmental influences on social-emotional development; 3) to review the existing research on risk and protective factors following childhood TBI, along with the advantages and applicability of assessing those risk and protective factors in medical, cognitive, and behavioral studies; and 4) to provide recommendations for inclusion of core risk and protective factors in TBI research studies to further enhance the quality of the research and approaches to intervention.
A Framework for Understanding Social-Environmental Influences
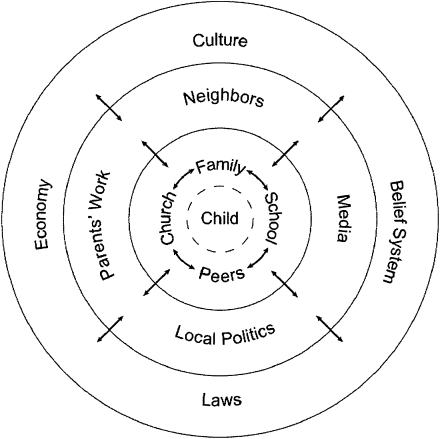
Bronfenbrenner (1979) conceptualized human development as an evolving interaction between the child and his or her experiences. Beginning with the child in the center, the environment is conceptualized as a series of nested bi-directional relationships (Fig. 1). The characteristics of the child, including biology/genetics, temperament, and behavior, along with the interactions that occur within the child's immediate home environment can be thought of as proximal variables or influences. More remote or distal influences, such as the social, religious, and political institutions of a particular culture, also indirectly impact the child's development. Distal variables exert their effects, in part, through the proximal environment, and their effects may increase as the child ages (Copeland-Linder et al., 2010; Stouthamer-Loeber et al., 2002).
FIG. 1.
The basic ecological model of child development shows the proximal and distal environmental variables that influence the growing child. The inner circle of proximal variables has the most direct influence on the life of the child and the outer circles exert indirect influence. Each of these variables has the potential of contributing a positive or a negative factor toward the child's developmental outcome.
Each of these interconnected environments exerts direct and indirect influences on the child's development that can be conceptualized as risk and/or protective factors. With respect to childhood TBI, if the child lives in a crowded, single-parent household at the time of injury, this family system may place the child at risk for adverse outcomes, as the parent may not have the time or the financial ability to deal with the multiple needs of the injured child (Wells et al., 2009). The parent may not be able to attend all of the necessary school meetings to insure that the child will have optimal school services for that child's deficits. A more distant or distal risk factor would be the inability to obtain funding from a state agency for necessary equipment that would hasten the child's recovery. Importantly, the interrelationships between the child's development and the social environment are reciprocal. For example, the child's injury may result in frequent work absences for the parent that in turn may lead to dismissal from employment, and a great drop in family income, thus constituting an additional risk for the child.
Many social-environmental influences may function as either a risk or a protective factor depending upon the situation or level (e.g., high versus low income) (Masten, 2001; Stouthamer-Loeber et al., 2002). Therefore, the child's family environment may constitute a risk factor at high levels of dysfunction, or a protective factor when functioning well. Additionally, the absence of protective factors, such as social resources or a supportive second parent in the home, may constitute a risk in its own right. Each individual's social context consists of interrelated levels or layers of risk and protective factors, e.g., the risk factor of an ill parent, and the protective factor of a supportive, involved school. Because few, if any, investigations have considered the broad range of potential risk and protective factors and the interrelationships among them, conclusions that one is more important than another cannot be drawn (Kessler et al., 1997). However, for certain outcomes, a specific risk or protective factor may be particularly salient; whereas at other times risk and protective factors may balance each other, with neutral or negligible effect on outcome, as in the above example of the ill parent and the supportive school (Garmezy et al., 1984; Masten et al., 1988). Protective factors were initially conceptualized as contributing to positive outcomes by moderating or buffering the effects of risk factors on adverse outcomes (i.e., effective parenting reduces the risk associated with living in a high-crime neighborhood). However, investigators have increasingly begun to consider the effects of protective factors on adjustment independent of risk factors (i.e., main or direct effects) (Luthar et al, 2000). Different approaches have been taken to examine the relationship of risk and protective factors to cognitive, behavioral, and social development. In the first approach, investigators have sought to identify factors that are associated or correlated with cognitive or behavioral development. In these studies, significant correlations indicate that the environmental factor (i.e., family functioning) has a main effect on the outcome (i.e., child behavior). Examples of this approach within the field of pediatric TBI include studies by Anderson and Rivara and are considered in greater detail here (Anderson et al., 2005; Nadebaum et al. 2007; Rivara et al., 1993, 1994).
Many studies of the effects of the social environment on TBI recovery, such as those by Rutter, Gerring, and Max described subsequently (Rutter, 1987; Gerring et al., 1998; Max et al., 2005), examined the relationship of psychosocial adversity indices to behavioral and psychiatric outcomes. Such indices are constructed by dichotomizing risk factors at cut points or thresholds that are believed to be associated with poorer outcomes (i.e., high levels of family dysfunction). A psychosocial adversity or cumulative risk index is then obtained by summing the number of risks for each individual. Some risk factors are dichotomous by nature such as living in a single-parent household. Although dichotomizing naturally continuous variables such as income can result in a loss of predictive power, the approach can be appropriate when a factor increases risk only when it exceeds a certain threshold. For example, income may only constitute a risk factor when it falls below the national poverty level. Recent research has identified several limitations of cumulative risk indices (Green et al., 2010; Szatmari et al., 1994). Specifically, such additive models may artificially inflate associations with disorder, as many risk factors cluster or covary (i.e., single-parent status, low income, lack of health insurance). Additionally, more sophisticated multivariate models (see Green et al., 2010) provide evidence that specific psychosocial adversities do not confer equal risk. Some types of adversity may be unrelated to outcomes whereas other risks may exacerbate the effects of one another (moderation effects). Examination of moderation effects represents the third approach and is described in the next section.
