Abstract
This study was undertaken to evaluate outcomes for single (SLT) vs. bilateral lung transplantation (BLT) in patients with interstitial lung disease (ILD). One hundred and eleven patients with ILD who underwent lung transplantation between January 1993 and March 2009 were evaluated. Recipients with BLT were younger (43 ± 12 vs. 57 ± 7 years), and significantly more patients with non-idiopathic pulmonary fibrosis (IPF) received BLT (50%) vs. patients with IPF (18%). BLT recipients had a significantly longer mean waitlist time (240 vs. 125 days), significantly higher systolic (51 ± 18 vs. 40 ± 11 mmHg) pulmonary artery pressures, were placed on cardiopulmonary bypass more frequently (67 vs. 31%), had a higher incidence of primary graft dysfunction (63 vs. 17%), more frequently were given prolonged peri-operative inhaled nitric oxide and more frequently required prolonged post-operative mechanical ventilatory support (6.0 vs. 1.7 days). Additionally, BLT recipients had a significantly longer intensive care unit (8 vs. 4 days) and hospital (24 vs. 15 days) length of stay. We did not detect a difference in survival (Kaplan–Meier) for SLT vs. BLT. Our findings suggest that outcomes for SLT for patients with ILD are comparable or somewhat superior to those for BLT, and short- and long-term survival are not significantly different for the two procedures.
Keywords: Lung transplantation, Idiopathic pulmonary fibrosis, Interstitial lung disease, Lung allocation score, Single lung transplant, Bilateral lung transplant
INTRODUCTION
The interstitial lung diseases (ILD) comprise a heterogeneous group of diffuse parenchymal lung disorders that are often associated with significant lung fibrosis [1, 2]. Many of these disorders, especially idiopathic pulmonary fibrosis (IPF), are subacute or chronic conditions that can lead to respiratory insufficiency and death. IPF is the most commonly diagnosed form of idiopathic interstitial pneumonia, and epidemiologic studies have shown a significant incidence and prevalence rate for IPF and other forms of ILD that can lead to end-stage fibrosis [3]. Currently available pharmacologic therapies such as corticosteroids or cytotoxic agents may not arrest the disease process for many forms of ILD, especially if the diagnosis is IPF, and progressive respiratory failure and death is particularly likely to occur in patients with IPF [4]. The high failure rate of currently available treatments for advanced lung disease due to ILD makes alternative therapeutic options a necessity. Because of the poor outcomes with non-surgical therapies for advanced forms of ILD and particularly IPF, referral to a lung transplant centre has been recommended at the time of diagnosis [5].
Lung transplantation (LTX) is a therapeutic option for selected patients with severe ILD refractory to medical therapy that can potentially improve both the quality of life and survival [6]. According to the latest data from the International Society for Heart and Lung Transplantation (ISHLT), IPF represents 2.9% of heart–lung transplants, 29.1% of single lung transplantations (SLTs) and 14.5% of sequential bilateral lung transplants (BLTs) performed in the adult population [7]. Although many obstacles to LTX remain, such as the shortage of donor lungs, opportunistic infection or refractory/fatal allograft rejection and the recurrence of disease in the donor lung, LTX is the ultimate treatment for patients with progressive loss of pulmonary function due to progressive pulmonary fibrosis.
The question of which procedure provides optimum results for patients with ILD and, in particular patients with IPF, has generated a considerable amount of debate. One donor can benefit two recipients when SLT is performed, and SLT allows transplant to succeed when only one of two donor lungs is acceptable for transplant or when recipients have contraindications to lung implantation in one hemithorax due to severe pleural or chest wall issues. Additionally, SLT can have good functional outcomes and can be performed more rapidly and with less peri-operative complications than BLT. However, native lung complications such as opportunistic infection or pneumothorax may occur when SLT is performed for pulmonary fibrosis [8]. BLT can potentially provide improved functional outcomes and better long-term survival while eliminating the potential for complications to occur in a residual native lung, and recipients may be better able to tolerate chronic complications such as bronchiolitis obliterans syndrome (BOS). However, BLT is a more complicated operation that can be associated with increased peri-operative complications and early mortality, and if patients are listed for BLT only, they have an increased risk of dying on the waitlist [9]. It still remains controversial which procedure, SLT or BLT, is more beneficial to ILD patients.
The purpose of this study is to determine whether significant differences for SLT vs. BLT could be found in our cohort of patients with ILD and the subset of ILD patients with IPF. We examined our outcome data for recipient survival for SLT vs. BLT performed on patients with ILD and also analyzed these data for the subset of patients with IPF.