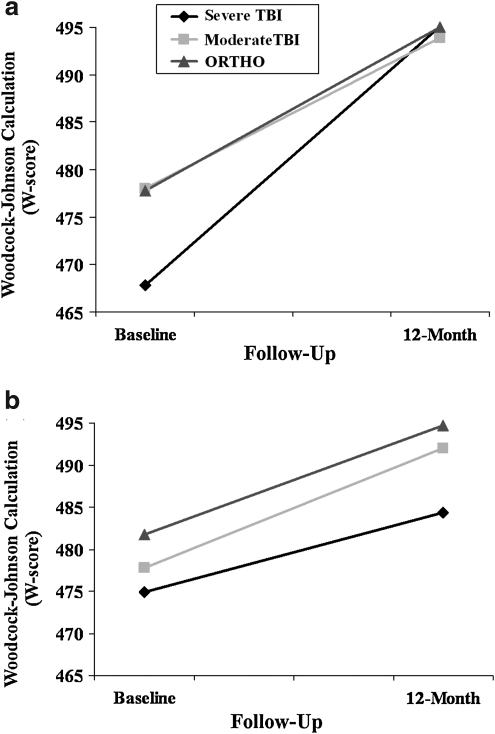
Finally, models can examine whether social-environmental risk and protective factors moderate the relationship between a factor such as TBI and cognitive or behavioral outcomes. Moderation exists when the strength of the association or relationship between two variables (i.e., TBI and academic achievement) is affected by a third variable (i.e., caregiver life stress). Figure 2 depicts how the risk factor of life stresses moderated recovery and subsequent development of mathematics achievement following pediatric TBI. Deficits in mathematics achievement persisted at 12 months post-injury among children with severe TBI and high family stresses (Taylor et al. 2002). Conversely, the achievement of children with severe TBI and low family stresses caught up to that of their peers with orthopedic injuries over the same time period. These moderation models provide evidence that the effects of risk or protective factors may differ as a function of the nature and severity of the injury.
FIG. 2.
The figure depicts estimates of mean scores on the calculation subtest of the Woodcock–Johnson Tests of Achievement–Revised at baseline and 12 months post-injury for children with a) low and b) high levels of family stressors as defined by scores one standard deviation above and below the mean, respectively. (a) Children with severe TBI are shown to catch up in mathematics skills relative to children with orthopedic injuries with low levels of family stressors. However, as depicted in b, deficits in mathematics skills following severe TBI persist at 12 months when there are high levels of family stress.
Influence of Risk and Protective Factors on Recovery following Pediatric TBI
Beginning with the seminal studies of Rutter in the early 1980's (Brown et al., 1981; Chadwick et al., 1981a,b; Rutter et al., 1980), investigators have sought to more clearly understand the relationship of social-environmental risk factors to cognitive and behavioral outcomes and recovery following TBI. Rutter and colleagues prospectively studied children age 5–14 years with mild and severe TBI, and orthopedic injury controls, and rated their level of psychosocial adversity using the Psychosocial Adversity Index (Brown et al., 1981). Results indicated an interaction between the severity of the brain injury and the total number of psychosocial risks or adversities in predicting the outcome of pre-injury and post-injury psychiatric disorders. In children with severe TBI and high psychosocial adversity (i.e., high numbers of social-environmental risks), the percent of new, post-injury psychiatric disorder was very high, 60%, compared to 14% for children with severe TBI and low psychosocial adversity. Conversely, there was no increased incidence of disorders associated with high psychosocial adversity following mild brain injury. These data indicated that psychosocial adversity moderated the effects of severe TBI on psychiatric outcome following childhood TBI, and demonstrated that psychiatric outcome following severe TBI is better in the context of low psychosocial adversity.
In a series of studies Taylor and colleagues (Stancin et al., 2002; Taylor et al., 1999, 2001, 2002; Yeates, 1997, 2002, 2004) recruited and followed children between the ages of 6 and 12 who had sustained a severe TBI (n=42), moderate TBI (n=52), or orthopedic injury not involving the central nervous system (n=58). These children were followed prospectively and assessed shortly after the injury, and at 6 and 12 months post-injury as well as at three annual longer-term follow-up assessments an average of 4, 5, and 6 years post-injury. These investigators examined whether social-environmental factors moderated the effects of severe TBI on cognitive, behavioral, and social outcomes. Their results provided compelling evidence regarding the relationship of both distal and proximal social-environmental risk factors to both cognitive and behavioral outcomes. Specifically, a composite index of socioeconomic status (SES) incorporating parental education, occupation, and income moderated the effects of injury severity on the child's adaptive abilities (Taylor et al., 2002), academic performance (Taylor et al., 1999), and behavior problems (Taylor et al., 2002). In each case, children had poorer outcomes following severe TBI in the context of lower SES.
With respect to more proximal risk factors, these investigators have linked parental mental health (Taylor et al., 1999; 2001), caregiver burden (Taylor et al., 1999), family functioning (Stancin et al., 2002; Taylor et al., 1999; Yeates et al., 2004), and chronic caregiver life stressors (Taylor et al., 2002; Yeates et al., 2002) to various aspects of the child's recovery following TBI. Depending upon the risk factor under consideration, these results supported both main effects and moderation models of social-environmental influences. Specifically, higher levels of parental distress were associated with poorer fine motor control, poorer social competence, and higher levels of behavior problems regardless of the nature or severity of the injury (Taylor et al., 1999). Parental burden was also predictive of poorer adaptive functioning and fine motor control across injury severity. Additionally, higher levels of caregiver burden were associated with lower verbal IQ scores and worse adaptive functioning particularly following severe TBI (moderating effect). Chronic stressors in the parent's life also moderated the effects of injury severity on academic achievement and performance (Taylor et al., 2002) and some aspects of neuropsychological functioning (Yeates et al., 2002). Taken together, these findings provide support for the influence of both distal and proximal environmental risk factors on a range of outcomes following pediatric TBI. In several instances, environmental influences were greatest in the context of more severe injuries, consistent with a ‘double risk’ model.
A recent study of the recovery of children who sustained a TBI (n=80) or orthopedic injury (n=113) between the ages of 3 and 7 has provided further evidence of both main and moderating effects of environmental risk factors on recovery (Chapman et al., 2010; Gerrard-Morris et al., 2009; Wade et al., 2011; Yeates et al., 2010). Moreover, this investigation of recovery in younger children has provided new evidence regarding the importance of both parenting style and specific parenting behaviors to emerging behavior problems. Specifically, overly controlling, authoritarian parenting exacerbated negative behavioral outcomes for children with both moderate and severe TBI, with increasing time since injury. Permissive parenting and lower quality home environments were shown to contribute to poorer social outcomes especially among children with mild-moderate TBI (Yeates et al., 2010). With respect to parent–child interactions, parental negativity exacerbated emerging externalizing behaviors and attention-deficit/hyperactivity disorder (ADHD) symptoms following severe TBI (Wade et al., 2011).
Further evidence regarding the influence of psychosocial risk factors on the emergence of secondary attention-deficit/hyperactivity disorder (SADHD) following childhood TBI comes from a collaborative study including investigators at five medical centers (Max et al., 2005 a,b). In this investigation, children with mild, moderate, and severe TBI were followed prospectively at 6, 12, and 24 months post-injury. These investigators adopted a hybrid approach that considered both the main effects of SES and family functioning and the cumulative risks associated with total scores on a psychosocial adversity index. The psychosocial adversity index included in this study was similar to that developed by Brown and associates (1981) and included the child not living with biological or adoptive parents, overcrowding as defined by four or more children or more than one person per room, involvement of child services in the child's care because of family problems, elevated maternal distress, paternal criminal history, and either parent with an unskilled or semi-skilled job. SES was a significant predictor of SADHD at 6 months post-injury, whereas pre-injury psychosocial adversity emerged as a stronger predictor of SADHD during the second year post-injury. Interestingly, family functioning was not an independent predictor when SES and psychosocial adversity were included in the model, perhaps because of the high intercorrelations between family functioning and psychosocial adversity.
Gerring and associates (1998) adopted a cumulative risk approach in their study of 99 children and adolescents 4–19 years of age across the initial year following moderate and severe closed head injuries. Predictor variables in a series of studies on this cohort included an 8-item Psychosocial Adversity Scale modified from Rutter's scale (Brown et al., 1981). Each risk factor was counted as one point if it occurred within 1 year preceding injury. DSM disorders and symptoms of SADHD, oppositional defiant disorder, conduct disorder, and anxiety were the outcome variables. Children who developed SADHD by 1 year post-injury scored significantly higher on the psychosocial scale (mean, 2.60) than children who did not develop SADHD (mean, 1.09) (Gerring et al., 1998). Children who developed oppositional defiant disorder and conduct disorder by 1 year post-injury scored significantly higher on the psychosocial scale, using both univariate and multivariate regressions, than children who did not develop oppositional defiant disorder and conduct disorder (Gerring et al., 2009). Within the same cohort, children with TBI and obsessive-compulsive symptoms had significantly higher psychosocial adversity scores than children with TBI only, using unpaired student t tests (Grados et al., 2008). In contrast, psychosocial adversity was not correlated with either post-injury anxiety disorders or post-injury anxiety symptoms in this sample (Vasa et al., 2002). These varying contributions of childhood risk factors to the appearance of new psychiatric disorders in this sample emphasize the importance of including these predictor variables in studies examining behavioral and social outcomes of children and youth with TBI.