PATIENTS AND METHODS
Donor and recipient characteristics
Between January 1993 and March 2009, a total of 423 lung transplants from deceased donors were performed in 405 patients at UWHC. Among these patients, 111 (26.2%) consecutive patients with ILD (IPF = 79, sarcoidosis = 12, lymphangioleiomyomatosis = 4 and other forms of ILD = 16) underwent LTX. Primary graft dysfunction (PGD) was defined and graded according to the ISHLT definition: PaO2/FiO2 < 300 and a chest radiograph with a characteristic diffuse infiltrates [10]. BOS was also defined by ISHLT criteria [11]. Patient demographics, donor characteristics, graft function, post-transplant complications and patient and graft survival rates were assessed.
Organ procurement and preservation
After median sternotomy, 30 000 units of heparin and 10 mg of phentolamine were given intravenously to prevent vasospasm and to facilitate subsequent organ flushing. Four litres of preservative solution is infused in situ via the main pulmonary artery, and 2 l of retrograde flush through the pulmonary veins. The majority of our donors were perfused with UW solution, but since 2007 patients exclusively received Perfadex® (Vitrolife, Göteborg, Sweden) as the preservation solution. The lungs are then stored in the preservation solution at 4°C and returned to our centre.
Indication for single or bilateral lung transplantation
All patients with ILD are listed for either BLT or SLT to decrease the risk of death on the waitlist while awaiting transplantation [9]. Decisions are based on recipient variables as well as quality of the donor lungs. If donor lungs are considered marginal or if the donor is a donation after cardiac death donor, the recipient will likely receive both lungs. If the donor lung meets the standard criteria, we would not hesitate to use a single lung only to provide benefit to two recipients.
Statistical analysis
Categorical data were summarized with frequency distributions and percentages. The mean ± standard deviations were calculated for variables that were normally distributed, and the medians with IQRs were presented for those that were skewed. Continuous variables were compared by the unpaired t-test or non-parametric Mann–Whitney U-test, whereas nominal variables were compared by means of the χ2 or the Fisher's exact test, as appropriate. The Kaplan–Meier method was used to assess lung transplant patient survival, lung graft survival and freedom from airway complications and BOS. Log-rank tests were used to assess statistical significance in survival differences between the pre-LAS and LAS groups. A P-value of <0.05 (two-sided) was considered to be statistically significant. All analyses were performed using the SPSS statistical software program (SPSS for Windows version 17.0; SPSS Inc., Chicago, IL, USA).
RESULTS
The overall survival rate of the lung transplant recipients with IPF at 1, 3, 5 and 10 years were 82.3, 63.4, 63.4 and 40.1%, respectively. To evaluate the impact of the type of lung transplant procedure for ILD patients, the patients who underwent SLT (n = 81) were compared with those with BLT (n = 30). For the BLT group, the age of the recipients was significantly younger (P < 0.01); the proportion of those with a diagnosis of IPF was lower (P < 0.01), % predicted forced expiratory volume in 1 s (FEV1) was lower (P = 0.01) and the recipients had higher pulmonary artery pressure (P < 0.01), when compared with the SLT recipients (Table 1). The waiting time for transplant was significantly longer (P = 0.03), the utilization of cardiopulmonary bypass was more frequent (P < 0.01) and the cold ischemic time was longer (P < 0.01) in the BLT recipients.
Table 1:
Patient demographics for SLT vs. BLT
| Parameter | SLT (n = 81) | BLT (n = 30) | P-value |
|---|---|---|---|
| Age (years) | 56.8 ± 7.2 | 43.4 ± 12.3 | <0.01 |
| Gender (females) | 19 (23.5%) | 9 (30.0%) | 0.48 |
| Race (Caucasian) | 75 (95.6%) | 30 (100%) | 0.31 |
| BMI (kg/m2) | 27 ± 4.0 | 26 ± 5.0 | 0.20 |
| Diagnosis | <0.01 | ||
| IPF | 65 (80.2%) | 14 (46.7%) | |
| Non-IPF | 16 (19.8%) | 16 (53.3%) | |
| Pulmonary function | |||
| FVC (% of predicted) | 48 ± 17 | 44 ± 16 | 0.34 |
| FEV1 (% of predicted) | 50 ± 18 | 41 ± 15 | 0.01 |
| Required oxygen (l) | 4 ± 3 | 5 ± 4 | 0.74 |
| Continuous mechanical ventilation | 1 (1.2%) | 3 (10.0%) | 0.06 |
| Haemodynamics | |||
| Systolic PAP (mmHg) | 40 ± 11 | 51 ± 18 | <0.01 |
| Mean PAP (mmHg) | 26 ± 8 | 36 ± 13 | <0.01 |
| PCWP (mmHg) | 12 ± 8 | 17 ± 9 | 0.39 |
| Cardiac index (l/min/m2) | 2.8 ± 0.6 | 3.1 ± 1.0 | 0.06 |
| Serum creatinine (mg/dl) | 1.0 ± 0.2 | 0.9 ± 0.3 | 0.20 |
| History of diabetes | 19 (23.4%) | 4 (13.3%) | 0.24 |
| History of smoking | 51 (63.0%) | 12 (40.0%) | 0.03 |
| Time on waiting list (days) | 125 (IQR, 33–331) | 240 (IQR, 115–473) | 0.03 |
| LAS estimation | 40.7 (IQR, 37.0–46.2) | 38.8 (IQR, 34.8–53.0) | 0.78 |
| Cardiopulmonary bypass | 25 (30.9%) | 20 (66.7%) | <0.01 |
| Cold ischemic time (min) | 344 ± 124 | 435 ± 115 | <0.01 |
| Donor age (years) | 33.2 ± 13.2 | 33.7 ± 14.3 | 0.99 |
| Donor gender (females) | 23 (28.4%) | 10 (33.3%) | 0.61 |
| Donor (Caucasian) | 66 (81.5%) | 27 (90.0%) | 0.55 |
SLT, single lung transplant; BLT, bilateral lung transplant; BMI, body mass index; IPF, idiopathic pulmonary fibrosis; PF, pulmonary fibrosis; FVC, forced vital capacity; FEV1, forced expiratory volume in 1 s; PAP, pulmonary arterial pressure; PCWP, pulmonary capillary wedge pressure; IQR, interquartile range.
In regard to post-operative outcomes, the BLT recipients had a higher incidence of PGD (grade 2 or 3, P < 0.01). BLT recipients also required more prolonged iNO, mechanical ventilator support and intensive care unit (ICU) and hospital stay (P < 0.01). However, the hospital mortality was not statistically different between the two procedures (7.4% in SLT vs. 13.3% in BLT, P = 0.46, Table 2).
Table 2:
Post-operative outcomes for SLT vs. BLT
| Parameter | SLT (n = 81) | BLT (n = 30) | P-value |
|---|---|---|---|
| PGD | <0.01 | ||
| Grade 0 or 1 | 67 (82.7%) | 11 (36.7%) | |
| Grade 2 or 3 | 14 (17.3%) | 19 (63.3%) | |
| Required ECMO support | 3 (3.7%) | 0 (0%) | 0.56 |
| Inhalation of nitric oxide | 43 (53.1%) | 18 (60.0%) | 0.52 |
| ≥48 h of inhalation | 13 (16.0%) | 13 (43.3%) | <0.01 |
| Reintubation | 16 (19.8%) | 9 (30.0%) | 0.25 |
| Mechanical ventilated period (days) | 1.7 (IQR, 1.0–4.0) | 6.0 (IQR, 2.6–20) | <0.01 |
| ≥48 h of ventilator support | 17 (30.4%) | 34 (61.8%) | <0.01 |
| Reoperation | 7 (8.6%) | 3 (10.0%) | >0.99 |
| Dialysis | 1 (1.2%) | 2 (6.7%) | 0.18 |
| Length of ICU stay (days) | 4 (IQR, 3–9) | 8 (IQR, 6–24) | <0.01 |
| Length of hospital stay (days) | 15 (IQR, 10–25) | 24 (IQR, 16–48) | <0.01 |
| Hospital mortality | 6 (7.4%) | 4 (13.3%) | 0.46 |
| Readmission <30 days | 21 (25.9%) | 8 (26.7%) | 0.94 |
ECMO, extracorporeal membrane oxygenation; IQR, interquartile range; ICU, intensive care unit.