Other prospective longitudinal investigations have highlighted the role of environmental risk factors in recovery from pediatric TBI. Anderson and colleagues (Anderson et al., 2005; Nadelbaum et al., 2007) have examined the main effects of social-environmental risk factors on recovery across the initial 5 years following TBI in children who sustained mild (n=14), moderate (n=46), and severe TBI (n=24) between the ages of 2 and 7 relative to a healthy control group (n=33). Consistent with the findings from other studies, SES was found to be a significant predictor of 30-month outcomes including IQ, language, and memory abilities. At 5 years post-injury, psychosocial risk factors predicted executive functioning skills, with SES contributing to visual-spatial processing and parent-reported executive functioning, whereas pre-injury family functioning predicted processing speed and overall executive functioning. In general, greater psychosocial adversity as characterized by lower SES or worse premorbid family functioning was associated with a lower level of executive functioning at 5 years post-injury. Contrary to this overall trend, lower SES was associated with a higher level of parent-reported executive functioning. In a separate study of 150 children who sustained mild (n=42), moderate (n=70), or severe TBI (n=38) between the ages of 3 and 12 years, Anderson and colleagues (2005) found that SES was predictive of full scale IQ and attention; whereas family burden was predictive of behavioral functioning. Taken together, the results provide considerable support for the influence of both SES and family functioning on cognitive and behavioral recovery over time. However, because these investigators did not examine moderation effects, it is not possible to determine whether environmental influences varied as a function of injury severity.
Similarly, studies by Rivara and associates (1993, 1994) examined the main effects of family functioning on recovery from mild (n=50), moderate (n=25), and severe TBI (n=19) at 1 and 3 years post-injury. These investigators found that interviewer ratings of pre-injury family functioning and relationships were correlated with social competence, with poorer overall functioning and peer and marital relationships contributing to worse social competence. They also found associations between ratings of both global family functioning and total relationship strains and ratings of global child functioning, with greater dysfunction and stress resulting in poorer child outcomes. In regression models, high levels of family control were associated with worse child outcomes at 12 months. In a separate report (Rivara et al., 1994), these same investigators found ratings of pre-injury family functioning to be more closely related to child behavior at 12 months post-injury than to measures of academic functioning.
Protective Factors and Recovery
Thus far, we have focused on studies examining the relationship of social-environmental risk factors to recovery. However, many of these investigations have also examined the role of protective factors such as social resources, enriched home environments, and positive parenting behaviors in moderating recovery (Chapman et al., 2010; Gerrard-Morris et al., 2009; Taylor et al., 2002; Wade et al., 2011; Yeates et al., 2002, 2010). With respect to cognitive recovery, Yeates and associates (2002) reported less pronounced short-term differences in verbal learning between children with severe TBI and those with orthopedic injuries among those with greater caregiver resources such as supportive relationships with spouse, family, and friends. Gerard-Morris and associates (2009) found evidence that home environments with more supportive parents and greater access to books, educational games, and creative activities were associated with better performance on tasks of intellectual functioning, pragmatic judgment, verbal fluency, visual recognition, and executive functioning following TBI in early childhood. Pragmatic judgment refers to the awareness of and ability to modify appropriate language in a context. More favorable home environments were also associated with more rapid recovery of auditory memory over the initial 12 months post-injury, indicating a moderation effect of a good environment on auditory memory recovery. Parental warm responsiveness was predictive of intellectual functioning and pragmatic judgment. Moreover, parental support or verbal structuring of the child's activities was associated with better memory, language, and executive functioning performance (Gerrard-Morris et al., 2009). Thus, positive parenting behaviors and more enriched home environments contributed to better cognitive recovery following TBI in young children.
With respect to behavioral and social outcomes, the effects of severe TBI on social competence were in part ameliorated by high levels of caregiver resources (Yeates et al., 2004). Similarly, Yeates and associates (2010) found that authoritative or democratic parenting style was associated with better social competence, whereas the quality of the home environment moderated adaptive functioning, with less pronounced effects of TBI among children from more enriched home environments. These authors concluded that the presence of multiple significant interactions provides compelling evidence of “the existence of a complex interplay between the damaged brain and its environmental context during recovery from TBI in young children” (Yeates et al., 2010, p. 353). There is some evidence that the effects of the social environment on recovery are stronger with respect to academic, social, and behavioral outcomes than to cognitive and neuropsychological outcomes involving memory, attention, and visual-spatial skills (Taylor et al., 2002; Yeates et al., 2002, 2004, 2010). Although social-environmental factors have been linked to a range of neuropsychological, cognitive, and behavioral outcomes, in part because these same factors influence typical development (Halle et al., 2009), evidence for psychosocial moderation (i.e., greater effects in the context of more severe injury) is stronger with respect to social and behavioral outcomes. One explanation for this pattern of results (Yeates et al. 2010) is that cognitive functioning following a neurological insult such as TBI depends largely upon central nervous system integrity, and is therefore less influenced by social-environmental factors. Conversely, behavioral and social outcomes are likely to be determined by both the integrity of the central nervous system and the quality of the social environment.
Common Data Elements (CDE) Recommendations
This review of the role of social-environmental influences on recovery following pediatric TBI highlights the importance of a variety of risk and protective factors including parent–child interactions, parent behaviors, family functioning, social stressors and resources, SES, and cumulative psychosocial adversity. In accordance with other CDE work groups, well-established core measures were recommended as part of the pediatric work group (McCauley et al., 2011; Miller et al., 2012). These core measures covered risk and protective factors relevant to most TBI studies. As recommended in the article by McCauley et al. (2012), core measures of psychosocial risk and protective factors include the 12-item McMaster Family Assessment Device, General Functioning Scale (Miller et al., 1985), an index of SES (Maas et al., 2010), and an 11-item index assessing psychosocial risk factors. (Table 1).
Table 1.
Screening Psychosocial Risk Factors for Pediatric TBI Research
| Risk Factor | Questions |
|---|---|
| Child not living with caregiver | Has your child lived away from home for any reason for a period of 3 months or longer before 16 years of age? |
| Caregiver death/divorce/loss | Has there been divorce, separation, or the death of a caregiver; how old was your child when this happened? |
| Single caregiver | Are you raising the child by yourself without another adult caregiver? |
| Overcrowding | Are there the same or a fewer number of rooms in your house than there are people living there? |
| Low income | Are you receiving welfare, subsidized housing, food subsidies, or disability payments for your family? |
| Poor marriage/relationship | Do you have frequent verbal or physical arguments with your spouse or your partner? |
| Low education level of primary caregiver | What is the highest grade you have finished? |
| Caregiver chronic poor health | Do you have serious health problems that have lasted for the last 6 months? |
| Parental mental health disorder | Have you or your partner ever been treated or hospitalized for depression, anxiety, or severe mental illness ? |
| Parental alcoholism/substance abuse | Have you or your partner ever been treated for or hospitalized for alcoholism or illicit drug use? |
| Parental criminal behavior | Have you or your partner ever been arrested or put in jail for any crime? |
The 11-item index or list of psychosocial risk factors was selected from an extensive list of childhood adversities compiled for the Ontario Child Health Study (Boyle et al., 1987). This study was conducted with a community sample of 1869 children ages 4 to 16 years born between 1966 and 1979. The risk factors included household, family, caregiver, and child variables and were selected because they could be obtained reliably, and were useful in illuminating etiologic mechanisms or could be potentially targeted in interventions. These predictive risk factors have been used in a variety of bivariate and multivariate statistical models of child emotional, behavioral, and academic outcomes (Szatmari et al., 1994). Although there have been numerous variations of psychosocial adversity indices, this list of 11 was chosen because it is relatively brief, assesses a range of risks, can be reliably obtained, has considerable predictive validity, and has been broadly used in the developmental psychopathology literature.
The CDE work group also proposed a limited number of supplemental and emerging measures of the social environment. Recommended supplemental measures include the complete Family Assessment Device (Miller et al., 1985), the Family Burden of Injury Interview (Burgess et al., 1999), and the Conflict Behavior Questionnaire (Prinz et al., 1979). The self-report Family Burden of Injury Interview and the Child and Adolescent Scale of Environment were recommended as emerging measures given their lack of prior use in the literature. However, these suggestions may require further refinement given that some important measures discussed here (e.g., parenting) were not included because the findings had not yet been published.
The three recommended CDEs provide an abbreviated assessment of psychosocial risk and protection and have been used widely in the pediatric literature reviewed previously. Use of the recommended measures will serve as a screen for psychosocial risk and protective factors. However, such an abbreviated assessment is unlikely to capture the complexity of the interaction between multiple aspects of the social environment and recovery. The relationships among risk and protective factors and outcomes are complex, and consideration of any individual risk or protective factor in isolation is likely to provide an inaccurate understanding of its influence on cognitive, behavioral, or social recovery (Green et al. 2010). Recent research highlights the importance of considering the goodness of fit for various models of associations among multiple risk factors, including additive versus interactive effects.
Recommendations and Conclusions
Further research is needed to fully understand the relationship of the range of psychosocial risk and protective factors to cognitive and behavioral recovery over time. Longitudinal designs are critical for understanding the reciprocal relationships between social-environmental factors, such as family functioning, and child recovery over time. As illustrated by a growing number of studies (e.g., Taylor et al., 2001), these relationships are bidirectional and only sophisticated longitudinal designs can begin to tease out causality. Structural equation modeling, a statistical technique for testing hypothesized causal relationships between predictor and dependent variables, affords an approach to examining reciprocal relationships over time (Byrne, 2001; Yeates et al., 2004). Hierarchical linear models, or growth modeling, can also be a powerful approach to modeling the pattern of change in outcomes over time when there are incomplete data or unequal assessment intervals (Singer, 1998; Yeates et al., 2010).
Additional research on the role of risk and protective factors is likely to also have implications for intervention. Factors depicted in Bronfenbrenner's ecological framework (Fig. 1) and implicated in recovery from childhood TBI can be classified as modifiable and non-modifiable. For example, the fact that a child's parent has died or been incarcerated cannot be changed. However, one can potentially improve family functioning, strengthen family resources and supports, and promote positive parent–child interactions. Targeting modifiable risks and seeking to promote protective factors in the child's environment may facilitate resiliency (Masten, 2001; Wallander and Varni, 1998) and form the foundation for clinical interventions to improve cognitive behavioral outcomes following pediatric TBI (see Wade et al., 2009). Therefore, including risk and protective factors in pediatric TBI research will provide the evidence base needed to design treatments that will address critical modifiable risks and promote important protective factors.
Despite differing methodologies and measures, the existing literature provides consistent support for the importance of the social environment in recovery following childhood TBI. In many studies, social-environmental factors account for a greater portion of the variance in child behavioral outcomes than does the severity of the injury itself (e.g., Taylor et al., 2002). Consequently, any study examining recovery following pediatric TBI must assess potential psychosocial risk and protective factors. This recommendation is particularly valid if the investigators wish to understand the effects of specific interventions, as previous investigations have shown that environmental factors such as SES moderate and promote the effectiveness of interventions for TBI (Wade et al., 2006).