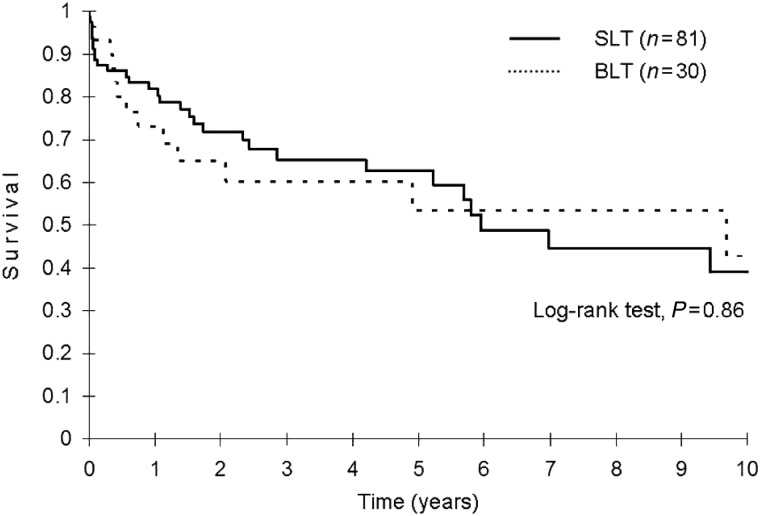
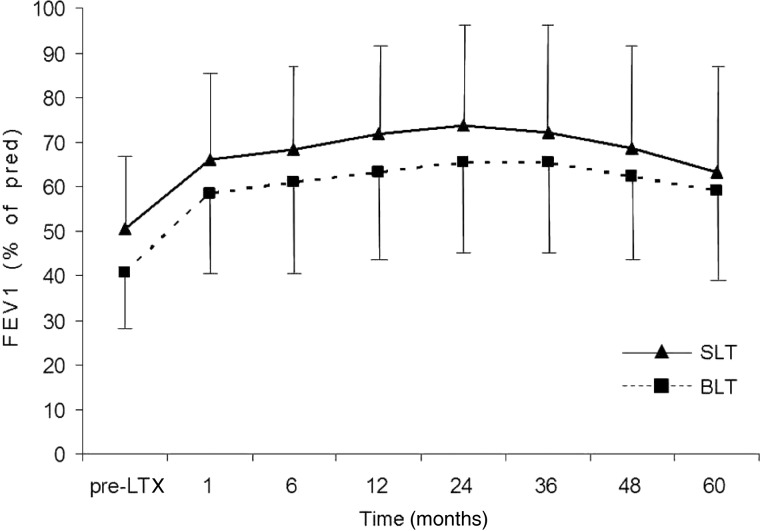
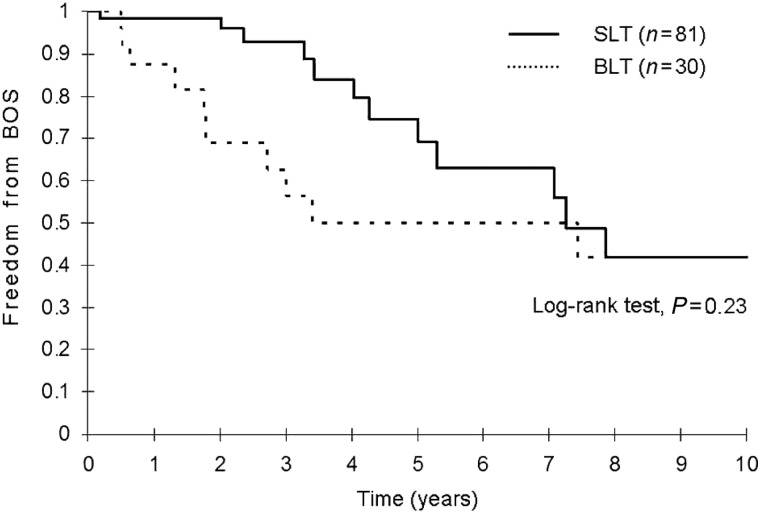
The post-transplant survival rates at 1, 3, 5 and 10 years were not different between the two procedures (81.8, 65.4, 62.7 and 39.0% in SLT vs. 73.0, 60.2, 53.5 and 42.8% in BLT, P = 0.86, Fig. 1). The post-transplant % of predicted FEV1 and freedom from BOS were not statistically different for BLT vs. SLT recipients (Figs 2 and 3). Similarly, post-transplant survival for the subset of patients with IPF as their transplant indication was not significant for SLT vs. BLT. The 1-, 3-, 5- and 10-year survival rates for SLT were 81.7, 65.1, 65.1 and 48.5%, and the 1-, 3-, 5- and 10-year survival rates for BLT were 85.7, 55.1, 55.1 and 55.1% (Fig. 4).
Figure 1:
Post-transplant survival after SLT and BLT for ILD by the Kaplan-Meier analysis. SLT, single lung transplant; BLT, bilateral lung transplant.
Figure 2:
Per cent of predicted forced expiratory volume in 1 s after lung transplant for ILD. SLT, single lung transplant; BLT, bilateral lung transplant.
Figure 3:
Freedom from BOS after SLT and BLT for ILD by the Kaplan-Meier analysis. SLT, single lung transplant; BLT, bilateral lung transplant.
Figure 4:
Post-transplant survival after SLT and BLT for IPF by the Kaplan-Meier analysis. SLT, single lung transplant; BLT, bilateral lung transplant.
DISCUSSION
Our analysis of the data for SLT vs. BLT recipients also revealed some interesting trends. Patients who received BLT were significantly younger, had higher pre-transplant pulmonary artery pressure, had increased cold ischemia time and more frequently required cardiopulmonary bypass support vs. SLT recipients. BLT was more frequently performed for non-IPF ILD than for recipients with IPF. Patients who underwent BLT had a significantly prolonged wait time that was double that for SLT recipients. Our cohort was too small to assess the risk of death on the waitlist for patients listed for BLT only, but an analysis of UNOS data by Nathan et al. [9] has shown that patients listed for BLT only are at increased risk of dying without receiving donor lungs. Interestingly, although BLT recipients required significantly more prolonged nitric oxide administration, more prolonged mechanical ventilation and had longer length of stay in the ICU and considerably prolonged hospital length of stay, we did not detect any significant difference in post-transplant survival for BLT vs. SLT recipients.
Although some centres have reported worse survival outcomes for IPF patients receiving SLT vs. BLT [12, 13], other reports that comprise a more comprehensive data set suggest that post-transplant survival for patients undergoing SLT is not significantly different than that for BLT for patients with IPF [14]. Thabut et al. [14] examined survival for 2146 patients who received SLT for IPF vs. 1181 who received BLT between 1987 and 2009 and concluded that survival was not significantly different for SLT vs. BLT, but the data showed short-term worsened survival for BLT vs. SLT but long-term benefit for BLT.
Our data do not show a negative impact of SLT on overall survival when compared with BLT for our entire cohort of ILD patients. Similarly, although the number of IPF patients who received a BLT was only 14 vs. 65 patients who received SLT, a similar survival pattern was found for recipients with IPF, which are consistent with other reports in the literature [13, 14], although high-risk patients [those with high lung allocation scores (LASs)] have been suggested to have better survival with BLT vs. SLT [12]. Weiss et al. [15] have also found that high-LASs correlate with lower short-term survival for patients with pulmonary fibrosis. Unfortunately, our patient cohort was not large enough to detect a significant impact of LAS on overall survival or outcomes for SLT vs. BLT.
Limitations of this study include the retrospective analysis of our data. Our clinical data were obtained by the chart review, which has inherent limitations that include access and accuracy of the recorded data. Additionally, as a retrospective observational study, it can be subject to selection bias and incomplete data collection. However, the data used in the analysis were all prospectively obtained in our transplant database for all ILD patients.
In summary, we found no significant difference in post-transplant survival for SLT vs. BLT recipients. Our data and data published by other investigators indicate that for the subset of transplant candidates with ILD, outcomes with SLT are acceptable. SLT may pose less risk for older patients, particularly when significant co-morbidities are present. However, BLT may be a preferable operation for younger patients, especially if significant pulmonary hypertension is present. As shown by Nathan et al. [9], however, listing for BLT only vs. SLT or BLT can increase wait time and may place a potential recipient with fibrotic lung disease at increased risk for death while awaiting transplant. Additional clinical research is needed to determine if significant differences in outcomes exist for patients with high LAS values who undergo SLT vs. BLT.
FUNDING
This research was supported in part by the George and Julie Mosher Pulmonary Research Fund at the University of Wisconsin School of Medicine and Public Health.
Conflict of interest: none declared.