Acknowledgments
This project was jointly supported by the National Institutes of Health (National Institute of Neurological Disorders and Stroke; NIH/NINDS) and the United States Department of Education/National Institute on Disability and Rehabilitation Research (DOE/NIDRR) including NIDRR Rehabilitation Research and Training Center grant H133B090010.
Views expressed are those of the authors and do not necessarily reflect those of the agencies or institutions with which they are affiliated, including the United States Department of Veterans Affairs, the United States Department of Education, and the National Institutes of Health. This work is not an official document, guidance, or policy of the United States government, nor should any official endorsement be inferred.
Author Disclosure Statement
No competing financial interests exist.
References
- Anderson V. Catroppa C. Morse S. Haritou F. Rosenfeld J. Identifying factors contributing to child and family outcome at 30 months following traumatic brain injury in children. J. Neurol., Neurosurg. Psychiatry. 2005;76:401–408. doi: 10.1136/jnnp.2003.019174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyle M.H. Offord D.R. Hofmann H.G. Catlin G.P. Byles J.A. Cadman D.T. Crawford J.W. Links P.S. Rae–GGrant N.I. Szatmari P. Ontario Child Health Study: I. Methodology. Arch. Gen. Psychiatry. 1987;44:826–831. doi: 10.1001/archpsyc.1987.01800210078012. [DOI] [PubMed] [Google Scholar]
- Burgess E. S. Drotar D. Taylor H. G. Wade S. Stancin T. Yeates K. O. The Family Burden of Injury Interview: reliability and validity studies. J. Head Trauma Rehabil. 1999;14:394–405. doi: 10.1097/00001199-199908000-00008. [DOI] [PubMed] [Google Scholar]
- Bronfenbrenner U. The Ecology of Human Development. Harvard University Press; Cambridge, MA: 1979. [Google Scholar]
- Brown G. Chadwick O. Shaffer D. Rutter M. Traub M. A prospective study of children with head injuries: III. Psychiatric sequelae. Psychol. Med. 1981;11:63–78. doi: 10.1017/s0033291700053289. [DOI] [PubMed] [Google Scholar]
- Byrne B. M. Structural Equation Modeling with AMOS – Basic Concepts, Applications, and Programming. Lawrence Erlbaum Associates; Mahwah, NJ: 2001. [Google Scholar]
- Chadwick O. Rutter M. Brown G. Shaffer D. Traub M.U. A prospective study of children with head injuries: II. Cognitive sequelae. Psychol. Med. 1981a;11:49–61. doi: 10.1017/s0033291700053277. [DOI] [PubMed] [Google Scholar]
- Chadwick O. Rutter M. Shaffer D. Shrout P.E. A prospective study of children with head injuries: IV. Specific cognitive deficits. J. Clin. Neuropsychol. 1981b;3:101–120. doi: 10.1080/01688638108403117. [DOI] [PubMed] [Google Scholar]
- Chapman L.A. Wade S.L. Walz N.C. Taylor H.G. Stancin T. Yeates K.O. Clinically significant behavior problems during the initial 18 months following early childhood traumatic brain injury. Rehabil. Psychol. 2010;55:48–57. doi: 10.1037/a0018418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Copeland–Linder N. Lambert S.F. Ialongo N.S. Community violence, protective factors, and adolescent mental health. J. Clin. Child Adolesc. Psychol. 2010;39:176–186. doi: 10.1080/15374410903532601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garmezy N. Masten A.S. Tellegen A. The study of stress and competence in children: a building block for developmental psychopathology. Child Dev. 1984;55:97–111. [PubMed] [Google Scholar]
- Gerrard–Morris A. Taylor H.G. Yeates K.O. Walz N.C. Stancin T. Minich N. Wade S.L. Cognitive development after traumatic brain injury in young children. J. Int. Neuropsychol. Soc. 2009;16:1–12. doi: 10.1017/S1355617709991135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerring J.P. Brady K.D. Chen A. Vasa R. Grados M. Bandeen–Roche K.J. Bryan R.N. Denckla M.B. Premorbid prevalence of ADHD and development of secondary ADHD after closed head injury. J. Am. Acad. Child Adolesc. Psychiatry. 1998;37:647–654. doi: 10.1097/00004583-199806000-00015. [DOI] [PubMed] [Google Scholar]
- Gerring J.P. Grados M.A. Slomine B. Christensen J.R. Salorio C.F. Cole W.R. Vasa R.A. Disruptive behavior disorders and disruptive symptoms after severe paediatric traumatic brain injury. Brain Inj. 2009;23:944–955. doi: 10.3109/02699050903285531. [DOI] [PubMed] [Google Scholar]
- Grados M.A. Vasa R.A. Riddle M.A. Slomine B.S. Salorio C. Christensen J. Gerring J. New onset obsessive-compulsive symptoms in children and adolescents with severe traumatic brain injury. Depress. Anxiety. 2008;25:398–407. doi: 10.1002/da.20398. [DOI] [PubMed] [Google Scholar]
- Green J.G. McLaughlin K.A. Berglund P.A. Gruber M.J. Sampson N.A. Zaslavsky A.M. Kessler R.C. Childhood adversities and adult psychiatric disorders in the National Comorbidity Survey Replication I: Associations with first onset of DSM-IV disorders. Arch. Gen. Psychiatry. 2010;67:113–123. doi: 10.1001/archgenpsychiatry.2009.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halle T. Forry N. Hair E. Perper K. Wandner L. Wessel J. Vick J. Disparities in Early Learning and Development: Lessons from the Early Childhood Longitudinal Study-Birth Cohort (ECLS-B) Child Trends; Washington, DC: 2009. [Google Scholar]
- Kessler R.C. Davis C.G. Kendler K.S. Childhood and adult psychiatric disorder in the US National Comorbidity Survey. Psychol. Med. 1997;27:1101–1119. doi: 10.1017/s0033291797005588. [DOI] [PubMed] [Google Scholar]
- Luthar S.S. Cicchetti D. Becker B. The construct of resilience: a critical evaluation and guidelines for future work. Child Dev. 2000;71:543–562. doi: 10.1111/1467-8624.00164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maas A.I. Harrison–Felix C.L. Menon D. Adelson P.D. Balkin T. Bullock R. Engel D.C. Gordon W. Orman J.L. Lew H.L. Robertson C. Temkin N. Valadka A. Verfaellie M. Wainwright M. Wright D.W. Schwab K. Common data elements for traumatic brain injury: recommendations from the interagency working group on demographics and clinical assessment. Arch. Phys. Med. Rehabil. 2010;91:1641–1649. doi: 10.1016/j.apmr.2010.07.232. [DOI] [PubMed] [Google Scholar]
- Masten A.S. Ordinary magic: resilience processes in development. Am. Psychol. 2001;56:227–238. doi: 10.1037//0003-066x.56.3.227. [DOI] [PubMed] [Google Scholar]
- Masten A.S. Garmezy N. Tellegen A. Pellegrini D.S. Larkin D.S. Larkin K. Larsen A. Competence and stress in school children: the moderating effects of individual and family qualities. J. Child Psychol. Psychiatry. 1988;29:745–764. doi: 10.1111/j.1469-7610.1988.tb00751.x. [DOI] [PubMed] [Google Scholar]
- Max J.E. Levin H.S. Landis J. Schachar R. Saunders A. Ewing-Cobbs L. Chapman S.B. Dennis M. Predictors of personality change due to traumatic brain injury in children and adolescents in the first six months after injury. J. Am. Acad. Child Adolesc. Psych. 2005;44:434–442. doi: 10.1097/01.chi.0000156280.66240.61. [DOI] [PubMed] [Google Scholar]
- Max J.E. Schachar R.J. Levin H.S. Ewing–Cobbs L. Chapman S.B. Dennis M. Saunders A. Landis J. Predictors of attention-deficit/hyperactivity disorder within 6 months after pediatric traumatic brain injury. J. Am. Acad. Child Adolesc. Psychiatry. 2005a;44:1032–1040. doi: 10.1097/01.chi.0000173293.05817.b1. [DOI] [PubMed] [Google Scholar]
- Max J.E. Schacher R.J. Levin H.S. Ewing–Cobbs L. Chapman S.B. Dennis M. Saunders A. Landis J. Predictors of secondary attention-deficit/hyperactivity disorder in children and adolescents 6 to 24 months after traumatic brain injury. J. Am. Acad. Child Adolesc. Psychiatry. 2005b;44:1041–1049. doi: 10.1097/01.chi.0000173292.05817.f8. [DOI] [PubMed] [Google Scholar]
- McCauley S.R. Wilde E.A. Anderson V.A. Bedell G. Beers S.R. F C.T. Chapman S.B. Ewing–Cobbs L. Gerring J.P. Gioia G.A. Levin H.S. Michaud L.J. Prasad M.R. Swaine B.R. Turkstra L.S. Wade S.L. Yeates K.O. Recommendations for the use of common outcome measures in pediatric traumatic brain injury research. J Neurotrauma. 2011 doi: 10.1089/neu.2011.1838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller I. Bishop D. Epsten N. Keitner G. The McMaster Family Assessment Devise: reliability and validity. J. Marital Fam. Ther. 1985;11:345–356. [Google Scholar]
- Nadebaum C. Anderson V. Catroppa C. Executive function outcomes following traumatic brain injury in young children: a five year follow-up. Dev. Neuropsychol. 2007;32:703–728. doi: 10.1080/87565640701376086. [DOI] [PubMed] [Google Scholar]
- Prinz R.J. Foster S. Kent R.N. O'Leary K.D. Multivariate assessment of conflict in distressed and nondistressed mother–adolescent dyads. J. Appl. Behav. Anal. 1979;12:691–700. doi: 10.1901/jaba.1979.12-691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rivara J.B. Jaffe K.M. Fay G.C. Polissar N.L. Martin K.M. Shurtleff H.A. Liao S. Family functioning and injury severity as predictors of child functioning one year following traumatic brain injury. Arch. Phys. Med. Rehabil. 1993;74:1047–1055. doi: 10.1016/0003-9993(93)90060-n. [DOI] [PubMed] [Google Scholar]
- Rivara J.B. Jaffe K.M. Polissar N.L. Fay G.C. Martin K.M. Shurtleff H.A. Liao S. Family functioning and children's academic performance and behavior problems in the year following traumatic brain injury. Arch. Phys. Med. Rehabil. 1994;75:369–379. doi: 10.1016/0003-9993(94)90157-0. [DOI] [PubMed] [Google Scholar]