REFERENCES
- 1.Kim R, Meyer KC. Therapies of interstitial lung disease—past, present, and future. Ther Adv Respir Dis. 2008;2:319–38. doi: 10.1177/1753465808096948. [DOI] [PubMed] [Google Scholar]
- 2.ATS/ERS. International Multidisciplinary Consensus Classification of the Idiopathic Interstitial Pneumonias. Am J Respir Crit Care Med. 2002;165:277–304. doi: 10.1164/ajrccm.165.2.ats01. [DOI] [PubMed] [Google Scholar]
- 3.Raghu G, Weycker D, Edelsberg J, Bradford WZ, Oster G. Incidence and prevalence of idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2006;174:810–6. doi: 10.1164/rccm.200602-163OC. [DOI] [PubMed] [Google Scholar]
- 4.Kim DS, Collard HR, King TE., Jr Classification and natural history of the idiopathic interstitial pneumonias. Proc Am Thorac Soc. 2006;3:285–92. doi: 10.1513/pats.200601-005TK. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Orens JB, Estenne M, Arcasoy S, Conte JV, Corris P, Egan JJ, et al. International guidelines for the selection of lung transplant candidates: 2006 update—a consensus report from the Pulmonary Scientific Council of the International Society for Heart and Lung Transplantation. J Heart Lung Transplant. 2006;25:745–55. doi: 10.1016/j.healun.2006.03.011. [DOI] [PubMed] [Google Scholar]
- 6.Thabut G, Mal H, Castier Y, Groussard O, Brugiere O, Marrash-Chahla R, et al. Survival benefit of lung transplantation for patients with idiopathic pulmonary fibrosis. J Thorac Cardiovasc Surg. 2003;126:469–75. doi: 10.1016/s0022-5223(03)00600-7. [DOI] [PubMed] [Google Scholar]
- 7.Christie JD, Edwards LB, Aurora P, Dobbels F, Kirk R, Rahmel AO, et al. The Registry of the International Society for Heart and Lung Transplantation: Twenty-sixth Official Adult Lung and Heart-Lung Transplantation Report-2009. J Heart Lung Transplant. 2009;28:1031–49. doi: 10.1016/j.healun.2009.08.004. [DOI] [PubMed] [Google Scholar]
- 8.King CS, Khandhar S, Burton N, Shlobin OA, Ahmad S, Lefrak E, et al. Native lung complications in single-lung transplant recipients and the role of pneumonectomy. J Heart Lung Transplant. 2009;28:851–6. doi: 10.1016/j.healun.2009.04.023. [DOI] [PubMed] [Google Scholar]
- 9.Nathan SD, Shiobin OA, Burton AS, Barnett SD, Edwards E. Comparison of wait times and mortality for idiopathic pulmonary fibrosis patients listed for single or bilateral lung transplantation. J Heart Lung Transplant. 2010;29:1165–71. doi: 10.1016/j.healun.2010.05.014. [DOI] [PubMed] [Google Scholar]
- 10.Christie JD, Carby M, Bag R, Corris P, Hertz M, Weill D ISHLT Working Group on Primary Lung Graft Dysfunction. Report of the ISHLT working group on primary lung graft dysfunction. Part II: Definition. A consensus statement of the International Society for Heart and Lung Transplantation. J Heart Lung Transplant. 2005;24:1454–9. doi: 10.1016/j.healun.2004.11.049. [DOI] [PubMed] [Google Scholar]
- 11.Cooper JD, Billingham M, Egan T, Hertz MI, Higenbottam T, Lynch J, et al. A working formulation for the standardization of nomenclature and for clinical staging of chronic dysfunction in lung allografts. International Society for Heart and Lung Transplantation. J Heart Lung Transplant. 1993;12:713–6. [PubMed] [Google Scholar]
- 12.Weiss ES, Allen JG, Merlo CA, Conte JV, Shah AS. Survival after single versus bilateral lung transplantation for high-risk patients with pulmonary fibrosis. Ann Thorac Surg. 2009;88:1616–25. doi: 10.1016/j.athoracsur.2009.06.044. [DOI] [PubMed] [Google Scholar]
- 13.Force SD, Kilgo P, Neujahr DC, Pelaez A, Pickens A, Fernandez FG, et al. Bilateral lung transplantation offers better long-term survival, compared with single-lung transplantation, for younger patients with idiopathic pulmonary fibrosis. Ann Thorac Surg. 2011;91:244–9. doi: 10.1016/j.athoracsur.2010.08.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Thabut G, Christie JD, Ravaud P, Castier Y, Dauriate G, Jebrak G, et al. Survival after bilateral versus single-lung transplantation for idiopathic pulmonary fibrosis. Ann Intern Med. 2009;151:767–74. doi: 10.7326/0003-4819-151-11-200912010-00004. [DOI] [PubMed] [Google Scholar]
- 15.Weiss ES, Allen JG, Merlo CA, Conte JV, Shah AS. Lung allocation score predicts survival in lung transplantation patients with pulmonary fibrosis. Ann Thorac Surg. 2009;88:1757–64. doi: 10.1016/j.athoracsur.2009.07.005. [DOI] [PubMed] [Google Scholar]