- Rutter M. Psychosocial resilience and protective mechanisms. Am. J. Orthopsychiatry. 1987;57:316–331. doi: 10.1111/j.1939-0025.1987.tb03541.x. [DOI] [PubMed] [Google Scholar]
- Rutter R. Chadwick O. Shaffer D. Brown G. A prospective study of children with head injuries: I. Design and methods. Psychol. Med. 1980;10:633–645. doi: 10.1017/s0033291700054933. [DOI] [PubMed] [Google Scholar]
- Singer J.D. Using SAS PROC MIXED to fit multilevel models, hierarchical models, and individual growth models. J. Educ. Behav. Stat. 1998;23:323–355. [Google Scholar]
- Stancin T. Drotar D. Taylor H.G. Yeates K.O. Wade S.L. Health related quality of life of children and adolescents following traumatic brain injury. Pediatrics (electronic version) 2002;109:e34. doi: 10.1542/peds.109.2.e34. [DOI] [PubMed] [Google Scholar]
- Stouthamer–Loeber M. Loeber R. Wei E. Risk and promotive effects in the explanation of persistent serious delinquency in boys. J. Consult. Clin. Psychol. 2002;70:11–123. doi: 10.1037//0022-006x.70.1.111. [DOI] [PubMed] [Google Scholar]
- Szatmari P. Shannon H.S. Offord D.R. Models of multiple risk: Psychiatric disorder and poor school performance. Int. J. Methods Psychiatr. Res. 1994;4:231–240. [Google Scholar]
- Taylor H.G. Yeates K.O. Wade S.L. Drotar D. Klein S. Stancin T. Influences on first-year recovery from traumatic brain injury in children. Neuropsychology. 1999;13:76–89. doi: 10.1037//0894-4105.13.1.76. [DOI] [PubMed] [Google Scholar]
- Taylor H.G. Yeates K.O. Wade S.L. Drotar D. Stancin T. Burant C. Bidirectional child–family influences on outcomes of traumatic brain injury in children. J. Int. Neuropsychol. Soc. 2001;7:755–767. doi: 10.1017/s1355617701766118. [DOI] [PubMed] [Google Scholar]
- Taylor H.G. Yeates K.O. Wade S.L. Drotar D. Stancin T. Minich N. A prospective study of short- and long-term outcomes after traumatic brain injury in children: behavior and achievement. Neuropsychology. 2002;16:15–27. doi: 10.1037//0894-4105.16.1.15. [DOI] [PubMed] [Google Scholar]
- Vasa R.A. Gerring J.P. Grados M. Slomine B. Christensen J.R. Rising W. Denckla M.B. Riddle M.A. Anxiety after severe pediatric closed head injury. J. Am. Acad. Child Adolesc. Psychiatry. 2002;41:148–156. doi: 10.1097/00004583-200202000-00008. [DOI] [PubMed] [Google Scholar]
- Wade S.L. Carey J. Wolfe C.R. The efficacy of an online cognitive-behavioral, family intervention in improving child behavior and social competence following pediatric brain injury. Rehabil. Psychol. 2006;51:179–189. [Google Scholar]
- Wade S.L. Cassedy A. Walz N.C. Taylor H.G. Stancin T. Yeates K.O. The relationship of parental warm responsiveness and negativity to emerging behavior problems following traumatic brain injury in young children. Dev. Psychol. 2011;47:119–133. doi: 10.1037/a0021028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wade S.L. Oberjohn K. Burkhardt A. Greenberg I. Preliminary feasibility and efficacy of a positive parenting intervention for young children with TBI. J. Head Trauma Rehabil. 2009;24:239–247. doi: 10.1097/HTR.0b013e3181ad6680. [DOI] [PubMed] [Google Scholar]
- Wallander J.L. Varni J.W. Effects of pediatric chronic physical disorders on child and family adjustment. J. Child Psychol. Psychiatry. 1998;39:29–46. [PubMed] [Google Scholar]
- Wells R. Minnes P. Phillips M. Predicting social and functional outcomes for individuals sustaining paediatric traumatic brain injury. Dev. Neurorehabil. 2009;12:12–23. doi: 10.1080/17518420902773109. [DOI] [PubMed] [Google Scholar]
- Yeates K.O. Swift E. Taylor H.G. Wade S.L. Drotar D. Stancin T. Minich N. Short- and long-term social outcomes following pediatric brain injury. J. Int. Neuropsychol. Soc. 2004;10:412–426. doi: 10.1017/S1355617704103093. [DOI] [PubMed] [Google Scholar]
- Yeates K.O. Taylor H.G. Drotar D. Wade S.L. Klein S. Stancin T. Schatschneider C. Pre-injury family environment as a determinant of recovery from traumatic brain injuries in school-age children. Int. J. Neuropsychol. 1997;3:617–630. [PubMed] [Google Scholar]
- Yeates K.O. Taylor H.G. Wade S.L. Drotar D. Stancin T. Minich N. A prospective study of short- and long-term neuropsychological outcomes after traumatic brain injury in children. Neuropsychology. 2002;16:514–523. doi: 10.1037//0894-4105.16.4.514. [DOI] [PubMed] [Google Scholar]
- Yeates K. O. Taylor H. G. Walz N. C. Stancin T. Wade S. L. The family environment as a moderator of psychosocial outcomes following traumatic brain injury in young children. Neuropsychology. 2010;24:345–356. doi: 10.1037/a0018387. [DOI] [PMC free article] [PubMed] [Google Scholar]